Analysis of Acute Severe Asthma: Case Study and Treatment
VerifiedAdded on 2023/06/07
|9
|3225
|337
Homework Assignment
AI Summary
This document presents a detailed case study of a patient diagnosed with acute severe asthma. It begins with an overview of the patient's clinical presentation, including symptoms like dyspnea, tachypnea, and signs of respiratory acidosis and hypoxia. The document then delves into the pathophysiology of asthma, explaining the mechanisms of airway constriction, inflammation, and mucus hypersecretion. It discusses the diagnostic process, including the use of family history, clinical manifestations, and laboratory tests. The analysis covers nursing interventions, such as airway management, oxygen administration, and patient education on breathing techniques and triggers. The document also explores the pharmacologic therapy prescribed, including nebulized salbutamol, ipratropium bromide, and IV hydrocortisone, explaining their mechanisms of action and nursing implications. The document concludes by emphasizing the importance of monitoring the patient's response to treatment and managing potential side effects. This case study provides valuable insights into the comprehensive management of acute severe asthma, offering a practical guide for healthcare professionals and students alike. The document also references key medical texts and research papers to support the analysis and recommendations.
1
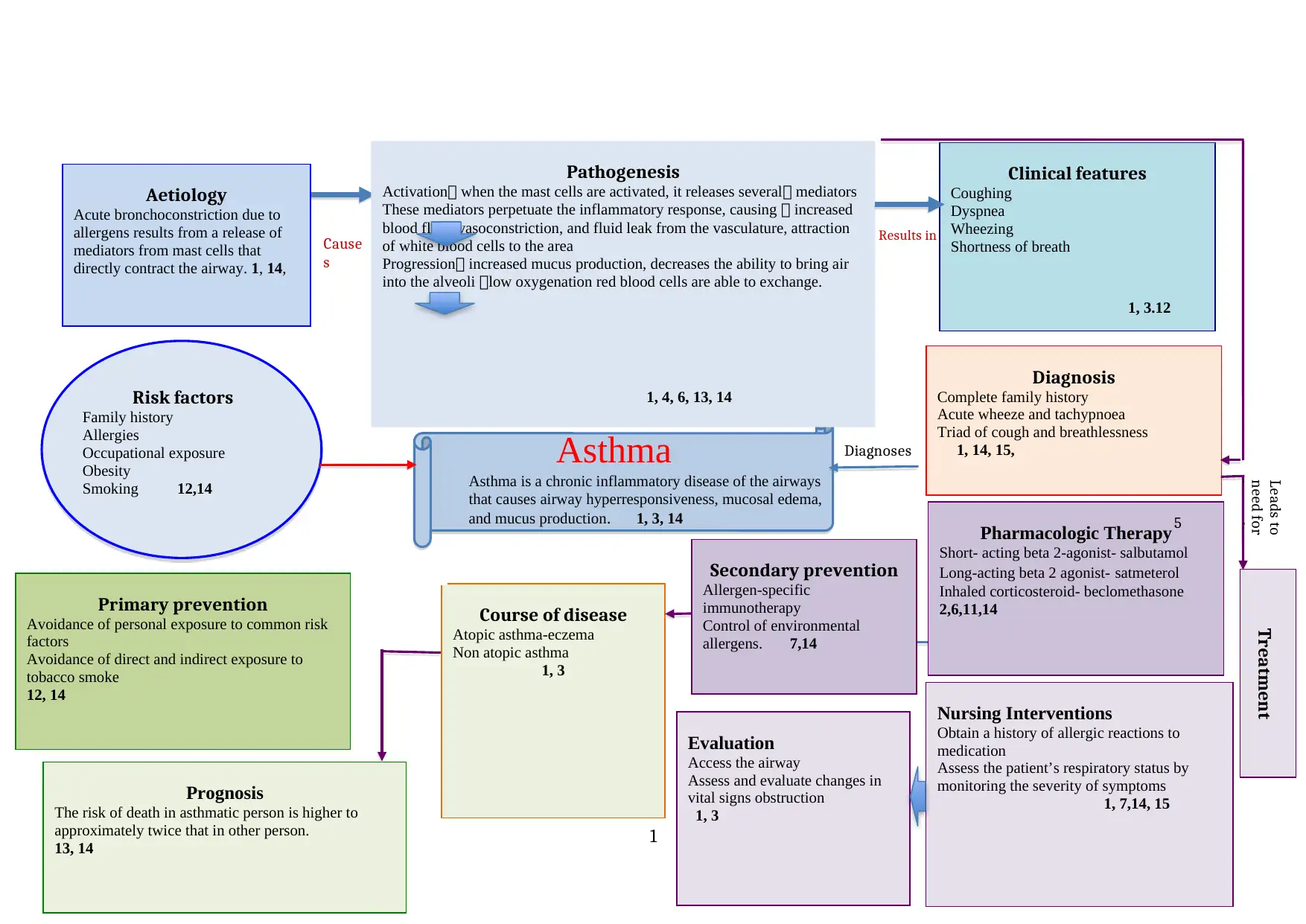
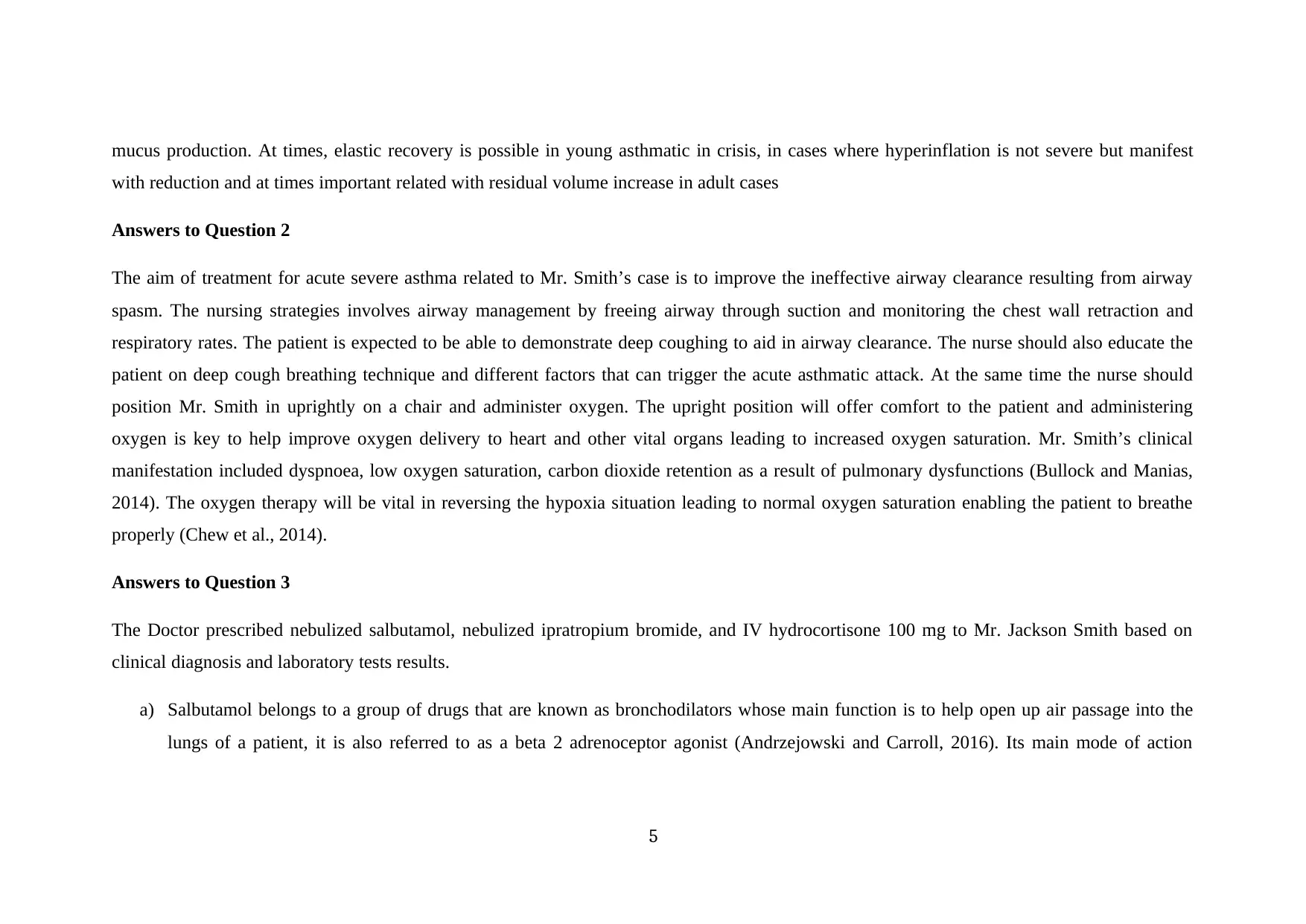
Asthma
Results in
Aetiology
Acute bronchoconstriction due to
allergens results from a release of
mediators from mast cells that
