NURS 521: Analysis of Advanced Directives and POLST Forms, New York
VerifiedAdded on 2022/10/11
|8
|1837
|19
Homework Assignment
AI Summary
This assignment, for NURS 521, analyzes advanced directives and Physical Orders for Life-Sustaining Treatment (POLST) forms. Part I focuses on the student's experience completing an advanced directive, obtained from AARP and compliant with New York State law. It explores the legal aspects and the ease or difficulty of the process, referencing relevant literature. Part II introduces POLST forms, emphasizing their role in end-of-life care and communication between healthcare providers and patients. Part III compares and contrasts advanced directives and POLST forms, highlighting their differences in terms of document type, aim, surrogate appointment, and understanding. The paper also discusses the role of registered nurses in ensuring patient rights and guiding them through healthcare decisions. Key differences are explored, such as the patient making their own decisions in AD, while the healthcare professional makes decisions in POLST. The assignment underscores the importance of these documents in respecting patient autonomy and facilitating informed healthcare choices.

Running head: NURS 521
NURS 521
Name of Student
Name of University
Author’s Note
NURS 521
Name of Student
Name of University
Author’s Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURS 521
Part I
Advanced directive is a document which is legal outlining the needs and
wishes for the medical treatment and care for end of life, so that the individual can
inform their peer ones and health care professionals about their wishes (Rao et al.,
2014). I obtained my advanced directive from the online website of AARP
(http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3289) which complied with
the state of New York.
In order to specify the individual’s wishes in advance regarding the kind of
treatment they will need from the health care professionals during end of life, the
Federal Patient Self Determination Act enacted by the United States in 1990, assists in
addressing these health rights of the individuals. The individuals fluently express
mostly these wishes by a stipulate document, Advanced Directive (AD). The main
agenda behind this Act is to provide the individuals with an opportunity to articulate
their wishes in advance regarding their health care treatment and to impart knowledge
about the importance of the AD in the entire population (Silveira, Wiitala & Piette,
2014). Another objective behind this Act was to counteract the distinguished disparity
among the health care [providers and the individuals. The individuals are not required
to complete the form of AD or any other state laws as per the Federal law; in addition,
the law forbids expressly the requirement of AD for care and treatment as a requisite.
In New York, three types of AD are there, Health Care Proxy form, Do Not
Resuscitate Order and Living Will (Goede & Wheeler, 2015). The kind of medical
treatment is entirely an individual’s choice based on their values, culture and beliefs,
whether an individual wants to obtain the medical treatment or wants to decline the
medical services. Therefore, with the help of AD, the individual’s wishes and
decisions are respected and stay in trustworthy hands. With the launching of Family
Part I
Advanced directive is a document which is legal outlining the needs and
wishes for the medical treatment and care for end of life, so that the individual can
inform their peer ones and health care professionals about their wishes (Rao et al.,
2014). I obtained my advanced directive from the online website of AARP
(http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3289) which complied with
the state of New York.
In order to specify the individual’s wishes in advance regarding the kind of
treatment they will need from the health care professionals during end of life, the
Federal Patient Self Determination Act enacted by the United States in 1990, assists in
addressing these health rights of the individuals. The individuals fluently express
mostly these wishes by a stipulate document, Advanced Directive (AD). The main
agenda behind this Act is to provide the individuals with an opportunity to articulate
their wishes in advance regarding their health care treatment and to impart knowledge
about the importance of the AD in the entire population (Silveira, Wiitala & Piette,
2014). Another objective behind this Act was to counteract the distinguished disparity
among the health care [providers and the individuals. The individuals are not required
to complete the form of AD or any other state laws as per the Federal law; in addition,
the law forbids expressly the requirement of AD for care and treatment as a requisite.
In New York, three types of AD are there, Health Care Proxy form, Do Not
Resuscitate Order and Living Will (Goede & Wheeler, 2015). The kind of medical
treatment is entirely an individual’s choice based on their values, culture and beliefs,
whether an individual wants to obtain the medical treatment or wants to decline the
medical services. Therefore, with the help of AD, the individual’s wishes and
decisions are respected and stay in trustworthy hands. With the launching of Family
2NURS 521
Health Care Decisions Act by the New York legislature in 2010, it allows the peer
ones of the individual to take effective decisions on their behalf regarding their
medical treatment according to the individual’s wishes or if the wishes are not known,
then according to the individual’s interests.
