NURBN 2012: Clinical Scenario Report on Acute Coronary Syndrome
VerifiedAdded on 2023/01/23
|13
|3190
|91
Report
AI Summary
This report provides a comprehensive analysis of a clinical scenario involving acute coronary syndrome (ACS). It begins with an executive summary and introduction, followed by an in-depth discussion of the pathophysiology of angina pectoris, including stable, unstable, NSTEMI, and STEMI angina. The report examines the rationale for performing an ECG and interprets the patient's ECG results, identifying sinus tachycardia and ST-segment elevation. It explores the risk factors associated with ACS, such as hypertension and type II diabetes mellitus. The report then details the clinical criteria for diagnosing ACS, including ST-segment elevation, sinus tachycardia, and increased heart rate. A detailed discussion of the mechanism of action, side effects, and nursing considerations for various drugs used in ACS treatment, including GTN, Diltiazem, Pravastatin, Aspirin, Ticagrelor, and Morphine is included. Furthermore, the report explores the use of morphine in ACS and the relationship between coronary heart disease and depression. The report concludes with a summary of the key findings and provides a list of relevant references.

Running Head: ACUTE CORONARY SYNDROME
Acute Coronary Syndrome
Acute Coronary Syndrome
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 2
Executive Summary
Angina is a medical condition characterized by chest pain and discomfort due to coronary
heart disease. In the following evaluation, the pathophysiology of the disease has been
discussed briefly. The types of angina and the reasons for performing an ECG have also been
analyzed. Several abnormal interpretations have also been examined on the patient's ECG. In
the evaluation, several important factors that may be useful in the diagnosis of coronary
syndrome have also been identified. In addition, the mechanism of action of drugs, as well as
the relationship between depression and chronic diseases has also been explained.
Executive Summary
Angina is a medical condition characterized by chest pain and discomfort due to coronary
heart disease. In the following evaluation, the pathophysiology of the disease has been
discussed briefly. The types of angina and the reasons for performing an ECG have also been
analyzed. Several abnormal interpretations have also been examined on the patient's ECG. In
the evaluation, several important factors that may be useful in the diagnosis of coronary
syndrome have also been identified. In addition, the mechanism of action of drugs, as well as
the relationship between depression and chronic diseases has also been explained.
ACUTE CORONARY SYNDROME 3
CONTENTS
Executive Summary.............................................................................................................................2
INTRODUCTION...............................................................................................................................4
ECG RATIONALE:............................................................................................................................5
ANGINA PECTORIS PATHOPHYSIOLOGY:...............................................................................5
Stable angina:................................................................................................................................6
Unstable angina:............................................................................................................................6
NSTEMI angina.............................................................................................................................6
Angina STEMI..............................................................................................................................6
RISK FACTOR'S..............................................................................................................................6
ECG INTERPRETATION:................................................................................................................6
DIAGNOSING ACUTE CORONARY SYNDROME:.....................................................................7
DRUGS DISCUSSION........................................................................................................................7
THE ACTION MECHANISM AND USE:........................................................................................9
THE UTILISATION OF MORPHINE IN ACS:............................................................................10
CORONARY HEART DISEASE AND DEPRESSION:................................................................10
CONCLUSION:.................................................................................................................................11
REFERENCES..................................................................................................................................12
CONTENTS
Executive Summary.............................................................................................................................2
INTRODUCTION...............................................................................................................................4
ECG RATIONALE:............................................................................................................................5
ANGINA PECTORIS PATHOPHYSIOLOGY:...............................................................................5
Stable angina:................................................................................................................................6
Unstable angina:............................................................................................................................6
NSTEMI angina.............................................................................................................................6
Angina STEMI..............................................................................................................................6
RISK FACTOR'S..............................................................................................................................6
ECG INTERPRETATION:................................................................................................................6
DIAGNOSING ACUTE CORONARY SYNDROME:.....................................................................7
DRUGS DISCUSSION........................................................................................................................7
THE ACTION MECHANISM AND USE:........................................................................................9
THE UTILISATION OF MORPHINE IN ACS:............................................................................10
CORONARY HEART DISEASE AND DEPRESSION:................................................................10
CONCLUSION:.................................................................................................................................11
REFERENCES..................................................................................................................................12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE CORONARY SYNDROME 4
INTRODUCTION:
Angina is a medical condition characterized by chest pain and discomfort due to
coronary heart disease. In the following evaluation, the pathophysiology of the disease has
been discussed briefly. The types of angina and the reasons for performing an ECG have also
been analyzed. Several abnormal interpretations have also been examined on the patient's
ECG. In the evaluation, several important factors that may be useful in the diagnosis of
coronary syndrome have also been identified. In addition, the mechanism of action of drugs,
as well as the relationship between depression and chronic diseases has also been explained.
ECG RATIONALE:
To have underlying evidence the buddy nurse was said to have an ECG test, even she
was not having any chest pain. We know that ECG is being performed for the patients that
undergo surgery or previously they had the history of COPD or having shortness of breath
issue with the cardiac (Rawat & Sharma, 2018). Moreover, the complications along with the
abnormalities in 12 Lead electrocardiograms can help to analyse and predict the future
complications of myocardial infractions, heart failure and angina for the professionals. It can
be done by the ST elevation, ST depression and T wave inversion. Therefore, the rationale of
the ECG is done to study and examine the cardiac complications that exist within the patient.
ANGINA PECTORIS PATHOPHYSIOLOGY:
Betsy is diagnosed with angina pectoris, which is characterized by extreme chest pain.
It is the consequence of myocardial ischemia that is mainly due to a disturbance in the
balance between the oxygen demand and the blood supply to the myocardium.
Atherosclerosis is one of the main causes that lead to angina (Bentzon, Otsuka, Virmani, &
Falk, 2015). It is a condition in which plaque builds up inside the arteries that restrict the flow
of oxygen-rich blood to the heart muscles. The plaque is mainly composed of cholesterol, fat
and other substances that are found in the blood. To compensate for the loss of oxygen-rich
blood, the heart muscles begin to work rigorously by pumping blood into the muscles more
INTRODUCTION:
Angina is a medical condition characterized by chest pain and discomfort due to
coronary heart disease. In the following evaluation, the pathophysiology of the disease has
been discussed briefly. The types of angina and the reasons for performing an ECG have also
been analyzed. Several abnormal interpretations have also been examined on the patient's
ECG. In the evaluation, several important factors that may be useful in the diagnosis of
coronary syndrome have also been identified. In addition, the mechanism of action of drugs,
as well as the relationship between depression and chronic diseases has also been explained.
