University Nursing Report: Gibbs Reflective Cycle, NURBN3021
VerifiedAdded on 2022/10/13
|9
|2236
|181
Report
AI Summary
This report presents a Gibbs Reflective Cycle analysis of a nursing student's experience managing a patient's airway post-coronary artery bypass graft (CABG) surgery. The student describes the clinical scenario, including the patient's medical history, medications, and the nursing interventions performed. The report details the student's feelings during the experience, including initial nervousness and eventual confidence. An evaluation of the actions taken is provided, highlighting both successes and areas for improvement, such as communication with the healthcare team. The analysis section explores the rationale behind the nursing interventions, referencing relevant literature on airway management, hygiene, and oxygen therapy. The conclusion summarizes the key learning points, and an action plan outlines specific steps the student will take to improve clinical practice in the future, using SMART goals to enhance confidence and communication skills.

Running head: NURSING
Gibbs’ Reflective Cycle
Name of the Student
Name of the University
Gibbs’ Reflective Cycle
Name of the Student
Name of the University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
NURSING
Table of Contents
Description.................................................................................................................................2
Feelings......................................................................................................................................2
Evaluation..................................................................................................................................3
Analysis......................................................................................................................................4
Conclusion..................................................................................................................................5
Action Plan.................................................................................................................................5
Reference-..................................................................................................................................7
NURSING
Table of Contents
Description.................................................................................................................................2
Feelings......................................................................................................................................2
Evaluation..................................................................................................................................3
Analysis......................................................................................................................................4
Conclusion..................................................................................................................................5
Action Plan.................................................................................................................................5
Reference-..................................................................................................................................7
2
NURSING
Description
I was an airway nurse of Edna Murray, who was hospitalized with unstable angina.
Following her angiogram of CABG (Coronary artery Bypass grafts), she was under
observation in a ward. She possessed a history of two CABG with saphenous vein graft to her
right coronary artery (RCA), and one SVG to her left Circumflex artery. Edna also possesses
hypertension and she have a family history of cardiovascular diseases. Edna is prescribed
medicines such as telmisartan, atenolol, ticagrelor, aspirin and rosuvastatin. Scott and Glen
(2015) reported that in adult cardiac surgery patient, post-operative hypoxaemia is a problem
that needs urgent attention. So, I am given the responsibility of airway management of the
patient, as adequate ventilation is necessary in post-operative care of patients. I cleansed my
hands with sanitizer, and helped the patient sit in a semi-Fowler’s position. I checked the
medicine chart to review the medication uptake of Edna. I kept a close eye on the cleanliness
of the room, because dust being a potent allergen can interfere with the airway of such
patient, and cause hypoxia. I assessed her respiratory tract and airway, by asking her to open
her mouth. I checked her Respiratory Rate (RR), SpO2 (Oxygen saturation) level and
detected her respiratory sounds by chest auscultation. At first she was having respiratory
trouble, so I consulted her doctor to prescribe her medications, and helped her with oxygen
therapy by use of a face mask. I kept her under observation during the whole period and
reassessed her status every two hours, and I documented every details in the chart.
Feelings
This was my very first experience with airway management in post-operative care of
a patient who had undergone a major surgery. I was tensed and perplexed but also felt excited
at the beginning, as it would be my very first exposure in such a patient. But, when I went to
her room to check her condition, the smell of medicine made me nervous as I faced the reality
NURSING
Description
I was an airway nurse of Edna Murray, who was hospitalized with unstable angina.
Following her angiogram of CABG (Coronary artery Bypass grafts), she was under
observation in a ward. She possessed a history of two CABG with saphenous vein graft to her
right coronary artery (RCA), and one SVG to her left Circumflex artery. Edna also possesses
hypertension and she have a family history of cardiovascular diseases. Edna is prescribed
medicines such as telmisartan, atenolol, ticagrelor, aspirin and rosuvastatin. Scott and Glen
(2015) reported that in adult cardiac surgery patient, post-operative hypoxaemia is a problem
that needs urgent attention. So, I am given the responsibility of airway management of the
patient, as adequate ventilation is necessary in post-operative care of patients. I cleansed my
hands with sanitizer, and helped the patient sit in a semi-Fowler’s position. I checked the
medicine chart to review the medication uptake of Edna. I kept a close eye on the cleanliness
of the room, because dust being a potent allergen can interfere with the airway of such
patient, and cause hypoxia. I assessed her respiratory tract and airway, by asking her to open
her mouth. I checked her Respiratory Rate (RR), SpO2 (Oxygen saturation) level and
detected her respiratory sounds by chest auscultation. At first she was having respiratory
trouble, so I consulted her doctor to prescribe her medications, and helped her with oxygen
therapy by use of a face mask. I kept her under observation during the whole period and
reassessed her status every two hours, and I documented every details in the chart.
