NURBN 2012: Betsy's Acute Coronary Syndrome - A Nursing Case Study
VerifiedAdded on 2022/11/29
|10
|3121
|160
Case Study
AI Summary
This nursing case study delves into the diagnosis and management of Acute Coronary Syndrome (ACS) through the fictional case of Betsy. It begins by justifying the use of ECG despite the absence of typical chest pain symptoms, highlighting the importance of recognizing atypical presentations like shortness of breath and nausea. The study thoroughly explains the pathophysiology of various types of angina (stable, unstable, STEMI, and NSTEMI), emphasizing the role of blocked arteries and reduced oxygen supply. An analysis of Betsy's ECG results suggests a possible inferolateral NSTEMI, prompting further cardiac analysis. The report discusses key findings indicative of ACS, such as ST-segment elevation and T-wave inversion, and explores the mechanisms of action, side effects, and nursing considerations for drugs like GTN, diltiazem, and pravastatin. Furthermore, it elucidates the combined use of aspirin and ticagrelor in cardiac patients and addresses the controversial use of morphine in ACS, considering its potential to delay antiplatelet drug administration. The assignment concludes with a comprehensive understanding of ACS management and related pharmacological interventions.

Running head: NURSING CASE STUDY: BETSY
1
Nursing Case Study: Betsy
Student’s Name
University
1
Nursing Case Study: Betsy
Student’s Name
University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY: BETSY
2
Nursing Case Study: Betsy
Introduction
Acute coronary arteries are the major cause of common cardiac related challenges. This is based
on the narrowing of the arteries due to the presence of fatty acids which block the arteries and in
critical situations can lead to perfusion. The effect is on the heart since it has to work abnormally
to supply the body with the necessary blood flow and oxygen (Azad & Mielniczuk, 2018). The
signs and symptoms of this problem are commonly reported as angina or chest pain. However, as
seen in the case of Betsy the patient may not always feel chest pain but there are indicators like
shortness of breath, nausea, and fatigue among others.
Question 1: rationale for ECG
Despite the fact that Betsy is not feeling any chest pain, she is presenting challenging heart-
related symptoms that have prompted the practitioner to order for an ECG. This is because Betsy
is feeling short of breath, and nauseous which can be an early sign of a heart attack (Ogunlade, et
al., 2015). The role of ECG is to check the electoral activity of the heart through assessing the
rhythm of the heart by detecting signs of irregular heartbeat or any other complications that can
be associated with heart failure. The role of this test is to validate the shortness of breath that she
is feeling to detect any signs of an imminent heart attack.
Question 2:
2a. the pathophysiology of angina
Angina results from the shortness of breath that the patients feel due to reduced supply of oxygen
in the heart thus creating challenges of circulation. In most cases, it is caused by blocked arteries
due to the presence of fats, cholesterol, and lipoproteins that accumulate in the arteries to form
fatty acids which produce extracellular matrix forming atherosclerotic plaque that narrows the
2
Nursing Case Study: Betsy
Introduction
Acute coronary arteries are the major cause of common cardiac related challenges. This is based
on the narrowing of the arteries due to the presence of fatty acids which block the arteries and in
critical situations can lead to perfusion. The effect is on the heart since it has to work abnormally
to supply the body with the necessary blood flow and oxygen (Azad & Mielniczuk, 2018). The
signs and symptoms of this problem are commonly reported as angina or chest pain. However, as
seen in the case of Betsy the patient may not always feel chest pain but there are indicators like
shortness of breath, nausea, and fatigue among others.
Question 1: rationale for ECG
Despite the fact that Betsy is not feeling any chest pain, she is presenting challenging heart-
related symptoms that have prompted the practitioner to order for an ECG. This is because Betsy
is feeling short of breath, and nauseous which can be an early sign of a heart attack (Ogunlade, et
al., 2015). The role of ECG is to check the electoral activity of the heart through assessing the
rhythm of the heart by detecting signs of irregular heartbeat or any other complications that can
be associated with heart failure. The role of this test is to validate the shortness of breath that she
is feeling to detect any signs of an imminent heart attack.
Question 2:
2a. the pathophysiology of angina
Angina results from the shortness of breath that the patients feel due to reduced supply of oxygen
in the heart thus creating challenges of circulation. In most cases, it is caused by blocked arteries
due to the presence of fats, cholesterol, and lipoproteins that accumulate in the arteries to form
fatty acids which produce extracellular matrix forming atherosclerotic plaque that narrows the
NURSING CASE STUDY: BETSY
3
luminal space (Mansour, Reda, Mena, Ghaleb, & Elkersh, 2016). This leads to any of the four
conditions of angina stable/unstable angina and STEMI/NSTEMI. Stable angina
pathophysiology is based on the lack of enough blood supply to the heart due to blockage arteries
from the accumulation of fats.
Cheung & Li (2012) argue that as the arteries block and reduce circulation, the patient feels
squeezing and uncomfortable pressure that extends to the shoulder, neck or jaw. The reason why
this is called stable angina is that the signs can be easily identified from intense physical activity
that the patient engages in. in most cases, the signs start slowly and progress with time. On the
hand, unstable angina is the opposite of stable angina because the signs are normally seen when
one is resting. However, the pathophysiology of its development is similar to stable angina since
it is a result of blocked arteries that reduce the blood flow thus creating discomfort.
