UTS Nursing: Complex Patient Plan of Care - Alice McCallum Case Study
VerifiedAdded on 2022/09/06
|11
|3082
|9
Report
AI Summary
This report provides a comprehensive analysis of Alice McCallum's nursing plan of care, focusing on the assessment data, identified patient problems, and the proposed nursing interventions. The report addresses two primary medical conditions: hypoxemia (low oxygen levels) and the risk of increased temperatures (fever). For hypoxemia, the analysis includes the pathophysiology, assessment data (SpO2 of 93%, cool peripheries, and increased work of breathing), and nursing interventions such as supplemental oxygen administration, raising the head of the bed, deep breathing exercises, and medication. The report also examines the expected outcomes, such as increased oxygen levels, reduced work of breathing, and improved tissue perfusion. The second condition, increased temperatures, is explored by examining the pathophysiology of fever, assessment data (temperature of 38.2°C), and the relevant nursing interventions, which include administering antipyretics and employing cooling methods. The report references the case study and incorporates relevant literature to support the analysis, emphasizing the importance of patient rights, quality care, professionalism, and the role of the nurse as a patient advocate. The report is structured around the nursing process or clinical reasoning cycle, offering a practical approach to patient care planning.
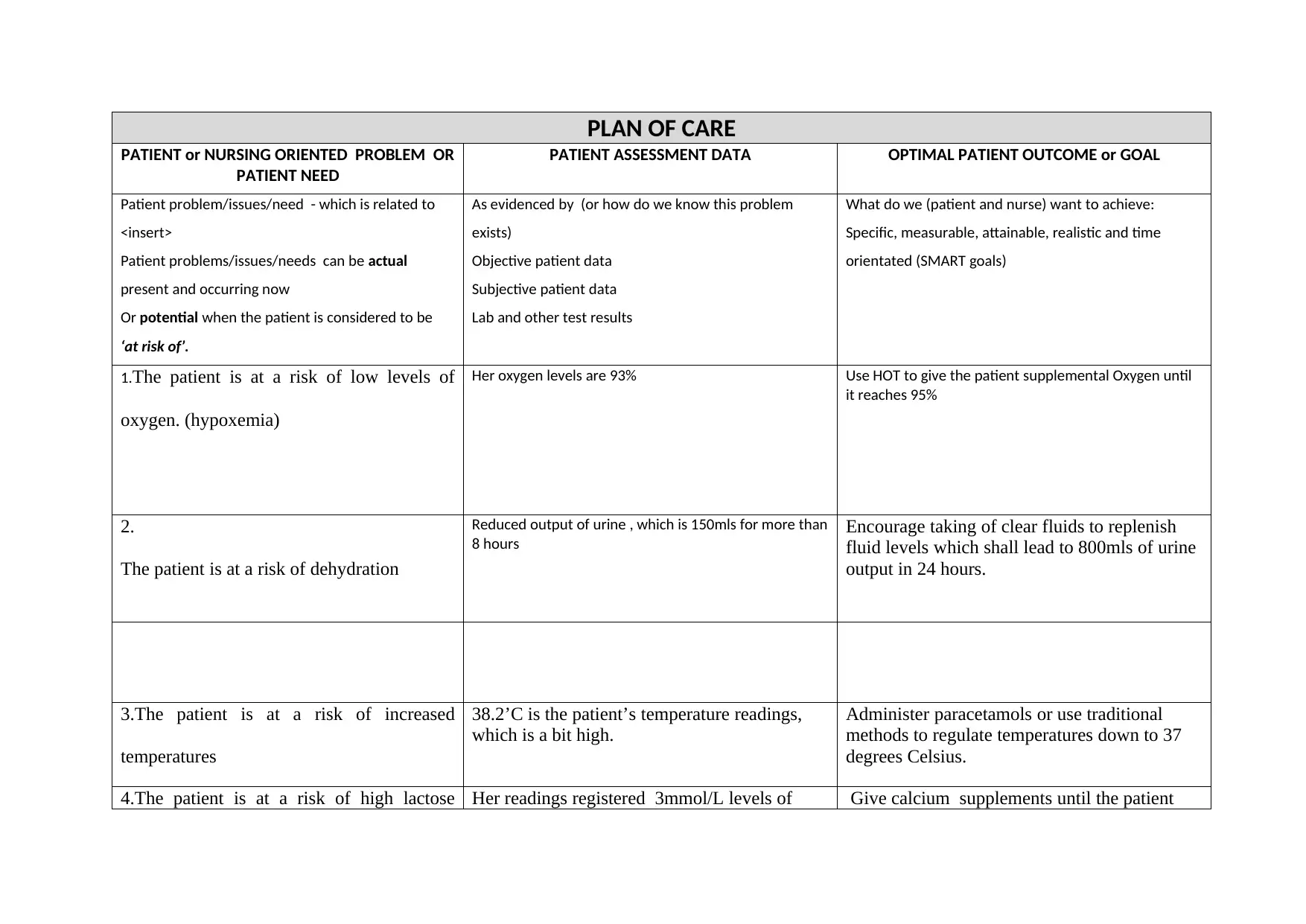
PLAN OF CARE
PATIENT or NURSING ORIENTED PROBLEM OR
PATIENT NEED
PATIENT ASSESSMENT DATA OPTIMAL PATIENT OUTCOME or GOAL
Patient problem/issues/need - which is related to
<insert>
Patient problems/issues/needs can be actual
present and occurring now
Or potential when the patient is considered to be
‘at risk of’.
