Amy's Case Study: Therapeutics 3 Report on Alzheimer's Medications
VerifiedAdded on 2021/06/17
|19
|4669
|89
Report
AI Summary
This report presents a comprehensive medication review for Amy, a patient diagnosed with Alzheimer's disease. It details her medical history, presenting complaints, and current medications, including acetylcholinesterase inhibitors and NMDA receptor antagonists. The report explores the progression of the disease, transition to palliative care, and medications used during this phase, such as antidepressants (SSRIs) and morphine for pain management. It covers the diagnostic process, expected medications, and the challenges faced during the patient's end-of-life, emphasizing the importance of palliative care in improving the quality of life. Laboratory results and imaging findings are included to support the diagnosis, along with recommendations for maintaining the patient's well-being. The report highlights the significance of comfort care, routine maintenance, and effective communication in managing the patient's physical, emotional, and spiritual distress during the final stages of the disease. The primary goal of this report is to present a medication review for achieving appropriate and safe use of medicines, for the patient Amy.

Running head: THERAPEUTICS 3
Amy’s case story
Name of the Student
Name of the University
Author Note
Amy’s case story
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1THERAPEUTICS 3
Executive summary
A Medication Management Review is formulated with the aim of providing medication
management related services to all patients in an aged care setting or the community. Medication
management review services most often involve taking an interview of the patient, followed by a
clinical assessment. The information is generally disseminated in the form of a written referral
report to the GP. The primary aim of this report is to present a medication review for achieving
appropriate and safe use of medicines, for the patient Amy. This will be accomplished by
addressing the potential or current medications that she must be administered or medicines that
are or might interfere with the desired treatment outcomes, thereby deteriorating the quality of
life of the patient. The patient Amy, initially named Lan migrated to Australia, at 18 years of age
and stays with her son Eric and octogenarian mother Mei. Her recent symptoms of forgetfulness
and memory disruption have been noticed by her son. These might suggest the onset of
Alzheimer’s disease that results in a gradual decline in the working memory of an individual.
The report will elaborate on the condition that she has been diagnosed, and will also illustrate the
medications that she is expected show compliance to, after diagnosis, and during the transition to
palliative care.
Executive summary
A Medication Management Review is formulated with the aim of providing medication
management related services to all patients in an aged care setting or the community. Medication
management review services most often involve taking an interview of the patient, followed by a
clinical assessment. The information is generally disseminated in the form of a written referral
report to the GP. The primary aim of this report is to present a medication review for achieving
appropriate and safe use of medicines, for the patient Amy. This will be accomplished by
addressing the potential or current medications that she must be administered or medicines that
are or might interfere with the desired treatment outcomes, thereby deteriorating the quality of
life of the patient. The patient Amy, initially named Lan migrated to Australia, at 18 years of age
and stays with her son Eric and octogenarian mother Mei. Her recent symptoms of forgetfulness
and memory disruption have been noticed by her son. These might suggest the onset of
Alzheimer’s disease that results in a gradual decline in the working memory of an individual.
The report will elaborate on the condition that she has been diagnosed, and will also illustrate the
medications that she is expected show compliance to, after diagnosis, and during the transition to
palliative care.
2THERAPEUTICS 3
Table of Contents
Part A...............................................................................................................................................3
Diagnosed condition....................................................................................................................3
Expected Medications..................................................................................................................5
Summary of assumption..............................................................................................................6
Medicines that were used during transition to palliative care and medications required
during the progress to end-of-life............................................................................................6
GP letter...................................................................................................................................8
Patient Demographics............................................................................................................10
Medical Condition.................................................................................................................11
Patient History.......................................................................................................................11
Presenting complaints............................................................................................................11
Medication history.................................................................................................................11
Current medications...............................................................................................................12
Laboratory results..................................................................................................................12
Table of recommendations........................................................................................................13
Maintenance of the quality of life..............................................................................................14
Table of Contents
Part A...............................................................................................................................................3
Diagnosed condition....................................................................................................................3
Expected Medications..................................................................................................................5
Summary of assumption..............................................................................................................6
Medicines that were used during transition to palliative care and medications required
during the progress to end-of-life............................................................................................6
GP letter...................................................................................................................................8
Patient Demographics............................................................................................................10
Medical Condition.................................................................................................................11
Patient History.......................................................................................................................11
Presenting complaints............................................................................................................11
Medication history.................................................................................................................11
Current medications...............................................................................................................12
Laboratory results..................................................................................................................12
Table of recommendations........................................................................................................13
Maintenance of the quality of life..............................................................................................14
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3THERAPEUTICS 3
Part A
Diagnosed condition
The patient Amy first reported problems in finding appropriate words and was also found
to repeat herself, while participating in conversations. This was noticed by her son Eric, who also
noted that his mother faced difficulties in concentrating on certain tasks for long period of time.
