Exploring Pathophysiology and Nursing Care for Acute Severe Asthma
VerifiedAdded on 2023/06/04
|9
|2116
|88
Case Study
AI Summary
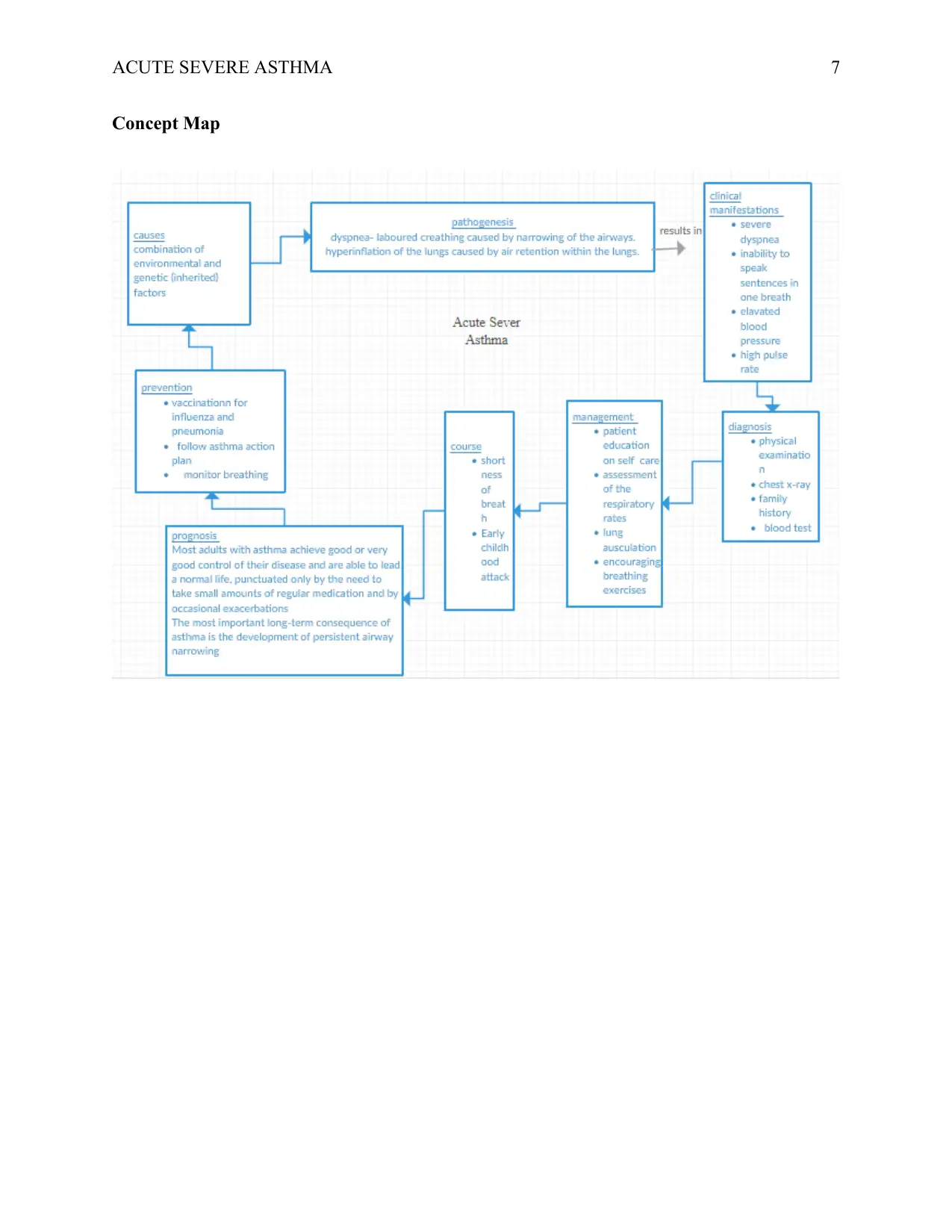
This case study provides a comprehensive analysis of acute severe asthma, focusing on its pathogenesis, clinical manifestations, and nursing management. It begins by explaining the underlying causes and mechanisms of asthma, particularly in the context of Jackson Smith's case, highlighting factors like early onset, environmental triggers, and physiological responses such as airway narrowing, mucus production, and reduced oxygen saturation. The study then delves into specific clinical observations, including dyspnea, increased respiratory rate, elevated blood pressure, tachycardia, and abnormal blood gas values, linking these to the pathophysiology of the condition. Furthermore, the case study outlines key nursing strategies, such as addressing ineffective airway clearance and promoting health-seeking behaviors related to asthma prevention, detailing specific interventions and their rationales. Finally, it discusses the mechanism of action and nursing implications of commonly used drugs like nebulized salbutamol, ipratropium bromide, and IV hydrocortisone, emphasizing the importance of patient education and monitoring for adverse effects. The case study concludes with a concept map visually summarizing the key aspects of acute severe asthma.