According to Díez-Villanueva & Alfonso (2016) STEMI is caused by the buildup of fats that
block arteries reducing blood flow and leading to a heart attack. As the heart struggles to pump
more so that the body can receive enough blood supply, it becomes weakened and leads to other
complications. This means that the heart will be affected while the arteries may rupture due to
excessive pressure to supply blood. Therefore STEMI leads to major complications for the heart
that make it difficult for blood supply, this means that the heart has to pump blood more which in
turn damages its cells. In this case, the arteries may rapture due to excess pressure and pumping
which leads to extensive damage to the heart (Mirza, Taha, & Khdhirc, 2018). In NSTEMI the
complications are similar to STEMI since it is caused by blocking of arteries but the effects are
less since the obstructed coronary arteries are partially damaged leading to less damage to the
heart. In all the three conditions, one common thing in all the conditions is that they result from
blocked arteries which lead to different complications of the heart.
3
luminal space (Mansour, Reda, Mena, Ghaleb, & Elkersh, 2016). This leads to any of the four
conditions of angina stable/unstable angina and STEMI/NSTEMI. Stable angina
pathophysiology is based on the lack of enough blood supply to the heart due to blockage arteries
from the accumulation of fats.
Cheung & Li (2012) argue that as the arteries block and reduce circulation, the patient feels
squeezing and uncomfortable pressure that extends to the shoulder, neck or jaw. The reason why
this is called stable angina is that the signs can be easily identified from intense physical activity
that the patient engages in. in most cases, the signs start slowly and progress with time. On the
hand, unstable angina is the opposite of stable angina because the signs are normally seen when
one is resting. However, the pathophysiology of its development is similar to stable angina since
it is a result of blocked arteries that reduce the blood flow thus creating discomfort.
According to Díez-Villanueva & Alfonso (2016) STEMI is caused by the buildup of fats that
block arteries reducing blood flow and leading to a heart attack. As the heart struggles to pump
more so that the body can receive enough blood supply, it becomes weakened and leads to other
complications. This means that the heart will be affected while the arteries may rupture due to
excessive pressure to supply blood. Therefore STEMI leads to major complications for the heart
that make it difficult for blood supply, this means that the heart has to pump blood more which in
turn damages its cells. In this case, the arteries may rapture due to excess pressure and pumping
which leads to extensive damage to the heart (Mirza, Taha, & Khdhirc, 2018). In NSTEMI the
complications are similar to STEMI since it is caused by blocking of arteries but the effects are
less since the obstructed coronary arteries are partially damaged leading to less damage to the
heart. In all the three conditions, one common thing in all the conditions is that they result from
blocked arteries which lead to different complications of the heart.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING CASE STUDY: BETSY
4
2b. risk factors specific to Bets
Hypertension and type 2 Diabetes Mellitus
3. Analysis of ECG results
The role of ECG is to assess the heart rate of the patient to determine if there is a problem or not.
From the results, Betsy does not show challenges of angina or heart attack because she is
presenting normal signs in QTc and ST/T analysis and an inverted T wave of I, II, III and Avf,
the V4-V5.ST elevation in Avr>1mm. These results show that there could be silent angina which
has not been realized by the ECG. However, the patient may be having an inferolated NSTEMI
from the t-wave inversion that fits in the ischemic chest pain. The fact that Betsy has not
reported any signs of angina and the ST elevation shows that her left main occlusion which
means that there is the need for cardiac analysis of the patient to determine the Percutaneous
coronary intervention that can be done on the patient to reduce the narrowed artery effects.
Question 4: findings of Acute Coronary Syndrome is suspected when specific clinical criteria are
met
ECG measures are one of the primary measures that can be used to determine the presence of
acute coronary syndrome signs in a patient. Through ECG, electromagnetic abnormalities can be
measured in a patient to detect specific signs that point to the presence of the condition. The first
indicator that can be seen from the tests done to Betsy is the ST-segment elevation that is mostly
regarded as a measure of raptured unstable atheroma plaque due to occlusion of an epicardial
artery (Oliveira, Feitosa-Filho, & FontelesRitt, 2012). From the signs, Betsy seems to have an
acute coronary syndrome. The second sign of the presence of the problem that Betsy is having is
the fact that the ECG signs show T-wave tenting or inversion. This inversion shows that there is
a problem with the heart rate of the patient because there is an inverted lead of AVR showing
4
2b. risk factors specific to Bets
Hypertension and type 2 Diabetes Mellitus
3. Analysis of ECG results
The role of ECG is to assess the heart rate of the patient to determine if there is a problem or not.
From the results, Betsy does not show challenges of angina or heart attack because she is
presenting normal signs in QTc and ST/T analysis and an inverted T wave of I, II, III and Avf,
the V4-V5.ST elevation in Avr>1mm. These results show that there could be silent angina which
has not been realized by the ECG. However, the patient may be having an inferolated NSTEMI
from the t-wave inversion that fits in the ischemic chest pain. The fact that Betsy has not
reported any signs of angina and the ST elevation shows that her left main occlusion which
means that there is the need for cardiac analysis of the patient to determine the Percutaneous
coronary intervention that can be done on the patient to reduce the narrowed artery effects.