Individuals above 18 can fill their Health Care Proxy Form, which allows
them to nominate someone they trust to take their health care decisions on their
behalf, if the individual loses the ability to do so.
Another way the AD works in New York is by signing a Living Will, in which
one expresses their wishes about medical treatment in writing.
Lastly, the Do Not Resuscitate (DNR) order under the law of New York, is a
list of instructions written by a doctor prohibiting the health care professionals to
perform CPR, if an individual’s breathing or heartbeat stops, in order to restart their
lungs or heart.
While completing the AD, it was more of a difficult task rather than an easy
task, because firstly, I had to decide my health care treatment wishes in advance,
which is quite uncertain. In future, what kind of disease or any ailment, which will
occur to me and what kind of treatment will be required to cure those treatments, are
unknown (Stein & Fineberg, 2013). If I mention that, I do not want to through any
kind of pain in my treatment, but what if the only treatment, which can cure me and
for which I will be able to live long, comprises pain. I would give anything to live
long, so filling an AD is quite difficult (Hartog et al., 2014). On the other hand, the
easy part is that I can nominate my closed and loved ones for taking decisions on my
behalf, because they will never try to hurt me in any way possible.
Health Care Decisions Act by the New York legislature in 2010, it allows the peer
ones of the individual to take effective decisions on their behalf regarding their
medical treatment according to the individual’s wishes or if the wishes are not known,
then according to the individual’s interests.
Individuals above 18 can fill their Health Care Proxy Form, which allows
them to nominate someone they trust to take their health care decisions on their
behalf, if the individual loses the ability to do so.
Another way the AD works in New York is by signing a Living Will, in which
one expresses their wishes about medical treatment in writing.
Lastly, the Do Not Resuscitate (DNR) order under the law of New York, is a
list of instructions written by a doctor prohibiting the health care professionals to
perform CPR, if an individual’s breathing or heartbeat stops, in order to restart their
lungs or heart.
While completing the AD, it was more of a difficult task rather than an easy
task, because firstly, I had to decide my health care treatment wishes in advance,
which is quite uncertain. In future, what kind of disease or any ailment, which will
occur to me and what kind of treatment will be required to cure those treatments, are
unknown (Stein & Fineberg, 2013). If I mention that, I do not want to through any
kind of pain in my treatment, but what if the only treatment, which can cure me and
for which I will be able to live long, comprises pain. I would give anything to live
long, so filling an AD is quite difficult (Hartog et al., 2014). On the other hand, the
easy part is that I can nominate my closed and loved ones for taking decisions on my
behalf, because they will never try to hurt me in any way possible.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURS 521
Part II
Physical Orders for Life Sustaining Treatment (POLST)
To improve the care and treatment of end of life, the United States have taken
an approach by encouraging the health care providers to communicate with their
patients regarding their stipulate medical needs, which needs to be taken care of
during the period of a medical crisis, this is referred as Physical Orders For Life
Sustaining Treatment (Brugger et al., 2013). The approach is conducted by giving a
POLST form to the medical providers to be filled after communicating with their
patients.
This form is completed when the medical provider is not astonished to know
that the life expectancy of their patient is one year or less than one year (Fritz &
Barclay, 2014).
Only the medical professional can complete this form.
It is only legal and valid when signed by a health care professional, which
varies state by state (Pedraza et al., 2016).
