Clinical Report and Care Plan: Agatha's Schizophrenia Management, Uni
VerifiedAdded on 2022/11/25
|11
|2914
|240
Report
AI Summary
This clinical report details the case of Agatha, a patient diagnosed with schizophrenia, and outlines a comprehensive care plan. The report begins with an analysis of Agatha's medical history, including her previous treatment with aripiprazole and her non-compliance. It then explores various interventions, such as transcranial direct current stimulation (tDCS) and oxytocin, targeting social cognitive domains. The report emphasizes the importance of psychosocial interventions, including individual therapy, social skills training, and family therapy, alongside medication management with Aripiprazole. It further details the patient's priorities, focusing on her concerns about medication affecting her unborn child, and the need for a patient-centered approach. The report includes both short-term and long-term goals for Agatha, along with strategies for monitoring and evaluation. It also addresses family education, crisis planning, and specifies appointments with various clinicians, providing a holistic approach to Agatha's care.

Clinical report and plan
1
Clinical report and plan
Student name:
Student ID:
University name:
1
Clinical report and plan
Student name:
Student ID:
University name:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical report and plan
2
P1 – Clinical care report
What and how things would work for Agatha
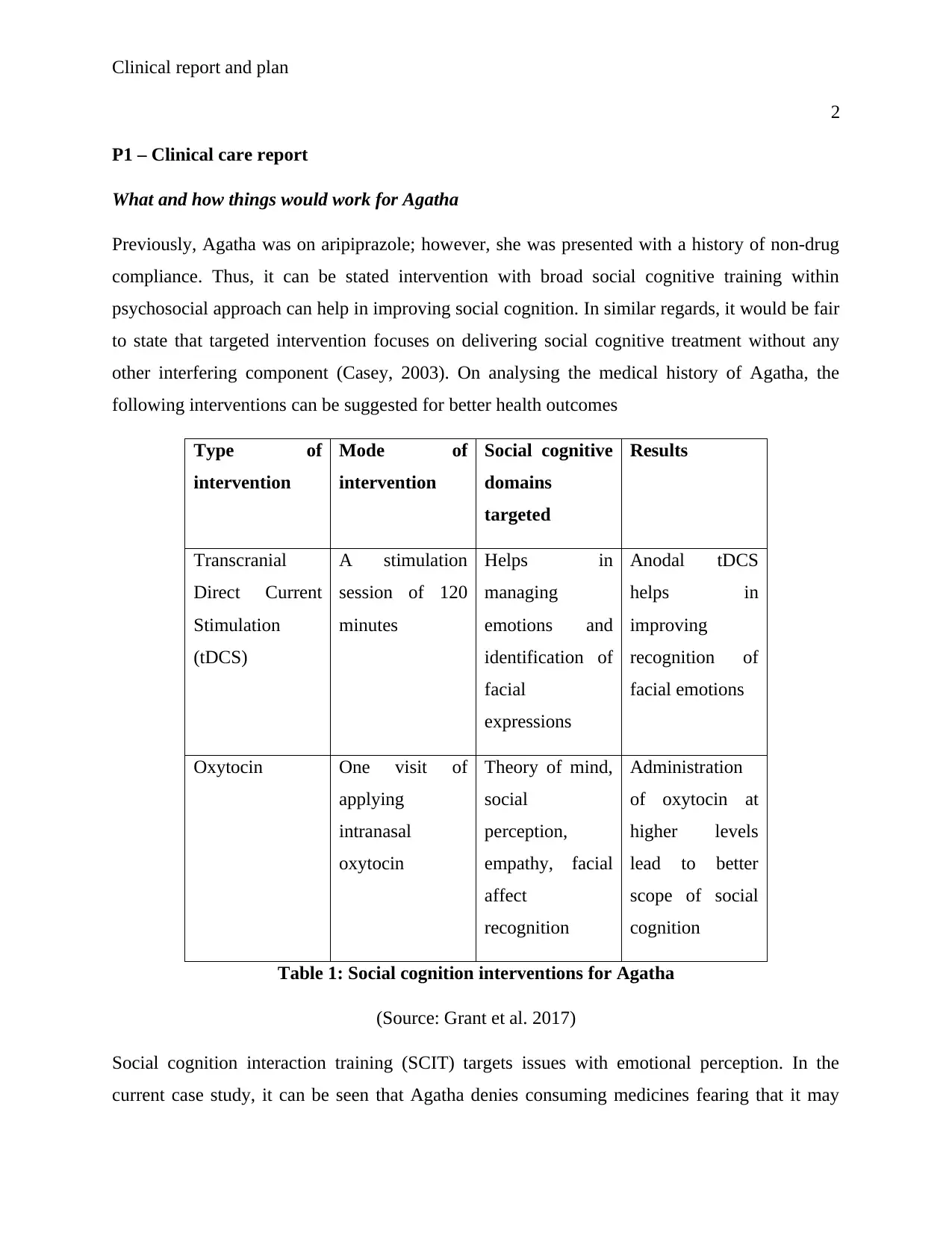
Previously, Agatha was on aripiprazole; however, she was presented with a history of non-drug
compliance. Thus, it can be stated intervention with broad social cognitive training within
psychosocial approach can help in improving social cognition. In similar regards, it would be fair
to state that targeted intervention focuses on delivering social cognitive treatment without any
other interfering component (Casey, 2003). On analysing the medical history of Agatha, the
following interventions can be suggested for better health outcomes
Type of
intervention
Mode of
intervention
Social cognitive
domains
targeted
Results
Transcranial
Direct Current
Stimulation
(tDCS)
A stimulation
session of 120
minutes
Helps in
managing
emotions and
identification of
facial
expressions
Anodal tDCS
helps in
improving
recognition of
facial emotions
Oxytocin One visit of
applying
intranasal
oxytocin
Theory of mind,
social
perception,
empathy, facial
affect
recognition
Administration
of oxytocin at
higher levels
lead to better
scope of social
cognition
Table 1: Social cognition interventions for Agatha
(Source: Grant et al. 2017)
Social cognition interaction training (SCIT) targets issues with emotional perception. In the
current case study, it can be seen that Agatha denies consuming medicines fearing that it may
2
P1 – Clinical care report
What and how things would work for Agatha
Previously, Agatha was on aripiprazole; however, she was presented with a history of non-drug
compliance. Thus, it can be stated intervention with broad social cognitive training within
psychosocial approach can help in improving social cognition. In similar regards, it would be fair
to state that targeted intervention focuses on delivering social cognitive treatment without any
other interfering component (Casey, 2003). On analysing the medical history of Agatha, the
following interventions can be suggested for better health outcomes
Type of
intervention
Mode of
intervention
Social cognitive
domains
targeted
Results
Transcranial
Direct Current
Stimulation
(tDCS)
A stimulation
session of 120
minutes
Helps in
managing
emotions and
identification of
facial
expressions
Anodal tDCS
helps in
improving
recognition of
facial emotions
Oxytocin One visit of
applying
intranasal
oxytocin
Theory of mind,
social
perception,
empathy, facial
affect
recognition
Administration
of oxytocin at
higher levels
lead to better
scope of social
cognition
Table 1: Social cognition interventions for Agatha
(Source: Grant et al. 2017)
Social cognition interaction training (SCIT) targets issues with emotional perception. In the
current case study, it can be seen that Agatha denies consuming medicines fearing that it may
Clinical report and plan
3
harm her unborn foetus. Thus, SCIT can emerge as a useful intervention. The treatment
constitutes of three phases, as follows. Firstly, “emotional training” which aims to improve
emotional perception of Agatha through the use of commercial software (smartphone