Question 4: findings of Acute Coronary Syndrome is suspected when specific clinical criteria are
met
ECG measures are one of the primary measures that can be used to determine the presence of
acute coronary syndrome signs in a patient. Through ECG, electromagnetic abnormalities can be
measured in a patient to detect specific signs that point to the presence of the condition. The first
indicator that can be seen from the tests done to Betsy is the ST-segment elevation that is mostly
regarded as a measure of raptured unstable atheroma plaque due to occlusion of an epicardial
artery (Oliveira, Feitosa-Filho, & FontelesRitt, 2012). From the signs, Betsy seems to have an
acute coronary syndrome. The second sign of the presence of the problem that Betsy is having is
the fact that the ECG signs show T-wave tenting or inversion. This inversion shows that there is
a problem with the heart rate of the patient because there is an inverted lead of AVR showing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY: BETSY
5
that there is a problem with her heart. The fact that the wave and QRS are not in the same
direction and is asymmetric and the first half is moving slowly means that the patient is having
problems with her heart. Lastly, the presence of chest discomfort or angina pectoris that has been
reported by the patient means there is the presence of acute coronary artery problem which has
created discomfort due to heaviness in breathing.
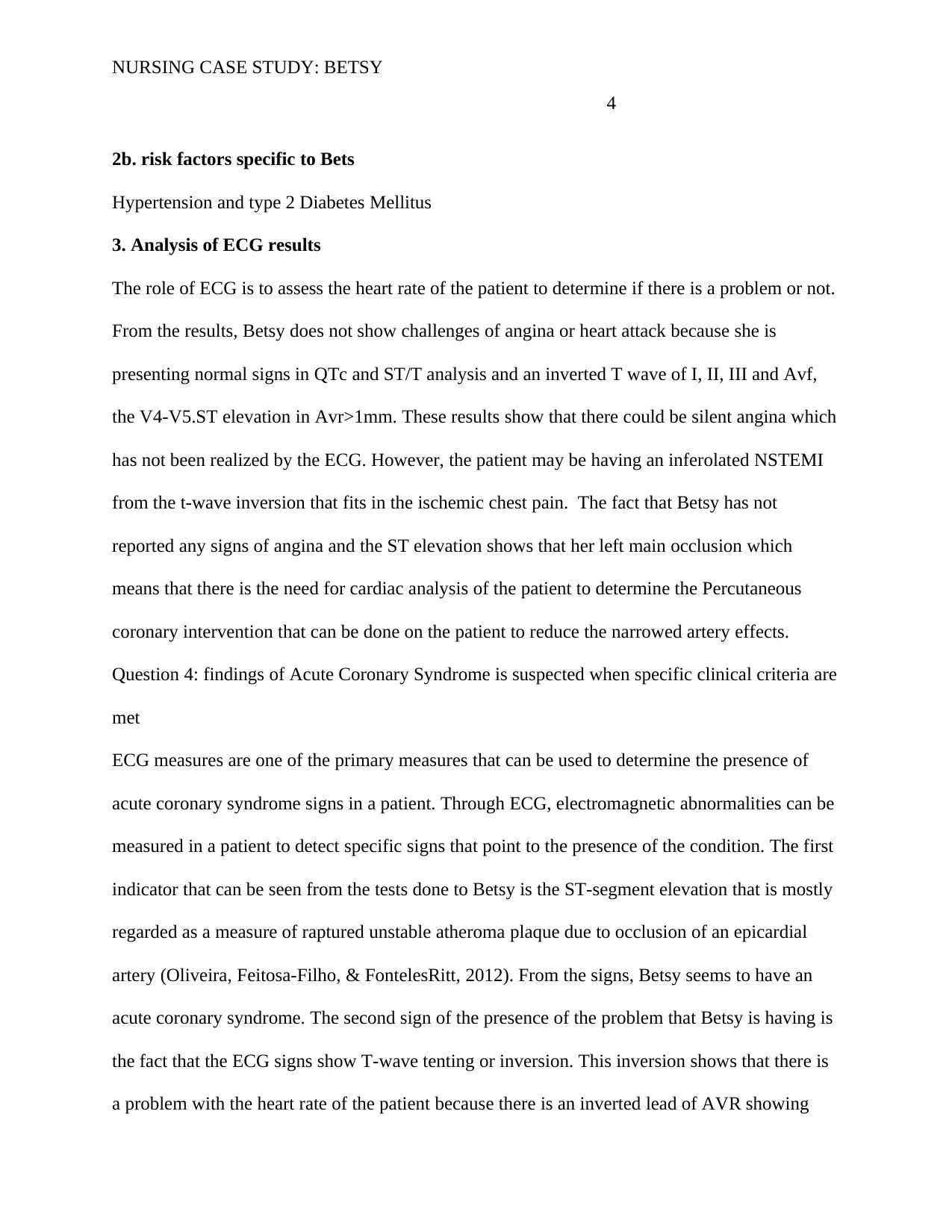
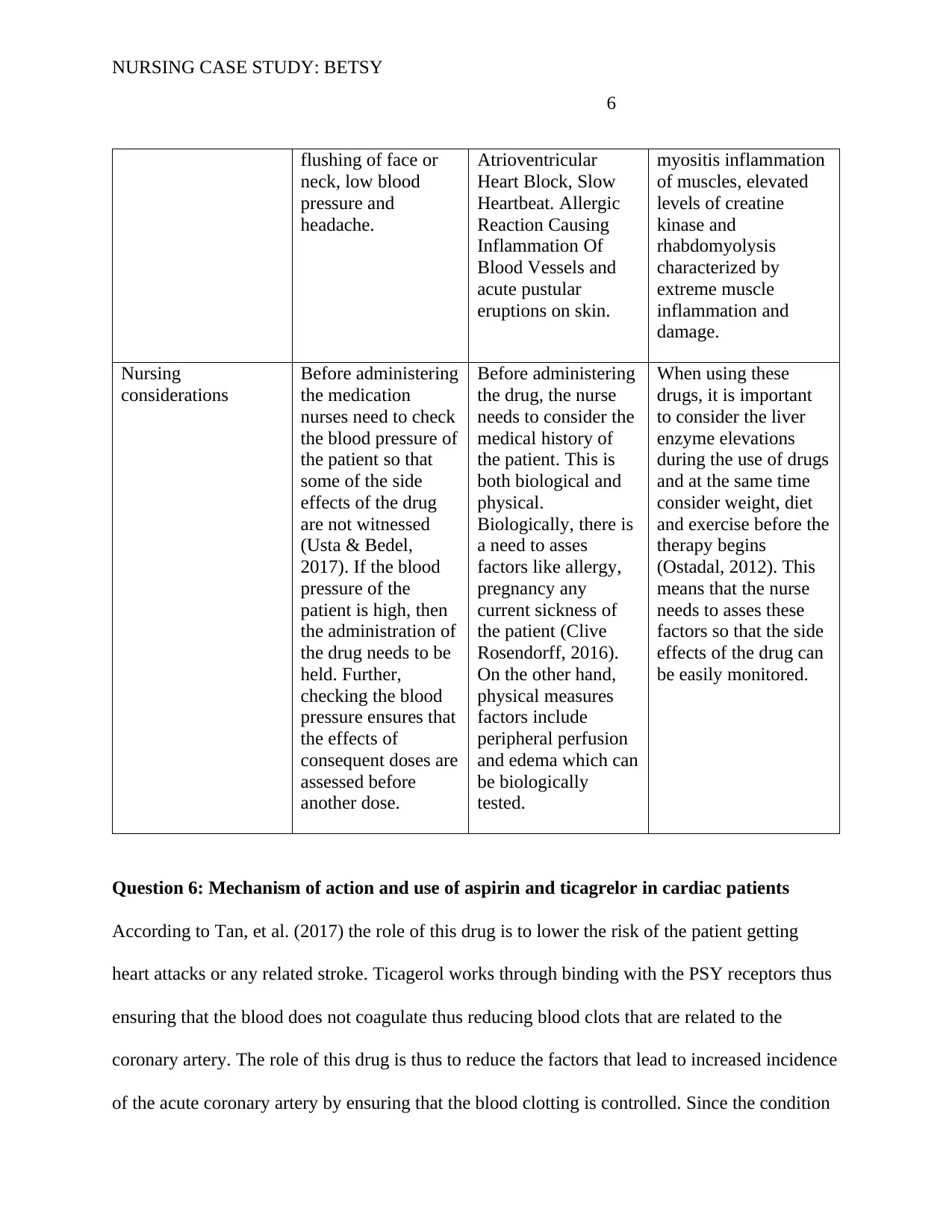
Question 5 discussion of drugs: GTN, diltiazem and pravastatin
Generic Name GTN Diltiazaen Pravastatin
Drug group nitrates Calcium-channel
blockers
Statins
Mechanism of action This drug works as a
vasodilating agent
for relaxing the
vascular muscles
thus increasing blood
circulation. Usta &
Bedel (2017) suggest
that the outcome of
the action is
reducing ventricular
pressure if taken in
small doses while
high doses of the
drug lead to reduced
systematic vascular
afterload thus