ECG RATIONALE:
To have underlying evidence the buddy nurse was said to have an ECG test, even she
was not having any chest pain. We know that ECG is being performed for the patients that
undergo surgery or previously they had the history of COPD or having shortness of breath
issue with the cardiac (Rawat & Sharma, 2018). Moreover, the complications along with the
abnormalities in 12 Lead electrocardiograms can help to analyse and predict the future
complications of myocardial infractions, heart failure and angina for the professionals. It can
be done by the ST elevation, ST depression and T wave inversion. Therefore, the rationale of
the ECG is done to study and examine the cardiac complications that exist within the patient.
ANGINA PECTORIS PATHOPHYSIOLOGY:
Betsy is diagnosed with angina pectoris, which is characterized by extreme chest pain.
It is the consequence of myocardial ischemia that is mainly due to a disturbance in the
balance between the oxygen demand and the blood supply to the myocardium.
Atherosclerosis is one of the main causes that lead to angina (Bentzon, Otsuka, Virmani, &
Falk, 2015). It is a condition in which plaque builds up inside the arteries that restrict the flow
of oxygen-rich blood to the heart muscles. The plaque is mainly composed of cholesterol, fat
and other substances that are found in the blood. To compensate for the loss of oxygen-rich
blood, the heart muscles begin to work rigorously by pumping blood into the muscles more
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 5
strongly, which results in the development of angina. To compensate for the loss of oxygen,
the heart muscles begin the transition from aerobic to anaerobic metabolism. According to
Prisby, adenosine is the key factor that regulates the progression of angina. It has been
reported that to dilate arteries and increase blood supply, adenosine triphosphate degrades
during low blood supply and diffuses into the extracellular space. What results in extreme
chest pain. There are many types of angina pectoris, some of which are the following:
Stable angina: Stable angina is characterized by chest pain or severe discomfort that
occurs more frequently due to stress, anxiety or depression. It is caused by the restriction of
blood flow through the vessels to the heart.
Unstable angina: Unstable angina is a type of angina that develops spontaneously
and unpredictably. Unlike other types, it is not triggered by any stressful activity or condition.
NSTEMI angina (myocardial infarction with ST-segment elevation): is a type of
angina pectoris in which no ST segment is elevated in the 12-lead ECG (Lu et al., 2019).
Angina STEMI (Elevated Myocardial Infarction of the ST Segment): is a type of
angina in which the manifestation of the symptoms of angina occurs as a consequence of a
cardiac necrosis. In this type, the ST segment is elevated in a 12-lead ECG (Acharya et al.,
2017).
RISK FACTOR'S
The two main risk factors that are crucial in this case are: Hypertension and type II
diabetes mellitus. According to the researchers, these conditions are some of the main risk
factors for the development of acute coronary syndrome (Jia, Hill, & Sowers, 2018).
ECG INTERPRETATION:
The ECG report of the patient gave the following results.
Rhythm: The Sinus rhythm is showing complications as sinus tachycardia
Rate: Patients heartbeat is 100 per minute
The regularity of P wave: There is a presence Of P wave, and it is regular too.
strongly, which results in the development of angina. To compensate for the loss of oxygen,
the heart muscles begin the transition from aerobic to anaerobic metabolism. According to
Prisby, adenosine is the key factor that regulates the progression of angina. It has been
reported that to dilate arteries and increase blood supply, adenosine triphosphate degrades
during low blood supply and diffuses into the extracellular space. What results in extreme
chest pain. There are many types of angina pectoris, some of which are the following:
Stable angina: Stable angina is characterized by chest pain or severe discomfort that
occurs more frequently due to stress, anxiety or depression. It is caused by the restriction of
blood flow through the vessels to the heart.
Unstable angina: Unstable angina is a type of angina that develops spontaneously
and unpredictably. Unlike other types, it is not triggered by any stressful activity or condition.
NSTEMI angina (myocardial infarction with ST-segment elevation): is a type of
angina pectoris in which no ST segment is elevated in the 12-lead ECG (Lu et al., 2019).
Angina STEMI (Elevated Myocardial Infarction of the ST Segment): is a type of
angina in which the manifestation of the symptoms of angina occurs as a consequence of a
cardiac necrosis. In this type, the ST segment is elevated in a 12-lead ECG (Acharya et al.,
2017).
RISK FACTOR'S
The two main risk factors that are crucial in this case are: Hypertension and type II
diabetes mellitus. According to the researchers, these conditions are some of the main risk
factors for the development of acute coronary syndrome (Jia, Hill, & Sowers, 2018).
ECG INTERPRETATION:
The ECG report of the patient gave the following results.
Rhythm: The Sinus rhythm is showing complications as sinus tachycardia
Rate: Patients heartbeat is 100 per minute
The regularity of P wave: There is a presence Of P wave, and it is regular too.
ACUTE CORONARY SYNDROME 6
ST segment: Elevation of approximate >=0.1mv.
These deduced results showed that the patient is facing the inferior wall myocardial infarction
and the changes are reciprocal.
DIAGNOSING ACUTE CORONARY SYNDROME:
You can diagnose acute coronary syndrome when the required criteria are met. The
three mains that confirm the acute coronary syndrome are as follows:
1. ST-segment elevation: The ST-elevation is observed when the arteries are blocked
that supply oxygen. That may be due to the formation of thrombus. So, the lasting ST-
elevation leads to a chronic myocardial infarction.
2. Sinus Tachycardia: It occurs to sinus node dysfunction, as well as the withdrawal of
beta-blockers and substance abuse (Sanchis-Gomar, Perez-Quilis, Leischik & Lucia, 2016).
3. Increase Heart rate: It is also leading cause of the acute coronary syndrome as the
not having sufficient supply of blood to heart, that increases the function of heart muscles by
myocardial muscles and heart rate increases.