Furthermore, memory deficits were also heightened by the fact that she forgot to pay the
telephone bills for two consecutive months. This behaviour was quite unlikely of her and made
her son worried. Furthermore, it is quite evident from Amy’s story that she is gradually facing
problems in remembering things or words that have already been communicated, such as the
visit of her son with his partner. The aforementioned symptoms and presenting complaints led to
the diagnosis of Alzheimer’s disease. This was usually diagnosed based on the medical history,
the information from the close relatives and behavioural observations. Persisting
neuropsychological and neurological features also supported the diagnosis of Alzheimer’s
disease that can ne defined as a condition involving a chronic neurodegenerative disease. This
condition usually worsens over time (1). This has also been established as the major reason of
dementia in around 60-70% individuals.
Research evidences have investigated the most common symptoms of the condition as
short term memory loss that makes it difficult for the affected individuals to remember recent
events. The gradual loss of bodily functions often makes it difficult for the individual to form an
active part of the society and community, and ultimately results in death (2). According to the
reports, there were approximately 46.8million people suffering from dementia on a global scale.
Furthermore, the report also suggested that 58% of individuals with dementia and Alzheimer’s
Part A
Diagnosed condition
The patient Amy first reported problems in finding appropriate words and was also found
to repeat herself, while participating in conversations. This was noticed by her son Eric, who also
noted that his mother faced difficulties in concentrating on certain tasks for long period of time.
Furthermore, memory deficits were also heightened by the fact that she forgot to pay the
telephone bills for two consecutive months. This behaviour was quite unlikely of her and made
her son worried. Furthermore, it is quite evident from Amy’s story that she is gradually facing
problems in remembering things or words that have already been communicated, such as the
visit of her son with his partner. The aforementioned symptoms and presenting complaints led to
the diagnosis of Alzheimer’s disease. This was usually diagnosed based on the medical history,
the information from the close relatives and behavioural observations. Persisting
neuropsychological and neurological features also supported the diagnosis of Alzheimer’s
disease that can ne defined as a condition involving a chronic neurodegenerative disease. This
condition usually worsens over time (1). This has also been established as the major reason of
dementia in around 60-70% individuals.
Research evidences have investigated the most common symptoms of the condition as
short term memory loss that makes it difficult for the affected individuals to remember recent
events. The gradual loss of bodily functions often makes it difficult for the individual to form an
active part of the society and community, and ultimately results in death (2). According to the
reports, there were approximately 46.8million people suffering from dementia on a global scale.
Furthermore, the report also suggested that 58% of individuals with dementia and Alzheimer’s
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4THERAPEUTICS 3
disease live in middle and low income countries (3). The fastest growth is observed among the
elderly population in India, China, and other south Asian and western Pacific regions.
The genetic heritability of the condition is based on different twin and family studies that
have been conducted on a large scale. Most research studies provide evidence for the fact that
0.1% of the diseases are familial kinds of autosomal dominant inheritance that shows an onset
near 60-65 years of age (4). Most of the autosomal dominant familial condition can be attributed
to presence of mutations in one of the three genes, namely amyloid precursor
protein (APP), presenilins 1 and presenilins 2 (5). Furthermore, the amyloid hypothesis
postulatws that extracellular deposits of amyloid beta (Aβ) acts as the contributing factor to the
development of the disease (6). In addition, abnormalities or misfolding of the tau proteins have
also been identified as major risk factors for the condition. These give rise to the formation of
neurofibrillary tangles inside the cyton of neurons, thereby resulting in disintegration of the
microtubules (7).
