HLSC122: EBP Critical Appraisal - Stroke Rehabilitation Case
VerifiedAdded on 2023/06/11
|13
|9741
|459
Case Study
AI Summary
This case study critically appraises a research paper related to supporting a stroke patient's activities of daily living, fulfilling the requirements for HLSC122: Evidence for Practice. The assignment involves a critical evaluation of a research article focusing on evidence-based practice (EBP) in physiotherapy, specifically within the context of stroke rehabilitation. It synthesizes findings on barriers, enablers, and interventions related to EBP implementation by physiotherapists. The study uses a systematic review approach, examining literature from 2000-2012, and involves data extraction, synthesis, and quality appraisal of included articles, highlighting key themes such as attitudes, knowledge, skills, and barriers to EBP adoption. The ultimate goal is to identify methods for enhancing the consistency and quality of EBP implementation in physiotherapy practice.
This article appeared in a journal published by Elsevier. The attached
copy is furnished to the author for internal non-commercial research
and education use, including for instruction at the authors institution
and sharing with colleagues.
Other uses, including reproduction and distribution, or selling or
licensing copies, or posting to personal, institutional or third party
websites are prohibited.
In most cases authors are permitted to post their version of the
article (e.g. in Word or Tex form) to their personal website or
institutional repository. Authors requiring further information
regarding Elsevier’s archiving and manuscript policies are
encouraged to visit:
http://www.elsevier.com/authorsrights
copy is furnished to the author for internal non-commercial research
and education use, including for instruction at the authors institution
and sharing with colleagues.
Other uses, including reproduction and distribution, or selling or
licensing copies, or posting to personal, institutional or third party
websites are prohibited.
In most cases authors are permitted to post their version of the
article (e.g. in Word or Tex form) to their personal website or
institutional repository. Authors requiring further information
regarding Elsevier’s archiving and manuscript policies are
encouraged to visit:
http://www.elsevier.com/authorsrights
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Author's personal copy
Physiotherapy 100 (2014) 208–219
Systematic review
Evidence-Based Practice in physiotherapy: a systematic
review of barriers, enablers and interventions
Laura Scurlock-Evansa,∗, Penney Upton b, Dominic Upton c
a Psychological Sciences, Institute of Health and Society, University of Worcester,Henwick Grove, Worcester WR2 6AJ, UK
b Institute of Health and Society, University of Worcester,Henwick Grove, Worcester WR2 6AJ, UK
c Faculty of Health, University of Canberra, University Dr, Bruce ACT 2617, Australia
Abstract
Background Despite clear benefits of the Evidence-Based Practice (EBP) approach to ensuring quality and consistency of care, its uptake
within physiotherapy has been inconsistent.
Objectives Synthesise the findings of research into EBP barriers, facilitators and interventions in physiotherapy and identify methods of
enhancing adoption and implementation.
Data sources Literature concerning physiotherapists’ practice between 2000 and 2012 was systematically searched using: Academic Search
Complete, Cumulative Index of Nursing and Allied Health Literature Plus, American Psychological Association databases, Medline, Journal
Storage, and Science Direct. Reference lists were searched to identify additional studies.
Study selection Thirty-two studies, focusing either on physiotherapists’ EBP knowledge, attitudes or implementation, or EBP interventions
in physiotherapy were included.
Data extraction and synthesis One author undertook all data extraction and a second author reviewed to ensure consistency and rigour.
Synthesis was organised around the themes of EBP barriers/enablers, attitudes, knowledge/skills, use and interventions.
Results Many physiotherapists hold positive attitudes towards EBP. However, this does not necessarily translate into consistent, high-quality
EBP. Many barriers to EBP implementation are apparent, including: lack of time and skills, and misperceptions of EBP.
Limitations Only studies published in the English language, in peer-reviewed journals were included, thereby introducing possible publication
bias. Furthermore, narrative synthesis may be subject to greater confirmation bias.
Conclusion and implications There is no “one-size fits all” approach to enhancing EBP implementation; assessing organisational culture
prior to designing interventions is crucial. Although some interventions appear promising, further research is required to explore the most
effective methods of supporting physiotherapists’ adoption of EBP.
© 2014 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
Keywords: Evidence-Based Practice; Physiotherapists; Best Practices; Review; Decision Making; Practice-Research Gap
Background
Evidence-Based Practice (EBP) is a 5 step process
whereby clinicians integrate best research evidence with clin-
ical expertise and client preferences, producing the most
appropriate and effective service [1,2]. As a result there has
been growing pressure on physiotherapy to embrace EBP
[3]. Engaging with both research and clinical findings can
enhance the proficiency of physiotherapists’ clinical practice
∗ Corresponding author.
E-mail address: l.scurlock-evans@worc.ac.uk (L. Scurlock-Evans).
[2] and help prevent the misuse, overuse and underuse of
healthcare services [4]. In an era of growing accountability
of healthcare practitioners, this may provide a useful frame-
work within which to work. Indeed, this has led some to argue
that there is a moral obligation to base decision-making on
research findings [3].
Despite the clear benefits of EBP, its uptake within phys-
iotherapy (and other healthcare domains) has been patchy
and inconsistent in quality [5]. Concerns over the compat-
ibility of aspects of EBP and lack of clinically relevant
research [3,6], have been raised by researchers and clinicians
alike.
http://dx.doi.org/10.1016/j.physio.2014.03.001
0031-9406/© 2014 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
Physiotherapy 100 (2014) 208–219
Systematic review
Evidence-Based Practice in physiotherapy: a systematic
review of barriers, enablers and interventions
Laura Scurlock-Evansa,∗, Penney Upton b, Dominic Upton c
a Psychological Sciences, Institute of Health and Society, University of Worcester,Henwick Grove, Worcester WR2 6AJ, UK
b Institute of Health and Society, University of Worcester,Henwick Grove, Worcester WR2 6AJ, UK
c Faculty of Health, University of Canberra, University Dr, Bruce ACT 2617, Australia
Abstract
Background Despite clear benefits of the Evidence-Based Practice (EBP) approach to ensuring quality and consistency of care, its uptake
within physiotherapy has been inconsistent.
Objectives Synthesise the findings of research into EBP barriers, facilitators and interventions in physiotherapy and identify methods of
enhancing adoption and implementation.
Data sources Literature concerning physiotherapists’ practice between 2000 and 2012 was systematically searched using: Academic Search
Complete, Cumulative Index of Nursing and Allied Health Literature Plus, American Psychological Association databases, Medline, Journal
Storage, and Science Direct. Reference lists were searched to identify additional studies.
Study selection Thirty-two studies, focusing either on physiotherapists’ EBP knowledge, attitudes or implementation, or EBP interventions
in physiotherapy were included.
Data extraction and synthesis One author undertook all data extraction and a second author reviewed to ensure consistency and rigour.
Synthesis was organised around the themes of EBP barriers/enablers, attitudes, knowledge/skills, use and interventions.
Results Many physiotherapists hold positive attitudes towards EBP. However, this does not necessarily translate into consistent, high-quality
EBP. Many barriers to EBP implementation are apparent, including: lack of time and skills, and misperceptions of EBP.
Limitations Only studies published in the English language, in peer-reviewed journals were included, thereby introducing possible publication
bias. Furthermore, narrative synthesis may be subject to greater confirmation bias.
Conclusion and implications There is no “one-size fits all” approach to enhancing EBP implementation; assessing organisational culture
prior to designing interventions is crucial. Although some interventions appear promising, further research is required to explore the most
effective methods of supporting physiotherapists’ adoption of EBP.
© 2014 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
Keywords: Evidence-Based Practice; Physiotherapists; Best Practices; Review; Decision Making; Practice-Research Gap
Background
Evidence-Based Practice (EBP) is a 5 step process
whereby clinicians integrate best research evidence with clin-
ical expertise and client preferences, producing the most
appropriate and effective service [1,2]. As a result there has
been growing pressure on physiotherapy to embrace EBP
[3]. Engaging with both research and clinical findings can
enhance the proficiency of physiotherapists’ clinical practice
∗ Corresponding author.
E-mail address: l.scurlock-evans@worc.ac.uk (L. Scurlock-Evans).
[2] and help prevent the misuse, overuse and underuse of
healthcare services [4]. In an era of growing accountability
of healthcare practitioners, this may provide a useful frame-
work within which to work. Indeed, this has led some to argue
that there is a moral obligation to base decision-making on
research findings [3].
Despite the clear benefits of EBP, its uptake within phys-
iotherapy (and other healthcare domains) has been patchy
and inconsistent in quality [5]. Concerns over the compat-
ibility of aspects of EBP and lack of clinically relevant
research [3,6], have been raised by researchers and clinicians
alike.
http://dx.doi.org/10.1016/j.physio.2014.03.001
0031-9406/© 2014 Chartered Society of Physiotherapy. Published by Elsevier Ltd. All rights reserved.
Author's personal copy
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 209
Objectives
Research has identified a number of challenges phy-
siotherapists face when implementing EBP [6], which are
sometimes inconsistent. This review aimed to synthesise
research findings regarding barriers and enablers of EBP, and
the effectiveness of current EBP interventions in physiother-
apy, to help identify methods of increasing the consistency
and quality of EBP implementation.
Method
The review followed the PRISMA guidelines [7] for
reporting systematic reviews. A narrative analysis approach
was adopted, whereby text is used to summarise and explain
review synthesis findings, as it is suitably flexible to allow
for the inclusion of diverse methodologies.
Data sources
Literature concerning physiotherapists’ practice between
2000 and 2012 was systematically searched using free-text
keywords and MeSH or equivalent terms in combination (see
Table S1). Reference lists were searched to identify additional
studies.
Study selection
Articles were initially reviewed according to the following
inclusion criteria;
• Published in a peer-reviewed journal in English;
• Published between 2002 and 2012;
• Primary research conducted with qualified physiothera-
pists;
• Focused on at least one of the following;
- Physiotherapists’ knowledge/understanding of EBP
- Physiotherapists’ attitudes towards EBP
- Physiotherapists’ practice/implementation of EBP.
- EBP interventions in Physiotherapy.
To enhance comparability of researching findings, only
studies from the following Western cultures/regions were
included: UK, Ireland, Europe, USA, Canada, Australia and
New Zealand.
In total, 32 articles were retrieved that met the criteria; 27
used a quantitative method, 3 used a qualitative method and 2
used mixed-methods designs. A flow chart of study retrieval
and selection is presented in Fig. S1.
Data extraction and synthesis
One author undertook all data extraction using a
pre-defined template, and a second reviewed to ensure
consistency and rigour. Synthesis was organised around the
themes of EBP barriers/enablers, attitudes, knowledge/skills,
use and interventions.
Quality appraisal
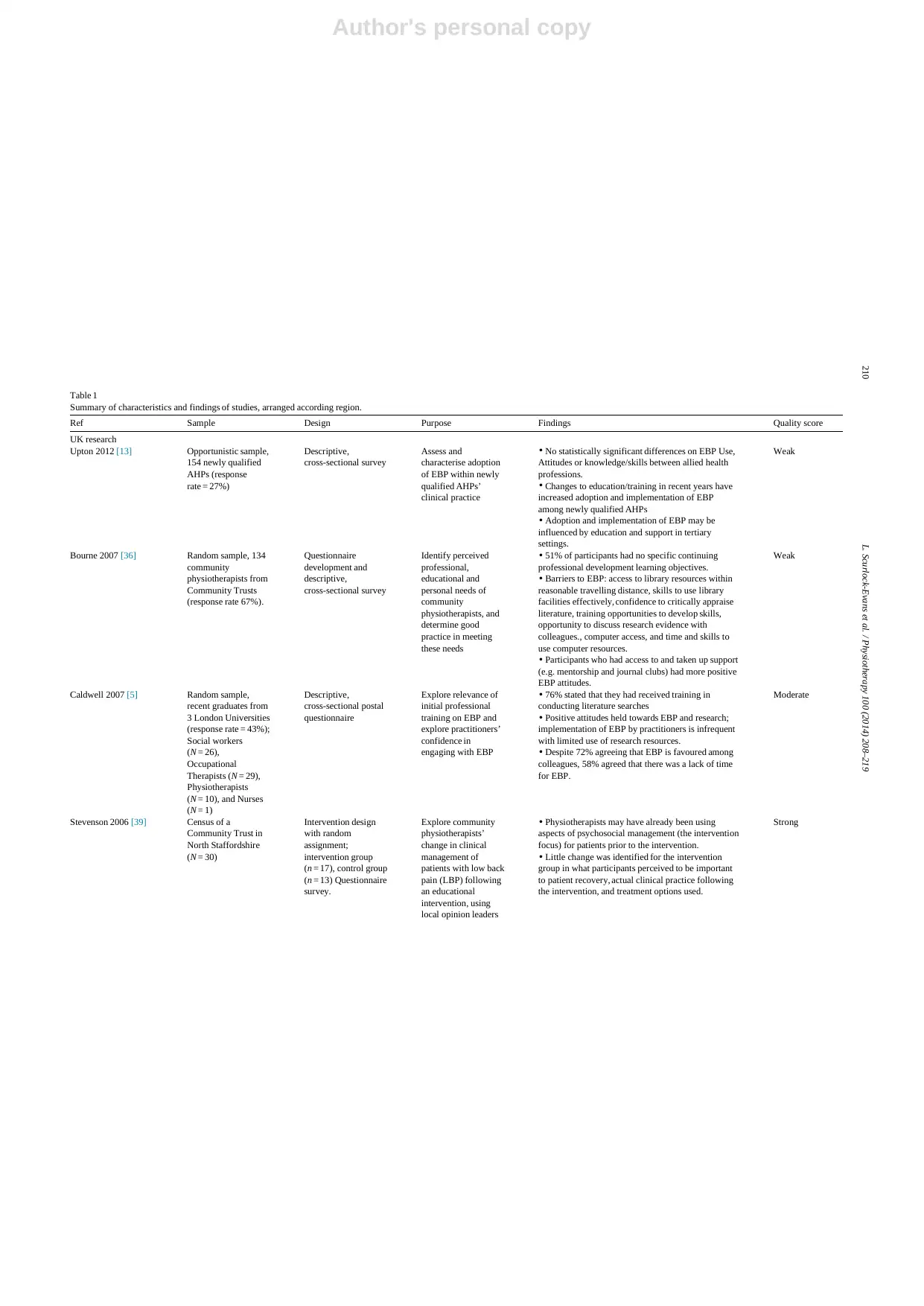
Quantitative articles were assessed using the Effective
Public Health Practice Project (EPHPP; [8]) tool: each study
was rated as strong, moderate or weak (see Table 1). Quali-
tative articles were appraised using the consolidated criteria
for reporting qualitative research (COREQ; [9]), modified
to rate articles as strong, moderate or weak. Mixed-methods
research was evaluated using both tools.