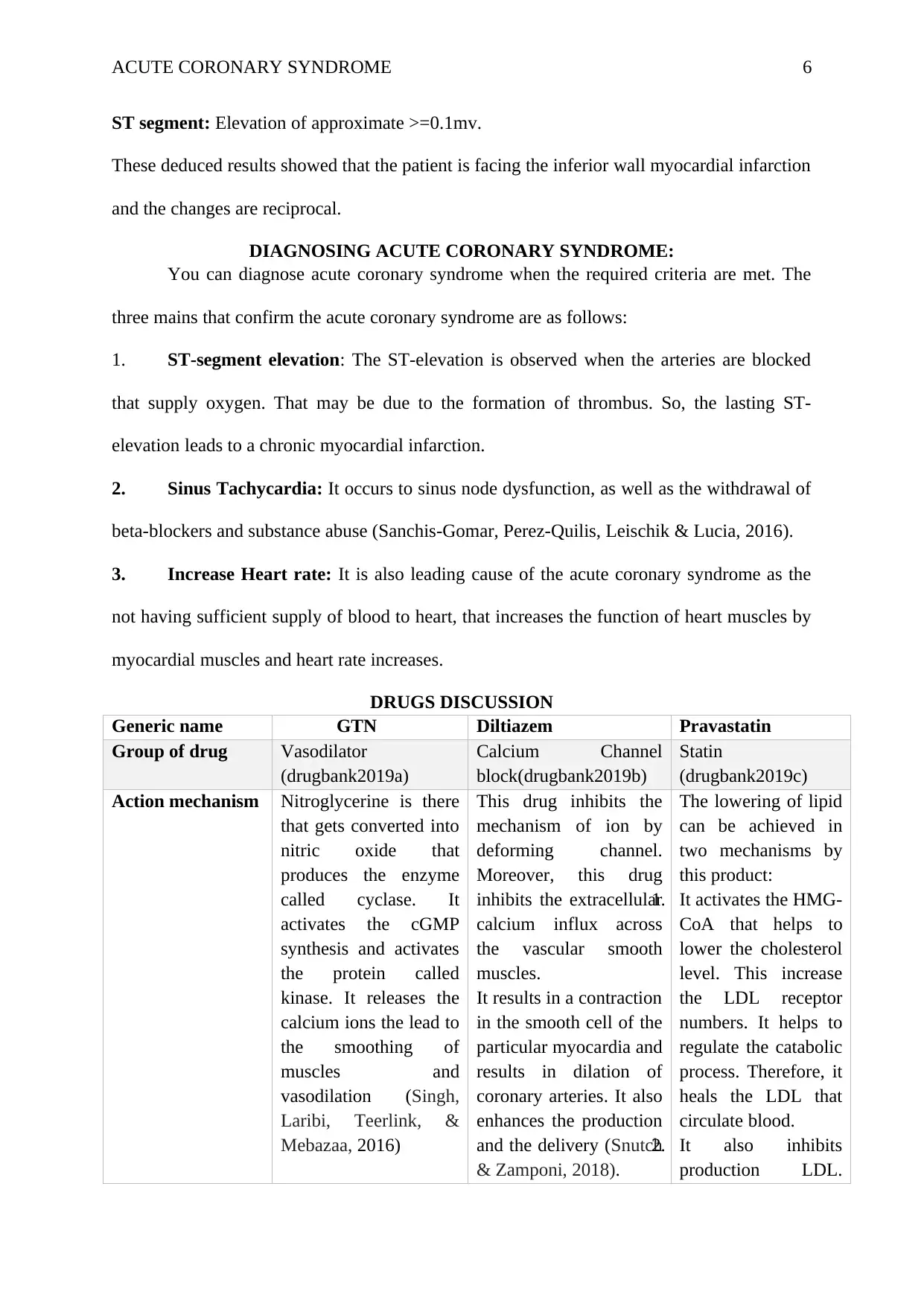
DRUGS DISCUSSION
Generic name GTN Diltiazem Pravastatin
Group of drug Vasodilator
(drugbank2019a)
Calcium Channel
block(drugbank2019b)
Statin
(drugbank2019c)
Action mechanism Nitroglycerine is there
that gets converted into
nitric oxide that
produces the enzyme
called cyclase. It
activates the cGMP
synthesis and activates
the protein called
kinase. It releases the
calcium ions the lead to
the smoothing of
muscles and
vasodilation (Singh,
Laribi, Teerlink, &
Mebazaa, 2016)
This drug inhibits the
mechanism of ion by
deforming channel.
Moreover, this drug
inhibits the extracellular
calcium influx across
the vascular smooth
muscles.
It results in a contraction
in the smooth cell of the
particular myocardia and
results in dilation of
coronary arteries. It also
enhances the production
and the delivery (Snutch
& Zamponi, 2018).
The lowering of lipid
can be achieved in
two mechanisms by
this product:
1. It activates the HMG-
CoA that helps to
lower the cholesterol
level. This increase
the LDL receptor
numbers. It helps to
regulate the catabolic
process. Therefore, it
heals the LDL that
circulate blood.
2. It also inhibits
production LDL.
ST segment: Elevation of approximate >=0.1mv.
These deduced results showed that the patient is facing the inferior wall myocardial infarction
and the changes are reciprocal.
DIAGNOSING ACUTE CORONARY SYNDROME:
You can diagnose acute coronary syndrome when the required criteria are met. The
three mains that confirm the acute coronary syndrome are as follows:
1. ST-segment elevation: The ST-elevation is observed when the arteries are blocked
that supply oxygen. That may be due to the formation of thrombus. So, the lasting ST-
elevation leads to a chronic myocardial infarction.
2. Sinus Tachycardia: It occurs to sinus node dysfunction, as well as the withdrawal of
beta-blockers and substance abuse (Sanchis-Gomar, Perez-Quilis, Leischik & Lucia, 2016).
3. Increase Heart rate: It is also leading cause of the acute coronary syndrome as the
not having sufficient supply of blood to heart, that increases the function of heart muscles by
myocardial muscles and heart rate increases.