As evidenced by (or how do we know this problem
exists)
Objective patient data
Subjective patient data
Lab and other test results
What do we (patient and nurse) want to achieve:
Specific, measurable, attainable, realistic and time
orientated (SMART goals)
1.The patient is at a risk of low levels of
oxygen. (hypoxemia)
Her oxygen levels are 93% Use HOT to give the patient supplemental Oxygen until
it reaches 95%
2.
The patient is at a risk of dehydration
Reduced output of urine , which is 150mls for more than
8 hours
Encourage taking of clear fluids to replenish
fluid levels which shall lead to 800mls of urine
output in 24 hours.
3.The patient is at a risk of increased
temperatures
38.2’C is the patient’s temperature readings,
which is a bit high.
Administer paracetamols or use traditional
methods to regulate temperatures down to 37
degrees Celsius.
4.The patient is at a risk of high lactose Her readings registered 3mmol/L levels of Give calcium supplements until the patient
PATIENT or NURSING ORIENTED PROBLEM OR
PATIENT NEED
PATIENT ASSESSMENT DATA OPTIMAL PATIENT OUTCOME or GOAL
Patient problem/issues/need - which is related to
<insert>
Patient problems/issues/needs can be actual
present and occurring now
Or potential when the patient is considered to be
‘at risk of’.
As evidenced by (or how do we know this problem
exists)
Objective patient data
Subjective patient data
Lab and other test results
What do we (patient and nurse) want to achieve:
Specific, measurable, attainable, realistic and time
orientated (SMART goals)
1.The patient is at a risk of low levels of
oxygen. (hypoxemia)
Her oxygen levels are 93% Use HOT to give the patient supplemental Oxygen until
it reaches 95%
2.
The patient is at a risk of dehydration
Reduced output of urine , which is 150mls for more than
8 hours
Encourage taking of clear fluids to replenish
fluid levels which shall lead to 800mls of urine
output in 24 hours.
3.The patient is at a risk of increased
temperatures
38.2’C is the patient’s temperature readings,
which is a bit high.
Administer paracetamols or use traditional
methods to regulate temperatures down to 37
degrees Celsius.
4.The patient is at a risk of high lactose Her readings registered 3mmol/L levels of Give calcium supplements until the patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
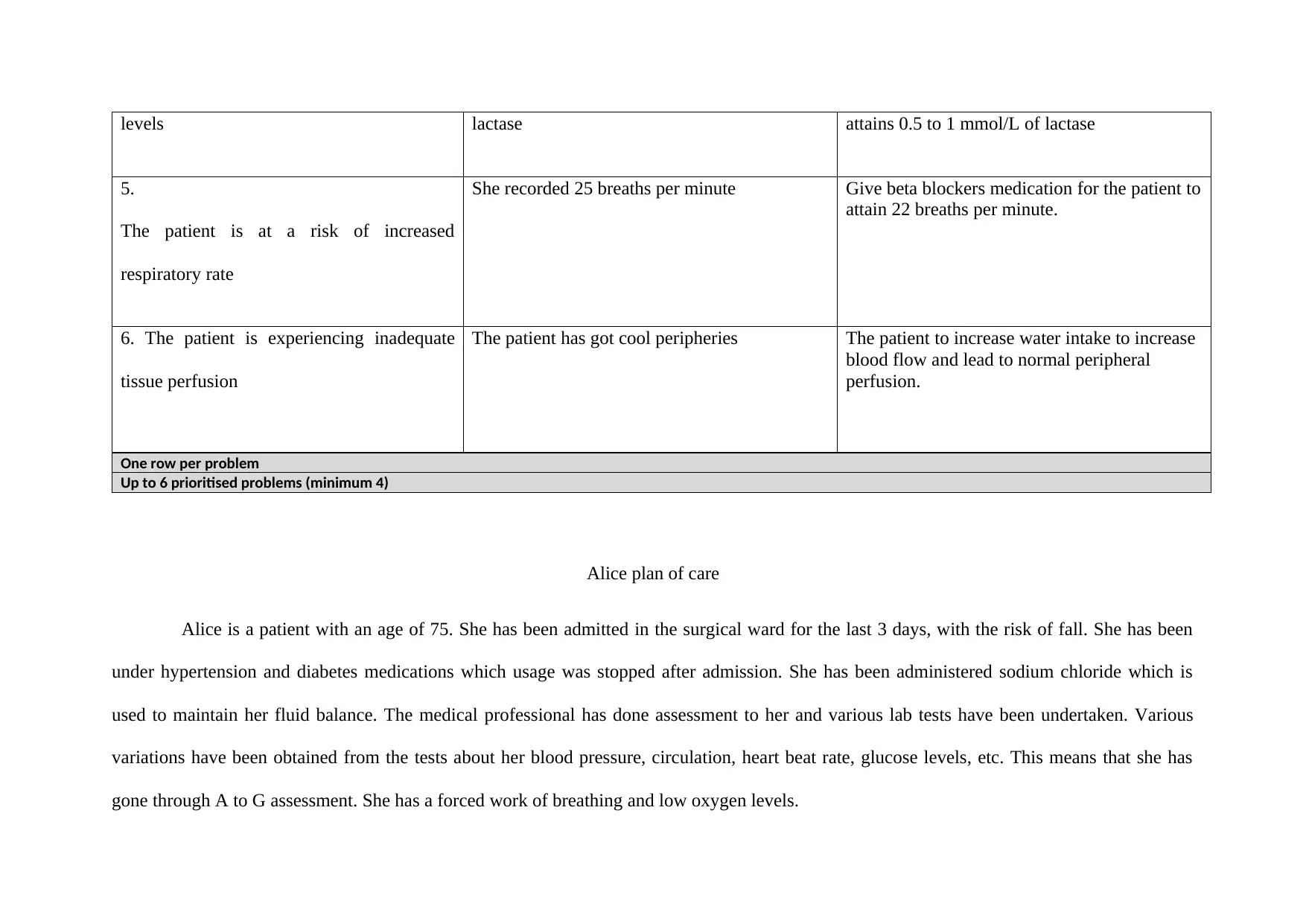
levels lactase attains 0.5 to 1 mmol/L of lactase
5.
The patient is at a risk of increased
respiratory rate
She recorded 25 breaths per minute Give beta blockers medication for the patient to
attain 22 breaths per minute.
6. The patient is experiencing inadequate
tissue perfusion
The patient has got cool peripheries The patient to increase water intake to increase
blood flow and lead to normal peripheral
perfusion.
One row per problem
Up to 6 prioritised problems (minimum 4)
Alice plan of care
Alice is a patient with an age of 75. She has been admitted in the surgical ward for the last 3 days, with the risk of fall. She has been