increasing cardiac
output.
The drug is
commonly used for
the treatment of high
blood pressure and
limiting the signs and
symptoms of angina
that always create
discomfort in most
patients (Clive
Rosendorff, 2016).
By relaxing the blood
vessels, the drug
makes it easy for
pumping blood thus
reducing the stress
that the heart suffers
from blocked
arteries. When the
supply of oxygen is
increased and the
heart does not have
to pump harder than
normal, then the
chest pain is reduced
since there is an
increased supply of
oxygen.
This type of drug
works through
inhibiting the function
of
Hydroxymethyl
glutaryl-COA
reductase. The action
of the drug is through
hindering the action of
HMG-CoA. Chest pain
is caused by blocked
arteries due to the
presence of
lipoproteins (Ostadal,
2012). Thus by
limiting their synthesis
the supply of
cholesterol in the
bloodstream is reduced
thus reducing the pain
and discomfort caused
by excessive pumping
of the heart.
Complications/side
effects
The common side
effects that the
Side effects of this
drug are seen in a
The common side
effects of this drug are
5
that there is a problem with her heart. The fact that the wave and QRS are not in the same
direction and is asymmetric and the first half is moving slowly means that the patient is having
problems with her heart. Lastly, the presence of chest discomfort or angina pectoris that has been
reported by the patient means there is the presence of acute coronary artery problem which has
created discomfort due to heaviness in breathing.
Question 5 discussion of drugs: GTN, diltiazem and pravastatin
Generic Name GTN Diltiazaen Pravastatin
Drug group nitrates Calcium-channel
blockers
Statins
Mechanism of action This drug works as a
vasodilating agent
for relaxing the
vascular muscles
thus increasing blood
circulation. Usta &
Bedel (2017) suggest
that the outcome of
the action is
reducing ventricular
pressure if taken in
small doses while
high doses of the
drug lead to reduced
systematic vascular
afterload thus
increasing cardiac
output.