DRUGS DISCUSSION
Generic name GTN Diltiazem Pravastatin
Group of drug Vasodilator
(drugbank2019a)
Calcium Channel
block(drugbank2019b)
Statin
(drugbank2019c)
Action mechanism Nitroglycerine is there
that gets converted into
nitric oxide that
produces the enzyme
called cyclase. It
activates the cGMP
synthesis and activates
the protein called
kinase. It releases the
calcium ions the lead to
the smoothing of
muscles and
vasodilation (Singh,
Laribi, Teerlink, &
Mebazaa, 2016)
This drug inhibits the
mechanism of ion by
deforming channel.
Moreover, this drug
inhibits the extracellular
calcium influx across
the vascular smooth
muscles.
It results in a contraction
in the smooth cell of the
particular myocardia and
results in dilation of
coronary arteries. It also
enhances the production
and the delivery (Snutch
& Zamponi, 2018).
The lowering of lipid
can be achieved in
two mechanisms by
this product:
1. It activates the HMG-
CoA that helps to
lower the cholesterol
level. This increase
the LDL receptor
numbers. It helps to
regulate the catabolic
process. Therefore, it
heals the LDL that
circulate blood.
2. It also inhibits
production LDL.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE CORONARY SYNDROME 7
That is done by
blocking the hepatic
synthesis of VLDL.
This acts as the
precursor of LDL
(Mammen, 2016).
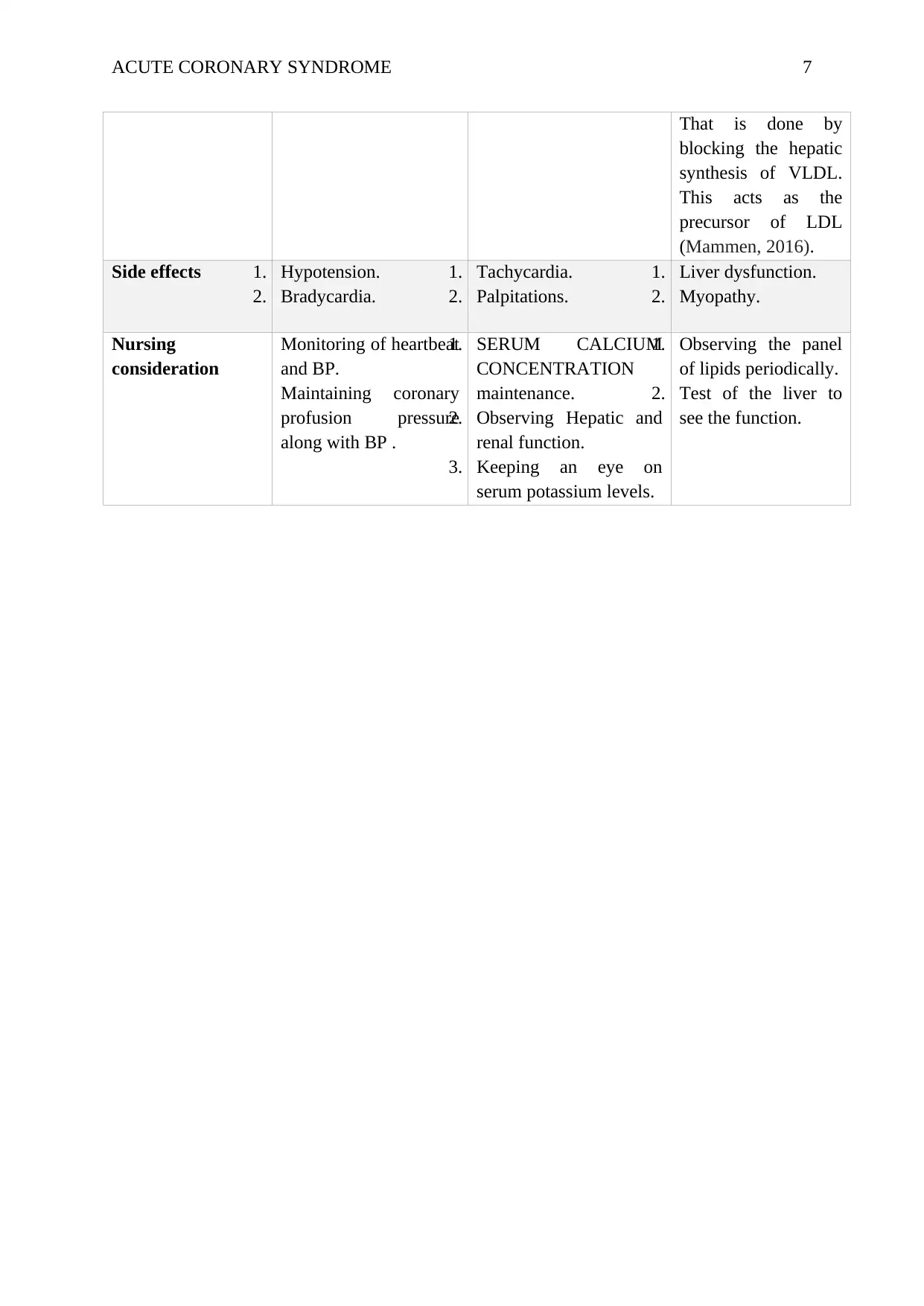
Side effects 1. Hypotension.
2. Bradycardia.
1. Tachycardia.
2. Palpitations.
1. Liver dysfunction.
2. Myopathy.
Nursing
consideration
Monitoring of heartbeat
and BP.
Maintaining coronary
profusion pressure
along with BP .
1. SERUM CALCIUM
CONCENTRATION
maintenance.
2. Observing Hepatic and
renal function.
3. Keeping an eye on
serum potassium levels.
1. Observing the panel
of lipids periodically.
2. Test of the liver to
see the function.
That is done by
blocking the hepatic
synthesis of VLDL.
This acts as the
precursor of LDL
(Mammen, 2016).
Side effects 1. Hypotension.
2. Bradycardia.
1. Tachycardia.
2. Palpitations.
1. Liver dysfunction.
2. Myopathy.
Nursing
consideration
Monitoring of heartbeat
and BP.
Maintaining coronary
profusion pressure
along with BP .
1. SERUM CALCIUM
CONCENTRATION
maintenance.
2. Observing Hepatic and
renal function.