directly contract the airway. 1, 14,
Pathogenesis
Activation when the mast cells are activated, it releases several mediators
These mediators perpetuate the inflammatory response, causing increased
blood flow, vasoconstriction, and fluid leak from the vasculature, attraction
of white blood cells to the area
Progression increased mucus production, decreases the ability to bring air
into the alveoli low oxygenation red blood cells are able to exchange.
Risk factors
Family history
Allergies
Occupational exposure
Obesity
Smoking 12,14
Clinical features
Coughing
Dyspnea
Wheezing
Shortness of breath
Diagnosis
Complete family history
Acute wheeze and tachypnoea
Triad of cough and breathlessness
1, 14, 15,
Primary prevention
Avoidance of personal exposure to common risk
factors
Avoidance of direct and indirect exposure to
tobacco smoke
12, 14
Treatment
Pharmacologic Therapy
Short- acting beta 2-agonist- salbutamol
Long-acting beta 2 agonist- satmeterol
Inhaled corticosteroid- beclomethasone
2,6,11,14
Nursing Interventions
Obtain a history of allergic reactions to
medication
Assess the patient’s respiratory status by
monitoring the severity of symptoms
1, 7,14, 15
Evaluation
Access the airway
Assess and evaluate changes in
vital signs obstruction
1, 3
Secondary prevention
Allergen-specific
immunotherapy
Control of environmental
allergens. 7,14
Course of disease
Atopic asthma-eczema
Non atopic asthma
1, 3
Asthma is a chronic inflammatory disease of the airways
that causes airway hyperresponsiveness, mucosal edema,
and mucus production. 1, 3, 14
Prognosis
The risk of death in asthmatic person is higher to
approximately twice that in other person.
