Foundations of Medicine 2: Air Pollution and COPD Research Report
VerifiedAdded on 2022/09/14
|10
|2689
|11
Report
AI Summary
This report, prepared for a Foundations of Medicine 2 assignment, investigates the impact of air pollution on individuals with chronic obstructive pulmonary disease (COPD). The research begins with a specific research question formulated using the PICO framework, focusing on the correlation between poor air quality and health outcomes in COPD patients. A comprehensive search strategy was employed, utilizing Google Scholar, Cochrane Library, and the Western Sydney University School of Medicine library database, with keywords such as "health impacts of air pollution" and "COPD vulnerability to air pollution." Inclusion and exclusion criteria were applied to a large pool of initial articles, resulting in the selection of 20 relevant studies published between 2015 and 2020. The findings consistently highlight the detrimental effects of air pollution on COPD patients, including increased mortality, exacerbation of respiratory diseases, and increased hospitalizations. The report discusses the biological plausibility of these effects, noting mechanisms such as inflammatory responses and damage to lung function. Finally, the report identifies gaps in the existing literature, particularly the need for comparative studies between COPD and non-COPD populations exposed to air pollution, and suggests directions for future research, including the need for patient outcome studies. The report also includes an extensive list of references.
Environmental Epidemiology – Assignment 1
Student name: Student ID:
What is your Research Question? (10%)
o What segment of the COPD population is impacted from air pollution?
(P – Patient/ population affected by air pollution includes individual’s chronic
obstructive pulmonary disease (COPD))
o What is the correlation of poor air quality on health outcome on patients with
COPD?
(I – Intervention method for this search strategy includes evaluating the air quality
in the area which leads to the health outcome related to respiratory illnesses)
o How can the impact from air pollution be determined in COPD and non COPD
people?
(C – A comparison of the population exposed to air pollution with population not
exposed to air pollution needs to be evaluated)
o What is the outcome of air pollution on health?
(O– Outcome from the impacts of ait pollution includes lung diseases of several
types, rapid deterioration of coronary heart diseases)
Search Strategy (including data sources, keywords/synonyms, inclusion
and exclusion criteria, a flow chart of search hits, etc) (40%)
In order to conduct this research, data and information will be searched from Google
Scholar, Cochrane Library and the library database of Western Sydney University School
of Medicine. These three data sources will be used and the keywords that have been used
for undertaking this research includes, “health impacts of air pollution”, “effects of air
Student name: Student ID:
What is your Research Question? (10%)
o What segment of the COPD population is impacted from air pollution?
(P – Patient/ population affected by air pollution includes individual’s chronic
obstructive pulmonary disease (COPD))
o What is the correlation of poor air quality on health outcome on patients with
COPD?
(I – Intervention method for this search strategy includes evaluating the air quality
in the area which leads to the health outcome related to respiratory illnesses)
o How can the impact from air pollution be determined in COPD and non COPD
people?
(C – A comparison of the population exposed to air pollution with population not
exposed to air pollution needs to be evaluated)
o What is the outcome of air pollution on health?