3. Keeping an eye on
serum potassium levels.
1. Observing the panel
of lipids periodically.
2. Test of the liver to
see the function.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 8
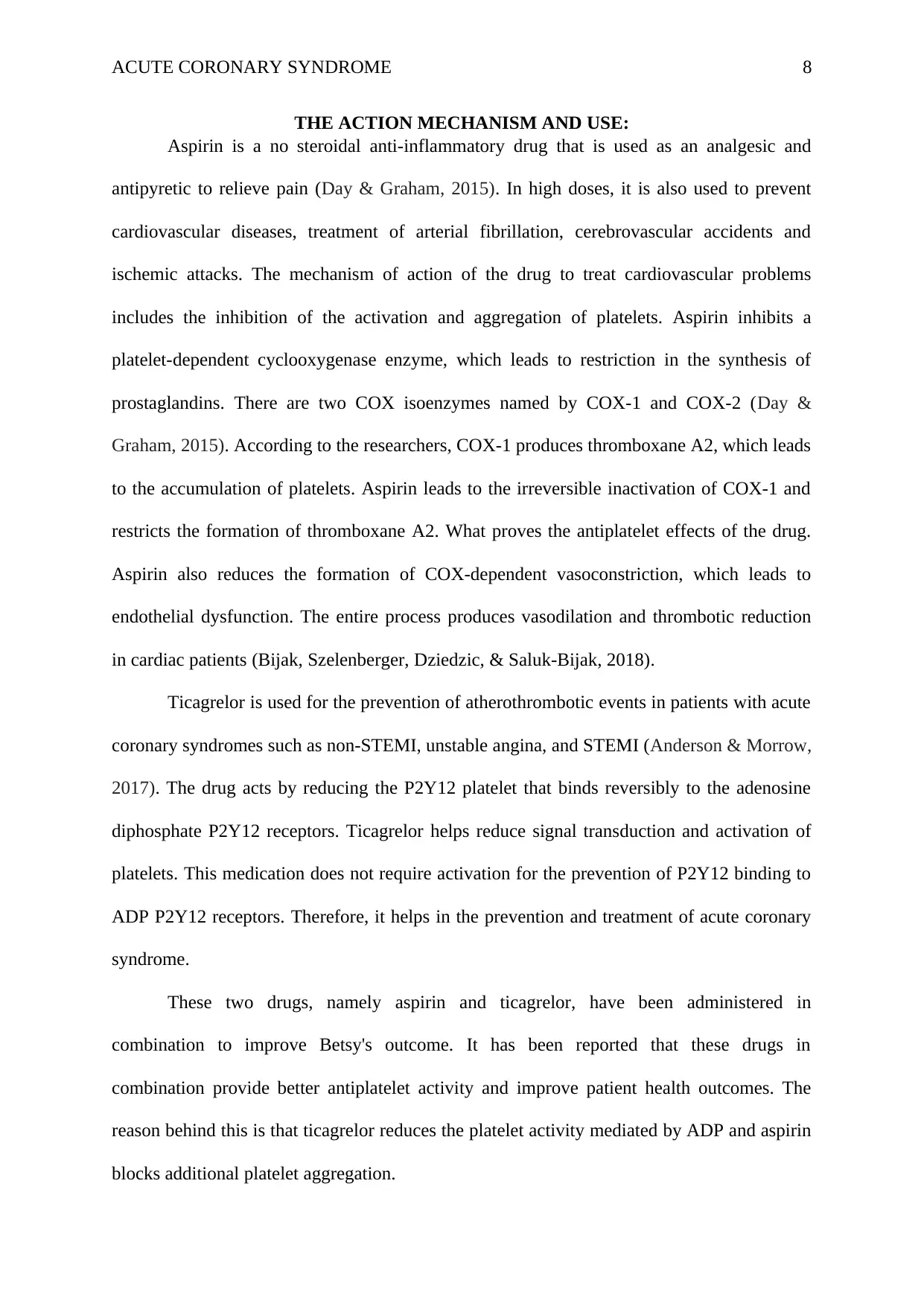
THE ACTION MECHANISM AND USE:
Aspirin is a no steroidal anti-inflammatory drug that is used as an analgesic and
antipyretic to relieve pain (Day & Graham, 2015). In high doses, it is also used to prevent
cardiovascular diseases, treatment of arterial fibrillation, cerebrovascular accidents and
ischemic attacks. The mechanism of action of the drug to treat cardiovascular problems
includes the inhibition of the activation and aggregation of platelets. Aspirin inhibits a
platelet-dependent cyclooxygenase enzyme, which leads to restriction in the synthesis of
prostaglandins. There are two COX isoenzymes named by COX-1 and COX-2 (Day &
Graham, 2015). According to the researchers, COX-1 produces thromboxane A2, which leads
to the accumulation of platelets. Aspirin leads to the irreversible inactivation of COX-1 and
restricts the formation of thromboxane A2. What proves the antiplatelet effects of the drug.
Aspirin also reduces the formation of COX-dependent vasoconstriction, which leads to
endothelial dysfunction. The entire process produces vasodilation and thrombotic reduction
in cardiac patients (Bijak, Szelenberger, Dziedzic, & Saluk-Bijak, 2018).
Ticagrelor is used for the prevention of atherothrombotic events in patients with acute
coronary syndromes such as non-STEMI, unstable angina, and STEMI (Anderson & Morrow,
2017). The drug acts by reducing the P2Y12 platelet that binds reversibly to the adenosine
diphosphate P2Y12 receptors. Ticagrelor helps reduce signal transduction and activation of
platelets. This medication does not require activation for the prevention of P2Y12 binding to
ADP P2Y12 receptors. Therefore, it helps in the prevention and treatment of acute coronary
syndrome.
These two drugs, namely aspirin and ticagrelor, have been administered in
combination to improve Betsy's outcome. It has been reported that these drugs in
combination provide better antiplatelet activity and improve patient health outcomes. The
reason behind this is that ticagrelor reduces the platelet activity mediated by ADP and aspirin
blocks additional platelet aggregation.
