A Case Study on Acute Pancreatitis, Type 2 Diabetes, Hypertension
VerifiedAdded on 2023/06/18
|14
|4309
|199
Case Study
AI Summary
This case study examines a 40-year-old woman presenting with severe abdominal pain indicative of acute pancreatitis, further complicated by type 2 diabetes and hypertension. The analysis delves into the symptoms, diagnostic process, and underlying pathology of acute pancreatitis, highlighting the roles of gallstones, alcohol consumption, and pre-existing conditions like diabetes and hypertension. The case presentation details the patient's symptoms, including abdominal pain radiating to the back, vomiting, and associated risk factors. Diagnosis involves medical history, physical examinations, blood tests for digestive enzymes, and radiological studies such as CT scans to confirm the condition and rule out other potential causes of abdominal pain. The study also discusses the pathophysiology of acute pancreatitis, including the loss of intracellular compartmentation and activation of pancreatic enzymes, emphasizing the importance of early diagnosis and appropriate management to prevent severe complications.
CASE STUDY: A case of
Acute Pancreatitis in
association with type 2 diabetes
and hypertension
Acute Pancreatitis in
association with type 2 diabetes
and hypertension
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

INTRODUCTION
The case study has shown that a 40- year old woman is suffering from abdominal pain
that is a sign leading to several problems. Acute pancreatitis is the inflammation of the pancreas
which is developed at quick pace. Some of the main symptoms of this disease is having an
abdominal pain which in most of the cases settle in few days while becomes severe and highly
serious in other cases (Ye & et.al., (2017)). Most common causes for the acute pancreatitis
includes gallstones and consuming a lot of alcohol. In mild cases this is solved without any
treatment however, in the severe cases this problem can lead to trigger some fatal complications.
The most common cause of acute pancreatitis is having gallstones which are inflammations in
the pancreas as the stone which is passed through gets stuck in the bile or in the pancreatic duct
(Lee, & Papachristou, (2019)). This is also known as gallstone pancreatitis. Pathology of acute
pancreatitis is about the loss of intracellular as well as extracellular compartmentation. This is
done by the obstruction of pancreatic secretory transport and the activation of the enzymes of
pancreas. The incidence of acute pancreatitis is increasing globally with the increase in cases of
obesity and gallstones. The epidemiology of acute pancreatitis is ranged from 13 to 45 per
100000 population years and that of chronic pancreatitis ranges from 5 to 12 per 100000
population years (Ouyang, & et.al., (2020)). There are many treatments for acute pancreatitis
such as treating dehydration, medications, following a low- fat diet and so on. Some mild cases
of prognosis has low mortality rate but in the severe cases, patients are more likely to develop
complications and have more chances of higher death rate. This case study will evaluate the root
cause of acute pancreatitis with a discussion about ways of diagnosing the problem.
CASE PRESENTATION
The burden of acute pancreatitis is expected to increase over time. In this case study it
can be seen that a middle- aged woman is experiencing a severe pain in her abdominal area
which is radiating towards her back. This pain increases when she is lying on her back however,
sitting up and leaning towards the forward direction makes the pain bearable. The main
symptoms of acute pancreatitis includes abdominal pain which starts from below the ribs and
increases quickly over few hours (Karjula, & et.al., (2019)). This pain is severe when it is felt
spreading at the back and is sudden as well as intense. This pain starts as being mild by eating
and then is grown to increase slowly. This problem is very common in case of diabetes or to the
The case study has shown that a 40- year old woman is suffering from abdominal pain
that is a sign leading to several problems. Acute pancreatitis is the inflammation of the pancreas
which is developed at quick pace. Some of the main symptoms of this disease is having an
abdominal pain which in most of the cases settle in few days while becomes severe and highly
serious in other cases (Ye & et.al., (2017)). Most common causes for the acute pancreatitis
includes gallstones and consuming a lot of alcohol. In mild cases this is solved without any
treatment however, in the severe cases this problem can lead to trigger some fatal complications.
The most common cause of acute pancreatitis is having gallstones which are inflammations in
the pancreas as the stone which is passed through gets stuck in the bile or in the pancreatic duct
(Lee, & Papachristou, (2019)). This is also known as gallstone pancreatitis. Pathology of acute
pancreatitis is about the loss of intracellular as well as extracellular compartmentation. This is
done by the obstruction of pancreatic secretory transport and the activation of the enzymes of
pancreas. The incidence of acute pancreatitis is increasing globally with the increase in cases of
obesity and gallstones. The epidemiology of acute pancreatitis is ranged from 13 to 45 per
100000 population years and that of chronic pancreatitis ranges from 5 to 12 per 100000
population years (Ouyang, & et.al., (2020)). There are many treatments for acute pancreatitis
such as treating dehydration, medications, following a low- fat diet and so on. Some mild cases
of prognosis has low mortality rate but in the severe cases, patients are more likely to develop
complications and have more chances of higher death rate. This case study will evaluate the root
cause of acute pancreatitis with a discussion about ways of diagnosing the problem.
CASE PRESENTATION
The burden of acute pancreatitis is expected to increase over time. In this case study it
can be seen that a middle- aged woman is experiencing a severe pain in her abdominal area
which is radiating towards her back. This pain increases when she is lying on her back however,
sitting up and leaning towards the forward direction makes the pain bearable. The main
symptoms of acute pancreatitis includes abdominal pain which starts from below the ribs and
increases quickly over few hours (Karjula, & et.al., (2019)). This pain is severe when it is felt
spreading at the back and is sudden as well as intense. This pain starts as being mild by eating
and then is grown to increase slowly. This problem is very common in case of diabetes or to the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
individuals having kidney problems. Another symptom is being sick, high temperatures of body
and having the feeling of being unwell. The abdomen is swollen and one can even experience
lack of fluid in the body. It also results in having a low blood pressure. The table below depicts
the most common and initial symptoms for acute pancreatitis.
Vomiting
Nausea
Diarrhoea
Loss of appetite
Rapid pulse
Pain while coughing
Skin to take on yellowish tinge
Blood pressure to fall or rise,
causing faintness
Pain which is not controlled even
by strong painkillers
A lot of these possible symptoms for acute pancreatitis matches with the things
experienced by the women in the case study. She had vomiting which made her better regarding
the abdominal pain. There can me many reason behind the cause of this issue such as gallstones
and high consumption of alcohol. The gall stones are very common in UK. It passes through bile
duct and in the part of the just after stomach known as duodenum. In some cases this gallstone is
stuck in the bile duct. It affects the chemicals present in the duct and triggers pancreatitis. A lot
of cases of pancreatitis are associated with alcohol. Alcohol makes the cells of pancreas more
sensitive leading in blood and high infection. Another cause for acute pancreatitis is high blood
fat levels which is also known as hypertriglyceridaemia (Shah, Mourad, & Bramhall, (2018)). In
very rare cases autoimmune is where the immune system of an individual attacks the pancreas
leading to such problems within the body. In this case the woman denies of having any alcohol
consumption but has the problem of uncontrollable hyper tension and diabetes of type 2. These
are factors which lead her to the illness of acute pancreatitis. The diagnosis of acute pancreatitis
and having the feeling of being unwell. The abdomen is swollen and one can even experience
lack of fluid in the body. It also results in having a low blood pressure. The table below depicts
the most common and initial symptoms for acute pancreatitis.
