HLTENN011: Implement and Monitor Care for Acute Health Issues
VerifiedAdded on 2022/12/27
|14
|3880
|29
Homework Assignment
AI Summary
This assignment, addressing the unit HLTENN011, delves into the multifaceted realm of acute health problems and the corresponding nursing care strategies. It begins by defining various acute conditions, such as kidney failure, angina, and fractures, detailing their clinical manifestations. The assignment then explores key differences between conditions like deep vein thrombosis and venous thromboembolism, as well as greenstick and impacted fractures. Surgical nursing principles, anaesthesia types, and surgical interventions are discussed, including open reduction, amputation, and hysterectomy. The document further covers critical aspects of monitoring and managing patients with intravenous infusions, CPAP, BiPAP, and nasogastric tubes. Furthermore, it addresses complications of acute bed rest, holistic approaches to angina care, and first aid procedures for unconscious patients. Finally, it outlines situations necessitating a Code Blue in an acute healthcare setting, providing a comprehensive guide to acute healthcare practices.
HLTENN011 Implement and
monitor care for a person
with acute health problems
monitor care for a person
with acute health problems
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
PART A ..........................................................................................................................................3
PART B .........................................................................................................................................11
REFERENCES .............................................................................................................................13
PART A ..........................................................................................................................................3
PART B .........................................................................................................................................11
REFERENCES .............................................................................................................................13
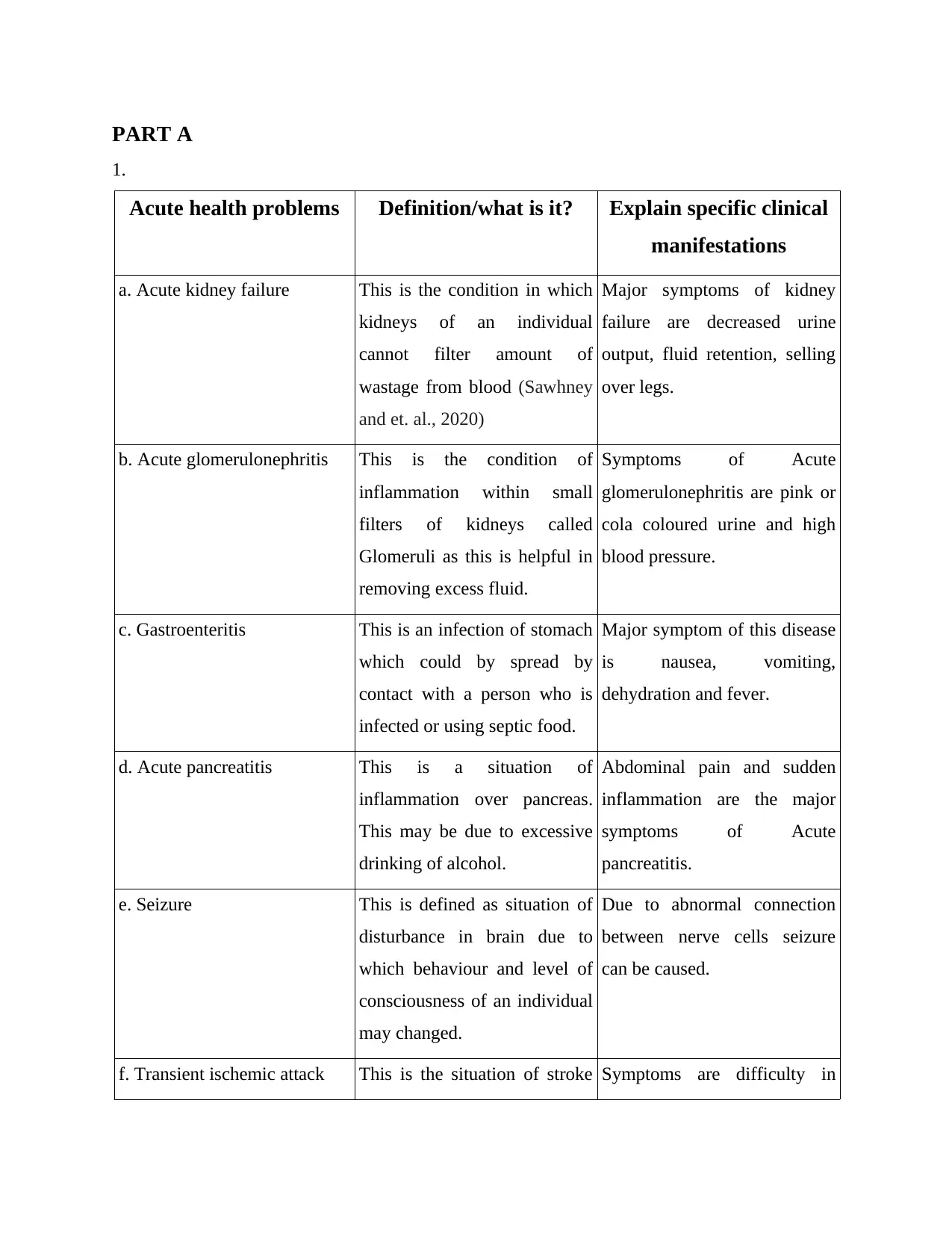
PART A
1.