THE ACTION MECHANISM AND USE:
Aspirin is a no steroidal anti-inflammatory drug that is used as an analgesic and
antipyretic to relieve pain (Day & Graham, 2015). In high doses, it is also used to prevent
cardiovascular diseases, treatment of arterial fibrillation, cerebrovascular accidents and
ischemic attacks. The mechanism of action of the drug to treat cardiovascular problems
includes the inhibition of the activation and aggregation of platelets. Aspirin inhibits a
platelet-dependent cyclooxygenase enzyme, which leads to restriction in the synthesis of
prostaglandins. There are two COX isoenzymes named by COX-1 and COX-2 (Day &
Graham, 2015). According to the researchers, COX-1 produces thromboxane A2, which leads
to the accumulation of platelets. Aspirin leads to the irreversible inactivation of COX-1 and
restricts the formation of thromboxane A2. What proves the antiplatelet effects of the drug.
Aspirin also reduces the formation of COX-dependent vasoconstriction, which leads to
endothelial dysfunction. The entire process produces vasodilation and thrombotic reduction
in cardiac patients (Bijak, Szelenberger, Dziedzic, & Saluk-Bijak, 2018).
Ticagrelor is used for the prevention of atherothrombotic events in patients with acute
coronary syndromes such as non-STEMI, unstable angina, and STEMI (Anderson & Morrow,
2017). The drug acts by reducing the P2Y12 platelet that binds reversibly to the adenosine
diphosphate P2Y12 receptors. Ticagrelor helps reduce signal transduction and activation of
platelets. This medication does not require activation for the prevention of P2Y12 binding to
ADP P2Y12 receptors. Therefore, it helps in the prevention and treatment of acute coronary
syndrome.
These two drugs, namely aspirin and ticagrelor, have been administered in
combination to improve Betsy's outcome. It has been reported that these drugs in
combination provide better antiplatelet activity and improve patient health outcomes. The
reason behind this is that ticagrelor reduces the platelet activity mediated by ADP and aspirin
blocks additional platelet aggregation.
ACUTE CORONARY SYNDROME 9
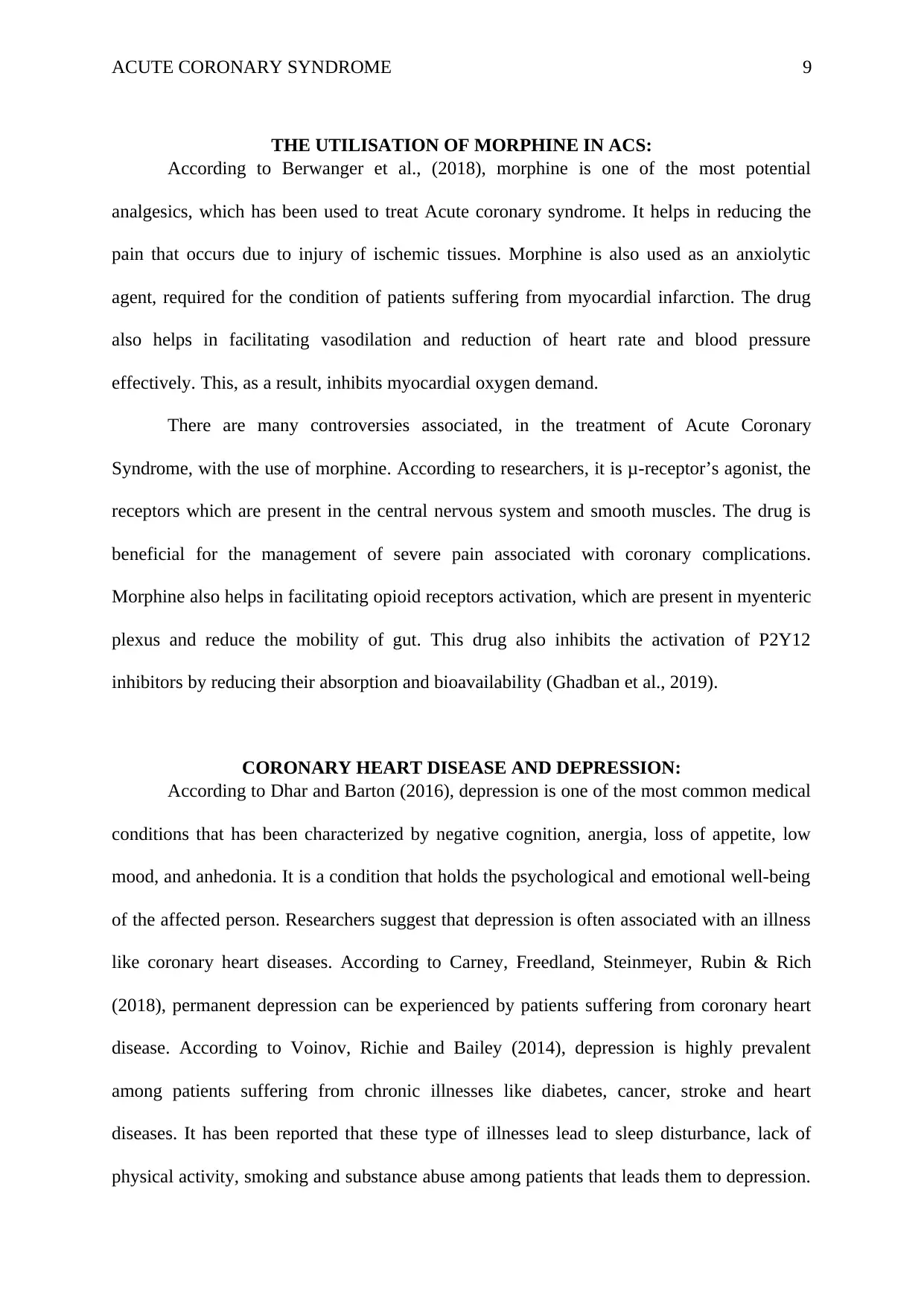
THE UTILISATION OF MORPHINE IN ACS:
According to Berwanger et al., (2018), morphine is one of the most potential
analgesics, which has been used to treat Acute coronary syndrome. It helps in reducing the
pain that occurs due to injury of ischemic tissues. Morphine is also used as an anxiolytic
agent, required for the condition of patients suffering from myocardial infarction. The drug
also helps in facilitating vasodilation and reduction of heart rate and blood pressure
effectively. This, as a result, inhibits myocardial oxygen demand.