Running head: ACUTE SEVERE ASTHMA 1
Acute Severe Asthma
Name
Institution
Acute Severe Asthma
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE SEVERE ASTHMA 2
Question 1: Pathogenesis causing the presented clinical manifestation
Asthma can be described as having episodic symptoms and variable obstructions of the airflow
that may result from a spontaneous reaction to environmental exposures. Patients like Jackson
with asthmatic conditions usually experience exacerbations that may be triggered by viral
respiratory infections among other causes (Carlsen et al., 2010). Patients with this condition have
symptoms that may be difficult to control. The most common of these symptoms are wheezing,
cough, and dyspnea (Jackson, Sykes, Mallia & Johnston, 2011). The condition is further
characterized by hyper-responsiveness of the airways and variable obstruction of the airways.
From the presented scenario, we realize that Jackson Smith has a history of asthma that had been
diagnosed when he was still just two years old. This is an indication that there was an early onset
of this condition which may have been caused by situations such as pneumonia or parental
smoking (Bush & Saglani, 2010). Other factors that might have led to Jackson’s condition at
such a young could be low birth weight, frequent respiratory infections, and growing up in a low-
income environment among others.
On admission to the emergency, department observations are made regarding his condition. He is
said to be suffering from severe dyspnea and he cannot speak sentences in one breath.
Additionally, his respiratory rate is 32 beats per minute. These symptoms are as a result of the
airways narrowing, swelling and producing excess mucus (Kitulwatte, 2011). As a result,
breathing becomes difficult and coughing and wheezing could be triggered. His SPO2 on room
air is measured to be 90% which is an indication of a respiratory disease because normally,
SPO2 should range between 94% and 99%. This reduced level of SPO2 is as a result of the
constricted airways thus resulting in low oxygen saturation (Lommatzsch & Virchow, 2014).
Question 1: Pathogenesis causing the presented clinical manifestation
Asthma can be described as having episodic symptoms and variable obstructions of the airflow
that may result from a spontaneous reaction to environmental exposures. Patients like Jackson
with asthmatic conditions usually experience exacerbations that may be triggered by viral
respiratory infections among other causes (Carlsen et al., 2010). Patients with this condition have
symptoms that may be difficult to control. The most common of these symptoms are wheezing,
cough, and dyspnea (Jackson, Sykes, Mallia & Johnston, 2011). The condition is further
characterized by hyper-responsiveness of the airways and variable obstruction of the airways.
From the presented scenario, we realize that Jackson Smith has a history of asthma that had been
diagnosed when he was still just two years old. This is an indication that there was an early onset
of this condition which may have been caused by situations such as pneumonia or parental
smoking (Bush & Saglani, 2010). Other factors that might have led to Jackson’s condition at
such a young could be low birth weight, frequent respiratory infections, and growing up in a low-
income environment among others.
On admission to the emergency, department observations are made regarding his condition. He is
said to be suffering from severe dyspnea and he cannot speak sentences in one breath.
Additionally, his respiratory rate is 32 beats per minute. These symptoms are as a result of the
airways narrowing, swelling and producing excess mucus (Kitulwatte, 2011). As a result,
breathing becomes difficult and coughing and wheezing could be triggered. His SPO2 on room
air is measured to be 90% which is an indication of a respiratory disease because normally,
SPO2 should range between 94% and 99%. This reduced level of SPO2 is as a result of the
constricted airways thus resulting in low oxygen saturation (Lommatzsch & Virchow, 2014).