Acute health problems Definition/what is it? Explain specific clinical
manifestations
a. Acute kidney failure This is the condition in which
kidneys of an individual
cannot filter amount of
wastage from blood (Sawhney
and et. al., 2020)
Major symptoms of kidney
failure are decreased urine
output, fluid retention, selling
over legs.
b. Acute glomerulonephritis This is the condition of
inflammation within small
filters of kidneys called
Glomeruli as this is helpful in
removing excess fluid.
Symptoms of Acute
glomerulonephritis are pink or
cola coloured urine and high
blood pressure.
c. Gastroenteritis This is an infection of stomach
which could by spread by
contact with a person who is
infected or using septic food.
Major symptom of this disease
is nausea, vomiting,
dehydration and fever.
d. Acute pancreatitis This is a situation of
inflammation over pancreas.
This may be due to excessive
drinking of alcohol.
Abdominal pain and sudden
inflammation are the major
symptoms of Acute
pancreatitis.
e. Seizure This is defined as situation of
disturbance in brain due to
which behaviour and level of
consciousness of an individual
may changed.
Due to abnormal connection
between nerve cells seizure
can be caused.
f. Transient ischemic attack This is the situation of stroke Symptoms are difficulty in
1.
Acute health problems Definition/what is it? Explain specific clinical
manifestations
a. Acute kidney failure This is the condition in which
kidneys of an individual
cannot filter amount of
wastage from blood (Sawhney
and et. al., 2020)
Major symptoms of kidney
failure are decreased urine
output, fluid retention, selling
over legs.
b. Acute glomerulonephritis This is the condition of
inflammation within small
filters of kidneys called
Glomeruli as this is helpful in
removing excess fluid.
Symptoms of Acute
glomerulonephritis are pink or
cola coloured urine and high
blood pressure.
c. Gastroenteritis This is an infection of stomach
which could by spread by
contact with a person who is
infected or using septic food.
Major symptom of this disease
is nausea, vomiting,
dehydration and fever.
d. Acute pancreatitis This is a situation of
inflammation over pancreas.
This may be due to excessive
drinking of alcohol.
Abdominal pain and sudden
inflammation are the major
symptoms of Acute
pancreatitis.
e. Seizure This is defined as situation of
disturbance in brain due to
which behaviour and level of
consciousness of an individual
may changed.
Due to abnormal connection
between nerve cells seizure
can be caused.
f. Transient ischemic attack This is the situation of stroke Symptoms are difficulty in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
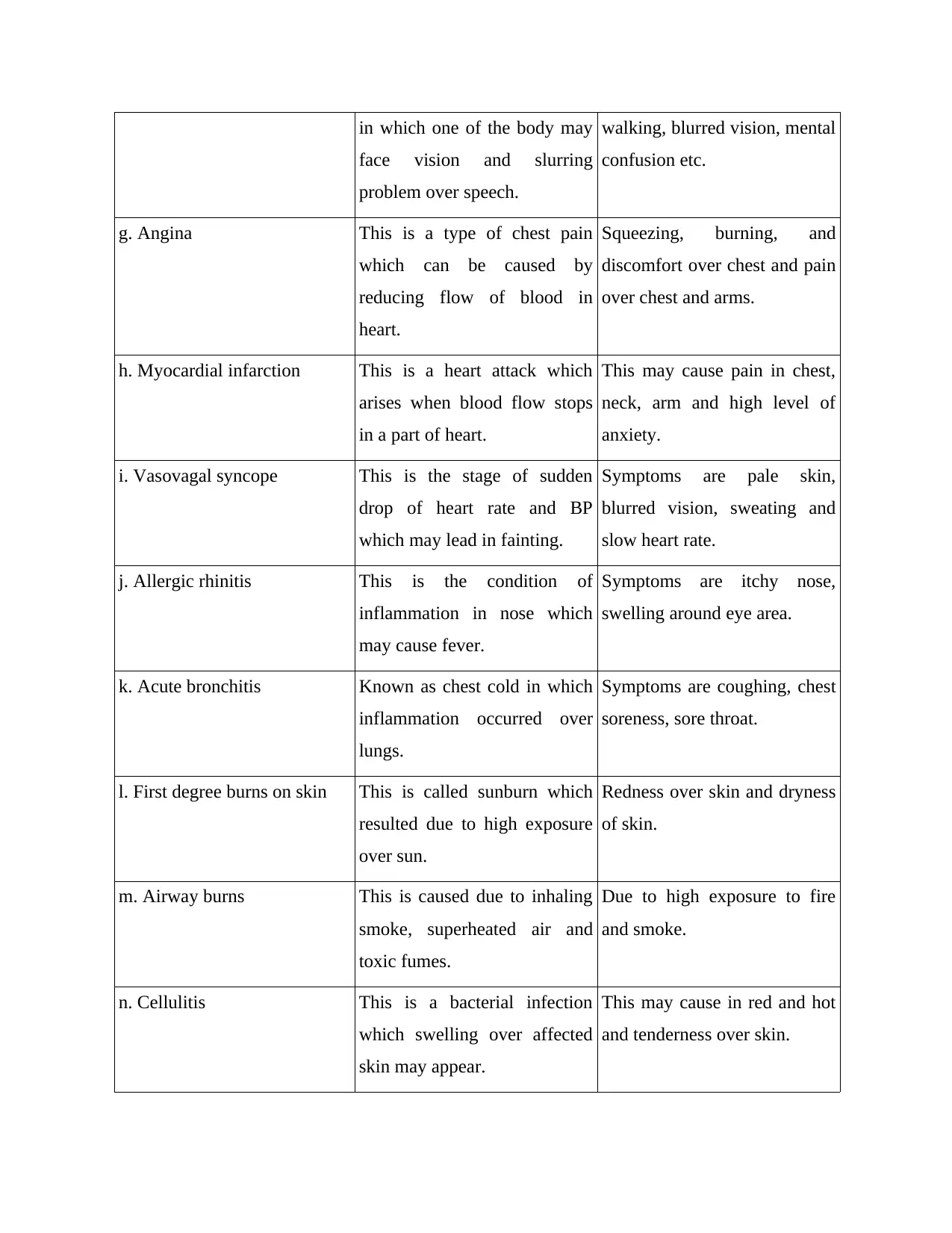
in which one of the body may
face vision and slurring
problem over speech.