Part III
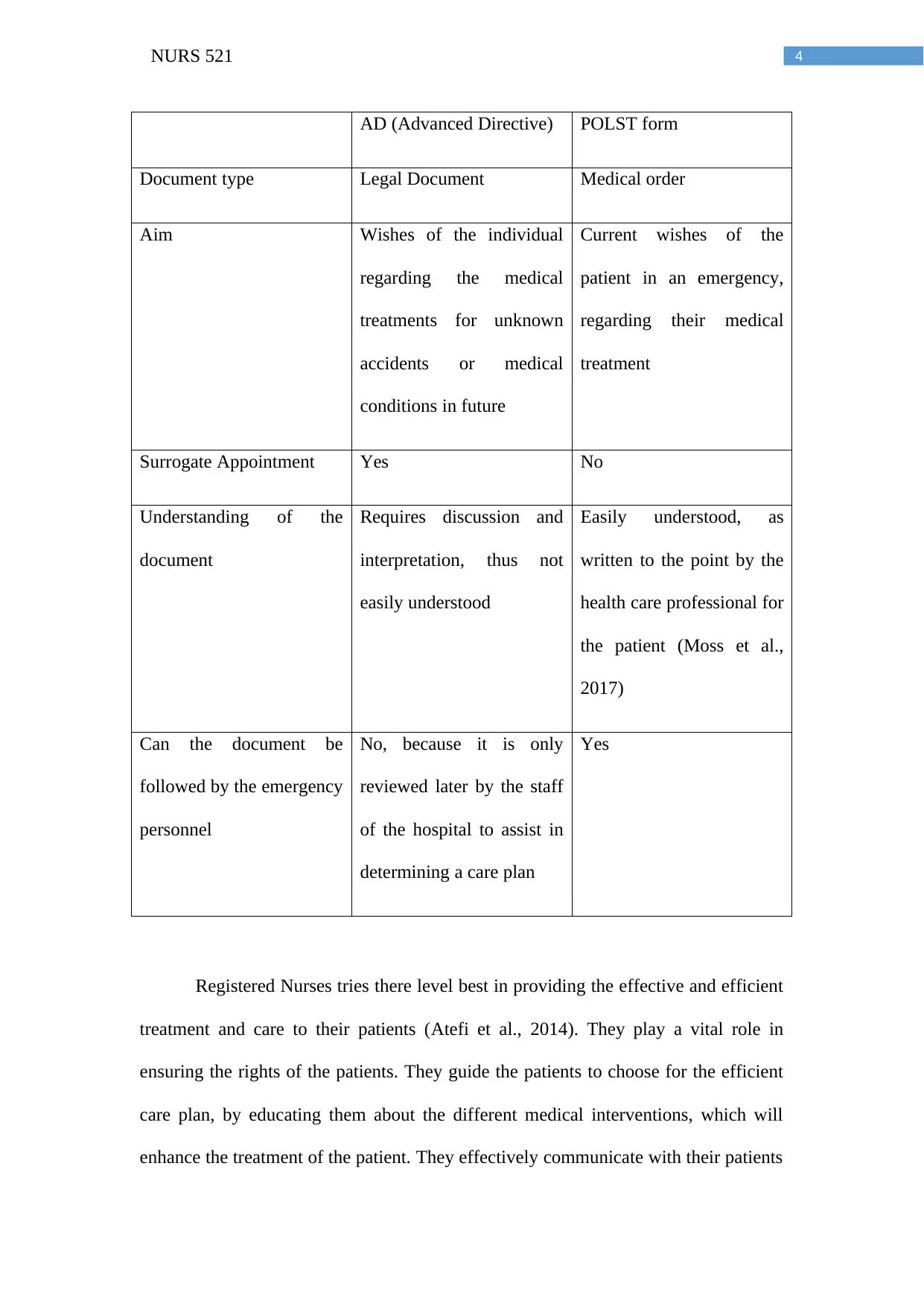
In order to summarize, Advanced Directive allows the patient to take the
decision about their medical treatment, however POLST is only valid when the health
care professional takes the decision for their patients, and this is the major difference
between AD and POLST.
Other differences are:
Part II
Physical Orders for Life Sustaining Treatment (POLST)
To improve the care and treatment of end of life, the United States have taken
an approach by encouraging the health care providers to communicate with their
patients regarding their stipulate medical needs, which needs to be taken care of
during the period of a medical crisis, this is referred as Physical Orders For Life
Sustaining Treatment (Brugger et al., 2013). The approach is conducted by giving a
POLST form to the medical providers to be filled after communicating with their
patients.
This form is completed when the medical provider is not astonished to know
that the life expectancy of their patient is one year or less than one year (Fritz &
Barclay, 2014).
Only the medical professional can complete this form.