ACUTE SEVERE ASTHMA 3
His blood pressure is measured to be 150/85 mmHg which is way above the normal blood
pressure that normally is around 120/80 mmHg. Asthma is linked to cardiovascular diseases that
in most cases cause hypertension in adults. The increase in the blood pressure could be due to the
disturbance of the airways during a severe acute asthma that may lead to tachycardia (Marik,
2010). A pulse rate of 130 beats per minute further indicates the presence of tachycardia which
may be correlated with asthma.
When a lung auscultation was conducted, there was an observation of widespread wheezing and
diminished breath sounds. These observations are as a result of suppressed airways thus making
gaseous exchange difficult. From a chest x-ray, hyper-inflated lung fields were observed. These
result from damage to the lung tissues by the acute severe asthma that causes the lungs to
become less elastic. As a result, the expulsion of air from the lungs becomes difficult thus getting
trapped within the lungs. Hyperinflation of the lungs could lead to conditions such as shortness
of breath that is observed in the provided case and exercise intolerance among others. Patients
with asthma are unable to inhale or exhale properly. As a result, the lungs retain some air within
thus leading to hyperinflation.
Additionally, we can see from the assessment of Jackson Smith, we notice that his blood gas
values are not entirely normal. He has an arterial blood pH of 7.35, PaO2 of 60 mmHg PaCO2 of
50 mmHg, SaO2 of 90%, HCO3 of 25 mEq/L, and lactate of 1. Normally, the pH of blood
should be between 7.38-7.42. In Jackson’s case, the pH is 7.35 which could be an indication of
acidosis. This condition could be as a result of the hyperinflation of the lungs that causes air dull
of carbon IV oxide to be retained in the blood thus lowering the pH value (Murphy et al., 2012).
He also has a PaO2 value of 60 mmHg which is an indication of mild hypoxemia. Normally, the
value of SaO2 should be between 94%-100%. Jackson’s value is 90% which indicates low
His blood pressure is measured to be 150/85 mmHg which is way above the normal blood
pressure that normally is around 120/80 mmHg. Asthma is linked to cardiovascular diseases that
in most cases cause hypertension in adults. The increase in the blood pressure could be due to the
disturbance of the airways during a severe acute asthma that may lead to tachycardia (Marik,
2010). A pulse rate of 130 beats per minute further indicates the presence of tachycardia which
may be correlated with asthma.
When a lung auscultation was conducted, there was an observation of widespread wheezing and
diminished breath sounds. These observations are as a result of suppressed airways thus making
gaseous exchange difficult. From a chest x-ray, hyper-inflated lung fields were observed. These
result from damage to the lung tissues by the acute severe asthma that causes the lungs to
become less elastic. As a result, the expulsion of air from the lungs becomes difficult thus getting
trapped within the lungs. Hyperinflation of the lungs could lead to conditions such as shortness
of breath that is observed in the provided case and exercise intolerance among others. Patients
with asthma are unable to inhale or exhale properly. As a result, the lungs retain some air within
thus leading to hyperinflation.
Additionally, we can see from the assessment of Jackson Smith, we notice that his blood gas
values are not entirely normal. He has an arterial blood pH of 7.35, PaO2 of 60 mmHg PaCO2 of
50 mmHg, SaO2 of 90%, HCO3 of 25 mEq/L, and lactate of 1. Normally, the pH of blood
should be between 7.38-7.42. In Jackson’s case, the pH is 7.35 which could be an indication of
acidosis. This condition could be as a result of the hyperinflation of the lungs that causes air dull
of carbon IV oxide to be retained in the blood thus lowering the pH value (Murphy et al., 2012).
He also has a PaO2 value of 60 mmHg which is an indication of mild hypoxemia. Normally, the
value of SaO2 should be between 94%-100%. Jackson’s value is 90% which indicates low
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE SEVERE ASTHMA 4
oxygen content in the blood. PaCO2 ranges from 38-42 mmHg thus a value of 50 mmHg
indicates that the amount of carbon IV oxide dissolved in blood is high. HCO3 value is however
normal.
