Acute Nursing: Comprehensive Care Plan for Cardiac Failure Patient
VerifiedAdded on 2023/04/10
|11
|2032
|353
Report
AI Summary
This report presents a case study focused on the acute nursing care of a 75-year-old patient, Sharon, diagnosed with congestive cardiac failure. It outlines the disease, its causes, incidence, and risk factors, including Sharon's history of high blood pressure and heart arrhythmias. The report discusses the impact of the disease on the patient and her family, detailing common signs and symptoms such as shortness of breath, ankle swelling, and cold extremities, along with their underlying pathophysiology. It further explores the pharmacodynamics and pharmacokinetics of Hydralazine and nitrates, common drugs used in treating congestive cardiac failure. Finally, the report develops a nursing care plan for the first 8 hours post-ward admission, prioritizing assessment, diagnosis, interventions, and rationales to improve patient outcomes. This includes managing fluid overload, improving activity tolerance, and educating the patient on medication and diet.

Running head: ACUTE NURSING 2 1
Acute nursing 2
Name
Institution
Acute nursing 2
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE NURSING 2 2
Acute nursing
1. Outline the disease, causes, incidence and risk factors. Discuss the impact
of the selected disease on the patient and their family (450 words)
Congestive cardiac failure happens when the heart muscles do not pump blood as it is
expected (Matthew & Kevin, 2010). One of the causes of congestive cardiac failures is high
blood pressure. This condition weakens the heart and makes it unable to pump blood efficiently
(Van & Viviane, 2010). Sharon experienced shortness in breath due to high blood pressure which
was 170/110mmHg above the normal rate. Also, the inspiratory crackles which were within the
lung bases made her swell the ankles because the muscles could not pump the blood well back to
the heart. Moreover, the reason for feeling nausea and dizziness were as a result of high blood
pressure because it affects the amount of blood the heart pumps from the lungs to the rest of the
body.
According to Marianne (2010), at least over 200,000 Australians have a congestive
cardiac failure of which 4% of the population have 45 years and above with more than 30,000
new cases diagnosed each year. Sharon has 75yrs and this means that she is at high risk of
getting a congestive cardiac failure.
The risk factors associated with congestive cardiac failure include obesity, diabetes and
heart arrhythmias, (Rodica, 2016). According to examinations done to Sharon, they proved that
she had heart arrhythmias. This condition can be defined as abnormal heart rhythms which may
make it breathe too fast hence creating more work (Priscilla & Frank, 2014). This may, therefore,
weaken the heart hence making the vessels unable to pump the blood well. This situation can
cause shortness in a breath as it was reported with Sharon.
Acute nursing
1. Outline the disease, causes, incidence and risk factors. Discuss the impact
of the selected disease on the patient and their family (450 words)
Congestive cardiac failure happens when the heart muscles do not pump blood as it is
expected (Matthew & Kevin, 2010). One of the causes of congestive cardiac failures is high
blood pressure. This condition weakens the heart and makes it unable to pump blood efficiently
(Van & Viviane, 2010). Sharon experienced shortness in breath due to high blood pressure which
was 170/110mmHg above the normal rate. Also, the inspiratory crackles which were within the
lung bases made her swell the ankles because the muscles could not pump the blood well back to
the heart. Moreover, the reason for feeling nausea and dizziness were as a result of high blood
pressure because it affects the amount of blood the heart pumps from the lungs to the rest of the
body.
According to Marianne (2010), at least over 200,000 Australians have a congestive
cardiac failure of which 4% of the population have 45 years and above with more than 30,000
new cases diagnosed each year. Sharon has 75yrs and this means that she is at high risk of
getting a congestive cardiac failure.
The risk factors associated with congestive cardiac failure include obesity, diabetes and
heart arrhythmias, (Rodica, 2016). According to examinations done to Sharon, they proved that
she had heart arrhythmias. This condition can be defined as abnormal heart rhythms which may
make it breathe too fast hence creating more work (Priscilla & Frank, 2014). This may, therefore,
weaken the heart hence making the vessels unable to pump the blood well. This situation can
cause shortness in a breath as it was reported with Sharon.
ACUTE NURSING 2 3
Also, the MI disease which Sharon was diagnosed with at the age of 65 can be a risk
factor of congestive cardiac failure. This occurs when there is a decrease in the amount of blood
flow to parts of the heart hence damaging its muscles (Tracy, 2011). Once these muscles are
damaged, there would be insufficient blood in the heart hence causing breathing problems.
People with cardiac failure experience difficulties in breathing, working and also their
bodies become prone to other diseases (Priscilla & Frank, 2014). Like in this case, Sharon has
experienced shortness in breathing due to the inability of the heart to pump sufficient blood as
expected. Also, this has made her not to do work which is essential for body exercise because it
affects her breathing. Moreover, it has made her swell the ankles because the muscles cannot
pump the blood back to the heart hence causing retention.
Congestive cardiac failure has also affected Sharon’s family negatively because they
always live in fear of losing her. It has also affected their standards of living since most of the
income is used in paying the hospital bills.