Feelings
This was my very first experience with airway management in post-operative care of
a patient who had undergone a major surgery. I was tensed and perplexed but also felt excited
at the beginning, as it would be my very first exposure in such a patient. But, when I went to
her room to check her condition, the smell of medicine made me nervous as I faced the reality
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
NURSING
that it was my time to take some action. My palms began to sweat profusely and my feet
remained cemented to the ground. Then, I gained courage and followed all the protocols
necessary in patient care. After my first move, I felt a little bit more confident and continued
my work without further hesitation. Levett- Jones et al., (2015) suggested that clinical
placement can be very exciting and overwhelming as well as, is a time, when they get a lot of
mixed feelings. I felt proud when I was able to help the patient successfully. I was also very
happy, thinking that I have successfully completed the work and did not neglect my duty
towards the patient. I was also very excited, and couldn’t wait to share my experience with
my friends and family.
Evaluation
The task was challenging enough for me. I regret the fact that I could not take prompt
action after entering Edna’s room. The Nursing and Midwifery Board of Australia (2019)
suggests that a nurse must incur proper care to people by assessing the patient
comprehensively and must take actions after evaluating the situation. So, I could have acted
sooner because later on during my practice, I can be exposed to more challenging situations. I
feel proud that I did my duties quite successfully and incurred proper care to the patient. But,
there was one mishap which happened on my part. I forgot to communicate with my team
members or with the team leader, about the status of the patient. Apart from the doctor, I did
not communicate with any other members. It was not right on my part, as in my absence it
would have been impossible in emergent conditions for others to intervene, with lack of
knowledge. Stewart (2016) re-emphasized on this issue revealing that a nurse must share
information with doctor and others in duty of a patient, for better patient outcome.
NURSING
that it was my time to take some action. My palms began to sweat profusely and my feet
remained cemented to the ground. Then, I gained courage and followed all the protocols
necessary in patient care. After my first move, I felt a little bit more confident and continued
my work without further hesitation. Levett- Jones et al., (2015) suggested that clinical
placement can be very exciting and overwhelming as well as, is a time, when they get a lot of
mixed feelings. I felt proud when I was able to help the patient successfully. I was also very
happy, thinking that I have successfully completed the work and did not neglect my duty
towards the patient. I was also very excited, and couldn’t wait to share my experience with
my friends and family.
Evaluation
The task was challenging enough for me. I regret the fact that I could not take prompt
action after entering Edna’s room. The Nursing and Midwifery Board of Australia (2019)
suggests that a nurse must incur proper care to people by assessing the patient
comprehensively and must take actions after evaluating the situation. So, I could have acted
sooner because later on during my practice, I can be exposed to more challenging situations. I
feel proud that I did my duties quite successfully and incurred proper care to the patient. But,
there was one mishap which happened on my part. I forgot to communicate with my team
members or with the team leader, about the status of the patient. Apart from the doctor, I did
not communicate with any other members. It was not right on my part, as in my absence it
would have been impossible in emergent conditions for others to intervene, with lack of
knowledge. Stewart (2016) re-emphasized on this issue revealing that a nurse must share
information with doctor and others in duty of a patient, for better patient outcome.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
NURSING
Analysis
My first step in the process of intervention was cleansing my hand properly with
sanitizer. Hand Hygiene Australia (2019) suggested that hand hygiene is the main criteria for
preventing infections and passage of antimicrobial resistance. Then I assisted Edna to sit in a
semi-Fowler’s position. Evidence suggests that oxygenation in a semi-recumbent or semi-
Fowler’s position helps in relaxing the abdominal muscles, enhancing the breathing
(Pourmand et al., 2017). I checked the cleanliness of the room to check the possibility of
allergy. Olivieri et al., (2016) suggested that in respiratory troubles, allergen exposure may
lead to elevation of IgE level causing enhanced complications. I checked her airway tract as
well as documented her RR, SpO2 level and performed chest auscultation. Sarkar et al.,
(2015) revealed that auscultation helps in assessing airflow through the trachea and bronchial
