Principles of Wound Management in Clinical Environment
VerifiedAdded on 2023/06/10
|24
|8587
|441
AI Summary
The case study discusses burn injury and the wound healing process. It also covers skin assessment, pain management, surgical wound debridement, skin grafting, and common complications in wound assessment. The study material is relevant for healthcare professionals and students studying wound management principles in clinical environment.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Apply principles of wound management in
the clinical environment
123 TMP E – Assessment Template – Written v1.3 Page 1 of 24
the clinical environment
123 TMP E – Assessment Template – Written v1.3 Page 1 of 24
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

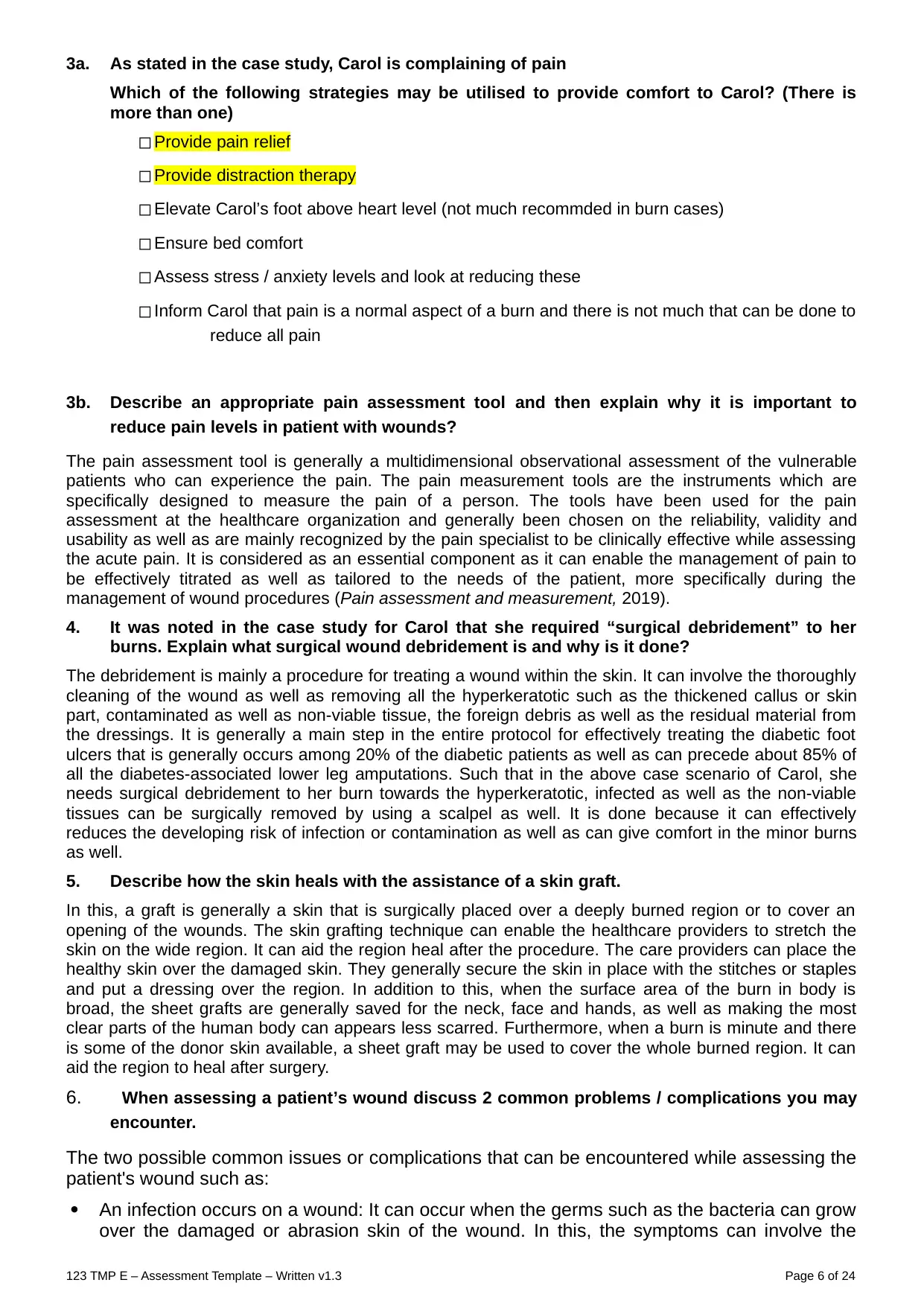
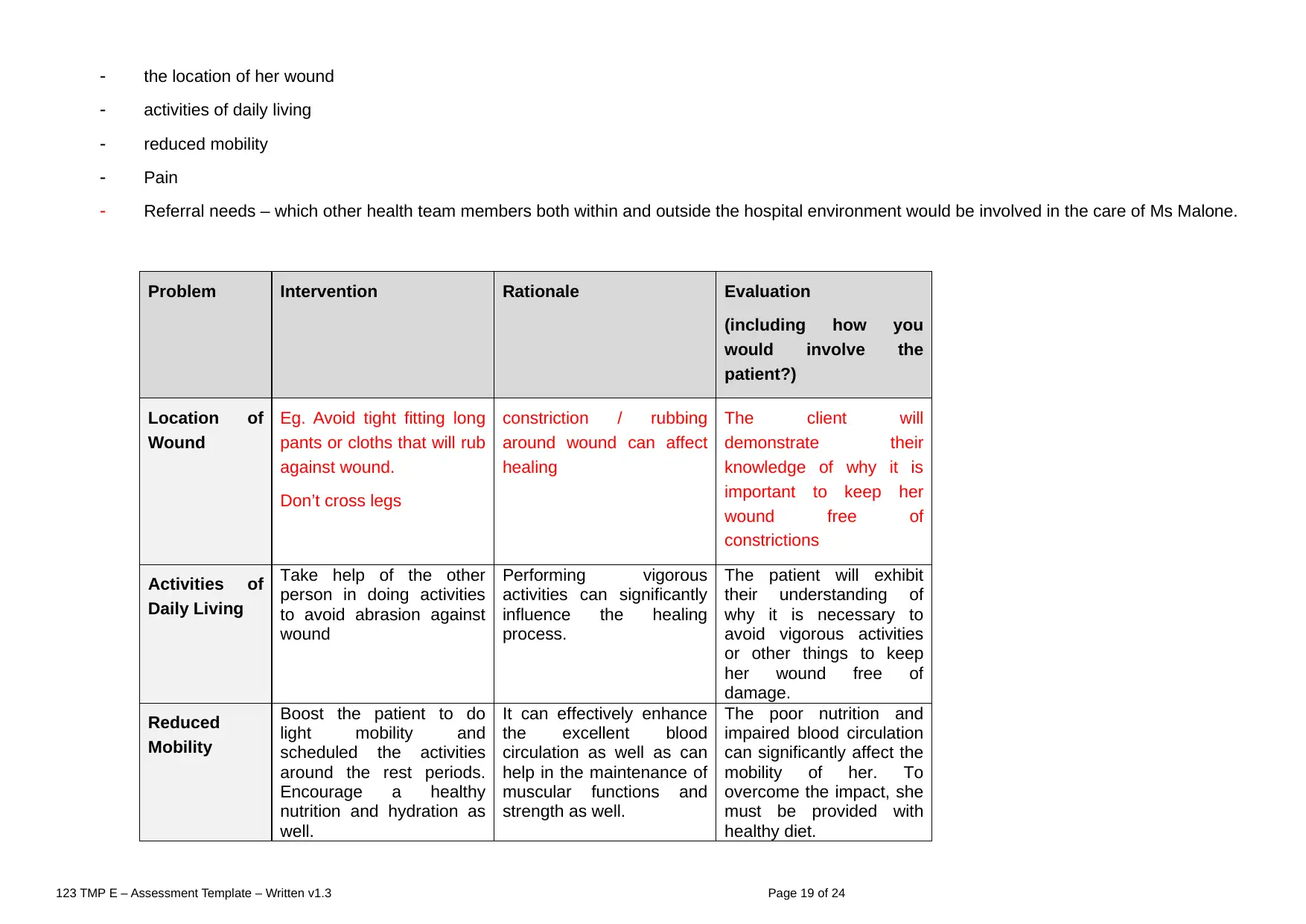
Case Study Scenario 1 – Burn Injury:
Carol Mitchell, aged 64 was admitted to the burns unit after sustaining burns to the front and back of her left
lower leg and foot. Carol had been cooking in her kitchen, when she accidently knocked a saucepan full of hot
oil over herself. Carol’s husband drove her to the nearest medical centre where Carol’s burn was treated and
then she was transported by ambulance to the hospital for further assessment.
15595171 / Bork / shutterstock.com
In the emergency room, Carol was conscious and in evident distress. Her admission notes were: areas of
variable depth of injury over her posterior lower leg and foot only; dark pink discoloration with sluggish capillary
refill, blistering is evident; an area on her inner left ankle has an area of blotchy red/white with sluggish to
absent capillary refill, patient is complaining of pain on her lower leg, but states that her ankle is somewhat
pain free.
After consultation with the Burns team, the burns are to be surgically debrided and a small skin graft will be
applied to her inner ankle injury.
123 TMP E – Assessment Template – Written v1.3 Page 2 of 24
Carol Mitchell, aged 64 was admitted to the burns unit after sustaining burns to the front and back of her left
lower leg and foot. Carol had been cooking in her kitchen, when she accidently knocked a saucepan full of hot
oil over herself. Carol’s husband drove her to the nearest medical centre where Carol’s burn was treated and
then she was transported by ambulance to the hospital for further assessment.
15595171 / Bork / shutterstock.com
In the emergency room, Carol was conscious and in evident distress. Her admission notes were: areas of
variable depth of injury over her posterior lower leg and foot only; dark pink discoloration with sluggish capillary
refill, blistering is evident; an area on her inner left ankle has an area of blotchy red/white with sluggish to
absent capillary refill, patient is complaining of pain on her lower leg, but states that her ankle is somewhat
pain free.
After consultation with the Burns team, the burns are to be surgically debrided and a small skin graft will be
applied to her inner ankle injury.
123 TMP E – Assessment Template – Written v1.3 Page 2 of 24
Case Study 1 - Short answer questions: word count and referencing stated where
required
Read each question carefully and ensure you answer each part.
1. The wound healing process commences when any damage to the skin
has occurred. Once the skin is impaired and a wound is created the
healing process begins. This is a dynamic and complex process. It consists
of four stages
Match the stage with the physiological and biochemical processes
haemostasis – stage 1
inflammation phase – stage 2
proliferation or reconstruction phase – stage 3
maturation phase – stage 4.
Stage Physiological and Biochemical Processes
proliferation or reconstruction
phase – stage 3 During this phase tissue is temporarily replaced and the area is cleaned up b
macrophages which digest the dead bacteria and debris. New blood capillaries ar
developed and granulation tissue (mainly collagen) is laid down. As granulation tissu
continues to be laid the epithelium thickens to 4 to 5 layers forming the epidermis. Th
wound contracts and becomes smaller. This stage can take from 2 to 24 days
inflammation phase – stage 2 Process of the wound being closed by clotting. Starts when blood leaks out of th
body. The first step is when blood vessels constrict to restrict the blood flow. Nex
platelets stick together in order to seal the break in the wall of the blood vessel. Finall
coagulation occurs and reinforces the platelet plug with threads of fibrin which are lik
a molecular binding agent, this stage happens very quickly
homeostasis – stage 1 Vasodilation of surrounding tissues occurs due to the release of histamine and othe
vasoactive chemicals. This increases blood flow to the surrounding areas which lead
erythema, swelling, heat and pain. White blood cells descend into the area as
defense response. This phase lasts approximately three days
maturation phase – stage 4 The wound and surrounding tissue is gradually remodeled and the collagen cells lai
down are strengthened. This stage can last from 24 days to approximately one yea
During this stage the wound is still at risk and should be protected.
123 TMP E – Assessment Template – Written v1.3 Page 3 of 24
required
Read each question carefully and ensure you answer each part.
1. The wound healing process commences when any damage to the skin
has occurred. Once the skin is impaired and a wound is created the
healing process begins. This is a dynamic and complex process. It consists
of four stages
Match the stage with the physiological and biochemical processes
haemostasis – stage 1
inflammation phase – stage 2
proliferation or reconstruction phase – stage 3
maturation phase – stage 4.
Stage Physiological and Biochemical Processes
proliferation or reconstruction
phase – stage 3 During this phase tissue is temporarily replaced and the area is cleaned up b
macrophages which digest the dead bacteria and debris. New blood capillaries ar
developed and granulation tissue (mainly collagen) is laid down. As granulation tissu
continues to be laid the epithelium thickens to 4 to 5 layers forming the epidermis. Th
wound contracts and becomes smaller. This stage can take from 2 to 24 days
inflammation phase – stage 2 Process of the wound being closed by clotting. Starts when blood leaks out of th
body. The first step is when blood vessels constrict to restrict the blood flow. Nex
platelets stick together in order to seal the break in the wall of the blood vessel. Finall
coagulation occurs and reinforces the platelet plug with threads of fibrin which are lik
a molecular binding agent, this stage happens very quickly
homeostasis – stage 1 Vasodilation of surrounding tissues occurs due to the release of histamine and othe
vasoactive chemicals. This increases blood flow to the surrounding areas which lead
erythema, swelling, heat and pain. White blood cells descend into the area as
defense response. This phase lasts approximately three days
maturation phase – stage 4 The wound and surrounding tissue is gradually remodeled and the collagen cells lai
down are strengthened. This stage can last from 24 days to approximately one yea
During this stage the wound is still at risk and should be protected.