1 Discuss three (3) common signs and symptoms of the selected disease and
explain the underlying pathophysiology of each (350 words)
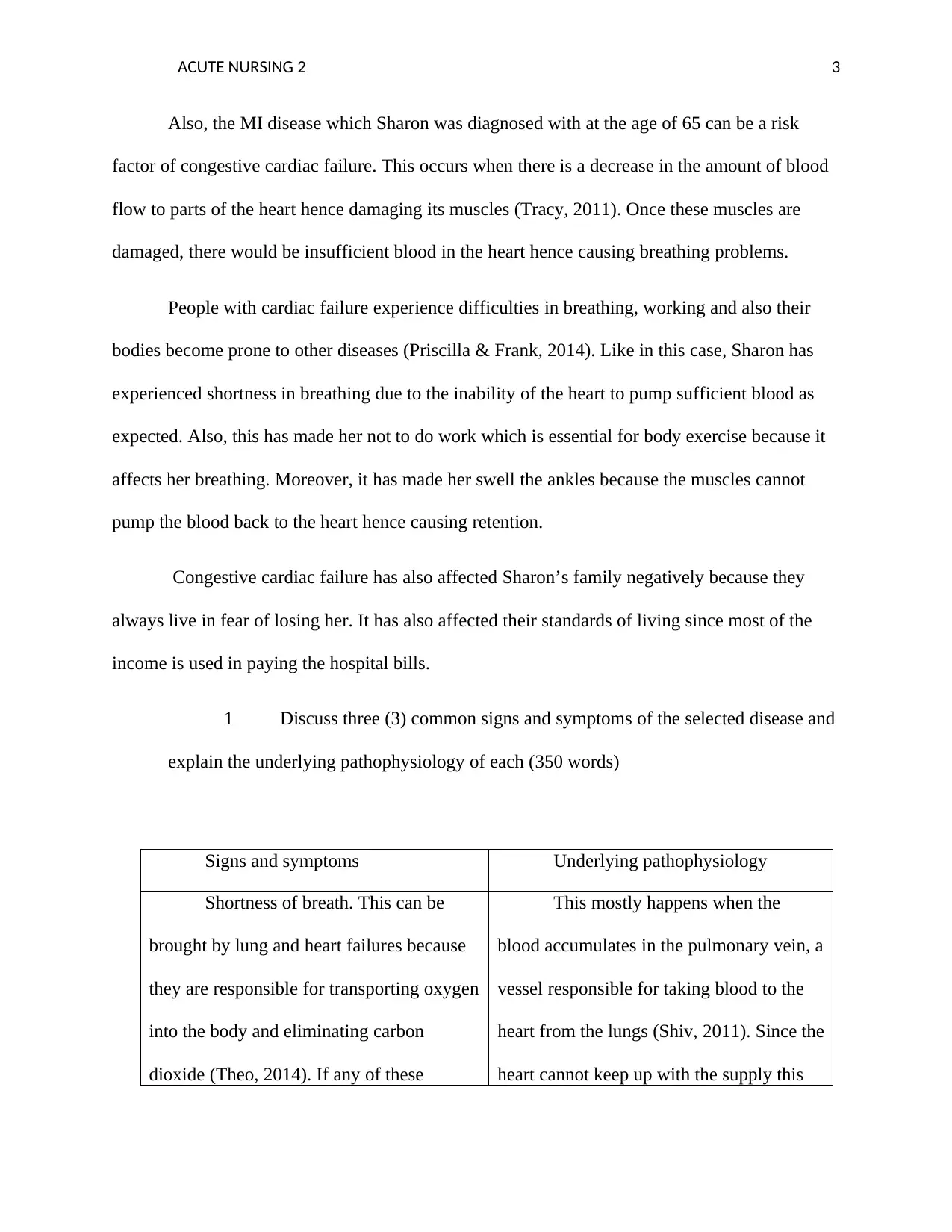
Signs and symptoms Underlying pathophysiology
Shortness of breath. This can be
brought by lung and heart failures because
they are responsible for transporting oxygen
into the body and eliminating carbon
dioxide (Theo, 2014). If any of these
This mostly happens when the
blood accumulates in the pulmonary vein, a
vessel responsible for taking blood to the
heart from the lungs (Shiv, 2011). Since the
heart cannot keep up with the supply this
Also, the MI disease which Sharon was diagnosed with at the age of 65 can be a risk
factor of congestive cardiac failure. This occurs when there is a decrease in the amount of blood
flow to parts of the heart hence damaging its muscles (Tracy, 2011). Once these muscles are
damaged, there would be insufficient blood in the heart hence causing breathing problems.
People with cardiac failure experience difficulties in breathing, working and also their
bodies become prone to other diseases (Priscilla & Frank, 2014). Like in this case, Sharon has
experienced shortness in breathing due to the inability of the heart to pump sufficient blood as
expected. Also, this has made her not to do work which is essential for body exercise because it
affects her breathing. Moreover, it has made her swell the ankles because the muscles cannot
pump the blood back to the heart hence causing retention.
Congestive cardiac failure has also affected Sharon’s family negatively because they
always live in fear of losing her. It has also affected their standards of living since most of the
income is used in paying the hospital bills.
1 Discuss three (3) common signs and symptoms of the selected disease and
explain the underlying pathophysiology of each (350 words)
Signs and symptoms Underlying pathophysiology
Shortness of breath. This can be
brought by lung and heart failures because
they are responsible for transporting oxygen
into the body and eliminating carbon
dioxide (Theo, 2014). If any of these
This mostly happens when the
blood accumulates in the pulmonary vein, a
vessel responsible for taking blood to the
heart from the lungs (Shiv, 2011). Since the
heart cannot keep up with the supply this
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE NURSING 2 4
develop problems, it would also affect one's
breathing system. In most cases, shortening
in breath is accompanied by swelling of feet
and ankles and trouble in breathing when
one does heavy exercise. Shortness in
breath has many causes but in our case,
McKenzie is experiencing that due to
cardiac failure.
causes some fluids to leak into the lungs
hence causing shortness in breath. A person
with cardiac failure may experience
breathless especially when doing activities
(Marianne, 2010). Like in this case,
McKenzie experienced shortness in a
breath when she went for gardening and
took a walk with her husband. However,
shortness in breathing can also occur while
resting or sleeping.
Ankle swelling. This refers to the
accumulation of fluids in the ankles and is
most common in old adults (Jessica &
Susan, 2014). Swelling occurs in lower
parts of the body due to gravity. Swelling of
ankles can be brought about by standing for
a long time. McKenzie experienced
swelling when she went to cultivate in the
garden and took a walk with her husband.