Vomiting
Nausea
Diarrhoea
Loss of appetite
Rapid pulse
Pain while coughing
Skin to take on yellowish tinge
Blood pressure to fall or rise,
causing faintness
Pain which is not controlled even
by strong painkillers
A lot of these possible symptoms for acute pancreatitis matches with the things
experienced by the women in the case study. She had vomiting which made her better regarding
the abdominal pain. There can me many reason behind the cause of this issue such as gallstones
and high consumption of alcohol. The gall stones are very common in UK. It passes through bile
duct and in the part of the just after stomach known as duodenum. In some cases this gallstone is
stuck in the bile duct. It affects the chemicals present in the duct and triggers pancreatitis. A lot
of cases of pancreatitis are associated with alcohol. Alcohol makes the cells of pancreas more
sensitive leading in blood and high infection. Another cause for acute pancreatitis is high blood
fat levels which is also known as hypertriglyceridaemia (Shah, Mourad, & Bramhall, (2018)). In
very rare cases autoimmune is where the immune system of an individual attacks the pancreas
leading to such problems within the body. In this case the woman denies of having any alcohol
consumption but has the problem of uncontrollable hyper tension and diabetes of type 2. These
are factors which lead her to the illness of acute pancreatitis. The diagnosis of acute pancreatitis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

is confirmed by medical history and conducting physical examinations which is by blood test and
for the digestive enzymes present in the pancreas.
The woman is a patient for type 2 diabetes which affects the ways by which body will
process blood sugar. This disease is very common among the middle age and older individuals.
This is related to pancreas as it produces the hormone insulin. The risk factors associated with
type 2 diabtetes includes heart and blood vessel disease and high blood pressure. Moreover, she
is also going through hypertension which also increases the blood pressure. The differential
diagnosis for acute pancreatitis is overall differential for pain in the abdominal section of the
body. Acute pancreatitis is reversible in the inflammatory process of the pancreas and has
variety of causes which ranges from mild to severe and even life threatening. All of the
symptoms in the woman leads to acute pancreatitis (Gravito-Soares, & et.al., (2018)). There is an
intracellular and extracellular compartmentation caused due to the obstruction of the pancreatic
transport. Acute pancreatitis causes outflow with the pancreatic duct. Hypertension contributes to
disruption of pancreatic ductules. The diagnosis of the acute pancreatitis is based on criteria such
as abdominal pain and characteristic findings from abdominal imaging. It is important to have a
radiological evidence. CT scan provides accurate results and gives confirmation about the
diagnosis.
Pathology: Pathophysiology of acute pancreatitis is when there is loss of intracellular and extra
cellular compartmentation which is caused by the obstruction of pancreatic secretory transport
during the activation of pancreatic enzymes (Fan, & et.al., (2020)). The start of this disease is
when digestive enzymes become activated within the pancreas and irritation of these cells causes
inflammation within the pancreas. It damages the pancreas and can lead to chronic pancreatitis.
DIAGNOSIS
Acute pancreatitis is an inflammatory disorder within pancreas is one of the leading cause of
admission in hospital. Most of the patients acute pancreatitis experience pain in the abdomen
which is known to radiate backwards. This swift in pain is increased in intensity within 30
minutes and is associated with nausea and vomiting. The diagnosis of acute pancreatitis is based
on some criteria such as abdominal pain which is consistent with the acute pancreatitis. The
serum amylase is three times greater than the normal upper limit is also a cause of concern for
this problem (Van DIjk, and et.al., (2017)). This is a most common gastrointestinal cause for
for the digestive enzymes present in the pancreas.
The woman is a patient for type 2 diabetes which affects the ways by which body will
process blood sugar. This disease is very common among the middle age and older individuals.
This is related to pancreas as it produces the hormone insulin. The risk factors associated with
type 2 diabtetes includes heart and blood vessel disease and high blood pressure. Moreover, she
is also going through hypertension which also increases the blood pressure. The differential
diagnosis for acute pancreatitis is overall differential for pain in the abdominal section of the
body. Acute pancreatitis is reversible in the inflammatory process of the pancreas and has
variety of causes which ranges from mild to severe and even life threatening. All of the
symptoms in the woman leads to acute pancreatitis (Gravito-Soares, & et.al., (2018)). There is an
intracellular and extracellular compartmentation caused due to the obstruction of the pancreatic
transport. Acute pancreatitis causes outflow with the pancreatic duct. Hypertension contributes to
disruption of pancreatic ductules. The diagnosis of the acute pancreatitis is based on criteria such
as abdominal pain and characteristic findings from abdominal imaging. It is important to have a
radiological evidence. CT scan provides accurate results and gives confirmation about the
diagnosis.
Pathology: Pathophysiology of acute pancreatitis is when there is loss of intracellular and extra
cellular compartmentation which is caused by the obstruction of pancreatic secretory transport
during the activation of pancreatic enzymes (Fan, & et.al., (2020)). The start of this disease is
when digestive enzymes become activated within the pancreas and irritation of these cells causes
inflammation within the pancreas. It damages the pancreas and can lead to chronic pancreatitis.
DIAGNOSIS
Acute pancreatitis is an inflammatory disorder within pancreas is one of the leading cause of
admission in hospital. Most of the patients acute pancreatitis experience pain in the abdomen
which is known to radiate backwards. This swift in pain is increased in intensity within 30
minutes and is associated with nausea and vomiting. The diagnosis of acute pancreatitis is based
on some criteria such as abdominal pain which is consistent with the acute pancreatitis. The
serum amylase is three times greater than the normal upper limit is also a cause of concern for
this problem (Van DIjk, and et.al., (2017)). This is a most common gastrointestinal cause for
hospitalization in the country. BMI score for a healthy middle aged woman is supposed to be
between 18.5 to 24.9. In this case the woman is having a BMI of 31 and this score above 30 is
considered to be indicating obesity. The patient is overweight that makes a risk factor for the
having acute pancreatitis. Severe cases of acute pancreatitis are much more frequent in the obese
patients. Patients with obese health conditions will develop systemic and local complications for
acute pancreatitis to occur more frequently. Acute pancreatitis is confirmed from the medical
history and physical examination which is by blood test for the digestive enzymes of the
pancreas. The lipase level because of acute pancreatitis is increased 3 times than the normal
level. The ideal levels for blood pressure are considered to be between 90/60mmhg and
120/80mmhg. The woman in the case study is having blood pressure of 100/60mmhg which is
low and also termed as hypotension (Zhao, & et.al., (2018)). This blood pressure is low because
the damage of the pancreas may permit the activated enzymes to enter the blood stream which
causes the blood pressure to go low. Moreover, the part of pancreas which dies leads to escape
the blood fluids which occur in the abdominal cavity, this decr4eases the blood volume and
results in great drop in the blood pressure.
Pulse rate of healthy adults is ranged from 60 to 100 beats per minute. However, this can
fluctuate and may increase during the time of exercise or some illness. Heart rate of 110 beats
per minute is a sign of sinus tachycardia (Chatila, Bilal, & Guturu, (2019)). Acute pancreatitis
patients are tend to look sick and have fast pulse rate which is ranged between 100- 140 beats per
minute which is followed by rapid breathing caused due to the inflammation and accumulation of
the fluid in the chest cavity. Moreover, acute pancreatitis can cause condition of shock where
several blood and fluid loss leave the heart making it unable to pump enough blood to the body.
Tachycardia and hypertension are the results caused from sequestration fluid in the pancreatic
bed in acute pancreatitis.