under hypertension and diabetes medications which usage was stopped after admission. She has been administered sodium chloride which is
used to maintain her fluid balance. The medical professional has done assessment to her and various lab tests have been undertaken. Various
variations have been obtained from the tests about her blood pressure, circulation, heart beat rate, glucose levels, etc. This means that she has
gone through A to G assessment. She has a forced work of breathing and low oxygen levels.
5.
The patient is at a risk of increased
respiratory rate
She recorded 25 breaths per minute Give beta blockers medication for the patient to
attain 22 breaths per minute.
6. The patient is experiencing inadequate
tissue perfusion
The patient has got cool peripheries The patient to increase water intake to increase
blood flow and lead to normal peripheral
perfusion.
One row per problem
Up to 6 prioritised problems (minimum 4)
Alice plan of care
Alice is a patient with an age of 75. She has been admitted in the surgical ward for the last 3 days, with the risk of fall. She has been
under hypertension and diabetes medications which usage was stopped after admission. She has been administered sodium chloride which is
used to maintain her fluid balance. The medical professional has done assessment to her and various lab tests have been undertaken. Various
variations have been obtained from the tests about her blood pressure, circulation, heart beat rate, glucose levels, etc. This means that she has
gone through A to G assessment. She has a forced work of breathing and low oxygen levels.
In this paper, I will address two medical conditions basing them on the assessment, lab results and the criteria presented in the patient’s plan of
care. These conditions will enable me to look at what a nurse/medical practitioner can do to ensure they are cured for the safety of the patient.
This shall be done in line to the patient’s rights ensuring quality care, professionalism and at the same time acting as the patient’s advocate.
One of the medical problems include low oxygen levels, also called hypoxemia. Its assessment data as provided in care plan is 93%
registering low oxygen levels. The pathophysiology of this condition is that it exists when there is reduction of oxygen pressure in the blood
below the normal range. Tissue hypoxia exists when the amount of oxygen is reduced in the body tissues (Koelwyn, Jones, & Moslehi 2014). In
patients with COPD, the predominat hypoxia is the mismatching of V/Q.in the presence or the absence of alveolar hypoventilation, (Adak,
Maity, Ghosh, & Mondal 2014). The hypoxemia that is simple to correct is the one caused by V/Q mismatching because only a little amounts of
supplemental oxygen are needed for LTOT (Negro & Hodder 2013). Hypoxemia is a problem that leads to more ventilation and leads to dyspnea
and other signs and symptoms, (Chao, Wood, & Gonzalez 2011). In patients with COPD, chronic alveolar hypoxia leads to the development of
pulmonale – right ventricular hypertrophy in the absence or presence of overt right ventricular failure, (Anderson et al 2019).