There are many controversies associated, in the treatment of Acute Coronary
Syndrome, with the use of morphine. According to researchers, it is μ-receptor’s agonist, the
receptors which are present in the central nervous system and smooth muscles. The drug is
beneficial for the management of severe pain associated with coronary complications.
Morphine also helps in facilitating opioid receptors activation, which are present in myenteric
plexus and reduce the mobility of gut. This drug also inhibits the activation of P2Y12
inhibitors by reducing their absorption and bioavailability (Ghadban et al., 2019).
CORONARY HEART DISEASE AND DEPRESSION:
According to Dhar and Barton (2016), depression is one of the most common medical
conditions that has been characterized by negative cognition, anergia, loss of appetite, low
mood, and anhedonia. It is a condition that holds the psychological and emotional well-being
of the affected person. Researchers suggest that depression is often associated with an illness
like coronary heart diseases. According to Carney, Freedland, Steinmeyer, Rubin & Rich
(2018), permanent depression can be experienced by patients suffering from coronary heart
disease. According to Voinov, Richie and Bailey (2014), depression is highly prevalent
among patients suffering from chronic illnesses like diabetes, cancer, stroke and heart
diseases. It has been reported that these type of illnesses lead to sleep disturbance, lack of
physical activity, smoking and substance abuse among patients that leads them to depression.
THE UTILISATION OF MORPHINE IN ACS:
According to Berwanger et al., (2018), morphine is one of the most potential
analgesics, which has been used to treat Acute coronary syndrome. It helps in reducing the
pain that occurs due to injury of ischemic tissues. Morphine is also used as an anxiolytic
agent, required for the condition of patients suffering from myocardial infarction. The drug
also helps in facilitating vasodilation and reduction of heart rate and blood pressure
effectively. This, as a result, inhibits myocardial oxygen demand.
There are many controversies associated, in the treatment of Acute Coronary
Syndrome, with the use of morphine. According to researchers, it is μ-receptor’s agonist, the
receptors which are present in the central nervous system and smooth muscles. The drug is
beneficial for the management of severe pain associated with coronary complications.
Morphine also helps in facilitating opioid receptors activation, which are present in myenteric
plexus and reduce the mobility of gut. This drug also inhibits the activation of P2Y12
inhibitors by reducing their absorption and bioavailability (Ghadban et al., 2019).
CORONARY HEART DISEASE AND DEPRESSION:
According to Dhar and Barton (2016), depression is one of the most common medical
conditions that has been characterized by negative cognition, anergia, loss of appetite, low
mood, and anhedonia. It is a condition that holds the psychological and emotional well-being
of the affected person. Researchers suggest that depression is often associated with an illness
like coronary heart diseases. According to Carney, Freedland, Steinmeyer, Rubin & Rich
(2018), permanent depression can be experienced by patients suffering from coronary heart
disease. According to Voinov, Richie and Bailey (2014), depression is highly prevalent
among patients suffering from chronic illnesses like diabetes, cancer, stroke and heart
diseases. It has been reported that these type of illnesses lead to sleep disturbance, lack of
physical activity, smoking and substance abuse among patients that leads them to depression.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE CORONARY SYNDROME 10
The fear of loss of life and reduce the quality of life imparts depression in patients. This thing
can affect the lifestyle, mobility, freedom, professional, personal and social relations, leading
these patients to depression (Dhar & Barton, 2016).
CONCLUSION:
In the evaluation, the judicious of completing an ECG has been talked about it has
been discovered that it is useful in foreseeing future heart complication. The pathophysiology
of angina pectoris is inspected alongside the variations from the norm in ECG of a given
patient. Also, there is a concise exchange about the components which affirm the coronary
syndrome alongside the instrument of activity of different medications.
The fear of loss of life and reduce the quality of life imparts depression in patients. This thing
can affect the lifestyle, mobility, freedom, professional, personal and social relations, leading
these patients to depression (Dhar & Barton, 2016).
CONCLUSION:
In the evaluation, the judicious of completing an ECG has been talked about it has
been discovered that it is useful in foreseeing future heart complication. The pathophysiology
of angina pectoris is inspected alongside the variations from the norm in ECG of a given
patient. Also, there is a concise exchange about the components which affirm the coronary
syndrome alongside the instrument of activity of different medications.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 11
REFERENCES
Acharya, U. R., Fujita, H., Oh, S. L., Hagiwara, Y., Tan, J. H., & Adam, M. (2017).
Application of deep convolutional neural network for automated detection of
myocardial infarction using ECG signals. Information Sciences, Vol. 415, pp. 190-
198.
Anderson, J. L., & Morrow, D. A. (2017). Acute myocardial infarction. New England Journal
of Medicine, Vol. 376(21), pp. 2053-2064.
Batra, G., Svennblad, B., Held, C., Jernberg, T., Johanson, P., Wallentin, L., & Oldgren, J.
(2016). All types of atrial fibrillation in the setting of myocardial infarction are
associated with impaired outcome. Heart, Vol. 102(12), pp. 926-933.
Bentzon, J. F., Otsuka, F., Virmani, R., & Falk, E. (2015). Mechanisms of plaque formation
and rupture. Circulation research, Vol. 114(12), pp. 1852-1866.
Berwanger, O., Santucci, E. V., de Andrade Jesuíno, I., Damiani, L. P., Barbosa, L. M.,
Santos, R. H., & de Andrade, P. B. (2018). Effect of a loading dose of atorvastatin
before planned percutaneous coronary intervention on major adverse cardiovascular
events in acute coronary syndrome: the SECURE-PCI randomised clinical trial. Jama,
Vol. 319(13), pp. 1331-1340.
Bijak, M., Szelenberger, R., Dziedzic, A., & Saluk-Bijak, J. (2018). Inhibitory Effect of
Flavonolignans on the P2Y12 Pathway in Blood Platelets. Molecules, Vol. 23(2), pp.
374.
Carney, R. M., Freedland, K. E., Steinmeyer, B. C., Rubin, E. H., & Rich, M. W. (2018).