tree. Measuring of SpO2 and respiratory rate is very important part of airway management, as
SpO2 below 90% can require oxygenation to prevent desaturation (White et al., 2017). I
found her having trouble with her breathing so I contacted the doctor to prescribe her
medications and also helped her with oxygen therapy. Oxygen masks can help in improving
the oxygen saturation. A standard oxygen mask provides oxygen at a rate of 10 l/min,
providing 60% oxygen (Lester & Berkow, 2015). The Nursing and Midwifery Council (2019)
stated that a nurse must assess the situation and act likewise to minimise the risk of the
patient. Through my experience of the first day I was able to do that. I forgot to acknowledge
the other persons of the team regarding the status of the patient. That could have caused
potential harm to the patient’s life. This is one incident that I could have avoided with proper
action. For comprehensive care of patients a nurse must be prompt along with being
empathetic towards her. I felt that I could have reassessed her airway along with watching her
vitals every time when I checked the patient. This could have dealt with the problem of the
patient more efficiently. The initial hindrance in this whole process was my reluctance. But,
NURSING
Analysis
My first step in the process of intervention was cleansing my hand properly with
sanitizer. Hand Hygiene Australia (2019) suggested that hand hygiene is the main criteria for
preventing infections and passage of antimicrobial resistance. Then I assisted Edna to sit in a
semi-Fowler’s position. Evidence suggests that oxygenation in a semi-recumbent or semi-
Fowler’s position helps in relaxing the abdominal muscles, enhancing the breathing
(Pourmand et al., 2017). I checked the cleanliness of the room to check the possibility of
allergy. Olivieri et al., (2016) suggested that in respiratory troubles, allergen exposure may
lead to elevation of IgE level causing enhanced complications. I checked her airway tract as
well as documented her RR, SpO2 level and performed chest auscultation. Sarkar et al.,
(2015) revealed that auscultation helps in assessing airflow through the trachea and bronchial
tree. Measuring of SpO2 and respiratory rate is very important part of airway management, as
SpO2 below 90% can require oxygenation to prevent desaturation (White et al., 2017). I
found her having trouble with her breathing so I contacted the doctor to prescribe her
medications and also helped her with oxygen therapy. Oxygen masks can help in improving
the oxygen saturation. A standard oxygen mask provides oxygen at a rate of 10 l/min,
providing 60% oxygen (Lester & Berkow, 2015). The Nursing and Midwifery Council (2019)
stated that a nurse must assess the situation and act likewise to minimise the risk of the
patient. Through my experience of the first day I was able to do that. I forgot to acknowledge
the other persons of the team regarding the status of the patient. That could have caused
potential harm to the patient’s life. This is one incident that I could have avoided with proper
action. For comprehensive care of patients a nurse must be prompt along with being
empathetic towards her. I felt that I could have reassessed her airway along with watching her
vitals every time when I checked the patient. This could have dealt with the problem of the
patient more efficiently. The initial hindrance in this whole process was my reluctance. But,
5
NURSING
after I overcame that problem I acted in the best interest of the patient to provide best care
possible. Koehn et al., (2016) suggested that initiatives must be taken by a nurse, who have
priorly committed mistakes and they must take proper actions to improve the outcomes of the
patient. The authors suggested that most of the nurses improved their service and patient care,
learning from the mistakes. So, I must also take proper actions to treat my nervousness and
for better patient-care.
Conclusion
In conclusion, I have performed more or less well in providing patient care and
securing her airways. But, again I did many mistakes, where I can improve myself in near
future to provide comprehensive care to patients. I was reluctant to intervene in patient care
being nervous and confused. Then, even after I performed all the protocols efficiently I forgot
to communicate with my team members apart from the doctor. This could have caused
potential risks to patient in my absence. I learned from the whole process that I need to be
more confident, and do away with my nervousness and reluctance for providing better
service. I should also improve my communication skills and should not be distracted while
looking after patients. That way, I could have informed my colleagues and the team leader
about the patient situation. I could have acted more promptly in the emergent situation. But,
in future I look forward to provide service to patients with same efficiency, overcoming my
shortcomings and improving myself consequently.