The drug is
commonly used for
the treatment of high
blood pressure and
limiting the signs and
symptoms of angina
that always create
discomfort in most
patients (Clive
Rosendorff, 2016).
By relaxing the blood
vessels, the drug
makes it easy for
pumping blood thus
reducing the stress
that the heart suffers
from blocked
arteries. When the
supply of oxygen is
increased and the
heart does not have
to pump harder than
normal, then the
chest pain is reduced
since there is an
increased supply of
oxygen.
This type of drug
works through
inhibiting the function
of
Hydroxymethyl
glutaryl-COA
reductase. The action
of the drug is through
hindering the action of
HMG-CoA. Chest pain
is caused by blocked
arteries due to the
presence of
lipoproteins (Ostadal,
2012). Thus by
limiting their synthesis
the supply of
cholesterol in the
bloodstream is reduced
thus reducing the pain
and discomfort caused
by excessive pumping
of the heart.
Complications/side
effects
The common side
effects that the
Side effects of this
drug are seen in a
The common side
effects of this drug are
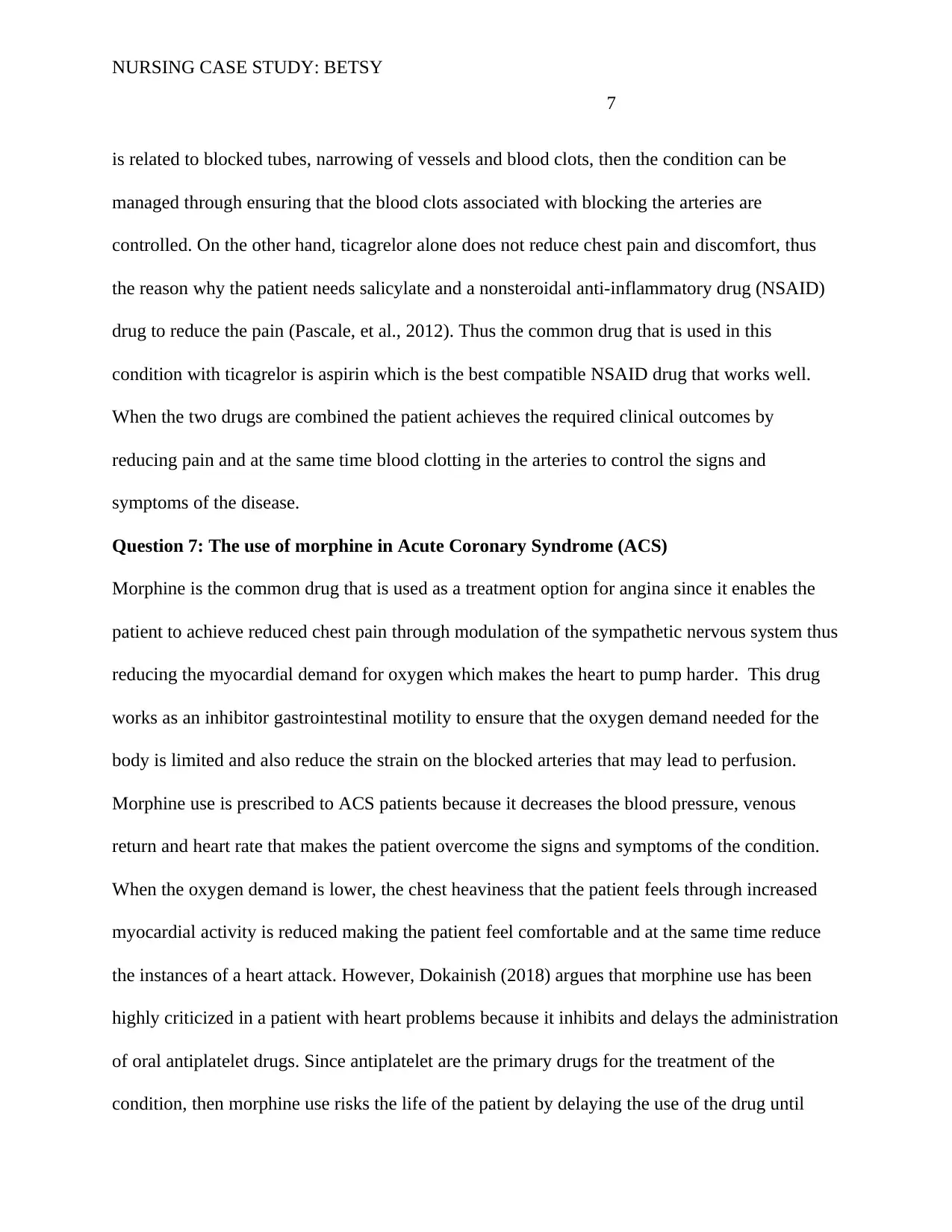
NURSING CASE STUDY: BETSY
6
flushing of face or
neck, low blood
pressure and
headache.
Atrioventricular
Heart Block, Slow
Heartbeat. Allergic
Reaction Causing
Inflammation Of
Blood Vessels and
acute pustular
eruptions on skin.
myositis inflammation
of muscles, elevated
levels of creatine
kinase and
rhabdomyolysis
characterized by
extreme muscle
inflammation and
damage.