Residual symptoms after treatment for depression in patients with coronary heart
disease. Psychosomatic medicine, Vol. 80(4), pp. 385-392.
Day, R. O., & Graham, G. G. (2015). Non-steroidal anti-inflammatory drugs. Encyclopedia
of Inflammatory Diseases, pp. 1-9.
REFERENCES
Acharya, U. R., Fujita, H., Oh, S. L., Hagiwara, Y., Tan, J. H., & Adam, M. (2017).
Application of deep convolutional neural network for automated detection of
myocardial infarction using ECG signals. Information Sciences, Vol. 415, pp. 190-
198.
Anderson, J. L., & Morrow, D. A. (2017). Acute myocardial infarction. New England Journal
of Medicine, Vol. 376(21), pp. 2053-2064.
Batra, G., Svennblad, B., Held, C., Jernberg, T., Johanson, P., Wallentin, L., & Oldgren, J.
(2016). All types of atrial fibrillation in the setting of myocardial infarction are
associated with impaired outcome. Heart, Vol. 102(12), pp. 926-933.
Bentzon, J. F., Otsuka, F., Virmani, R., & Falk, E. (2015). Mechanisms of plaque formation
and rupture. Circulation research, Vol. 114(12), pp. 1852-1866.
Berwanger, O., Santucci, E. V., de Andrade Jesuíno, I., Damiani, L. P., Barbosa, L. M.,
Santos, R. H., & de Andrade, P. B. (2018). Effect of a loading dose of atorvastatin
before planned percutaneous coronary intervention on major adverse cardiovascular
events in acute coronary syndrome: the SECURE-PCI randomised clinical trial. Jama,
Vol. 319(13), pp. 1331-1340.
Bijak, M., Szelenberger, R., Dziedzic, A., & Saluk-Bijak, J. (2018). Inhibitory Effect of
Flavonolignans on the P2Y12 Pathway in Blood Platelets. Molecules, Vol. 23(2), pp.
374.
Carney, R. M., Freedland, K. E., Steinmeyer, B. C., Rubin, E. H., & Rich, M. W. (2018).
Residual symptoms after treatment for depression in patients with coronary heart
disease. Psychosomatic medicine, Vol. 80(4), pp. 385-392.
Day, R. O., & Graham, G. G. (2015). Non-steroidal anti-inflammatory drugs. Encyclopedia
of Inflammatory Diseases, pp. 1-9.
ACUTE CORONARY SYNDROME 12
Dhar, A. K., & Barton, D. A. (2016). Depression and the link with cardiovascular
disease. Frontiers in psychiatry, Vol. 7, pp. 33.
Ghadban, R., Enezate, T., Payne, J., Allaham, H., Halawa, A., Fong, H. K., ... & Aggarwal,
K. (2019). The safety of morphine use in acute coronary syndrome: a meta-
analysis. Heart Asia, Vol. 11(1), e011142.
Jia, G., Hill, M. A., & Sowers, J. R. (2018). Diabetic cardiomyopathy: an update of
mechanisms contributing to this clinical entity. Circulation research, Vol. 122(4), pp.
624-638.
Lu, L., Rao, X., Cong, R., Zhang, C., Wang, Z., Xu, J., & Xie, W. (2019). Design, Synthesis
and Biological Evaluation of Nitrate Derivatives of Sauropunol A and B as Potent
Vasodilatory Agents. Molecules, Vol. 24(3), pp. 583.
Mammen, A. L. (2016). Statin-associated autoimmune myopathy. New England Journal of
Medicine, Vol. 374(7), pp. 664-669.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, Vol. 4(13).
Singh, A., Laribi, S., Teerlink, J. R., & Mebazaa, A. (2016). Agents with vasodilator
properties in acute heart failure. European heart journal, Vol. 38(5), pp. 317-325.
Snutch, T. P., & Zamponi, G. W. (2018). Recent advances in the development of T‐type
calcium channel blockers for pain intervention. British journal of pharmacology, Vol.
175(12), pp. 2375-2383.
Rawat, D., & Sharma, S. (2018). Case Study: 60-Year-Old Female Presenting With Shortness
of Breath. n StatPearls [Internet]. StatPearls Publishing.
Voinov, B., Richie, W. D., & Bailey, R. K. (2014). Depression and chronic diseases: it is
time for a synergistic mental health and primary care approach. The primary care
Dhar, A. K., & Barton, D. A. (2016). Depression and the link with cardiovascular
disease. Frontiers in psychiatry, Vol. 7, pp. 33.
Ghadban, R., Enezate, T., Payne, J., Allaham, H., Halawa, A., Fong, H. K., ... & Aggarwal,
K. (2019). The safety of morphine use in acute coronary syndrome: a meta-
analysis. Heart Asia, Vol. 11(1), e011142.
Jia, G., Hill, M. A., & Sowers, J. R. (2018). Diabetic cardiomyopathy: an update of
mechanisms contributing to this clinical entity. Circulation research, Vol. 122(4), pp.
624-638.
Lu, L., Rao, X., Cong, R., Zhang, C., Wang, Z., Xu, J., & Xie, W. (2019). Design, Synthesis
and Biological Evaluation of Nitrate Derivatives of Sauropunol A and B as Potent
Vasodilatory Agents. Molecules, Vol. 24(3), pp. 583.
Mammen, A. L. (2016). Statin-associated autoimmune myopathy. New England Journal of
Medicine, Vol. 374(7), pp. 664-669.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, Vol. 4(13).
Singh, A., Laribi, S., Teerlink, J. R., & Mebazaa, A. (2016). Agents with vasodilator
properties in acute heart failure. European heart journal, Vol. 38(5), pp. 317-325.
Snutch, T. P., & Zamponi, G. W. (2018). Recent advances in the development of T‐type
calcium channel blockers for pain intervention. British journal of pharmacology, Vol.
175(12), pp. 2375-2383.
Rawat, D., & Sharma, S. (2018). Case Study: 60-Year-Old Female Presenting With Shortness
of Breath. n StatPearls [Internet]. StatPearls Publishing.
Voinov, B., Richie, W. D., & Bailey, R. K. (2014). Depression and chronic diseases: it is
time for a synergistic mental health and primary care approach. The primary care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