walking, blurred vision, mental
confusion etc.
g. Angina This is a type of chest pain
which can be caused by
reducing flow of blood in
heart.
Squeezing, burning, and
discomfort over chest and pain
over chest and arms.
h. Myocardial infarction This is a heart attack which
arises when blood flow stops
in a part of heart.
This may cause pain in chest,
neck, arm and high level of
anxiety.
i. Vasovagal syncope This is the stage of sudden
drop of heart rate and BP
which may lead in fainting.
Symptoms are pale skin,
blurred vision, sweating and
slow heart rate.
j. Allergic rhinitis This is the condition of
inflammation in nose which
may cause fever.
Symptoms are itchy nose,
swelling around eye area.
k. Acute bronchitis Known as chest cold in which
inflammation occurred over
lungs.
Symptoms are coughing, chest
soreness, sore throat.
l. First degree burns on skin This is called sunburn which
resulted due to high exposure
over sun.
Redness over skin and dryness
of skin.
m. Airway burns This is caused due to inhaling
smoke, superheated air and
toxic fumes.
Due to high exposure to fire
and smoke.
n. Cellulitis This is a bacterial infection
which swelling over affected
skin may appear.
This may cause in red and hot
and tenderness over skin.
face vision and slurring
problem over speech.
walking, blurred vision, mental
confusion etc.
g. Angina This is a type of chest pain
which can be caused by
reducing flow of blood in
heart.
Squeezing, burning, and
discomfort over chest and pain
over chest and arms.
h. Myocardial infarction This is a heart attack which
arises when blood flow stops
in a part of heart.
This may cause pain in chest,
neck, arm and high level of
anxiety.
i. Vasovagal syncope This is the stage of sudden
drop of heart rate and BP
which may lead in fainting.
Symptoms are pale skin,
blurred vision, sweating and
slow heart rate.
j. Allergic rhinitis This is the condition of
inflammation in nose which
may cause fever.
Symptoms are itchy nose,
swelling around eye area.
k. Acute bronchitis Known as chest cold in which
inflammation occurred over
lungs.
Symptoms are coughing, chest
soreness, sore throat.
l. First degree burns on skin This is called sunburn which
resulted due to high exposure
over sun.
Redness over skin and dryness
of skin.
m. Airway burns This is caused due to inhaling
smoke, superheated air and
toxic fumes.
Due to high exposure to fire
and smoke.
n. Cellulitis This is a bacterial infection
which swelling over affected
skin may appear.