Results
Despite known variations between countries’ healthcare
provision a number of key themes were evident, suggesting
they represent factors common to the practice of physiother-
apy across contexts; as there were no obvious systematic
differences in the characteristics of the research across
regions or publication date, the results were structured around
these themes. However, to aid with interpretation Table 1
presents studies’ characteristics and findings by region and
date.
Practice of EBP
Some studies compared physiotherapists’ practice of
EBP with professionals’ from other healthcare domains.
Palfreyman et al. [10] found that although both nurses
and physiotherapists had access to a broad range of EBP
knowledge sources, physiotherapists used such sources and
implemented EBP more frequently. However, both pro-
fessions relied significantly on patients and colleagues as
knowledge sources.
In a study comparing Swedish physiotherapists, dieti-
cians and occupational therapists, physiotherapists read and
reviewed research more often and were more likely to say
EBP helped them with decision-making [11]. Complex dif-
ferences between physiotherapists’ and other allied health
professionals’ (AHPs) were identified in a UK sample [12];
physiotherapists outperformed on some aspects, such as iden-
tifying relevant research, but performed less well on others,
such as identifying knowledge-gaps. However, other research
with UK-based AHPs (physiotherapists, speech and language
therapists, occupational therapists, dieticians, radiographers
and podiatrists) found no statistically significant differences
in EBP implementation, attitudes, or knowledge and skills
[13]. These discrepancies may be explained by differences
in level of academic preparation and access to educational
initiatives (e.g. all professionals in [13]’s study had
access to a professional development programme, poten-
tially increasing consistency in EBP), and changes to EBP
teaching.
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 209
Objectives
Research has identified a number of challenges phy-
siotherapists face when implementing EBP [6], which are
sometimes inconsistent. This review aimed to synthesise
research findings regarding barriers and enablers of EBP, and
the effectiveness of current EBP interventions in physiother-
apy, to help identify methods of increasing the consistency
and quality of EBP implementation.
Method
The review followed the PRISMA guidelines [7] for
reporting systematic reviews. A narrative analysis approach
was adopted, whereby text is used to summarise and explain
review synthesis findings, as it is suitably flexible to allow
for the inclusion of diverse methodologies.
Data sources
Literature concerning physiotherapists’ practice between
2000 and 2012 was systematically searched using free-text
keywords and MeSH or equivalent terms in combination (see
Table S1). Reference lists were searched to identify additional
studies.
Study selection
Articles were initially reviewed according to the following
inclusion criteria;
• Published in a peer-reviewed journal in English;
• Published between 2002 and 2012;
• Primary research conducted with qualified physiothera-
pists;
• Focused on at least one of the following;
- Physiotherapists’ knowledge/understanding of EBP
- Physiotherapists’ attitudes towards EBP
- Physiotherapists’ practice/implementation of EBP.
- EBP interventions in Physiotherapy.
To enhance comparability of researching findings, only
studies from the following Western cultures/regions were
included: UK, Ireland, Europe, USA, Canada, Australia and
New Zealand.
In total, 32 articles were retrieved that met the criteria; 27
used a quantitative method, 3 used a qualitative method and 2
used mixed-methods designs. A flow chart of study retrieval
and selection is presented in Fig. S1.
Data extraction and synthesis
One author undertook all data extraction using a
pre-defined template, and a second reviewed to ensure
consistency and rigour. Synthesis was organised around the
themes of EBP barriers/enablers, attitudes, knowledge/skills,
use and interventions.
Quality appraisal
Quantitative articles were assessed using the Effective
Public Health Practice Project (EPHPP; [8]) tool: each study
was rated as strong, moderate or weak (see Table 1). Quali-
tative articles were appraised using the consolidated criteria
for reporting qualitative research (COREQ; [9]), modified
to rate articles as strong, moderate or weak. Mixed-methods
research was evaluated using both tools.
Results
Despite known variations between countries’ healthcare
provision a number of key themes were evident, suggesting
they represent factors common to the practice of physiother-
apy across contexts; as there were no obvious systematic
differences in the characteristics of the research across
regions or publication date, the results were structured around
these themes. However, to aid with interpretation Table 1
presents studies’ characteristics and findings by region and
date.
Practice of EBP
Some studies compared physiotherapists’ practice of
EBP with professionals’ from other healthcare domains.
Palfreyman et al. [10] found that although both nurses
and physiotherapists had access to a broad range of EBP
knowledge sources, physiotherapists used such sources and
implemented EBP more frequently. However, both pro-
fessions relied significantly on patients and colleagues as
knowledge sources.
In a study comparing Swedish physiotherapists, dieti-
cians and occupational therapists, physiotherapists read and
reviewed research more often and were more likely to say
EBP helped them with decision-making [11]. Complex dif-
ferences between physiotherapists’ and other allied health
professionals’ (AHPs) were identified in a UK sample [12];
physiotherapists outperformed on some aspects, such as iden-
tifying relevant research, but performed less well on others,
such as identifying knowledge-gaps. However, other research
with UK-based AHPs (physiotherapists, speech and language
therapists, occupational therapists, dieticians, radiographers
and podiatrists) found no statistically significant differences
in EBP implementation, attitudes, or knowledge and skills
[13]. These discrepancies may be explained by differences
in level of academic preparation and access to educational
initiatives (e.g. all professionals in [13]’s study had
access to a professional development programme, poten-
tially increasing consistency in EBP), and changes to EBP
teaching.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Author's personal copy
210 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Table 1
Summary of characteristics and findings of studies, arranged according region.
Ref Sample Design Purpose Findings Quality score
UK research
Upton 2012 [13] Opportunistic sample,
154 newly qualified
AHPs (response
rate = 27%)
Descriptive,
cross-sectional survey
Assess and
characterise adoption
of EBP within newly
qualified AHPs’
clinical practice
• No statistically significant differences on EBP Use,
Attitudes or knowledge/skills between allied health
professions.
• Changes to education/training in recent years have
increased adoption and implementation of EBP
among newly qualified AHPs
• Adoption and implementation of EBP may be
influenced by education and support in tertiary
settings.
Weak
Bourne 2007 [36] Random sample, 134
community
physiotherapists from
Community Trusts
(response rate 67%).
Questionnaire
development and
descriptive,
cross-sectional survey
Identify perceived
professional,
educational and
personal needs of
community
physiotherapists, and
determine good
practice in meeting
these needs
• 51% of participants had no specific continuing
professional development learning objectives.
• Barriers to EBP: access to library resources within
reasonable travelling distance, skills to use library
facilities effectively, confidence to critically appraise
literature, training opportunities to develop skills,
opportunity to discuss research evidence with
colleagues., computer access, and time and skills to
use computer resources.
• Participants who had access to and taken up support
(e.g. mentorship and journal clubs) had more positive
EBP attitudes.
Weak
Caldwell 2007 [5] Random sample,
recent graduates from
3 London Universities
(response rate = 43%);
Social workers
(N = 26),
Occupational
Therapists (N = 29),
Physiotherapists
(N = 10), and Nurses
(N = 1)
Descriptive,
cross-sectional postal
questionnaire
Explore relevance of
initial professional
training on EBP and
explore practitioners’
confidence in
engaging with EBP
• 76% stated that they had received training in
conducting literature searches
• Positive attitudes held towards EBP and research;
implementation of EBP by practitioners is infrequent
with limited use of research resources.
• Despite 72% agreeing that EBP is favoured among
colleagues, 58% agreed that there was a lack of time
for EBP.
Moderate
Stevenson 2006 [39] Census of a
Community Trust in
North Staffordshire
(N = 30)
Intervention design
with random
assignment;
intervention group
(n = 17), control group
(n = 13) Questionnaire
survey.
Explore community
physiotherapists’
change in clinical
management of
patients with low back
pain (LBP) following
an educational
intervention, using
local opinion leaders
• Physiotherapists may have already been using
aspects of psychosocial management (the intervention
focus) for patients prior to the intervention.
• Little change was identified for the intervention
group in what participants perceived to be important
to patient recovery, actual clinical practice following
the intervention, and treatment options used.
Strong
210 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Table 1
Summary of characteristics and findings of studies, arranged according region.
Ref Sample Design Purpose Findings Quality score
UK research
Upton 2012 [13] Opportunistic sample,
154 newly qualified
AHPs (response
rate = 27%)
Descriptive,
cross-sectional survey
Assess and
characterise adoption
of EBP within newly
qualified AHPs’
clinical practice
• No statistically significant differences on EBP Use,
Attitudes or knowledge/skills between allied health
professions.
• Changes to education/training in recent years have
increased adoption and implementation of EBP
among newly qualified AHPs
• Adoption and implementation of EBP may be
influenced by education and support in tertiary
settings.
Weak
Bourne 2007 [36] Random sample, 134
community
physiotherapists from
Community Trusts
(response rate 67%).
Questionnaire
development and
descriptive,
cross-sectional survey
Identify perceived
professional,
educational and
personal needs of
community
physiotherapists, and
determine good
practice in meeting
these needs
• 51% of participants had no specific continuing
professional development learning objectives.
• Barriers to EBP: access to library resources within
reasonable travelling distance, skills to use library
facilities effectively, confidence to critically appraise
literature, training opportunities to develop skills,
opportunity to discuss research evidence with
colleagues., computer access, and time and skills to
use computer resources.
• Participants who had access to and taken up support
(e.g. mentorship and journal clubs) had more positive
EBP attitudes.
Weak
Caldwell 2007 [5] Random sample,
recent graduates from
3 London Universities
(response rate = 43%);
Social workers
(N = 26),
Occupational
Therapists (N = 29),
Physiotherapists
(N = 10), and Nurses
(N = 1)
Descriptive,
cross-sectional postal
questionnaire
Explore relevance of
initial professional
training on EBP and
explore practitioners’
confidence in
engaging with EBP
• 76% stated that they had received training in
conducting literature searches
• Positive attitudes held towards EBP and research;
implementation of EBP by practitioners is infrequent
with limited use of research resources.
• Despite 72% agreeing that EBP is favoured among
colleagues, 58% agreed that there was a lack of time
for EBP.
Moderate
Stevenson 2006 [39] Census of a
Community Trust in
North Staffordshire
(N = 30)
Intervention design
with random
assignment;
intervention group
(n = 17), control group
(n = 13) Questionnaire
survey.
Explore community
physiotherapists’
change in clinical
management of
patients with low back
pain (LBP) following
an educational
intervention, using
local opinion leaders
• Physiotherapists may have already been using
aspects of psychosocial management (the intervention
focus) for patients prior to the intervention.
• Little change was identified for the intervention
group in what participants perceived to be important
to patient recovery, actual clinical practice following
the intervention, and treatment options used.