13, 14
Cause
s
Leads to
need for
immedia
Diagnoses
1, 4, 6, 13, 14
1, 3.12
5
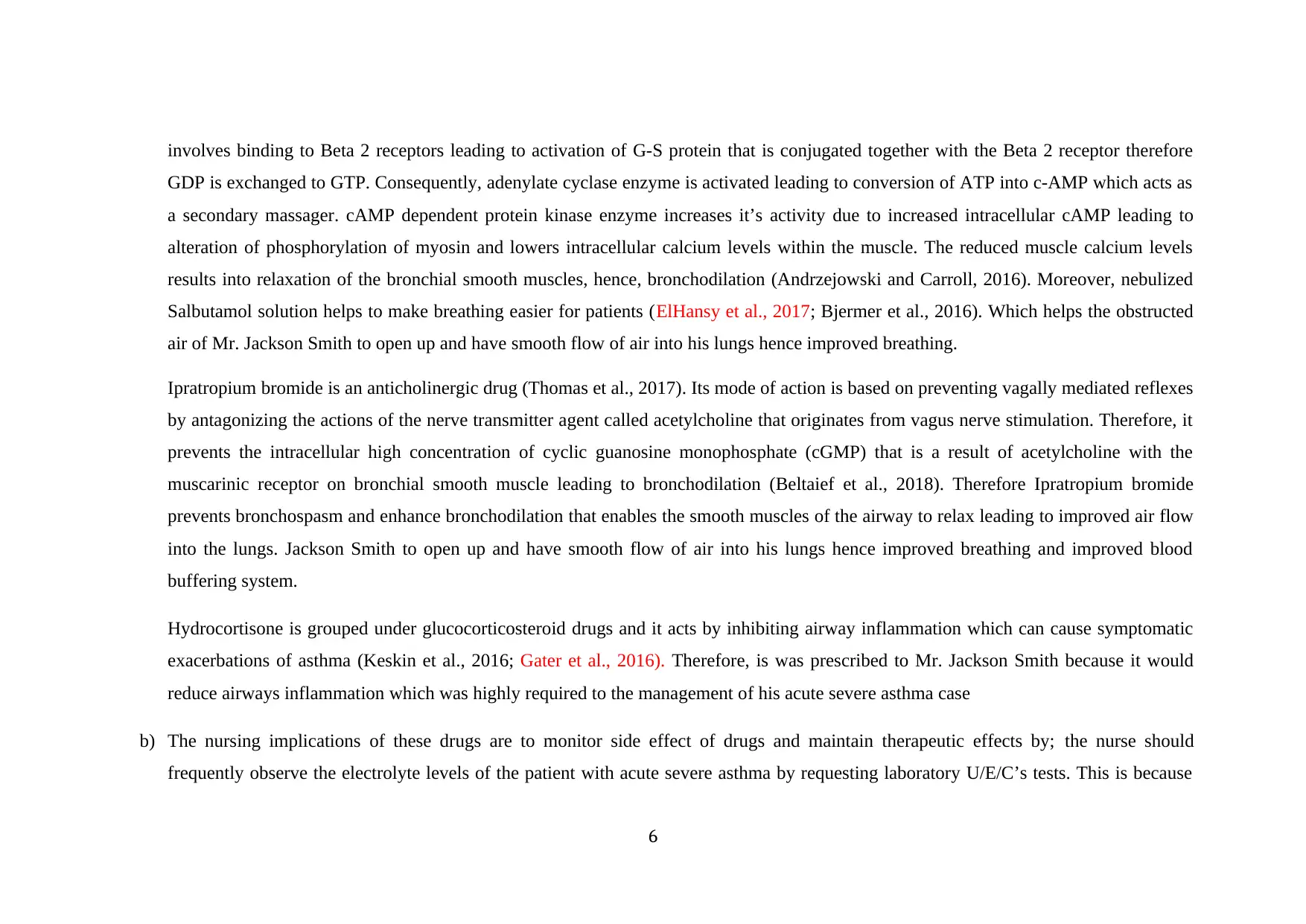
Asthma
Results in
Aetiology
Acute bronchoconstriction due to
allergens results from a release of
mediators from mast cells that
directly contract the airway. 1, 14,
Pathogenesis
Activation when the mast cells are activated, it releases several mediators
These mediators perpetuate the inflammatory response, causing increased
blood flow, vasoconstriction, and fluid leak from the vasculature, attraction
of white blood cells to the area
Progression increased mucus production, decreases the ability to bring air
into the alveoli low oxygenation red blood cells are able to exchange.
Risk factors
Family history
Allergies
Occupational exposure
Obesity
Smoking 12,14
Clinical features
Coughing
Dyspnea
Wheezing
Shortness of breath
Diagnosis
Complete family history
Acute wheeze and tachypnoea
Triad of cough and breathlessness
1, 14, 15,
Primary prevention
Avoidance of personal exposure to common risk
factors
Avoidance of direct and indirect exposure to
tobacco smoke
12, 14
Treatment
Pharmacologic Therapy
Short- acting beta 2-agonist- salbutamol
Long-acting beta 2 agonist- satmeterol
Inhaled corticosteroid- beclomethasone
2,6,11,14
Nursing Interventions
Obtain a history of allergic reactions to
medication
Assess the patient’s respiratory status by
monitoring the severity of symptoms
1, 7,14, 15
Evaluation
Access the airway
Assess and evaluate changes in
vital signs obstruction
1, 3
Secondary prevention
Allergen-specific
immunotherapy
Control of environmental
allergens. 7,14
Course of disease
Atopic asthma-eczema
Non atopic asthma
1, 3
Asthma is a chronic inflammatory disease of the airways
that causes airway hyperresponsiveness, mucosal edema,
and mucus production. 1, 3, 14
Prognosis
The risk of death in asthmatic person is higher to
approximately twice that in other person.