(O– Outcome from the impacts of ait pollution includes lung diseases of several
types, rapid deterioration of coronary heart diseases)
Search Strategy (including data sources, keywords/synonyms, inclusion
and exclusion criteria, a flow chart of search hits, etc) (40%)
In order to conduct this research, data and information will be searched from Google
Scholar, Cochrane Library and the library database of Western Sydney University School
of Medicine. These three data sources will be used and the keywords that have been used
for undertaking this research includes, “health impacts of air pollution”, “effects of air
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
400862, Foundations of Medicine 2 – Population Health
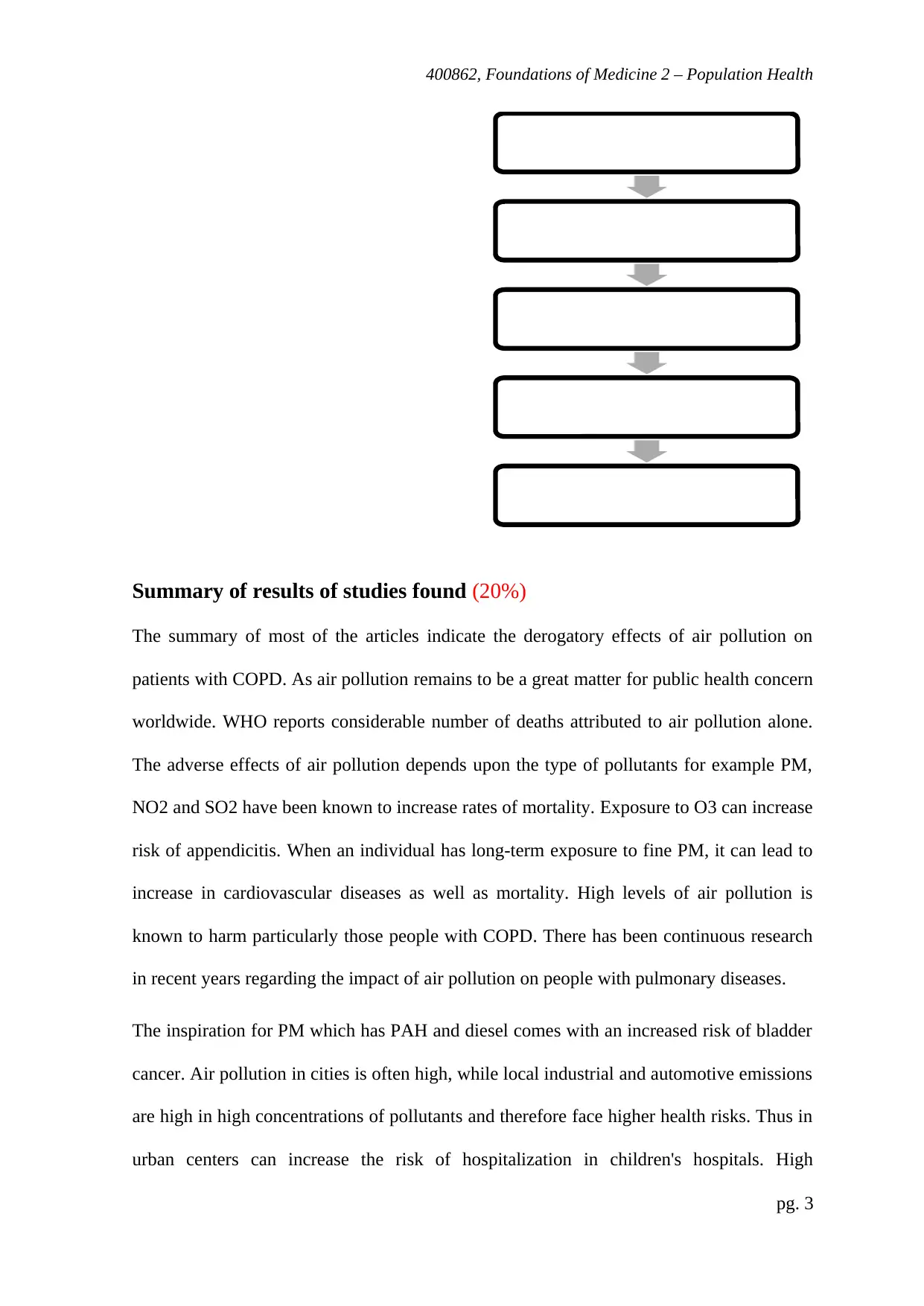
pollution on health”, “diseases caused by air pollution”, “effect of air pollution on COPD
patients”, “COPD vulnerability to air pollution”. The results of search strategy revealed
approximately 200 articles, from which peer-reviewed and recent articles published in the
last 5 years have been used. Time period selected for the article was between 2015 till
2020. 80 articles was obtained from google Scholar, 40 from Cochrane library and 80 from
the library of Western Sydney. Finally, from total of 200 articles, applying exclusion
criteria, 100 articles were rejected. Amongst the 100 articles finalised, almost a 80 articles
was excluded as they had information on specific targeted population only such as
coronary heart patients, with heart diseases, coronary artery diseases, congestive heart
failure, individuals with lung diseases such as asthma, or emphysema, pregnant women,
outdoor workers, older adults and elderly people, children under the age of 14 years and
athletes who exercise vigorously outdoors. These articles did not confirm to the specific
target population that the study aimed at ascertaining. Hence, they were excluded from the
study. Finally, there was 20 articles, which were considered for the purpose of undertaking
this research. 10 articles was selected from Cochrane database, 50 articles from Google
Scholar and 5 from Western Sydney University database.