Patients having the acute pancreatitis have severe pain with radiation at the back. This
pain is characterised as being constant and becomes worse when the patient is supine. This
discomfort might minimise when lying in the foetal position. A heavy meal or a lot of drinking
can lead to increase the pain with the feeling of nausea and vomiting. The clinical diagnosis of
acute pancreatitis is difficult to make and can be missed by many patients. Diagnosis can be also
be made with the help of an autopsy report along with history and physical examination. The
severity of the acute pancreatitis can be determined by physical examination. There will be signs
between 18.5 to 24.9. In this case the woman is having a BMI of 31 and this score above 30 is
considered to be indicating obesity. The patient is overweight that makes a risk factor for the
having acute pancreatitis. Severe cases of acute pancreatitis are much more frequent in the obese
patients. Patients with obese health conditions will develop systemic and local complications for
acute pancreatitis to occur more frequently. Acute pancreatitis is confirmed from the medical
history and physical examination which is by blood test for the digestive enzymes of the
pancreas. The lipase level because of acute pancreatitis is increased 3 times than the normal
level. The ideal levels for blood pressure are considered to be between 90/60mmhg and
120/80mmhg. The woman in the case study is having blood pressure of 100/60mmhg which is
low and also termed as hypotension (Zhao, & et.al., (2018)). This blood pressure is low because
the damage of the pancreas may permit the activated enzymes to enter the blood stream which
causes the blood pressure to go low. Moreover, the part of pancreas which dies leads to escape
the blood fluids which occur in the abdominal cavity, this decr4eases the blood volume and
results in great drop in the blood pressure.
Pulse rate of healthy adults is ranged from 60 to 100 beats per minute. However, this can
fluctuate and may increase during the time of exercise or some illness. Heart rate of 110 beats
per minute is a sign of sinus tachycardia (Chatila, Bilal, & Guturu, (2019)). Acute pancreatitis
patients are tend to look sick and have fast pulse rate which is ranged between 100- 140 beats per
minute which is followed by rapid breathing caused due to the inflammation and accumulation of
the fluid in the chest cavity. Moreover, acute pancreatitis can cause condition of shock where
several blood and fluid loss leave the heart making it unable to pump enough blood to the body.
Tachycardia and hypertension are the results caused from sequestration fluid in the pancreatic
bed in acute pancreatitis.
Patients having the acute pancreatitis have severe pain with radiation at the back. This
pain is characterised as being constant and becomes worse when the patient is supine. This
discomfort might minimise when lying in the foetal position. A heavy meal or a lot of drinking
can lead to increase the pain with the feeling of nausea and vomiting. The clinical diagnosis of
acute pancreatitis is difficult to make and can be missed by many patients. Diagnosis can be also
be made with the help of an autopsy report along with history and physical examination. The
severity of the acute pancreatitis can be determined by physical examination. There will be signs
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