13, 14
Cause
s
Leads to
need for
immedia
Diagnoses
1, 4, 6, 13, 14
1, 3.12
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1. Aitken, L., & Chaboyer, W. (2016). ACCCN's Critical Care Nursing. Elsevier Health Sciences.
2. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher Education AU.
3. Craft, J., & Gordon, C. (2015). Introduction to clinical science. In Understanding Pathophysiology [2nd. Ed.] (pp. 3-19). Elsevier.
4. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015). Understanding pathophysiology-ANZ adaptation.
Elsevier Health Sciences.
5. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ... & Sampson, H. (2015). Consensus
communication on early peanut introduction and the prevention of peanut allergy in high-risk infants. World Allergy Organization
Journal, 8(1), 1.
6. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of allergic rhinitis as a strategy for preventing asthma.
Current allergy and asthma reports, 18(4), 23.
7. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S. (2014). Allergy and asthma prevention 2014.
Pediatric Allergy and Immunology, 25(6), 516-533.
8. Sher, L., Yiu, G., Sakov, A., Liu, S., & Caracta, C. (2017). Treatment of Asthmatic Patients with Fluticasone Propionate and Fluticasone
Propionate/Salmeterol Multidose Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of Life. Journal
of Allergy and Clinical Immunology, 139(2), AB97.
9. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid exposure and adverse effects in asthmatic
patients. Journal of Allergy and Clinical Immunology, 141(1), 110-116.
10. Toskala, E., & Kennedy, D. W. (2015). Asthma risk factors. In International forum of allergy & rhinology (Vol. 5, No. S1, pp. S11-S16).
11. Tuomisto, L. E., Ilmarinen, P., & Kankaanranta, H. (2015). Prognosis of new-onset asthma diagnosed at adult age. Respiratory medicine,
109(8), 944-954.
2
2. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher Education AU.
3. Craft, J., & Gordon, C. (2015). Introduction to clinical science. In Understanding Pathophysiology [2nd. Ed.] (pp. 3-19). Elsevier.
4. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015). Understanding pathophysiology-ANZ adaptation.
Elsevier Health Sciences.
5. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ... & Sampson, H. (2015). Consensus
communication on early peanut introduction and the prevention of peanut allergy in high-risk infants. World Allergy Organization
Journal, 8(1), 1.
6. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of allergic rhinitis as a strategy for preventing asthma.
Current allergy and asthma reports, 18(4), 23.
7. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S. (2014). Allergy and asthma prevention 2014.
Pediatric Allergy and Immunology, 25(6), 516-533.
8. Sher, L., Yiu, G., Sakov, A., Liu, S., & Caracta, C. (2017). Treatment of Asthmatic Patients with Fluticasone Propionate and Fluticasone
Propionate/Salmeterol Multidose Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of Life. Journal
of Allergy and Clinical Immunology, 139(2), AB97.
9. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid exposure and adverse effects in asthmatic
patients. Journal of Allergy and Clinical Immunology, 141(1), 110-116.
10. Toskala, E., & Kennedy, D. W. (2015). Asthma risk factors. In International forum of allergy & rhinology (Vol. 5, No. S1, pp. S11-S16).
11. Tuomisto, L. E., Ilmarinen, P., & Kankaanranta, H. (2015). Prognosis of new-onset asthma diagnosed at adult age. Respiratory medicine,
109(8), 944-954.
2
12. Who.int. (2018).WHO | WHO Strategy for prevention and control of Chronic
RespiratoryDiseases.[online]Availableat:http://www.who.int/respiratory/publications/strategy/en/index5.html [Accessed 7 Sep. 2018].
13. Wagner, K.D. (2014). High acuity nursing (6th ed.). Upper Saddler River, New Jersey: Pearson. Chapter13.
Answers to assignment 2
Based on both family history, clinical manifestation, and laboratory diagnosis in the cases study, Mr. Jackson Smith has been diagnosed with
acute severe asthma. The family confirmed that the patient has a history of asthma having been diagnosed when he was two years old. According
to Mr. Smith’s clinical signs, he presented with severe dysponoea, high respiratory rates, and the blood gas results indicated chances of
respiratory acidosis and hypoxia, having raised level of Partial pressure of carbon dioxide (paCO2) and Low levels of arterial oxygen pressure
values (PaO2). Acute severe asthma takes place when the airway diameter is reduced due to physiological contraction of the smooth muscles,
inflammation of the bronchial walls and mucus hypersecretion along the airway (Wawrzyniak et al., 2017). According to Gon and Hashimoto
(2018), repeated damage and regeneration of airway’s smooth muscles epithelial cells due to exposure to environmental allergens and
inflammation leads to physiological dysfunction and histological changes of mucosal epithelium. Furthermore, Whitsett and Alenghat (2015),
described the hallmark of asthma attack to an increased airway responsiveness (AHR) which is inflated airway narrowing as a response to
allergen with the degree of AHR being associated to asthma symptoms and prerequisite for treatment.
3
RespiratoryDiseases.[online]Availableat:http://www.who.int/respiratory/publications/strategy/en/index5.html [Accessed 7 Sep. 2018].