123 TMP E – Assessment Template – Written v1.3 Page 3 of 24
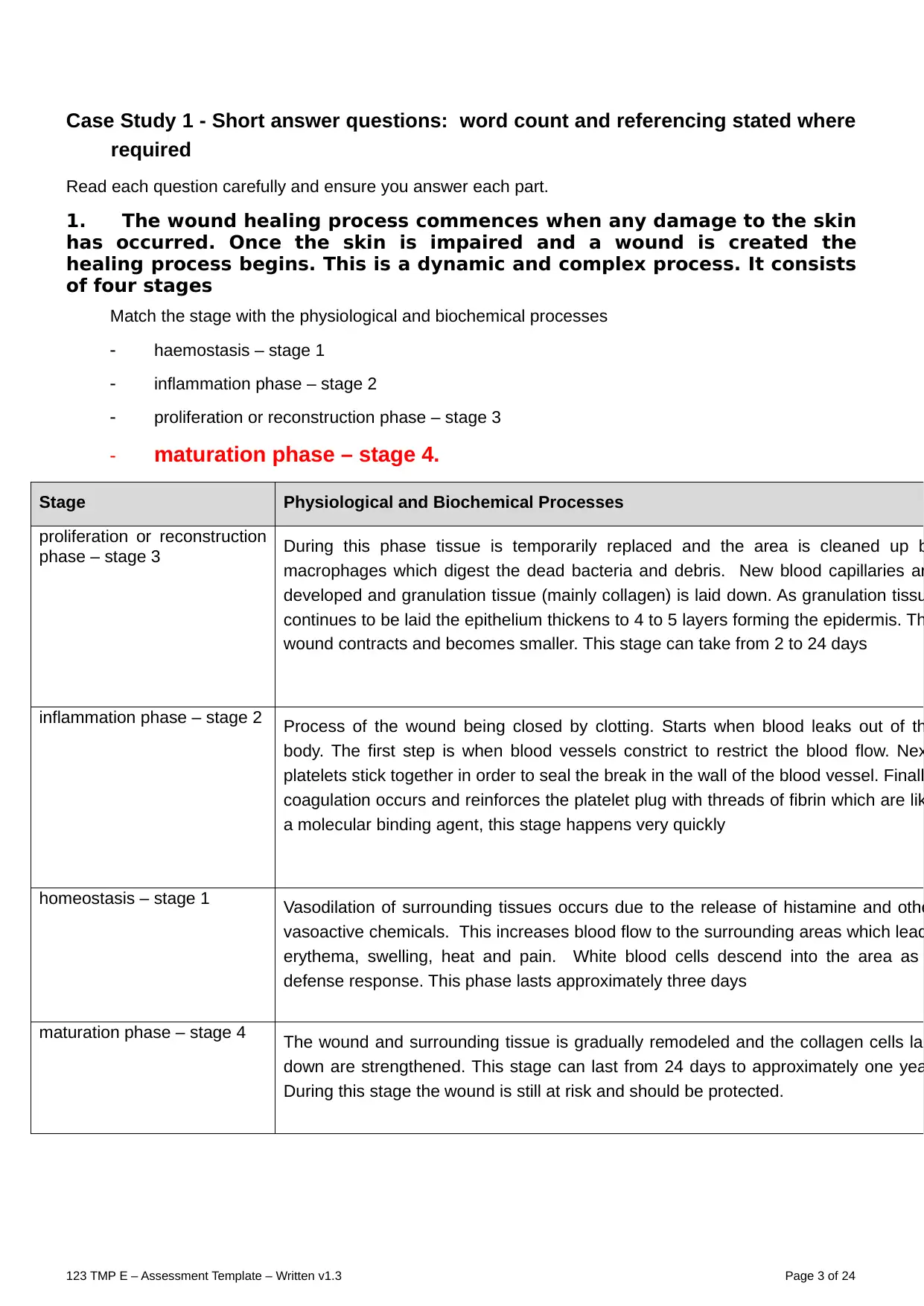
2a. Skin Assessment – outline the steps of the skin assessment for Carol’s burn that would be
carried out immediately on admission to the emergency department.
The burn assessment in Carol's burn case can include the assessment of airways, breathing,
circulation, disability, exposure as well as the requirement for the resuscitation of the fluids. In the
emergency department, the care nurses must visualize Carol's burn that can be sustained while the
victim accidentally knocked a saucepan which is full of hot oil over herself. As per the rule of nine, the
surface area of the body can be categorized into an anatomical area which can represent the 9%, or
multiple of 9% of overall body surface. However, the 9% each of the head and each of the upper limb,
about 18% for each lower limb, front of trunk as well as the back of trunk. The care nurse may consider
the depth of burn. As the burn wounds are generally dynamic and need a re-assessment within the first
24 to 72 hours because the depth can enhance as a result of an inadequate care treatments or a
supper-added contamination.
https://patient.info/doctor/burns-assessment-and-management
2b. Part of the assessment (here is a clue for the above question) is burn size. Using the burn
chart (below), tick the correct estimate of the size of Carol’s burn using the information in
the scenario
◻ Burn percentage 20% approx.
◻ Burn percentage 9% approx.
◻ Burn percentage 27% approx.
◻ Burn percentage 0.7% approx.
224297740 / stihii / shutterstock.com
2c. When a patient suffers a burn injury it is important to classify the wound.
Provide a description for each of the classifications in the table below.
Classification Description
123 TMP E – Assessment Template – Written v1.3 Page 4 of 24
carried out immediately on admission to the emergency department.
The burn assessment in Carol's burn case can include the assessment of airways, breathing,
circulation, disability, exposure as well as the requirement for the resuscitation of the fluids. In the
emergency department, the care nurses must visualize Carol's burn that can be sustained while the
victim accidentally knocked a saucepan which is full of hot oil over herself. As per the rule of nine, the
surface area of the body can be categorized into an anatomical area which can represent the 9%, or
multiple of 9% of overall body surface. However, the 9% each of the head and each of the upper limb,
about 18% for each lower limb, front of trunk as well as the back of trunk. The care nurse may consider
the depth of burn. As the burn wounds are generally dynamic and need a re-assessment within the first
24 to 72 hours because the depth can enhance as a result of an inadequate care treatments or a
supper-added contamination.
https://patient.info/doctor/burns-assessment-and-management
2b. Part of the assessment (here is a clue for the above question) is burn size. Using the burn
chart (below), tick the correct estimate of the size of Carol’s burn using the information in
the scenario
◻ Burn percentage 20% approx.
◻ Burn percentage 9% approx.
◻ Burn percentage 27% approx.
◻ Burn percentage 0.7% approx.
224297740 / stihii / shutterstock.com
2c. When a patient suffers a burn injury it is important to classify the wound.
Provide a description for each of the classifications in the table below.
Classification Description
123 TMP E – Assessment Template – Written v1.3 Page 4 of 24
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Superficial The superficial burn wound can involve only the epidermal layers of the skin.
these generally do not blister but are very painful, red, blanch with pressure,
and dry as well. in this, the slight alterations within the air current moving past
to the exposed superficial burn can cause a patient to experience a
excruciating pain.
Partial thickness The partial thickness is generally the second degree burn which can include
the epidermis as well as a part of the dermis layer of the skin. the site of the
burn can appear blistered, red as well as can be swollen and painful as well.
the burn can cause a mild pain and slight discomfort, specifically when
something like a cloth rubbing against the burned area.
Full thickness In the full thickness burns, the skin of a patient either be black, white, brown,
leathery in appearance and many more. in this, in the burn it can frequently
form an eschar around the wound. since the nerve endings are generally
damaged along with the dermis, and these such types of wound are quite
painless (Full Thickness Burns are a Life- Threatening Injury that require
medical attention, 2018).
State which one would most likely apply to Carol’s area of her burn around her inner left
ankle and give a rationale for your choice.
From the above scenario of Carol’s area of burn, it is identified that her injury can involve a full
thickness type of burn wound. it is because the nerve endings are mainly responsible for the sensations
that are damaged. From her case scenario, it is analyzed that the third degree burn can damage the
epidermis and dermis of a patient.
2d. When undertaking a wound assessment, the main purpose is to optimize the healing
process and to produce a baseline status against which the healing process can be
measured
Outline four (4) aspects you may consider when conducting a holistic wound assessment.
Provide a reason for each of your choices.
In this, a holistic wound assessment can include the medical history of a patient, consisting the current
and past medical conditions, it can also include the psychological, social as well as the spiritual history,
their wound care environment as well as can assess to the specialized well-being care services. the
wound healing process can include the four phases which are as mentioned below:
Hemostasis Stage: It is generally an easy pathway to identify that the body has started the hemostasis
stage is that the blood will begin to clot. if a patient can experience a break within the skin as well as are
begin to bleed, then their blood vessels will work to constrict the flow of blood. the platelets then
generally stick collaboratively to seal the break within the skin.
Inflammatory Stage: This particular stage can occur right when the skin can break. when a person gets
injured, then their blood vessels begin to leak, and swelling can occur. In this, the swelling as well as
inflammation can aid to control the bleed as well as can prevent the infections. the white blood cells
known as Neutrophils that can enter the wound to remove the bacteria and debris as well.
Proliferative Stage: It is mainly the third stage, when the wound can rebuild itself as well as the new
skin can rise the new tissue oxygen and nutrients as well. in this, the cells known as fibroblast can work
to effectively heal the wound by gripping the edges of the wound as well as pull them combined.
Maturation Stage: It is the stage also known as remodeling stage is when the collagen within the skin is
regenerated as well as the wound can completely close. in context with earlier stage, the collagen which
can rebuild the skin is generally uneven and thick as well. within the maturation stage, the collagen fibre
can begin to align more efficiently with each other as well as can lie more close combined to cross-link
(Wound Care Stage, 2021).
123 TMP E – Assessment Template – Written v1.3 Page 5 of 24
these generally do not blister but are very painful, red, blanch with pressure,
and dry as well. in this, the slight alterations within the air current moving past
to the exposed superficial burn can cause a patient to experience a
excruciating pain.
Partial thickness The partial thickness is generally the second degree burn which can include
the epidermis as well as a part of the dermis layer of the skin. the site of the
burn can appear blistered, red as well as can be swollen and painful as well.
the burn can cause a mild pain and slight discomfort, specifically when
something like a cloth rubbing against the burned area.
Full thickness In the full thickness burns, the skin of a patient either be black, white, brown,
leathery in appearance and many more. in this, in the burn it can frequently
form an eschar around the wound. since the nerve endings are generally
damaged along with the dermis, and these such types of wound are quite
painless (Full Thickness Burns are a Life- Threatening Injury that require
medical attention, 2018).
State which one would most likely apply to Carol’s area of her burn around her inner left
ankle and give a rationale for your choice.
From the above scenario of Carol’s area of burn, it is identified that her injury can involve a full
thickness type of burn wound. it is because the nerve endings are mainly responsible for the sensations
that are damaged. From her case scenario, it is analyzed that the third degree burn can damage the
epidermis and dermis of a patient.
2d. When undertaking a wound assessment, the main purpose is to optimize the healing
process and to produce a baseline status against which the healing process can be
measured
Outline four (4) aspects you may consider when conducting a holistic wound assessment.
Provide a reason for each of your choices.
In this, a holistic wound assessment can include the medical history of a patient, consisting the current
and past medical conditions, it can also include the psychological, social as well as the spiritual history,
their wound care environment as well as can assess to the specialized well-being care services. the
wound healing process can include the four phases which are as mentioned below:
Hemostasis Stage: It is generally an easy pathway to identify that the body has started the hemostasis
stage is that the blood will begin to clot. if a patient can experience a break within the skin as well as are
begin to bleed, then their blood vessels will work to constrict the flow of blood. the platelets then
generally stick collaboratively to seal the break within the skin.
Inflammatory Stage: This particular stage can occur right when the skin can break. when a person gets
injured, then their blood vessels begin to leak, and swelling can occur. In this, the swelling as well as
inflammation can aid to control the bleed as well as can prevent the infections. the white blood cells
known as Neutrophils that can enter the wound to remove the bacteria and debris as well.
Proliferative Stage: It is mainly the third stage, when the wound can rebuild itself as well as the new
skin can rise the new tissue oxygen and nutrients as well. in this, the cells known as fibroblast can work
to effectively heal the wound by gripping the edges of the wound as well as pull them combined.
Maturation Stage: It is the stage also known as remodeling stage is when the collagen within the skin is
regenerated as well as the wound can completely close. in context with earlier stage, the collagen which
can rebuild the skin is generally uneven and thick as well. within the maturation stage, the collagen fibre
can begin to align more efficiently with each other as well as can lie more close combined to cross-link
(Wound Care Stage, 2021).
123 TMP E – Assessment Template – Written v1.3 Page 5 of 24
3a. As stated in the case study, Carol is complaining of pain
Which of the following strategies may be utilised to provide comfort to Carol? (There is
more than one)
◻ Provide pain relief
◻ Provide distraction therapy
◻ Elevate Carol’s foot above heart level (not much recommded in burn cases)
◻ Ensure bed comfort
◻ Assess stress / anxiety levels and look at reducing these
◻ Inform Carol that pain is a normal aspect of a burn and there is not much that can be done to
reduce all pain
3b. Describe an appropriate pain assessment tool and then explain why it is important to
reduce pain levels in patient with wounds?
The pain assessment tool is generally a multidimensional observational assessment of the vulnerable
patients who can experience the pain. The pain measurement tools are the instruments which are
specifically designed to measure the pain of a person. The tools have been used for the pain
assessment at the healthcare organization and generally been chosen on the reliability, validity and
usability as well as are mainly recognized by the pain specialist to be clinically effective while assessing
the acute pain. It is considered as an essential component as it can enable the management of pain to
be effectively titrated as well as tailored to the needs of the patient, more specifically during the
management of wound procedures (Pain assessment and measurement, 2019).
4. It was noted in the case study for Carol that she required “surgical debridement” to her
burns. Explain what surgical wound debridement is and why is it done?
The debridement is mainly a procedure for treating a wound within the skin. It can involve the thoroughly
cleaning of the wound as well as removing all the hyperkeratotic such as the thickened callus or skin
part, contaminated as well as non-viable tissue, the foreign debris as well as the residual material from
the dressings. It is generally a main step in the entire protocol for effectively treating the diabetic foot
ulcers that is generally occurs among 20% of the diabetic patients as well as can precede about 85% of
all the diabetes-associated lower leg amputations. Such that in the above case scenario of Carol, she
needs surgical debridement to her burn towards the hyperkeratotic, infected as well as the non-viable
tissues can be surgically removed by using a scalpel as well. It is done because it can effectively
reduces the developing risk of infection or contamination as well as can give comfort in the minor burns
as well.