This occurs when the muscles are
inactive such that they cannot pump body
fluids up towards the heart (Maryana &
Liubov, 2019). This retention of water and
blood, therefore, causes swelling of ankles.
Also, high blood pressure which was
examined in McKenzie can result in the
poor circulation of body fluids hence
causing swelling of ankles.
Cold hands and feet. In most cases,
People with cardiac failure find their hands
and legs too cold because there is no
sufficient blood to warm them (Dilip,
This may happen due to the failure
of the muscles to pump blood from the
heart to all parts of the body (Marianne,
2010). It’s common in people with cardiac
develop problems, it would also affect one's
breathing system. In most cases, shortening
in breath is accompanied by swelling of feet
and ankles and trouble in breathing when
one does heavy exercise. Shortness in
breath has many causes but in our case,
McKenzie is experiencing that due to
cardiac failure.
causes some fluids to leak into the lungs
hence causing shortness in breath. A person
with cardiac failure may experience
breathless especially when doing activities
(Marianne, 2010). Like in this case,
McKenzie experienced shortness in a
breath when she went for gardening and
took a walk with her husband. However,
shortness in breathing can also occur while
resting or sleeping.
Ankle swelling. This refers to the
accumulation of fluids in the ankles and is
most common in old adults (Jessica &
Susan, 2014). Swelling occurs in lower
parts of the body due to gravity. Swelling of
ankles can be brought about by standing for
a long time. McKenzie experienced
swelling when she went to cultivate in the
garden and took a walk with her husband.
This occurs when the muscles are
inactive such that they cannot pump body
fluids up towards the heart (Maryana &
Liubov, 2019). This retention of water and
blood, therefore, causes swelling of ankles.
Also, high blood pressure which was
examined in McKenzie can result in the
poor circulation of body fluids hence
causing swelling of ankles.
Cold hands and feet. In most cases,
People with cardiac failure find their hands
and legs too cold because there is no
sufficient blood to warm them (Dilip,
This may happen due to the failure
of the muscles to pump blood from the
heart to all parts of the body (Marianne,
2010). It’s common in people with cardiac
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE NURSING 2 5
2016). failure.
2 Discuss the pharmacodynamics & pharmacokinetics of one (1) common
class of drug relevant to the chosen patient (300 words)
Congestive cardiac failure can be treated with different drugs but in this case,
would talk about Hydralazine and nitrates. These drugs give mortality and symptomatic
benefit in people with cardiac failure with decreased ejection fraction because of systolic
dysfunction (Tracy, 2011). One of the pharmacodynamics of these drugs is that they help
in opening blood vessels to make it easier for the heart to receive and pump blood. This
helps in preventing occurrences like short breathing and swelling of legs and ankles
(Jessica & Susan, 2014). Also, these drugs have a direct effect on the vascular smooth
muscle hence helps in lowering blood pressure. Hydralazine and nitrates would,
therefore, bring positive effects to McKenzie for they will help in lowering her blood
pressure.
The pharmacokinetics of hydralazine involves various stages from the time of
absorption to excretion. Hydralazine drugs are absorbed from the GI tract immediately
after admitted in the mouth (Theo, 2014). In this stage, bioavailability is usually 30-50%
and the absorption is mostly boosted by food. People are therefore advised to take their
meals before taking these hydralazine drugs for it aids in absorption. After absorption,
these drugs are usually circulated to all parts of the body and at this stage, the drugs are
80-90 % protein bound (Jessica & Susan, 2014). After the drugs are distributed
2016). failure.
2 Discuss the pharmacodynamics & pharmacokinetics of one (1) common
class of drug relevant to the chosen patient (300 words)
Congestive cardiac failure can be treated with different drugs but in this case,
would talk about Hydralazine and nitrates. These drugs give mortality and symptomatic
benefit in people with cardiac failure with decreased ejection fraction because of systolic
dysfunction (Tracy, 2011). One of the pharmacodynamics of these drugs is that they help
in opening blood vessels to make it easier for the heart to receive and pump blood. This
helps in preventing occurrences like short breathing and swelling of legs and ankles
(Jessica & Susan, 2014). Also, these drugs have a direct effect on the vascular smooth
muscle hence helps in lowering blood pressure. Hydralazine and nitrates would,
therefore, bring positive effects to McKenzie for they will help in lowering her blood
pressure.
The pharmacokinetics of hydralazine involves various stages from the time of
absorption to excretion. Hydralazine drugs are absorbed from the GI tract immediately
after admitted in the mouth (Theo, 2014). In this stage, bioavailability is usually 30-50%
and the absorption is mostly boosted by food. People are therefore advised to take their
meals before taking these hydralazine drugs for it aids in absorption. After absorption,
these drugs are usually circulated to all parts of the body and at this stage, the drugs are
80-90 % protein bound (Jessica & Susan, 2014). After the drugs are distributed
ACUTE NURSING 2 6
throughout the body, they are then metabolized thoroughly in the GI mucosa and the
liver. Hydralazine in most cases brings about polymorphic acetylation (Theo, 2014).
People with slow acetylation mostly have high plasma levels and are therefore required to
take lower doses. After all those stages, hydralazine is excreted from the body through
urine or feces. In most cases, the dose is usually excreted through urine and only 10 % is
eliminated through feces.