13. Wagner, K.D. (2014). High acuity nursing (6th ed.). Upper Saddler River, New Jersey: Pearson. Chapter13.
Answers to assignment 2
Based on both family history, clinical manifestation, and laboratory diagnosis in the cases study, Mr. Jackson Smith has been diagnosed with
acute severe asthma. The family confirmed that the patient has a history of asthma having been diagnosed when he was two years old. According
to Mr. Smith’s clinical signs, he presented with severe dysponoea, high respiratory rates, and the blood gas results indicated chances of
respiratory acidosis and hypoxia, having raised level of Partial pressure of carbon dioxide (paCO2) and Low levels of arterial oxygen pressure
values (PaO2). Acute severe asthma takes place when the airway diameter is reduced due to physiological contraction of the smooth muscles,
inflammation of the bronchial walls and mucus hypersecretion along the airway (Wawrzyniak et al., 2017). According to Gon and Hashimoto
(2018), repeated damage and regeneration of airway’s smooth muscles epithelial cells due to exposure to environmental allergens and
inflammation leads to physiological dysfunction and histological changes of mucosal epithelium. Furthermore, Whitsett and Alenghat (2015),
described the hallmark of asthma attack to an increased airway responsiveness (AHR) which is inflated airway narrowing as a response to
allergen with the degree of AHR being associated to asthma symptoms and prerequisite for treatment.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Despite the fact that, acute severe asthma is a disease that affects the airways, all the other pulmonary functions are negatively affected during
asthmatic attacks. There is parallel between the increase in the resistance offered by the bronchial walls and the severity of the clinical
manifestation and is supplemented by the increased extent of reduced ventilation. In the case of Mr. Smith there is drastic reduction in maximum
expiratory volume per second and the average respiratory air flow rate. Hence, in this case Mr. Smith’s respiratory rates are low, with severe
dysponoea, and in ability to complete full statement in one breath. Furthermore, with reduction in maximum expiratory volume per second and
reduced respiratory rates flow the patient will experience acute respiratory acidosis this is due hypoventilation causing disturbance in the acid-
base equilibrium (Brinkman and Sharma, 2018). There is carbon dioxide retention in the circulatory system of Mr. Smith leading to respiratory
acidosis. Hence, in this cases the blood gas tests revealed increased (paCO2) and PH in the borderline. Moreover, due to the respiratory acidosis
there is reduced breathing and severe dyspnoea as witnessed in Mr. Smith’s case.
According to Contoli et al. (2018), when a patient with acute severe asthmatic attack gets into the emergency room all most all his parameters
goes below 40% of the predicted figures. At the same time, due to constriction and obstruction of the bronchioles caused by the immunological
response caused by the allergens during acute asthmatic attack. The ability of the patients to inhale and exhale is reduced leading to contraction
of air sacs, consequently the amount of carbon dioxide being expelled is reduced leading to hyperinflation of the lung fields. According to
Durlinger et al. (2017), PaO2 is a good indicator of Hemoglobin oxygen saturation. At the same time the values are used to measure the oxygen
availability to vital body organs such as lungs and PaO2 and PaCO2 gradient serves as index of lung effectiveness in gas exchange. The
disturbance in the airway caused by bronchoconstriction and inflammation during the acute asthmatic attack leading to respiratory insufficiency
and as a result the patient suffers hypoxia. Due to hypoventilation leading to low PaO2 as presented in Mr. Smith case, there is incomplete
metabolism within the muscles cells leading to net accumulation of lactic acid causing metabolic acidosis at the same time. The episode of lung
failure in acute severe asthmatic attack is due to ventilator labor that is attributable to increased airway resistance, inflammation, and increased
4
asthmatic attacks. There is parallel between the increase in the resistance offered by the bronchial walls and the severity of the clinical
manifestation and is supplemented by the increased extent of reduced ventilation. In the case of Mr. Smith there is drastic reduction in maximum
expiratory volume per second and the average respiratory air flow rate. Hence, in this case Mr. Smith’s respiratory rates are low, with severe
dysponoea, and in ability to complete full statement in one breath. Furthermore, with reduction in maximum expiratory volume per second and
reduced respiratory rates flow the patient will experience acute respiratory acidosis this is due hypoventilation causing disturbance in the acid-
base equilibrium (Brinkman and Sharma, 2018). There is carbon dioxide retention in the circulatory system of Mr. Smith leading to respiratory
acidosis. Hence, in this cases the blood gas tests revealed increased (paCO2) and PH in the borderline. Moreover, due to the respiratory acidosis
there is reduced breathing and severe dyspnoea as witnessed in Mr. Smith’s case.