This may cause in red and hot
and tenderness over skin.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
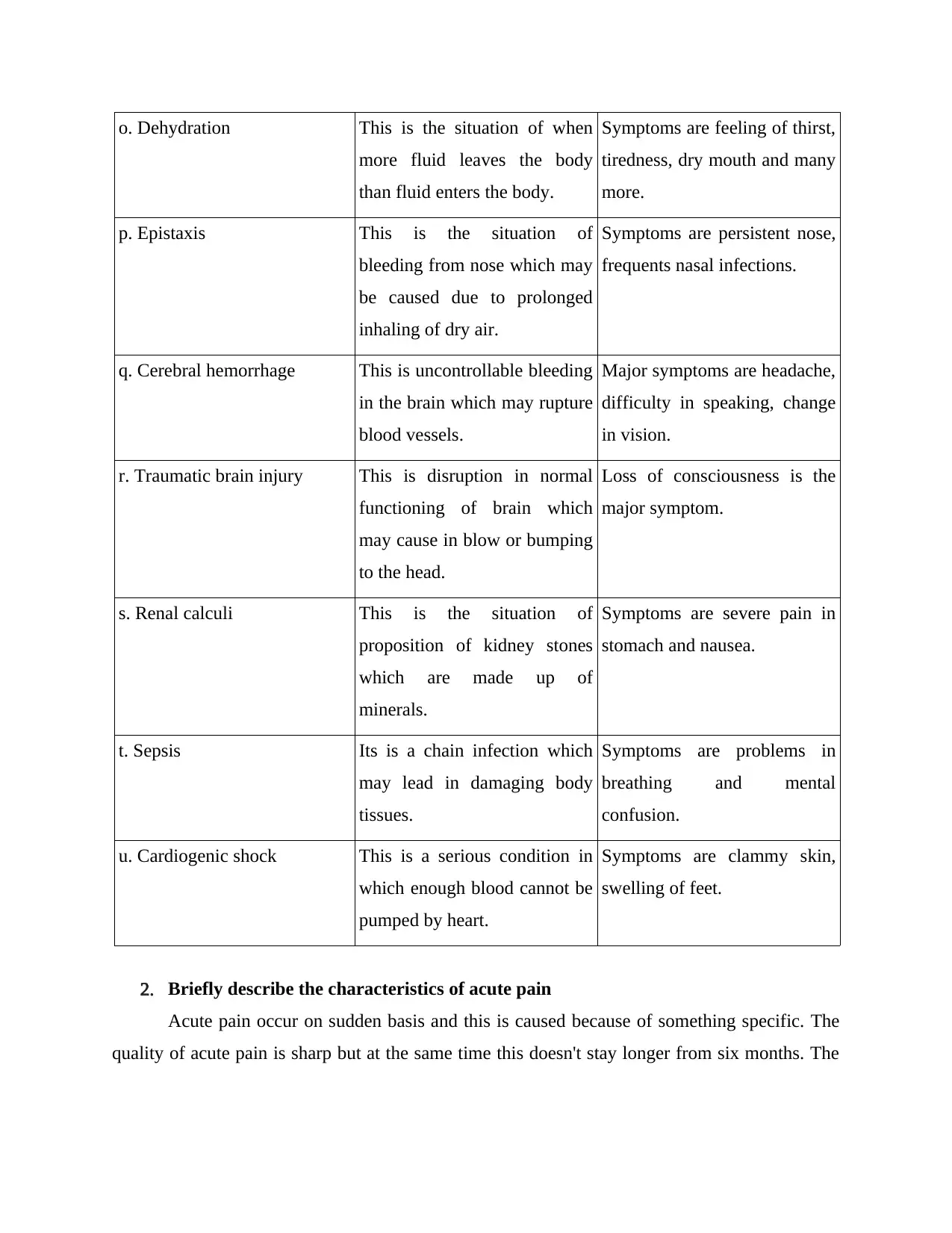
o. Dehydration This is the situation of when
more fluid leaves the body
than fluid enters the body.
Symptoms are feeling of thirst,
tiredness, dry mouth and many
more.
p. Epistaxis This is the situation of
bleeding from nose which may
be caused due to prolonged
inhaling of dry air.
Symptoms are persistent nose,
frequents nasal infections.
q. Cerebral hemorrhage This is uncontrollable bleeding
in the brain which may rupture
blood vessels.
Major symptoms are headache,
difficulty in speaking, change
in vision.
r. Traumatic brain injury This is disruption in normal
functioning of brain which
may cause in blow or bumping
to the head.
Loss of consciousness is the
major symptom.
s. Renal calculi This is the situation of
proposition of kidney stones
which are made up of
minerals.
Symptoms are severe pain in
stomach and nausea.
t. Sepsis Its is a chain infection which
may lead in damaging body
tissues.
Symptoms are problems in
breathing and mental
confusion.
u. Cardiogenic shock This is a serious condition in
which enough blood cannot be
pumped by heart.
Symptoms are clammy skin,
swelling of feet.
2. Briefly describe the characteristics of acute pain
Acute pain occur on sudden basis and this is caused because of something specific. The
quality of acute pain is sharp but at the same time this doesn't stay longer from six months. The
more fluid leaves the body
than fluid enters the body.
Symptoms are feeling of thirst,
tiredness, dry mouth and many
more.
p. Epistaxis This is the situation of
bleeding from nose which may
be caused due to prolonged
inhaling of dry air.
Symptoms are persistent nose,
frequents nasal infections.
q. Cerebral hemorrhage This is uncontrollable bleeding
in the brain which may rupture
blood vessels.
Major symptoms are headache,
difficulty in speaking, change
in vision.
r. Traumatic brain injury This is disruption in normal
functioning of brain which
may cause in blow or bumping
to the head.
Loss of consciousness is the
major symptom.
s. Renal calculi This is the situation of
proposition of kidney stones
which are made up of
minerals.
Symptoms are severe pain in
stomach and nausea.
t. Sepsis Its is a chain infection which
may lead in damaging body
tissues.
Symptoms are problems in
breathing and mental
confusion.
u. Cardiogenic shock This is a serious condition in
which enough blood cannot be
pumped by heart.
Symptoms are clammy skin,
swelling of feet.
2. Briefly describe the characteristics of acute pain
Acute pain occur on sudden basis and this is caused because of something specific. The
quality of acute pain is sharp but at the same time this doesn't stay longer from six months. The
example of acute pain can be infection, burning or broken bone (Griffioen and et. al., 2017).