Nursing
considerations
Before administering
the medication
nurses need to check
the blood pressure of
the patient so that
some of the side
effects of the drug
are not witnessed
(Usta & Bedel,
2017). If the blood
pressure of the
patient is high, then
the administration of
the drug needs to be
held. Further,
checking the blood
pressure ensures that
the effects of
consequent doses are
assessed before
another dose.
Before administering
the drug, the nurse
needs to consider the
medical history of
the patient. This is
both biological and
physical.
Biologically, there is
a need to asses
factors like allergy,
pregnancy any
current sickness of
the patient (Clive
Rosendorff, 2016).
On the other hand,
physical measures
factors include
peripheral perfusion
and edema which can
be biologically
tested.
When using these
drugs, it is important
to consider the liver
enzyme elevations
during the use of drugs
and at the same time
consider weight, diet
and exercise before the
therapy begins
(Ostadal, 2012). This
means that the nurse
needs to asses these
factors so that the side
effects of the drug can
be easily monitored.
Question 6: Mechanism of action and use of aspirin and ticagrelor in cardiac patients
According to Tan, et al. (2017) the role of this drug is to lower the risk of the patient getting
heart attacks or any related stroke. Ticagerol works through binding with the PSY receptors thus
ensuring that the blood does not coagulate thus reducing blood clots that are related to the
coronary artery. The role of this drug is thus to reduce the factors that lead to increased incidence
of the acute coronary artery by ensuring that the blood clotting is controlled. Since the condition
6
flushing of face or
neck, low blood
pressure and
headache.
Atrioventricular
Heart Block, Slow
Heartbeat. Allergic
Reaction Causing
Inflammation Of
Blood Vessels and
acute pustular
eruptions on skin.
myositis inflammation
of muscles, elevated
levels of creatine
kinase and
rhabdomyolysis
characterized by
extreme muscle
inflammation and
damage.
Nursing
considerations
Before administering
the medication
nurses need to check
the blood pressure of
the patient so that
some of the side
effects of the drug
are not witnessed
(Usta & Bedel,
2017). If the blood
pressure of the
patient is high, then
the administration of
the drug needs to be
held. Further,
checking the blood
pressure ensures that
the effects of
consequent doses are
assessed before
another dose.
Before administering
the drug, the nurse
needs to consider the
medical history of
the patient. This is
both biological and
physical.
Biologically, there is
a need to asses
factors like allergy,
pregnancy any
current sickness of
the patient (Clive
Rosendorff, 2016).
On the other hand,
physical measures
factors include
peripheral perfusion
and edema which can
be biologically
tested.
When using these
drugs, it is important
to consider the liver
enzyme elevations
during the use of drugs
and at the same time
consider weight, diet
and exercise before the
therapy begins
(Ostadal, 2012). This
means that the nurse
needs to asses these
factors so that the side
effects of the drug can
be easily monitored.
Question 6: Mechanism of action and use of aspirin and ticagrelor in cardiac patients
According to Tan, et al. (2017) the role of this drug is to lower the risk of the patient getting
heart attacks or any related stroke. Ticagerol works through binding with the PSY receptors thus
ensuring that the blood does not coagulate thus reducing blood clots that are related to the
coronary artery. The role of this drug is thus to reduce the factors that lead to increased incidence
of the acute coronary artery by ensuring that the blood clotting is controlled. Since the condition
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING CASE STUDY: BETSY
7
is related to blocked tubes, narrowing of vessels and blood clots, then the condition can be
managed through ensuring that the blood clots associated with blocking the arteries are
controlled. On the other hand, ticagrelor alone does not reduce chest pain and discomfort, thus
the reason why the patient needs salicylate and a nonsteroidal anti-inflammatory drug (NSAID)
drug to reduce the pain (Pascale, et al., 2012). Thus the common drug that is used in this
condition with ticagrelor is aspirin which is the best compatible NSAID drug that works well.
When the two drugs are combined the patient achieves the required clinical outcomes by
reducing pain and at the same time blood clotting in the arteries to control the signs and
symptoms of the disease.
Question 7: The use of morphine in Acute Coronary Syndrome (ACS)
Morphine is the common drug that is used as a treatment option for angina since it enables the
patient to achieve reduced chest pain through modulation of the sympathetic nervous system thus
reducing the myocardial demand for oxygen which makes the heart to pump harder. This drug
works as an inhibitor gastrointestinal motility to ensure that the oxygen demand needed for the
body is limited and also reduce the strain on the blocked arteries that may lead to perfusion.
Morphine use is prescribed to ACS patients because it decreases the blood pressure, venous
return and heart rate that makes the patient overcome the signs and symptoms of the condition.
When the oxygen demand is lower, the chest heaviness that the patient feels through increased
myocardial activity is reduced making the patient feel comfortable and at the same time reduce
the instances of a heart attack. However, Dokainish (2018) argues that morphine use has been
highly criticized in a patient with heart problems because it inhibits and delays the administration
of oral antiplatelet drugs. Since antiplatelet are the primary drugs for the treatment of the
condition, then morphine use risks the life of the patient by delaying the use of the drug until
7
is related to blocked tubes, narrowing of vessels and blood clots, then the condition can be
managed through ensuring that the blood clots associated with blocking the arteries are
controlled. On the other hand, ticagrelor alone does not reduce chest pain and discomfort, thus
the reason why the patient needs salicylate and a nonsteroidal anti-inflammatory drug (NSAID)
drug to reduce the pain (Pascale, et al., 2012). Thus the common drug that is used in this
condition with ticagrelor is aspirin which is the best compatible NSAID drug that works well.