pg. 2
pollution on health”, “diseases caused by air pollution”, “effect of air pollution on COPD
patients”, “COPD vulnerability to air pollution”. The results of search strategy revealed
approximately 200 articles, from which peer-reviewed and recent articles published in the
last 5 years have been used. Time period selected for the article was between 2015 till
2020. 80 articles was obtained from google Scholar, 40 from Cochrane library and 80 from
the library of Western Sydney. Finally, from total of 200 articles, applying exclusion
criteria, 100 articles were rejected. Amongst the 100 articles finalised, almost a 80 articles
was excluded as they had information on specific targeted population only such as
coronary heart patients, with heart diseases, coronary artery diseases, congestive heart
failure, individuals with lung diseases such as asthma, or emphysema, pregnant women,
outdoor workers, older adults and elderly people, children under the age of 14 years and
athletes who exercise vigorously outdoors. These articles did not confirm to the specific
target population that the study aimed at ascertaining. Hence, they were excluded from the
study. Finally, there was 20 articles, which were considered for the purpose of undertaking
this research. 10 articles was selected from Cochrane database, 50 articles from Google
Scholar and 5 from Western Sydney University database.
pg. 2
400862, Foundations of Medicine 2 – Population Health
Summary of results of studies found (20%)
The summary of most of the articles indicate the derogatory effects of air pollution on
patients with COPD. As air pollution remains to be a great matter for public health concern
worldwide. WHO reports considerable number of deaths attributed to air pollution alone.
The adverse effects of air pollution depends upon the type of pollutants for example PM,
NO2 and SO2 have been known to increase rates of mortality. Exposure to O3 can increase
risk of appendicitis. When an individual has long-term exposure to fine PM, it can lead to
increase in cardiovascular diseases as well as mortality. High levels of air pollution is
known to harm particularly those people with COPD. There has been continuous research
in recent years regarding the impact of air pollution on people with pulmonary diseases.
The inspiration for PM which has PAH and diesel comes with an increased risk of bladder
cancer. Air pollution in cities is often high, while local industrial and automotive emissions
are high in high concentrations of pollutants and therefore face higher health risks. Thus in
urban centers can increase the risk of hospitalization in children's hospitals. High
pg. 3
200 articles obtained (80 Google
Scholar + 40 Cochcrane + 80
Western Sydney University)
Remove non peer-reviewed/
articles older than 5 years
100 articles
Reject articles not having
specific patient distribution+
age+ medical condition criteria
Finally = 20 articles from the
databses
Summary of results of studies found (20%)
The summary of most of the articles indicate the derogatory effects of air pollution on
patients with COPD. As air pollution remains to be a great matter for public health concern
worldwide. WHO reports considerable number of deaths attributed to air pollution alone.
The adverse effects of air pollution depends upon the type of pollutants for example PM,
NO2 and SO2 have been known to increase rates of mortality. Exposure to O3 can increase
risk of appendicitis. When an individual has long-term exposure to fine PM, it can lead to
increase in cardiovascular diseases as well as mortality. High levels of air pollution is
known to harm particularly those people with COPD. There has been continuous research
in recent years regarding the impact of air pollution on people with pulmonary diseases.
The inspiration for PM which has PAH and diesel comes with an increased risk of bladder
cancer. Air pollution in cities is often high, while local industrial and automotive emissions
are high in high concentrations of pollutants and therefore face higher health risks. Thus in
urban centers can increase the risk of hospitalization in children's hospitals. High
pg. 3
200 articles obtained (80 Google
Scholar + 40 Cochcrane + 80
Western Sydney University)
Remove non peer-reviewed/
articles older than 5 years
100 articles
Reject articles not having
specific patient distribution+
age+ medical condition criteria
Finally = 20 articles from the
databses
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
400862, Foundations of Medicine 2 – Population Health
concentrations of environmental particles can cause acute heart attacks and increase
hospitalization of cardiovascular disease. Nanometric particles easily cross the brain
barrier and pass through the central nervous system, where it can cause inflammation and
changes in the blood-brain barrier, increasing the risk of stroke, Parkinson's disease and
neurodevelopment. Indoor air pollutants, such as formaldehyde and benzene, can cause
leukemia. High air pollution is harmful to people, especially those with chronic lung
disease. Adverse effects include decreased lung function, increased infection, increased
respiratory diseases, acute deterioration of chronic obstructive pulmonary disease, asthma
attacks, increased hospital incidence, increased respiratory mortality and incidence of
childhood asthma.
