CNA254 Case Study: Terminal Stage Lung Cancer Patient Care Analysis
VerifiedAdded on 2022/09/18
|10
|2165
|31
Case Study
AI Summary
This case study focuses on a 55-year-old Aboriginal man, Tom, with advanced lung cancer and multiple metastases, who is in the terminal phase of his illness. The case presents several critical issues, including the patient's pain and agitation, the dilemma between ensuring comfort and preventing death, unclear decision-making authority, a non-resuscitation request, and the emotional distress of Tom's daughter. The study explores the goals of care, which prioritize reducing suffering, providing support, upholding dignity, respecting wishes, offering information, and providing culturally sensitive and personalized care. The analysis provides a detailed action plan, addressing communication strategies with the family, assessing the patient's capacity to make decisions, and determining the appropriate medical interventions, including pain management through medications like morphine, diamorphine, and fentanyl. The plan also considers the need for social support, symptom management, and honoring the family's cultural and spiritual beliefs. The case underscores the importance of family involvement, ethical considerations, and culturally appropriate care in palliative and terminal care settings, including the involvement of Aboriginal health workers and respecting the family's customs regarding death and dying. References to various medical and ethical guidelines are included.

TERMINAL STAGE
1
A PATIENT WITH MULTIPLE METASTASES AND LATE –STAGE LUNG CANCER
The Name of the Class (Course)
Professor (Tutor)
The Name of the School (University)
The City and State where it is located
The Date
1
A PATIENT WITH MULTIPLE METASTASES AND LATE –STAGE LUNG CANCER
The Name of the Class (Course)
Professor (Tutor)
The Name of the School (University)
The City and State where it is located
The Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TERMINAL STAGE
2
Issues in the case
1. Tom is in pain and agitated
2. There is a dilemma of whether to prevent the patient from dying or ensure comfort
3. Unclear identity of who ought to make medical decisions on Tom’s behalf
4. A non-resuscitation request exists
5. Tom’s daughter has an emotional disturbance
6. Respect of Aborigine culture on healthcare and dying
7. Involvement of family in treatment
8. The choice of medication
9.Medical staff decision on treatment against family preferences(Thomaset al., 2014)
The goals
1. Reduce the suffering of the patient
2. Provide social, spiritual and emotional support
3. Uphold the dignity of the patient
4. Respect the patients and family’s wishes
5. To provide information to the family
6. To give care that is respectful of the culture of the patient
2
Issues in the case
1. Tom is in pain and agitated
2. There is a dilemma of whether to prevent the patient from dying or ensure comfort
3. Unclear identity of who ought to make medical decisions on Tom’s behalf
4. A non-resuscitation request exists
5. Tom’s daughter has an emotional disturbance
6. Respect of Aborigine culture on healthcare and dying
7. Involvement of family in treatment
8. The choice of medication
9.Medical staff decision on treatment against family preferences(Thomaset al., 2014)
The goals
1. Reduce the suffering of the patient
2. Provide social, spiritual and emotional support
3. Uphold the dignity of the patient
4. Respect the patients and family’s wishes
5. To provide information to the family
6. To give care that is respectful of the culture of the patient
TERMINAL STAGE
3
7. To provide personalized care to the patient (The state of Victoria,2015)
Action plan
Since Tom’s daughter is angry and agitated, I would tell her what she feels is completely
expected. Then I would ask to talk with her outside for a while. It would be preferable to find a
place to sit, in another room or outside the main building of the hospital. I would then let her
calm down for a few minutes. After a while, I would listen to her explain what she wants for her
father. We could then return to the room when she has calmed down. If this technique fails I
would ask help from other staff members such as a fellow nurse. During the whole incident, I
would ask for the assistance of the health worker involved with Aboriginal Liaison to help if the
family permitted it. An interpreter might be important if one of the family members is not fluent
in English. This will require the approval of the family and also if such an individual is not
within the hospital at the time, one of the family members would be called upon to
assist(Carman,2016).