5. Describe how the skin heals with the assistance of a skin graft.
In this, a graft is generally a skin that is surgically placed over a deeply burned region or to cover an
opening of the wounds. The skin grafting technique can enable the healthcare providers to stretch the
skin on the wide region. It can aid the region heal after the procedure. The care providers can place the
healthy skin over the damaged skin. They generally secure the skin in place with the stitches or staples
and put a dressing over the region. In addition to this, when the surface area of the burn in body is
broad, the sheet grafts are generally saved for the neck, face and hands, as well as making the most
clear parts of the human body can appears less scarred. Furthermore, when a burn is minute and there
is some of the donor skin available, a sheet graft may be used to cover the whole burned region. It can
aid the region to heal after surgery.
6. When assessing a patient’s wound discuss 2 common problems / complications you may
encounter.
The two possible common issues or complications that can be encountered while assessing the
patient's wound such as:
An infection occurs on a wound: It can occur when the germs such as the bacteria can grow
over the damaged or abrasion skin of the wound. In this, the symptoms can involve the
123 TMP E – Assessment Template – Written v1.3 Page 6 of 24
Which of the following strategies may be utilised to provide comfort to Carol? (There is
more than one)
◻ Provide pain relief
◻ Provide distraction therapy
◻ Elevate Carol’s foot above heart level (not much recommded in burn cases)
◻ Ensure bed comfort
◻ Assess stress / anxiety levels and look at reducing these
◻ Inform Carol that pain is a normal aspect of a burn and there is not much that can be done to
reduce all pain
3b. Describe an appropriate pain assessment tool and then explain why it is important to
reduce pain levels in patient with wounds?
The pain assessment tool is generally a multidimensional observational assessment of the vulnerable
patients who can experience the pain. The pain measurement tools are the instruments which are
specifically designed to measure the pain of a person. The tools have been used for the pain
assessment at the healthcare organization and generally been chosen on the reliability, validity and
usability as well as are mainly recognized by the pain specialist to be clinically effective while assessing
the acute pain. It is considered as an essential component as it can enable the management of pain to
be effectively titrated as well as tailored to the needs of the patient, more specifically during the
management of wound procedures (Pain assessment and measurement, 2019).
4. It was noted in the case study for Carol that she required “surgical debridement” to her
burns. Explain what surgical wound debridement is and why is it done?
The debridement is mainly a procedure for treating a wound within the skin. It can involve the thoroughly
cleaning of the wound as well as removing all the hyperkeratotic such as the thickened callus or skin
part, contaminated as well as non-viable tissue, the foreign debris as well as the residual material from
the dressings. It is generally a main step in the entire protocol for effectively treating the diabetic foot
ulcers that is generally occurs among 20% of the diabetic patients as well as can precede about 85% of
all the diabetes-associated lower leg amputations. Such that in the above case scenario of Carol, she
needs surgical debridement to her burn towards the hyperkeratotic, infected as well as the non-viable
tissues can be surgically removed by using a scalpel as well. It is done because it can effectively
reduces the developing risk of infection or contamination as well as can give comfort in the minor burns
as well.
5. Describe how the skin heals with the assistance of a skin graft.
In this, a graft is generally a skin that is surgically placed over a deeply burned region or to cover an
opening of the wounds. The skin grafting technique can enable the healthcare providers to stretch the
skin on the wide region. It can aid the region heal after the procedure. The care providers can place the
healthy skin over the damaged skin. They generally secure the skin in place with the stitches or staples
and put a dressing over the region. In addition to this, when the surface area of the burn in body is
broad, the sheet grafts are generally saved for the neck, face and hands, as well as making the most
clear parts of the human body can appears less scarred. Furthermore, when a burn is minute and there
is some of the donor skin available, a sheet graft may be used to cover the whole burned region. It can
aid the region to heal after surgery.
6. When assessing a patient’s wound discuss 2 common problems / complications you may
encounter.
The two possible common issues or complications that can be encountered while assessing the
patient's wound such as:
An infection occurs on a wound: It can occur when the germs such as the bacteria can grow
over the damaged or abrasion skin of the wound. In this, the symptoms can involve the
123 TMP E – Assessment Template – Written v1.3 Page 6 of 24
enhanced pain, redness and swelling as well. In addition to this, the more severe
contamination can cause nausea, fever or chills as well.
A blood infection: The infection of blood is also known as sepsis that is a serious
complication of the septicemia. It is generally a life-threatening issue of an infection or
contamination. Sepsis can occurs when the released chemicals within the bloodstream to
fight against an infection which can trigger the inflammation via all over the body.
Case study
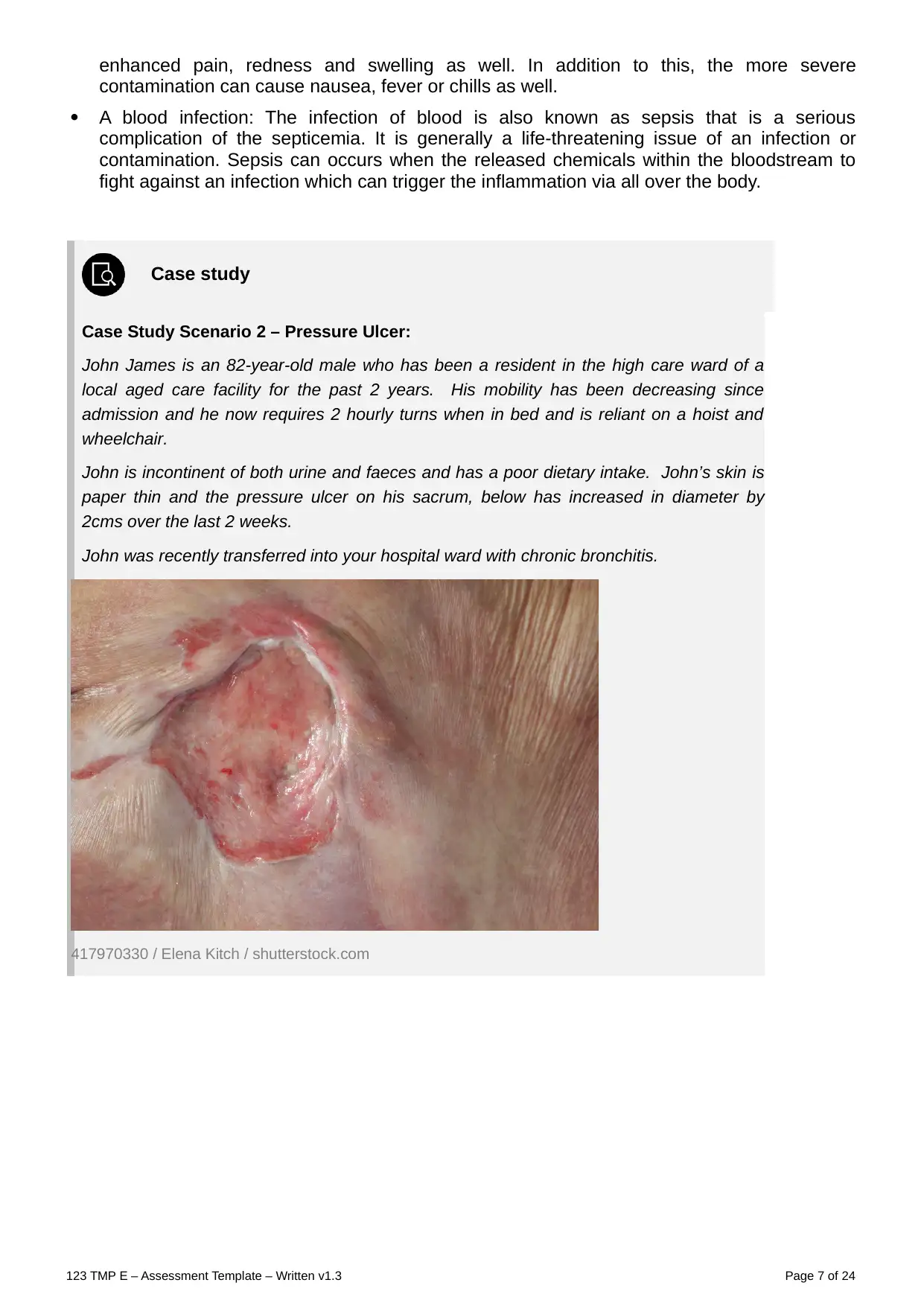
Case Study Scenario 2 – Pressure Ulcer:
John James is an 82-year-old male who has been a resident in the high care ward of a
local aged care facility for the past 2 years. His mobility has been decreasing since
admission and he now requires 2 hourly turns when in bed and is reliant on a hoist and
wheelchair.
John is incontinent of both urine and faeces and has a poor dietary intake. John’s skin is
paper thin and the pressure ulcer on his sacrum, below has increased in diameter by
2cms over the last 2 weeks.
John was recently transferred into your hospital ward with chronic bronchitis.
417970330 / Elena Kitch / shutterstock.com
123 TMP E – Assessment Template – Written v1.3 Page 7 of 24
contamination can cause nausea, fever or chills as well.
A blood infection: The infection of blood is also known as sepsis that is a serious
complication of the septicemia. It is generally a life-threatening issue of an infection or
contamination. Sepsis can occurs when the released chemicals within the bloodstream to
fight against an infection which can trigger the inflammation via all over the body.
Case study
Case Study Scenario 2 – Pressure Ulcer:
John James is an 82-year-old male who has been a resident in the high care ward of a
local aged care facility for the past 2 years. His mobility has been decreasing since
admission and he now requires 2 hourly turns when in bed and is reliant on a hoist and
wheelchair.
John is incontinent of both urine and faeces and has a poor dietary intake. John’s skin is
paper thin and the pressure ulcer on his sacrum, below has increased in diameter by
2cms over the last 2 weeks.
John was recently transferred into your hospital ward with chronic bronchitis.
417970330 / Elena Kitch / shutterstock.com
123 TMP E – Assessment Template – Written v1.3 Page 7 of 24
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Case Study 2 - Short answer questions: word count and referencing stated where
required
Read each question carefully and ensure you answer each part.
1a. You have been asked to attend to the dressing of John’s wound. What would be a suitable
dressing to use on John’s wound? (you must give a rationale for your choice).
Type of dressing: From the above case scenario, the care nurse must provide him a hydrocolloid
dressings that can include a gel which can supports the growth of a new skin cells within the ulcer, while
maintaining the surrounding skin dry. In this the other types of dressing can involve such as foam,
hydrofibres, gels and antimicrobial dressings can also be used (Treatment Pressure Ulcer, 2020).
Rationale: The pressure region care are generally an essential part of the nursing practice. While
handling the patients having such ulcers, it is identified that patients preferences must be taken in to
consideration is also important factor.
1b. Explain the goal of this treatment as per Q1a – what are you trying to achieve by
maintaining a moist wound environment.
The decubitus ulcers are also known as the bedsores or the pressure ulcers are the soft and skin tissue
harms which can form as an outcome of the constant or a prolonged pressure that is exerted on the skin.
These such ulcers can occur at the bony regions of the human body like ischium, greater trochanter,
heel, sacrum and many other as well. The possible goal of the specific care treatment is to reduce the
pressure which is being exerted over the ulcer, reduces the contact of the ulcer with a hard surface,
reduces the moisture as well as to keep it as a aseptic or least septic as possible. The goal is not only to
keep the integrity of the skin but can also to give the vulnerable patient-centered plan of a care that is
geared towards the positive results (Pressure Injury/Ulcer Risk Assessment, 2018).
1c. Explain whether John required a primary or secondary dressing, or both, and provide a
rationale for your choice.
The primary dressing is generally a therapeutic or a protective covering that can be applied directly over
the wound on the skin or can be caused by an opening to the skin as well.
The secondary dressing are generally the material which can serve as a protective or a therapeutic
function as well as are required to secure a primary dressing as well. As per the above case scenario,
the care treatment of the patient having pressure ulcer is generally a two folds consisting the relief of the
pressure generally allied with the management of wound (Hydrocolloid dressing for treating pressure
ulcers, 2018).
2a. Most infections agents are micro-organisms, these include: – (choose one answer)
◻ Bacteria, viruses, Soil, protozoa and prions
◻ Bacteria, Candida, fungi, protozoa and prions
◻ Bacteria, viruses, fungi, protozoa and prions
◻ Bacteria, viruses, fungi, protozoa and dust
2b. Match the common fungal infections with their major reservoir
Common fungal infection: Candida albicans, Aspergillus organisms
Common fungal infection Major reservoir
123 TMP E – Assessment Template – Written v1.3 Page 8 of 24
required
Read each question carefully and ensure you answer each part.
1a. You have been asked to attend to the dressing of John’s wound. What would be a suitable
dressing to use on John’s wound? (you must give a rationale for your choice).
Type of dressing: From the above case scenario, the care nurse must provide him a hydrocolloid
dressings that can include a gel which can supports the growth of a new skin cells within the ulcer, while
maintaining the surrounding skin dry. In this the other types of dressing can involve such as foam,
hydrofibres, gels and antimicrobial dressings can also be used (Treatment Pressure Ulcer, 2020).
Rationale: The pressure region care are generally an essential part of the nursing practice. While
handling the patients having such ulcers, it is identified that patients preferences must be taken in to
consideration is also important factor.
1b. Explain the goal of this treatment as per Q1a – what are you trying to achieve by
maintaining a moist wound environment.
The decubitus ulcers are also known as the bedsores or the pressure ulcers are the soft and skin tissue
harms which can form as an outcome of the constant or a prolonged pressure that is exerted on the skin.
These such ulcers can occur at the bony regions of the human body like ischium, greater trochanter,
heel, sacrum and many other as well. The possible goal of the specific care treatment is to reduce the
pressure which is being exerted over the ulcer, reduces the contact of the ulcer with a hard surface,
reduces the moisture as well as to keep it as a aseptic or least septic as possible. The goal is not only to
keep the integrity of the skin but can also to give the vulnerable patient-centered plan of a care that is
geared towards the positive results (Pressure Injury/Ulcer Risk Assessment, 2018).
1c. Explain whether John required a primary or secondary dressing, or both, and provide a
rationale for your choice.
The primary dressing is generally a therapeutic or a protective covering that can be applied directly over
the wound on the skin or can be caused by an opening to the skin as well.
The secondary dressing are generally the material which can serve as a protective or a therapeutic
function as well as are required to secure a primary dressing as well. As per the above case scenario,
the care treatment of the patient having pressure ulcer is generally a two folds consisting the relief of the
pressure generally allied with the management of wound (Hydrocolloid dressing for treating pressure
ulcers, 2018).