It is only legal and valid when signed by a health care professional, which
varies state by state (Pedraza et al., 2016).
Part III
In order to summarize, Advanced Directive allows the patient to take the
decision about their medical treatment, however POLST is only valid when the health
care professional takes the decision for their patients, and this is the major difference
between AD and POLST.
Other differences are:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURS 521
AD (Advanced Directive) POLST form
Document type Legal Document Medical order
Aim Wishes of the individual
regarding the medical
treatments for unknown
accidents or medical
conditions in future
Current wishes of the
patient in an emergency,
regarding their medical
treatment
Surrogate Appointment Yes No
Understanding of the
document
Requires discussion and
interpretation, thus not
easily understood
Easily understood, as
written to the point by the
health care professional for
the patient (Moss et al.,
2017)
Can the document be
followed by the emergency
personnel
No, because it is only
reviewed later by the staff
of the hospital to assist in
determining a care plan
Yes
Registered Nurses tries there level best in providing the effective and efficient
treatment and care to their patients (Atefi et al., 2014). They play a vital role in
ensuring the rights of the patients. They guide the patients to choose for the efficient
care plan, by educating them about the different medical interventions, which will
enhance the treatment of the patient. They effectively communicate with their patients
AD (Advanced Directive) POLST form
Document type Legal Document Medical order
Aim Wishes of the individual
regarding the medical
treatments for unknown
accidents or medical
conditions in future
Current wishes of the
patient in an emergency,
regarding their medical
treatment
Surrogate Appointment Yes No
Understanding of the
document
Requires discussion and
interpretation, thus not
easily understood
Easily understood, as
written to the point by the
health care professional for
the patient (Moss et al.,
2017)
Can the document be
followed by the emergency
personnel
No, because it is only
reviewed later by the staff
of the hospital to assist in
determining a care plan
Yes
Registered Nurses tries there level best in providing the effective and efficient
treatment and care to their patients (Atefi et al., 2014). They play a vital role in
ensuring the rights of the patients. They guide the patients to choose for the efficient
care plan, by educating them about the different medical interventions, which will
enhance the treatment of the patient. They effectively communicate with their patients
5NURS 521
regarding the benefits and the drawbacks of the health care interventions, so that the
patient has clear knowledge about their conditions and can take the decision
accordingly (Johansson, Sandahl & Hasson, 2013). Registered nurses guide the
individuals to fill an AD, in order to secure their plan of medical treatment and
according to the individual’s wishes (Martin et al., 2016). For the patient, whose life
expectancy is very low, the health care providers and the registered nurses supervise
the patients about the POLST form, so that they can do everything, which is possible
in order to save their lives.
regarding the benefits and the drawbacks of the health care interventions, so that the
patient has clear knowledge about their conditions and can take the decision
accordingly (Johansson, Sandahl & Hasson, 2013). Registered nurses guide the
individuals to fill an AD, in order to secure their plan of medical treatment and
according to the individual’s wishes (Martin et al., 2016). For the patient, whose life
expectancy is very low, the health care providers and the registered nurses supervise
the patients about the POLST form, so that they can do everything, which is possible
in order to save their lives.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURS 521
References
Atefi, N., Abdullah, K. L., Wong, L. P., & Mazlom, R. (2014). Factors influencing
registered nurses perception of their overall job satisfaction: a qualitative
study. International nursing review, 61(3), 352-360.
Brugger, C., Breschi, L. C., Hart, E. M., Kummer, M., Lane, J. I., Morrow, P. T., ... &
Buscher, S. (2013). The POLST paradigm and form: Facts and analysis. The
Linacre Quarterly, 80(2), 103-138.
Fritz, Z., & Barclay, S. I. (2014). Patients' resuscitation preferences in context: lessons
from POLST.
Goede, M., & Wheeler, M. (2015). Advance directives, living wills, and futility in
perioperative care. Surgical Clinics, 95(2), 443-451.
Hartog, C. S., Peschel, I., Schwarzkopf, D., Curtis, J. R., Westermann, I., Kabisch, B.,
... & Reinhart, K. (2014). Are written advance directives helpful to guide end-
of-life therapy in the intensive care unit? A retrospective matched-cohort
study. Journal of critical care, 29(1), 128-133.