Acute pain may cause due to damaging of tissues which may cause inflammation over skin.
3. Briefly describe the key difference between deep vein thrombosis and venous
thromboembolism.
Deep vein thrombosis is defined as blood clotting in deep veins whereas venous
thromboembolism is the term in which health care team is referring to Deep vein thrombosis.
DVT is the situation in which veins that can carry blood away from arms and legs. These are
associated with those veins which are carrying blood away from brain, neck and liver (Othieno,
Okpo and Forster, 2018). Besides this venous thromboembolism is the medical term of Deep
vein thrombosis.
4. Briefly describe four (4) common symptoms of a bone fracture.
The major symptom of bone fracture are
Swelling over the bone which is causing fracture
Inability to bear weight over affected area and pain get worse when affected area is
moved (Taylor and et. al, 2016).
People loose functioning over affected are visibility regarding out of the place over joint
of affected limb
5. Briefly describe the key difference between greenstick and impacted fractures
A greenstick fracture is occurring due to bending or cracking over bone in which bone
gets completely separated into pieces. Greenstick fracture may be faced by an individual during
childhood of 10 years of younger (Xu and et. al., 2018). As bones of children are softer and
flexible and at the same time this fracture can be healed in a very short span of time.
Impacted fracture is a complete fracture in which line of fracture is blurry. This is
resultant due to compression of cancellous bone and when two bones are jammed together. This
kind of fracture takes time to get cure.
6. Discuss three (3) key principles of surgical nursing.
Managing fluid and balance of electrolyte as surgery may cause loss of blood and other
fluid so this is imperative that balance between water and electrolytes should be
maintained (DeWit, Stromberg and Dallred, 2016).
Emotional support is the another principle which is followed by surgical nursing in order
to communicate and coordinate with patients.
Acute pain may cause due to damaging of tissues which may cause inflammation over skin.
3. Briefly describe the key difference between deep vein thrombosis and venous
thromboembolism.
Deep vein thrombosis is defined as blood clotting in deep veins whereas venous
thromboembolism is the term in which health care team is referring to Deep vein thrombosis.
DVT is the situation in which veins that can carry blood away from arms and legs. These are
associated with those veins which are carrying blood away from brain, neck and liver (Othieno,
Okpo and Forster, 2018). Besides this venous thromboembolism is the medical term of Deep
vein thrombosis.
4. Briefly describe four (4) common symptoms of a bone fracture.
The major symptom of bone fracture are
Swelling over the bone which is causing fracture
Inability to bear weight over affected area and pain get worse when affected area is
moved (Taylor and et. al, 2016).
People loose functioning over affected are visibility regarding out of the place over joint
of affected limb
5. Briefly describe the key difference between greenstick and impacted fractures
A greenstick fracture is occurring due to bending or cracking over bone in which bone
gets completely separated into pieces. Greenstick fracture may be faced by an individual during
childhood of 10 years of younger (Xu and et. al., 2018). As bones of children are softer and
flexible and at the same time this fracture can be healed in a very short span of time.
Impacted fracture is a complete fracture in which line of fracture is blurry. This is
resultant due to compression of cancellous bone and when two bones are jammed together. This
kind of fracture takes time to get cure.
6. Discuss three (3) key principles of surgical nursing.
Managing fluid and balance of electrolyte as surgery may cause loss of blood and other
fluid so this is imperative that balance between water and electrolytes should be
maintained (DeWit, Stromberg and Dallred, 2016).
Emotional support is the another principle which is followed by surgical nursing in order
to communicate and coordinate with patients.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Assessing planning, implementing and evaluation are the another principle which is
essential for surgical nursing so that to fill gap between treatment and patient problem.
7. Briefly describe the key difference between elective surgery and emergency surgery.
Elective surgery is scheduled in advance due to which patient can schedule the same as
according to their convenience (Howard and et. al., 2019). Besides this emergency surgery in
which patient has to deal with acute threat of life which may create complications to their life.
8. Briefly describe the key difference between general, local and epidural anaesthesia.
General anaesthesia is the combination of medications which are used before a surgery
and this do not cause complete unconsciousness to patient. On the other hand local anaesthesia is
an one time injection which numbs small area of the body and used by medical team to treat
broken bone or deep cut (Horn and et. al., 2016). Whereas epidural anaesthesia is defined as the
method of medication which is injected into epidural space around the spinal cord.
9. Briefly describe the key difference between spinal anaesthesia and peripheral nerve
block.
Spinal anaesthesia is a form of regional anaesthesia which involves injection of local
anaesthesia through a fine needle. Whereas peripheral nerve block is the type of regional
anaesthesia which is injected near a specific nerve or bundle of nerve. Nerve blocks are lasting
longer than local anaesthesia (Hunter and et. al., 2019).