When the two drugs are combined the patient achieves the required clinical outcomes by
reducing pain and at the same time blood clotting in the arteries to control the signs and
symptoms of the disease.
Question 7: The use of morphine in Acute Coronary Syndrome (ACS)
Morphine is the common drug that is used as a treatment option for angina since it enables the
patient to achieve reduced chest pain through modulation of the sympathetic nervous system thus
reducing the myocardial demand for oxygen which makes the heart to pump harder. This drug
works as an inhibitor gastrointestinal motility to ensure that the oxygen demand needed for the
body is limited and also reduce the strain on the blocked arteries that may lead to perfusion.
Morphine use is prescribed to ACS patients because it decreases the blood pressure, venous
return and heart rate that makes the patient overcome the signs and symptoms of the condition.
When the oxygen demand is lower, the chest heaviness that the patient feels through increased
myocardial activity is reduced making the patient feel comfortable and at the same time reduce
the instances of a heart attack. However, Dokainish (2018) argues that morphine use has been
highly criticized in a patient with heart problems because it inhibits and delays the administration
of oral antiplatelet drugs. Since antiplatelet are the primary drugs for the treatment of the
condition, then morphine use risks the life of the patient by delaying the use of the drug until
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY: BETSY
8
tests have been done. Thus despite the effectiveness of the drug, it presents other medical
compatibility challenges that can complicate the medication process.
Question 8: the link between depressions with chronic illness.
Recent research has indicated increased depression in patients who have been admitted with
chronic conditions such as acute coronary syndrome. Most of these life-threatening conditions
come with old age which makes their management difficult thus the reason why most patients
with the problem feel depressed and sometimes reported exacerbated chronic conditions and
depression (Fung, et al., 2018). Thus when depressed such patients report higher and risky
symptoms of the chronic conditions that they have making it difficult for them to manage. This is
the reason why depression is the leading mortality factor in patients with chronic conditions.
This calls for the need for research to determine strategies that can be used to control late
depression in patients with chronic conditions.
Conclusion
Acute coronary arteries is a condition that can be managed if the patient understands the triggers
and signs that create the effects of the drug. Through patient-centered approaches, Betsy can be
assisted to manage the condition and live a normal life by taking the medications appropriately
and at the same time understanding the factors that exacerbate the condition. Healthcare
professionals need to assist the patient to develop a care plan that ensures that he leads a life that
allows her to manage the condition and reduce the risk of admission or adverse effects.
8
tests have been done. Thus despite the effectiveness of the drug, it presents other medical
compatibility challenges that can complicate the medication process.
Question 8: the link between depressions with chronic illness.
Recent research has indicated increased depression in patients who have been admitted with
chronic conditions such as acute coronary syndrome. Most of these life-threatening conditions
come with old age which makes their management difficult thus the reason why most patients
with the problem feel depressed and sometimes reported exacerbated chronic conditions and
depression (Fung, et al., 2018). Thus when depressed such patients report higher and risky
symptoms of the chronic conditions that they have making it difficult for them to manage. This is
the reason why depression is the leading mortality factor in patients with chronic conditions.
This calls for the need for research to determine strategies that can be used to control late
depression in patients with chronic conditions.
Conclusion
Acute coronary arteries is a condition that can be managed if the patient understands the triggers
and signs that create the effects of the drug. Through patient-centered approaches, Betsy can be
assisted to manage the condition and live a normal life by taking the medications appropriately
and at the same time understanding the factors that exacerbate the condition. Healthcare
professionals need to assist the patient to develop a care plan that ensures that he leads a life that
allows her to manage the condition and reduce the risk of admission or adverse effects.
NURSING CASE STUDY: BETSY
9
References
Azad, N., & Mielniczuk, L. (2018). A call for collaboration: improving cardiogeriatric care.
Canadian Journal of Cardiology, 22, 1041-1044.
Cheung, B. M., & Li, C. (2012). Diabetes and Hypertension: Is There a Common Metabolic
Pathway? Current Atherosclerosis Reports, 14(2), 160-166.
Clive Rosendorff. (2016). Treatment of Hypertension in Patients with Coronary Artery Disease.
A Case-Based Summary of the 2015 AHA/ACC/ASH Scientific Statement. The
American Journal of Medicine, 129(4), 373-378.
Díez-Villanueva, P., & Alfonso, F. (2016). Heart failure in the elderly. Revista Latino-
Americana de Enfermagem,, 13(2), 115-117.
Dokainish, H. (2018). Medical therapy for heart failure: the evidence exists, but is it being
followed? The Lancet Global Health, 6(9), 42-43.
Fung, E., Hui, E., Yang, X., Lui, L. T., Cheng, K. F., Li, Q., & Woo, J. (2018). Heart Failure and
Frailty in the Community-Living Elderly Population: What the UFO Study Will Tell Us.
Frontiers in Psychology,, 9(347), 15-22.
Mansour, H., Reda, A., Mena, M., Ghaleb, R., & Elkersh, A. (2016). Pattern of risk factors and
management strategies in patients with acute coronary syndrome, in different age groups
and sex categories. Atherosclerosis Supplements, 25, 7-15.