Chronic obstructive pulmonary disease is characterized by an increase in chronic
inflammatory reactions in the airways and lungs from harmful particles or gases. Studies
have shown that women in developing countries are at high risk of chronic obstructive
pulmonary disease from exposure to cooking wood smoke. Atmospheric pollutants, such
as the burning of certain fossil fuels, can cause pneumonia and further impair lung function
in cabbage patients. When patients with chronic obstructive pulmonary disease are exposed
to particle contamination, they tend to receive more acute treatment, hospitalizations and
even death in some cases. Infection is one of the triggers for copy deterioration. Since PM
can provide many microbial surfaces, inhaling PM can lead to more frequent deterioration
of COPD. Other mechanisms, such as damage to mucosal extraction, increased adhesion to
respiratory mucosa cells, and damage to immune system resilience, include negative
effects of impurities.
Epidemiological studies have shown a link between increased air pollution and
cardiopulmonary mortality and morbidity. Increased concentrations of particulate matter
pg. 4
concentrations of environmental particles can cause acute heart attacks and increase
hospitalization of cardiovascular disease. Nanometric particles easily cross the brain
barrier and pass through the central nervous system, where it can cause inflammation and
changes in the blood-brain barrier, increasing the risk of stroke, Parkinson's disease and
neurodevelopment. Indoor air pollutants, such as formaldehyde and benzene, can cause
leukemia. High air pollution is harmful to people, especially those with chronic lung
disease. Adverse effects include decreased lung function, increased infection, increased
respiratory diseases, acute deterioration of chronic obstructive pulmonary disease, asthma
attacks, increased hospital incidence, increased respiratory mortality and incidence of
childhood asthma.
Chronic obstructive pulmonary disease is characterized by an increase in chronic
inflammatory reactions in the airways and lungs from harmful particles or gases. Studies
have shown that women in developing countries are at high risk of chronic obstructive
pulmonary disease from exposure to cooking wood smoke. Atmospheric pollutants, such
as the burning of certain fossil fuels, can cause pneumonia and further impair lung function
in cabbage patients. When patients with chronic obstructive pulmonary disease are exposed
to particle contamination, they tend to receive more acute treatment, hospitalizations and
even death in some cases. Infection is one of the triggers for copy deterioration. Since PM
can provide many microbial surfaces, inhaling PM can lead to more frequent deterioration
of COPD. Other mechanisms, such as damage to mucosal extraction, increased adhesion to
respiratory mucosa cells, and damage to immune system resilience, include negative
effects of impurities.
Epidemiological studies have shown a link between increased air pollution and
cardiopulmonary mortality and morbidity. Increased concentrations of particulate matter
pg. 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
400862, Foundations of Medicine 2 – Population Health
(PM), ozone, nitrogen oxides (NOx) and sulphur dioxide (SO2) in North America and
Western Europe have led to increased morbidity, emergency visits and hospitalizations for
chronic respiratory diseases such as asthma and chronic obstructive pulmonary disease,
according to a multicentre study in North America and Western Europe. In a recent study,
patients with COPD investigated the possible air pollution effects of the respiratory tract.
The results suggest that DEP may play a role in the pathogenesis of chronic lung diseases
such as COPD by changing viability, apoptosis, the release of cytokines and proteins that
regulate CS and alveol epithelial cells and apoptosis.
Air pollution can affect asthma, morbidity, symptoms and responses to treatment. Air
quality plays an important role in early asthma attacks and acts as an asthma trigger that
worsens later in life. Exposure to NO2 in childhood increases the risk of developing
asthma in a child. Studies have shown that air pollution associated with childhood transport
is associated with reduced lung function and long-term respiratory effects in sensitive
children. Exposure to the inner legs can also cause asthma symptoms or worsen asthma.