Strong
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Author's personal copy
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 211
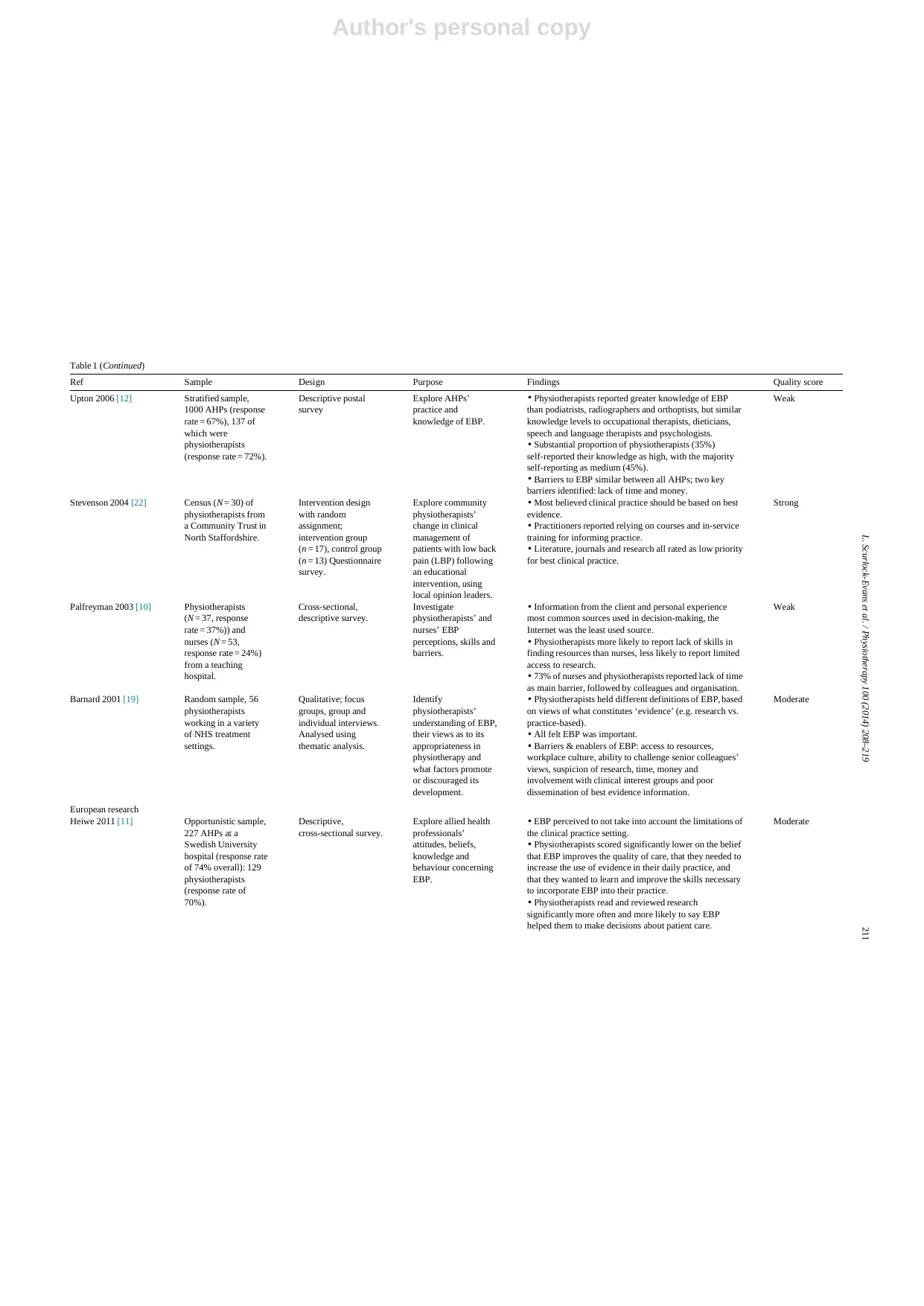
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Upton 2006 [12] Stratified sample,
1000 AHPs (response
rate = 67%), 137 of
which were
physiotherapists
(response rate = 72%).
Descriptive postal
survey
Explore AHPs’
practice and
knowledge of EBP.
• Physiotherapists reported greater knowledge of EBP
than podiatrists, radiographers and orthoptists, but similar
knowledge levels to occupational therapists, dieticians,
speech and language therapists and psychologists.
• Substantial proportion of physiotherapists (35%)
self-reported their knowledge as high, with the majority
self-reporting as medium (45%).
• Barriers to EBP similar between all AHPs; two key
barriers identified: lack of time and money.
Weak
Stevenson 2004 [22] Census (N = 30) of
physiotherapists from
a Community Trust in
North Staffordshire.
Intervention design
with random
assignment;
intervention group
(n = 17), control group
(n = 13) Questionnaire
survey.
Explore community
physiotherapists’
change in clinical
management of
patients with low back
pain (LBP) following
an educational
intervention, using
local opinion leaders.
• Most believed clinical practice should be based on best
evidence.
• Practitioners reported relying on courses and in-service
training for informing practice.
• Literature, journals and research all rated as low priority
for best clinical practice.
Strong
Palfreyman 2003 [10] Physiotherapists
(N = 37, response
rate = 37%)) and
nurses (N = 53,
response rate = 24%)
from a teaching
hospital.
Cross-sectional,
descriptive survey.
Investigate
physiotherapists’ and
nurses’ EBP
perceptions, skills and
barriers.
• Information from the client and personal experience
most common sources used in decision-making, the
Internet was the least used source.
• Physiotherapists more likely to report lack of skills in
finding resources than nurses, less likely to report limited
access to research.
• 73% of nurses and physiotherapists reported lack of time
as main barrier, followed by colleagues and organisation.
Weak
Barnard 2001 [19] Random sample, 56
physiotherapists
working in a variety
of NHS treatment
settings.
Qualitative; focus
groups, group and
individual interviews.
Analysed using
thematic analysis.
Identify
physiotherapists’
understanding of EBP,
their views as to its
appropriateness in
physiotherapy and
what factors promote
or discouraged its
development.
• Physiotherapists held different definitions of EBP, based
on views of what constitutes ‘evidence’ (e.g. research vs.
practice-based).
• All felt EBP was important.
• Barriers & enablers of EBP: access to resources,
workplace culture, ability to challenge senior colleagues’
views, suspicion of research, time, money and
involvement with clinical interest groups and poor
dissemination of best evidence information.
Moderate
European research
Heiwe 2011 [11] Opportunistic sample,
227 AHPs at a
Swedish University
hospital (response rate
of 74% overall): 129
physiotherapists
(response rate of
70%).
Descriptive,
cross-sectional survey.
Explore allied health
professionals’
attitudes, beliefs,
knowledge and
behaviour concerning
EBP.
• EBP perceived to not take into account the limitations of
the clinical practice setting.
• Physiotherapists scored significantly lower on the belief
that EBP improves the quality of care, that they needed to
increase the use of evidence in their daily practice, and
that they wanted to learn and improve the skills necessary
to incorporate EBP into their practice.
• Physiotherapists read and reviewed research
significantly more often and more likely to say EBP
helped them to make decisions about patient care.
Moderate
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 211
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Upton 2006 [12] Stratified sample,
1000 AHPs (response
rate = 67%), 137 of
which were
physiotherapists
(response rate = 72%).
Descriptive postal
survey
Explore AHPs’
practice and
knowledge of EBP.
• Physiotherapists reported greater knowledge of EBP
than podiatrists, radiographers and orthoptists, but similar
knowledge levels to occupational therapists, dieticians,
speech and language therapists and psychologists.
• Substantial proportion of physiotherapists (35%)
self-reported their knowledge as high, with the majority
self-reporting as medium (45%).
• Barriers to EBP similar between all AHPs; two key
barriers identified: lack of time and money.
Weak
Stevenson 2004 [22] Census (N = 30) of
physiotherapists from
a Community Trust in
North Staffordshire.
Intervention design
with random
assignment;
intervention group
(n = 17), control group
(n = 13) Questionnaire
survey.
Explore community
physiotherapists’
change in clinical
management of
patients with low back
pain (LBP) following
an educational
intervention, using
local opinion leaders.
• Most believed clinical practice should be based on best
evidence.
• Practitioners reported relying on courses and in-service
training for informing practice.
• Literature, journals and research all rated as low priority
for best clinical practice.
Strong
Palfreyman 2003 [10] Physiotherapists
(N = 37, response
rate = 37%)) and
nurses (N = 53,
response rate = 24%)
from a teaching
hospital.
Cross-sectional,
descriptive survey.
Investigate
physiotherapists’ and
nurses’ EBP
perceptions, skills and
barriers.
• Information from the client and personal experience
most common sources used in decision-making, the
Internet was the least used source.
• Physiotherapists more likely to report lack of skills in
finding resources than nurses, less likely to report limited
access to research.
• 73% of nurses and physiotherapists reported lack of time
as main barrier, followed by colleagues and organisation.
Weak
Barnard 2001 [19] Random sample, 56
physiotherapists
working in a variety
of NHS treatment
settings.
Qualitative; focus
groups, group and
individual interviews.
Analysed using
thematic analysis.
Identify
physiotherapists’
understanding of EBP,
their views as to its
appropriateness in
physiotherapy and
what factors promote
or discouraged its
development.
• Physiotherapists held different definitions of EBP, based
on views of what constitutes ‘evidence’ (e.g. research vs.
practice-based).
• All felt EBP was important.
• Barriers & enablers of EBP: access to resources,
workplace culture, ability to challenge senior colleagues’
views, suspicion of research, time, money and
involvement with clinical interest groups and poor
dissemination of best evidence information.
Moderate
European research
Heiwe 2011 [11] Opportunistic sample,
227 AHPs at a
Swedish University
hospital (response rate
of 74% overall): 129
physiotherapists
(response rate of
70%).
Descriptive,
cross-sectional survey.
Explore allied health
professionals’
attitudes, beliefs,
knowledge and
behaviour concerning
EBP.
• EBP perceived to not take into account the limitations of
the clinical practice setting.
• Physiotherapists scored significantly lower on the belief
that EBP improves the quality of care, that they needed to
increase the use of evidence in their daily practice, and
that they wanted to learn and improve the skills necessary
to incorporate EBP into their practice.
• Physiotherapists read and reviewed research
significantly more often and more likely to say EBP
helped them to make decisions about patient care.
Moderate
Author's personal copy
212 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
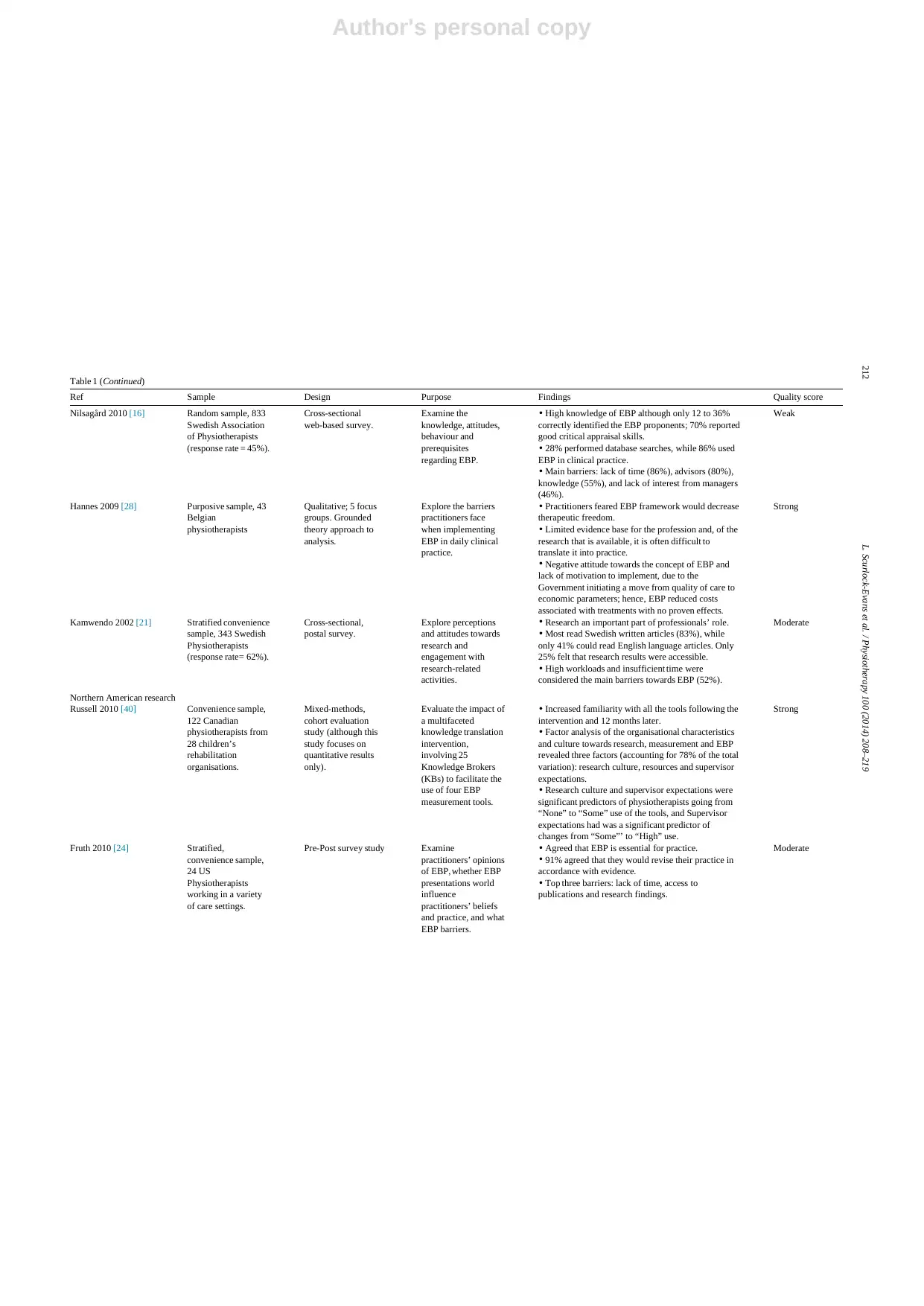
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Nilsagård 2010 [16] Random sample, 833
Swedish Association
of Physiotherapists
(response rate = 45%).