Laboratory tests conducted on the patient included FBC, ESR, thyroid function test,
vitamin B12 and folate, cholesterol tests, LFT, U&E, and calcium and magnesium tests. The
results were within the normal range for each of these tests. An advanced medical imaging of the
patient Amy with CT scan and MRI showed loss of synapses and neurons from the cerebral
cortex and subcortical regions of the brain. This eventually leads to atrophy of the regions
affected, including a gradual degeneration of the parietal and temporal lobe, and specific portions
of the cingulate and frontal cortex (8). Furthermore, her diagnosis was confirmed by the mini-
mental state examination (MMSE), which evaluated presence of cognitive impairment. This was
followed by an assessment of the intellectual functioning of the patient that included tests for
memory and helped in further characterizing the state of the prevailing disease (9). The patient
disease live in middle and low income countries (3). The fastest growth is observed among the
elderly population in India, China, and other south Asian and western Pacific regions.
The genetic heritability of the condition is based on different twin and family studies that
have been conducted on a large scale. Most research studies provide evidence for the fact that
0.1% of the diseases are familial kinds of autosomal dominant inheritance that shows an onset
near 60-65 years of age (4). Most of the autosomal dominant familial condition can be attributed
to presence of mutations in one of the three genes, namely amyloid precursor
protein (APP), presenilins 1 and presenilins 2 (5). Furthermore, the amyloid hypothesis
postulatws that extracellular deposits of amyloid beta (Aβ) acts as the contributing factor to the
development of the disease (6). In addition, abnormalities or misfolding of the tau proteins have
also been identified as major risk factors for the condition. These give rise to the formation of
neurofibrillary tangles inside the cyton of neurons, thereby resulting in disintegration of the
microtubules (7).
Laboratory tests conducted on the patient included FBC, ESR, thyroid function test,
vitamin B12 and folate, cholesterol tests, LFT, U&E, and calcium and magnesium tests. The
results were within the normal range for each of these tests. An advanced medical imaging of the
patient Amy with CT scan and MRI showed loss of synapses and neurons from the cerebral
cortex and subcortical regions of the brain. This eventually leads to atrophy of the regions
affected, including a gradual degeneration of the parietal and temporal lobe, and specific portions
of the cingulate and frontal cortex (8). Furthermore, her diagnosis was confirmed by the mini-
mental state examination (MMSE), which evaluated presence of cognitive impairment. This was
followed by an assessment of the intellectual functioning of the patient that included tests for
memory and helped in further characterizing the state of the prevailing disease (9). The patient
5THERAPEUTICS 3
Amy, exhibited loss of motivation, mood swings, problems in language comprehension and
disorientation. Hence, all the aforementioned test results confirmed Alzheimer’s disease.
Expected Medications
The medications were administered by the nurse unit manager Misha, to manage the
presenting complaints of the patient. There is no absolute cure for Alzheimer’s disease.
However, the commonly administered treatments are found to offer relatively small benefits,
although being palliative in nature. The patient Amy was under several medications that were
administered to treat the cognitive problems that she suffered from. The major medications that
were given to her include acetylcholinesterase inhibitors, NMDA receptor antagonists. One
characteristic feature of the condition is a reduction in the activity of cholinergic neurons.
Acetylcholinesterase inhibitors are generally administered with the aim of reducing or
eliminating high rates of breakdown of the neurotransmitter acetylcholine (ACh), thereby
increasing ACh concentration in the brain (10). This helps to combat the loss of the
neurotransmitter that occurs due death of cholinergic neurons. There are several evidences that
have investigated the effectiveness these medications in treating mild to moderate Alzheimer's
disease. Upon administration of this medication, some common side effects that might have been
encountered by Amy include vomiting and nausea, both of which are associated with cholinergic
excess. These adverse effects are mild in their severity and generally get adjusted with the
medication doses (11). Rivastigmine was administered via a transdermal patch and reduced the
severity of the presenting symptoms.
On the other hand, the NMDA receptor antagonist belongs to a class of anesthetics that
were prescribed for inhibiting the action of the NMDA receptors. This can be attributed to the
fact that hypofunction of these receptors are most common with aging of the brain, which in turn
Amy, exhibited loss of motivation, mood swings, problems in language comprehension and
disorientation. Hence, all the aforementioned test results confirmed Alzheimer’s disease.