There needs to be a determination of whether Tom can talk or understand what is going on. This
will help assess his capacity to make decisions for himself. It is common for patients at this
period to be agitated or sedated. If this is the case Tom will be unable to decide. However, if he
should be awake and conscious, I will proceed to ask him to tell me his name and then proceed to
ask if he remembers me. Further, I would ask him to nod if he understands or shows me
anywhere he might be feeling pain.
3
7. To provide personalized care to the patient (The state of Victoria,2015)
Action plan
Since Tom’s daughter is angry and agitated, I would tell her what she feels is completely
expected. Then I would ask to talk with her outside for a while. It would be preferable to find a
place to sit, in another room or outside the main building of the hospital. I would then let her
calm down for a few minutes. After a while, I would listen to her explain what she wants for her
father. We could then return to the room when she has calmed down. If this technique fails I
would ask help from other staff members such as a fellow nurse. During the whole incident, I
would ask for the assistance of the health worker involved with Aboriginal Liaison to help if the
family permitted it. An interpreter might be important if one of the family members is not fluent
in English. This will require the approval of the family and also if such an individual is not
within the hospital at the time, one of the family members would be called upon to
assist(Carman,2016).
There needs to be a determination of whether Tom can talk or understand what is going on. This
will help assess his capacity to make decisions for himself. It is common for patients at this
period to be agitated or sedated. If this is the case Tom will be unable to decide. However, if he
should be awake and conscious, I will proceed to ask him to tell me his name and then proceed to
ask if he remembers me. Further, I would ask him to nod if he understands or shows me
anywhere he might be feeling pain.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
TERMINAL STAGE
4
If he remains unresponsive then I would infer he is incapable of understating what is going on
and thus not able to make a decision. There will however need to consult with fellow nurses and
the doctor before declaring him unable to make his own choices. A determination of Tom’s
inability to make a decision would result in me asking for the details of the powers of Attorney
from the daughter. It is important to determine the extent to which Tom allowed her to control
his affairs. It is likely it involved the financial aspects of Tom’s life. In Tasmania, the decisions
of the enduring guardian, as well as those expressed in the advanced care plan, have to be
upheld. (Carter,2016)
Tom’s wife may also not have the total power to determine all treatment options. Since Tom’s
son was not sure if the plan was in place, there needs to be a presentation of the signed
documents with the appropriate witnesses. The Health worker would be key in determining who
is expected to make medical decisions according to the family’s customs. Tom’s wife and
daughter also have to be informed to make the best decision on Tom’s behalf while respecting
his wishes and values.
4
If he remains unresponsive then I would infer he is incapable of understating what is going on
and thus not able to make a decision. There will however need to consult with fellow nurses and
the doctor before declaring him unable to make his own choices. A determination of Tom’s
inability to make a decision would result in me asking for the details of the powers of Attorney
from the daughter. It is important to determine the extent to which Tom allowed her to control
his affairs. It is likely it involved the financial aspects of Tom’s life. In Tasmania, the decisions
of the enduring guardian, as well as those expressed in the advanced care plan, have to be
upheld. (Carter,2016)
Tom’s wife may also not have the total power to determine all treatment options. Since Tom’s
son was not sure if the plan was in place, there needs to be a presentation of the signed
documents with the appropriate witnesses. The Health worker would be key in determining who
is expected to make medical decisions according to the family’s customs. Tom’s wife and
daughter also have to be informed to make the best decision on Tom’s behalf while respecting
his wishes and values.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TERMINAL STAGE
5
I would urge the family to resolve the matter within themselves by use of their set traditions.