Cross-sectional
web-based survey.
Examine the
knowledge, attitudes,
behaviour and
prerequisites
regarding EBP.
• High knowledge of EBP although only 12 to 36%
correctly identified the EBP proponents; 70% reported
good critical appraisal skills.
• 28% performed database searches, while 86% used
EBP in clinical practice.
• Main barriers: lack of time (86%), advisors (80%),
knowledge (55%), and lack of interest from managers
(46%).
Weak
Hannes 2009 [28] Purposive sample, 43
Belgian
physiotherapists
Qualitative; 5 focus
groups. Grounded
theory approach to
analysis.
Explore the barriers
practitioners face
when implementing
EBP in daily clinical
practice.
• Practitioners feared EBP framework would decrease
therapeutic freedom.
• Limited evidence base for the profession and, of the
research that is available, it is often difficult to
translate it into practice.
• Negative attitude towards the concept of EBP and
lack of motivation to implement, due to the
Government initiating a move from quality of care to
economic parameters; hence, EBP reduced costs
associated with treatments with no proven effects.
Strong
Kamwendo 2002 [21] Stratified convenience
sample, 343 Swedish
Physiotherapists
(response rate= 62%).
Cross-sectional,
postal survey.
Explore perceptions
and attitudes towards
research and
engagement with
research-related
activities.
• Research an important part of professionals’ role.
• Most read Swedish written articles (83%), while
only 41% could read English language articles. Only
25% felt that research results were accessible.
• High workloads and insufficient time were
considered the main barriers towards EBP (52%).
Moderate
Northern American research
Russell 2010 [40] Convenience sample,
122 Canadian
physiotherapists from
28 children’s
rehabilitation
organisations.
Mixed-methods,
cohort evaluation
study (although this
study focuses on
quantitative results
only).
Evaluate the impact of
a multifaceted
knowledge translation
intervention,
involving 25
Knowledge Brokers
(KBs) to facilitate the
use of four EBP
measurement tools.
• Increased familiarity with all the tools following the
intervention and 12 months later.
• Factor analysis of the organisational characteristics
and culture towards research, measurement and EBP
revealed three factors (accounting for 78% of the total
variation): research culture, resources and supervisor
expectations.
• Research culture and supervisor expectations were
significant predictors of physiotherapists going from
“None” to “Some” use of the tools, and Supervisor
expectations had was a significant predictor of
changes from “Some”’ to “High” use.
Strong
Fruth 2010 [24] Stratified,
convenience sample,
24 US
Physiotherapists
working in a variety
of care settings.
Pre-Post survey study Examine
practitioners’ opinions
of EBP, whether EBP
presentations world
influence
practitioners’ beliefs
and practice, and what
EBP barriers.
• Agreed that EBP is essential for practice.
• 91% agreed that they would revise their practice in
accordance with evidence.
• Top three barriers: lack of time, access to
publications and research findings.
Moderate
212 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Nilsagård 2010 [16] Random sample, 833
Swedish Association
of Physiotherapists
(response rate = 45%).
Cross-sectional
web-based survey.
Examine the
knowledge, attitudes,
behaviour and
prerequisites
regarding EBP.
• High knowledge of EBP although only 12 to 36%
correctly identified the EBP proponents; 70% reported
good critical appraisal skills.
• 28% performed database searches, while 86% used
EBP in clinical practice.
• Main barriers: lack of time (86%), advisors (80%),
knowledge (55%), and lack of interest from managers
(46%).
Weak
Hannes 2009 [28] Purposive sample, 43
Belgian
physiotherapists
Qualitative; 5 focus
groups. Grounded
theory approach to
analysis.
Explore the barriers
practitioners face
when implementing
EBP in daily clinical
practice.
• Practitioners feared EBP framework would decrease
therapeutic freedom.
• Limited evidence base for the profession and, of the
research that is available, it is often difficult to
translate it into practice.
• Negative attitude towards the concept of EBP and
lack of motivation to implement, due to the
Government initiating a move from quality of care to
economic parameters; hence, EBP reduced costs
associated with treatments with no proven effects.
Strong
Kamwendo 2002 [21] Stratified convenience
sample, 343 Swedish
Physiotherapists
(response rate= 62%).
Cross-sectional,
postal survey.
Explore perceptions
and attitudes towards
research and
engagement with
research-related
activities.
• Research an important part of professionals’ role.
• Most read Swedish written articles (83%), while
only 41% could read English language articles. Only
25% felt that research results were accessible.
• High workloads and insufficient time were
considered the main barriers towards EBP (52%).
Moderate
Northern American research
Russell 2010 [40] Convenience sample,
122 Canadian
physiotherapists from
28 children’s
rehabilitation
organisations.
Mixed-methods,
cohort evaluation
study (although this
study focuses on
quantitative results
only).
Evaluate the impact of
a multifaceted
knowledge translation
intervention,
involving 25
Knowledge Brokers
(KBs) to facilitate the
use of four EBP
measurement tools.
• Increased familiarity with all the tools following the
intervention and 12 months later.
• Factor analysis of the organisational characteristics
and culture towards research, measurement and EBP
revealed three factors (accounting for 78% of the total
variation): research culture, resources and supervisor
expectations.
• Research culture and supervisor expectations were
significant predictors of physiotherapists going from
“None” to “Some” use of the tools, and Supervisor
expectations had was a significant predictor of
changes from “Some”’ to “High” use.
Strong
Fruth 2010 [24] Stratified,
convenience sample,
24 US
Physiotherapists
working in a variety
of care settings.
Pre-Post survey study Examine
practitioners’ opinions
of EBP, whether EBP
presentations world
influence
practitioners’ beliefs
and practice, and what
EBP barriers.
• Agreed that EBP is essential for practice.
• 91% agreed that they would revise their practice in
accordance with evidence.
• Top three barriers: lack of time, access to
publications and research findings.
Moderate
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Author's personal copy
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 213
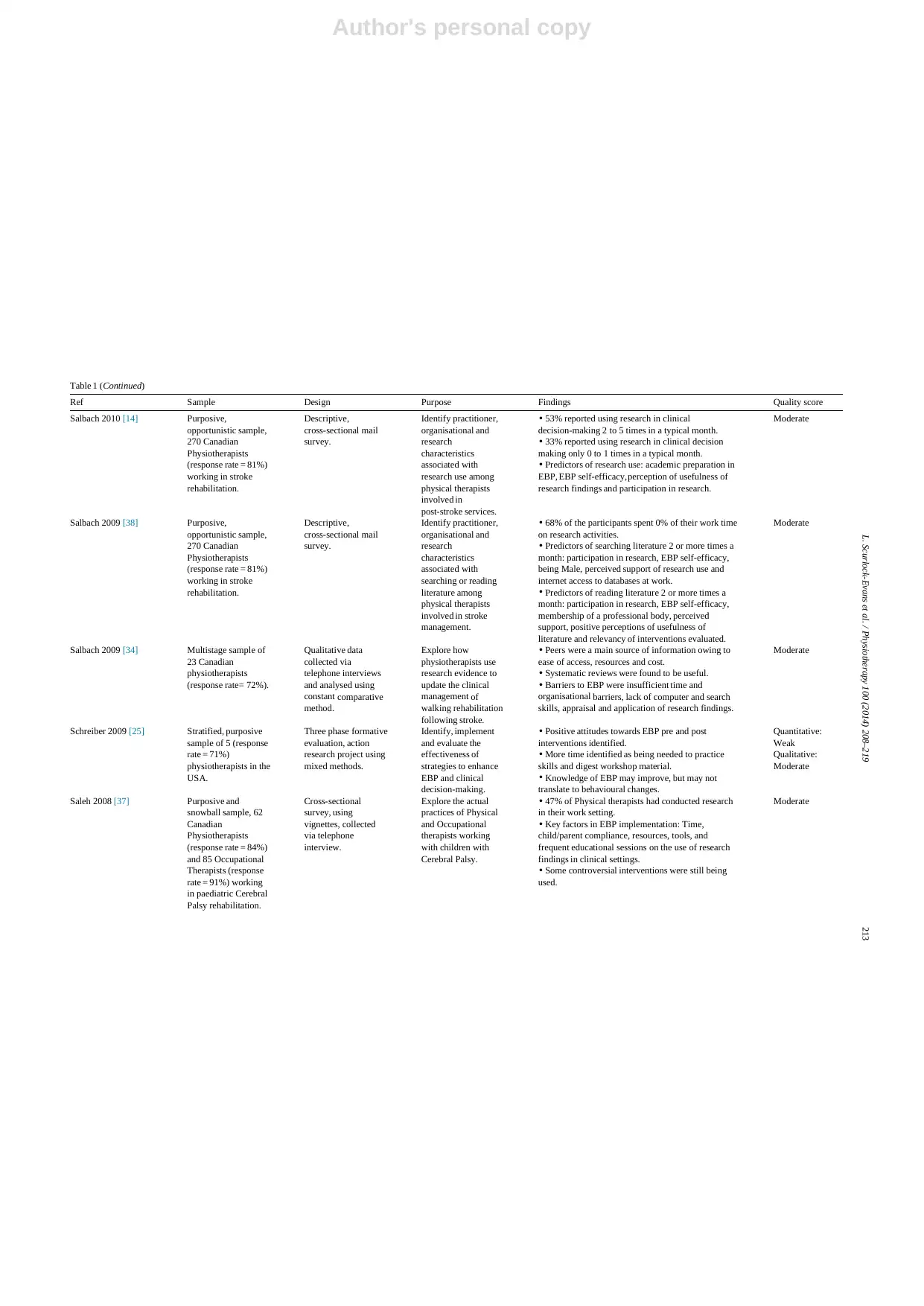
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Salbach 2010 [14] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner,
organisational and
research
characteristics
associated with
research use among
physical therapists
involved in
post-stroke services.
• 53% reported using research in clinical
decision-making 2 to 5 times in a typical month.
• 33% reported using research in clinical decision
making only 0 to 1 times in a typical month.
• Predictors of research use: academic preparation in
EBP, EBP self-efficacy, perception of usefulness of
research findings and participation in research.
Moderate
Salbach 2009 [38] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner,
organisational and
research
characteristics
associated with
searching or reading
literature among
physical therapists
involved in stroke
management.
• 68% of the participants spent 0% of their work time
on research activities.
• Predictors of searching literature 2 or more times a
month: participation in research, EBP self-efficacy,
being Male, perceived support of research use and
internet access to databases at work.
• Predictors of reading literature 2 or more times a
month: participation in research, EBP self-efficacy,
membership of a professional body, perceived
support, positive perceptions of usefulness of
literature and relevancy of interventions evaluated.
Moderate
Salbach 2009 [34] Multistage sample of
23 Canadian
physiotherapists
(response rate= 72%).
Qualitative data
collected via
telephone interviews
and analysed using
constant comparative
method.
Explore how
physiotherapists use
research evidence to
update the clinical
management of
walking rehabilitation
following stroke.
• Peers were a main source of information owing to
ease of access, resources and cost.
• Systematic reviews were found to be useful.
• Barriers to EBP were insufficient time and
organisational barriers, lack of computer and search
skills, appraisal and application of research findings.
Moderate
Schreiber 2009 [25] Stratified, purposive
sample of 5 (response
rate = 71%)
physiotherapists in the
USA.
Three phase formative
evaluation, action
research project using
mixed methods.
Identify, implement
and evaluate the
effectiveness of
strategies to enhance
EBP and clinical
decision-making.
• Positive attitudes towards EBP pre and post
interventions identified.
• More time identified as being needed to practice
skills and digest workshop material.
• Knowledge of EBP may improve, but may not
translate to behavioural changes.
Quantitative:
Weak
Qualitative:
Moderate
Saleh 2008 [37] Purposive and
snowball sample, 62
Canadian
Physiotherapists
(response rate = 84%)
and 85 Occupational
Therapists (response
rate = 91%) working
in paediatric Cerebral
Palsy rehabilitation.
Cross-sectional
survey, using
vignettes, collected
via telephone
interview.
Explore the actual
practices of Physical
and Occupational
therapists working
with children with
Cerebral Palsy.
• 47% of Physical therapists had conducted research
in their work setting.
• Key factors in EBP implementation: Time,
child/parent compliance, resources, tools, and
frequent educational sessions on the use of research
findings in clinical settings.
• Some controversial interventions were still being
used.
Moderate
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 213
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Salbach 2010 [14] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner,
organisational and
research
characteristics
associated with
research use among
physical therapists
involved in
post-stroke services.
• 53% reported using research in clinical
decision-making 2 to 5 times in a typical month.
• 33% reported using research in clinical decision
making only 0 to 1 times in a typical month.
• Predictors of research use: academic preparation in
EBP, EBP self-efficacy, perception of usefulness of
research findings and participation in research.
Moderate
Salbach 2009 [38] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner,
organisational and
research
characteristics
associated with
searching or reading
literature among
physical therapists
involved in stroke
management.