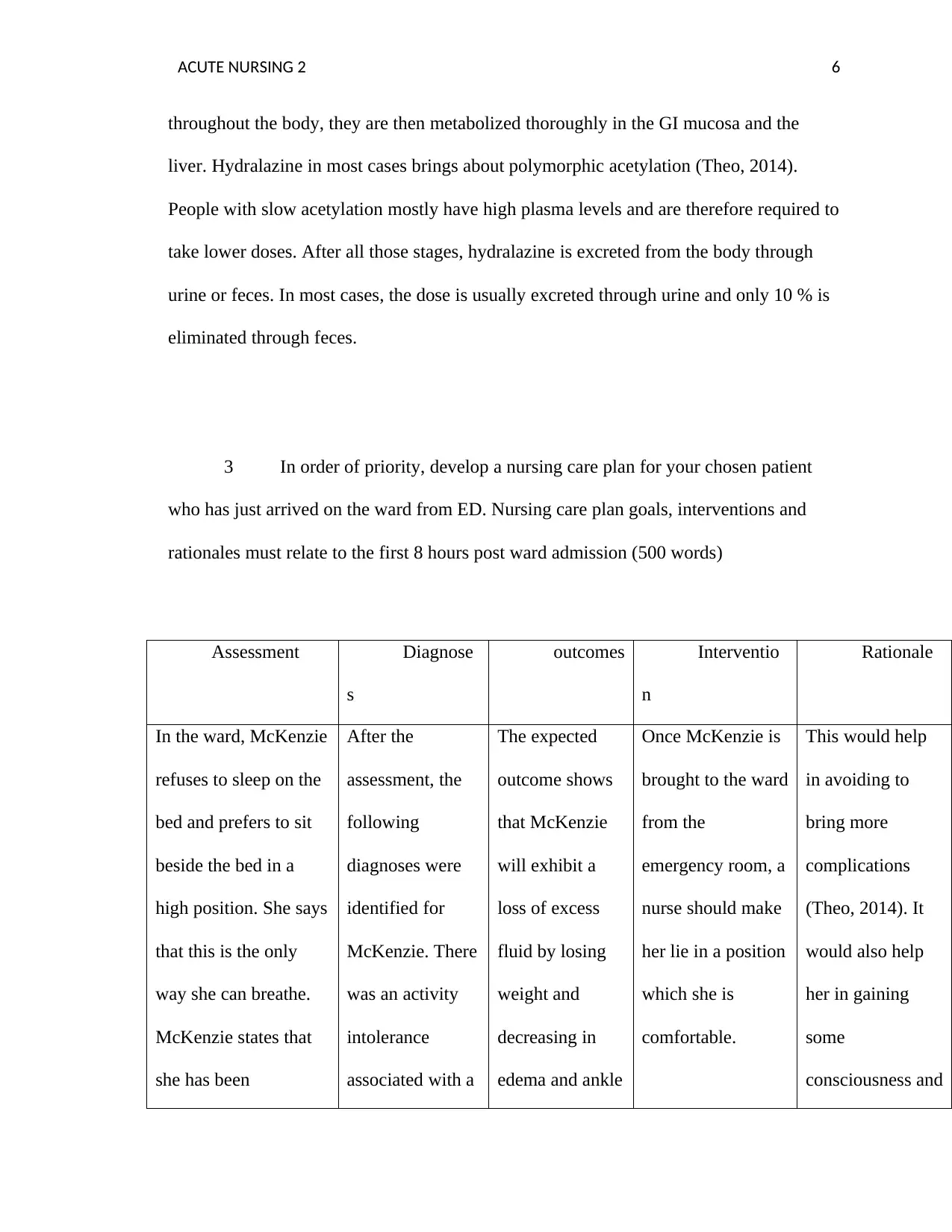
3 In order of priority, develop a nursing care plan for your chosen patient
who has just arrived on the ward from ED. Nursing care plan goals, interventions and
rationales must relate to the first 8 hours post ward admission (500 words)
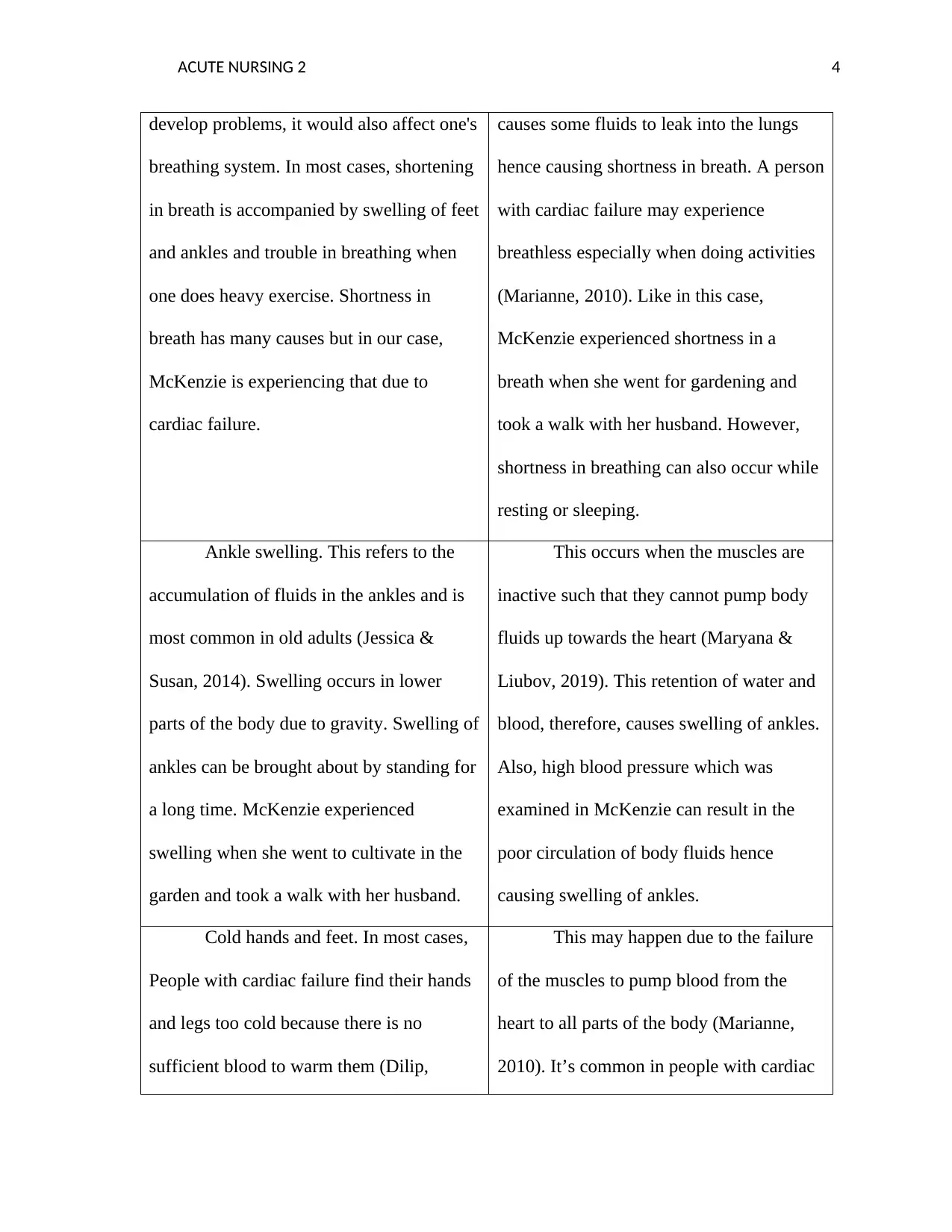
Assessment Diagnose
s
outcomes Interventio
n
Rationale
In the ward, McKenzie
refuses to sleep on the
bed and prefers to sit
beside the bed in a
high position. She says
that this is the only
way she can breathe.