Expected Medications
The medications were administered by the nurse unit manager Misha, to manage the
presenting complaints of the patient. There is no absolute cure for Alzheimer’s disease.
However, the commonly administered treatments are found to offer relatively small benefits,
although being palliative in nature. The patient Amy was under several medications that were
administered to treat the cognitive problems that she suffered from. The major medications that
were given to her include acetylcholinesterase inhibitors, NMDA receptor antagonists. One
characteristic feature of the condition is a reduction in the activity of cholinergic neurons.
Acetylcholinesterase inhibitors are generally administered with the aim of reducing or
eliminating high rates of breakdown of the neurotransmitter acetylcholine (ACh), thereby
increasing ACh concentration in the brain (10). This helps to combat the loss of the
neurotransmitter that occurs due death of cholinergic neurons. There are several evidences that
have investigated the effectiveness these medications in treating mild to moderate Alzheimer's
disease. Upon administration of this medication, some common side effects that might have been
encountered by Amy include vomiting and nausea, both of which are associated with cholinergic
excess. These adverse effects are mild in their severity and generally get adjusted with the
medication doses (11). Rivastigmine was administered via a transdermal patch and reduced the
severity of the presenting symptoms.
On the other hand, the NMDA receptor antagonist belongs to a class of anesthetics that
were prescribed for inhibiting the action of the NMDA receptors. This can be attributed to the
fact that hypofunction of these receptors are most common with aging of the brain, which in turn
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6THERAPEUTICS 3
contributes to the aging associated with memory deficits (12). Memantine was frequently
administered as the NMDA antagonist that acted on the glutamergic system and blocked the
receptors, thereby inhibiting glutamate overstimulation. However, some of the major side effects
that might have been encountered due to the prescribed medication include headache, fatigue,
dizziness, and confusion (13).
Summary of assumption
Medicines that were used during transition to palliative care and medications required
during the progress to end-of-life
With a progress of the neurodegenerative condition in the patient Amy, her behavioural
and neuropsychiatric changes became more prevalent. Some of the most common manifestations
were in the form of irritability, wandering, and labile affect. This often resulted in outbursts,
crying or unpremeditated aggression. Furthermore, a resistance was also displayed towards
caregiving. Approximately 30% of individuals, suffering from AD are known to develop
delusion and other illusionary misidentification related symptoms (14). In this case scenario, the
patient probably lost an insight of her disease process and suffered from anosognosia. These
advanced age symptoms often created stress for the carers and relatives, which was partly
reduced by moving the patient Amy from home care to and aged-care facilities. During her final
stages, the patient was found to be completely dependent upon her caregivers.
The language comprehension ability was reduced to single words and simple phrases that
eventually resulted in complete speech loss. Despite the loss of ability that pertained to verbal
language disabilities, the patient could often return emotional signals. Furthermore, Amy also
became unsteady on her feet and faced difficulties in performing simple tasks independently. The
contributes to the aging associated with memory deficits (12). Memantine was frequently
administered as the NMDA antagonist that acted on the glutamergic system and blocked the
receptors, thereby inhibiting glutamate overstimulation. However, some of the major side effects
that might have been encountered due to the prescribed medication include headache, fatigue,
dizziness, and confusion (13).
Summary of assumption
Medicines that were used during transition to palliative care and medications required
during the progress to end-of-life
With a progress of the neurodegenerative condition in the patient Amy, her behavioural
and neuropsychiatric changes became more prevalent. Some of the most common manifestations
were in the form of irritability, wandering, and labile affect. This often resulted in outbursts,
crying or unpremeditated aggression. Furthermore, a resistance was also displayed towards
caregiving. Approximately 30% of individuals, suffering from AD are known to develop
delusion and other illusionary misidentification related symptoms (14). In this case scenario, the
patient probably lost an insight of her disease process and suffered from anosognosia. These
advanced age symptoms often created stress for the carers and relatives, which was partly
reduced by moving the patient Amy from home care to and aged-care facilities. During her final
stages, the patient was found to be completely dependent upon her caregivers.