• 68% of the participants spent 0% of their work time
on research activities.
• Predictors of searching literature 2 or more times a
month: participation in research, EBP self-efficacy,
being Male, perceived support of research use and
internet access to databases at work.
• Predictors of reading literature 2 or more times a
month: participation in research, EBP self-efficacy,
membership of a professional body, perceived
support, positive perceptions of usefulness of
literature and relevancy of interventions evaluated.
Moderate
Salbach 2009 [34] Multistage sample of
23 Canadian
physiotherapists
(response rate= 72%).
Qualitative data
collected via
telephone interviews
and analysed using
constant comparative
method.
Explore how
physiotherapists use
research evidence to
update the clinical
management of
walking rehabilitation
following stroke.
• Peers were a main source of information owing to
ease of access, resources and cost.
• Systematic reviews were found to be useful.
• Barriers to EBP were insufficient time and
organisational barriers, lack of computer and search
skills, appraisal and application of research findings.
Moderate
Schreiber 2009 [25] Stratified, purposive
sample of 5 (response
rate = 71%)
physiotherapists in the
USA.
Three phase formative
evaluation, action
research project using
mixed methods.
Identify, implement
and evaluate the
effectiveness of
strategies to enhance
EBP and clinical
decision-making.
• Positive attitudes towards EBP pre and post
interventions identified.
• More time identified as being needed to practice
skills and digest workshop material.
• Knowledge of EBP may improve, but may not
translate to behavioural changes.
Quantitative:
Weak
Qualitative:
Moderate
Saleh 2008 [37] Purposive and
snowball sample, 62
Canadian
Physiotherapists
(response rate = 84%)
and 85 Occupational
Therapists (response
rate = 91%) working
in paediatric Cerebral
Palsy rehabilitation.
Cross-sectional
survey, using
vignettes, collected
via telephone
interview.
Explore the actual
practices of Physical
and Occupational
therapists working
with children with
Cerebral Palsy.
• 47% of Physical therapists had conducted research
in their work setting.
• Key factors in EBP implementation: Time,
child/parent compliance, resources, tools, and
frequent educational sessions on the use of research
findings in clinical settings.
• Some controversial interventions were still being
used.
Moderate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Author's personal copy
214 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
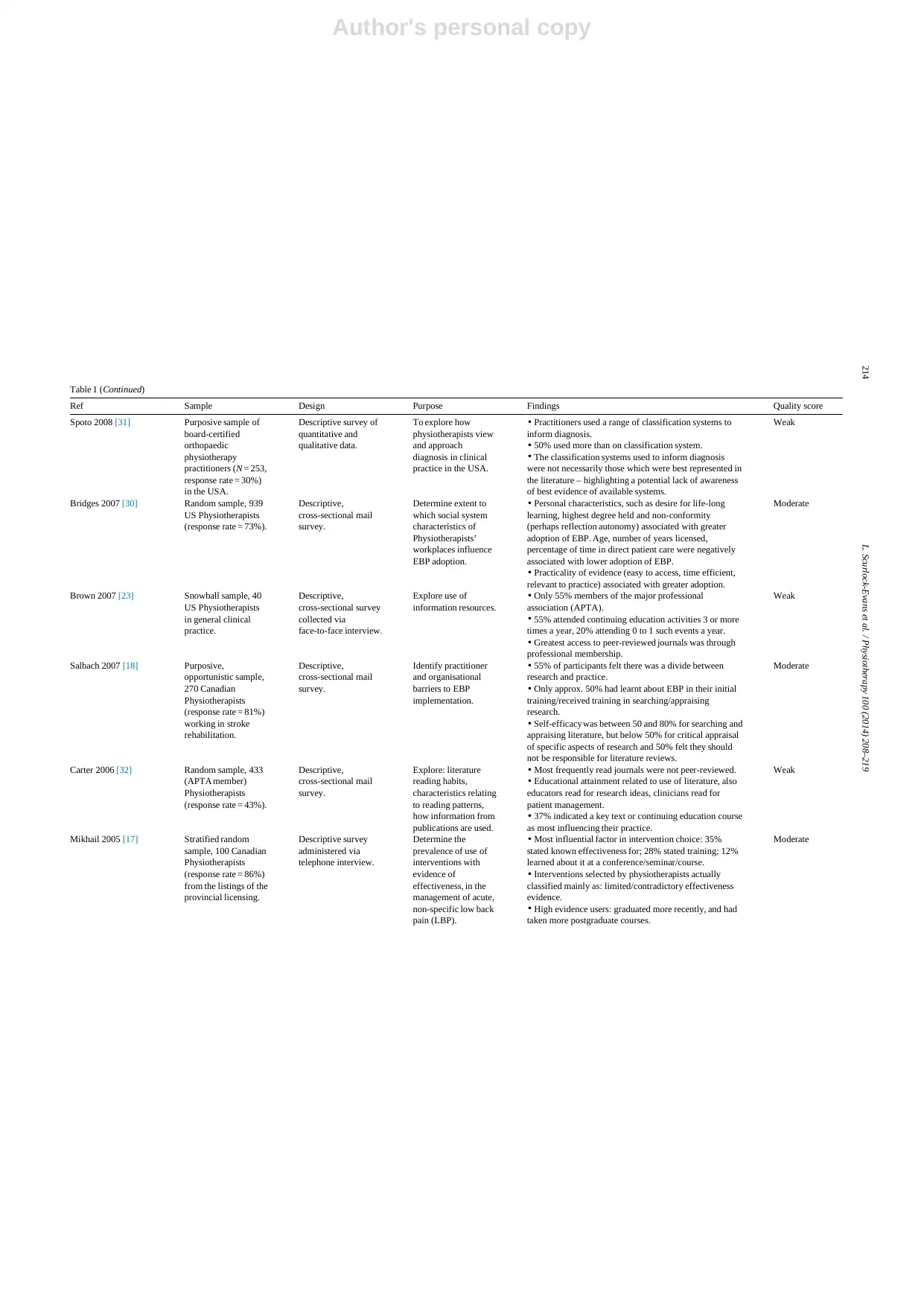
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Spoto 2008 [31] Purposive sample of
board-certified
orthopaedic
physiotherapy
practitioners (N = 253,
response rate = 30%)
in the USA.
Descriptive survey of
quantitative and
qualitative data.
To explore how
physiotherapists view
and approach
diagnosis in clinical
practice in the USA.
• Practitioners used a range of classification systems to
inform diagnosis.
• 50% used more than on classification system.
• The classification systems used to inform diagnosis
were not necessarily those which were best represented in
the literature – highlighting a potential lack of awareness
of best evidence of available systems.
Weak
Bridges 2007 [30] Random sample, 939
US Physiotherapists
(response rate = 73%).
Descriptive,
cross-sectional mail
survey.
Determine extent to
which social system
characteristics of
Physiotherapists’
workplaces influence
EBP adoption.
• Personal characteristics, such as desire for life-long
learning, highest degree held and non-conformity
(perhaps reflection autonomy) associated with greater
adoption of EBP. Age, number of years licensed,
percentage of time in direct patient care were negatively
associated with lower adoption of EBP.
• Practicality of evidence (easy to access, time efficient,
relevant to practice) associated with greater adoption.
Moderate
Brown 2007 [23] Snowball sample, 40
US Physiotherapists
in general clinical
practice.
Descriptive,
cross-sectional survey
collected via
face-to-face interview.
Explore use of
information resources.
• Only 55% members of the major professional
association (APTA).
• 55% attended continuing education activities 3 or more
times a year, 20% attending 0 to 1 such events a year.
• Greatest access to peer-reviewed journals was through
professional membership.
Weak
Salbach 2007 [18] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner
and organisational
barriers to EBP
implementation.
• 55% of participants felt there was a divide between
research and practice.
• Only approx. 50% had learnt about EBP in their initial
training/received training in searching/appraising
research.
• Self-efficacy was between 50 and 80% for searching and
appraising literature, but below 50% for critical appraisal
of specific aspects of research and 50% felt they should
not be responsible for literature reviews.
Moderate
Carter 2006 [32] Random sample, 433
(APTA member)
Physiotherapists
(response rate = 43%).
Descriptive,
cross-sectional mail
survey.
Explore: literature
reading habits,
characteristics relating
to reading patterns,
how information from
publications are used.
• Most frequently read journals were not peer-reviewed.
• Educational attainment related to use of literature, also
educators read for research ideas, clinicians read for
patient management.
• 37% indicated a key text or continuing education course
as most influencing their practice.
Weak
Mikhail 2005 [17] Stratified random
sample, 100 Canadian
Physiotherapists
(response rate = 86%)
from the listings of the
provincial licensing.
Descriptive survey
administered via
telephone interview.
Determine the
prevalence of use of
interventions with
evidence of
effectiveness, in the
management of acute,
non-specific low back
pain (LBP).
• Most influential factor in intervention choice: 35%
stated known effectiveness for; 28% stated training; 12%
learned about it at a conference/seminar/course.
• Interventions selected by physiotherapists actually
classified mainly as: limited/contradictory effectiveness
evidence.
• High evidence users: graduated more recently, and had
taken more postgraduate courses.
Moderate
214 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Spoto 2008 [31] Purposive sample of
board-certified
orthopaedic
physiotherapy
practitioners (N = 253,
response rate = 30%)
in the USA.
Descriptive survey of
quantitative and
qualitative data.
To explore how
physiotherapists view
and approach
diagnosis in clinical
practice in the USA.
• Practitioners used a range of classification systems to
inform diagnosis.
• 50% used more than on classification system.
• The classification systems used to inform diagnosis
were not necessarily those which were best represented in
the literature – highlighting a potential lack of awareness
of best evidence of available systems.
Weak
Bridges 2007 [30] Random sample, 939
US Physiotherapists
(response rate = 73%).
Descriptive,
cross-sectional mail
survey.
Determine extent to
which social system
characteristics of
Physiotherapists’
workplaces influence
EBP adoption.
• Personal characteristics, such as desire for life-long
learning, highest degree held and non-conformity
(perhaps reflection autonomy) associated with greater
adoption of EBP. Age, number of years licensed,
percentage of time in direct patient care were negatively
associated with lower adoption of EBP.
• Practicality of evidence (easy to access, time efficient,
relevant to practice) associated with greater adoption.
Moderate
Brown 2007 [23] Snowball sample, 40
US Physiotherapists
in general clinical
practice.
Descriptive,
cross-sectional survey
collected via
face-to-face interview.
Explore use of
information resources.
• Only 55% members of the major professional
association (APTA).
• 55% attended continuing education activities 3 or more
times a year, 20% attending 0 to 1 such events a year.
• Greatest access to peer-reviewed journals was through
professional membership.
Weak
Salbach 2007 [18] Purposive,
opportunistic sample,
270 Canadian
Physiotherapists
(response rate = 81%)
working in stroke
rehabilitation.
Descriptive,
cross-sectional mail
survey.
Identify practitioner
and organisational
barriers to EBP
implementation.
• 55% of participants felt there was a divide between
research and practice.
• Only approx. 50% had learnt about EBP in their initial
training/received training in searching/appraising
research.
• Self-efficacy was between 50 and 80% for searching and
appraising literature, but below 50% for critical appraisal
of specific aspects of research and 50% felt they should
not be responsible for literature reviews.
Moderate
Carter 2006 [32] Random sample, 433
(APTA member)
Physiotherapists
(response rate = 43%).
Descriptive,
cross-sectional mail
survey.
Explore: literature
reading habits,
characteristics relating
to reading patterns,
how information from
publications are used.
• Most frequently read journals were not peer-reviewed.
• Educational attainment related to use of literature, also
educators read for research ideas, clinicians read for
patient management.
• 37% indicated a key text or continuing education course
as most influencing their practice.
Weak
Mikhail 2005 [17] Stratified random
sample, 100 Canadian
Physiotherapists
(response rate = 86%)
from the listings of the
provincial licensing.
Descriptive survey
administered via
telephone interview.
Determine the
prevalence of use of
interventions with
evidence of
effectiveness, in the
management of acute,
non-specific low back
pain (LBP).
• Most influential factor in intervention choice: 35%
stated known effectiveness for; 28% stated training; 12%
learned about it at a conference/seminar/course.
• Interventions selected by physiotherapists actually
classified mainly as: limited/contradictory effectiveness
evidence.
• High evidence users: graduated more recently, and had
taken more postgraduate courses.