McKenzie states that
she has been
After the
assessment, the
following
diagnoses were
identified for
McKenzie. There
was an activity
intolerance
associated with a
The expected
outcome shows
that McKenzie
will exhibit a
loss of excess
fluid by losing
weight and
decreasing in
edema and ankle
Once McKenzie is
brought to the ward
from the
emergency room, a
nurse should make
her lie in a position
which she is
comfortable.
This would help
in avoiding to
bring more
complications
(Theo, 2014). It
would also help
her in gaining
some
consciousness and
throughout the body, they are then metabolized thoroughly in the GI mucosa and the
liver. Hydralazine in most cases brings about polymorphic acetylation (Theo, 2014).
People with slow acetylation mostly have high plasma levels and are therefore required to
take lower doses. After all those stages, hydralazine is excreted from the body through
urine or feces. In most cases, the dose is usually excreted through urine and only 10 % is
eliminated through feces.
3 In order of priority, develop a nursing care plan for your chosen patient
who has just arrived on the ward from ED. Nursing care plan goals, interventions and
rationales must relate to the first 8 hours post ward admission (500 words)
Assessment Diagnose
s
outcomes Interventio
n
Rationale
In the ward, McKenzie
refuses to sleep on the
bed and prefers to sit
beside the bed in a
high position. She says
that this is the only
way she can breathe.
McKenzie states that
she has been
After the
assessment, the
following
diagnoses were
identified for
McKenzie. There
was an activity
intolerance
associated with a
The expected
outcome shows
that McKenzie
will exhibit a
loss of excess
fluid by losing
weight and
decreasing in
edema and ankle
Once McKenzie is
brought to the ward
from the
emergency room, a
nurse should make
her lie in a position
which she is
comfortable.
This would help
in avoiding to
bring more
complications
(Theo, 2014). It
would also help
her in gaining
some
consciousness and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
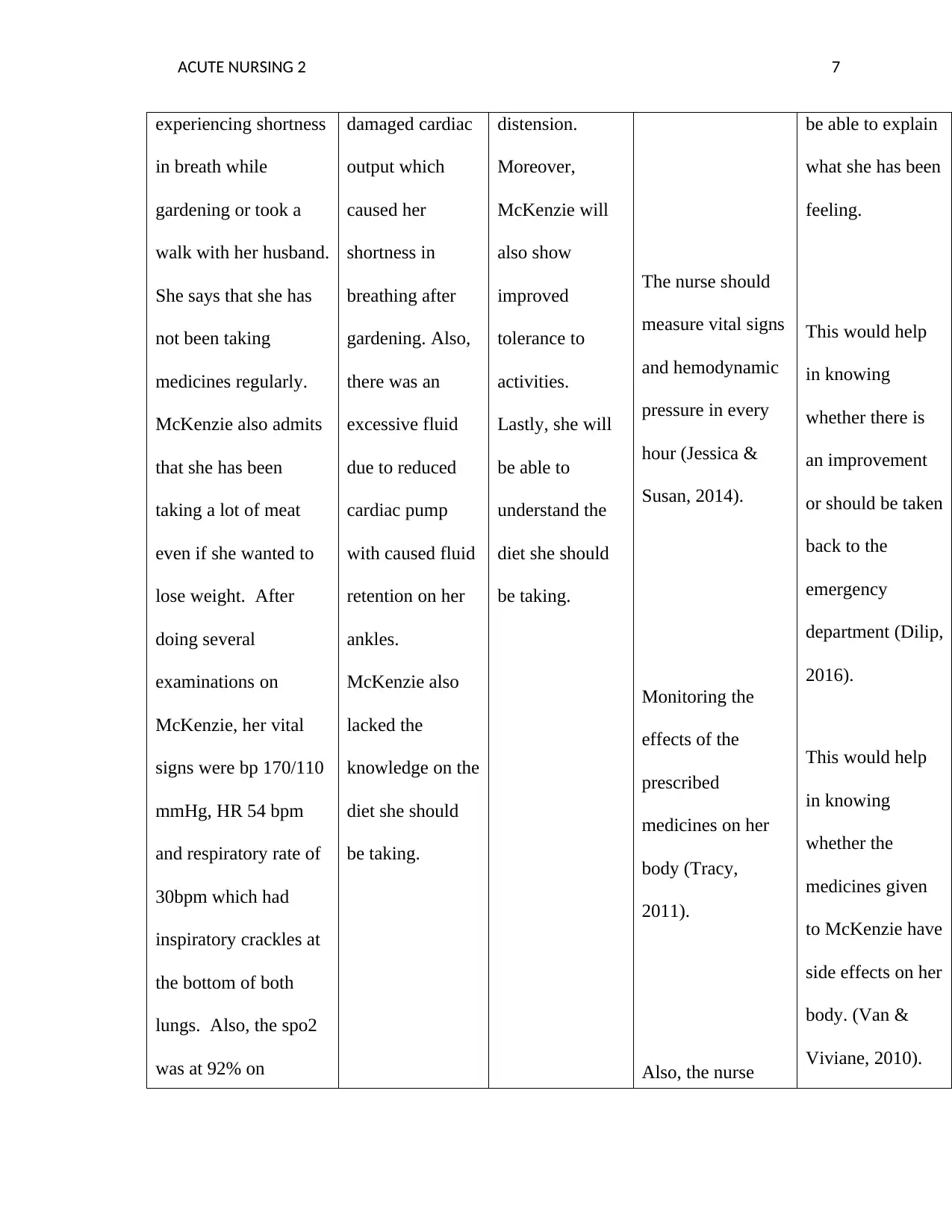
ACUTE NURSING 2 7
experiencing shortness
in breath while
gardening or took a
walk with her husband.