Question 2: Nursing Strategies
i) Ineffective Airway Clearance
This can be described as the inability to get rid of obstructions or secretions from the respiratory
tract. As a result, the patient fails to maintain a clear airway. It may be related to ineffective
coughing, increased pulmonary secretions, and bronchospasms. This condition can be evidenced
by some of the following symptoms: cyanosis, chest tightness, cough, changes in the rate and
rhythm of respiration, retained secretions, dyspnea, wheezes, and abnormal arterial blood gasses
among others (Perkin & Ledoux, 2013). The desired outcome for this nursing strategy is to help
the patient in understanding therapeutic management regimen. Additionally, the strategy helps in
ensuring that the patient can maintain a clear airway patency. This airway patency can be
evidenced by an improved exchange of oxygen, clear breath sounds, and normal respirations
depths and rates among others.
Some of the nursing interventions may include assessing the respiratory rate, rhythm, and depth.
As evidenced by several studies, this rationale for this intervention indicates that changes in the
rhythm and rate of respiration may be an early indication of an impending respiratory distress
(Shah & Saltoun, 2012). Another intervention involves lung auscultation for adventitious
breathing. Wheezes may be an indication of partial obstruction of the airways.
ii) Health-Seeking Behavior such as Prevention of Asthma attack
oxygen content in the blood. PaCO2 ranges from 38-42 mmHg thus a value of 50 mmHg
indicates that the amount of carbon IV oxide dissolved in blood is high. HCO3 value is however
normal.
Question 2: Nursing Strategies
i) Ineffective Airway Clearance
This can be described as the inability to get rid of obstructions or secretions from the respiratory
tract. As a result, the patient fails to maintain a clear airway. It may be related to ineffective
coughing, increased pulmonary secretions, and bronchospasms. This condition can be evidenced
by some of the following symptoms: cyanosis, chest tightness, cough, changes in the rate and
rhythm of respiration, retained secretions, dyspnea, wheezes, and abnormal arterial blood gasses
among others (Perkin & Ledoux, 2013). The desired outcome for this nursing strategy is to help
the patient in understanding therapeutic management regimen. Additionally, the strategy helps in
ensuring that the patient can maintain a clear airway patency. This airway patency can be
evidenced by an improved exchange of oxygen, clear breath sounds, and normal respirations
depths and rates among others.
Some of the nursing interventions may include assessing the respiratory rate, rhythm, and depth.
As evidenced by several studies, this rationale for this intervention indicates that changes in the
rhythm and rate of respiration may be an early indication of an impending respiratory distress
(Shah & Saltoun, 2012). Another intervention involves lung auscultation for adventitious
breathing. Wheezes may be an indication of partial obstruction of the airways.
ii) Health-Seeking Behavior such as Prevention of Asthma attack
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE SEVERE ASTHMA 5
These health-seeking behaviors may involve an individual actively seeking for ways to alter their
health and move towards a much better level of health. It involves looking for information
regarding behavior changes and preventive measures (Twamley, 2010). The desired outcome for
this strategy is that parents understand what triggers asthma and the prevention measures.
Some of the nursing interventions may include assessing the patient’s family history of allergies.
This may include the causative factors of attacks and the behaviors that may result from the
attacks. This rationale for this intervention is aimed at revealing the tendency of the family to
any airway reactive disease. It may also reveal a history of eczema in the family (Twamley,
2010). Another intervention for this nursing strategy may be encouraging breathing exercises
that may include controlled breathing and relaxation. The rationale, in this case, is to prevent an
attack before it begins and to increase ventilation.
Question 3
a) Mechanism of Action of Drugs
i) Nebulised Salbutamol
This drug belongs to a group of medications known as bronchodilators. This group of drugs
helps in opening the passage in the lungs to aid breathing in patients with recurrent breathing
difficulties and also to treat acute severe asthma attacks like is the case with Jackson Smith
(Hossain et al., 2013). This medication is inhaled as an aerosol and it acts on the β2-
adrenoreceptors found on the smooth muscles that surround the bronchi.
ii) Nebulised Ipratropium Bromide (4/24)
These health-seeking behaviors may involve an individual actively seeking for ways to alter their
health and move towards a much better level of health. It involves looking for information
regarding behavior changes and preventive measures (Twamley, 2010). The desired outcome for
this strategy is that parents understand what triggers asthma and the prevention measures.
Some of the nursing interventions may include assessing the patient’s family history of allergies.