Moderate
Author's personal copy
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 215
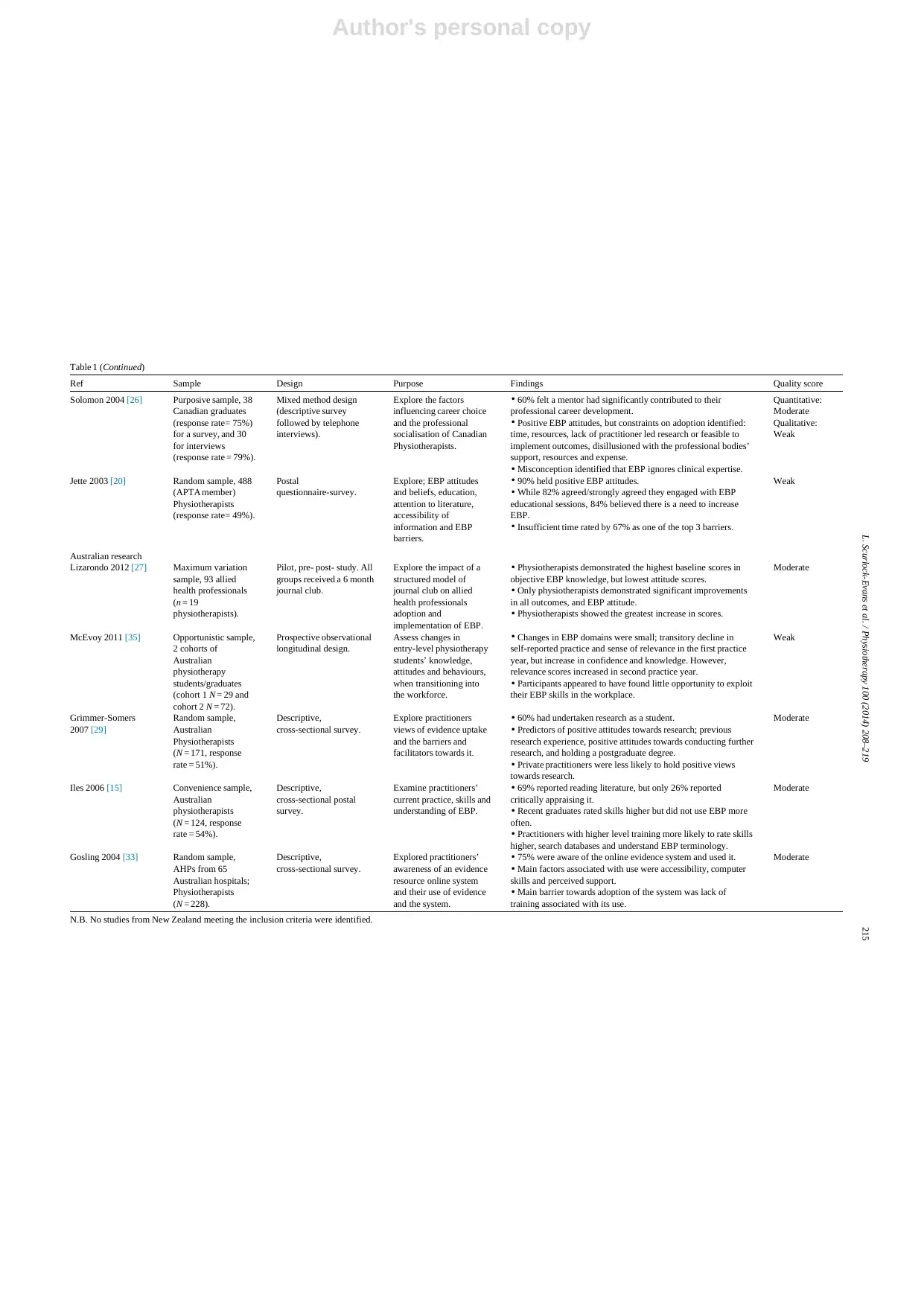
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Solomon 2004 [26] Purposive sample, 38
Canadian graduates
(response rate= 75%)
for a survey, and 30
for interviews
(response rate = 79%).
Mixed method design
(descriptive survey
followed by telephone
interviews).
Explore the factors
influencing career choice
and the professional
socialisation of Canadian
Physiotherapists.
• 60% felt a mentor had significantly contributed to their
professional career development.
• Positive EBP attitudes, but constraints on adoption identified:
time, resources, lack of practitioner led research or feasible to
implement outcomes, disillusioned with the professional bodies’
support, resources and expense.
• Misconception identified that EBP ignores clinical expertise.
Quantitative:
Moderate
Qualitative:
Weak
Jette 2003 [20] Random sample, 488
(APTA member)
Physiotherapists
(response rate= 49%).
Postal
questionnaire-survey.
Explore; EBP attitudes
and beliefs, education,
attention to literature,
accessibility of
information and EBP
barriers.
• 90% held positive EBP attitudes.
• While 82% agreed/strongly agreed they engaged with EBP
educational sessions, 84% believed there is a need to increase
EBP.
• Insufficient time rated by 67% as one of the top 3 barriers.
Weak
Australian research
Lizarondo 2012 [27] Maximum variation
sample, 93 allied
health professionals
(n = 19
physiotherapists).
Pilot, pre- post- study. All
groups received a 6 month
journal club.
Explore the impact of a
structured model of
journal club on allied
health professionals
adoption and
implementation of EBP.
• Physiotherapists demonstrated the highest baseline scores in
objective EBP knowledge, but lowest attitude scores.
• Only physiotherapists demonstrated significant improvements
in all outcomes, and EBP attitude.
• Physiotherapists showed the greatest increase in scores.
Moderate
McEvoy 2011 [35] Opportunistic sample,
2 cohorts of
Australian
physiotherapy
students/graduates
(cohort 1 N = 29 and
cohort 2 N = 72).
Prospective observational
longitudinal design.
Assess changes in
entry-level physiotherapy
students’ knowledge,
attitudes and behaviours,
when transitioning into
the workforce.
• Changes in EBP domains were small; transitory decline in
self-reported practice and sense of relevance in the first practice
year, but increase in confidence and knowledge. However,
relevance scores increased in second practice year.
• Participants appeared to have found little opportunity to exploit
their EBP skills in the workplace.
Weak
Grimmer-Somers
2007 [29]
Random sample,
Australian
Physiotherapists
(N = 171, response
rate = 51%).
Descriptive,
cross-sectional survey.
Explore practitioners
views of evidence uptake
and the barriers and
facilitators towards it.
• 60% had undertaken research as a student.
• Predictors of positive attitudes towards research; previous
research experience, positive attitudes towards conducting further
research, and holding a postgraduate degree.
• Private practitioners were less likely to hold positive views
towards research.
Moderate
Iles 2006 [15] Convenience sample,
Australian
physiotherapists
(N = 124, response
rate = 54%).
Descriptive,
cross-sectional postal
survey.
Examine practitioners’
current practice, skills and
understanding of EBP.
• 69% reported reading literature, but only 26% reported
critically appraising it.
• Recent graduates rated skills higher but did not use EBP more
often.
• Practitioners with higher level training more likely to rate skills
higher, search databases and understand EBP terminology.
Moderate
Gosling 2004 [33] Random sample,
AHPs from 65
Australian hospitals;
Physiotherapists
(N = 228).
Descriptive,
cross-sectional survey.
Explored practitioners’
awareness of an evidence
resource online system
and their use of evidence
and the system.
• 75% were aware of the online evidence system and used it.
• Main factors associated with use were accessibility, computer
skills and perceived support.
• Main barrier towards adoption of the system was lack of
training associated with its use.
Moderate
N.B. No studies from New Zealand meeting the inclusion criteria were identified.
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 215
Table 1 (Continued)
Ref Sample Design Purpose Findings Quality score
Solomon 2004 [26] Purposive sample, 38
Canadian graduates
(response rate= 75%)
for a survey, and 30
for interviews
(response rate = 79%).
Mixed method design
(descriptive survey
followed by telephone
interviews).
Explore the factors
influencing career choice
and the professional
socialisation of Canadian
Physiotherapists.
• 60% felt a mentor had significantly contributed to their
professional career development.
• Positive EBP attitudes, but constraints on adoption identified:
time, resources, lack of practitioner led research or feasible to
implement outcomes, disillusioned with the professional bodies’
support, resources and expense.
• Misconception identified that EBP ignores clinical expertise.
Quantitative:
Moderate
Qualitative:
Weak
Jette 2003 [20] Random sample, 488
(APTA member)
Physiotherapists
(response rate= 49%).
Postal
questionnaire-survey.
Explore; EBP attitudes
and beliefs, education,
attention to literature,
accessibility of
information and EBP
barriers.
• 90% held positive EBP attitudes.
• While 82% agreed/strongly agreed they engaged with EBP
educational sessions, 84% believed there is a need to increase
EBP.
• Insufficient time rated by 67% as one of the top 3 barriers.
Weak
Australian research
Lizarondo 2012 [27] Maximum variation
sample, 93 allied
health professionals
(n = 19
physiotherapists).
Pilot, pre- post- study. All
groups received a 6 month
journal club.
Explore the impact of a
structured model of
journal club on allied
health professionals
adoption and
implementation of EBP.
• Physiotherapists demonstrated the highest baseline scores in
objective EBP knowledge, but lowest attitude scores.
• Only physiotherapists demonstrated significant improvements
in all outcomes, and EBP attitude.
• Physiotherapists showed the greatest increase in scores.
Moderate
McEvoy 2011 [35] Opportunistic sample,
2 cohorts of
Australian
physiotherapy
students/graduates
(cohort 1 N = 29 and
cohort 2 N = 72).
Prospective observational
longitudinal design.
Assess changes in
entry-level physiotherapy
students’ knowledge,
attitudes and behaviours,
when transitioning into
the workforce.
• Changes in EBP domains were small; transitory decline in
self-reported practice and sense of relevance in the first practice
year, but increase in confidence and knowledge. However,
relevance scores increased in second practice year.
• Participants appeared to have found little opportunity to exploit
their EBP skills in the workplace.
Weak
Grimmer-Somers
2007 [29]
Random sample,
Australian
Physiotherapists
(N = 171, response
rate = 51%).
Descriptive,
cross-sectional survey.
Explore practitioners
views of evidence uptake
and the barriers and
facilitators towards it.
• 60% had undertaken research as a student.
• Predictors of positive attitudes towards research; previous
research experience, positive attitudes towards conducting further
research, and holding a postgraduate degree.
• Private practitioners were less likely to hold positive views
towards research.
Moderate
Iles 2006 [15] Convenience sample,
Australian
physiotherapists
(N = 124, response
rate = 54%).
Descriptive,
cross-sectional postal
survey.
Examine practitioners’
current practice, skills and
understanding of EBP.
• 69% reported reading literature, but only 26% reported
critically appraising it.
• Recent graduates rated skills higher but did not use EBP more
often.
• Practitioners with higher level training more likely to rate skills
higher, search databases and understand EBP terminology.
Moderate
Gosling 2004 [33] Random sample,
AHPs from 65
Australian hospitals;
Physiotherapists
(N = 228).
Descriptive,
cross-sectional survey.
Explored practitioners’
awareness of an evidence
resource online system
and their use of evidence
and the system.
• 75% were aware of the online evidence system and used it.
• Main factors associated with use were accessibility, computer
skills and perceived support.
• Main barrier towards adoption of the system was lack of
training associated with its use.
Moderate
N.B. No studies from New Zealand meeting the inclusion criteria were identified.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Author's personal copy
216 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Research suggests physiotherapists’ EBP is infrequent and
varying in quality [6]. One study [14] reported that 53% of
respondents used research in clinical decision-making only
2 to 5 times in a typical month and 33% used research only
once a month or less. Another study discovered that although
69% stated they read relevant research, only 26% critically
appraised it [15]. Furthermore, high self-ratings of EBP skills
does not necessarily translate to greater or more accurate
implementation [15]. For example, Nilsagård and Lohse [16]
found that although practitioners rated their knowledge of
EBP highly, only 12 to 36% correctly defined the EBP com-
ponents [16]. Similarly, when asked about the most influential
factors in intervention choice, 35% of a sample of Amer-
ican physiotherapists stated “known effectiveness”, despite
the interventions actually chosen having limited or contradic-
tory evidence [17]. This suggests a disparity between research
awareness, critical appraisal skills and practice. However, it
is not clear what physiotherapists in this study took “known
effectiveness” to mean.
Lastly, although physiotherapists may believe EBP is
important, they may not feel it is their responsibility to under-
take all its steps [18].
Attitudes towards EBP
The majority of studies identified positive attitudes
towards EBP and research use in practice [5,11,17–27], with
many physiotherapists viewing EBP as a necessary part of
their role which helped inform clinical decision-making.
However, misconceptions of EBP were also identified. Some
research [28] revealed less positive attitudes towards EBP
arising from concerns that it would decrease therapeutic
autonomy, resulting in a lack of motivation to implement it.
Therapists felt the drive towards EBP was economic, rather
than quality of care.
Importantly, this review highlights a disparity between
attitudes and behaviour, with some practitioners with posi-
tive attitudes failing to consistently implement EBP [15,16]
and others with less positive attitudes implementing it more
frequently [11]. This raises questions about the link between
attitudes and behaviour; particularly for EBP self-efficacy
studies, which have identified attitudes as an important, mod-
ifiable factor in EBP adoption and implementation [14].
Knowledge, skills & educational preparation
A study comparing AHP’s self-reported EBP knowledge
revealed physiotherapists’ ratings as similar to occupational
therapists, dieticians, speech and language therapists and psy-
chologists, but greater than podiatrists, radiotherapists and
orthoptists; with the vast majority (80%) of physiotherapists
rating their knowledge as mid to high [12]. In another study
[20], physiotherapists rated their self-efficacy in research and
appraising literature as mid to high (50 to 80%), but criti-
cal appraisal of psychometrics and statistics as low (<50%).