applications), can be used. The second phase “Figuring Out Situation” works on addressing
attributional biases. The last stage is the “Integration” phase which allows Agatha to practise the
skills she learned during the session of therapies.
Currently Agatha is subjected to social exclusion due to events in life. The relationship
separation and immediate pregnancy lead to immense mental depression and eventually
schizophrenia. Thus, from the perspective of treatment, it can be easily stated schizophrenia
demands a lifelong treatment, irrespective in absence of symptoms. The medicinal treatment with
psychosocial therapies can help in managing the condition for Agatha. Medication can be termed
as a cornerstone for treating schizophrenia and antipsychotic medications are often prescribed in
form of drugs. As stated by Tan et al. (2018), antipsychotic medications are known to control the
symptoms by managing the levels of neurotransmitters such as dopamine. Hence, the goal of
medication is to manage the symptoms and signs of schizophrenia with lowest levels of drugs.
The medication provided to Agatha is Aripiprazole, a first generation anti-psychotic medication,
which is highly preferred due to low health risk in relation to side effects (Mayo Clinic, 2019).
However, on analysing the medical condition of Agatha, it can be clearly stated that her
condition is a long term event that can be administered through the use of first generation of
antipsychotics.
Psychosocial interventions
Once the issue relating to psychosis is seen to recede, in addition to continuation of drugs social
and psychosocial therapies are important and include the following:
Individual therapy: Psychotherapy in the mentioned case aims to normalise thought patterns and
also teach Agatha to cope with stress. In current scenario, it can be stated that Agatha is
subjected to relationship and maternity stress. Hence, it can be stated identifying the early sign
associated with relapse can help individuals with schizophrenia to manage their problems (Sekar
et al. 2016)
3
harm her unborn foetus. Thus, SCIT can emerge as a useful intervention. The treatment
constitutes of three phases, as follows. Firstly, “emotional training” which aims to improve
emotional perception of Agatha through the use of commercial software (smartphone
applications), can be used. The second phase “Figuring Out Situation” works on addressing
attributional biases. The last stage is the “Integration” phase which allows Agatha to practise the
skills she learned during the session of therapies.
Currently Agatha is subjected to social exclusion due to events in life. The relationship
separation and immediate pregnancy lead to immense mental depression and eventually
schizophrenia. Thus, from the perspective of treatment, it can be easily stated schizophrenia
demands a lifelong treatment, irrespective in absence of symptoms. The medicinal treatment with
psychosocial therapies can help in managing the condition for Agatha. Medication can be termed
as a cornerstone for treating schizophrenia and antipsychotic medications are often prescribed in
form of drugs. As stated by Tan et al. (2018), antipsychotic medications are known to control the
symptoms by managing the levels of neurotransmitters such as dopamine. Hence, the goal of
medication is to manage the symptoms and signs of schizophrenia with lowest levels of drugs.
The medication provided to Agatha is Aripiprazole, a first generation anti-psychotic medication,
which is highly preferred due to low health risk in relation to side effects (Mayo Clinic, 2019).
However, on analysing the medical condition of Agatha, it can be clearly stated that her
condition is a long term event that can be administered through the use of first generation of
antipsychotics.
Psychosocial interventions
Once the issue relating to psychosis is seen to recede, in addition to continuation of drugs social
and psychosocial therapies are important and include the following:
Individual therapy: Psychotherapy in the mentioned case aims to normalise thought patterns and
also teach Agatha to cope with stress. In current scenario, it can be stated that Agatha is
subjected to relationship and maternity stress. Hence, it can be stated identifying the early sign
associated with relapse can help individuals with schizophrenia to manage their problems (Sekar
et al. 2016)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical report and plan
4
Training for social skills: Concentrates on improving social interaction and communication.