This may include the causative factors of attacks and the behaviors that may result from the
attacks. This rationale for this intervention is aimed at revealing the tendency of the family to
any airway reactive disease. It may also reveal a history of eczema in the family (Twamley,
2010). Another intervention for this nursing strategy may be encouraging breathing exercises
that may include controlled breathing and relaxation. The rationale, in this case, is to prevent an
attack before it begins and to increase ventilation.
Question 3
a) Mechanism of Action of Drugs
i) Nebulised Salbutamol
This drug belongs to a group of medications known as bronchodilators. This group of drugs
helps in opening the passage in the lungs to aid breathing in patients with recurrent breathing
difficulties and also to treat acute severe asthma attacks like is the case with Jackson Smith
(Hossain et al., 2013). This medication is inhaled as an aerosol and it acts on the β2-
adrenoreceptors found on the smooth muscles that surround the bronchi.
ii) Nebulised Ipratropium Bromide (4/24)
ACUTE SEVERE ASTHMA 6
This medication is used to control the symptoms caused by an ongoing lung disease and
conditions such as asthma (Iramain et al., 2011). It operates by relaxing the muscles that exist
around the airways thus making them open up and ensure that easy breathing is achieved
(Hossain et al., 2013). It is described as an anticholinergic agent and helps in decreasing the
contractility of the smooth muscles that surround the airways.
iii) IV Hydrocortisone 100mg (6/24)
This drug is used to treat inflammation due to different conditions of diseases that may include
acute severe asthma attack. It is attached to the cytosolic glucocorticoid receptor. Thereafter, the
receptor-ligand complex receptor that is newly formed shifts to the cell nucleus and binds to
several glucocorticoid response elements. An anti-inflammatory action is thus initiated and as a
result, inflammation is treated or prevented.
b) Nursing Implications
Nursing implications may be categorized as assessment and drug effect and patient and family
education. Assessment may include periodic lab tests for pulse oximetry and consultation of a
physician about the administration of the last dosage of the medicine several hours before
bedtime if the patient is experiencing problems with drug-induced insomnia. For the education of
both the patients and their families, they have to avoid contact between the eyes and the
inhalation drugs. Additionally, it is important to contact the physician if the medication fails to
provide relief. It is also important to note that some of these drugs can cause vertigo or dizziness
and therefore the necessary precaution must be taken.
This medication is used to control the symptoms caused by an ongoing lung disease and
conditions such as asthma (Iramain et al., 2011). It operates by relaxing the muscles that exist
around the airways thus making them open up and ensure that easy breathing is achieved
(Hossain et al., 2013). It is described as an anticholinergic agent and helps in decreasing the
contractility of the smooth muscles that surround the airways.
iii) IV Hydrocortisone 100mg (6/24)
This drug is used to treat inflammation due to different conditions of diseases that may include
acute severe asthma attack. It is attached to the cytosolic glucocorticoid receptor. Thereafter, the
receptor-ligand complex receptor that is newly formed shifts to the cell nucleus and binds to
several glucocorticoid response elements. An anti-inflammatory action is thus initiated and as a
result, inflammation is treated or prevented.
b) Nursing Implications
Nursing implications may be categorized as assessment and drug effect and patient and family
education. Assessment may include periodic lab tests for pulse oximetry and consultation of a
physician about the administration of the last dosage of the medicine several hours before
bedtime if the patient is experiencing problems with drug-induced insomnia. For the education of
both the patients and their families, they have to avoid contact between the eyes and the
inhalation drugs. Additionally, it is important to contact the physician if the medication fails to
provide relief. It is also important to note that some of these drugs can cause vertigo or dizziness
and therefore the necessary precaution must be taken.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ACUTE SEVERE ASTHMA 7
Concept Map
Concept Map
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE SEVERE ASTHMA 8
References
Bush, A., & Saglani, S. (2010). Management of severe asthma in children. The
lancet, 376(9743), 814-825.
Carlsen, K. L., Hedlin, G., Bush, A., Wennergren, G., de Benedictis, F. M., De Jongste, J. C., ...
& Pohunek, P. (2010). Assessment of problematic severe asthma in children. European
Respiratory Journal, erj00914-2010.
Hossain, A. S., Barua, U. K., Roy, G. C., Sutradhar, S. R., Rahman, I., & Rahman, G. (2013).