There are four types of hypoxia, referred to as hypoxic hypoxia, stagnant hypoxia, histotoxic hypoxia and hypemic hypoxia (McDonnell &
Chandraharan 2014). They all have the same impacts to a patient. Hypoxemia may be caused by heart conditions such as the heart defects and
lung conditions such as bronchitis and asthma, (Javed & Moore 2018). In the case provided above, the oxygen levels have reduced to 93%
instead of 95%. Another symptom from the medical assessment that shows that there is inadequate oxygen in the patient’s circulatory system is
the poor tissue perfusion due to cool peripheries. This means that the oxygen in the blood is not enough to reach all the body parts hence the
care. These conditions will enable me to look at what a nurse/medical practitioner can do to ensure they are cured for the safety of the patient.
This shall be done in line to the patient’s rights ensuring quality care, professionalism and at the same time acting as the patient’s advocate.
One of the medical problems include low oxygen levels, also called hypoxemia. Its assessment data as provided in care plan is 93%
registering low oxygen levels. The pathophysiology of this condition is that it exists when there is reduction of oxygen pressure in the blood
below the normal range. Tissue hypoxia exists when the amount of oxygen is reduced in the body tissues (Koelwyn, Jones, & Moslehi 2014). In
patients with COPD, the predominat hypoxia is the mismatching of V/Q.in the presence or the absence of alveolar hypoventilation, (Adak,
Maity, Ghosh, & Mondal 2014). The hypoxemia that is simple to correct is the one caused by V/Q mismatching because only a little amounts of
supplemental oxygen are needed for LTOT (Negro & Hodder 2013). Hypoxemia is a problem that leads to more ventilation and leads to dyspnea
and other signs and symptoms, (Chao, Wood, & Gonzalez 2011). In patients with COPD, chronic alveolar hypoxia leads to the development of
pulmonale – right ventricular hypertrophy in the absence or presence of overt right ventricular failure, (Anderson et al 2019).
There are four types of hypoxia, referred to as hypoxic hypoxia, stagnant hypoxia, histotoxic hypoxia and hypemic hypoxia (McDonnell &
Chandraharan 2014). They all have the same impacts to a patient. Hypoxemia may be caused by heart conditions such as the heart defects and
lung conditions such as bronchitis and asthma, (Javed & Moore 2018). In the case provided above, the oxygen levels have reduced to 93%
instead of 95%. Another symptom from the medical assessment that shows that there is inadequate oxygen in the patient’s circulatory system is
the poor tissue perfusion due to cool peripheries. This means that the oxygen in the blood is not enough to reach all the body parts hence the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
inadequate tissue perfusion. Alice suffers high work of breathing because the heart is straining to supply the blood to the body parts. The signs
and symptoms of hypoxemia include changes in the colour of the skin where the patient may look pale or reddish, confusion just as Alice is, a
fast heart rate, a high rate of breathing, sweating and also wheezing. All these symptoms may not appear at the same time. Poor tissue perfusion
due to cool peripheries is also a symptom in Alice during assessment, an indication of less oxygen in the circulatory system that can reach all the
body parts, (Ait-Oufella & Bakker 2016).
Medical interventions for this condition include giving supplemental oxygen by the use of HOT, ("Supplemental Oxygen Devices with
Automatic or Manual Presentation,"). This provides the body with the extra needed oxygen to support all the body vital functions. An oxygen
concentrator is used to give the patient oxygen that is higher than the oxygen available in the air.
Another intervention is raising the head of the patient off the bed that facilitates effective breathing and descent of the diaphragm. This makes it
possible to maximize inhalation and decrease the increased breathing work in the patient. The patient is as well able to gain relief due to the
raised position. poor tissue perfusion due to cool peripheries
Intervention involves practicing deep breathing and coughing techniques which enables the patient to clearly open the airway and maintain their
levels of oxygen. The nurse taches the patient controlled coughing by taking a deep breath in and deeply cough with a slightly open mouth. The
patient takes a medium breath and makes sound to push air out. the exercise is done for three to four times until they get instructions to cough.
Dehydration may be done in this case if the patient has thick and tenacious secretions that shows the need of extra fluids. Another intervention
and symptoms of hypoxemia include changes in the colour of the skin where the patient may look pale or reddish, confusion just as Alice is, a
fast heart rate, a high rate of breathing, sweating and also wheezing. All these symptoms may not appear at the same time. Poor tissue perfusion
due to cool peripheries is also a symptom in Alice during assessment, an indication of less oxygen in the circulatory system that can reach all the
body parts, (Ait-Oufella & Bakker 2016).