According to Contoli et al. (2018), when a patient with acute severe asthmatic attack gets into the emergency room all most all his parameters
goes below 40% of the predicted figures. At the same time, due to constriction and obstruction of the bronchioles caused by the immunological
response caused by the allergens during acute asthmatic attack. The ability of the patients to inhale and exhale is reduced leading to contraction
of air sacs, consequently the amount of carbon dioxide being expelled is reduced leading to hyperinflation of the lung fields. According to
Durlinger et al. (2017), PaO2 is a good indicator of Hemoglobin oxygen saturation. At the same time the values are used to measure the oxygen
availability to vital body organs such as lungs and PaO2 and PaCO2 gradient serves as index of lung effectiveness in gas exchange. The
disturbance in the airway caused by bronchoconstriction and inflammation during the acute asthmatic attack leading to respiratory insufficiency
and as a result the patient suffers hypoxia. Due to hypoventilation leading to low PaO2 as presented in Mr. Smith case, there is incomplete
metabolism within the muscles cells leading to net accumulation of lactic acid causing metabolic acidosis at the same time. The episode of lung
failure in acute severe asthmatic attack is due to ventilator labor that is attributable to increased airway resistance, inflammation, and increased
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
mucus production. At times, elastic recovery is possible in young asthmatic in crisis, in cases where hyperinflation is not severe but manifest
with reduction and at times important related with residual volume increase in adult cases
Answers to Question 2
The aim of treatment for acute severe asthma related to Mr. Smith’s case is to improve the ineffective airway clearance resulting from airway
spasm. The nursing strategies involves airway management by freeing airway through suction and monitoring the chest wall retraction and
respiratory rates. The patient is expected to be able to demonstrate deep coughing to aid in airway clearance. The nurse should also educate the
patient on deep cough breathing technique and different factors that can trigger the acute asthmatic attack. At the same time the nurse should
position Mr. Smith in uprightly on a chair and administer oxygen. The upright position will offer comfort to the patient and administering
oxygen is key to help improve oxygen delivery to heart and other vital organs leading to increased oxygen saturation. Mr. Smith’s clinical
manifestation included dyspnoea, low oxygen saturation, carbon dioxide retention as a result of pulmonary dysfunctions (Bullock and Manias,
2014). The oxygen therapy will be vital in reversing the hypoxia situation leading to normal oxygen saturation enabling the patient to breathe
properly (Chew et al., 2014).
Answers to Question 3
The Doctor prescribed nebulized salbutamol, nebulized ipratropium bromide, and IV hydrocortisone 100 mg to Mr. Jackson Smith based on
clinical diagnosis and laboratory tests results.
a) Salbutamol belongs to a group of drugs that are known as bronchodilators whose main function is to help open up air passage into the
lungs of a patient, it is also referred to as a beta 2 adrenoceptor agonist (Andrzejowski and Carroll, 2016). Its main mode of action
5
with reduction and at times important related with residual volume increase in adult cases
Answers to Question 2
The aim of treatment for acute severe asthma related to Mr. Smith’s case is to improve the ineffective airway clearance resulting from airway
spasm. The nursing strategies involves airway management by freeing airway through suction and monitoring the chest wall retraction and
respiratory rates. The patient is expected to be able to demonstrate deep coughing to aid in airway clearance. The nurse should also educate the
patient on deep cough breathing technique and different factors that can trigger the acute asthmatic attack. At the same time the nurse should
position Mr. Smith in uprightly on a chair and administer oxygen. The upright position will offer comfort to the patient and administering
oxygen is key to help improve oxygen delivery to heart and other vital organs leading to increased oxygen saturation. Mr. Smith’s clinical
manifestation included dyspnoea, low oxygen saturation, carbon dioxide retention as a result of pulmonary dysfunctions (Bullock and Manias,
2014). The oxygen therapy will be vital in reversing the hypoxia situation leading to normal oxygen saturation enabling the patient to breathe
properly (Chew et al., 2014).
Answers to Question 3
The Doctor prescribed nebulized salbutamol, nebulized ipratropium bromide, and IV hydrocortisone 100 mg to Mr. Jackson Smith based on
clinical diagnosis and laboratory tests results.
a) Salbutamol belongs to a group of drugs that are known as bronchodilators whose main function is to help open up air passage into the
lungs of a patient, it is also referred to as a beta 2 adrenoceptor agonist (Andrzejowski and Carroll, 2016). Its main mode of action
5
involves binding to Beta 2 receptors leading to activation of G-S protein that is conjugated together with the Beta 2 receptor therefore
GDP is exchanged to GTP. Consequently, adenylate cyclase enzyme is activated leading to conversion of ATP into c-AMP which acts as
a secondary massager. cAMP dependent protein kinase enzyme increases it’s activity due to increased intracellular cAMP leading to
alteration of phosphorylation of myosin and lowers intracellular calcium levels within the muscle. The reduced muscle calcium levels
results into relaxation of the bronchial smooth muscles, hence, bronchodilation (Andrzejowski and Carroll, 2016). Moreover, nebulized
Salbutamol solution helps to make breathing easier for patients (ElHansy et al., 2017; Bjermer et al., 2016). Which helps the obstructed
air of Mr. Jackson Smith to open up and have smooth flow of air into his lungs hence improved breathing.
Ipratropium bromide is an anticholinergic drug (Thomas et al., 2017). Its mode of action is based on preventing vagally mediated reflexes
by antagonizing the actions of the nerve transmitter agent called acetylcholine that originates from vagus nerve stimulation. Therefore, it
prevents the intracellular high concentration of cyclic guanosine monophosphate (cGMP) that is a result of acetylcholine with the
muscarinic receptor on bronchial smooth muscle leading to bronchodilation (Beltaief et al., 2018). Therefore Ipratropium bromide
prevents bronchospasm and enhance bronchodilation that enables the smooth muscles of the airway to relax leading to improved air flow
into the lungs. Jackson Smith to open up and have smooth flow of air into his lungs hence improved breathing and improved blood
buffering system.