There remains no evidence that could suggest that Agatha is suffering from social exclusion. Her
family is extremely supportive and already improved the police about her degrading mental
condition. In addition to that the case study does not report assault by Agatha on family members
Family therapy: Being supportive enough towards the needs of affected individual is not enough.
The family needs to be educated enough against schizophrenia for ensuring positive health
outcomes (Searles, 2018)
Vocational rehabilitation: Medication and therapy reduce the signs of schizophrenia. However, it
is important to find a source of livelihood and the mentioned training can help Agatha (Green et
al. 2015)
Making a differential diagnosis of mental disorder is a key step in treating illness. As pointed out
by Fromer et al. (2016), sertraline was not recommended for treating the schizoaffective disorder
and even associated depression as it would exacerbate positive symptoms. However, the
controversy remains the same whether the use of anti-psychotics should be done.
Agatha’s priorities
In addition to that interaction with client is important, keeping in mind the importance of
personal space. As pointed out by Fromer et al. (2016), clients experiencing schizophrenia are
often mistrustful about closeness. In case of Agatha she did face relationship issue that made her
to loose trust on support. Helping the client with daily physical activities provided the client has
given information can help in gaining trust and eventually socializing with client.
One to one level of interaction is important as it would help the nurse to concentrate on
incongruities. Hence, it can be stated modelling of expression can provide a clear idea about the
exact intervention to be undertaken. Her priority is to protect her baby an d it is for the same
reason she refused to take medications. Understanding her priorities, her of prime importance as
it can work on providing better scope of care for Agatha. Thus, it would be fair enough to state
that a patient centred approach is important for Agatha that can help her building trust on the
healthcare professionals and improving her healthcare outcomes
4
Training for social skills: Concentrates on improving social interaction and communication.
There remains no evidence that could suggest that Agatha is suffering from social exclusion. Her
family is extremely supportive and already improved the police about her degrading mental
condition. In addition to that the case study does not report assault by Agatha on family members
Family therapy: Being supportive enough towards the needs of affected individual is not enough.
The family needs to be educated enough against schizophrenia for ensuring positive health
outcomes (Searles, 2018)
Vocational rehabilitation: Medication and therapy reduce the signs of schizophrenia. However, it
is important to find a source of livelihood and the mentioned training can help Agatha (Green et
al. 2015)
Making a differential diagnosis of mental disorder is a key step in treating illness. As pointed out
by Fromer et al. (2016), sertraline was not recommended for treating the schizoaffective disorder
and even associated depression as it would exacerbate positive symptoms. However, the
controversy remains the same whether the use of anti-psychotics should be done.
Agatha’s priorities
In addition to that interaction with client is important, keeping in mind the importance of
personal space. As pointed out by Fromer et al. (2016), clients experiencing schizophrenia are
often mistrustful about closeness. In case of Agatha she did face relationship issue that made her
to loose trust on support. Helping the client with daily physical activities provided the client has
given information can help in gaining trust and eventually socializing with client.
One to one level of interaction is important as it would help the nurse to concentrate on
incongruities. Hence, it can be stated modelling of expression can provide a clear idea about the
exact intervention to be undertaken. Her priority is to protect her baby an d it is for the same
reason she refused to take medications. Understanding her priorities, her of prime importance as
it can work on providing better scope of care for Agatha. Thus, it would be fair enough to state
that a patient centred approach is important for Agatha that can help her building trust on the
healthcare professionals and improving her healthcare outcomes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical report and plan
5
Part 1.1 – Description of targeted interventions
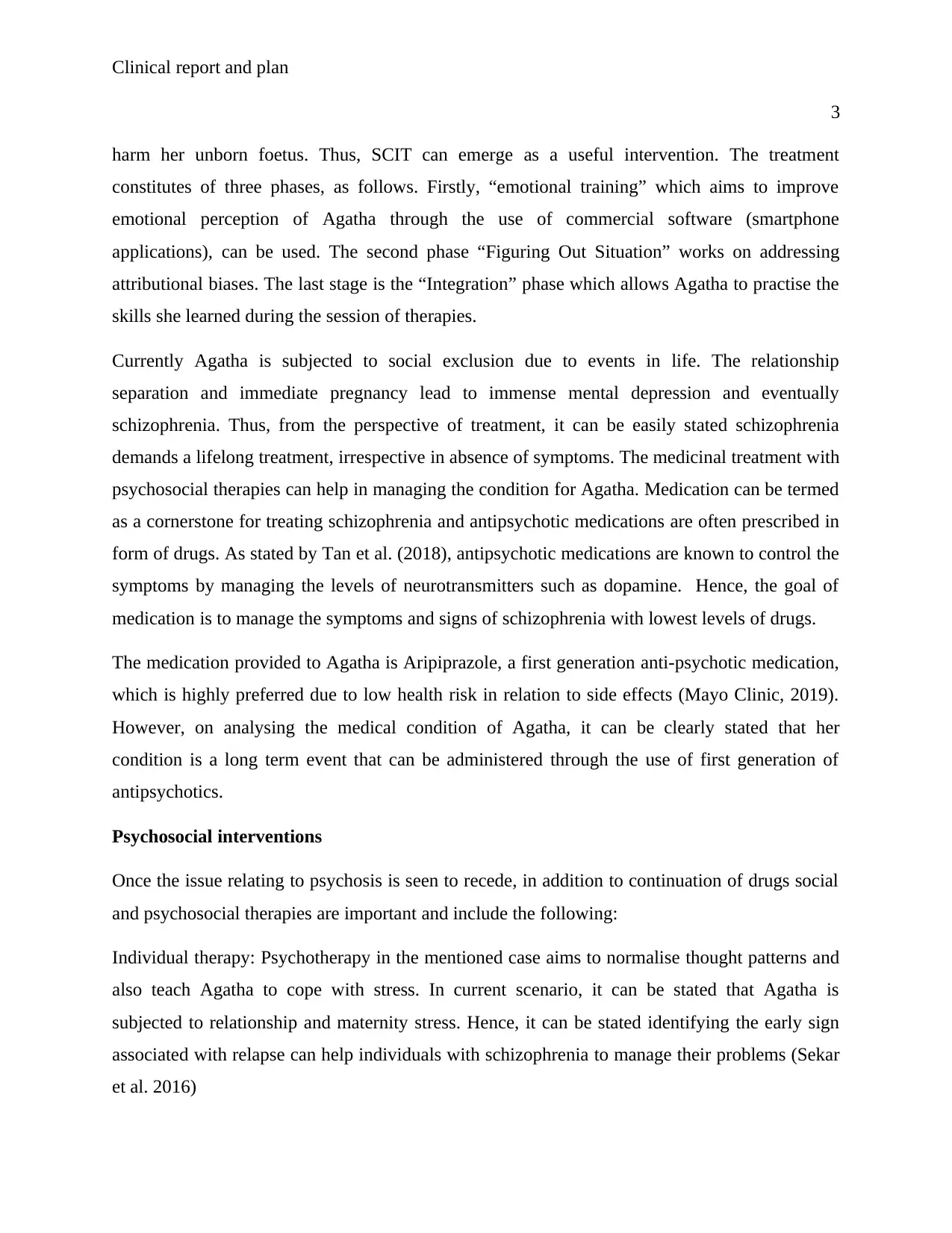