Medical interventions for this condition include giving supplemental oxygen by the use of HOT, ("Supplemental Oxygen Devices with
Automatic or Manual Presentation,"). This provides the body with the extra needed oxygen to support all the body vital functions. An oxygen
concentrator is used to give the patient oxygen that is higher than the oxygen available in the air.
Another intervention is raising the head of the patient off the bed that facilitates effective breathing and descent of the diaphragm. This makes it
possible to maximize inhalation and decrease the increased breathing work in the patient. The patient is as well able to gain relief due to the
raised position. poor tissue perfusion due to cool peripheries
Intervention involves practicing deep breathing and coughing techniques which enables the patient to clearly open the airway and maintain their
levels of oxygen. The nurse taches the patient controlled coughing by taking a deep breath in and deeply cough with a slightly open mouth. The
patient takes a medium breath and makes sound to push air out. the exercise is done for three to four times until they get instructions to cough.
Dehydration may be done in this case if the patient has thick and tenacious secretions that shows the need of extra fluids. Another intervention
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
involves Oxygen therapy and equipment. In case the patient is on supplemental oxygen, the equipment used should be turned on and always set
in the required way to ensure that it is well connected to the source of oxygen. In case a portable oxygen supply tank is being used, the oxygen
levels should be checked. The practitioner should ensure that Alice is also connected to the oxygen flow port if there is the use of medical air.
Another intervention is that the nurse should assess the need of bronchodilators that can be used to open the airway after relaxing smooth
muscles especially when a patient suffers from COPD, (Thompson 2015). Adequate hydration should as well be maintained to decrease the
thickness of pulmonary secretions for easy expectoration.
Oral suctioning is another intervention that is necessary when the patient is not able to clear secretions, mucous, or the foreign debris from the
mouth and the pharynx. Weakened cough may hinder a patient from clearing the secretions from the mouth and the throat.
Another intervention involves relieving the patient of pain to enable reduced oxygen needs because pain increases the body’s metabolic demands
which in turn leads to increased supply of oxygen. Devices that enhance secretion clearance such as vests may be given to the patients. This
depends on the situation of the patient.
Another intervention involves frequent rests in between activities. Patients with hypoxemia get fatigue easily and so they should be allowed to
rest frequently. The underlying causes of hypoxia should be verified by making complete respiratory and cardiovascular assessments that may
finally reveal the abnormalities they have.
in the required way to ensure that it is well connected to the source of oxygen. In case a portable oxygen supply tank is being used, the oxygen
levels should be checked. The practitioner should ensure that Alice is also connected to the oxygen flow port if there is the use of medical air.
Another intervention is that the nurse should assess the need of bronchodilators that can be used to open the airway after relaxing smooth
muscles especially when a patient suffers from COPD, (Thompson 2015). Adequate hydration should as well be maintained to decrease the
thickness of pulmonary secretions for easy expectoration.
Oral suctioning is another intervention that is necessary when the patient is not able to clear secretions, mucous, or the foreign debris from the
mouth and the pharynx. Weakened cough may hinder a patient from clearing the secretions from the mouth and the throat.
Another intervention involves relieving the patient of pain to enable reduced oxygen needs because pain increases the body’s metabolic demands
which in turn leads to increased supply of oxygen. Devices that enhance secretion clearance such as vests may be given to the patients. This
depends on the situation of the patient.
Another intervention involves frequent rests in between activities. Patients with hypoxemia get fatigue easily and so they should be allowed to
rest frequently. The underlying causes of hypoxia should be verified by making complete respiratory and cardiovascular assessments that may
finally reveal the abnormalities they have.
Another intervention involves anxiety and depression which is a common COPD co – morbidity. Anxiety comes from inability to breath
effectively and chronic shortness of breath. These two can be relieved through retraining the patient, counselling, using exercising techniques
and /or giving anti-anxiety medications when necessary.
The evidence of reduced hypoxemia is increased oxygen levels in the blood of up to 95% that reduces the work of breathing, (Javed &
Moore 2018). The signs and symptoms of hypoxia reduces drastically after increased oxygen. In this case, it means that confusion from place to
place like in Alice reduces, respiratory rate comes back to normal, she receives normal tissue perfusion by changing the red and pale skin to
normal. Stress and anxiety in the patient reduces and she stars looking relieved.