10. Define the following surgical interventions and briefly describe the surgical
procedures involved in each of them.
a. Open reduction
This is a surgery to fix severely broken bones in which orthopedic surgeons reposition
bone pieces during surgery (Gonzalez and et. al., 2016).
b. Amputation
This is the situation of general anaesthesia in which body from waist and down get
numbed.
c. Total hip replacement
Under this the damaged bone and cartilage is removed and replaced with prosthetic
components. The damaged femoral head is removed and replaced with a metal stem that is
placed into the hollow centre of the femur.
d. Craniotomy
essential for surgical nursing so that to fill gap between treatment and patient problem.
7. Briefly describe the key difference between elective surgery and emergency surgery.
Elective surgery is scheduled in advance due to which patient can schedule the same as
according to their convenience (Howard and et. al., 2019). Besides this emergency surgery in
which patient has to deal with acute threat of life which may create complications to their life.
8. Briefly describe the key difference between general, local and epidural anaesthesia.
General anaesthesia is the combination of medications which are used before a surgery
and this do not cause complete unconsciousness to patient. On the other hand local anaesthesia is
an one time injection which numbs small area of the body and used by medical team to treat
broken bone or deep cut (Horn and et. al., 2016). Whereas epidural anaesthesia is defined as the
method of medication which is injected into epidural space around the spinal cord.
9. Briefly describe the key difference between spinal anaesthesia and peripheral nerve
block.
Spinal anaesthesia is a form of regional anaesthesia which involves injection of local
anaesthesia through a fine needle. Whereas peripheral nerve block is the type of regional
anaesthesia which is injected near a specific nerve or bundle of nerve. Nerve blocks are lasting
longer than local anaesthesia (Hunter and et. al., 2019).
10. Define the following surgical interventions and briefly describe the surgical
procedures involved in each of them.
a. Open reduction
This is a surgery to fix severely broken bones in which orthopedic surgeons reposition
bone pieces during surgery (Gonzalez and et. al., 2016).
b. Amputation
This is the situation of general anaesthesia in which body from waist and down get
numbed.
c. Total hip replacement
Under this the damaged bone and cartilage is removed and replaced with prosthetic
components. The damaged femoral head is removed and replaced with a metal stem that is
placed into the hollow centre of the femur.
d. Craniotomy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
It is surgical removal of part of bone from skull and specialised tools are used to remove
the section from bone flap and it get replaced after the surgery get over.
e. Tonsillectomy
This is defined as surgical removal of tonsils which is performed over children and gives
mild pain to patients.
f. Appendectomy
This is the surgical method of removing of appendix which is performed in order to deal
with appendicitis.
h. Hysterectomy
This is known as the operation for removing of uterus by incision in lower abdomen of
patient.
i. Prostatectomy
This is the surgical condition to remove prostate in which a combined visual and surgical
equipment is inserted through urethra.
j. Cataract extraction
This is an eye surgery required when lenses of eyes become cloudy and get replaced with
some an artificial lenses.
11. Briefly describe the characteristics of internal abdominal bleeding due to trauma
and its management.
Characteristics:
dizziness
severe abdominal pain
vomiting (Araki, Yokota and Morita, 2016)
low blood pressure
Management
In order to treat this treatment and rest is required by patient. On the other hand in some serious
conditions operation can also be executed.
12. Outline five (5) key considerations when monitoring and managing a person on
intravenous infusion via peripherally inserted central catheter
(PICC)/midline/central venous catheter (CVC).
Using infection prevention strategies
the section from bone flap and it get replaced after the surgery get over.
e. Tonsillectomy
This is defined as surgical removal of tonsils which is performed over children and gives
mild pain to patients.
f. Appendectomy
This is the surgical method of removing of appendix which is performed in order to deal
with appendicitis.
h. Hysterectomy
This is known as the operation for removing of uterus by incision in lower abdomen of
patient.
i. Prostatectomy
This is the surgical condition to remove prostate in which a combined visual and surgical
equipment is inserted through urethra.
j. Cataract extraction
This is an eye surgery required when lenses of eyes become cloudy and get replaced with
some an artificial lenses.
11. Briefly describe the characteristics of internal abdominal bleeding due to trauma
and its management.
Characteristics:
dizziness
severe abdominal pain
vomiting (Araki, Yokota and Morita, 2016)
low blood pressure
Management
In order to treat this treatment and rest is required by patient. On the other hand in some serious
conditions operation can also be executed.
12. Outline five (5) key considerations when monitoring and managing a person on
intravenous infusion via peripherally inserted central catheter
(PICC)/midline/central venous catheter (CVC).
Using infection prevention strategies
PICCs should be inserted in an area where asepsis can be maintained
The catheter tip position should be confirmed by a modified chest x-ray study
prior to use
using of alcohol containing skin preparatory
using sterilised equipments
Clinicians should not palpate the insertion site after the application of antiseptic,
unless aseptic technique is maintained (Shanja-Grabarz and et. al., 2020)
13. Outline five (5) key considerations when monitoring and managing a person on
continuous positive airway pressure (CPAP).
Level of consciousness
measuring pulse through oximeter
respiratory system management with the help of bi-level ventilation
Measuring heart rate
Confirm the CPAP device is correctly set up and is functional on the desired pressure
(McEvoy and et. al., 2016)
14. Outline five (5) key considerations when monitoring and managing a person on
Bilevel positive airway pressure (BiPAP).