They ought to each present what they feel is the best treatment regimen for Tom. A common
ground needs to be found. I would urge the family to talk with Carina about her wishes and then
communicate what they agree to the staff. Working together with the team treating Tom, I would
suggest we shift from Morphine use (Hoffmannet al.,2014).Just like, Tom had got a simplified
explanation of morphine use; I would try to talk to the daughter as well. This would be in simple
terms and emphasizing the great efficacy of morphine as well as side effects. The imminent
death of the patient should also be compared to the expected effects. The need for greater pain
control could necessitate the use of Diamorphine whose effectiveness is three times that of
morphine. While renal or liver toxicity might occur there use is for a limited duration. For pain
relief, opioid analgesics such as oxycodone or methadone would be used. A possible alternative
might be a fentanyl patch which reduces the need for tablets or injections. The choice of drug
depends on the type of pain that the patient has. 4 milligrams of dexamethasone injection via the
subcutaneous route would be given in the morning for musculoskeletal pain (Clark,2017). Tom
could also get a drip if the family agrees or the family representative insists. I would also be
prepared to prescribe any necessary medication as death approaches such as benzodiazepine due
to anxiety or delirium. There is no need to get any laboratory tests and would be discontinued
like the medication (Veal et al.,2014)
There also needs to be consideration of Tom’s state which will inform the routes of
administration chosen. If he is sedated or has obstruction due to vomiting, oral administration is
stopped.The best option is the use of the subcutaneous route of drug injection.A drug to choice
then is hydromorphone.Assessment is also required to determine whether the dosage has to be
altered. Too little of it may not adequately address the pain while a large dosage might make him
5
I would urge the family to resolve the matter within themselves by use of their set traditions.
They ought to each present what they feel is the best treatment regimen for Tom. A common
ground needs to be found. I would urge the family to talk with Carina about her wishes and then
communicate what they agree to the staff. Working together with the team treating Tom, I would
suggest we shift from Morphine use (Hoffmannet al.,2014).Just like, Tom had got a simplified
explanation of morphine use; I would try to talk to the daughter as well. This would be in simple
terms and emphasizing the great efficacy of morphine as well as side effects. The imminent
death of the patient should also be compared to the expected effects. The need for greater pain
control could necessitate the use of Diamorphine whose effectiveness is three times that of
morphine. While renal or liver toxicity might occur there use is for a limited duration. For pain
relief, opioid analgesics such as oxycodone or methadone would be used. A possible alternative
might be a fentanyl patch which reduces the need for tablets or injections. The choice of drug
depends on the type of pain that the patient has. 4 milligrams of dexamethasone injection via the
subcutaneous route would be given in the morning for musculoskeletal pain (Clark,2017). Tom
could also get a drip if the family agrees or the family representative insists. I would also be
prepared to prescribe any necessary medication as death approaches such as benzodiazepine due
to anxiety or delirium. There is no need to get any laboratory tests and would be discontinued
like the medication (Veal et al.,2014)
There also needs to be consideration of Tom’s state which will inform the routes of
administration chosen. If he is sedated or has obstruction due to vomiting, oral administration is
stopped.The best option is the use of the subcutaneous route of drug injection.A drug to choice
then is hydromorphone.Assessment is also required to determine whether the dosage has to be
altered. Too little of it may not adequately address the pain while a large dosage might make him
TERMINAL STAGE
6
drowsy. His previous wish to talk with his family should be honored and thus he ought to be able
to communicate if it remains possible.
The family will also need to know what to expect. I will thus make it clear the various symptoms
associated with the terminal phase. These symptoms include nausea, pain, vomiting, dyspnoea,
agitation and secretions from the respiratory tract. Apart from the feeding challenges being
experienced, Tom might be bowel incontinence. I would offer social support for dressing,
bathing and mouth hygiene. Pain and dyspnoea are critical symptoms. Other possible symptoms
I would cite are fear, sorrow, delirium, despair or a loss of hope (Campos-Calderón et
al.,2016).Tom might also feel that he is being a burden to his family. These are expected but the
presence of the family even though he might not be talking is important. There is a need to
ensure that a family member is with him in his room at all times. Given the large number of
people expected to visit Tom, I would try to ensure visitation periods are flexible.The room
would be well ventilated with the conversation being hopeful and friendly. (Cherny et al.,2015)
I would ask to talk with the individual responsible for health decisions in the family. The non-
resuscitation request has to follow and this has to be understood both by the family and the team
dealing with the case. I would advocate for the request to be adhered to for both ethical and legal
reasons. Continued treatment may not change the situation. The passing on of an individual must
be viewed as inevitable and a natural process. The family also needs to understand it is not
giving up on the patient (Sharma et al.,2011)During this time, I would ensure there is no mention
of Tom’s name to honor the customs of this family. An agreed name has to assign to Tom by the
family for communication. The worsening of symptoms is indicative of impending death.This
might be through the inability to rouse the patient or increased restlessness. Tom’s daughter
needs to be particularly involved so that she may get closure and be able to respond to death. I
6
drowsy. His previous wish to talk with his family should be honored and thus he ought to be able
to communicate if it remains possible.