Comparison of salbutamol and ipratropium bromide versus salbutamol alone in the
treatment of acute severe asthma. Mymensingh medical journal: MMJ, 22(2), 345-352.
Iramain, R., López-Herce, J., Coronel, J., Spitters, C., Guggiari, J., & Bogado, N. (2011). Inhaled
salbutamol plus ipratropium in moderate and severe asthma crises in children. Journal of
Asthma, 48(3), 298-303.
Jackson, D. J., Sykes, A., Mallia, P., & Johnston, S. L. (2011). Asthma exacerbations: origin,
effect, and prevention. Journal of Allergy and Clinical Immunology, 128(6), 1165-1174.
Kitulwatte, N. (2011). Acute severe asthma. Sri Lanka Journal of Child Health, 40(1).
Lommatzsch, M., & Virchow, C. J. (2014). Severe asthma: definition, diagnosis and
treatment. Deutsches Ärzteblatt International, 111(50), 847.
Marik, P. E. (2010). Acute Severe Asthma. Handbook of Evidence-Based Critical Care, 261-
269.
References
Bush, A., & Saglani, S. (2010). Management of severe asthma in children. The
lancet, 376(9743), 814-825.
Carlsen, K. L., Hedlin, G., Bush, A., Wennergren, G., de Benedictis, F. M., De Jongste, J. C., ...
& Pohunek, P. (2010). Assessment of problematic severe asthma in children. European
Respiratory Journal, erj00914-2010.
Hossain, A. S., Barua, U. K., Roy, G. C., Sutradhar, S. R., Rahman, I., & Rahman, G. (2013).
Comparison of salbutamol and ipratropium bromide versus salbutamol alone in the
treatment of acute severe asthma. Mymensingh medical journal: MMJ, 22(2), 345-352.
Iramain, R., López-Herce, J., Coronel, J., Spitters, C., Guggiari, J., & Bogado, N. (2011). Inhaled
salbutamol plus ipratropium in moderate and severe asthma crises in children. Journal of
Asthma, 48(3), 298-303.
Jackson, D. J., Sykes, A., Mallia, P., & Johnston, S. L. (2011). Asthma exacerbations: origin,
effect, and prevention. Journal of Allergy and Clinical Immunology, 128(6), 1165-1174.
Kitulwatte, N. (2011). Acute severe asthma. Sri Lanka Journal of Child Health, 40(1).
Lommatzsch, M., & Virchow, C. J. (2014). Severe asthma: definition, diagnosis and
treatment. Deutsches Ärzteblatt International, 111(50), 847.
Marik, P. E. (2010). Acute Severe Asthma. Handbook of Evidence-Based Critical Care, 261-
269.
ACUTE SEVERE ASTHMA 9
Murphy, A. C., Proeschal, A., Brightling, C. E., Wardlaw, A. J., Pavord, I., Bradding, P., &
Green, R. H. (2012). The relationship between clinical outcomes and medication
adherence in difficult-to-control asthma. Thorax, thoraxjnl-2011.
Perkin, R. M., & Ledoux, M. R. (2013). Acute Severe Asthma. Primary Care Reports, 19(5).
Shah, R., & Saltoun, C. A. (2012, May). Acute severe asthma (status asthmaticus). In Allergy
and Asthma proceedings (Vol. 33, No. 3, p. 47). OceanSide Publications.
Twamley, H. (2010). Acute severe asthma. A Beginner's Guide to Intensive Care Medicine: A
Handbook for Junior Doctors and Allied Professionals, 150.
Murphy, A. C., Proeschal, A., Brightling, C. E., Wardlaw, A. J., Pavord, I., Bradding, P., &
Green, R. H. (2012). The relationship between clinical outcomes and medication
adherence in difficult-to-control asthma. Thorax, thoraxjnl-2011.
Perkin, R. M., & Ledoux, M. R. (2013). Acute Severe Asthma. Primary Care Reports, 19(5).
Shah, R., & Saltoun, C. A. (2012, May). Acute severe asthma (status asthmaticus). In Allergy
and Asthma proceedings (Vol. 33, No. 3, p. 47). OceanSide Publications.
Twamley, H. (2010). Acute severe asthma. A Beginner's Guide to Intensive Care Medicine: A
Handbook for Junior Doctors and Allied Professionals, 150.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