In current case study for Agatha, it can be clearly defined that she is suffering from poor social
skills. Intervention cited in these reviews is primarily used as therapist related intervention, aided
by software. In case of Agatha, intervention is composed of social cognitive treatment, either
standalone treatment or an amalgamation of therapies, such as skills training and even
neurocognitive therapies. Implemented the terminology coined by Kerkemeyer et al. (2015),
broad based intervention is those that is inclusive of social cognitive training with broad aspects
of psychosocial approach. The current demand of Agatha is to improve social cognition and
skills. The case study provides a clear idea to the fact that Agatha is delusional and failed to
differentiate between the right and wrong. Thus, based on the case study of Agatha, it can be
clearly seen:
Agatha is in need of therapy and medicine
However, she is seen to reject medicine as she feels it may harm the child
Then the only viable option left is the use of social therapies
Agatha fails to understand the emotion of her near and dear ones; thus perceives everyone
around her as a threat
Therapy can work on providing better social cognition and reducing the risks
Criterion Part 2: Goals and Integrated Care Plan or Inpatient Care Plan or Transfer of
Care Plan –
Part 2.1 Integrated care plan with minimum 3 short term and 3 long term goals
Long term goal #1: Agatha should maintain minimum level of functioning despite the prevalence
of disorganized thinking patterns
Long term goal #2: Agatha should verbalise a plan for increasing the events related to
socialization within clinical settings.
Long term goal #3: Agatha should exhibit adaptive skills of coping
5
Part 1.1 – Description of targeted interventions
In current case study for Agatha, it can be clearly defined that she is suffering from poor social
skills. Intervention cited in these reviews is primarily used as therapist related intervention, aided
by software. In case of Agatha, intervention is composed of social cognitive treatment, either
standalone treatment or an amalgamation of therapies, such as skills training and even
neurocognitive therapies. Implemented the terminology coined by Kerkemeyer et al. (2015),
broad based intervention is those that is inclusive of social cognitive training with broad aspects
of psychosocial approach. The current demand of Agatha is to improve social cognition and
skills. The case study provides a clear idea to the fact that Agatha is delusional and failed to
differentiate between the right and wrong. Thus, based on the case study of Agatha, it can be
clearly seen:
Agatha is in need of therapy and medicine
However, she is seen to reject medicine as she feels it may harm the child
Then the only viable option left is the use of social therapies
Agatha fails to understand the emotion of her near and dear ones; thus perceives everyone
around her as a threat
Therapy can work on providing better social cognition and reducing the risks
Criterion Part 2: Goals and Integrated Care Plan or Inpatient Care Plan or Transfer of
Care Plan –
Part 2.1 Integrated care plan with minimum 3 short term and 3 long term goals
Long term goal #1: Agatha should maintain minimum level of functioning despite the prevalence
of disorganized thinking patterns
Long term goal #2: Agatha should verbalise a plan for increasing the events related to
socialization within clinical settings.
Long term goal #3: Agatha should exhibit adaptive skills of coping
Clinical report and plan
6
Short term goal 1: Agatha will verbalise her feelings of acceptance and security while
differentiation between unrealistic and realistic thoughts
Short term goal 2: Agatha will interact with the nurse while exhibit congruent non-verbal and
verbal communication
Short term goal 3: Agatha will learn effective coping strategies to deal with stressful scenario
Goal Strategy (intervention/action/clinician) Review meeting/time Outcome
Communication with Agatha in a clear and calm voice promotes trust. Use of vague expression
with complicated interactions may promote series of mistrust and Agatha is subjected to
conflicting emotions and may fail to understand the meaning of complicated communication. In
similar regards, teaching Agatha to focus on the voice of caregiver in case disturbing thoughts
occur is a must (Lauriello & Perkins, 2019). This can help Agatha to maintain attention within
the reality. The mentioned intervention of learning to disregard disturbing thoughts can help
Agatha to focus and function in the real world.
Details of clinician signed off approval of accountable component of the plan.