The other medical problem I will discuss is the risk of increased temperatures. Alice temperatures read 82 ‘c which seems a little bit
higher. High temperatures are realized through high fever after coming into contact with the patient. The immediate action after realizing that a
patient’s temperatures are high, the nurse should take the necessary measures to calm them down to 37 degrees Celsius. The assessment data of
Alice in this case shows that she registered a high temperature of 38.2 ‘C.The pathophysiology of fever is that it is in non-infectious disorders
such as myocardial infarction and neoplasms, (Hall 2010). For example, post-surgery patients can undergo some days of fever. There is
neurogenic fever that emerges from the central nervous system due to impaired hypothalamus caused by trauma. These fevers are characterized
by high temperatures and it is not associated with sweating. There are patterns of fever, namely intermittent, remittent, sustained or a relapsing
fever (Ogoina 2011). In a remittent fever, the body temperature of the patient does not return to normal and varies in degrees either direction. In
effectively and chronic shortness of breath. These two can be relieved through retraining the patient, counselling, using exercising techniques
and /or giving anti-anxiety medications when necessary.
The evidence of reduced hypoxemia is increased oxygen levels in the blood of up to 95% that reduces the work of breathing, (Javed &
Moore 2018). The signs and symptoms of hypoxia reduces drastically after increased oxygen. In this case, it means that confusion from place to
place like in Alice reduces, respiratory rate comes back to normal, she receives normal tissue perfusion by changing the red and pale skin to
normal. Stress and anxiety in the patient reduces and she stars looking relieved.
The other medical problem I will discuss is the risk of increased temperatures. Alice temperatures read 82 ‘c which seems a little bit
higher. High temperatures are realized through high fever after coming into contact with the patient. The immediate action after realizing that a
patient’s temperatures are high, the nurse should take the necessary measures to calm them down to 37 degrees Celsius. The assessment data of
Alice in this case shows that she registered a high temperature of 38.2 ‘C.The pathophysiology of fever is that it is in non-infectious disorders
such as myocardial infarction and neoplasms, (Hall 2010). For example, post-surgery patients can undergo some days of fever. There is
neurogenic fever that emerges from the central nervous system due to impaired hypothalamus caused by trauma. These fevers are characterized
by high temperatures and it is not associated with sweating. There are patterns of fever, namely intermittent, remittent, sustained or a relapsing
fever (Ogoina 2011). In a remittent fever, the body temperature of the patient does not return to normal and varies in degrees either direction. In
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
intermittent fever, the patient’s body temperature returns to normal at least on a single time within 24 hours. In a sustained or continuous fever,
the body temperature of the patient remains above normal with less variations. They are brought about by drugs.
There is recurrent or relapsing fever which contains one or a number of fever episodes where in some days the patient experiences normal
temperatures and in other days’ experiences abnormal body temperatures. They are brought about by infectious diseases such as fungal. Another
clue that causes fever is the relationship of the heart rate and the body’s temperature elevation. High temperatures leads to high heart beat rate
and a rapid heartbeat rate. There are stages of fever through which a patient’s signs and symptoms can be identified, (Sung 2017). These stages
include prodromal stage where the patient displays nonspecific symptoms such as fatigue and general malaise. The second stage is called chill
where the patients feels chilled and develops shaking and elevated temperatures. The patient’s skin becomes pale and ends up covering the body
with clothes or the purpose of energy conservation. After this, the patient starts feeling warm again. The third stage is called flush in which the
skin becomes flushed as a result of vasodilation of the cutaneous skin layer. At the stage the patient feels too hot. The other stage includes
defervescence in which the patient sweats profusely. The patient’s fever breaks and then the body temperature comes back to normal.
The common signs and symptoms of fever include dehydration due to tachypnoea and tachycardia that bring profuse sweating and vapour losses
as a result of increased respiratory rate, (Holtz 2019). Fever is evident in Alice due to high respiratory rate too. Fever manifests itself in form of
high metabolic rate, and high oxygen needs.
the body temperature of the patient remains above normal with less variations. They are brought about by drugs.
There is recurrent or relapsing fever which contains one or a number of fever episodes where in some days the patient experiences normal
temperatures and in other days’ experiences abnormal body temperatures. They are brought about by infectious diseases such as fungal. Another
clue that causes fever is the relationship of the heart rate and the body’s temperature elevation. High temperatures leads to high heart beat rate
and a rapid heartbeat rate. There are stages of fever through which a patient’s signs and symptoms can be identified, (Sung 2017). These stages
include prodromal stage where the patient displays nonspecific symptoms such as fatigue and general malaise. The second stage is called chill
where the patients feels chilled and develops shaking and elevated temperatures. The patient’s skin becomes pale and ends up covering the body
with clothes or the purpose of energy conservation. After this, the patient starts feeling warm again. The third stage is called flush in which the
skin becomes flushed as a result of vasodilation of the cutaneous skin layer. At the stage the patient feels too hot. The other stage includes
defervescence in which the patient sweats profusely. The patient’s fever breaks and then the body temperature comes back to normal.