Prolonged exposure to air pollution can affect children's lungs. Air pollution is associated
with asthma control. Increased air pollution is associated with increased use of asthma by
first responders. Recent exposure to NO2 and possibly O3 may reduce the response in
children with asthma to short-acting beta agonists. Air pollution affects lung cancer. Lung
cancer is one of the most common cancers in the urban population. Studies have shown
that increased traffic is associated with lung cancer. Air pollution, especially PM and NO2,
is associated with an increased risk of lung cancer. PM is significantly associated with lung
cancer, especially adenocarcinoma.
pg. 5
(PM), ozone, nitrogen oxides (NOx) and sulphur dioxide (SO2) in North America and
Western Europe have led to increased morbidity, emergency visits and hospitalizations for
chronic respiratory diseases such as asthma and chronic obstructive pulmonary disease,
according to a multicentre study in North America and Western Europe. In a recent study,
patients with COPD investigated the possible air pollution effects of the respiratory tract.
The results suggest that DEP may play a role in the pathogenesis of chronic lung diseases
such as COPD by changing viability, apoptosis, the release of cytokines and proteins that
regulate CS and alveol epithelial cells and apoptosis.
Air pollution can affect asthma, morbidity, symptoms and responses to treatment. Air
quality plays an important role in early asthma attacks and acts as an asthma trigger that
worsens later in life. Exposure to NO2 in childhood increases the risk of developing
asthma in a child. Studies have shown that air pollution associated with childhood transport
is associated with reduced lung function and long-term respiratory effects in sensitive
children. Exposure to the inner legs can also cause asthma symptoms or worsen asthma.
Prolonged exposure to air pollution can affect children's lungs. Air pollution is associated
with asthma control. Increased air pollution is associated with increased use of asthma by
first responders. Recent exposure to NO2 and possibly O3 may reduce the response in
children with asthma to short-acting beta agonists. Air pollution affects lung cancer. Lung
cancer is one of the most common cancers in the urban population. Studies have shown
that increased traffic is associated with lung cancer. Air pollution, especially PM and NO2,
is associated with an increased risk of lung cancer. PM is significantly associated with lung
cancer, especially adenocarcinoma.
pg. 5
400862, Foundations of Medicine 2 – Population Health
Biological plausibility (10%)
The biological plausibility of this research question lies in ascertaining the underlying
health impacts from air pollution. While air pollution has been known to cause severe and
significant health impacts and outcomes, it is known to be detrimental in patients suffering
from COPD and can reduce their lifespan. It can lead to increased comorbidities and
increase in mortality rates, which is pertinent to explore. Thus, the scope of this research
undertakes such evaluation to understand the impacts from air pollution on patients who
have an underlying condition, COPD.
Gaps in the literature and future research direction(s) (10%)
Most of the articles that has been finalised for undertaking this research signifies the
impact of air pollution on patient with COPD. However, there are no comparison
mechanism adopted for understanding the impact of such pollution on people with COPD
and those with no COPD. Moreover, the patient outcome has not been ascertained in most
cases. Thus, the current scope of research direction will aim at ascertaining a comparative
framework for analysing the impacts of air pollution. Most importantly, the outcome across
varied patients suffering from COPD will be attempted through this research. This study
will aim at finding the final outcome of patient with COPD and those exposed to air
pollution.
pg. 6
Biological plausibility (10%)
The biological plausibility of this research question lies in ascertaining the underlying
health impacts from air pollution. While air pollution has been known to cause severe and
significant health impacts and outcomes, it is known to be detrimental in patients suffering
from COPD and can reduce their lifespan. It can lead to increased comorbidities and
increase in mortality rates, which is pertinent to explore. Thus, the scope of this research
undertakes such evaluation to understand the impacts from air pollution on patients who
have an underlying condition, COPD.