Part 2.2 Provide details about plans for ongoing monitoring of the goals and interviews
In order to follow up the plan there is constant communication between the medical professional
and Agatha’s family. The use of goal update with progression of treatment is often implemented
and the risk factors are identified. For example, in the current scenario, no response to drug
administration can be termed as a leading cause of concern as it may degrade the health
conditions of Agatha. Unfortunately, medications for schizophrenia can lead to serious side
effects and affected individuals are often reluctant to consume them. It is for the same reason;
Agatha is not cooperating with medication requirements and is apprehensive about the fact that
the medicine may affect her unborn baby. In similar regards, it can be stated willingness to
cooperate with the mode of treatment may lead to affect the choice of drug administered.
Health risk for the unborn foetus
In addition to that schizophrenia is often feared to be a genetic disorder, in that regards, it can be
conclusively stated the unborn foetus is at risk of developing similar mental condition during the
6
Short term goal 1: Agatha will verbalise her feelings of acceptance and security while
differentiation between unrealistic and realistic thoughts
Short term goal 2: Agatha will interact with the nurse while exhibit congruent non-verbal and
verbal communication
Short term goal 3: Agatha will learn effective coping strategies to deal with stressful scenario
Goal Strategy (intervention/action/clinician) Review meeting/time Outcome
Communication with Agatha in a clear and calm voice promotes trust. Use of vague expression
with complicated interactions may promote series of mistrust and Agatha is subjected to
conflicting emotions and may fail to understand the meaning of complicated communication. In
similar regards, teaching Agatha to focus on the voice of caregiver in case disturbing thoughts
occur is a must (Lauriello & Perkins, 2019). This can help Agatha to maintain attention within
the reality. The mentioned intervention of learning to disregard disturbing thoughts can help
Agatha to focus and function in the real world.
Details of clinician signed off approval of accountable component of the plan.
Part 2.2 Provide details about plans for ongoing monitoring of the goals and interviews
In order to follow up the plan there is constant communication between the medical professional
and Agatha’s family. The use of goal update with progression of treatment is often implemented
and the risk factors are identified. For example, in the current scenario, no response to drug
administration can be termed as a leading cause of concern as it may degrade the health
conditions of Agatha. Unfortunately, medications for schizophrenia can lead to serious side
effects and affected individuals are often reluctant to consume them. It is for the same reason;
Agatha is not cooperating with medication requirements and is apprehensive about the fact that
the medicine may affect her unborn baby. In similar regards, it can be stated willingness to
cooperate with the mode of treatment may lead to affect the choice of drug administered.
Health risk for the unborn foetus
In addition to that schizophrenia is often feared to be a genetic disorder, in that regards, it can be
conclusively stated the unborn foetus is at risk of developing similar mental condition during the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical report and plan
7
later stages of life. Thus, for teens it becomes difficult to detect the early stages for the mental
health condition. Thus, it can be stated Agatha needs to be treated with no possible scope of
relapse and her child needs to be monitored for early signs of schizophrenia. However, the
current danger remains in the point of premature birth of mothers with schizophrenia. Thus
Agatha needs to be monitored during the course of her pregnancy to prevent premature birth or
abnormal weight of foetus. Thus, Agatha’s family is asked to remain in touch through calls or
even face to face meetings.
Part 2.3 Description of patient and family/carer education provided: crisis plan,
health/mental health literacy, behaviour management plan, specific intervention etc. Must
include crisis plan that is developmentally appropriate as relevant to risk (key dot points)
Agatha’s family is well aware of her degrading mental condition and it is for the same reason
they have informed the police. However, in scenario of crisis, immediate steps are appreciated.
In case of crisis it is important to rest and relax and if possible increase the dose of medication.
However, at certain times medicine does not respond effectively. The first thing to do is to
activate personal crisis plan. (livingwithschizophreniauk.org, 2019)
Schizophrenia often acts as an immense threat to wellbeing which cannot be managed alone.
Thus, there are number of ways which Agatha or her family can reach for help during the event
of crisis; which are as follows:
Get in touch with consultant psychiatrist if still under psychotherapy
Make an appointment to meet general practitioners
Call medical helpline numbers for obtaining immediate help
However, if things are not under control then it is important to seek sanctuary in a place which
keeps Agatha away from stress. In similar regards, increasing the dose of medication also works
provided the same thing is discussed with doctor beforehand. In addition to that it is important to
take care of the fact to involved Agatha in mode of treatment in order to facilitate patient centred
care.
7
later stages of life. Thus, for teens it becomes difficult to detect the early stages for the mental
health condition. Thus, it can be stated Agatha needs to be treated with no possible scope of
relapse and her child needs to be monitored for early signs of schizophrenia. However, the
current danger remains in the point of premature birth of mothers with schizophrenia. Thus
Agatha needs to be monitored during the course of her pregnancy to prevent premature birth or
abnormal weight of foetus. Thus, Agatha’s family is asked to remain in touch through calls or
even face to face meetings.
Part 2.3 Description of patient and family/carer education provided: crisis plan,
health/mental health literacy, behaviour management plan, specific intervention etc. Must
include crisis plan that is developmentally appropriate as relevant to risk (key dot points)
Agatha’s family is well aware of her degrading mental condition and it is for the same reason
they have informed the police. However, in scenario of crisis, immediate steps are appreciated.
In case of crisis it is important to rest and relax and if possible increase the dose of medication.
However, at certain times medicine does not respond effectively. The first thing to do is to
activate personal crisis plan. (livingwithschizophreniauk.org, 2019)
Schizophrenia often acts as an immense threat to wellbeing which cannot be managed alone.