She says that she has
not been taking
medicines regularly.
McKenzie also admits
that she has been
taking a lot of meat
even if she wanted to
lose weight. After
doing several
examinations on
McKenzie, her vital
signs were bp 170/110
mmHg, HR 54 bpm
and respiratory rate of
30bpm which had
inspiratory crackles at
the bottom of both
lungs. Also, the spo2
was at 92% on
damaged cardiac
output which
caused her
shortness in
breathing after
gardening. Also,
there was an
excessive fluid
due to reduced
cardiac pump
with caused fluid
retention on her
ankles.
McKenzie also
lacked the
knowledge on the
diet she should
be taking.
distension.
Moreover,
McKenzie will
also show
improved
tolerance to
activities.
Lastly, she will
be able to
understand the
diet she should
be taking.
The nurse should
measure vital signs
and hemodynamic
pressure in every
hour (Jessica &
Susan, 2014).
Monitoring the
effects of the
prescribed
medicines on her
body (Tracy,
2011).
Also, the nurse
be able to explain
what she has been
feeling.
This would help
in knowing
whether there is
an improvement
or should be taken
back to the
emergency
department (Dilip,
2016).
This would help
in knowing
whether the
medicines given
to McKenzie have
side effects on her
body. (Van &
Viviane, 2010).
experiencing shortness
in breath while
gardening or took a
walk with her husband.
She says that she has
not been taking
medicines regularly.
McKenzie also admits
that she has been
taking a lot of meat
even if she wanted to
lose weight. After
doing several
examinations on
McKenzie, her vital
signs were bp 170/110
mmHg, HR 54 bpm
and respiratory rate of
30bpm which had
inspiratory crackles at
the bottom of both
lungs. Also, the spo2
was at 92% on
damaged cardiac
output which
caused her
shortness in
breathing after
gardening. Also,
there was an
excessive fluid
due to reduced
cardiac pump
with caused fluid
retention on her
ankles.
McKenzie also
lacked the
knowledge on the
diet she should
be taking.
distension.
Moreover,
McKenzie will
also show
improved
tolerance to
activities.
Lastly, she will
be able to
understand the
diet she should
be taking.
The nurse should
measure vital signs
and hemodynamic
pressure in every
hour (Jessica &
Susan, 2014).
Monitoring the
effects of the
prescribed
medicines on her