The common signs and symptoms of fever include dehydration due to tachypnoea and tachycardia that bring profuse sweating and vapour losses
as a result of increased respiratory rate, (Holtz 2019). Fever is evident in Alice due to high respiratory rate too. Fever manifests itself in form of
high metabolic rate, and high oxygen needs.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The interventions of high temperatures include assessing the patient’s temperature after every four hours where if the temperatures are
greater than 100.4 per md order, the nurse administers the antipyretics, (Khardori 2012). The other intervention is encouraging the patient to take
more fluids to calm the system after every two hours. The other intervention is urging the patient to rate their energy levels in a scale of 1 to 10,
where 10 should be the highest energy within 72 hours. The nurse should remove excess blankets when the patient feels cold and offer extra
warmth when the patient feels chilled. Another intervention includes providing prescribed IV fluids as according to the physician’s order,
provide good oral hygiene to protect herpetic lesions in the mouth. To ensure comfort, the nurse should provide dry clothing and bed linens. the
other intervention is offering antipyretics as ordered especially in this case of Alice where temperatures are above 38.5 ‘C. the other intervention
includes providing TSB (Temperature of water) to enhance heat loss through evaporation and conduction. The other intervention involves
monitoring WBC, HTC and other laboratory tests. This enables the nurse to recognize infections and dehydration in the patient. Elevated WBC
like in Alice case shows infection presence while elevated HTC indicates that the patient is dehydrated.
After using these interventions, the evidence is reduced body temperatures. The patient stops complaining of chills and fevers with
time. Profuse sweating comes to an end and the patient can respond well to the underlying environmental conditions, the patient’s circulatory
rate and respiratory rates also comes back to normal. poor tissue perfusion due to cool peripheries
When nursing assessment and the right interventions are done in the right manner and appropriately, the health professional does the right
diagnosis that ultimately treats the patients’ underlying medical condition. This is done with professionalism and maintaining quality care and
the patient’s rights.
greater than 100.4 per md order, the nurse administers the antipyretics, (Khardori 2012). The other intervention is encouraging the patient to take
more fluids to calm the system after every two hours. The other intervention is urging the patient to rate their energy levels in a scale of 1 to 10,
where 10 should be the highest energy within 72 hours. The nurse should remove excess blankets when the patient feels cold and offer extra
warmth when the patient feels chilled. Another intervention includes providing prescribed IV fluids as according to the physician’s order,
provide good oral hygiene to protect herpetic lesions in the mouth. To ensure comfort, the nurse should provide dry clothing and bed linens. the
other intervention is offering antipyretics as ordered especially in this case of Alice where temperatures are above 38.5 ‘C. the other intervention
includes providing TSB (Temperature of water) to enhance heat loss through evaporation and conduction. The other intervention involves
monitoring WBC, HTC and other laboratory tests. This enables the nurse to recognize infections and dehydration in the patient. Elevated WBC
like in Alice case shows infection presence while elevated HTC indicates that the patient is dehydrated.
After using these interventions, the evidence is reduced body temperatures. The patient stops complaining of chills and fevers with
time. Profuse sweating comes to an end and the patient can respond well to the underlying environmental conditions, the patient’s circulatory
rate and respiratory rates also comes back to normal. poor tissue perfusion due to cool peripheries
When nursing assessment and the right interventions are done in the right manner and appropriately, the health professional does the right
diagnosis that ultimately treats the patients’ underlying medical condition. This is done with professionalism and maintaining quality care and
the patient’s rights.

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Adak, A., Maity, C., Ghosh, K., & Mondal, K. (2014). Alteration of Predominant Gastrointestinal Flora and Oxidative Damage of Large
Intestine Under Simulated Hypobaric Hypoxia. Zeitschrift für Gastroenterologie, 52(02), 180-186. doi:10.1055/s-0033-1336007
Ait-Oufella, H., & Bakker, J. (2016). Understanding clinical signs of poor tissue perfusion during septic shock. Intensive Care
Medicine, 42(12), 2070-2072. doi:10.1007/s00134-016-4250-6
Anderson, R. H., Krishna, K., Mussato, K. A., Redington, A., Tweddell, J. S., & Tretter, J. (2019). Anderson’s Pediatric Cardiology E-Book. St.
Louis, MO: Elsevier Health Sciences.
Chao, J., Wood, J. G., & Gonzalez, N. C. (2011). Alveolar macrophages initiate the systemic microvascular inflammatory response to alveolar
hypoxia. Respiratory Physiology & Neurobiology, 178(3), 439-448. doi:10.1016/j.resp.2011.03.008
Hall, J. E. (2010). FARSI-Guyton and Hall Textbook of Medical Physiology. St. Louis, MO: Elsevier Health Sciences.