Thus, there are number of ways which Agatha or her family can reach for help during the event
of crisis; which are as follows:
Get in touch with consultant psychiatrist if still under psychotherapy
Make an appointment to meet general practitioners
Call medical helpline numbers for obtaining immediate help
However, if things are not under control then it is important to seek sanctuary in a place which
keeps Agatha away from stress. In similar regards, increasing the dose of medication also works
provided the same thing is discussed with doctor beforehand. In addition to that it is important to
take care of the fact to involved Agatha in mode of treatment in order to facilitate patient centred
care.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical report and plan
8
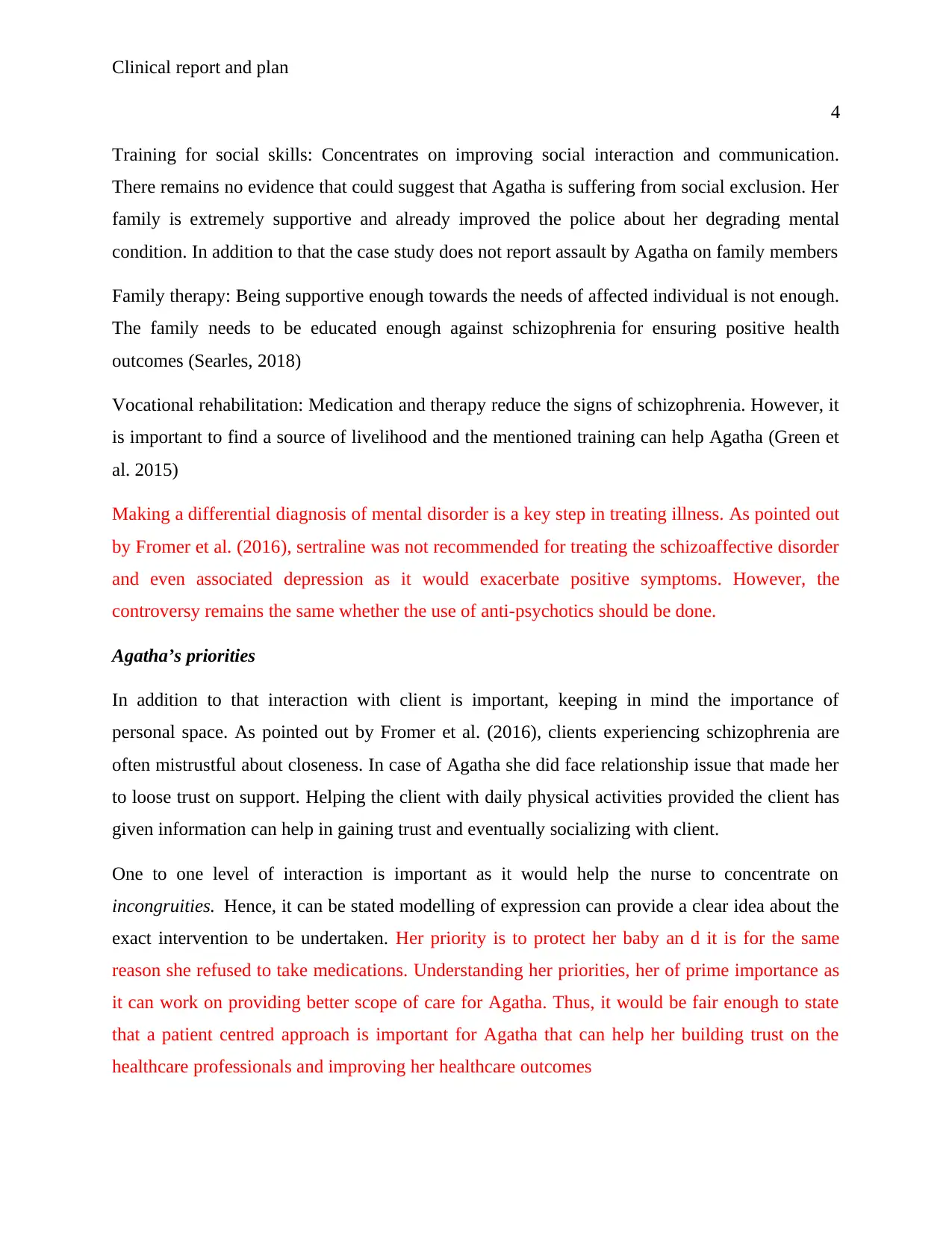
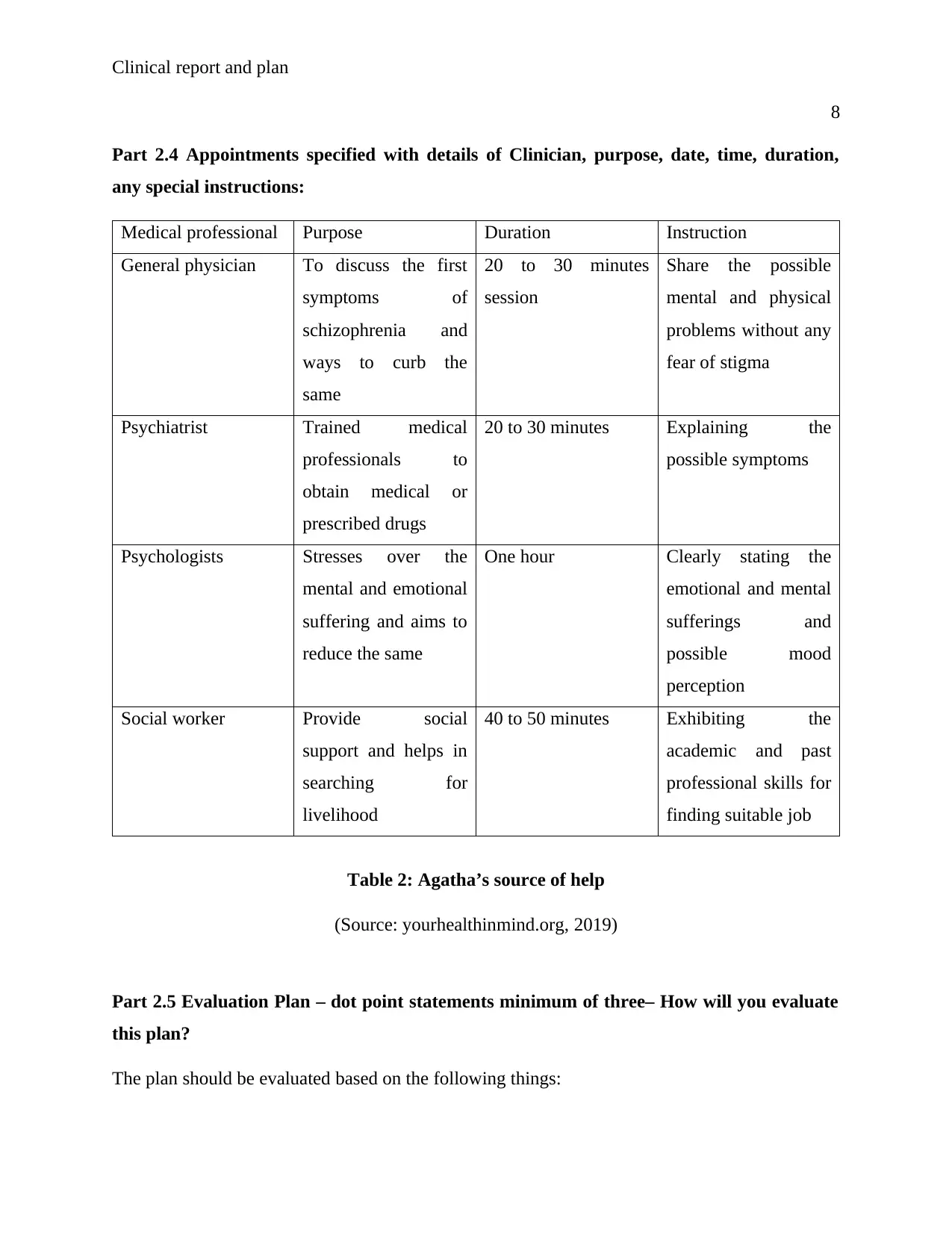
Part 2.4 Appointments specified with details of Clinician, purpose, date, time, duration,
any special instructions:
Medical professional Purpose Duration Instruction
General physician To discuss the first
symptoms of
schizophrenia and
ways to curb the
same
20 to 30 minutes
session
Share the possible
mental and physical
problems without any
fear of stigma
Psychiatrist Trained medical
professionals to
obtain medical or
prescribed drugs
20 to 30 minutes Explaining the
possible symptoms
Psychologists Stresses over the
mental and emotional
suffering and aims to
reduce the same
One hour Clearly stating the
emotional and mental
sufferings and
possible mood
perception
Social worker Provide social
support and helps in
searching for
livelihood
40 to 50 minutes Exhibiting the
academic and past
professional skills for
finding suitable job
Table 2: Agatha’s source of help
(Source: yourhealthinmind.org, 2019)
Part 2.5 Evaluation Plan – dot point statements minimum of three– How will you evaluate
this plan?
The plan should be evaluated based on the following things:
8
Part 2.4 Appointments specified with details of Clinician, purpose, date, time, duration,
any special instructions:
Medical professional Purpose Duration Instruction
General physician To discuss the first
symptoms of
schizophrenia and
ways to curb the
same
20 to 30 minutes
session
Share the possible