The family will also need to know what to expect. I will thus make it clear the various symptoms
associated with the terminal phase. These symptoms include nausea, pain, vomiting, dyspnoea,
agitation and secretions from the respiratory tract. Apart from the feeding challenges being
experienced, Tom might be bowel incontinence. I would offer social support for dressing,
bathing and mouth hygiene. Pain and dyspnoea are critical symptoms. Other possible symptoms
I would cite are fear, sorrow, delirium, despair or a loss of hope (Campos-Calderón et
al.,2016).Tom might also feel that he is being a burden to his family. These are expected but the
presence of the family even though he might not be talking is important. There is a need to
ensure that a family member is with him in his room at all times. Given the large number of
people expected to visit Tom, I would try to ensure visitation periods are flexible.The room
would be well ventilated with the conversation being hopeful and friendly. (Cherny et al.,2015)
I would ask to talk with the individual responsible for health decisions in the family. The non-
resuscitation request has to follow and this has to be understood both by the family and the team
dealing with the case. I would advocate for the request to be adhered to for both ethical and legal
reasons. Continued treatment may not change the situation. The passing on of an individual must
be viewed as inevitable and a natural process. The family also needs to understand it is not
giving up on the patient (Sharma et al.,2011)During this time, I would ensure there is no mention
of Tom’s name to honor the customs of this family. An agreed name has to assign to Tom by the
family for communication. The worsening of symptoms is indicative of impending death.This
might be through the inability to rouse the patient or increased restlessness. Tom’s daughter
needs to be particularly involved so that she may get closure and be able to respond to death. I
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
TERMINAL STAGE
7
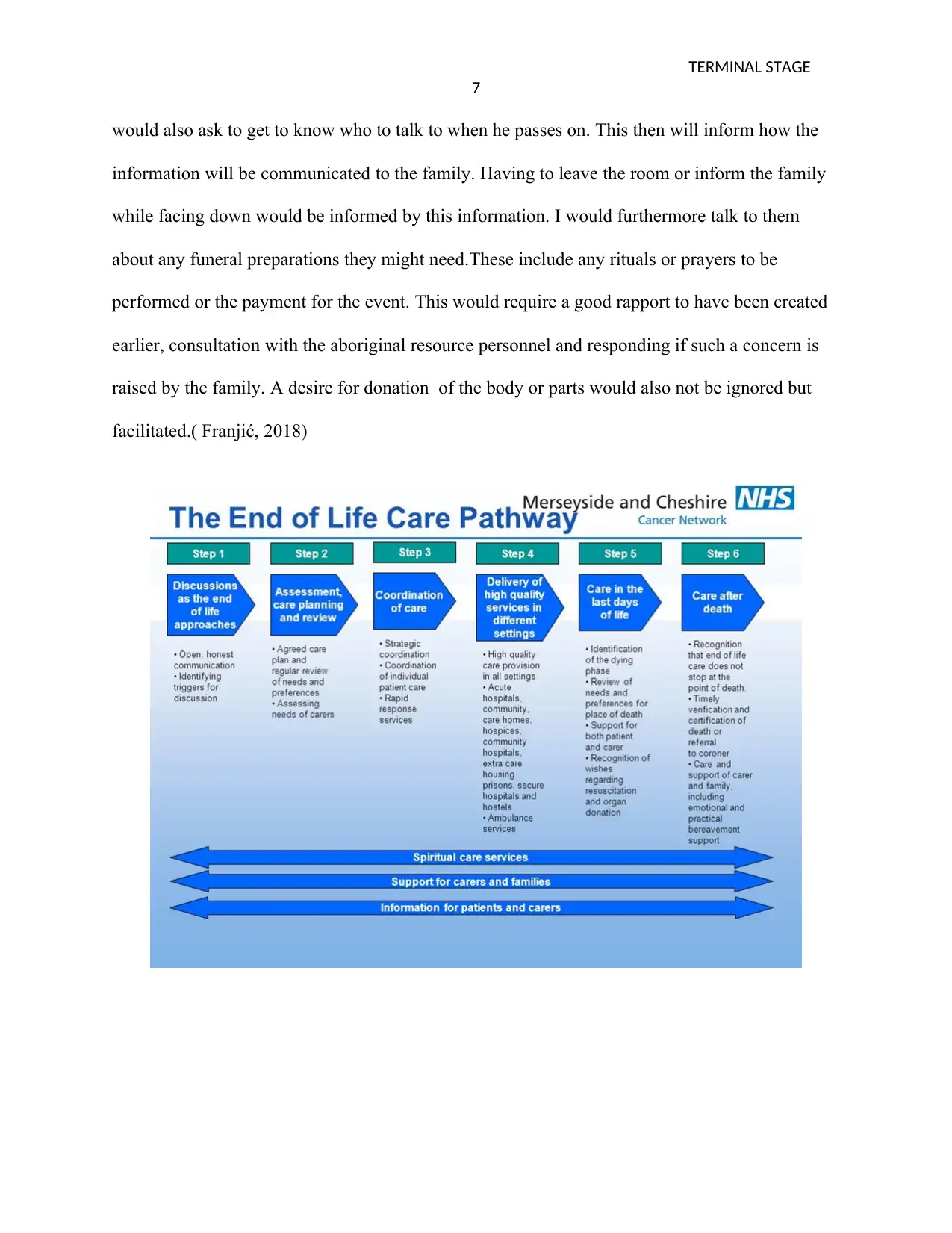
would also ask to get to know who to talk to when he passes on. This then will inform how the
information will be communicated to the family. Having to leave the room or inform the family