Holtz, D. (2019). Signs and Symptoms. Emergency Medicine, 1-42. doi:10.1093/med/9780190852955.003.0001
Javed, J. K., & Moore, J. E. (2018). Respiratory Failure and Hypoxemia (DRAFT). Oxford Medicine Online.
doi:10.1093/med/9780190612474.003.0006
Javed, J. K., & Moore, J. E. (2018). Respiratory Failure and Hypoxemia (DRAFT). Oxford Medicine Online.
doi:10.1093/med/9780190612474.003.0006
Adak, A., Maity, C., Ghosh, K., & Mondal, K. (2014). Alteration of Predominant Gastrointestinal Flora and Oxidative Damage of Large
Intestine Under Simulated Hypobaric Hypoxia. Zeitschrift für Gastroenterologie, 52(02), 180-186. doi:10.1055/s-0033-1336007
Ait-Oufella, H., & Bakker, J. (2016). Understanding clinical signs of poor tissue perfusion during septic shock. Intensive Care
Medicine, 42(12), 2070-2072. doi:10.1007/s00134-016-4250-6
Anderson, R. H., Krishna, K., Mussato, K. A., Redington, A., Tweddell, J. S., & Tretter, J. (2019). Anderson’s Pediatric Cardiology E-Book. St.
Louis, MO: Elsevier Health Sciences.
Chao, J., Wood, J. G., & Gonzalez, N. C. (2011). Alveolar macrophages initiate the systemic microvascular inflammatory response to alveolar
hypoxia. Respiratory Physiology & Neurobiology, 178(3), 439-448. doi:10.1016/j.resp.2011.03.008
Hall, J. E. (2010). FARSI-Guyton and Hall Textbook of Medical Physiology. St. Louis, MO: Elsevier Health Sciences.
Holtz, D. (2019). Signs and Symptoms. Emergency Medicine, 1-42. doi:10.1093/med/9780190852955.003.0001
Javed, J. K., & Moore, J. E. (2018). Respiratory Failure and Hypoxemia (DRAFT). Oxford Medicine Online.
doi:10.1093/med/9780190612474.003.0006
Javed, J. K., & Moore, J. E. (2018). Respiratory Failure and Hypoxemia (DRAFT). Oxford Medicine Online.
doi:10.1093/med/9780190612474.003.0006
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Khardori, N. M. (2012). Interventions in Infectious Disease Emergencies, An Issue of Medical Clinics,. St. Louis, MO: Elsevier Health
Sciences.
Koelwyn, G. J., Jones, L. W., & Moslehi, J. (2014). Unravelling the Causes of Reduced Peak Oxygen Consumption in Patients With
Cancer. Journal of the American College of Cardiology, 64(13), 1320-1322. doi:10.1016/j.jacc.2014.07.949
McDonnell, S., & Chandraharan, E. (2014). The Pathophysiology of CTGs and Types of Intrapartum Hypoxia. Current Women's Health
Reviews, 9(3), 158-168. doi:10.2174/157340480903140131111654
Negro, R. W., & Hodder, R. V. (2013). Long-term oxygen therapy: New insights and perspectives. Berlin, Germany: Springer Science &
Business Media.
Ogoina, D. (2011). Fever, fever patterns and diseases called ‘fever’ – A review. Journal of Infection and Public Health, 4(3), 108-124.
doi:10.1016/j.jiph.2011.05.002
Sung, H. (2017). Spectacle Fever: The Politics of Unbalanced Stages. National Gugak Center, 36, 11-24. doi:10.29028/jngc.2017.36.011
Supplemental Oxygen Devices with Automatic or Manual Presentation. (n.d.). doi:10.4271/arp4287a
Thompson, H. J. (2015). Evidence-Base for Fever Interventions Following Stroke. Stroke, 46(5), e98-e100. doi:10.1161/strokeaha.115.008188
Sciences.
Koelwyn, G. J., Jones, L. W., & Moslehi, J. (2014). Unravelling the Causes of Reduced Peak Oxygen Consumption in Patients With
Cancer. Journal of the American College of Cardiology, 64(13), 1320-1322. doi:10.1016/j.jacc.2014.07.949
McDonnell, S., & Chandraharan, E. (2014). The Pathophysiology of CTGs and Types of Intrapartum Hypoxia. Current Women's Health
Reviews, 9(3), 158-168. doi:10.2174/157340480903140131111654
Negro, R. W., & Hodder, R. V. (2013). Long-term oxygen therapy: New insights and perspectives. Berlin, Germany: Springer Science &
Business Media.
Ogoina, D. (2011). Fever, fever patterns and diseases called ‘fever’ – A review. Journal of Infection and Public Health, 4(3), 108-124.
doi:10.1016/j.jiph.2011.05.002
Sung, H. (2017). Spectacle Fever: The Politics of Unbalanced Stages. National Gugak Center, 36, 11-24. doi:10.29028/jngc.2017.36.011
Supplemental Oxygen Devices with Automatic or Manual Presentation. (n.d.). doi:10.4271/arp4287a
Thompson, H. J. (2015). Evidence-Base for Fever Interventions Following Stroke. Stroke, 46(5), e98-e100. doi:10.1161/strokeaha.115.008188
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