Hydrocortisone is grouped under glucocorticosteroid drugs and it acts by inhibiting airway inflammation which can cause symptomatic
exacerbations of asthma (Keskin et al., 2016; Gater et al., 2016). Therefore, is was prescribed to Mr. Jackson Smith because it would
reduce airways inflammation which was highly required to the management of his acute severe asthma case
b) The nursing implications of these drugs are to monitor side effect of drugs and maintain therapeutic effects by; the nurse should
frequently observe the electrolyte levels of the patient with acute severe asthma by requesting laboratory U/E/C’s tests. This is because
6
GDP is exchanged to GTP. Consequently, adenylate cyclase enzyme is activated leading to conversion of ATP into c-AMP which acts as
a secondary massager. cAMP dependent protein kinase enzyme increases it’s activity due to increased intracellular cAMP leading to
alteration of phosphorylation of myosin and lowers intracellular calcium levels within the muscle. The reduced muscle calcium levels
results into relaxation of the bronchial smooth muscles, hence, bronchodilation (Andrzejowski and Carroll, 2016). Moreover, nebulized
Salbutamol solution helps to make breathing easier for patients (ElHansy et al., 2017; Bjermer et al., 2016). Which helps the obstructed
air of Mr. Jackson Smith to open up and have smooth flow of air into his lungs hence improved breathing.
Ipratropium bromide is an anticholinergic drug (Thomas et al., 2017). Its mode of action is based on preventing vagally mediated reflexes
by antagonizing the actions of the nerve transmitter agent called acetylcholine that originates from vagus nerve stimulation. Therefore, it
prevents the intracellular high concentration of cyclic guanosine monophosphate (cGMP) that is a result of acetylcholine with the
muscarinic receptor on bronchial smooth muscle leading to bronchodilation (Beltaief et al., 2018). Therefore Ipratropium bromide
prevents bronchospasm and enhance bronchodilation that enables the smooth muscles of the airway to relax leading to improved air flow
into the lungs. Jackson Smith to open up and have smooth flow of air into his lungs hence improved breathing and improved blood
buffering system.
Hydrocortisone is grouped under glucocorticosteroid drugs and it acts by inhibiting airway inflammation which can cause symptomatic
exacerbations of asthma (Keskin et al., 2016; Gater et al., 2016). Therefore, is was prescribed to Mr. Jackson Smith because it would
reduce airways inflammation which was highly required to the management of his acute severe asthma case
b) The nursing implications of these drugs are to monitor side effect of drugs and maintain therapeutic effects by; the nurse should
frequently observe the electrolyte levels of the patient with acute severe asthma by requesting laboratory U/E/C’s tests. This is because
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
salbutamol and hypoxia are known to have the ability to cause low potassium levels in the blood of the patient leading to hypokalaemia
that results to dehydration and headache (Andrzejowski and Carroll, 2016). Hence, the nurse should evaluate and maintain the
electrolytes level within normal range. At the same time, patients on experiencing hypoxia and taking salbutamol at the same time might
experience cardiovascular problems due to systemic vascular side effect caused (Andrzejowski and Carroll, 2016). Therefore the nurse
should monitor closely the patient’s vital signs during treatment.
Reference
Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology, prescribing and controversies. Archives of Disease in
Childhood-Education and Practice, 101(4), 194-197.
Beltaief, K., Msolli, M. A., Zorgati, A., Sekma, A., Fakhfakh, M., Ben Marzouk, M., ... & Belguith, A. (2018). Nebulized terbutaline &
ipratropium bromide vs terbutaline alone in acute exacerbation of COPD requiring noninvasive ventilation: a randomized double blind
controlled trial. Academic Emergency Medicine.
Bjermer, L., Stewart, J., Abbott-Banner, K., & Newman, K. (2016). RPL554, an inhaled PDE3/4 inhibitor, causes comparable bronchodilation to
high dose nebulised salbutamol in asthmatics with fewer systemic effects.
Bullock, S &Manias, E.(2014). Fundamental of pharmacology (7th ed.). Frenchs Forest, NSW: pearson Australi
Chew, D. P., Scott, I. A., Cullen, L., French, J. K., Briffa, T. G., Tideman, P. A., ... & Aylward, P. E. (2016). National Heart Foundation of
Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary
syndromes 2016. Med J Aust, 205(3), 128-133.
7
that results to dehydration and headache (Andrzejowski and Carroll, 2016). Hence, the nurse should evaluate and maintain the
electrolytes level within normal range. At the same time, patients on experiencing hypoxia and taking salbutamol at the same time might
experience cardiovascular problems due to systemic vascular side effect caused (Andrzejowski and Carroll, 2016). Therefore the nurse
should monitor closely the patient’s vital signs during treatment.
Reference
Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology, prescribing and controversies. Archives of Disease in
Childhood-Education and Practice, 101(4), 194-197.
Beltaief, K., Msolli, M. A., Zorgati, A., Sekma, A., Fakhfakh, M., Ben Marzouk, M., ... & Belguith, A. (2018). Nebulized terbutaline &
ipratropium bromide vs terbutaline alone in acute exacerbation of COPD requiring noninvasive ventilation: a randomized double blind
controlled trial. Academic Emergency Medicine.
Bjermer, L., Stewart, J., Abbott-Banner, K., & Newman, K. (2016). RPL554, an inhaled PDE3/4 inhibitor, causes comparable bronchodilation to
high dose nebulised salbutamol in asthmatics with fewer systemic effects.