while facing down would be informed by this information. I would furthermore talk to them
about any funeral preparations they might need.These include any rituals or prayers to be
performed or the payment for the event. This would require a good rapport to have been created
earlier, consultation with the aboriginal resource personnel and responding if such a concern is
raised by the family. A desire for donation of the body or parts would also not be ignored but
facilitated.( Franjić, 2018)
7
would also ask to get to know who to talk to when he passes on. This then will inform how the
information will be communicated to the family. Having to leave the room or inform the family
while facing down would be informed by this information. I would furthermore talk to them
about any funeral preparations they might need.These include any rituals or prayers to be
performed or the payment for the event. This would require a good rapport to have been created
earlier, consultation with the aboriginal resource personnel and responding if such a concern is
raised by the family. A desire for donation of the body or parts would also not be ignored but
facilitated.( Franjić, 2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TERMINAL STAGE
8
Conclusion
There is a need for involvement of the family in palliative care as well as in terminal cases.
Moreover, the cultural, spiritual and religious views of the patient and the family have to keep in
mind during healthcare provision. (Mitchell,2011)
8
Conclusion
There is a need for involvement of the family in palliative care as well as in terminal cases.
Moreover, the cultural, spiritual and religious views of the patient and the family have to keep in
mind during healthcare provision. (Mitchell,2011)
TERMINAL STAGE
9
References
Campos-Calderón, C., Montoya-Juárez, R., Hueso-Montoro, C. et al.,2016. Interventions and
decision-making at the end of life: the effect of establishing the terminal illness situation.
BMC Palliative Care 15, 91.
Carman, N., 2016. Healthcare Law & Ethics.
Carter, R.Z., Detering, K.M., Silvester, W. and Sutton, E., 2016. Advance care planning in
Australia: what does the law say?Australian Health Review, 40(4), pp.405-414.
Clark ,K,2017. Care at the Very End-of-Life: Dying Cancer Patients and Their Chosen Family’s
Needs.Cancers (Basel). 2017 Feb; 9(2): 11.