of abdominal distension followed by the epigastric pain and tenderness in left- upper positions
(Habtezion, Gukovskaya, & Pandol, (2019)). Other signs include fever which is seen in this
woman as her body temperature is 38.5°C while the normal body temperature is 37°C. She is
having a low grade fever. Moreover, signs such as tachycardia and jaundice where the patient is
often feels restless and dehydrated. The laboratory diagnosis includes checking the serum
amylase levels of the patient which can vary as it depends on the severity of acute pancreatitis.
The level of serum amylase levels are starts to increase within 2 to 12 hours after the symptoms
takes place and this starts to peak within 12 to 72 hours (Pan, & et.al., (2017)). These symptoms
return within 1 week. Measuring the serum amylase is very common method to diagnose acute
pancreatitis. It is performed quickly and the results are easily obtained along with being an
inexpensive method. In addition to this, lipase levels are tested in the laboratory examination.
The level of lipase peaks with this disease which if followed by its decrease within 8 to 14 days.
Based on the sensitivities, elevation in the typsin level is used for detecting acute pancreatitis as
this test is very accurate indicator for the same.
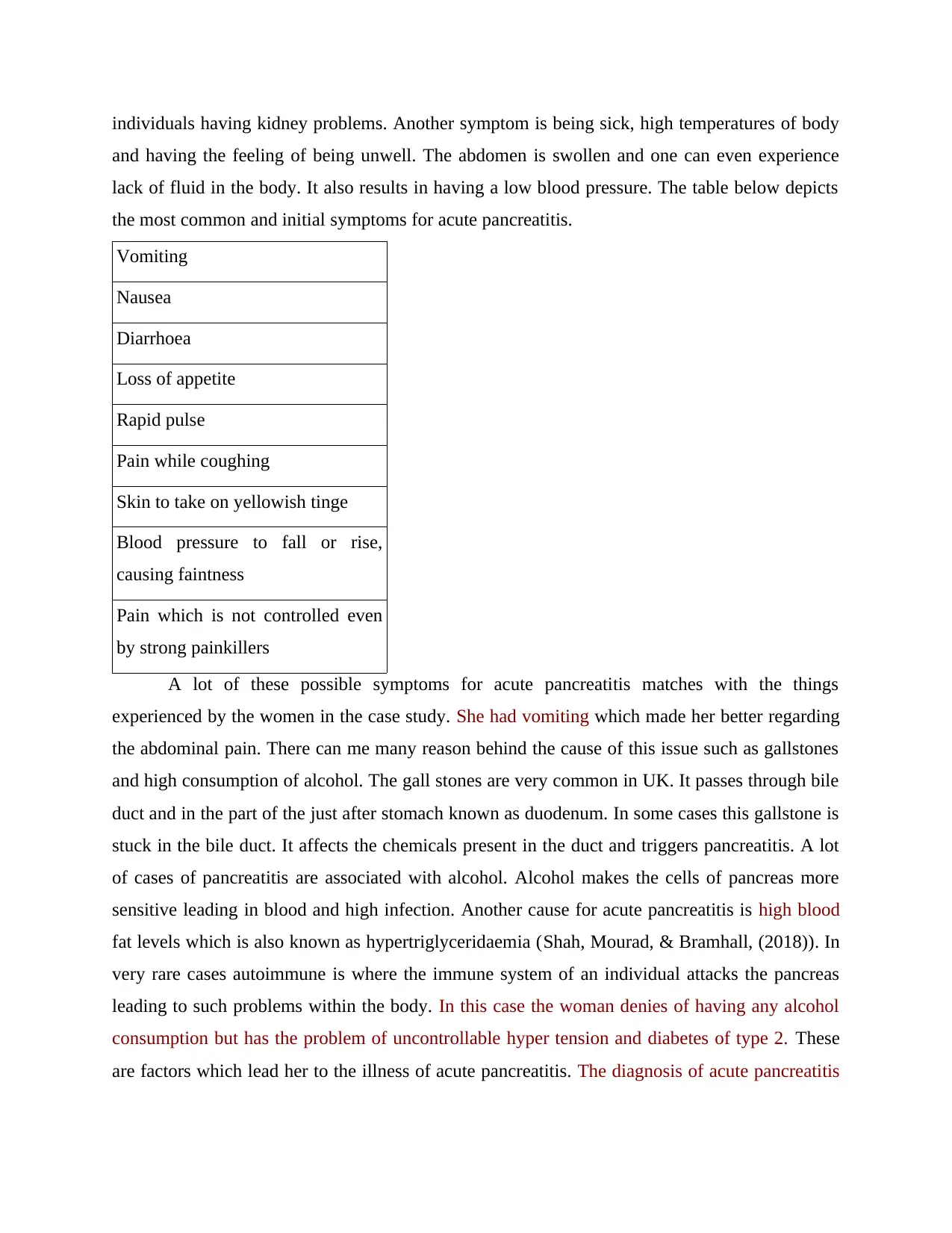
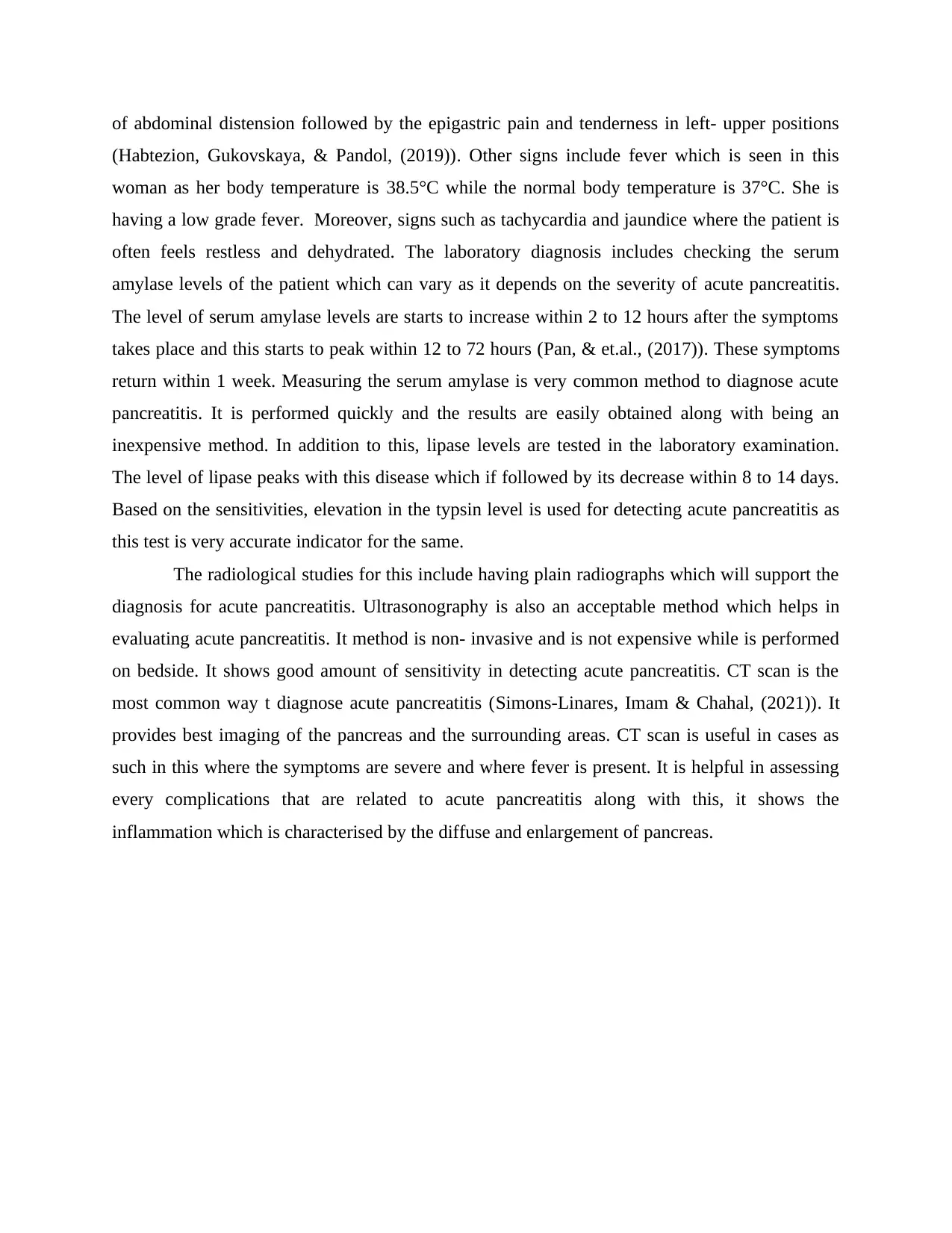
The radiological studies for this include having plain radiographs which will support the
diagnosis for acute pancreatitis. Ultrasonography is also an acceptable method which helps in
evaluating acute pancreatitis. It method is non- invasive and is not expensive while is performed
on bedside. It shows good amount of sensitivity in detecting acute pancreatitis. CT scan is the
most common way t diagnose acute pancreatitis (Simons-Linares, Imam & Chahal, (2021)). It
provides best imaging of the pancreas and the surrounding areas. CT scan is useful in cases as
such in this where the symptoms are severe and where fever is present. It is helpful in assessing
every complications that are related to acute pancreatitis along with this, it shows the
inflammation which is characterised by the diffuse and enlargement of pancreas.
(Habtezion, Gukovskaya, & Pandol, (2019)). Other signs include fever which is seen in this
woman as her body temperature is 38.5°C while the normal body temperature is 37°C. She is
having a low grade fever. Moreover, signs such as tachycardia and jaundice where the patient is
often feels restless and dehydrated. The laboratory diagnosis includes checking the serum
amylase levels of the patient which can vary as it depends on the severity of acute pancreatitis.
The level of serum amylase levels are starts to increase within 2 to 12 hours after the symptoms
takes place and this starts to peak within 12 to 72 hours (Pan, & et.al., (2017)). These symptoms
return within 1 week. Measuring the serum amylase is very common method to diagnose acute
pancreatitis. It is performed quickly and the results are easily obtained along with being an
inexpensive method. In addition to this, lipase levels are tested in the laboratory examination.
The level of lipase peaks with this disease which if followed by its decrease within 8 to 14 days.
Based on the sensitivities, elevation in the typsin level is used for detecting acute pancreatitis as
this test is very accurate indicator for the same.