2a. Most infections agents are micro-organisms, these include: – (choose one answer)
◻ Bacteria, viruses, Soil, protozoa and prions
◻ Bacteria, Candida, fungi, protozoa and prions
◻ Bacteria, viruses, fungi, protozoa and prions
◻ Bacteria, viruses, fungi, protozoa and dust
2b. Match the common fungal infections with their major reservoir
Common fungal infection: Candida albicans, Aspergillus organisms
Common fungal infection Major reservoir
123 TMP E – Assessment Template – Written v1.3 Page 8 of 24
Aspergillus organisms Soil, dust, mouth, skin, colon, genital tract
Candida albicans Mouth, skin, colon, genital tract
2c. Match the common viral infections with their major reservoir.
Common viral infections Viral infection, Hepatitis A virus, Hepatitis B virus, Hepatitis C virus,
Human immunodeficiency virus (HIV), Herpes simplex virus (type I)
Common viral infection Major reservoir
Viral infection Reservoir
Hepatitis A virus Faeces
Human
immunodeficiency
virus
Blood and body fluids
Hepatitis C virus Blood
Hepatitis B virus Blood, semen, vaginal secretions (also isolated in saliva, tears,
urine and breast milk, but not proved to be sources of
transmission)
Herpes simplex virus Lesions of mouth or skin, saliva, genitalia plus herpes zoster
(shingles) or viral warts or herpangina (oral ulcers)
123 TMP E – Assessment Template – Written v1.3 Page 9 of 24
Candida albicans Mouth, skin, colon, genital tract
2c. Match the common viral infections with their major reservoir.
Common viral infections Viral infection, Hepatitis A virus, Hepatitis B virus, Hepatitis C virus,
Human immunodeficiency virus (HIV), Herpes simplex virus (type I)
Common viral infection Major reservoir
Viral infection Reservoir
Hepatitis A virus Faeces
Human
immunodeficiency
virus
Blood and body fluids
Hepatitis C virus Blood
Hepatitis B virus Blood, semen, vaginal secretions (also isolated in saliva, tears,
urine and breast milk, but not proved to be sources of
transmission)
Herpes simplex virus Lesions of mouth or skin, saliva, genitalia plus herpes zoster
(shingles) or viral warts or herpangina (oral ulcers)
123 TMP E – Assessment Template – Written v1.3 Page 9 of 24
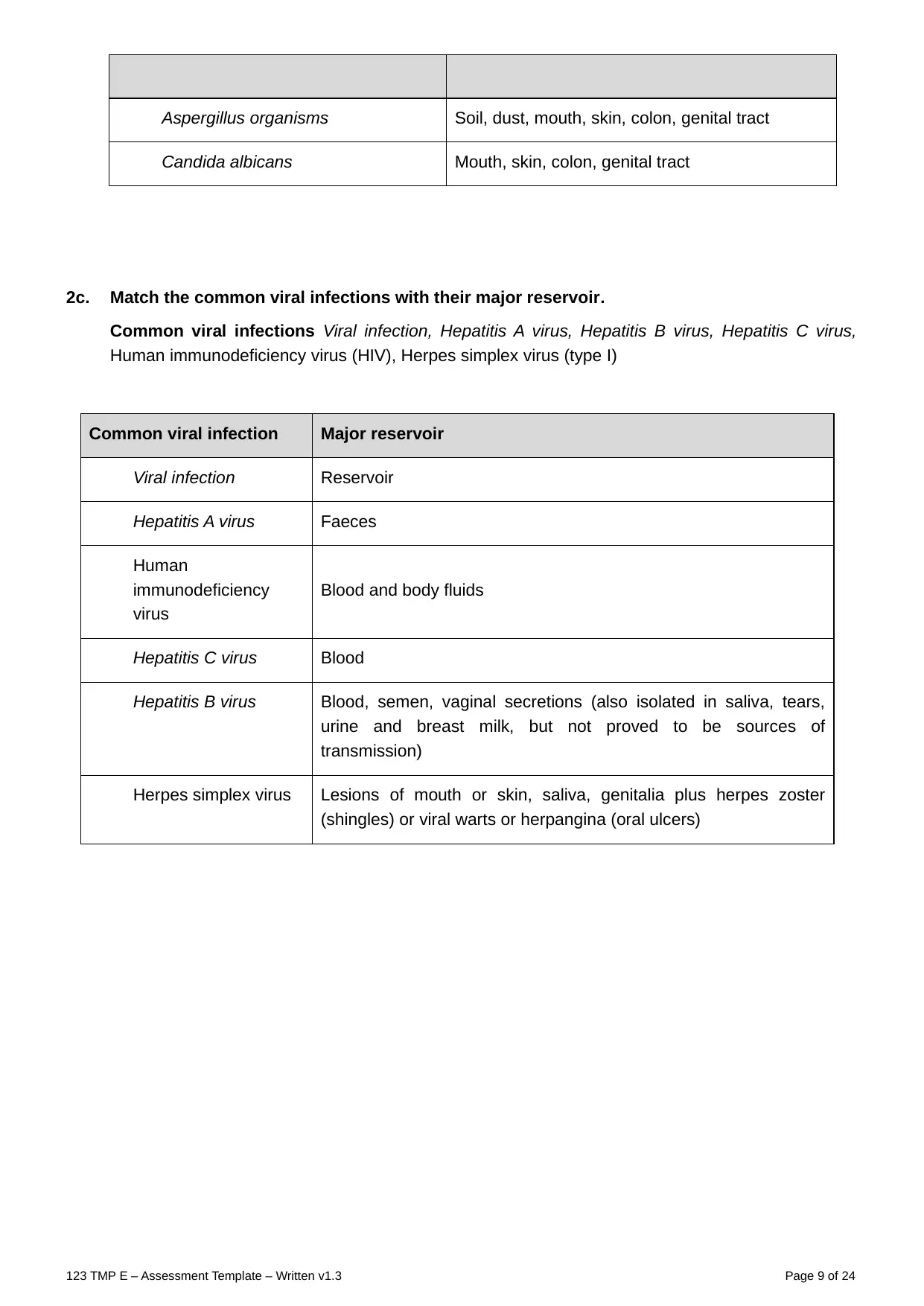
2d. On the picture below, place an X on each of the areas that pressure sores can develop (if
your computer doesn’t allow you to do this, you may write the answers underneath).
The pressure sores can be developed on the back or the sides of a head, the shoulder blades, lower
back or hips or can be tail bone, the ankle, heel as well as the skin behind the knees, back of the arms
and legs where they rest against the chair, shoulder blades and spine as well.
132726884 / Anna Rassadnikova / shutterstock.com
Discuss 4 pressure relieving devices that may be used for John either in hospital or when he
goes back to the aged care facility.
The pressure relieving devices which can be used in John's case when he goes back to an aged care
facility such as:
Crash mats
Hip and elbow pads
Pressure relieving mattresses
Pressure cushions for elder people (Using Pressure Relieveing Equipment In a Care Home,
2018).
3. Match the Ulcer type with their specific characteristic
Ulcer type: Venous ulcers, Diabetic ulcers, Arterial ulcers, Pressure ulcer:
Ulcer type Characteristic
Arterial ulcers Caused by ischemia; related to the presence of arterial occlusive
disease; symptoms include pain and tissue loss
Venous ulcers Local losses of epidermis and various levels of dermis and
subcutaneous tissue, occurring over or near the malleoli at the
distal lower extremities; caused by edema and other sequalae of
impaired venous return.
Diabetic ulcers Caused by trauma or pressure secondary to neuropathy or
vascular disease related to diabetes mellitus.
123 TMP E – Assessment Template – Written v1.3 Page 10 of 24
your computer doesn’t allow you to do this, you may write the answers underneath).
The pressure sores can be developed on the back or the sides of a head, the shoulder blades, lower
back or hips or can be tail bone, the ankle, heel as well as the skin behind the knees, back of the arms
and legs where they rest against the chair, shoulder blades and spine as well.
132726884 / Anna Rassadnikova / shutterstock.com
Discuss 4 pressure relieving devices that may be used for John either in hospital or when he
goes back to the aged care facility.
The pressure relieving devices which can be used in John's case when he goes back to an aged care
facility such as:
Crash mats
Hip and elbow pads
Pressure relieving mattresses
Pressure cushions for elder people (Using Pressure Relieveing Equipment In a Care Home,
2018).
3. Match the Ulcer type with their specific characteristic
Ulcer type: Venous ulcers, Diabetic ulcers, Arterial ulcers, Pressure ulcer:
Ulcer type Characteristic
Arterial ulcers Caused by ischemia; related to the presence of arterial occlusive
disease; symptoms include pain and tissue loss
Venous ulcers Local losses of epidermis and various levels of dermis and
subcutaneous tissue, occurring over or near the malleoli at the
distal lower extremities; caused by edema and other sequalae of
impaired venous return.
Diabetic ulcers Caused by trauma or pressure secondary to neuropathy or
vascular disease related to diabetes mellitus.
123 TMP E – Assessment Template – Written v1.3 Page 10 of 24
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Pressure ulcer Caused by pressure which destroys soft tissue
4. As John is quite elderly and his mobility has decreased, outline 3 risk assessments you can
do, and using your research state 2 common risk assessment tools used in Australia.
Three risk assessments that can be done to aid elder people such as:
The 30-Second Chair Stand Test.
Orthostatic Blood Pressure
Allen Cognitive Screen
The very two risk assessment tools that are used in Australia are such as (Pressure Injury prevention
risk assessment, 2022):
The Braden Scale.
The Waterlow Score
5. There are four stages of pressure ulcer formation and each stage has its noted
characteristics.
Match the stage with the presentation.
Stage: Stage 1, stage 2, stage 3, stage 4.
Stage Presentation
Stage 1 pressure injuries present as shiny or dry shallow ulcers without
any bruising present
Stage 3 Pressure injuries are the most severe and represent full-thickness
tissue loss with exposed bone, tendon or muscle
Stage 4 pressure injuries present as areas of persistent, non-blanch able
redness when compared with the surrounding skin
Stage 2 Pressure injuries represent full-thickness skin loss. Subcutaneous
fat may be visible, but bone, tendons or muscle are not exposed.
From the case scenario of John, it is identified that his pressure ulcer formation is generally at stage 2, it
is because his ulcer can presents a full-thickness skin loss. His subcutaneous fat can be visible, but the
bone, tendon or the muscles are not still exposed (How to recognize the four stages of pressure ulcer,
2017).
6. When the nurse is assessing Johns wound, he/she documents what it looks like using a
variety of methods.
Choose from the following words and fill in the blanks with words that match them to the
sentences.
Probe, marking pen, wound tracing, a ruler, written consent, transparent acetate grid,
clinical wound photography, wound measurement.
Probe provides the most accurate and objective means of assessment and evaluation of wound
treatments. wound tracing can be used to provide an accurate measurement of the length and
123 TMP E – Assessment Template – Written v1.3 Page 11 of 24
4. As John is quite elderly and his mobility has decreased, outline 3 risk assessments you can
do, and using your research state 2 common risk assessment tools used in Australia.
Three risk assessments that can be done to aid elder people such as:
The 30-Second Chair Stand Test.
Orthostatic Blood Pressure
Allen Cognitive Screen
The very two risk assessment tools that are used in Australia are such as (Pressure Injury prevention
risk assessment, 2022):
The Braden Scale.
The Waterlow Score
5. There are four stages of pressure ulcer formation and each stage has its noted
characteristics.
Match the stage with the presentation.
Stage: Stage 1, stage 2, stage 3, stage 4.
Stage Presentation
Stage 1 pressure injuries present as shiny or dry shallow ulcers without
any bruising present
Stage 3 Pressure injuries are the most severe and represent full-thickness
tissue loss with exposed bone, tendon or muscle
Stage 4 pressure injuries present as areas of persistent, non-blanch able
redness when compared with the surrounding skin
Stage 2 Pressure injuries represent full-thickness skin loss. Subcutaneous
fat may be visible, but bone, tendons or muscle are not exposed.
From the case scenario of John, it is identified that his pressure ulcer formation is generally at stage 2, it
is because his ulcer can presents a full-thickness skin loss. His subcutaneous fat can be visible, but the
bone, tendon or the muscles are not still exposed (How to recognize the four stages of pressure ulcer,
2017).
6. When the nurse is assessing Johns wound, he/she documents what it looks like using a
variety of methods.
Choose from the following words and fill in the blanks with words that match them to the
sentences.
Probe, marking pen, wound tracing, a ruler, written consent, transparent acetate grid,
clinical wound photography, wound measurement.
Probe provides the most accurate and objective means of assessment and evaluation of wound
treatments. wound tracing can be used to provide an accurate measurement of the length and
123 TMP E – Assessment Template – Written v1.3 Page 11 of 24
width of a wound Assessment of the depth or length of a wound can be performed using a wound
measurement. Using a two-dimensional method, such as by tracing the margins of the wound,
can be assessed using a ruler and marking pen. It is essential that written consent is obtained
from the patient/relative or carer prior to taking photographs.
7. Johns doctor has ordered a Doppler ultrasound, explain what this means and how it is
performed?
Doppler ultrasound is generally a noninvasive test which can be used to determine the flow of blood via
the blood vessels by simply bouncing the high-frequency sound waves off circulating the red blood cells.
The healthcare professional of John have ordered one for him it is because it is more often used for
evaluating the inflammation of a subcutaneous tissue that is caused by the pressure ulcers, but the color
Doppler mode can aid to improve the determination of an inflammatory edema in the subcutaneous fat
and a necrotic tissue in the pressure ulcers as well (Color Doppler Ultrasonography to Evaluate
Hypoechoic Areas in Pressure Ulcers, 2018).
8. Identify and discuss 2 effects on wound healing in regards to complex and challenging)
wounds.
Factor Effect on wound healing
Age of the patient Everything can slow down as age of a person enhances. In
this, an inflammatory response is decreased or delayed as is
the proliferative response. The remodeling can occur, but to a
lesser degree as well as the collagen is formed is qualitatively
different.
Poor Blood
Circulation
It is generally the most dramatic element which can influence
the healing of a wound. The nutrients as well as the oxygen
which a new blood can carry towards the wound are generally
the key to a successful healing.
9. Many factors affect the wound-healing process. Therefore, wound management strategies
must be tailored to meet the individual holistic needs of the patient, their wound and their
environment.