Gaps in the literature and future research direction(s) (10%)
Most of the articles that has been finalised for undertaking this research signifies the
impact of air pollution on patient with COPD. However, there are no comparison
mechanism adopted for understanding the impact of such pollution on people with COPD
and those with no COPD. Moreover, the patient outcome has not been ascertained in most
cases. Thus, the current scope of research direction will aim at ascertaining a comparative
framework for analysing the impacts of air pollution. Most importantly, the outcome across
varied patients suffering from COPD will be attempted through this research. This study
will aim at finding the final outcome of patient with COPD and those exposed to air
pollution.
pg. 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

400862, Foundations of Medicine 2 – Population Health
References
Assad, N. A., Balmes, J., Mehta, S., Cheema, U., & Sood, A. (2015, June). Chronic
obstructive pulmonary disease secondary to household air pollution. In Seminars in
respiratory and critical care medicine (Vol. 36, No. 03, pp. 408-421). Thieme Medical
Publishers.
Berend, N. (2016). Contribution of air pollution to COPD and small airway
dysfunction. Respirology, 21(2), 237-244. DOI: 10.1111/resp.12644.
Bloemsma, L. D., Hoek, G., & Smit, L. A. (2016). Panel studies of air pollution in patients
with COPD: systematic review and meta-analysis. Environmental research, 151, 458-
468. DOI: 10.1016/j.envres.2016.08.018.
Cortez-Lugo, M., Ramírez-Aguilar, M., Pérez-Padilla, R., Sansores-Martínez, R., Ramírez-
Venegas, A., & Barraza-Villarreal, A. (2015). Effect of personal exposure to PM2. 5 on
respiratory health in a Mexican panel of patients with COPD. International journal of
environmental research and public health, 12(9), 10635-10647. DOI:
10.3390/ijerph120910635.
DeVries, R., Kriebel, D., & Sama, S. (2016). Low level air pollution and exacerbation of
existing copd: a case crossover analysis. Environmental Health, 15(1), 98. DOI:
10.1186/s12940-016-0179-z.
DeVries, R., Kriebel, D., & Sama, S. (2017). Outdoor air pollution and COPD-related
emergency department visits, hospital admissions, and mortality: a meta-
analysis. COPD: Journal of Chronic Obstructive Pulmonary Disease, 14(1), 113-121.
DOI: 10.1080/15412555.2016.1216956.
pg. 7
References
Assad, N. A., Balmes, J., Mehta, S., Cheema, U., & Sood, A. (2015, June). Chronic
obstructive pulmonary disease secondary to household air pollution. In Seminars in
respiratory and critical care medicine (Vol. 36, No. 03, pp. 408-421). Thieme Medical
Publishers.
Berend, N. (2016). Contribution of air pollution to COPD and small airway
dysfunction. Respirology, 21(2), 237-244. DOI: 10.1111/resp.12644.
Bloemsma, L. D., Hoek, G., & Smit, L. A. (2016). Panel studies of air pollution in patients
with COPD: systematic review and meta-analysis. Environmental research, 151, 458-
468. DOI: 10.1016/j.envres.2016.08.018.
Cortez-Lugo, M., Ramírez-Aguilar, M., Pérez-Padilla, R., Sansores-Martínez, R., Ramírez-
Venegas, A., & Barraza-Villarreal, A. (2015). Effect of personal exposure to PM2. 5 on
respiratory health in a Mexican panel of patients with COPD. International journal of
environmental research and public health, 12(9), 10635-10647. DOI:
10.3390/ijerph120910635.
DeVries, R., Kriebel, D., & Sama, S. (2016). Low level air pollution and exacerbation of
existing copd: a case crossover analysis. Environmental Health, 15(1), 98. DOI:
10.1186/s12940-016-0179-z.
DeVries, R., Kriebel, D., & Sama, S. (2017). Outdoor air pollution and COPD-related
emergency department visits, hospital admissions, and mortality: a meta-
analysis. COPD: Journal of Chronic Obstructive Pulmonary Disease, 14(1), 113-121.
DOI: 10.1080/15412555.2016.1216956.
pg. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
400862, Foundations of Medicine 2 – Population Health
Ding, P. H., Wang, G. S., Guo, Y. L., Chang, S. C., & Wan, G. H. (2017). Urban air
pollution and meteorological factors affect emergency department visits of elderly
patients with chronic obstructive pulmonary disease in Taiwan. Environmental
Pollution, 224, 751-758. DOI: 10.1016/j.envpol.2016.12.035.