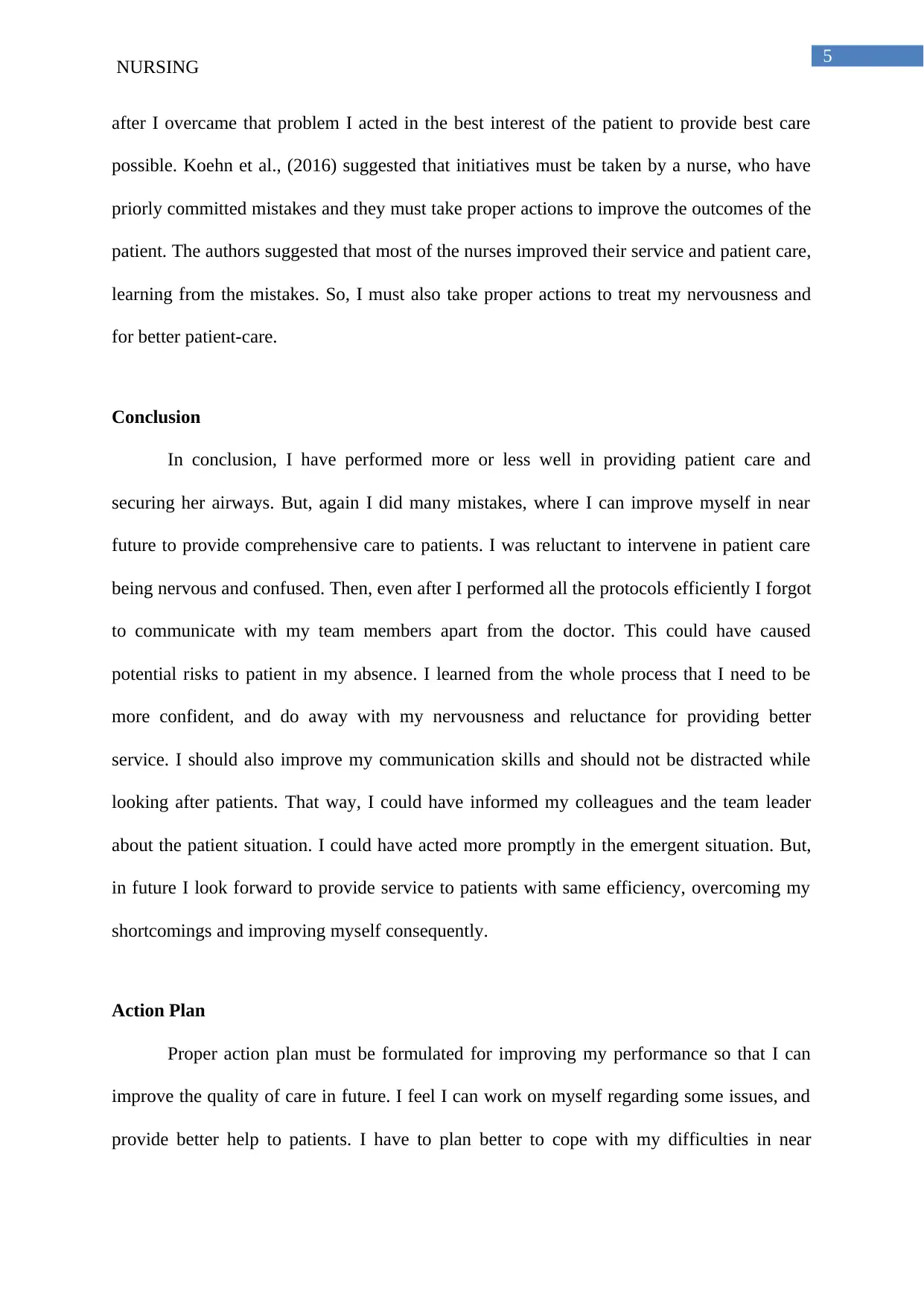
Action Plan
Proper action plan must be formulated for improving my performance so that I can
improve the quality of care in future. I feel I can work on myself regarding some issues, and
provide better help to patients. I have to plan better to cope with my difficulties in near
NURSING
after I overcame that problem I acted in the best interest of the patient to provide best care
possible. Koehn et al., (2016) suggested that initiatives must be taken by a nurse, who have
priorly committed mistakes and they must take proper actions to improve the outcomes of the
patient. The authors suggested that most of the nurses improved their service and patient care,
learning from the mistakes. So, I must also take proper actions to treat my nervousness and
for better patient-care.