Tick the sentence that best outlines the principles of wound management
◻ Assess and correct cause of tissue damage
◻ Assess wound history and characteristics
◻ Ensure adequate tissue perfusion
◻ Wound-bed preparation
◻ Wound cleansing
◻ Wound-cleansing solutions and techniques
◻ All of the above
Case study
Case Study Scenario 3 – Infected Surgical Wound:
Ms Maggie Malone is an obese 52-year-old female, who was admitted to the orthopaedic
ward for a total left knee replacement. Staples were the method of wound closure.
123 TMP E – Assessment Template – Written v1.3 Page 12 of 24
measurement. Using a two-dimensional method, such as by tracing the margins of the wound,
can be assessed using a ruler and marking pen. It is essential that written consent is obtained
from the patient/relative or carer prior to taking photographs.
7. Johns doctor has ordered a Doppler ultrasound, explain what this means and how it is
performed?
Doppler ultrasound is generally a noninvasive test which can be used to determine the flow of blood via
the blood vessels by simply bouncing the high-frequency sound waves off circulating the red blood cells.
The healthcare professional of John have ordered one for him it is because it is more often used for
evaluating the inflammation of a subcutaneous tissue that is caused by the pressure ulcers, but the color
Doppler mode can aid to improve the determination of an inflammatory edema in the subcutaneous fat
and a necrotic tissue in the pressure ulcers as well (Color Doppler Ultrasonography to Evaluate
Hypoechoic Areas in Pressure Ulcers, 2018).
8. Identify and discuss 2 effects on wound healing in regards to complex and challenging)
wounds.
Factor Effect on wound healing
Age of the patient Everything can slow down as age of a person enhances. In
this, an inflammatory response is decreased or delayed as is
the proliferative response. The remodeling can occur, but to a
lesser degree as well as the collagen is formed is qualitatively
different.
Poor Blood
Circulation
It is generally the most dramatic element which can influence
the healing of a wound. The nutrients as well as the oxygen
which a new blood can carry towards the wound are generally
the key to a successful healing.
9. Many factors affect the wound-healing process. Therefore, wound management strategies
must be tailored to meet the individual holistic needs of the patient, their wound and their
environment.
Tick the sentence that best outlines the principles of wound management
◻ Assess and correct cause of tissue damage
◻ Assess wound history and characteristics
◻ Ensure adequate tissue perfusion
◻ Wound-bed preparation
◻ Wound cleansing
◻ Wound-cleansing solutions and techniques
◻ All of the above
Case study
Case Study Scenario 3 – Infected Surgical Wound:
Ms Maggie Malone is an obese 52-year-old female, who was admitted to the orthopaedic
ward for a total left knee replacement. Staples were the method of wound closure.
123 TMP E – Assessment Template – Written v1.3 Page 12 of 24
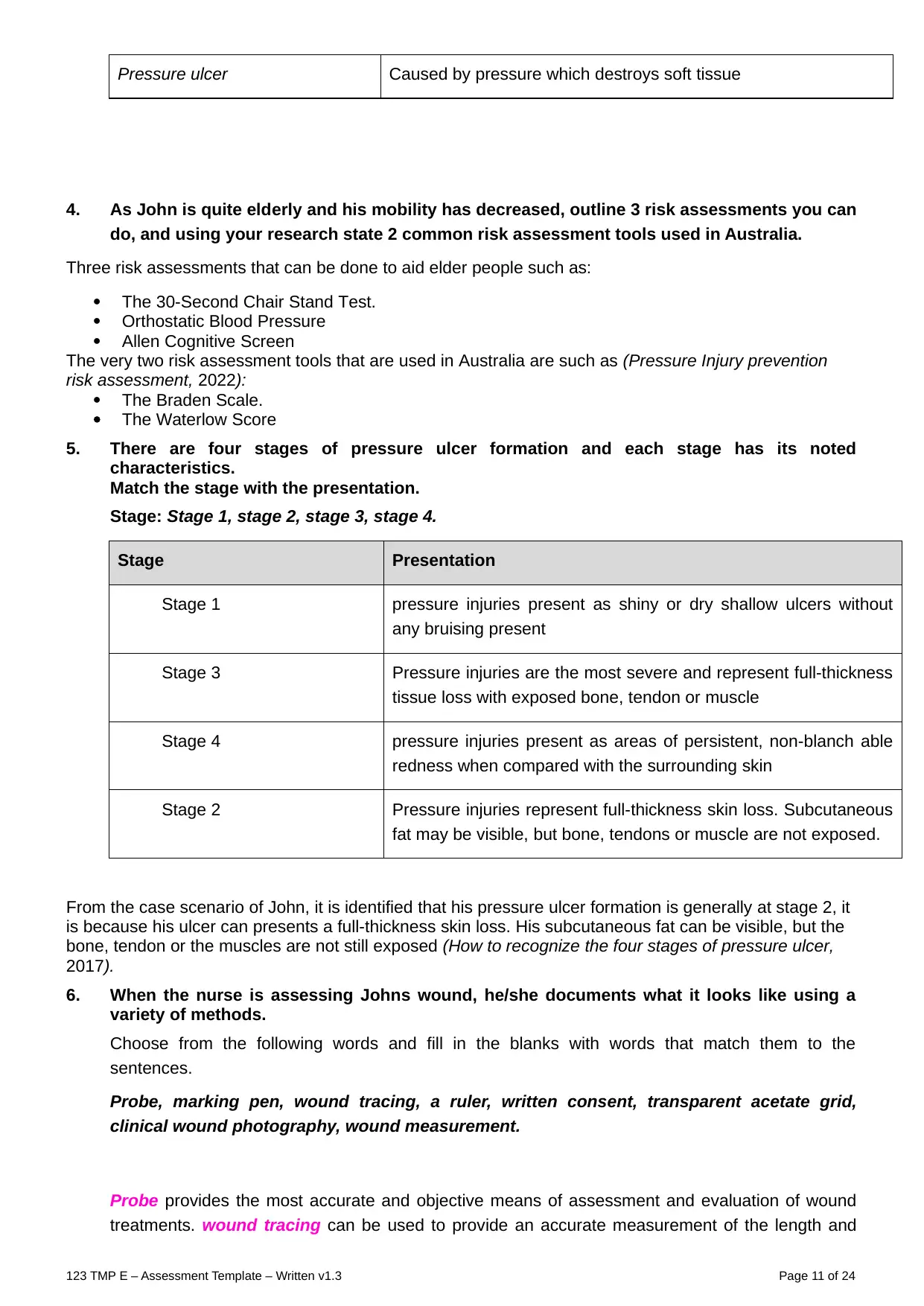
Ms Malones’ medical history reveals that she is a heavy smoker, smoking at least 30
cigarettes / day and was diagnosed with Diabetes type 2 around 4 years ago, but has not
been following a recommended diet.
Day 5 post-op: Maggie is complaining of pain in her left knee, she is febrile 38.7C and an
increase in discharge from her wound on her dressings is apparent. On removal of the
wound dressings, the wound appeared reddened and inflamed; staples are insitu; an open
1.3cm gap at the lower end of the wound was obvious and is oozing purulent fluid. A wound
swab is taken and results show a Methicillin-resistant Staphylococcus aureus (MRSA)
infection
On reading the surgeons’ instructions: “Antibiotics to be commenced; Wound cavity to be
dressed daily with Dressing as per directed by wound specialist
Ms Malone is reviewed by the wound management nurse who documented the following:
“Nursing: Wound to heal by secondary intention. Wound cavity measures 13mm long x
10mm wide and 8mm deep, extending to the subcutaneous tissue layer. Wound bed
consists of 100% granulation tissue; is malodorous and is oozing a moderate amount of
haemopurulent exudate. Staples to remain insitu until day 10 post-op”.
74838715 / jsouthby / shutterstock.com
◻
◻
Case Study 3- Short answer questions: word count and referencing stated where
required
Read each question carefully and ensure you answer each part.
1a. Maggie’s Husband comes to visit and he has asked you to explain Maggie’s infection, how she got
it and how long will she have it for. To be able to explain to Maggie’s husband you need to
understand the chain of infection
Listed below are the 6 elements required for a disease to be spread (starting with infectious agent).
Re-arrange the elements below in the in the correct order. Beside each element state how it
123 TMP E – Assessment Template – Written v1.3 Page 13 of 24
cigarettes / day and was diagnosed with Diabetes type 2 around 4 years ago, but has not
been following a recommended diet.
Day 5 post-op: Maggie is complaining of pain in her left knee, she is febrile 38.7C and an
increase in discharge from her wound on her dressings is apparent. On removal of the
wound dressings, the wound appeared reddened and inflamed; staples are insitu; an open
1.3cm gap at the lower end of the wound was obvious and is oozing purulent fluid. A wound
swab is taken and results show a Methicillin-resistant Staphylococcus aureus (MRSA)
infection
On reading the surgeons’ instructions: “Antibiotics to be commenced; Wound cavity to be
dressed daily with Dressing as per directed by wound specialist
Ms Malone is reviewed by the wound management nurse who documented the following:
“Nursing: Wound to heal by secondary intention. Wound cavity measures 13mm long x
10mm wide and 8mm deep, extending to the subcutaneous tissue layer. Wound bed
consists of 100% granulation tissue; is malodorous and is oozing a moderate amount of
haemopurulent exudate. Staples to remain insitu until day 10 post-op”.
74838715 / jsouthby / shutterstock.com
◻
◻
Case Study 3- Short answer questions: word count and referencing stated where
required
Read each question carefully and ensure you answer each part.
1a. Maggie’s Husband comes to visit and he has asked you to explain Maggie’s infection, how she got
it and how long will she have it for. To be able to explain to Maggie’s husband you need to
understand the chain of infection
Listed below are the 6 elements required for a disease to be spread (starting with infectious agent).
Re-arrange the elements below in the in the correct order. Beside each element state how it
123 TMP E – Assessment Template – Written v1.3 Page 13 of 24
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

applies to Maggie’s wound.
Problems with this picture. If you can’t type inside the circles, just list pl
123 TMP E – Assessment Template – Written v1.3 Page 14 of 24
Problems with this picture. If you can’t type inside the circles, just list pl
123 TMP E – Assessment Template – Written v1.3 Page 14 of 24
1. Infection Agent: As per the above case scenario, Superficial infection, after the knee
replacement operation, an infection can develop within the skin around the incision.
2. The Reservoir: as per the above case scenario, the wound can take time to heal, there can
be excess of the accumulation of the fluids within the tissue as a part of an inflammatory
chain that is leading to healing.
3. Portal of Exit: As per the case scenario, the incision is made along the front and towards the
middle or along the front and to the side of the knee. In this, the more traditional surgical
approach generally includes the cutting into the quadriceps tendon to turn the kneecap over
as well as can expose the arthritic joint.
4. Mode of transmission: As per the case scenario, a total joint of the patient can become
infected at the time of procedure. In this, the most common pathway of bacteria can enter the
body can involve via the breaks or the cuts within the skin (Knee replacement infection,
2018).
5. Portal of Entry: As per the case scenario, the infection can be occurred through skin. And in
order to prevent the infection the effective measures can be taken into considerations such
as; washing with chlorohexidine, antibiotics must be taken in the hour prior surgery and then
24 hours of interval afterwards.
6. Susceptible new host: As per the case scenario, the levels of immunity are generally the end
point to stop an infection. In addition to this, cleaning of wound on daily basis is also needed
to prevent the spread of infection.
123 TMP E – Assessment Template – Written v1.3 Page 15 of 24
replacement operation, an infection can develop within the skin around the incision.
2. The Reservoir: as per the above case scenario, the wound can take time to heal, there can
be excess of the accumulation of the fluids within the tissue as a part of an inflammatory
chain that is leading to healing.
3. Portal of Exit: As per the case scenario, the incision is made along the front and towards the
middle or along the front and to the side of the knee. In this, the more traditional surgical
approach generally includes the cutting into the quadriceps tendon to turn the kneecap over
as well as can expose the arthritic joint.
4. Mode of transmission: As per the case scenario, a total joint of the patient can become
infected at the time of procedure. In this, the most common pathway of bacteria can enter the
body can involve via the breaks or the cuts within the skin (Knee replacement infection,
2018).
5. Portal of Entry: As per the case scenario, the infection can be occurred through skin. And in
order to prevent the infection the effective measures can be taken into considerations such
as; washing with chlorohexidine, antibiotics must be taken in the hour prior surgery and then
24 hours of interval afterwards.
6. Susceptible new host: As per the case scenario, the levels of immunity are generally the end
point to stop an infection. In addition to this, cleaning of wound on daily basis is also needed
to prevent the spread of infection.
123 TMP E – Assessment Template – Written v1.3 Page 15 of 24
1b. Using the above model, it could be suggested that this is a healthcare-associated infection (HAI). Provide an example of a brief discussion on
how you would explain this type of infection and its development to Maggie’s husband. Provide this education as though you were speaking to the
client’s husband using appropriate terminology.
As per the case scenario, a total joint of the patient can become infected at the time of procedure. In this, the most common pathway of bacteria can enter the
body can involve via the breaks or the cuts within the skin. In context with the susceptible levels, the levels of immunity are generally the end point to stop an
infection. In addition to this, cleaning of wound on daily basis is also needed to prevent the spread of infection.