mental and physical
problems without any
fear of stigma
Psychiatrist Trained medical
professionals to
obtain medical or
prescribed drugs
20 to 30 minutes Explaining the
possible symptoms
Psychologists Stresses over the
mental and emotional
suffering and aims to
reduce the same
One hour Clearly stating the
emotional and mental
sufferings and
possible mood
perception
Social worker Provide social
support and helps in
searching for
livelihood
40 to 50 minutes Exhibiting the
academic and past
professional skills for
finding suitable job
Table 2: Agatha’s source of help
(Source: yourhealthinmind.org, 2019)
Part 2.5 Evaluation Plan – dot point statements minimum of three– How will you evaluate
this plan?
The plan should be evaluated based on the following things:
Clinical report and plan
9
Level of social interaction exhibited by Agatha before and after therapy
Willingness to consume medication
Analysing the effect of therapy
Relapse prevention plan
Signs of relapse:
Trouble in sleeping
Staying away from social functions
Aggression and suicidal talks
Tips to prevent relapse
Taking medications as per instructions. However, medication is not supported by Agatha and
thus use of psychosocial therapy is important
Working closely with health professionals, long lasting anti-psychotic medications by shots
for long lasting results
Avoiding illegal drugs
Positive paths to manage stress
Enough sleep
9
Level of social interaction exhibited by Agatha before and after therapy
Willingness to consume medication
Analysing the effect of therapy
Relapse prevention plan
Signs of relapse:
Trouble in sleeping
Staying away from social functions
Aggression and suicidal talks
Tips to prevent relapse
Taking medications as per instructions. However, medication is not supported by Agatha and
thus use of psychosocial therapy is important
Working closely with health professionals, long lasting anti-psychotic medications by shots
for long lasting results
Avoiding illegal drugs
Positive paths to manage stress
Enough sleep
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical report and plan
10
Reference list
Casey, D. E. (2003). Long-term treatment goals: enhancing healthy outcomes. CNS
spectrums, 8(S2), 26-28.