Conclusion
In conclusion, I have performed more or less well in providing patient care and
securing her airways. But, again I did many mistakes, where I can improve myself in near
future to provide comprehensive care to patients. I was reluctant to intervene in patient care
being nervous and confused. Then, even after I performed all the protocols efficiently I forgot
to communicate with my team members apart from the doctor. This could have caused
potential risks to patient in my absence. I learned from the whole process that I need to be
more confident, and do away with my nervousness and reluctance for providing better
service. I should also improve my communication skills and should not be distracted while
looking after patients. That way, I could have informed my colleagues and the team leader
about the patient situation. I could have acted more promptly in the emergent situation. But,
in future I look forward to provide service to patients with same efficiency, overcoming my
shortcomings and improving myself consequently.
Action Plan
Proper action plan must be formulated for improving my performance so that I can
improve the quality of care in future. I feel I can work on myself regarding some issues, and
provide better help to patients. I have to plan better to cope with my difficulties in near
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
NURSING
future. For that I can plan properly and make a routine to improve my skills. The action plan
is delineated here using SMART Goal, as it is an efficient manner (Revello & Fields, 2015):-
S (SPECIFIC) I aim to increase my efficiency for better outcome of patient
and want to deal with my problems of reluctance, nervousness,
and distraction. I want to more efficiently secure airways of
patient.
M(MEASURABLE) I want to improve my skills within one week by gradually
increasing the number of patients. First, I will start with
treating ten patients per day and then gradually increase the
number of patients.
A(Achievable) I want to improvise by training myself and seeking help from
my senior colleagues, to guide me and impart their knowledge,
so that I can help my patients without hesitation.
R(Relevant) I want to work on my skills, overcome my shortcomings and
improve my concentration by meditation. I plan to hear
encouraging stories and see videos regarding nursing
profession, to attain more confidence.
T(Time Bound) I want to improve my skills and diminish the errors and work
on my drawbacks within one week of my next placement so
that maximum patients are benefited at the earliest and also so
that I can achieve considerably in my profession.
NURSING
future. For that I can plan properly and make a routine to improve my skills. The action plan
is delineated here using SMART Goal, as it is an efficient manner (Revello & Fields, 2015):-
S (SPECIFIC) I aim to increase my efficiency for better outcome of patient
and want to deal with my problems of reluctance, nervousness,
and distraction. I want to more efficiently secure airways of
patient.
M(MEASURABLE) I want to improve my skills within one week by gradually
increasing the number of patients. First, I will start with
treating ten patients per day and then gradually increase the
number of patients.
A(Achievable) I want to improvise by training myself and seeking help from
my senior colleagues, to guide me and impart their knowledge,
so that I can help my patients without hesitation.
R(Relevant) I want to work on my skills, overcome my shortcomings and
improve my concentration by meditation. I plan to hear
encouraging stories and see videos regarding nursing
profession, to attain more confidence.
T(Time Bound) I want to improve my skills and diminish the errors and work
on my drawbacks within one week of my next placement so
that maximum patients are benefited at the earliest and also so
that I can achieve considerably in my profession.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING
Reference-
Hand Hygiene Australia. (2019). Hand Hygiene. Access Date: 30th July, 2019.[Online].
Retrieved from: https://www.hha.org.au/
Koehn, A. R., Ebright, P. R., & Draucker, C. B. (2016). Nurses' experiences with errors in
nursing. Nursing outlook, 64(6), 566-574.
Lester, L., & Berkow, L. (2015). Airway Emergencies. Anesthesia Emergencies.