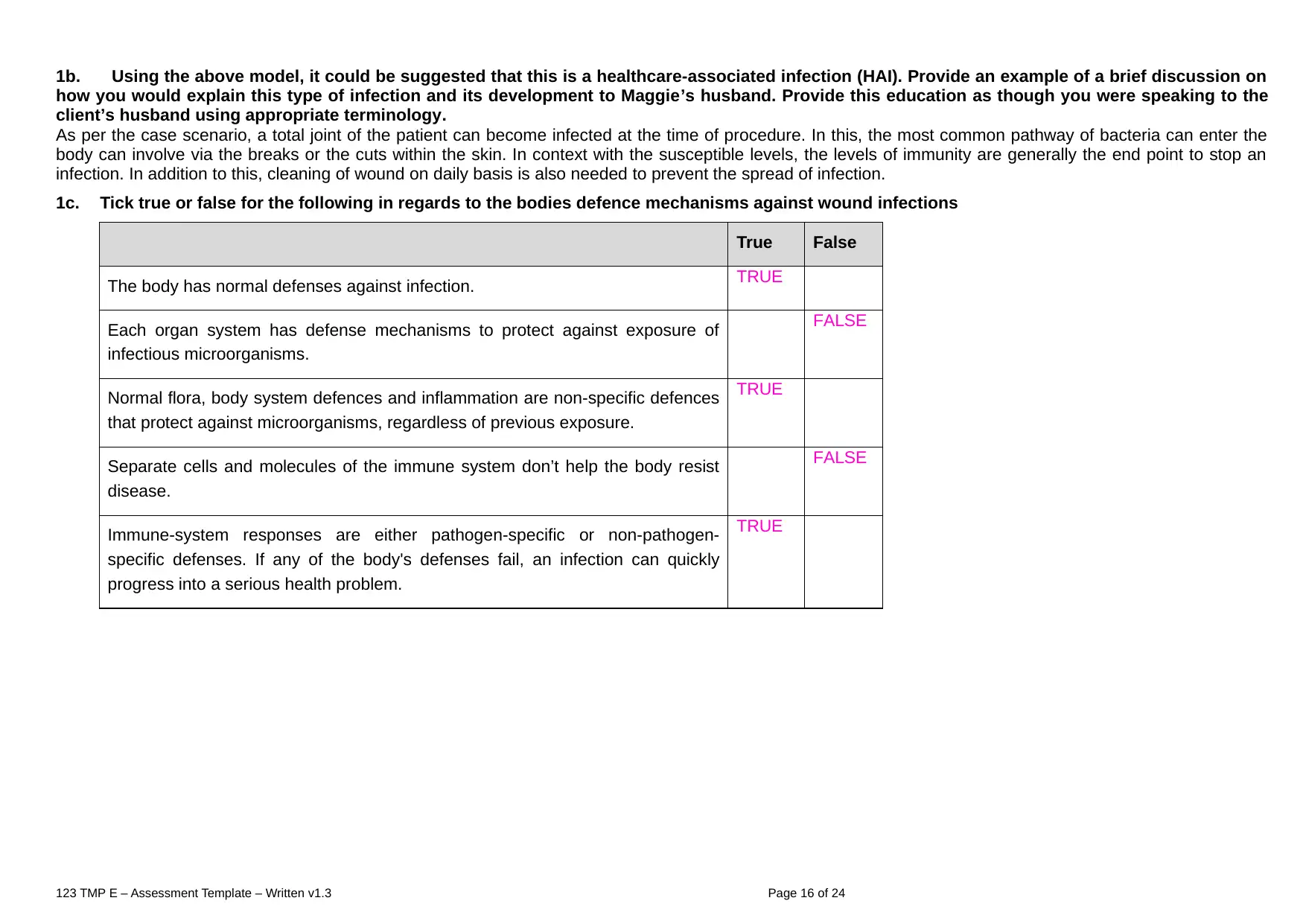
1c. Tick true or false for the following in regards to the bodies defence mechanisms against wound infections
True False
The body has normal defenses against infection. TRUE
Each organ system has defense mechanisms to protect against exposure of
infectious microorganisms.
FALSE
Normal flora, body system defences and inflammation are non-specific defences
that protect against microorganisms, regardless of previous exposure.
TRUE
Separate cells and molecules of the immune system don’t help the body resist
disease.
FALSE
Immune-system responses are either pathogen-specific or non-pathogen-
specific defenses. If any of the body's defenses fail, an infection can quickly
progress into a serious health problem.
TRUE
123 TMP E – Assessment Template – Written v1.3 Page 16 of 24
how you would explain this type of infection and its development to Maggie’s husband. Provide this education as though you were speaking to the
client’s husband using appropriate terminology.
As per the case scenario, a total joint of the patient can become infected at the time of procedure. In this, the most common pathway of bacteria can enter the
body can involve via the breaks or the cuts within the skin. In context with the susceptible levels, the levels of immunity are generally the end point to stop an
infection. In addition to this, cleaning of wound on daily basis is also needed to prevent the spread of infection.
1c. Tick true or false for the following in regards to the bodies defence mechanisms against wound infections
True False
The body has normal defenses against infection. TRUE
Each organ system has defense mechanisms to protect against exposure of
infectious microorganisms.
FALSE
Normal flora, body system defences and inflammation are non-specific defences
that protect against microorganisms, regardless of previous exposure.
TRUE
Separate cells and molecules of the immune system don’t help the body resist
disease.
FALSE
Immune-system responses are either pathogen-specific or non-pathogen-
specific defenses. If any of the body's defenses fail, an infection can quickly
progress into a serious health problem.
TRUE
123 TMP E – Assessment Template – Written v1.3 Page 16 of 24
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1d. Explain in terms that you can understand - the immune response in regards to infections.
Immune Response is defined as the response, When the foreign particle enters into the body and the way body defends itself by any harmful bacteria and
viruses. The immune system wants to attack on the particular microorganisms this is denotes as immune response.
The innate (non-specific immune system) and adaptive immune works together when a infective germ enter into the body. Foreign particle or antigens it
can be in any form like viruses, bacteria, pathogens and diseases causing parasites. B-cells recognizes the antigens further it can produce antibodies to fight
against antigens. After that antibody attached into the antigens (like a lock- key configuration). It can hold and pass signals to the other cells of the immune
system to take an action against the virus (Immune Response, 2022).
Note- White bloods cells are responsible to kill foreign particle or antigens.
2. Standard and Additional precautions – Using the word bank complete the sentences in regards to precautions. (fill in the blanks)
Word bank: Mucosa, airborne, fluids, single, all, contact, suspected, infection, skin, known, droplet, cohorted
Maggie requires both standard and additional precautions. Standard precautions are infection
control practices used for suspected patients, regardless of their known cohorted status. Standard Precautions dictate that personal protective equipment
(PPE) must be worn when there is a risk of contact with body fluids, non-intact or skin Infection may be transmitted in various ways. The 3
transmission categories are droplet, and airborne Maggie’s type of transmission is Transmission-Based Precautions are infection control practices used
for patients with single or all conditions.
As Maggie has MRSA (an infectious condition) she would require additional precautions and should be nursed in a room or in a room with a patient with
the same infectious condition.
3. As stated in the case study Maggie had a wound specimen taken. Which of the following are correct in regards to obtaining a wound specimen and
interpreting laboratory results (Tick 4 correct answers)
◻ Always collect a wound culture sample from viable granulation tissue near the centre of the wound that has just been cleansed or irrigated with 0.9%
sodium chloride solution.
◻ Evaluation findings and laboratory results must be communicated to the clinical team leader per the organization’s practice
◻ Cleanse the wound and surrounding skin with 0.9% sodium chloride solution from the most to least contaminated area.
123 TMP E – Assessment Template – Written v1.3 Page 17 of 24
Immune Response is defined as the response, When the foreign particle enters into the body and the way body defends itself by any harmful bacteria and
viruses. The immune system wants to attack on the particular microorganisms this is denotes as immune response.
The innate (non-specific immune system) and adaptive immune works together when a infective germ enter into the body. Foreign particle or antigens it
can be in any form like viruses, bacteria, pathogens and diseases causing parasites. B-cells recognizes the antigens further it can produce antibodies to fight
against antigens. After that antibody attached into the antigens (like a lock- key configuration). It can hold and pass signals to the other cells of the immune
system to take an action against the virus (Immune Response, 2022).
Note- White bloods cells are responsible to kill foreign particle or antigens.
2. Standard and Additional precautions – Using the word bank complete the sentences in regards to precautions. (fill in the blanks)
Word bank: Mucosa, airborne, fluids, single, all, contact, suspected, infection, skin, known, droplet, cohorted
Maggie requires both standard and additional precautions. Standard precautions are infection
control practices used for suspected patients, regardless of their known cohorted status. Standard Precautions dictate that personal protective equipment
(PPE) must be worn when there is a risk of contact with body fluids, non-intact or skin Infection may be transmitted in various ways. The 3
transmission categories are droplet, and airborne Maggie’s type of transmission is Transmission-Based Precautions are infection control practices used
for patients with single or all conditions.
As Maggie has MRSA (an infectious condition) she would require additional precautions and should be nursed in a room or in a room with a patient with
the same infectious condition.
3. As stated in the case study Maggie had a wound specimen taken. Which of the following are correct in regards to obtaining a wound specimen and
interpreting laboratory results (Tick 4 correct answers)
◻ Always collect a wound culture sample from viable granulation tissue near the centre of the wound that has just been cleansed or irrigated with 0.9%
sodium chloride solution.
◻ Evaluation findings and laboratory results must be communicated to the clinical team leader per the organization’s practice
◻ Cleanse the wound and surrounding skin with 0.9% sodium chloride solution from the most to least contaminated area.
123 TMP E – Assessment Template – Written v1.3 Page 17 of 24
◻ If there is more than one wound, obtain only one culture from each wound. Perform hand hygiene and change gloves between wounds.
◻ Determine when a dressing change is scheduled. If possible, plan the specimen collection and wound evaluation during the next scheduled dressing
change.
4. What impact will the following issues have on Ms Malones’ wound healing and her activities of daily living? (including psychological impact).
Put each of the above issues under a heading and discuss each in detail. Support each issue with research and a clear rationale (reason) for why it will affect
her healing. This question is looking for your ability to problem solve and critically think.
Poor nutrition
Wound healing: As per the case scenario, the malnutrition has also been effectively associated to the reduced wound tensile strength and enhanced the rates of
infection. The undernourished patient such as Ms. Malones can improve the infection, the pressure ulcers as well as delayed healing of wound which can
outcome in the chronic non-healing wounds.
ADLs: As per the case scenario, the poor nutrition can effectively contribute to the stress, tiredness as well as Ms. Malone’s capacity to work. It can also
contribute towards the developing risk of some of the disorders as well as its associated well-being issues like overweight, high blood pressure and so on.
Psychological impacts: As per the case scenario, the poor nutrition can play key role in worsening the mood issues like depression and anxiety. Therefore, the
diet rich in the vegetables as well as the olive oil like the Mediterranean diet, can effectively enhances the symptoms of anxiety and depression.
Smoking
Wound healing: As per the case scenario, the smoking can specifically distort the immune system of Ms. Malone and can delay her healing process, enhancing
the risk of infection at the site of surgical wound. Smoking can gradually reduces the ability of the body to deliver essential nutrients for the healing after surgery.
ADLs: As per the case scenario, smoking is mainly linked with the worse symptoms as well as the results with her behavioral well-being conditions consisting the
higher depressive symptoms, enhanced the suicidal behaviors as well as drug and alcohol use relapse.
Psychological impacts: As per the case scenario, her smoking is highly associated with the range of mental well-being issues consisting the anxiety illness,
schizophrenia and depression as well.
Diabetes
Wound healing: As per the case scenario, as Ms. Malone is having medical history of diabetes and the diabetes linked peripheral arterial illness can specifically
decreases the flow of blood to the surgical site’s outcomes in delayed recovery. The diabetic healing of wound is generally impaired because of the less oxygen
can reach the wound as well as the tissues do not heal as quickly.
ADLs: As per the case scenario, the diabetes can damage the cardiovascular system, the blood vessels, kidneys, as well as the nerves with time, can cause the
chronic issues as well as premature death.
Psychological impacts: As per the case scenario, changes in the blood sugar can effectively cause the rapid alterations in the mood as well as the other mental
symptoms like trouble thinking clearly, fatigue as well as anxiety (Diabetes And Mental Health, 2022).
5. Develop a nursing plan of care for Ms Malone. Your care plan must follow a nursing problem solving approach using the table below
Give one nursing intervention for each problem stated below i.e., a total of 5 nursing interventions that you would put into place to assist Ms Malone with
the following problems.
Support each intervention with a rationale/reason, evaluation and a reference
PROBLEMS:
123 TMP E – Assessment Template – Written v1.3 Page 18 of 24
◻ Determine when a dressing change is scheduled. If possible, plan the specimen collection and wound evaluation during the next scheduled dressing
change.
4. What impact will the following issues have on Ms Malones’ wound healing and her activities of daily living? (including psychological impact).
Put each of the above issues under a heading and discuss each in detail. Support each issue with research and a clear rationale (reason) for why it will affect
her healing. This question is looking for your ability to problem solve and critically think.
Poor nutrition
Wound healing: As per the case scenario, the malnutrition has also been effectively associated to the reduced wound tensile strength and enhanced the rates of
infection. The undernourished patient such as Ms. Malones can improve the infection, the pressure ulcers as well as delayed healing of wound which can
outcome in the chronic non-healing wounds.
ADLs: As per the case scenario, the poor nutrition can effectively contribute to the stress, tiredness as well as Ms. Malone’s capacity to work. It can also
contribute towards the developing risk of some of the disorders as well as its associated well-being issues like overweight, high blood pressure and so on.
Psychological impacts: As per the case scenario, the poor nutrition can play key role in worsening the mood issues like depression and anxiety. Therefore, the
diet rich in the vegetables as well as the olive oil like the Mediterranean diet, can effectively enhances the symptoms of anxiety and depression.
Smoking
Wound healing: As per the case scenario, the smoking can specifically distort the immune system of Ms. Malone and can delay her healing process, enhancing
the risk of infection at the site of surgical wound. Smoking can gradually reduces the ability of the body to deliver essential nutrients for the healing after surgery.
ADLs: As per the case scenario, smoking is mainly linked with the worse symptoms as well as the results with her behavioral well-being conditions consisting the
higher depressive symptoms, enhanced the suicidal behaviors as well as drug and alcohol use relapse.
Psychological impacts: As per the case scenario, her smoking is highly associated with the range of mental well-being issues consisting the anxiety illness,
schizophrenia and depression as well.
Diabetes
Wound healing: As per the case scenario, as Ms. Malone is having medical history of diabetes and the diabetes linked peripheral arterial illness can specifically
decreases the flow of blood to the surgical site’s outcomes in delayed recovery. The diabetic healing of wound is generally impaired because of the less oxygen
can reach the wound as well as the tissues do not heal as quickly.
ADLs: As per the case scenario, the diabetes can damage the cardiovascular system, the blood vessels, kidneys, as well as the nerves with time, can cause the
chronic issues as well as premature death.
Psychological impacts: As per the case scenario, changes in the blood sugar can effectively cause the rapid alterations in the mood as well as the other mental
symptoms like trouble thinking clearly, fatigue as well as anxiety (Diabetes And Mental Health, 2022).