Clinicians also reported difficulty in interpreting odds ratios
[11], and research written in English when it was not their
first language [21]. Physiotherapists may also be confused
regarding what the term “evidence” actually refers to [19],
and therefore what type of evidence they should implement
in practice.
Level of academic preparation was found to have a
positive relationship with knowledge of EBP [17], more pos-
itive attitudes and fewer perceived barriers towards research
utilisation [16,29], greater use of interventions with high
research-evidence support [17], greater levels of research use
in practice [14] and greater adoption of EBP [30]. Holding
higher educational qualifications may reflect a desire for life-
long learning, identified as a key predictor of EBP adoption
[2], which may account for these findings.
Research indicates that an individual’s personal and work-
place libraries may be dominated by those texts acquired
during entry-level education [23]. Furthermore, formal edu-
cational courses may influence choice of classification tools
in practice: Spoto and Collins [31] suggested that frequent
self-reported use of unsupported interventions may be due
to them featuring prominently in graduate and postgraduate
training. These findings indicate that continuing educational
engagement may be a means of ensuring core “go-to” infor-
mation remains up-to-date. Interestingly, Solomon et al. [26]
found that although physiotherapists wanted to continue with
their education and develop clinical specialisation, they did
not wish to do so formally. This suggests physiotherapists
may not view formal academic education as a useful means
of continuing professional development (CPD), which may
relate to the perception of “academic” peer-reviewed infor-
mation sources as being of limited practical value (e.g. [34]).
Information technology (IT) was consistently identified
as important in education and EBP implementation. Gosling
and Westbrook [33] found that one of the main factors
associated with awareness and use of an online evidence
resource was confidence in computer skills. In a study with
UK AHPs a gap was apparent between confidence in under-
standing the 5-step process of EBP and the skills required to
implement this knowledge [6]. In part this may be due to lack
of confidence with IT, as many may have graduated prior to
the widespread introduction of IT in the healthcare setting
[5]. Indeed, the Internet has been identified as the least used
source of information in decision-making [11], and lack of
computer skills as a predictor of lower EBP adoption [14,34].
The period of transition between completion of entry-level
education and entering the workforce also presents issues
for EBP implementation: there may be a mismatch between
the ideals learnt during a course and opportunities for newly
qualified practitioners to implement their skills [13,35]. Also,
being unable to challenge senior colleagues’ views and prac-
tices was a barrier to EBP for junior physiotherapists [19].
Barriers & enablers
Time/workload pressures were the most common bar-
rier to EBP implementation [5,11,12,16,18–21,24–26,30,34,
216 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
Research suggests physiotherapists’ EBP is infrequent and
varying in quality [6]. One study [14] reported that 53% of
respondents used research in clinical decision-making only
2 to 5 times in a typical month and 33% used research only
once a month or less. Another study discovered that although
69% stated they read relevant research, only 26% critically
appraised it [15]. Furthermore, high self-ratings of EBP skills
does not necessarily translate to greater or more accurate
implementation [15]. For example, Nilsagård and Lohse [16]
found that although practitioners rated their knowledge of
EBP highly, only 12 to 36% correctly defined the EBP com-
ponents [16]. Similarly, when asked about the most influential
factors in intervention choice, 35% of a sample of Amer-
ican physiotherapists stated “known effectiveness”, despite
the interventions actually chosen having limited or contradic-
tory evidence [17]. This suggests a disparity between research
awareness, critical appraisal skills and practice. However, it
is not clear what physiotherapists in this study took “known
effectiveness” to mean.
Lastly, although physiotherapists may believe EBP is
important, they may not feel it is their responsibility to under-
take all its steps [18].
Attitudes towards EBP
The majority of studies identified positive attitudes
towards EBP and research use in practice [5,11,17–27], with
many physiotherapists viewing EBP as a necessary part of
their role which helped inform clinical decision-making.
However, misconceptions of EBP were also identified. Some
research [28] revealed less positive attitudes towards EBP
arising from concerns that it would decrease therapeutic
autonomy, resulting in a lack of motivation to implement it.
Therapists felt the drive towards EBP was economic, rather
than quality of care.
Importantly, this review highlights a disparity between
attitudes and behaviour, with some practitioners with posi-
tive attitudes failing to consistently implement EBP [15,16]
and others with less positive attitudes implementing it more
frequently [11]. This raises questions about the link between
attitudes and behaviour; particularly for EBP self-efficacy
studies, which have identified attitudes as an important, mod-
ifiable factor in EBP adoption and implementation [14].
Knowledge, skills & educational preparation
A study comparing AHP’s self-reported EBP knowledge
revealed physiotherapists’ ratings as similar to occupational
therapists, dieticians, speech and language therapists and psy-
chologists, but greater than podiatrists, radiotherapists and
orthoptists; with the vast majority (80%) of physiotherapists
rating their knowledge as mid to high [12]. In another study
[20], physiotherapists rated their self-efficacy in research and
appraising literature as mid to high (50 to 80%), but criti-
cal appraisal of psychometrics and statistics as low (<50%).
Clinicians also reported difficulty in interpreting odds ratios
[11], and research written in English when it was not their
first language [21]. Physiotherapists may also be confused
regarding what the term “evidence” actually refers to [19],
and therefore what type of evidence they should implement
in practice.
Level of academic preparation was found to have a
positive relationship with knowledge of EBP [17], more pos-
itive attitudes and fewer perceived barriers towards research
utilisation [16,29], greater use of interventions with high
research-evidence support [17], greater levels of research use
in practice [14] and greater adoption of EBP [30]. Holding
higher educational qualifications may reflect a desire for life-
long learning, identified as a key predictor of EBP adoption
[2], which may account for these findings.
Research indicates that an individual’s personal and work-
place libraries may be dominated by those texts acquired
during entry-level education [23]. Furthermore, formal edu-
cational courses may influence choice of classification tools
in practice: Spoto and Collins [31] suggested that frequent
self-reported use of unsupported interventions may be due
to them featuring prominently in graduate and postgraduate
training. These findings indicate that continuing educational
engagement may be a means of ensuring core “go-to” infor-
mation remains up-to-date. Interestingly, Solomon et al. [26]
found that although physiotherapists wanted to continue with
their education and develop clinical specialisation, they did
not wish to do so formally. This suggests physiotherapists
may not view formal academic education as a useful means
of continuing professional development (CPD), which may
relate to the perception of “academic” peer-reviewed infor-
mation sources as being of limited practical value (e.g. [34]).
Information technology (IT) was consistently identified
as important in education and EBP implementation. Gosling
and Westbrook [33] found that one of the main factors
associated with awareness and use of an online evidence
resource was confidence in computer skills. In a study with
UK AHPs a gap was apparent between confidence in under-
standing the 5-step process of EBP and the skills required to
implement this knowledge [6]. In part this may be due to lack
of confidence with IT, as many may have graduated prior to
the widespread introduction of IT in the healthcare setting
[5]. Indeed, the Internet has been identified as the least used
source of information in decision-making [11], and lack of
computer skills as a predictor of lower EBP adoption [14,34].
The period of transition between completion of entry-level
education and entering the workforce also presents issues
for EBP implementation: there may be a mismatch between
the ideals learnt during a course and opportunities for newly
qualified practitioners to implement their skills [13,35]. Also,
being unable to challenge senior colleagues’ views and prac-
tices was a barrier to EBP for junior physiotherapists [19].
Barriers & enablers
Time/workload pressures were the most common bar-
rier to EBP implementation [5,11,12,16,18–21,24–26,30,34,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Author's personal copy
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 217
36,37]. However, as the demands on healthcare profession-
als seem unlikely to be alleviated in the future, this review
focuses on the other consistent but modifiable barriers iden-
tified in the research, as potential areas for intervention. If
such modifiable barriers are addressed, this may have a posi-
tive effect on time/workload pressures, as well as enhancing
the provision of appropriate and effective care.
Ambivalence
Only 55% of a sample of American physiotherapists
[23] were found to be members of the major professional
association, a theme replicated in other samples [24,27].
As professional bodies provide a key access-route to peer-
reviewed journals [30,36], and membership of a professional
body predicts reading literature twice a month or more
[38], this is concerning. Some research [26,28] revealed
that although many felt membership was important and pro-
vided their profession with a voice, a significant minority felt
disillusioned with the provision (particularly regarding pro-
hibitive costs), leading to ambivalence towards membership.
Perceptions of research
As well as the practical aspects of research utilisation
such as library and computer access, and having the skills
to use resources effectively [18,19,24,34,36], perceptual bar-
riers were also identified. Some practitioners viewed the
evidence-base as limited, difficult to translate into real-world
applications [19,28] and inaccessible [21], resulting in EBP
failing to take the limitations of the clinical practice setting
into account [11]. This may explain why some physiothera-
pists felt suspicious of research and did not value it [19].
Differences in perceptions of the role of research, levels of
engagement and views on methods of promoting EBP were
apparent between physiotherapists working in community
and academic hospitals [19].
Sources of evidence
A significant proportion of studies reported physiother-
apists’ primary sources of decision-making information as
the client, personal experience [10], courses and in-service
training [39]. Practitioners reported difficulty in reading
journal articles, and rated literature and research as low
priorities for implementing best clinical practice [22]. Non-
peer-reviewed literature was frequently read by practitioners
[32] and for many, peers were a core source of informa-
tion, owing to financial constraints and ease of access [14].
This may also arise from some clinicians’ concern about the
lack of practitioner-led research and feasible-to-implement
outcomes [26].
Previous research experience and positive attitudes
towards conducting research in the future [29] were identified
as predictors of positive attitudes towards research implemen-
tation. Unfortunately one common theme in the literature
was a lack of opportunity for physiotherapists to conduct
research [17,37,38]. Providing greater opportunity for phy-
siotherapists to engage in research may help increase positive
attitudes towards EBP, develop physiotherapists’ EBP skills,
and contribute to a practical, applied research base which
may provide physiotherapists with more accessible evidence
to guide them in their roles.
One worrying observation was the misconception that
EBP ignores clinical expertise, leading some physiotherapists
to feel they had to apologise for using it in their practice [26]
and suggesting there was a fundamental misunderstanding of
the premise of EBP. Other physiotherapists were concerned
about where the ‘patient’ fits into the process [19]. These con-
cerns could be addressed through in-house education [13],
which physiotherapists appeared to desire [37].
Interventions
A small number of articles explored the impact of
EBP enhancing interventions (n = 6), including: a psy-
chosocial management intervention using opinion leaders
[22,39]; a multi-faceted intervention using Knowledge Bro-
kers (individuals who facilitate collaborative working and
understanding between researchers and decision-makers
[40]); a formative evaluation project including an EBP work-
shop [25]; a Journal club [27] and a presentation-based
initiative to highlight local examples of EBP [24].
The interventions’ effectiveness received mixed results.
For example, little change on perceptions and practice were
identified following the psychosocial management [39] and
although positive attitudes towards EBP were identified
before and after the formative evaluation project, imple-
mentation of the taught strategies was variable [25]. The
Knowledge Broker [40], journal club [27] and the local
EBP presentation-based interventions [24] demonstrated
greater effectiveness, such as: greater familiarity of evidence-
supported tools, improvements in EBP practice and attitudes
and intentions to revise practice.
Limitations
Only studies published in the English language, in peer-
reviewed journals were included, potentially introducing
publication bias. Owing to the inclusion of both quantitative
and qualitative findings, textual (rather than statistical) syn-
thesis was performed. Although this approach may be subject
to greater confirmation bias (i.e. selection/interpretation
of information which confirms pre-existing beliefs), the
adoption of a systematic review methodology (i.e. system-
atic search strategy, quality appraisal, and data extraction
procedures), and independent raters help mitigate this
issue.
Reviewed studies’ limitations
Studies’ quality-ratings ranged from weak to strong, with
the modal award being moderate, therefore this synthesis of
research findings should be interpreted with a degree of cau-
tion. A number of methodological issues can be identified.
Many studies relied on subjective, self-report measures; the
L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219 217
36,37]. However, as the demands on healthcare profession-
als seem unlikely to be alleviated in the future, this review
focuses on the other consistent but modifiable barriers iden-
tified in the research, as potential areas for intervention. If
such modifiable barriers are addressed, this may have a posi-
tive effect on time/workload pressures, as well as enhancing
the provision of appropriate and effective care.
Ambivalence
Only 55% of a sample of American physiotherapists
[23] were found to be members of the major professional
association, a theme replicated in other samples [24,27].
As professional bodies provide a key access-route to peer-
reviewed journals [30,36], and membership of a professional
body predicts reading literature twice a month or more
[38], this is concerning. Some research [26,28] revealed
that although many felt membership was important and pro-
vided their profession with a voice, a significant minority felt
disillusioned with the provision (particularly regarding pro-
hibitive costs), leading to ambivalence towards membership.
Perceptions of research
As well as the practical aspects of research utilisation
such as library and computer access, and having the skills
to use resources effectively [18,19,24,34,36], perceptual bar-
riers were also identified. Some practitioners viewed the
evidence-base as limited, difficult to translate into real-world
applications [19,28] and inaccessible [21], resulting in EBP
failing to take the limitations of the clinical practice setting
into account [11]. This may explain why some physiothera-
pists felt suspicious of research and did not value it [19].