The radiological studies for this include having plain radiographs which will support the
diagnosis for acute pancreatitis. Ultrasonography is also an acceptable method which helps in
evaluating acute pancreatitis. It method is non- invasive and is not expensive while is performed
on bedside. It shows good amount of sensitivity in detecting acute pancreatitis. CT scan is the
most common way t diagnose acute pancreatitis (Simons-Linares, Imam & Chahal, (2021)). It
provides best imaging of the pancreas and the surrounding areas. CT scan is useful in cases as
such in this where the symptoms are severe and where fever is present. It is helpful in assessing
every complications that are related to acute pancreatitis along with this, it shows the
inflammation which is characterised by the diffuse and enlargement of pancreas.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
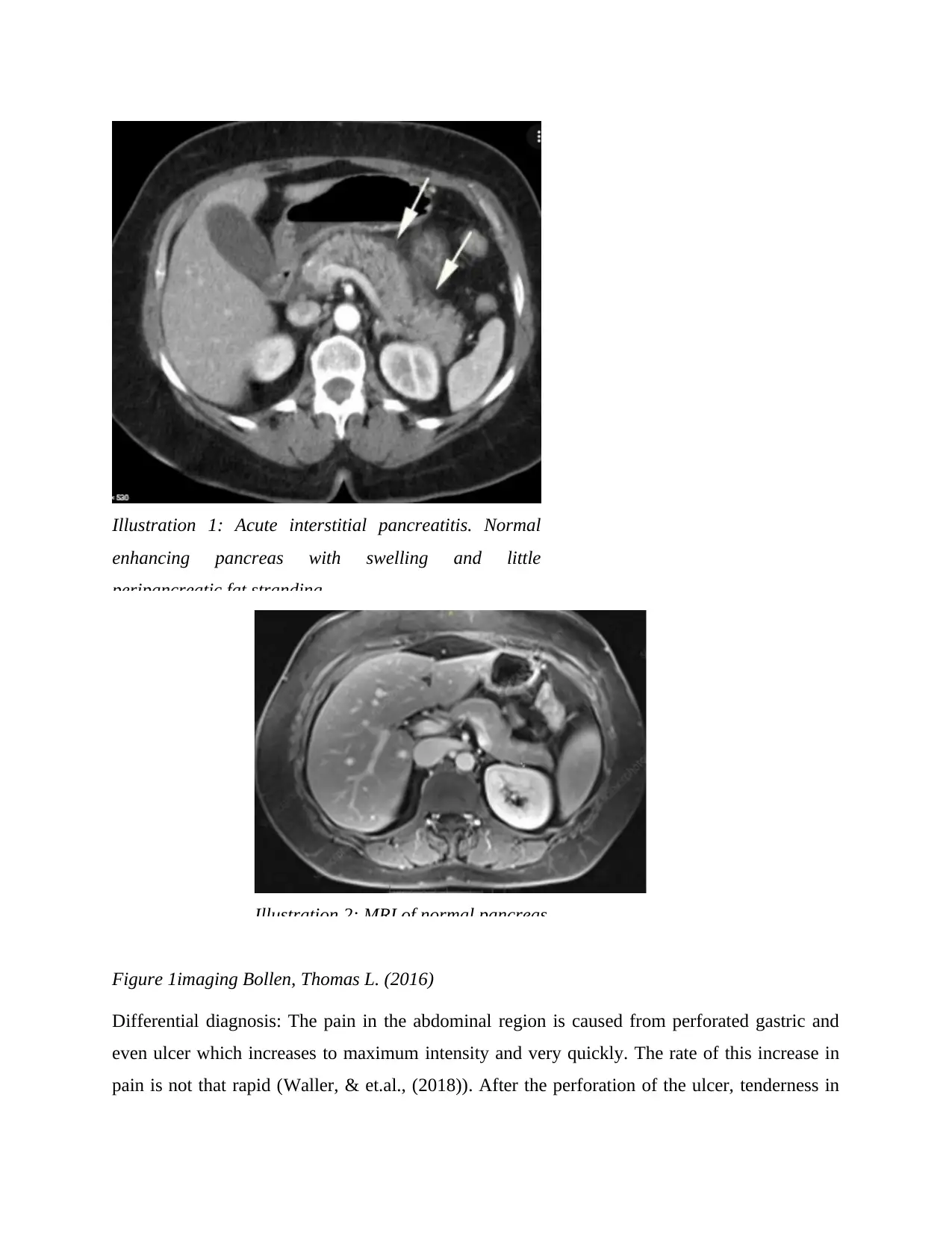
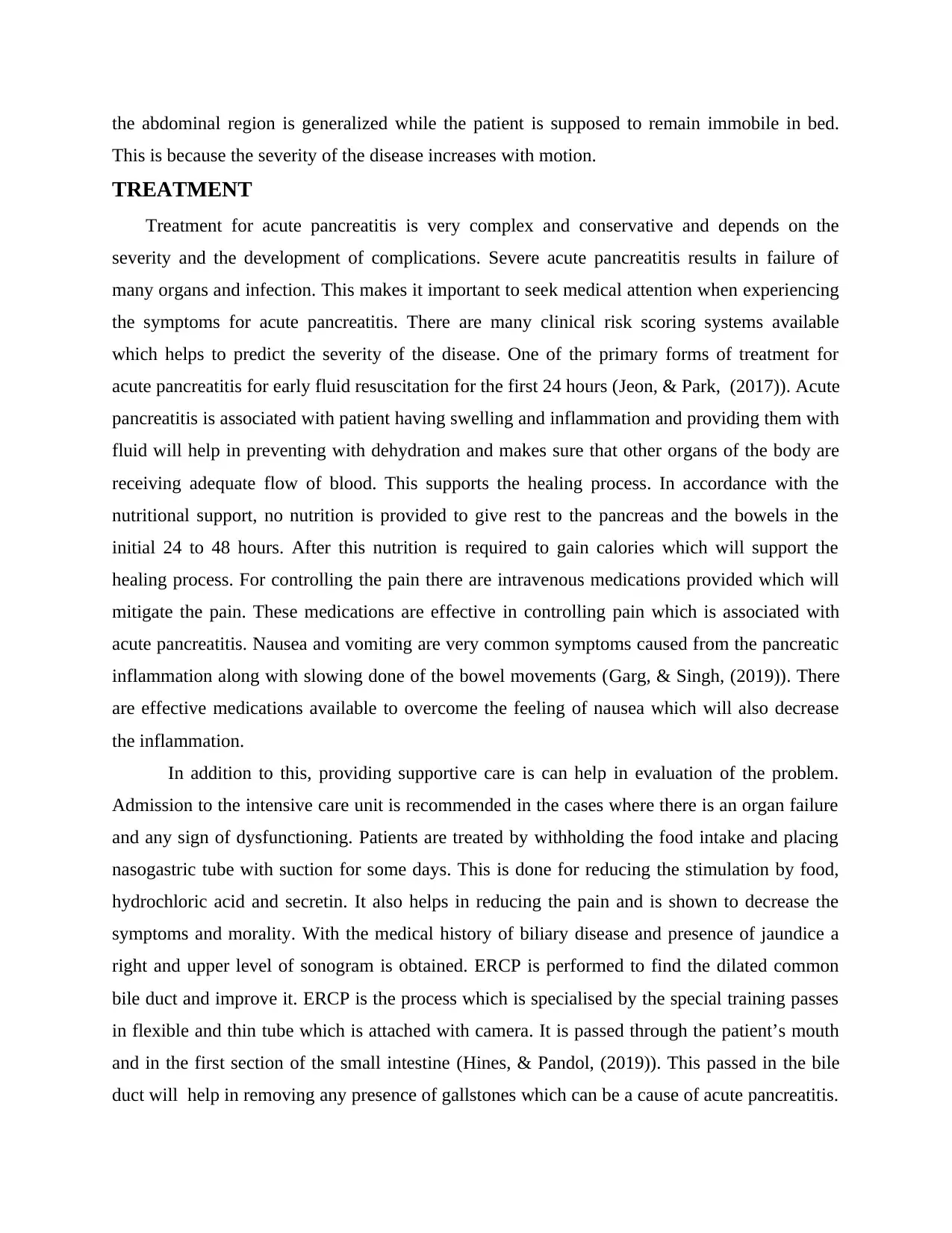
Illustration 1: Acute interstitial pancreatitis. Normal
enhancing pancreas with swelling and little
peripancreatic fat stranding.