Fisher, J.E., Loft, S., Ulrik, C.S., Raaschou-Nielsen, O., Hertel, O., Tjønneland, A.,
Overvad, K., Nieuwenhuijsen, M.J. and Andersen, Z.J. (2016). Physical activity, air
pollution, and the risk of asthma and chronic obstructive pulmonary disease. American
journal of respiratory and critical care medicine, 194(7), 855-865. DOI:
10.1164/rccm.201510-2036OC.
Hansel, N. N., McCormack, M. C., & Kim, V. (2016). The effects of air pollution and
temperature on COPD. COPD: Journal of Chronic Obstructive Pulmonary
Disease, 13(3), 372-379. DOI: 10.3109/15412555.2015.1089846.
Heinrich, J., & Schikowski, T. (2018). COPD patients as vulnerable subpopulation for
exposure to ambient air pollution. Current environmental health reports, 5(1), 70-76.
DOI: 10.1007/s40572-018-0178-z.
Hu, G., Zhong, N., & Ran, P. (2015). Air pollution and COPD in China. Journal of
thoracic disease, 7(1), 59. DOI: 10.3978/j.issn.2072-1439.2014.12.47.
Jiang, X. Q., Mei, X. D., & Feng, D. (2016). Air pollution and chronic airway diseases:
what should people know and do?. Journal of thoracic disease, 8(1), E31. DOI:
10.3978/j.issn.2072-1439.2015.11.50.
Lee, K.Y., Feng, P.H., Ho, S.C., Chuang, K.J., Chen, T.T., Su, C.L., Liu, W.T. and
Chuang, H.C. (2015). Inter-alpha-trypsin inhibitor heavy chain 4: a novel biomarker for
environmental exposure to particulate air pollution in patients with chronic obstructive
pg. 8
Ding, P. H., Wang, G. S., Guo, Y. L., Chang, S. C., & Wan, G. H. (2017). Urban air
pollution and meteorological factors affect emergency department visits of elderly
patients with chronic obstructive pulmonary disease in Taiwan. Environmental
Pollution, 224, 751-758. DOI: 10.1016/j.envpol.2016.12.035.
Fisher, J.E., Loft, S., Ulrik, C.S., Raaschou-Nielsen, O., Hertel, O., Tjønneland, A.,
Overvad, K., Nieuwenhuijsen, M.J. and Andersen, Z.J. (2016). Physical activity, air
pollution, and the risk of asthma and chronic obstructive pulmonary disease. American
journal of respiratory and critical care medicine, 194(7), 855-865. DOI:
10.1164/rccm.201510-2036OC.
Hansel, N. N., McCormack, M. C., & Kim, V. (2016). The effects of air pollution and
temperature on COPD. COPD: Journal of Chronic Obstructive Pulmonary
Disease, 13(3), 372-379. DOI: 10.3109/15412555.2015.1089846.
Heinrich, J., & Schikowski, T. (2018). COPD patients as vulnerable subpopulation for
exposure to ambient air pollution. Current environmental health reports, 5(1), 70-76.
DOI: 10.1007/s40572-018-0178-z.
Hu, G., Zhong, N., & Ran, P. (2015). Air pollution and COPD in China. Journal of
thoracic disease, 7(1), 59. DOI: 10.3978/j.issn.2072-1439.2014.12.47.
Jiang, X. Q., Mei, X. D., & Feng, D. (2016). Air pollution and chronic airway diseases:
what should people know and do?. Journal of thoracic disease, 8(1), E31. DOI:
10.3978/j.issn.2072-1439.2015.11.50.
Lee, K.Y., Feng, P.H., Ho, S.C., Chuang, K.J., Chen, T.T., Su, C.L., Liu, W.T. and
Chuang, H.C. (2015). Inter-alpha-trypsin inhibitor heavy chain 4: a novel biomarker for
environmental exposure to particulate air pollution in patients with chronic obstructive
pg. 8
400862, Foundations of Medicine 2 – Population Health
pulmonary disease. International journal of chronic obstructive pulmonary disease, 10,
831. doi: 10.2147/COPD.S81611
Li, L., Yang, J., Song, Y. F., Chen, P. Y., & Ou, C. Q. (2016). The burden of COPD
mortality due to ambient air pollution in Guangzhou, China. Scientific reports, 6, 25900.