Mirza, A. J., Taha, A. Y., & Khdhirc, B. R. (2018). Risk factors for acute coronary syndrome in
patients below the age of 40 years. The Egyptian heart journal, 70(4), 233–235.
Ogunlade, O., Ayoka, A. O., Akomolafe, R. O., Akinsomisoye, O. S., Irinoye, A. I., Ajao, A., &
Asafa, M. A. (2015). The role of electrocardiogram in the diagnosis of dextrocardia with
9
References
Azad, N., & Mielniczuk, L. (2018). A call for collaboration: improving cardiogeriatric care.
Canadian Journal of Cardiology, 22, 1041-1044.
Cheung, B. M., & Li, C. (2012). Diabetes and Hypertension: Is There a Common Metabolic
Pathway? Current Atherosclerosis Reports, 14(2), 160-166.
Clive Rosendorff. (2016). Treatment of Hypertension in Patients with Coronary Artery Disease.
A Case-Based Summary of the 2015 AHA/ACC/ASH Scientific Statement. The
American Journal of Medicine, 129(4), 373-378.
Díez-Villanueva, P., & Alfonso, F. (2016). Heart failure in the elderly. Revista Latino-
Americana de Enfermagem,, 13(2), 115-117.
Dokainish, H. (2018). Medical therapy for heart failure: the evidence exists, but is it being
followed? The Lancet Global Health, 6(9), 42-43.
Fung, E., Hui, E., Yang, X., Lui, L. T., Cheng, K. F., Li, Q., & Woo, J. (2018). Heart Failure and
Frailty in the Community-Living Elderly Population: What the UFO Study Will Tell Us.
Frontiers in Psychology,, 9(347), 15-22.
Mansour, H., Reda, A., Mena, M., Ghaleb, R., & Elkersh, A. (2016). Pattern of risk factors and
management strategies in patients with acute coronary syndrome, in different age groups
and sex categories. Atherosclerosis Supplements, 25, 7-15.
Mirza, A. J., Taha, A. Y., & Khdhirc, B. R. (2018). Risk factors for acute coronary syndrome in
patients below the age of 40 years. The Egyptian heart journal, 70(4), 233–235.
Ogunlade, O., Ayoka, A. O., Akomolafe, R. O., Akinsomisoye, O. S., Irinoye, A. I., Ajao, A., &
Asafa, M. A. (2015). The role of electrocardiogram in the diagnosis of dextrocardia with
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING CASE STUDY: BETSY
10
mirror image atrial arrangement and ventricular position in a young adult Nigerian in Ile-
Ife: a case report. Journal of Medical Care Reports, 9(222).
Oliveira, F. C., Feitosa-Filho, G. S., & FontelesRitt, L. E. (2012). Use of beta-blockers for the
treatment of cardiac arrest due to ventricular fibrillation/pulseless ventricular tachycardia.
A systematic review. Resuscitation, 83(6), 674-683.
Ostadal, P. (2012). Statins as first-line therapy for acute coronary syndrome? Experimental and
clinical cardiology, 17(4), 227–236.
Pascale, S., Petrucci, G., Dragani, A., Habib, A., Zaccardi, F., Pagliaccia, F., . . . Patrono, C.
(2012). Aspirin-insensitive thromboxane biosynthesis in essential thrombocythemia is
explained by accelerated renewal of the drug target. Blood, 10(5), 3595-3603.
Tan, Q., Jiang, X., Huang, S., Zhang, T., Chen, L., Xie, S., . . . Cai, S. (2017). The clinical
efficacy and safety evaluation of ticagrelor for acute coronary syndrome in general ACS
patients and diabetic patients: A systematic review and meta-analysis. PLoS One, 12(5).
Usta, C., & Bedel, A. (2017). Update on pharmacological treatment of acute coronary syndrome
without persistent ST segment elevation myocardial infarction in the elderly. Journal of
Geriatric Cardiology, 14(7), 457-464.
10
mirror image atrial arrangement and ventricular position in a young adult Nigerian in Ile-
Ife: a case report. Journal of Medical Care Reports, 9(222).
Oliveira, F. C., Feitosa-Filho, G. S., & FontelesRitt, L. E. (2012). Use of beta-blockers for the
treatment of cardiac arrest due to ventricular fibrillation/pulseless ventricular tachycardia.
A systematic review. Resuscitation, 83(6), 674-683.
Ostadal, P. (2012). Statins as first-line therapy for acute coronary syndrome? Experimental and
clinical cardiology, 17(4), 227–236.
Pascale, S., Petrucci, G., Dragani, A., Habib, A., Zaccardi, F., Pagliaccia, F., . . . Patrono, C.
(2012). Aspirin-insensitive thromboxane biosynthesis in essential thrombocythemia is
explained by accelerated renewal of the drug target. Blood, 10(5), 3595-3603.
Tan, Q., Jiang, X., Huang, S., Zhang, T., Chen, L., Xie, S., . . . Cai, S. (2017). The clinical
efficacy and safety evaluation of ticagrelor for acute coronary syndrome in general ACS
patients and diabetic patients: A systematic review and meta-analysis. PLoS One, 12(5).
Usta, C., & Bedel, A. (2017). Update on pharmacological treatment of acute coronary syndrome
without persistent ST segment elevation myocardial infarction in the elderly. Journal of
Geriatric Cardiology, 14(7), 457-464.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