Fromer, M., Roussos, P., Sieberts, S. K., Johnson, J. S., Kavanagh, D. H., Perumal, T. M., ...
&Klei, L. L. (2016). Gene expression elucidates functional impact of polygenic risk for
schizophrenia. Nature neuroscience, 19(11), 1442.
Grant, N., Lawrence, M., Preti, A., Wykes, T., &Cella, M. (2017). Social cognition interventions
for people with schizophrenia: a systematic review focussing on methodological quality
and intervention modality. Clinical psychology review, 56, 55-64.
Green, M. F., Horan, W. P., & Lee, J. (2015). Social cognition in schizophrenia. Nature Reviews
Neuroscience, 16(10), 620.
Hasan, A., Falkai, P., Wobrock, T., Lieberman, J., Glenthøj, B., Gattaz, W. F., ... & WFSBP
Task Force on Treatment Guidelines for Schizophrenia. (2017). World Federation of
Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of
schizophrenia–a short version for primary care. International journal of psychiatry in
clinical practice, 21(2), 82-90.
Kerkemeyer, L., Mostardt, S., Biermann, J., Wasem, J., Neumann, A., Walendzik, A., ...
&Breunig-Lyriti, V. (2015). Evaluation of an integrated care program for schizophrenia:
concept and study design. European archives of psychiatry and clinical
neuroscience, 265(2), 155-162.
Lauriello, J., & Perkins, D. O. (2019). Managing Transitions in Care and Adherence to Improve
Outcomes in Schizophrenia. The Journal of clinical psychiatry, 80(2).
mayoclinic.org (2019) Schizophrenia - Diagnosis and treatment - Mayo Clinic. (2019). Retrieved
from https://www.mayoclinic.org/diseases-conditions/schizophrenia/diagnosis-
treatment/drc-20354449
Searles, H. F. (2018). Collected papers on schizophrenia and related subjects. Routledge.
10
Reference list
Casey, D. E. (2003). Long-term treatment goals: enhancing healthy outcomes. CNS
spectrums, 8(S2), 26-28.
Fromer, M., Roussos, P., Sieberts, S. K., Johnson, J. S., Kavanagh, D. H., Perumal, T. M., ...
&Klei, L. L. (2016). Gene expression elucidates functional impact of polygenic risk for
schizophrenia. Nature neuroscience, 19(11), 1442.
Grant, N., Lawrence, M., Preti, A., Wykes, T., &Cella, M. (2017). Social cognition interventions
for people with schizophrenia: a systematic review focussing on methodological quality
and intervention modality. Clinical psychology review, 56, 55-64.
Green, M. F., Horan, W. P., & Lee, J. (2015). Social cognition in schizophrenia. Nature Reviews
Neuroscience, 16(10), 620.
Hasan, A., Falkai, P., Wobrock, T., Lieberman, J., Glenthøj, B., Gattaz, W. F., ... & WFSBP
Task Force on Treatment Guidelines for Schizophrenia. (2017). World Federation of
Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of
schizophrenia–a short version for primary care. International journal of psychiatry in
clinical practice, 21(2), 82-90.
Kerkemeyer, L., Mostardt, S., Biermann, J., Wasem, J., Neumann, A., Walendzik, A., ...
&Breunig-Lyriti, V. (2015). Evaluation of an integrated care program for schizophrenia:
concept and study design. European archives of psychiatry and clinical
neuroscience, 265(2), 155-162.
Lauriello, J., & Perkins, D. O. (2019). Managing Transitions in Care and Adherence to Improve
Outcomes in Schizophrenia. The Journal of clinical psychiatry, 80(2).
mayoclinic.org (2019) Schizophrenia - Diagnosis and treatment - Mayo Clinic. (2019). Retrieved
from https://www.mayoclinic.org/diseases-conditions/schizophrenia/diagnosis-
treatment/drc-20354449
Searles, H. F. (2018). Collected papers on schizophrenia and related subjects. Routledge.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical report and plan
11
Sekar, A., Bialas, A. R., de Rivera, H., Davis, A., Hammond, T. R., Kamitaki, N., ... &
Genovese, G. (2016). Schizophrenia risk from complex variation of complement
component 4. Nature, 530(7589), 177.
Tan, B. L., Lee, S. A., & Lee, J. (2018). Social cognitive interventions for people with
schizophrenia: a systematic review. Asian journal of psychiatry, 35, 115-131.
What to do in a Crisis - Living With Schizophrenia. (2019). Retrieved from
https://www.livingwithschizophreniauk.org/what-to-do-in-a-crisis/
yourhealthinmind.org (2019) Who can help with schizophrenia?. (2019). Retrieved from
https://www.yourhealthinmind.org/mental-illnesses-disorders/schizophrenia/who-can-
help
11
Sekar, A., Bialas, A. R., de Rivera, H., Davis, A., Hammond, T. R., Kamitaki, N., ... &
Genovese, G. (2016). Schizophrenia risk from complex variation of complement
component 4. Nature, 530(7589), 177.
Tan, B. L., Lee, S. A., & Lee, J. (2018). Social cognitive interventions for people with
schizophrenia: a systematic review. Asian journal of psychiatry, 35, 115-131.
What to do in a Crisis - Living With Schizophrenia. (2019). Retrieved from
https://www.livingwithschizophreniauk.org/what-to-do-in-a-crisis/
yourhealthinmind.org (2019) Who can help with schizophrenia?. (2019). Retrieved from
https://www.yourhealthinmind.org/mental-illnesses-disorders/schizophrenia/who-can-
help
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