DOI: 10.1038/srep25900.
Liu, Y., Yan, S., Poh, K., Liu, S., Iyioriobhe, E., & Sterling, D. A. (2016). Impact of air
quality guidelines on COPD sufferers. International journal of chronic obstructive
pulmonary disease, 11, 839. doi: 10.2147/COPD.S49378.
Nakao, M., Ishihara, Y., Kim, C. H., & Hyun, I. G. (2018). The impact of air pollution,
including asian sand dust, on respiratory symptoms and health-related quality of life in
outpatients with chronic respiratory disease in Korea: a panel study. Journal of
Preventive Medicine and Public Health, 51(3), 130. doi: 10.3961/jpmph.18.021.
Paulin, L., & Hansel, N. (2016). Particulate air pollution and impaired lung
function. F1000Research, 5. doi: 10.12688/f1000research.7108.1.
Wang, W., Ying, Y., Wu, Q., Zhang, H., Ma, D., & Xiao, W. (2015). A GIS-based spatial
correlation analysis for ambient air pollution and AECOPD hospitalizations in Jinan,
China. Respiratory medicine, 109(3), 372-378. DOI: 10.1016/j.rmed.2015.01.006.
Wu, S., Ni, Y., Li, H., Pan, L., Yang, D., Baccarelli, A. A., ... & Guo, X. (2016). Short-
term exposure to high ambient air pollution increases airway inflammation and
respiratory symptoms in chronic obstructive pulmonary disease patients in Beijing,
China. Environment international, 94, 76-82. DOI: 10.1016/j.envint.2016.05.004.
pg. 9
pulmonary disease. International journal of chronic obstructive pulmonary disease, 10,
831. doi: 10.2147/COPD.S81611
Li, L., Yang, J., Song, Y. F., Chen, P. Y., & Ou, C. Q. (2016). The burden of COPD
mortality due to ambient air pollution in Guangzhou, China. Scientific reports, 6, 25900.
DOI: 10.1038/srep25900.
Liu, Y., Yan, S., Poh, K., Liu, S., Iyioriobhe, E., & Sterling, D. A. (2016). Impact of air
quality guidelines on COPD sufferers. International journal of chronic obstructive
pulmonary disease, 11, 839. doi: 10.2147/COPD.S49378.
Nakao, M., Ishihara, Y., Kim, C. H., & Hyun, I. G. (2018). The impact of air pollution,
including asian sand dust, on respiratory symptoms and health-related quality of life in
outpatients with chronic respiratory disease in Korea: a panel study. Journal of
Preventive Medicine and Public Health, 51(3), 130. doi: 10.3961/jpmph.18.021.
Paulin, L., & Hansel, N. (2016). Particulate air pollution and impaired lung
function. F1000Research, 5. doi: 10.12688/f1000research.7108.1.
Wang, W., Ying, Y., Wu, Q., Zhang, H., Ma, D., & Xiao, W. (2015). A GIS-based spatial
correlation analysis for ambient air pollution and AECOPD hospitalizations in Jinan,
China. Respiratory medicine, 109(3), 372-378. DOI: 10.1016/j.rmed.2015.01.006.
Wu, S., Ni, Y., Li, H., Pan, L., Yang, D., Baccarelli, A. A., ... & Guo, X. (2016). Short-
term exposure to high ambient air pollution increases airway inflammation and
respiratory symptoms in chronic obstructive pulmonary disease patients in Beijing,
China. Environment international, 94, 76-82. DOI: 10.1016/j.envint.2016.05.004.
pg. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

400862, Foundations of Medicine 2 – Population Health
Zhang, S., Li, G., Tian, L., Guo, Q., & Pan, X. (2016). Short-term exposure to air pollution
and morbidity of COPD and asthma in East Asian area: A systematic review and meta-
analysis. Environmental research, 148, 15-23. DOI: 10.1016/j.envres.2016.03.008.
pg. 10
Zhang, S., Li, G., Tian, L., Guo, Q., & Pan, X. (2016). Short-term exposure to air pollution
and morbidity of COPD and asthma in East Asian area: A systematic review and meta-
analysis. Environmental research, 148, 15-23. DOI: 10.1016/j.envres.2016.03.008.
pg. 10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