Franjić S, 2018. Health Care In The Terminal Phase Of Disease. Palliative Medicine & Care
5(4): 1-5.
Hoffmann, T. C., Légaré, F., Simmons, M.B., McNamara, K., McCaffery, K., Trevena, L.J.,
Hudson, B., Glasziou, P.P, and Del Mar, C, B., 2014.Shared decision making: what do
clinicians need to know and why should they bother?The Medical Journal of Australia
201 (1): 35-39.
Mitchell, G.K., 2011. Palliative care in Australia. Ochsner Journal, 11(4), pp.334-337.
Nathan Cherny, Marie Fallon, Stein Kaasa, Russell K. Portenoy, and David C.
Currow(editors),2015.Textbook of Palliative Medicine (5 ed.)Oxford University Press.
9
References
Campos-Calderón, C., Montoya-Juárez, R., Hueso-Montoro, C. et al.,2016. Interventions and
decision-making at the end of life: the effect of establishing the terminal illness situation.
BMC Palliative Care 15, 91.
Carman, N., 2016. Healthcare Law & Ethics.
Carter, R.Z., Detering, K.M., Silvester, W. and Sutton, E., 2016. Advance care planning in
Australia: what does the law say?Australian Health Review, 40(4), pp.405-414.
Clark ,K,2017. Care at the Very End-of-Life: Dying Cancer Patients and Their Chosen Family’s
Needs.Cancers (Basel). 2017 Feb; 9(2): 11.
Franjić S, 2018. Health Care In The Terminal Phase Of Disease. Palliative Medicine & Care
5(4): 1-5.
Hoffmann, T. C., Légaré, F., Simmons, M.B., McNamara, K., McCaffery, K., Trevena, L.J.,
Hudson, B., Glasziou, P.P, and Del Mar, C, B., 2014.Shared decision making: what do
clinicians need to know and why should they bother?The Medical Journal of Australia
201 (1): 35-39.
Mitchell, G.K., 2011. Palliative care in Australia. Ochsner Journal, 11(4), pp.334-337.
Nathan Cherny, Marie Fallon, Stein Kaasa, Russell K. Portenoy, and David C.
Currow(editors),2015.Textbook of Palliative Medicine (5 ed.)Oxford University Press.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
TERMINAL STAGE
10
Sharma, R.K., Hughes, M.T., Nolan, M.T., Tudor, C., Kub, J., Terry, P.B. and Sulmasy, D.P.,
2011. Family understanding of seriously-ill patient preferences for family involvement in
healthcare decision making. Journal of general internal medicine, 26(8), pp.881-886.
The state of Victoria, Department of Health and Human Services, December 2015.End of life
care Standardized care process.
Thomas, R.L., Zubair, M.Y., Hayes, B. and Ashby, M.A., 2014. Goals of care: a clinical
framework for the limitation of medical treatment. Medical Journal of Australia, 201(8),
pp.452-455.
Veal, F.C., Bereznicki, L.R., Thompson, A.J. and Peterson, G.M., 2014. Pharmacological
management of pain in Australian aged care facilities. Age and aging, 43(6), pp.851-856.
10
Sharma, R.K., Hughes, M.T., Nolan, M.T., Tudor, C., Kub, J., Terry, P.B. and Sulmasy, D.P.,
2011. Family understanding of seriously-ill patient preferences for family involvement in
healthcare decision making. Journal of general internal medicine, 26(8), pp.881-886.
The state of Victoria, Department of Health and Human Services, December 2015.End of life
care Standardized care process.
Thomas, R.L., Zubair, M.Y., Hayes, B. and Ashby, M.A., 2014. Goals of care: a clinical
framework for the limitation of medical treatment. Medical Journal of Australia, 201(8),
pp.452-455.
Veal, F.C., Bereznicki, L.R., Thompson, A.J. and Peterson, G.M., 2014. Pharmacological
management of pain in Australian aged care facilities. Age and aging, 43(6), pp.851-856.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