Figure 1imaging Bollen, Thomas L. (2016)
Differential diagnosis: The pain in the abdominal region is caused from perforated gastric and
even ulcer which increases to maximum intensity and very quickly. The rate of this increase in
pain is not that rapid (Waller, & et.al., (2018)). After the perforation of the ulcer, tenderness in
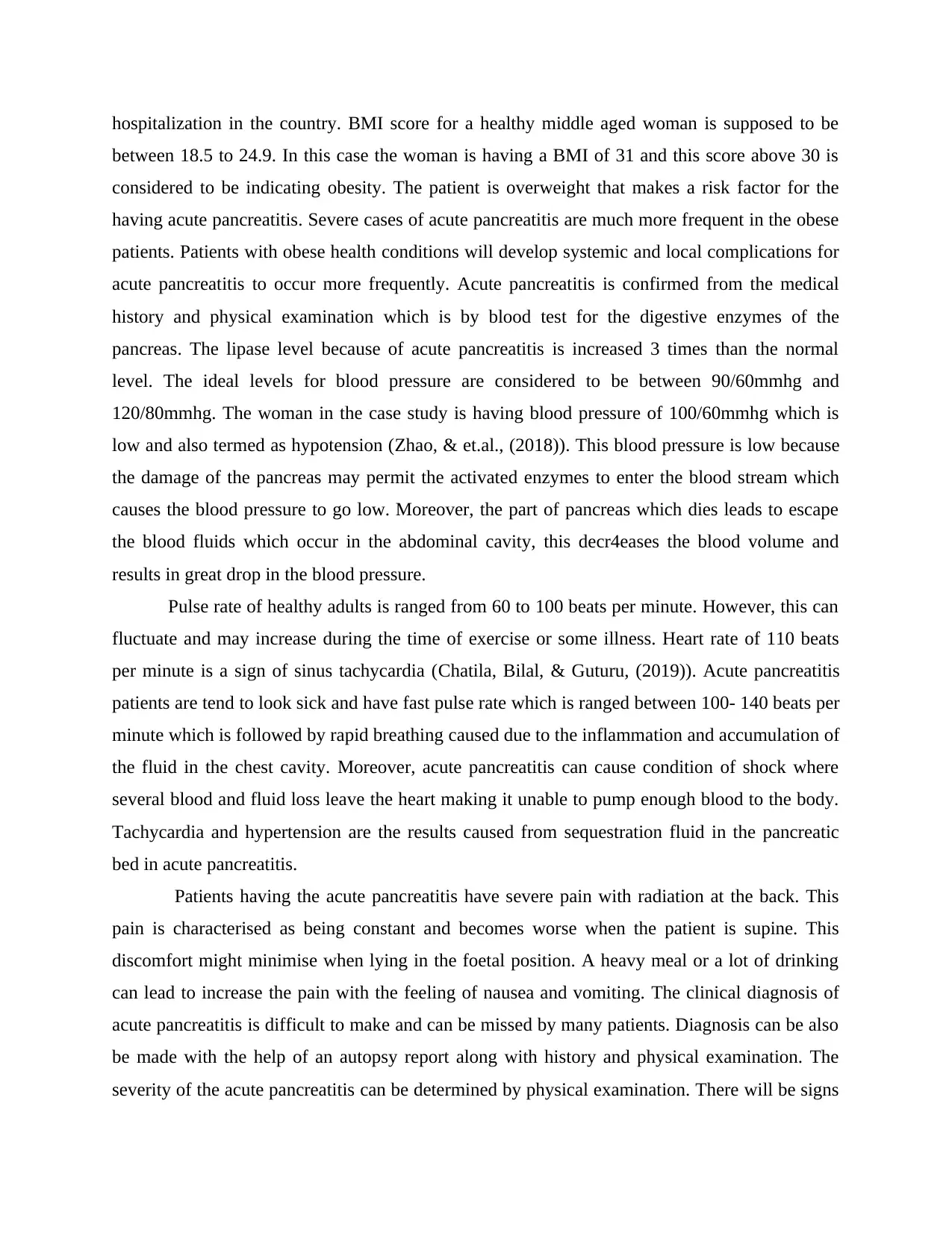
Illustration 2: MRI of normal pancreas
enhancing pancreas with swelling and little
peripancreatic fat stranding.
Figure 1imaging Bollen, Thomas L. (2016)
Differential diagnosis: The pain in the abdominal region is caused from perforated gastric and
even ulcer which increases to maximum intensity and very quickly. The rate of this increase in
pain is not that rapid (Waller, & et.al., (2018)). After the perforation of the ulcer, tenderness in
Illustration 2: MRI of normal pancreas
the abdominal region is generalized while the patient is supposed to remain immobile in bed.
This is because the severity of the disease increases with motion.
TREATMENT
Treatment for acute pancreatitis is very complex and conservative and depends on the
severity and the development of complications. Severe acute pancreatitis results in failure of
many organs and infection. This makes it important to seek medical attention when experiencing
the symptoms for acute pancreatitis. There are many clinical risk scoring systems available
which helps to predict the severity of the disease. One of the primary forms of treatment for
acute pancreatitis for early fluid resuscitation for the first 24 hours (Jeon, & Park, (2017)). Acute
pancreatitis is associated with patient having swelling and inflammation and providing them with
fluid will help in preventing with dehydration and makes sure that other organs of the body are
receiving adequate flow of blood. This supports the healing process. In accordance with the
nutritional support, no nutrition is provided to give rest to the pancreas and the bowels in the
initial 24 to 48 hours. After this nutrition is required to gain calories which will support the
healing process. For controlling the pain there are intravenous medications provided which will
mitigate the pain. These medications are effective in controlling pain which is associated with
acute pancreatitis. Nausea and vomiting are very common symptoms caused from the pancreatic
inflammation along with slowing done of the bowel movements (Garg, & Singh, (2019)). There
are effective medications available to overcome the feeling of nausea which will also decrease
the inflammation.
In addition to this, providing supportive care is can help in evaluation of the problem.
Admission to the intensive care unit is recommended in the cases where there is an organ failure
and any sign of dysfunctioning. Patients are treated by withholding the food intake and placing
nasogastric tube with suction for some days. This is done for reducing the stimulation by food,
hydrochloric acid and secretin. It also helps in reducing the pain and is shown to decrease the
symptoms and morality. With the medical history of biliary disease and presence of jaundice a
right and upper level of sonogram is obtained. ERCP is performed to find the dilated common
bile duct and improve it. ERCP is the process which is specialised by the special training passes
in flexible and thin tube which is attached with camera. It is passed through the patient’s mouth
and in the first section of the small intestine (Hines, & Pandol, (2019)). This passed in the bile
duct will help in removing any presence of gallstones which can be a cause of acute pancreatitis.
This is because the severity of the disease increases with motion.
TREATMENT
Treatment for acute pancreatitis is very complex and conservative and depends on the
severity and the development of complications. Severe acute pancreatitis results in failure of
many organs and infection. This makes it important to seek medical attention when experiencing
the symptoms for acute pancreatitis. There are many clinical risk scoring systems available
which helps to predict the severity of the disease. One of the primary forms of treatment for
acute pancreatitis for early fluid resuscitation for the first 24 hours (Jeon, & Park, (2017)). Acute
pancreatitis is associated with patient having swelling and inflammation and providing them with
fluid will help in preventing with dehydration and makes sure that other organs of the body are
receiving adequate flow of blood. This supports the healing process. In accordance with the
nutritional support, no nutrition is provided to give rest to the pancreas and the bowels in the
initial 24 to 48 hours. After this nutrition is required to gain calories which will support the
healing process. For controlling the pain there are intravenous medications provided which will
mitigate the pain. These medications are effective in controlling pain which is associated with
acute pancreatitis. Nausea and vomiting are very common symptoms caused from the pancreatic
inflammation along with slowing done of the bowel movements (Garg, & Singh, (2019)). There
are effective medications available to overcome the feeling of nausea which will also decrease
the inflammation.