Common initial inspiratory positive airway pressure (IPAP) is 10 cm H20 (larger patients
may need 15 cm H20)
patient should be awake
not facing any seizures
protect all their airways (Cimino and et. al., 2020)
not in vomiting condition
15. Outline five (5) key considerations when assisting a person with fluid intake via
nasogastric tube.
Facial and eye protection
providing oral and skin care
verifying NG tube placements
encouraging mouth breathing
lie patient complete flat (Brumbaugh and et. al., 2018)
wearing gloves to manage hygiene
The catheter tip position should be confirmed by a modified chest x-ray study
prior to use
using of alcohol containing skin preparatory
using sterilised equipments
Clinicians should not palpate the insertion site after the application of antiseptic,
unless aseptic technique is maintained (Shanja-Grabarz and et. al., 2020)
13. Outline five (5) key considerations when monitoring and managing a person on
continuous positive airway pressure (CPAP).
Level of consciousness
measuring pulse through oximeter
respiratory system management with the help of bi-level ventilation
Measuring heart rate
Confirm the CPAP device is correctly set up and is functional on the desired pressure
(McEvoy and et. al., 2016)
14. Outline five (5) key considerations when monitoring and managing a person on
Bilevel positive airway pressure (BiPAP).
Common initial inspiratory positive airway pressure (IPAP) is 10 cm H20 (larger patients
may need 15 cm H20)
patient should be awake
not facing any seizures
protect all their airways (Cimino and et. al., 2020)
not in vomiting condition
15. Outline five (5) key considerations when assisting a person with fluid intake via
nasogastric tube.
Facial and eye protection
providing oral and skin care
verifying NG tube placements
encouraging mouth breathing
lie patient complete flat (Brumbaugh and et. al., 2018)
wearing gloves to manage hygiene
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
16. Discuss four (4) complications of acute bed rest during post-operative period
constipation
weakness
deceased tolerance of carbohydrate
negative level of nitrogen (Thomazeau and et. al., 2016)
17. Discuss the holistic approach to care of a person admitted in an acute ward with
angina. Include in your response what specific nursing interventions should be
provided and what is the expected outcome of these nursing interventions.
Oxygen therapy
Pharmacologic Therapy
Interventions
Reducing anxiety
prevention of pain
decreasing demand of oxygen (Nilsson, Edvardsson and Rushton, 2019)
18. If you find a patient unconscious on the floor, what first aid procedures should you
follow?
Open airways
give rescue breathing (Grof, 2016)
alternating 30 compressions with rescue breaths
19. Discuss the situations in which a Code Blue will be initiated in an acute healthcare
setting.
During situation of cardiopulmonary arrest and needs resuscitation in which initial efforts
are placed by nurses (Spitzer and et. al., 2019). In this first responder will call for help and
second respondent will bring e-cart, third respondent will turn on AED, fourth respondent will
try to arrange medication and at last fifth respondent is keeping documentation.
20. Discuss the general pre-operative and immediate post-operative nursing
management of a person. Include in your response post-anaesthetic and post-
operative observations a nurse must perform.
During pre-operative period intense care is required as in this patient is prepared for the surgery.
Besides this during post-operative period healthcare provider is required to provide appropriate
constipation
weakness
deceased tolerance of carbohydrate
negative level of nitrogen (Thomazeau and et. al., 2016)
17. Discuss the holistic approach to care of a person admitted in an acute ward with
angina. Include in your response what specific nursing interventions should be
provided and what is the expected outcome of these nursing interventions.
Oxygen therapy
Pharmacologic Therapy
Interventions
Reducing anxiety
prevention of pain
decreasing demand of oxygen (Nilsson, Edvardsson and Rushton, 2019)
18. If you find a patient unconscious on the floor, what first aid procedures should you
follow?
Open airways
give rescue breathing (Grof, 2016)
alternating 30 compressions with rescue breaths
19. Discuss the situations in which a Code Blue will be initiated in an acute healthcare
setting.
During situation of cardiopulmonary arrest and needs resuscitation in which initial efforts
are placed by nurses (Spitzer and et. al., 2019). In this first responder will call for help and
second respondent will bring e-cart, third respondent will turn on AED, fourth respondent will
try to arrange medication and at last fifth respondent is keeping documentation.
20. Discuss the general pre-operative and immediate post-operative nursing
management of a person. Include in your response post-anaesthetic and post-
operative observations a nurse must perform.
During pre-operative period intense care is required as in this patient is prepared for the surgery.
Besides this during post-operative period healthcare provider is required to provide appropriate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
care to the patient (Harvey and Kovalesky, 2018). During post operative period sometimes
shivering may cause to individual which is a critical situation.
21. Discuss the post-operative pain management strategies a nurse could implement.
Pain assessment starts at the time of admission and should include an assessment of the patient’s
activities of daily living (ADL) and pain and stress coping skills (Jayakumar and et. al., 2019).
Post operative pain management strategies are aimed at minimising pains of patient and
minimise their discomfort. Holistic approaches are being followed by nurses dealing with post-
operative pain.