5. Develop a nursing plan of care for Ms Malone. Your care plan must follow a nursing problem solving approach using the table below
Give one nursing intervention for each problem stated below i.e., a total of 5 nursing interventions that you would put into place to assist Ms Malone with
the following problems.
Support each intervention with a rationale/reason, evaluation and a reference
PROBLEMS:
123 TMP E – Assessment Template – Written v1.3 Page 18 of 24
the location of her wound
activities of daily living
reduced mobility
Pain
Referral needs – which other health team members both within and outside the hospital environment would be involved in the care of Ms Malone.
Problem Intervention Rationale Evaluation
(including how you
would involve the
patient?)
Location of
Wound
Eg. Avoid tight fitting long
pants or cloths that will rub
against wound.
Don’t cross legs
constriction / rubbing
around wound can affect
healing
The client will
demonstrate their
knowledge of why it is
important to keep her
wound free of
constrictions
Activities of
Daily Living
Take help of the other
person in doing activities
to avoid abrasion against
wound
Performing vigorous
activities can significantly
influence the healing
process.
The patient will exhibit
their understanding of
why it is necessary to
avoid vigorous activities
or other things to keep
her wound free of
damage.
Reduced
Mobility
Boost the patient to do
light mobility and
scheduled the activities
around the rest periods.
Encourage a healthy
nutrition and hydration as
well.
It can effectively enhance
the excellent blood
circulation as well as can
help in the maintenance of
muscular functions and
strength as well.
The poor nutrition and
impaired blood circulation
can significantly affect the
mobility of her. To
overcome the impact, she
must be provided with
healthy diet.
123 TMP E – Assessment Template – Written v1.3 Page 19 of 24
activities of daily living
reduced mobility
Pain
Referral needs – which other health team members both within and outside the hospital environment would be involved in the care of Ms Malone.
Problem Intervention Rationale Evaluation
(including how you
would involve the
patient?)
Location of
Wound
Eg. Avoid tight fitting long
pants or cloths that will rub
against wound.
Don’t cross legs
constriction / rubbing
around wound can affect
healing
The client will
demonstrate their
knowledge of why it is
important to keep her
wound free of
constrictions
Activities of
Daily Living
Take help of the other
person in doing activities
to avoid abrasion against
wound
Performing vigorous
activities can significantly
influence the healing
process.
The patient will exhibit
their understanding of
why it is necessary to
avoid vigorous activities
or other things to keep
her wound free of
damage.
Reduced
Mobility
Boost the patient to do
light mobility and
scheduled the activities
around the rest periods.
Encourage a healthy
nutrition and hydration as
well.
It can effectively enhance
the excellent blood
circulation as well as can
help in the maintenance of
muscular functions and
strength as well.
The poor nutrition and
impaired blood circulation
can significantly affect the
mobility of her. To
overcome the impact, she
must be provided with
healthy diet.
123 TMP E – Assessment Template – Written v1.3 Page 19 of 24
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
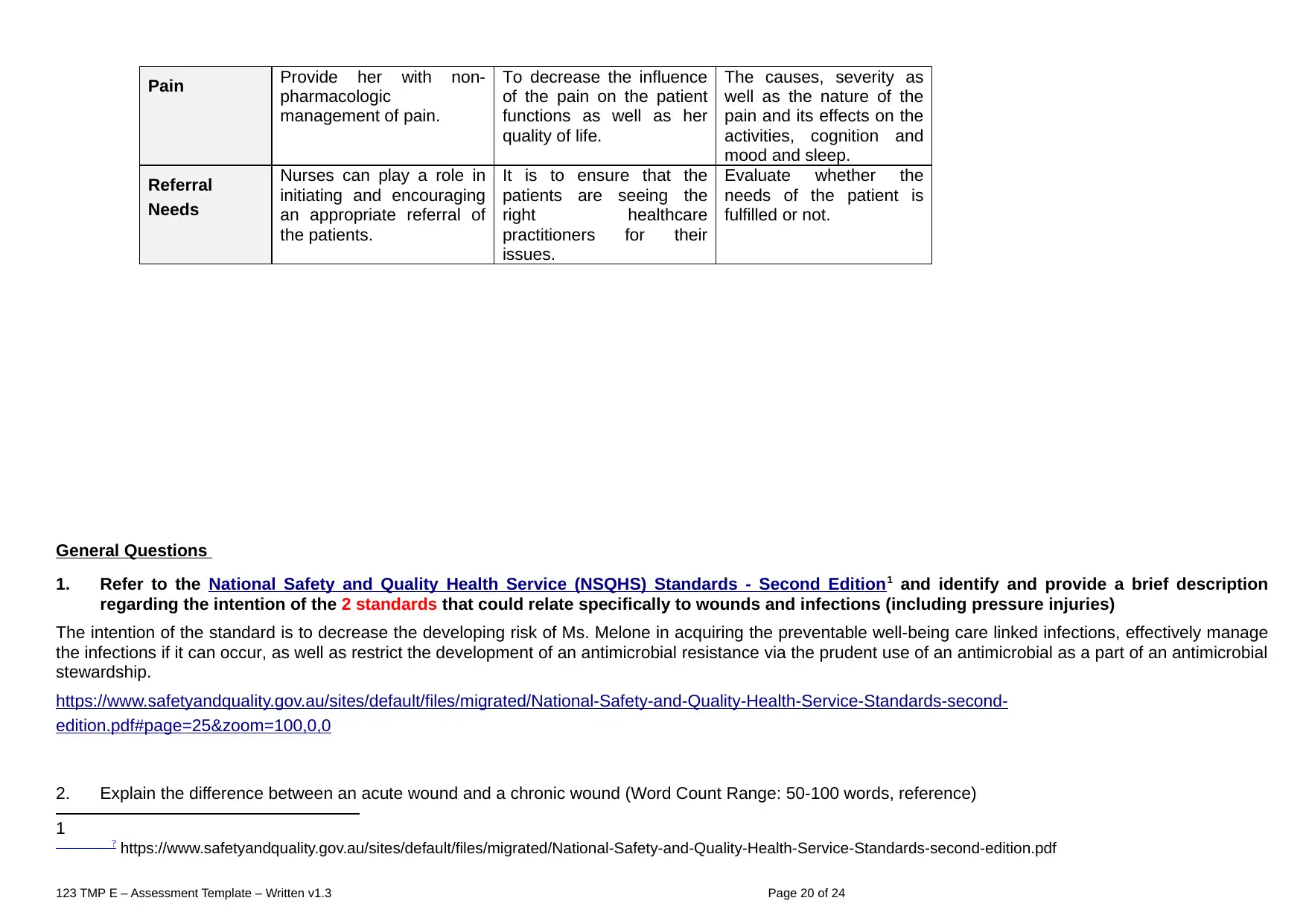
Pain Provide her with non-
pharmacologic
management of pain.
To decrease the influence
of the pain on the patient
functions as well as her
quality of life.
The causes, severity as
well as the nature of the
pain and its effects on the
activities, cognition and
mood and sleep.
Referral
Needs
Nurses can play a role in
initiating and encouraging
an appropriate referral of
the patients.
It is to ensure that the
patients are seeing the
right healthcare
practitioners for their
issues.
Evaluate whether the
needs of the patient is
fulfilled or not.
General Questions
1. Refer to the National Safety and Quality Health Service (NSQHS) Standards - Second Edition1 and identify and provide a brief description
regarding the intention of the 2 standards that could relate specifically to wounds and infections (including pressure injuries)
The intention of the standard is to decrease the developing risk of Ms. Melone in acquiring the preventable well-being care linked infections, effectively manage
the infections if it can occur, as well as restrict the development of an antimicrobial resistance via the prudent use of an antimicrobial as a part of an antimicrobial
stewardship.
https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-
edition.pdf#page=25&zoom=100,0,0
2. Explain the difference between an acute wound and a chronic wound (Word Count Range: 50-100 words, reference)
1 ? https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf
123 TMP E – Assessment Template – Written v1.3 Page 20 of 24
pharmacologic
management of pain.
To decrease the influence
of the pain on the patient
functions as well as her
quality of life.
The causes, severity as
well as the nature of the
pain and its effects on the
activities, cognition and
mood and sleep.
Referral
Needs
Nurses can play a role in
initiating and encouraging
an appropriate referral of
the patients.
It is to ensure that the
patients are seeing the
right healthcare
practitioners for their
issues.
Evaluate whether the
needs of the patient is
fulfilled or not.
General Questions
1. Refer to the National Safety and Quality Health Service (NSQHS) Standards - Second Edition1 and identify and provide a brief description
regarding the intention of the 2 standards that could relate specifically to wounds and infections (including pressure injuries)
The intention of the standard is to decrease the developing risk of Ms. Melone in acquiring the preventable well-being care linked infections, effectively manage
the infections if it can occur, as well as restrict the development of an antimicrobial resistance via the prudent use of an antimicrobial as a part of an antimicrobial
stewardship.
https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-
edition.pdf#page=25&zoom=100,0,0
2. Explain the difference between an acute wound and a chronic wound (Word Count Range: 50-100 words, reference)
1 ? https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf
123 TMP E – Assessment Template – Written v1.3 Page 20 of 24
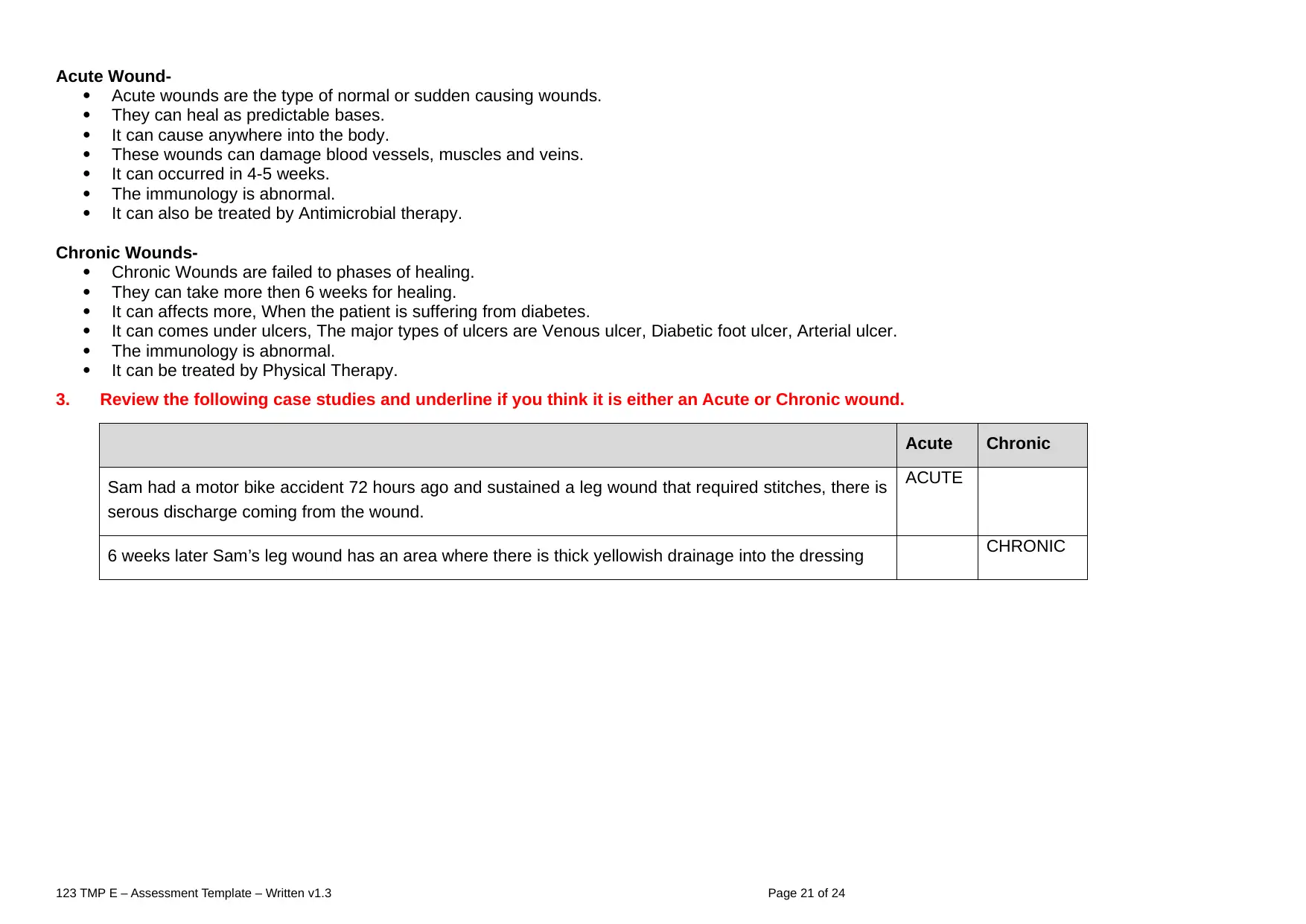
Acute Wound-
Acute wounds are the type of normal or sudden causing wounds.
They can heal as predictable bases.
It can cause anywhere into the body.
These wounds can damage blood vessels, muscles and veins.
It can occurred in 4-5 weeks.
The immunology is abnormal.
It can also be treated by Antimicrobial therapy.
Chronic Wounds-
Chronic Wounds are failed to phases of healing.
They can take more then 6 weeks for healing.
It can affects more, When the patient is suffering from diabetes.
It can comes under ulcers, The major types of ulcers are Venous ulcer, Diabetic foot ulcer, Arterial ulcer.
The immunology is abnormal.
It can be treated by Physical Therapy.
3. Review the following case studies and underline if you think it is either an Acute or Chronic wound.
Acute Chronic
Sam had a motor bike accident 72 hours ago and sustained a leg wound that required stitches, there is
serous discharge coming from the wound.
ACUTE
6 weeks later Sam’s leg wound has an area where there is thick yellowish drainage into the dressing CHRONIC
123 TMP E – Assessment Template – Written v1.3 Page 21 of 24
Acute wounds are the type of normal or sudden causing wounds.
They can heal as predictable bases.
It can cause anywhere into the body.
These wounds can damage blood vessels, muscles and veins.
It can occurred in 4-5 weeks.
The immunology is abnormal.
It can also be treated by Antimicrobial therapy.
Chronic Wounds-
Chronic Wounds are failed to phases of healing.
They can take more then 6 weeks for healing.