In addition to this, providing supportive care is can help in evaluation of the problem.
Admission to the intensive care unit is recommended in the cases where there is an organ failure
and any sign of dysfunctioning. Patients are treated by withholding the food intake and placing
nasogastric tube with suction for some days. This is done for reducing the stimulation by food,
hydrochloric acid and secretin. It also helps in reducing the pain and is shown to decrease the
symptoms and morality. With the medical history of biliary disease and presence of jaundice a
right and upper level of sonogram is obtained. ERCP is performed to find the dilated common
bile duct and improve it. ERCP is the process which is specialised by the special training passes
in flexible and thin tube which is attached with camera. It is passed through the patient’s mouth
and in the first section of the small intestine (Hines, & Pandol, (2019)). This passed in the bile
duct will help in removing any presence of gallstones which can be a cause of acute pancreatitis.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Special catheter is passed which helps the pancreas to heal. Formation of acute pancreatitis can
be associated with oxidative stress.
Free radical activity and oxidative stress are high in the blood for the patients with acute
pancreatitis. Antioxidants can help in managing acute pancreatitis and is the traditional therapy.
Antioxidants which contains the vitamin C, E, selenium and methionine is used in the overall
medical management. Antioxidants produces many benefits in managing acute pancreatitis.
Antibiotics are helpful in decreasing the morality and severity of the complications associated
with this disease. It controls the patients undergoing the surgical procedures that can contribute
in having infection. They show promising results and removes any toxic factors. Treatment for
acute pancreatitis also includes treating the dehydration which is one of the causes from it. This
is done by swallowing fluids by mouth. There is no specific treatment that will take the issue of
inflammation away. Strong painkillers by injecting them is used to ease the pain. A tube is
passed down from the nose to the stomach to stick the out the fluid present in the stomach
(Garber, & et.al. (2018)). This is useful to give relief from vomiting. Nasogastric tube is passed
down to feed the patient as they will not be able to eat properly. Intensive care treatment is
provided in severe cases which includes monitoring closely in the intensive care unit. Surgery is
performed in the cases that involves to remove the infected and damaged tissue near pancreas.
Some of the complication related to acute pancreatitis can even lead to death which occurs
within 2 weeks from the start of pain. These complications can even lead to have organ failure
which includes cardiovascular, pulmonary and renal systems (Guda, & et.al., (2018)).
Complication in the cardiovascular areas can lead to bleeding in the retroperitoneal space with
decrease in the vascular resistance. Insufficiency in the pulmonary is ranged between mild to life
threatening with adult respiratory distress syndrome. CT scan is very helpful to detect late
complication due to acute pancreatitis which occurs after three weeks. Most of the individuals
get better within a week however, in the severe cases its takes a longer time to overcome its
complications.
The treatment of acute pancreatitis requires the need for hospitalisation to stabilise the patient.
The patient is made to stop eating for a couple of days when admitted in hospital. This is done to
provide a chance for the pancreas to recover. However, in some cases, the patient is allowed to
eat as soon as they can tolerate the food that will help them heal their pancreas. It will also
improve the inflation present in the pancreas while mitigating the painful symptoms. Drinking
be associated with oxidative stress.
Free radical activity and oxidative stress are high in the blood for the patients with acute
pancreatitis. Antioxidants can help in managing acute pancreatitis and is the traditional therapy.
Antioxidants which contains the vitamin C, E, selenium and methionine is used in the overall
medical management. Antioxidants produces many benefits in managing acute pancreatitis.
Antibiotics are helpful in decreasing the morality and severity of the complications associated
with this disease. It controls the patients undergoing the surgical procedures that can contribute
in having infection. They show promising results and removes any toxic factors. Treatment for
acute pancreatitis also includes treating the dehydration which is one of the causes from it. This
is done by swallowing fluids by mouth. There is no specific treatment that will take the issue of
inflammation away. Strong painkillers by injecting them is used to ease the pain. A tube is
passed down from the nose to the stomach to stick the out the fluid present in the stomach
(Garber, & et.al. (2018)). This is useful to give relief from vomiting. Nasogastric tube is passed
down to feed the patient as they will not be able to eat properly. Intensive care treatment is
provided in severe cases which includes monitoring closely in the intensive care unit. Surgery is
performed in the cases that involves to remove the infected and damaged tissue near pancreas.
Some of the complication related to acute pancreatitis can even lead to death which occurs
within 2 weeks from the start of pain. These complications can even lead to have organ failure
which includes cardiovascular, pulmonary and renal systems (Guda, & et.al., (2018)).
Complication in the cardiovascular areas can lead to bleeding in the retroperitoneal space with
decrease in the vascular resistance. Insufficiency in the pulmonary is ranged between mild to life
threatening with adult respiratory distress syndrome. CT scan is very helpful to detect late
complication due to acute pancreatitis which occurs after three weeks. Most of the individuals
get better within a week however, in the severe cases its takes a longer time to overcome its
complications.
The treatment of acute pancreatitis requires the need for hospitalisation to stabilise the patient.
The patient is made to stop eating for a couple of days when admitted in hospital. This is done to
provide a chance for the pancreas to recover. However, in some cases, the patient is allowed to
eat as soon as they can tolerate the food that will help them heal their pancreas. It will also
improve the inflation present in the pancreas while mitigating the painful symptoms. Drinking
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

clear liquids and eating bland foods is advised by which slowly they can go back to their normal
diet. In the case where the pain is still persistent, it is recommended that feeding is done with the
help of tube to give nutrition to the patient. To mitigate the pain, pain killer medications are
given that will help in controlling the pain. The body of patient in this case requires energy and
fluids to repair the pancreas. This will lead to patient being dehydrated therefore, some extra
fluids are provided through veins in the arm and in hospital setting.
CONCLUSION
Acute pancreatitis is an illness which can be mild or even severe which can be life
threatening. It is important to have a rapid diagnosis of the problem with some specific
laboratory testing radiologic tests is very important. The severe sign of this disease includes
clinical deterioration after admission in the hospital where the surgeon is often recommended.
Appropriate care is required and in some cases even with that it the morality rate is high. Serum
lipase is used to establish the diagnosis of acute pancreatitis and increases its awareness. CT scan
for the abdominal region is useful for such patients. Acute pancreatitis usually resolves in few
days but in some cases patient is admitted to the hospital depending on the severity of its
symptoms. There are many complication of this disease such as obstruction of bile duct, leakage
from this duct and even rupture causing some infection. It can cause damage to pancreas and
multiple organ failures. Diagnosis of Acute pancreatitis is done by severe physical and laboratory
tests along with imaging process such as CT scan. In this case it is first done by the laboratory
tests followed by the imaging process.
diet. In the case where the pain is still persistent, it is recommended that feeding is done with the
help of tube to give nutrition to the patient. To mitigate the pain, pain killer medications are
given that will help in controlling the pain. The body of patient in this case requires energy and
fluids to repair the pancreas. This will lead to patient being dehydrated therefore, some extra
fluids are provided through veins in the arm and in hospital setting.
CONCLUSION
Acute pancreatitis is an illness which can be mild or even severe which can be life
threatening. It is important to have a rapid diagnosis of the problem with some specific
laboratory testing radiologic tests is very important. The severe sign of this disease includes
clinical deterioration after admission in the hospital where the surgeon is often recommended.