body (Tracy,
2011).
Also, the nurse
be able to explain
what she has been
feeling.
This would help
in knowing
whether there is
an improvement
or should be taken
back to the
emergency
department (Dilip,
2016).
This would help
in knowing
whether the
medicines given
to McKenzie have
side effects on her
body. (Van &
Viviane, 2010).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
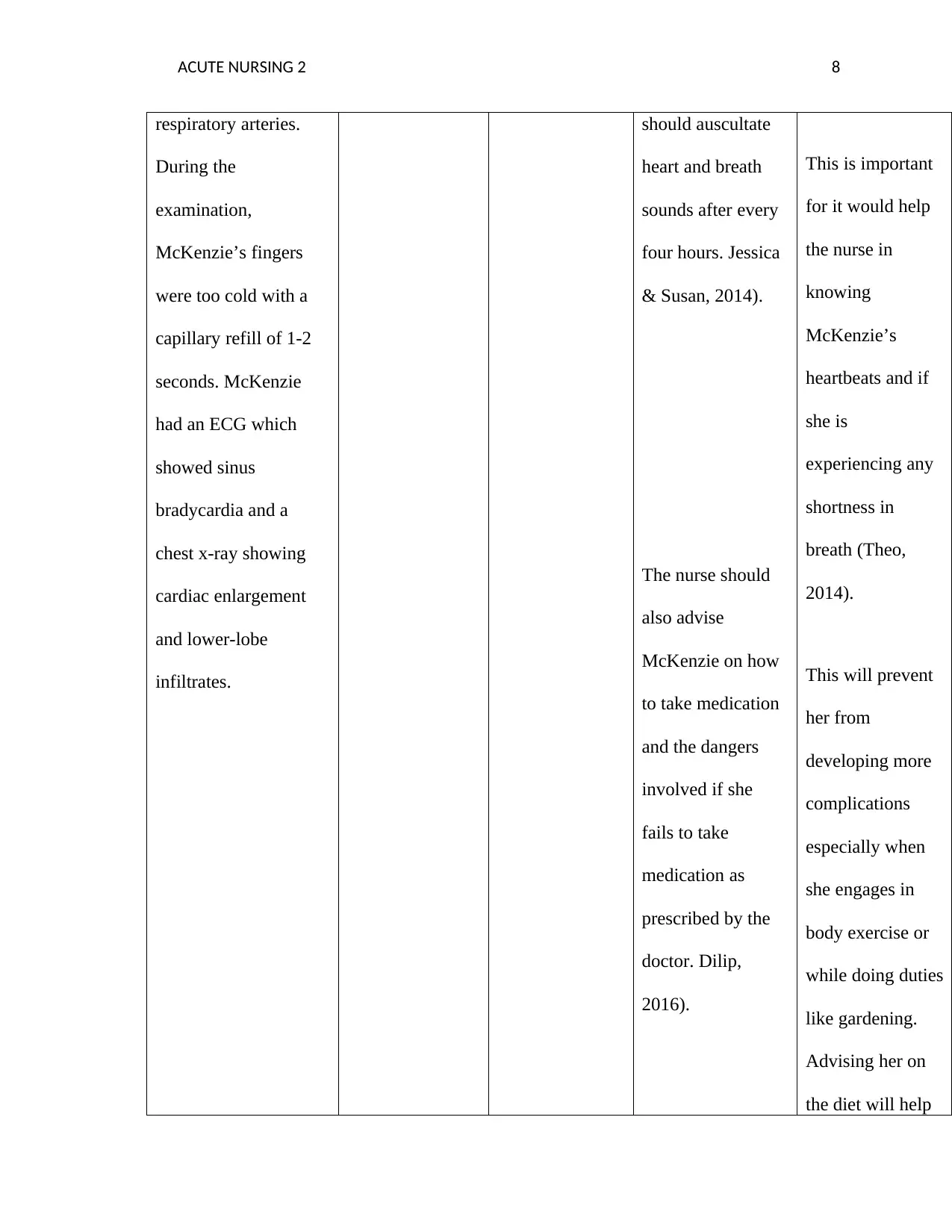
ACUTE NURSING 2 8
respiratory arteries.
During the
examination,
McKenzie’s fingers
were too cold with a
capillary refill of 1-2
seconds. McKenzie
had an ECG which
showed sinus
bradycardia and a
chest x-ray showing
cardiac enlargement
and lower-lobe
infiltrates.
should auscultate
heart and breath
sounds after every
four hours. Jessica
& Susan, 2014).
The nurse should
also advise
McKenzie on how
to take medication
and the dangers
involved if she
fails to take
medication as
prescribed by the
doctor. Dilip,
2016).
This is important
for it would help
the nurse in
knowing
McKenzie’s
heartbeats and if
she is
experiencing any
shortness in
breath (Theo,
2014).
This will prevent
her from
developing more
complications
especially when
she engages in
body exercise or
while doing duties
like gardening.
Advising her on
the diet will help
respiratory arteries.
During the
examination,
McKenzie’s fingers
were too cold with a
capillary refill of 1-2
seconds. McKenzie
had an ECG which
showed sinus
bradycardia and a
chest x-ray showing
cardiac enlargement
and lower-lobe
infiltrates.
should auscultate
heart and breath
sounds after every
four hours. Jessica
& Susan, 2014).
The nurse should
also advise
McKenzie on how
to take medication
and the dangers
involved if she
fails to take
medication as
prescribed by the
doctor. Dilip,
2016).
This is important
for it would help
the nurse in
knowing
McKenzie’s
heartbeats and if
she is
experiencing any
shortness in
breath (Theo,
2014).
This will prevent
her from
developing more
complications
especially when
she engages in
body exercise or
while doing duties
like gardening.
Advising her on
the diet will help
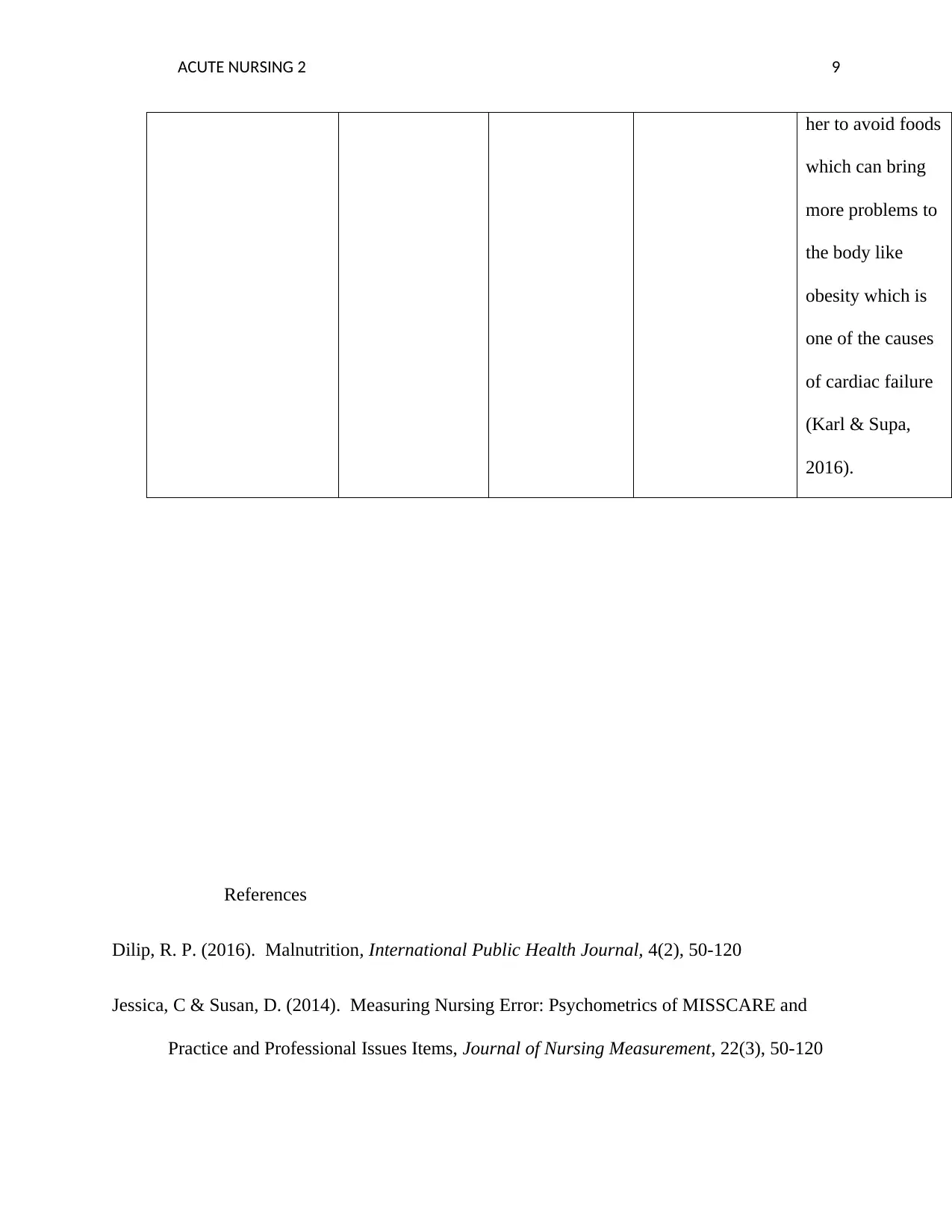
ACUTE NURSING 2 9
her to avoid foods
which can bring
more problems to
the body like
obesity which is
one of the causes
of cardiac failure
(Karl & Supa,
2016).