It can affects more, When the patient is suffering from diabetes.
It can comes under ulcers, The major types of ulcers are Venous ulcer, Diabetic foot ulcer, Arterial ulcer.
The immunology is abnormal.
It can be treated by Physical Therapy.
3. Review the following case studies and underline if you think it is either an Acute or Chronic wound.
Acute Chronic
Sam had a motor bike accident 72 hours ago and sustained a leg wound that required stitches, there is
serous discharge coming from the wound.
ACUTE
6 weeks later Sam’s leg wound has an area where there is thick yellowish drainage into the dressing CHRONIC
123 TMP E – Assessment Template – Written v1.3 Page 21 of 24
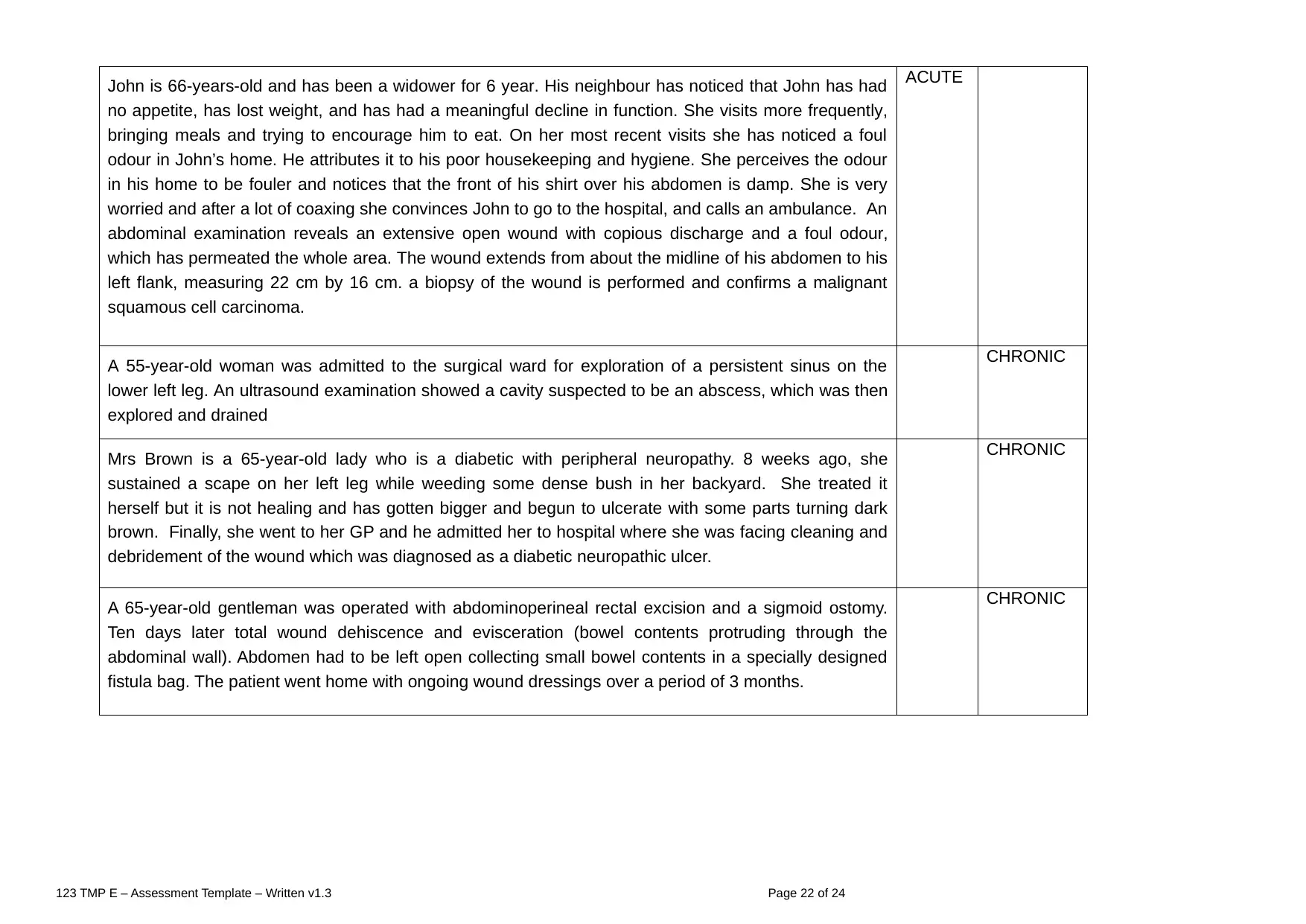
John is 66-years-old and has been a widower for 6 year. His neighbour has noticed that John has had
no appetite, has lost weight, and has had a meaningful decline in function. She visits more frequently,
bringing meals and trying to encourage him to eat. On her most recent visits she has noticed a foul
odour in John’s home. He attributes it to his poor housekeeping and hygiene. She perceives the odour
in his home to be fouler and notices that the front of his shirt over his abdomen is damp. She is very
worried and after a lot of coaxing she convinces John to go to the hospital, and calls an ambulance. An
abdominal examination reveals an extensive open wound with copious discharge and a foul odour,
which has permeated the whole area. The wound extends from about the midline of his abdomen to his
left flank, measuring 22 cm by 16 cm. a biopsy of the wound is performed and confirms a malignant
squamous cell carcinoma.
ACUTE
A 55-year-old woman was admitted to the surgical ward for exploration of a persistent sinus on the
lower left leg. An ultrasound examination showed a cavity suspected to be an abscess, which was then
explored and drained
CHRONIC
Mrs Brown is a 65-year-old lady who is a diabetic with peripheral neuropathy. 8 weeks ago, she
sustained a scape on her left leg while weeding some dense bush in her backyard. She treated it
herself but it is not healing and has gotten bigger and begun to ulcerate with some parts turning dark
brown. Finally, she went to her GP and he admitted her to hospital where she was facing cleaning and
debridement of the wound which was diagnosed as a diabetic neuropathic ulcer.
CHRONIC
A 65-year-old gentleman was operated with abdominoperineal rectal excision and a sigmoid ostomy.
Ten days later total wound dehiscence and evisceration (bowel contents protruding through the
abdominal wall). Abdomen had to be left open collecting small bowel contents in a specially designed
fistula bag. The patient went home with ongoing wound dressings over a period of 3 months.
CHRONIC
123 TMP E – Assessment Template – Written v1.3 Page 22 of 24
no appetite, has lost weight, and has had a meaningful decline in function. She visits more frequently,
bringing meals and trying to encourage him to eat. On her most recent visits she has noticed a foul
odour in John’s home. He attributes it to his poor housekeeping and hygiene. She perceives the odour
in his home to be fouler and notices that the front of his shirt over his abdomen is damp. She is very
worried and after a lot of coaxing she convinces John to go to the hospital, and calls an ambulance. An
abdominal examination reveals an extensive open wound with copious discharge and a foul odour,
which has permeated the whole area. The wound extends from about the midline of his abdomen to his
left flank, measuring 22 cm by 16 cm. a biopsy of the wound is performed and confirms a malignant
squamous cell carcinoma.
ACUTE
A 55-year-old woman was admitted to the surgical ward for exploration of a persistent sinus on the
lower left leg. An ultrasound examination showed a cavity suspected to be an abscess, which was then
explored and drained
CHRONIC
Mrs Brown is a 65-year-old lady who is a diabetic with peripheral neuropathy. 8 weeks ago, she
sustained a scape on her left leg while weeding some dense bush in her backyard. She treated it
herself but it is not healing and has gotten bigger and begun to ulcerate with some parts turning dark
brown. Finally, she went to her GP and he admitted her to hospital where she was facing cleaning and
debridement of the wound which was diagnosed as a diabetic neuropathic ulcer.
CHRONIC
A 65-year-old gentleman was operated with abdominoperineal rectal excision and a sigmoid ostomy.
Ten days later total wound dehiscence and evisceration (bowel contents protruding through the
abdominal wall). Abdomen had to be left open collecting small bowel contents in a specially designed
fistula bag. The patient went home with ongoing wound dressings over a period of 3 months.
CHRONIC
123 TMP E – Assessment Template – Written v1.3 Page 22 of 24
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4a. Jack Sparrow has a surgical wound with a Jackson Pratt drain. Which of the following are correct in regards to management of Jack’s drain
(Tick 4 correct answers)
◻ Check for infection
◻ Maintain bulb patency as per Drs Orders
◻ Immediately remove if you think it is blocked
◻ Adhere to facility policy and procedures when caring for a Jackson Pratt Drain
◻ Document the amount of drainage
◻ No need to check the connections as this is a closed system
4b. Mr Jones who has a history of chronic venous disease and leg ulcers has returned from theatre after hip surgery and is fitted with elastic
compression stockings (TED) and sequential compression device (SCDs).
Which of the following 2 points are NOT true when it comes to the management techniques of compression devices?
◻ The stockings are not to be rolled down, cut or otherwise altered
◻ Thigh-length stockings prevent proximal VTE better than knee-length stockings
◻ SCDs are not worn when a patient has an active VTE because of the risk of PE
◻ If the stockings are not fitted and worn correctly, venous return is impeded
◻ SCDs will still be effective if they are not applied correctly
◻ They apply external pressure to the lower extremities by means of an electric pump
◻ TED stockings are a part of VTE prevention in hospitalised patients
◻ SCDs are inflatable garments wrapped around the arms
5a. Provide a brief outline in regards to the historical development of contemporary wound management strategies.
The ancient Egyptians generally used honey as treating the wound. In the 1650 B.C Edwin Smith Surgical Papyrus, a similar of much an older document, can
123 TMP E – Assessment Template – Written v1.3 Page 23 of 24
(Tick 4 correct answers)
◻ Check for infection
◻ Maintain bulb patency as per Drs Orders
◻ Immediately remove if you think it is blocked
◻ Adhere to facility policy and procedures when caring for a Jackson Pratt Drain
◻ Document the amount of drainage
◻ No need to check the connections as this is a closed system
4b. Mr Jones who has a history of chronic venous disease and leg ulcers has returned from theatre after hip surgery and is fitted with elastic
compression stockings (TED) and sequential compression device (SCDs).
Which of the following 2 points are NOT true when it comes to the management techniques of compression devices?
◻ The stockings are not to be rolled down, cut or otherwise altered
◻ Thigh-length stockings prevent proximal VTE better than knee-length stockings
◻ SCDs are not worn when a patient has an active VTE because of the risk of PE
◻ If the stockings are not fitted and worn correctly, venous return is impeded
◻ SCDs will still be effective if they are not applied correctly
◻ They apply external pressure to the lower extremities by means of an electric pump
◻ TED stockings are a part of VTE prevention in hospitalised patients
◻ SCDs are inflatable garments wrapped around the arms
5a. Provide a brief outline in regards to the historical development of contemporary wound management strategies.
The ancient Egyptians generally used honey as treating the wound. In the 1650 B.C Edwin Smith Surgical Papyrus, a similar of much an older document, can
123 TMP E – Assessment Template – Written v1.3 Page 23 of 24
illustrate at least more 48 different types of wound. In context with ancient Greek wound treatment, they generally used the wine along with the boiled water as
well as vinegar to cleanse the wounds. In addition to this, the Egyptians were the masters in applying as well as rearranging the bandages, as well as they
identifies the cardinal signs of an infection and inflammation as well. The Egyptian drug therapy can be specifically regarded as having evolved from a system
rooted in the magic and an empirical observation as well. In context with Hippocrates, a Greek physician as well as surgeon, 460-377 BC, called as the father of
medicine, and used the vinegar to irrigate an open wound as well as can wrapped the dressings around the wounds to avoid further injury.
5b. Visceral wounds often involve the internal organs of the body, specifically those within the chest (heart, lungs) or abdomen (as the liver,
pancreas or intestines). Often injury is by gunshot or stabbing.
Steven was involved in a fight late at night where he was stabbed and sustained a deep penetrating abdominal wound. He was transferred to the
emergency department where he underwent a laparotomy to discover the extent of damage and a temporary closure to part of his wound was made with a
vacuum dressing. He was to have further surgery once stable.
Which of the following may NOT be included as wound management strategies for visceral wounds?
◻ Pain control
◻ Keep wound area clean
◻ Daily wound dressing change
◻ Watch for bleeding
5c. Research your local community to identify a minimum of 2 educational resources, community services, and/or professional organisations
associated with wound management and prevention programs.
The Australian Wound Management Associations is generally a multi-disciplinary, a non-profit association mainly involving of the person who are generally
committed to improving as well as enhancing the management of wound for all the people via education, communication, research and networks as well.
https://www.woundsource.com/resource/australian-wound-management-association-awma
the ......................................................................................................................................................
123 TMP E – Assessment Template – Written v1.3 Page 24 of 24
well as vinegar to cleanse the wounds. In addition to this, the Egyptians were the masters in applying as well as rearranging the bandages, as well as they
identifies the cardinal signs of an infection and inflammation as well. The Egyptian drug therapy can be specifically regarded as having evolved from a system
rooted in the magic and an empirical observation as well. In context with Hippocrates, a Greek physician as well as surgeon, 460-377 BC, called as the father of
medicine, and used the vinegar to irrigate an open wound as well as can wrapped the dressings around the wounds to avoid further injury.
5b. Visceral wounds often involve the internal organs of the body, specifically those within the chest (heart, lungs) or abdomen (as the liver,
pancreas or intestines). Often injury is by gunshot or stabbing.
Steven was involved in a fight late at night where he was stabbed and sustained a deep penetrating abdominal wound. He was transferred to the
emergency department where he underwent a laparotomy to discover the extent of damage and a temporary closure to part of his wound was made with a
vacuum dressing. He was to have further surgery once stable.
Which of the following may NOT be included as wound management strategies for visceral wounds?
◻ Pain control
◻ Keep wound area clean
◻ Daily wound dressing change
◻ Watch for bleeding
5c. Research your local community to identify a minimum of 2 educational resources, community services, and/or professional organisations
associated with wound management and prevention programs.
The Australian Wound Management Associations is generally a multi-disciplinary, a non-profit association mainly involving of the person who are generally
committed to improving as well as enhancing the management of wound for all the people via education, communication, research and networks as well.
https://www.woundsource.com/resource/australian-wound-management-association-awma
the ......................................................................................................................................................
123 TMP E – Assessment Template – Written v1.3 Page 24 of 24
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.