Levett-Jones, T., Pitt, V., Courtney-Pratt, H., Harbrow, G., & Rossiter, R. (2015). What are
the primary concerns of nursing students as they prepare for and contemplate their
first clinical placement experience?. Nurse education in practice, 15(4), 304-309.
Nursing and Midwifery Board Of Australia. Code of Ethics for Nurses in Australia. Access
Date: 30th July, 2019. [Online]. Retrieved from: file:///D:/PPT%20Materials/code
%20of%20nurse%20australia.pdf
Olivieri, M., Heinrich, J., Schlünssen, V., Antó, J. M., Forsberg, B., Janson, C., ... & Tischer,
C. (2016). The risk of respiratory symptoms on allergen exposure increases with
increasing specific IgE levels. Allergy, 71(6), 859-868.
Pourmand, A., Robinson, C., Dorwart, K., & O'Connell, F. (2017). Pre-oxygenation:
Implications in emergency airway management. The American journal of emergency
medicine, 35(8), 1177-1183.
Revello, K., & Fields, W. (2015). An educational intervention to increase nurse adherence in
eliciting patient daily goals. Rehabilitation Nursing, 40(5), 320-326.
Sarkar, M., Madabhavi, I., Niranjan, N., & Dogra, M. (2015). Auscultation of the respiratory
system. Annals of thoracic medicine, 10(3), 158.
NURSING
Reference-
Hand Hygiene Australia. (2019). Hand Hygiene. Access Date: 30th July, 2019.[Online].
Retrieved from: https://www.hha.org.au/
Koehn, A. R., Ebright, P. R., & Draucker, C. B. (2016). Nurses' experiences with errors in
nursing. Nursing outlook, 64(6), 566-574.
Lester, L., & Berkow, L. (2015). Airway Emergencies. Anesthesia Emergencies.
Levett-Jones, T., Pitt, V., Courtney-Pratt, H., Harbrow, G., & Rossiter, R. (2015). What are
the primary concerns of nursing students as they prepare for and contemplate their
first clinical placement experience?. Nurse education in practice, 15(4), 304-309.
Nursing and Midwifery Board Of Australia. Code of Ethics for Nurses in Australia. Access
Date: 30th July, 2019. [Online]. Retrieved from: file:///D:/PPT%20Materials/code
%20of%20nurse%20australia.pdf
Olivieri, M., Heinrich, J., Schlünssen, V., Antó, J. M., Forsberg, B., Janson, C., ... & Tischer,
C. (2016). The risk of respiratory symptoms on allergen exposure increases with
increasing specific IgE levels. Allergy, 71(6), 859-868.
Pourmand, A., Robinson, C., Dorwart, K., & O'Connell, F. (2017). Pre-oxygenation:
Implications in emergency airway management. The American journal of emergency
medicine, 35(8), 1177-1183.
Revello, K., & Fields, W. (2015). An educational intervention to increase nurse adherence in
eliciting patient daily goals. Rehabilitation Nursing, 40(5), 320-326.
Sarkar, M., Madabhavi, I., Niranjan, N., & Dogra, M. (2015). Auscultation of the respiratory
system. Annals of thoracic medicine, 10(3), 158.
8
NURSING
Stephens, R. S., & Whitman, G. J. (2015). Postoperative critical care of the adult cardiac
surgical patient. Part I: routine postoperative care. Critical care medicine, 43(7),
1477-1497.
Stewart, K. R. (2016). SBAR, communication, and patient safety: An integrated literature
review.
White, L. D., Melhuish, T. M., White, L. K., & Wallace, L. A. (2017). Apnoeic oxygenation
during intubation: a systematic review and meta-analysis. Anaesthesia and intensive
care, 45(1), 21-27.
NURSING
Stephens, R. S., & Whitman, G. J. (2015). Postoperative critical care of the adult cardiac
surgical patient. Part I: routine postoperative care. Critical care medicine, 43(7),
1477-1497.
Stewart, K. R. (2016). SBAR, communication, and patient safety: An integrated literature
review.
White, L. D., Melhuish, T. M., White, L. K., & Wallace, L. A. (2017). Apnoeic oxygenation
during intubation: a systematic review and meta-analysis. Anaesthesia and intensive
care, 45(1), 21-27.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