References
Dilip, R. P. (2016). Malnutrition, International Public Health Journal, 4(2), 50-120
Jessica, C & Susan, D. (2014). Measuring Nursing Error: Psychometrics of MISSCARE and
Practice and Professional Issues Items, Journal of Nursing Measurement, 22(3), 50-120
her to avoid foods
which can bring
more problems to
the body like
obesity which is
one of the causes
of cardiac failure
(Karl & Supa,
2016).
References
Dilip, R. P. (2016). Malnutrition, International Public Health Journal, 4(2), 50-120
Jessica, C & Susan, D. (2014). Measuring Nursing Error: Psychometrics of MISSCARE and
Practice and Professional Issues Items, Journal of Nursing Measurement, 22(3), 50-120
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE NURSING 2 10
Karl, P & Supa, P. (2016). Dietary Behaviour among Male and Female Chronic Disease Patients
in Cambodia, Myanmar and Vietnam, Gender & Behaviour, 14(1), 90-140
Marianne, R. (2010). A Practical Guide to Heart Failure in Older People, Care Management
Journals, 11(2), 90-120
Maryana, C & Liubov, C. (2019). Functional Condition of Ukrainian Schoolchildren with
Chronic Heart Failure of I-IIA Stages, Journal of Physical Education and Sport 90-150
Matthew, S.F & Kevin, L.K (2010). Focus on the Heart: Alcohol Consumption, HIV Infection,
and Cardiovascular Disease, Alcohol Research, 33(3), 90-150
Priscilla, O.O & Frank, G. (2014). Effects of Patients and Hospital Characteristics on
Myocardial Infarction Mortality: Health Disparity Outcomes, ABNF Journal, 25(1), 10-
120
Rodica, R. (2016). Obesity, a Risk Factor for Cardiac Remodeling, Romanian Journal of
Artistic Creativity, 4(3), 20-50
Shiv, G. (2011). Fourth Revolution in Psychiatry - Addressing Comorbidity with Chronic
Physical Disorders, Indian Journal of Psychiatry, 52 (3), 100-120
Theo, V. A. (2014). Revisiting Basic Nursing Care, Journal of Nursing Scholarship, 46(1), 100-
160
Tracy, A. T. (2011). Pharmaceutical Management of Chronic Heart Failure as Evidenced by
Clinical Trials, Journal of the National Society of Allied Health, 8(9), 50-120
Karl, P & Supa, P. (2016). Dietary Behaviour among Male and Female Chronic Disease Patients
in Cambodia, Myanmar and Vietnam, Gender & Behaviour, 14(1), 90-140
Marianne, R. (2010). A Practical Guide to Heart Failure in Older People, Care Management
Journals, 11(2), 90-120
Maryana, C & Liubov, C. (2019). Functional Condition of Ukrainian Schoolchildren with
Chronic Heart Failure of I-IIA Stages, Journal of Physical Education and Sport 90-150
Matthew, S.F & Kevin, L.K (2010). Focus on the Heart: Alcohol Consumption, HIV Infection,
and Cardiovascular Disease, Alcohol Research, 33(3), 90-150
Priscilla, O.O & Frank, G. (2014). Effects of Patients and Hospital Characteristics on
Myocardial Infarction Mortality: Health Disparity Outcomes, ABNF Journal, 25(1), 10-
120
Rodica, R. (2016). Obesity, a Risk Factor for Cardiac Remodeling, Romanian Journal of
Artistic Creativity, 4(3), 20-50
Shiv, G. (2011). Fourth Revolution in Psychiatry - Addressing Comorbidity with Chronic
Physical Disorders, Indian Journal of Psychiatry, 52 (3), 100-120
Theo, V. A. (2014). Revisiting Basic Nursing Care, Journal of Nursing Scholarship, 46(1), 100-
160
Tracy, A. T. (2011). Pharmaceutical Management of Chronic Heart Failure as Evidenced by
Clinical Trials, Journal of the National Society of Allied Health, 8(9), 50-120
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE NURSING 2 11
Van, D.D & Viviane, C. (2010). Symptoms and Clinical Signs Associated with Hospital
Admission and Mortality for Heart Failure, Central European Journal of Public Health,
18(4), 70-150
Van, D.D & Viviane, C. (2010). Symptoms and Clinical Signs Associated with Hospital
Admission and Mortality for Heart Failure, Central European Journal of Public Health,
18(4), 70-150
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