Differences in perceptions of the role of research, levels of
engagement and views on methods of promoting EBP were
apparent between physiotherapists working in community
and academic hospitals [19].
Sources of evidence
A significant proportion of studies reported physiother-
apists’ primary sources of decision-making information as
the client, personal experience [10], courses and in-service
training [39]. Practitioners reported difficulty in reading
journal articles, and rated literature and research as low
priorities for implementing best clinical practice [22]. Non-
peer-reviewed literature was frequently read by practitioners
[32] and for many, peers were a core source of informa-
tion, owing to financial constraints and ease of access [14].
This may also arise from some clinicians’ concern about the
lack of practitioner-led research and feasible-to-implement
outcomes [26].
Previous research experience and positive attitudes
towards conducting research in the future [29] were identified
as predictors of positive attitudes towards research implemen-
tation. Unfortunately one common theme in the literature
was a lack of opportunity for physiotherapists to conduct
research [17,37,38]. Providing greater opportunity for phy-
siotherapists to engage in research may help increase positive
attitudes towards EBP, develop physiotherapists’ EBP skills,
and contribute to a practical, applied research base which
may provide physiotherapists with more accessible evidence
to guide them in their roles.
One worrying observation was the misconception that
EBP ignores clinical expertise, leading some physiotherapists
to feel they had to apologise for using it in their practice [26]
and suggesting there was a fundamental misunderstanding of
the premise of EBP. Other physiotherapists were concerned
about where the ‘patient’ fits into the process [19]. These con-
cerns could be addressed through in-house education [13],
which physiotherapists appeared to desire [37].
Interventions
A small number of articles explored the impact of
EBP enhancing interventions (n = 6), including: a psy-
chosocial management intervention using opinion leaders
[22,39]; a multi-faceted intervention using Knowledge Bro-
kers (individuals who facilitate collaborative working and
understanding between researchers and decision-makers
[40]); a formative evaluation project including an EBP work-
shop [25]; a Journal club [27] and a presentation-based
initiative to highlight local examples of EBP [24].
The interventions’ effectiveness received mixed results.
For example, little change on perceptions and practice were
identified following the psychosocial management [39] and
although positive attitudes towards EBP were identified
before and after the formative evaluation project, imple-
mentation of the taught strategies was variable [25]. The
Knowledge Broker [40], journal club [27] and the local
EBP presentation-based interventions [24] demonstrated
greater effectiveness, such as: greater familiarity of evidence-
supported tools, improvements in EBP practice and attitudes
and intentions to revise practice.
Limitations
Only studies published in the English language, in peer-
reviewed journals were included, potentially introducing
publication bias. Owing to the inclusion of both quantitative
and qualitative findings, textual (rather than statistical) syn-
thesis was performed. Although this approach may be subject
to greater confirmation bias (i.e. selection/interpretation
of information which confirms pre-existing beliefs), the
adoption of a systematic review methodology (i.e. system-
atic search strategy, quality appraisal, and data extraction
procedures), and independent raters help mitigate this
issue.
Reviewed studies’ limitations
Studies’ quality-ratings ranged from weak to strong, with
the modal award being moderate, therefore this synthesis of
research findings should be interpreted with a degree of cau-
tion. A number of methodological issues can be identified.
Many studies relied on subjective, self-report measures; the

Author's personal copy
218 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
issues around the reliability and validity of self-report meas-
ures are well documented [41]. Furthermore there appears
to be a lack of consistent definitions of EBP or optimal
research use. For example, a common implication is that
greater amounts of time spent searching for literature indi-
cates greater engagement with research. However, this could
equally represent a lack of skills (i.e. inefficiency in iden-
tifying and acquiring salient information). Therefore, there
is a need to identify robust measures of the quality of EBP
implementation, not merely frequency and duration.
Many studies reported low response rates: although this
is common with survey research (and some studies exam-
ined non-response characteristics), it is reasonable to assume
that individuals with more positive attitudes towards research
were more likely to participate, thereby biasing results.
Furthermore, samples tended to be female and “urban” dom-
inated and recruited from professional bodies’ registration
lists, suggesting further research exploring the experiences
of other groups of physiotherapists would be useful.
Although some authors recognised that social desirabil-
ity effects may have impacted on their findings [14,17,37,38]
little attempt was made to control for this. Future research
should seek to include a measure of socially desirable
responding, as this may help to explain the disparity between
self-reported attitudes, skill, and actual performance.
Conclusion and implications of key findings
A large proportion of physiotherapists’ hold positive atti-
tudes towards the principles of EBP. However, these attitudes
do not necessarily translate into consistent, high-quality EBP.
Although there are resources available to enable physiother-
apists to implement EBP, they appear to struggle to do so on
a daily basis. Concerns regarding EBP are apparent at two
levels: EBP as a principle (i.e. using the best evidence in
practice), and EBP as a process (i.e. actually implementing
all the steps involved in EBP). Indeed, many barriers to EBP
implementation have become apparent, such as: lack of time
and skills, misperceptions of EBP and what constitutes “evi-
dence”. Furthermore, a significant challenge encountered by
physiotherapists is the lack of high quality (i.e. valid and reli-
able) research evidence available to them. This issue may be
compounded by confusion regarding what actually consti-
tutes “best” (i.e. valid, reliable and relevant) research.
Interventions focusing on modifiable factors, such as
increasing the practical/applied value of research, increas-
ing open-access resources and peer-reviewed “coffee table”
publications, may help reduce time and resource demands
for physiotherapists when implementing EBP. Furthermore,
there appears to be a preference for information-seeking
from ‘human’ as opposed to ‘computer’ sources, suggest-
ing interventions using knowledge brokers (such as the one
implemented by Russell et al. [40]) may be particularly
welcomed. Greater organisational commitment to signpost-
ing physiotherapists to key changes in policy, guidelines, or
research evidence may help alleviate the feeling of “shifting
sands”, which many encounter when trying to remain up-to-
date with best research evidence and applying it to their own
practice. Another important issue to recognise is that there
is no “one size fits all” intervention for enhancing EBP. For
example, physiotherapists working in different settings (e.g.
community, hospital, acute) may have different educational
needs and encounter different barriers [36,39]. Therefore,
assessing organisational culture prior to the development of
educational interventions is essential.
In-house CPD activities appear to be a key method of
ensuring knowledge and skills remain current, as well as cap-
italising on the preference for ‘human’ information sources.
Although a few promising interventions have been identi-
fied, further systematic evidence is required to understand
which are the most effective in enabling physiotherapists to
implement EBP.
Acknowledgements
The authors would like to express their thanks to Danielle
Stephens, for her assistance with the preparation of this arti-
cle.
Funding: This review received no grants from any funding
agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: There are no conflicts of interest to
disclose.
Appendix A. Supplementary data
Supplementary data associated with this article can be
found, in the online version, at http://dx.doi.org/10.1016/j.
physio.2014.03.001.
References
[1] Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R. Evidence-
based medicine how to practice and teach EBM. 2nd ed. Edinburgh:
Churchill-Livingstone; 2000.
[2] Bello A. Utilizing research findings in physiotherapy: a call for gap
bridging. Niger Postgrad Med J 2011;18/19:54–8.
[3] Dannapfel P, Peolsson A, Nilsen P. What supports physiothera-
pists’ use of research in clinical practice? A qualitative study
in Sweden. Implement Sci 2013:8. Available at: http://www.
implementationscience.com/content/8/1/31/prepub Accessed January
31, 2012.
[4] Kumar S, Grimmer-Somers K, Hughes B. The ethics of evidence imple-
mentation in health care. Physiother Res Int 2010;15:96–102.
[5] Caldwell K, Coleman K, Copp G, Bell L, Ghazi F. Preparing for profes-
sional practice: how well does professional training equip health and
social care practitioners to engage in evidence-based practice. Nurse
Educ Today 2007;27:518–28.
[6] Chan S, Clough A. A critical evaluation of evidence-based practices of
physiotherapy in musculoskeletal medicine. IMM 2010;32:163–6.
[7] Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group. Pre-
ferred reporting items for systematic reviews and meta-analyses: The
PRISMA Statement. Ann Intern Med 2009:151. Available at: http://
218 L. Scurlock-Evans et al. / Physiotherapy 100 (2014) 208–219
issues around the reliability and validity of self-report meas-
ures are well documented [41]. Furthermore there appears
to be a lack of consistent definitions of EBP or optimal
research use. For example, a common implication is that
greater amounts of time spent searching for literature indi-
cates greater engagement with research. However, this could
equally represent a lack of skills (i.e. inefficiency in iden-
tifying and acquiring salient information). Therefore, there
is a need to identify robust measures of the quality of EBP
implementation, not merely frequency and duration.
Many studies reported low response rates: although this
is common with survey research (and some studies exam-
ined non-response characteristics), it is reasonable to assume
that individuals with more positive attitudes towards research
were more likely to participate, thereby biasing results.
Furthermore, samples tended to be female and “urban” dom-
inated and recruited from professional bodies’ registration
lists, suggesting further research exploring the experiences
of other groups of physiotherapists would be useful.
Although some authors recognised that social desirabil-
ity effects may have impacted on their findings [14,17,37,38]
little attempt was made to control for this. Future research
should seek to include a measure of socially desirable
responding, as this may help to explain the disparity between
self-reported attitudes, skill, and actual performance.
Conclusion and implications of key findings
A large proportion of physiotherapists’ hold positive atti-
tudes towards the principles of EBP. However, these attitudes
do not necessarily translate into consistent, high-quality EBP.
Although there are resources available to enable physiother-
apists to implement EBP, they appear to struggle to do so on
a daily basis. Concerns regarding EBP are apparent at two
levels: EBP as a principle (i.e. using the best evidence in
practice), and EBP as a process (i.e. actually implementing
all the steps involved in EBP). Indeed, many barriers to EBP
implementation have become apparent, such as: lack of time
and skills, misperceptions of EBP and what constitutes “evi-
dence”. Furthermore, a significant challenge encountered by
physiotherapists is the lack of high quality (i.e. valid and reli-
able) research evidence available to them. This issue may be
compounded by confusion regarding what actually consti-
tutes “best” (i.e. valid, reliable and relevant) research.
Interventions focusing on modifiable factors, such as
increasing the practical/applied value of research, increas-
ing open-access resources and peer-reviewed “coffee table”
publications, may help reduce time and resource demands
for physiotherapists when implementing EBP. Furthermore,
there appears to be a preference for information-seeking
from ‘human’ as opposed to ‘computer’ sources, suggest-
ing interventions using knowledge brokers (such as the one
implemented by Russell et al. [40]) may be particularly
welcomed. Greater organisational commitment to signpost-
ing physiotherapists to key changes in policy, guidelines, or
research evidence may help alleviate the feeling of “shifting
sands”, which many encounter when trying to remain up-to-
date with best research evidence and applying it to their own
practice. Another important issue to recognise is that there
is no “one size fits all” intervention for enhancing EBP. For
example, physiotherapists working in different settings (e.g.
community, hospital, acute) may have different educational
needs and encounter different barriers [36,39]. Therefore,
assessing organisational culture prior to the development of
educational interventions is essential.
In-house CPD activities appear to be a key method of
ensuring knowledge and skills remain current, as well as cap-
italising on the preference for ‘human’ information sources.
Although a few promising interventions have been identi-
fied, further systematic evidence is required to understand
which are the most effective in enabling physiotherapists to
implement EBP.
Acknowledgements
The authors would like to express their thanks to Danielle
Stephens, for her assistance with the preparation of this arti-
cle.
Funding: This review received no grants from any funding
agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: There are no conflicts of interest to
disclose.
Appendix A. Supplementary data
Supplementary data associated with this article can be
found, in the online version, at http://dx.doi.org/10.1016/j.
physio.2014.03.001.
References
[1] Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R. Evidence-
based medicine how to practice and teach EBM. 2nd ed. Edinburgh:
Churchill-Livingstone; 2000.
[2] Bello A. Utilizing research findings in physiotherapy: a call for gap
bridging. Niger Postgrad Med J 2011;18/19:54–8.
[3] Dannapfel P, Peolsson A, Nilsen P. What supports physiothera-
pists’ use of research in clinical practice? A qualitative study
in Sweden. Implement Sci 2013:8. Available at: http://www.
implementationscience.com/content/8/1/31/prepub Accessed January
31, 2012.
[4] Kumar S, Grimmer-Somers K, Hughes B. The ethics of evidence imple-
mentation in health care. Physiother Res Int 2010;15:96–102.
[5] Caldwell K, Coleman K, Copp G, Bell L, Ghazi F. Preparing for profes-
sional practice: how well does professional training equip health and
social care practitioners to engage in evidence-based practice. Nurse
Educ Today 2007;27:518–28.
[6] Chan S, Clough A. A critical evaluation of evidence-based practices of
physiotherapy in musculoskeletal medicine. IMM 2010;32:163–6.
[7] Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group. Pre-
ferred reporting items for systematic reviews and meta-analyses: The
PRISMA Statement. Ann Intern Med 2009:151. Available at: http://
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