Appropriate care is required and in some cases even with that it the morality rate is high. Serum
lipase is used to establish the diagnosis of acute pancreatitis and increases its awareness. CT scan
for the abdominal region is useful for such patients. Acute pancreatitis usually resolves in few
days but in some cases patient is admitted to the hospital depending on the severity of its
symptoms. There are many complication of this disease such as obstruction of bile duct, leakage
from this duct and even rupture causing some infection. It can cause damage to pancreas and
multiple organ failures. Diagnosis of Acute pancreatitis is done by severe physical and laboratory
tests along with imaging process such as CT scan. In this case it is first done by the laboratory
tests followed by the imaging process.
REFERENCES
Books and Journals
Chatila, A. T., Bilal, M., & Guturu, P. (2019). Evaluation and management of acute
pancreatitis. World journal of clinical cases, 7(9), 1006.
Fan, & et.al., (2020). Identification of acute pancreatitis-related genes and pathways by
integrated bioinformatics analysis. Digestive diseases and sciences, 65(6), 1720-1732.
Garber, & et.al. (2018). Mechanisms and management of acute pancreatitis. Gastroenterology
research and practice, 2018.
Garg, P. K., & Singh, V. P. (2019). Organ failure due to systemic injury in acute
pancreatitis. Gastroenterology, 156(7), 2008-2023.
Gravito-Soares, & et.al., (2018). Red cell distribution width and red cell distribution width to
total serum calcium ratio as major predictors of severity and mortality in acute
pancreatitis. BMC gastroenterology, 18(1), 1-9.
Guda, & et.al., (2018). Recurrent acute pancreatitis: international state-of-the-science conference
with recommendations. Pancreas, 47(6), 653-666.
Habtezion, A., Gukovskaya, A. S., & Pandol, S. J. (2019). Acute pancreatitis: a multifaceted set
of organelle and cellular interactions. Gastroenterology, 156(7), 1941-1950.
Hines, O. J., & Pandol, S. J. (2019). Management of severe acute pancreatitis. Bmj, 367.
Jeon, T. J., & Park, J. Y. (2017). Clinical significance of the neutrophil-lymphocyte ratio as an
early predictive marker for adverse outcomes in patients with acute pancreatitis. World
journal of gastroenterology, 23(21), 3883.
Karjula, & et.al., (2019). Long-term outcome and causes of death for working-age patients
hospitalized due to acute pancreatitis with a median follow-up of 10 years. Annals of
surgery, 269(5), 932-936.
Lee, P. J., & Papachristou, G. I. (2019). New insights into acute pancreatitis. Nature Reviews
Gastroenterology & Hepatology, 16(8), 479-496. Shah, A. P., Mourad, M. M., &
Bramhall, S. R. (2018). Acute pancreatitis: current perspectives on diagnosis and
management. Journal of inflammation research, 11, 77.
Ouyang, & et.al., (2020). The global, regional, and national burden of pancreatitis in 195
countries and territories, 1990–2017: A systematic analysis for the Global Burden of
Disease Study 2017. BMC medicine, 18(1), 1-13.
Pan, & et.al., (2017). Recent advances on nutrition in treatment of acute pancreatitis. Frontiers in
immunology, 8, 762.
Shah, A. P., Mourad, M. M., & Bramhall, S. R. (2018). Acute pancreatitis: current perspectives
on diagnosis and management. Journal of inflammation research, 11, 77.
Simons-Linares, C. R., Imam, Z., & Chahal, P. (2021). Viral-Attributed acute pancreatitis: a
systematic review. Digestive Diseases and Sciences, 66(7), 2162-2172.
Van DIjk, and et.al., (2017). Acute pancreatitis: recent advances through randomised
trials. Gut, 66(11), 2024-2032.
Waller, & et.al., (2018). Acute pancreatitis: updates for emergency clinicians. The Journal of
emergency medicine, 55(6), 769-779.
Ye & et.al., (2017). Building and verifying a severity prediction model of acute pancreatitis (AP)
based on BISAP, MEWS and routine test indexes. Clinics and research in hepatology and
gastroenterology, 41(5), 585-591.
Books and Journals
Chatila, A. T., Bilal, M., & Guturu, P. (2019). Evaluation and management of acute
pancreatitis. World journal of clinical cases, 7(9), 1006.
Fan, & et.al., (2020). Identification of acute pancreatitis-related genes and pathways by
integrated bioinformatics analysis. Digestive diseases and sciences, 65(6), 1720-1732.
Garber, & et.al. (2018). Mechanisms and management of acute pancreatitis. Gastroenterology
research and practice, 2018.
Garg, P. K., & Singh, V. P. (2019). Organ failure due to systemic injury in acute
pancreatitis. Gastroenterology, 156(7), 2008-2023.
Gravito-Soares, & et.al., (2018). Red cell distribution width and red cell distribution width to
total serum calcium ratio as major predictors of severity and mortality in acute
pancreatitis. BMC gastroenterology, 18(1), 1-9.
Guda, & et.al., (2018). Recurrent acute pancreatitis: international state-of-the-science conference
with recommendations. Pancreas, 47(6), 653-666.
Habtezion, A., Gukovskaya, A. S., & Pandol, S. J. (2019). Acute pancreatitis: a multifaceted set
of organelle and cellular interactions. Gastroenterology, 156(7), 1941-1950.
Hines, O. J., & Pandol, S. J. (2019). Management of severe acute pancreatitis. Bmj, 367.
Jeon, T. J., & Park, J. Y. (2017). Clinical significance of the neutrophil-lymphocyte ratio as an
early predictive marker for adverse outcomes in patients with acute pancreatitis. World
journal of gastroenterology, 23(21), 3883.
Karjula, & et.al., (2019). Long-term outcome and causes of death for working-age patients
hospitalized due to acute pancreatitis with a median follow-up of 10 years. Annals of
surgery, 269(5), 932-936.
Lee, P. J., & Papachristou, G. I. (2019). New insights into acute pancreatitis. Nature Reviews
Gastroenterology & Hepatology, 16(8), 479-496. Shah, A. P., Mourad, M. M., &
Bramhall, S. R. (2018). Acute pancreatitis: current perspectives on diagnosis and
management. Journal of inflammation research, 11, 77.
Ouyang, & et.al., (2020). The global, regional, and national burden of pancreatitis in 195
countries and territories, 1990–2017: A systematic analysis for the Global Burden of
Disease Study 2017. BMC medicine, 18(1), 1-13.
Pan, & et.al., (2017). Recent advances on nutrition in treatment of acute pancreatitis. Frontiers in
immunology, 8, 762.
Shah, A. P., Mourad, M. M., & Bramhall, S. R. (2018). Acute pancreatitis: current perspectives
on diagnosis and management. Journal of inflammation research, 11, 77.
Simons-Linares, C. R., Imam, Z., & Chahal, P. (2021). Viral-Attributed acute pancreatitis: a
systematic review. Digestive Diseases and Sciences, 66(7), 2162-2172.
Van DIjk, and et.al., (2017). Acute pancreatitis: recent advances through randomised
trials. Gut, 66(11), 2024-2032.
Waller, & et.al., (2018). Acute pancreatitis: updates for emergency clinicians. The Journal of
emergency medicine, 55(6), 769-779.
Ye & et.al., (2017). Building and verifying a severity prediction model of acute pancreatitis (AP)
based on BISAP, MEWS and routine test indexes. Clinics and research in hepatology and
gastroenterology, 41(5), 585-591.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