Bullock, S &Manias, E.(2014). Fundamental of pharmacology (7th ed.). Frenchs Forest, NSW: pearson Australi
Chew, D. P., Scott, I. A., Cullen, L., French, J. K., Briffa, T. G., Tideman, P. A., ... & Aylward, P. E. (2016). National Heart Foundation of
Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary
syndromes 2016. Med J Aust, 205(3), 128-133.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Gater, A., Nelsen, L., Fleming, S., Lundy, J. J., Bonner, N., Hall, R., ... & Schatz, M. (2016). Assessing asthma symptoms in adolescents and
adults: Qualitative research supporting development of the asthma daily symptom diary. Value in Health, 19(4), 440-450.
Durlinger, E. M. J., Spoelstra-de Man, A. M. E., Smit, B., de Grooth, H. J., Girbes, A. R. J., Oudemans-van Straaten, H. M., & Smulders, Y. M.
(2017). Hyperoxia: At what level of SpO2 is a patient safe? A study in mechanically ventilated ICU patients. Journal of critical care, 39,
199-204.
ElHansy, M. H., Boules, M. E., El Essawy, A. F. M., Al-Kholy, M. B., Abdelrahman, M. M., Said, A. S., ... & Abdelrahim, M. E. (2017).
Inhaled salbutamol dose delivered by jet nebulizer, vibrating mesh nebulizer and metered dose inhaler with spacer during invasive
mechanical ventilation. Pulmonary pharmacology & therapeutics, 45, 159-163.
Keskin, O., Uluca, U., Keskin, M., Gogebakan, B., Kucukosmanoglu, E., Ozkars, M. Y., ... & Coskun, Y. (2016). The efficacy of single-high
dose inhaled corticosteroid versus oral prednisone treatment on exhaled leukotriene and 8-isoprostane levels in mild to moderate
asthmatic children with asthma exacerbation. Allergologia et immunopathologia, 44(2), 138-148.
Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price, D. B. (2017). Ipratropium/Salbutamol Comparator
Versus Originator for Chronic Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using the
Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
Brinkman, J. E., & Sharma, S. (2018). Physiology, Alkalosis, Respiratory.
Gon, Y., & Hashimoto, S. (2018). Role of airway epithelial barrier dysfunction in pathogenesis of asthma. Allergology International, 67(1), 12-
17.
8
adults: Qualitative research supporting development of the asthma daily symptom diary. Value in Health, 19(4), 440-450.
Durlinger, E. M. J., Spoelstra-de Man, A. M. E., Smit, B., de Grooth, H. J., Girbes, A. R. J., Oudemans-van Straaten, H. M., & Smulders, Y. M.
(2017). Hyperoxia: At what level of SpO2 is a patient safe? A study in mechanically ventilated ICU patients. Journal of critical care, 39,
199-204.
ElHansy, M. H., Boules, M. E., El Essawy, A. F. M., Al-Kholy, M. B., Abdelrahman, M. M., Said, A. S., ... & Abdelrahim, M. E. (2017).
Inhaled salbutamol dose delivered by jet nebulizer, vibrating mesh nebulizer and metered dose inhaler with spacer during invasive
mechanical ventilation. Pulmonary pharmacology & therapeutics, 45, 159-163.
Keskin, O., Uluca, U., Keskin, M., Gogebakan, B., Kucukosmanoglu, E., Ozkars, M. Y., ... & Coskun, Y. (2016). The efficacy of single-high
dose inhaled corticosteroid versus oral prednisone treatment on exhaled leukotriene and 8-isoprostane levels in mild to moderate
asthmatic children with asthma exacerbation. Allergologia et immunopathologia, 44(2), 138-148.
Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price, D. B. (2017). Ipratropium/Salbutamol Comparator
Versus Originator for Chronic Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using the
Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
Brinkman, J. E., & Sharma, S. (2018). Physiology, Alkalosis, Respiratory.
Gon, Y., & Hashimoto, S. (2018). Role of airway epithelial barrier dysfunction in pathogenesis of asthma. Allergology International, 67(1), 12-
17.
8
Wawrzyniak, P., Wawrzyniak, M., Wanke, K., Sokolowska, M., Bendelja, K., Rückert, B., & Akdis, M. (2017). Regulation of bronchial
epithelial barrier integrity by type 2 cytokines and histone deacetylases in asthmatic patients. Journal of Allergy and Clinical
Immunology, 139(1), 93-103.
Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary innate immunity. Nature immunology, 16(1), 27.
Contoli, M., Morandi, L., Bellini, F., Soave, S., Forini, G., Pauletti, A., ... & Papi, A. (2017). Small Airways Impairment In Severe Asthmatic
Patients With Fixed Airflow Obstruction And In COPD. In C80-B. Multi-Modality Assessment Of Copd, Asthma, And Asthma-Copd
Overlap Syndrome (pp. A6495-A6495). American Thoracic Society.
9
epithelial barrier integrity by type 2 cytokines and histone deacetylases in asthmatic patients. Journal of Allergy and Clinical
Immunology, 139(1), 93-103.
Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary innate immunity. Nature immunology, 16(1), 27.
Contoli, M., Morandi, L., Bellini, F., Soave, S., Forini, G., Pauletti, A., ... & Papi, A. (2017). Small Airways Impairment In Severe Asthmatic
Patients With Fixed Airflow Obstruction And In COPD. In C80-B. Multi-Modality Assessment Of Copd, Asthma, And Asthma-Copd
Overlap Syndrome (pp. A6495-A6495). American Thoracic Society.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