Johansson, G., Sandahl, C., & Hasson, D. (2013). Role stress among first‐line nurse
managers and registered nurses–a comparative study. Journal of Nursing
Management, 21(3), 449-458.
Martin, R. S., Hayes, B., Gregorevic, K., & Lim, W. K. (2016). The effects of
advance care planning interventions on nursing home residents: a systematic
review. Journal of the American Medical Directors Association, 17(4), 284-
293.
References
Atefi, N., Abdullah, K. L., Wong, L. P., & Mazlom, R. (2014). Factors influencing
registered nurses perception of their overall job satisfaction: a qualitative
study. International nursing review, 61(3), 352-360.
Brugger, C., Breschi, L. C., Hart, E. M., Kummer, M., Lane, J. I., Morrow, P. T., ... &
Buscher, S. (2013). The POLST paradigm and form: Facts and analysis. The
Linacre Quarterly, 80(2), 103-138.
Fritz, Z., & Barclay, S. I. (2014). Patients' resuscitation preferences in context: lessons
from POLST.
Goede, M., & Wheeler, M. (2015). Advance directives, living wills, and futility in
perioperative care. Surgical Clinics, 95(2), 443-451.
Hartog, C. S., Peschel, I., Schwarzkopf, D., Curtis, J. R., Westermann, I., Kabisch, B.,
... & Reinhart, K. (2014). Are written advance directives helpful to guide end-
of-life therapy in the intensive care unit? A retrospective matched-cohort
study. Journal of critical care, 29(1), 128-133.
Johansson, G., Sandahl, C., & Hasson, D. (2013). Role stress among first‐line nurse
managers and registered nurses–a comparative study. Journal of Nursing
Management, 21(3), 449-458.
Martin, R. S., Hayes, B., Gregorevic, K., & Lim, W. K. (2016). The effects of
advance care planning interventions on nursing home residents: a systematic
review. Journal of the American Medical Directors Association, 17(4), 284-
293.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURS 521
Moss, A. H., Zive, D. M., Falkenstine, E. C., & Dunithan, C. (2017). The quality of
POLST completion to guide treatment: a 2-state study. Journal of the
American Medical Directors Association, 18(9), 810-e5.
Pedraza, S. L., Culp, S., Falkenstine, E. C., & Moss, A. H. (2016). POST forms more
than advance directives associated with out-of-hospital death: Insights from a
state registry. Journal of pain and symptom management, 51(2), 240-246.
Rao, J. K., Anderson, L. A., Lin, F. C., & Laux, J. P. (2014). Completion of advance
directives among US consumers. American journal of preventive medicine,
46(1), 65-70.
Silveira, M. J., Wiitala, W., & Piette, J. (2014). Advance directive completion by
elderly Americans: a decade of change. Journal of the American Geriatrics
Society, 62(4), 706-710.
Stein, G. L., & Fineberg, I. C. (2013). Advance care planning in the USA and UK: a
comparative analysis of policy, implementation and the social work role.
British Journal of Social Work, 43(2), 233-248.
Moss, A. H., Zive, D. M., Falkenstine, E. C., & Dunithan, C. (2017). The quality of
POLST completion to guide treatment: a 2-state study. Journal of the
American Medical Directors Association, 18(9), 810-e5.
Pedraza, S. L., Culp, S., Falkenstine, E. C., & Moss, A. H. (2016). POST forms more
than advance directives associated with out-of-hospital death: Insights from a
state registry. Journal of pain and symptom management, 51(2), 240-246.
Rao, J. K., Anderson, L. A., Lin, F. C., & Laux, J. P. (2014). Completion of advance
directives among US consumers. American journal of preventive medicine,
46(1), 65-70.
Silveira, M. J., Wiitala, W., & Piette, J. (2014). Advance directive completion by
elderly Americans: a decade of change. Journal of the American Geriatrics
Society, 62(4), 706-710.
Stein, G. L., & Fineberg, I. C. (2013). Advance care planning in the USA and UK: a
comparative analysis of policy, implementation and the social work role.
British Journal of Social Work, 43(2), 233-248.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