22. Explain risk assessment of a patient’s stability on their feet before assisting them
with ambulation during the immediate post-operative period
Person sitting for a longer period of time may face vertigo and in this condition patient should sit
with legs dangling. Process of patient handling is elaborated as under:
Checking of order of physician
Assessment of patient's muscle strength and activity tolerance
Assessment of patient's risk (Carantini and et. al., 2020)
Using assistive devices so that to provide ultimate care to patient.
23. Outline the steps involved in performing tracheostomy suctioning under the
headings:
• Prepare the person and the environment: Under this step the person who is treated will be
prepared as according to the environment so that treatment can be initiated.
• Perform tracheostomy suctioning: Under this step suction of catheter tip into clean water so
that residual can be exerted. (Freeman, 2017)
• Perform aftercare: In this step after care services are given to patient so that they can recover
in fast manner.
24. Discuss key considerations when managing underwater seal drainage (UWSD) tube
including intercostal catheter care when assisting an adult patient with ambulation.
The major consideration is associated with checking of patient in such a way that fluid
filled dependent loops due to which drainage can be promoted (Kashani and Saberinia, 2019). A
patient may require a chest drainage system any time the negative pressure in the pleural cavity
is disrupted, resulting in respiratory distress.
shivering may cause to individual which is a critical situation.
21. Discuss the post-operative pain management strategies a nurse could implement.
Pain assessment starts at the time of admission and should include an assessment of the patient’s
activities of daily living (ADL) and pain and stress coping skills (Jayakumar and et. al., 2019).
Post operative pain management strategies are aimed at minimising pains of patient and
minimise their discomfort. Holistic approaches are being followed by nurses dealing with post-
operative pain.
22. Explain risk assessment of a patient’s stability on their feet before assisting them
with ambulation during the immediate post-operative period
Person sitting for a longer period of time may face vertigo and in this condition patient should sit
with legs dangling. Process of patient handling is elaborated as under:
Checking of order of physician
Assessment of patient's muscle strength and activity tolerance
Assessment of patient's risk (Carantini and et. al., 2020)
Using assistive devices so that to provide ultimate care to patient.
23. Outline the steps involved in performing tracheostomy suctioning under the
headings:
• Prepare the person and the environment: Under this step the person who is treated will be
prepared as according to the environment so that treatment can be initiated.
• Perform tracheostomy suctioning: Under this step suction of catheter tip into clean water so
that residual can be exerted. (Freeman, 2017)
• Perform aftercare: In this step after care services are given to patient so that they can recover
in fast manner.
24. Discuss key considerations when managing underwater seal drainage (UWSD) tube
including intercostal catheter care when assisting an adult patient with ambulation.
The major consideration is associated with checking of patient in such a way that fluid
filled dependent loops due to which drainage can be promoted (Kashani and Saberinia, 2019). A
patient may require a chest drainage system any time the negative pressure in the pleural cavity
is disrupted, resulting in respiratory distress.
PART B
1. Briefly describe the expected responses from an enrolled nurse in this situation.
The major response from nurse can be giving optimal care to Irene so that she can
recover in early stage. Besides this nurse can ensure that the amount of water intake by her is
appropriate so that to minimise health complication to her.
2. The registered nurse asked you to continue monitoring Irene’s level of
consciousness. Which clinical assessment should you undertake?
As Irene has undergone a surgery due to which she may face differential level of consciousness
(Greig, 2017). In the day time she may feel normal and conduct regular activities in appropriate
manner but at the time of night the RPM required by lungs gets increased and due to this
situation she may feel uneasy and bear risk of severe condition.
3. The eye opening score was 2 at the time of your clinical assessment. What does this
indicate? What is the recommended nursing intervention in this scenario?
The normal eye score is 6 and Irene scored 2 which is quite low and shows lowering of
eye sight. This situation indicates that she is facing problem of low eye sight and this scenario
she needs proper medication and care. The recommended intervention in this situation is that she
can use eye drops so that to cop up with eye problem and may take proper sleep so that to avoid
any hypertension situation.
1. Briefly describe the expected responses from an enrolled nurse in this situation.
The major response from nurse can be giving optimal care to Irene so that she can
recover in early stage. Besides this nurse can ensure that the amount of water intake by her is
appropriate so that to minimise health complication to her.
2. The registered nurse asked you to continue monitoring Irene’s level of
consciousness. Which clinical assessment should you undertake?
As Irene has undergone a surgery due to which she may face differential level of consciousness
(Greig, 2017). In the day time she may feel normal and conduct regular activities in appropriate
manner but at the time of night the RPM required by lungs gets increased and due to this
situation she may feel uneasy and bear risk of severe condition.
3. The eye opening score was 2 at the time of your clinical assessment. What does this
indicate? What is the recommended nursing intervention in this scenario?
The normal eye score is 6 and Irene scored 2 which is quite low and shows lowering of
eye sight. This situation indicates that she is facing problem of low eye sight and this scenario
she needs proper medication and care. The recommended intervention in this situation is that she
can use eye drops so that to cop up with eye problem and may take proper sleep so that to avoid
any hypertension situation.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