The language comprehension ability was reduced to single words and simple phrases that
eventually resulted in complete speech loss. Despite the loss of ability that pertained to verbal
language disabilities, the patient could often return emotional signals. Furthermore, Amy also
became unsteady on her feet and faced difficulties in performing simple tasks independently. The
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7THERAPEUTICS 3
overall objective of palliative care is to improve the quality of life of the patient. The palliative
approach was provided in a way that was not only beneficial at the end-of-life but often during
the months in advanced stage of the disease (15). Involvement of a palliative care team was
useful for Amy in a plethora of ways. Palliative care assisted in helping the patient cope with
some of the major Alzheimer’s disease symptoms, such as, anxiety, depression, and sleeping
difficulties. Owing to the fact that Amy has been shifted to a palliative care unit due to
deterioration of her symptoms, it is expected that the care team focused on administration of
antidepressant drugs (16). The antidepressant that was prescribed for Amy in palliative care
include selective serotonin reuptake inhibitors. Research evidences suggest that SSRI drugs
increase the extracellular serotonin levels, thereby limiting the absorption of the neurotransmitter
into the presynaptic bulb. This increases the levels of serotonin that is available in the synaptic
cleft to bind to the postsynaptic receptors.
Furthermore, SSRIs have also been established as the first line of treatment for severe
depression in most individuals. Individuals suffering from Alzheimer’s disease are at an
increased likelihood of suffering from depression (17). Hence, SSRIs were administered during
the palliative care. It is well known that the neurological changes that occur in the brain
in Alzheimer's disease and other dementia forms are incapable to causing pain (18). However,
people with Alzheimer’s are more susceptible to experiencing pain due to the fact that they
remain at increased risk of accidents, falls, and injuries, which might result in pain. The primary
task of palliative care professionals is to provide assistance to individuals who suffer distress due
to pain, at the end of their lives. An impairment in physical mobility results in pain. It is expected
that the health professionals administered morphine as the first line treatment for pain
management. It belongs to the opioid class of drugs and directly acts on the central nervous
overall objective of palliative care is to improve the quality of life of the patient. The palliative
approach was provided in a way that was not only beneficial at the end-of-life but often during
the months in advanced stage of the disease (15). Involvement of a palliative care team was
useful for Amy in a plethora of ways. Palliative care assisted in helping the patient cope with
some of the major Alzheimer’s disease symptoms, such as, anxiety, depression, and sleeping
difficulties. Owing to the fact that Amy has been shifted to a palliative care unit due to
deterioration of her symptoms, it is expected that the care team focused on administration of
antidepressant drugs (16). The antidepressant that was prescribed for Amy in palliative care
include selective serotonin reuptake inhibitors. Research evidences suggest that SSRI drugs
increase the extracellular serotonin levels, thereby limiting the absorption of the neurotransmitter
into the presynaptic bulb. This increases the levels of serotonin that is available in the synaptic
cleft to bind to the postsynaptic receptors.
Furthermore, SSRIs have also been established as the first line of treatment for severe
depression in most individuals. Individuals suffering from Alzheimer’s disease are at an
increased likelihood of suffering from depression (17). Hence, SSRIs were administered during
the palliative care. It is well known that the neurological changes that occur in the brain
in Alzheimer's disease and other dementia forms are incapable to causing pain (18). However,
people with Alzheimer’s are more susceptible to experiencing pain due to the fact that they
remain at increased risk of accidents, falls, and injuries, which might result in pain. The primary
task of palliative care professionals is to provide assistance to individuals who suffer distress due
to pain, at the end of their lives. An impairment in physical mobility results in pain. It is expected
that the health professionals administered morphine as the first line treatment for pain
management. It belongs to the opioid class of drugs and directly acts on the central nervous
8THERAPEUTICS 3
system to reduce feelings of pain (19). It primarily interacts with the μ-opioid receptors that are
located distinctly in the hypothalamus, thalamus, amygdala, putamen and nucleus caudatus (20).
Upon binding to the receptors, morphine has proved successful in initiating sedation and
analgesia. Keeping in consideration the health status of the patient, a low dose of morphine was
prescribed for Amy. Further evidences suggest that morphine creates little or no effect on the
survival rate of a patient in palliative care settings (21). However, care was taken to prevent
overdose of the drug, in order to eliminate risks of respiratory distress or asphyxia. During
transition of the patient to the end-stage of the condition, symptoms related to severe pain,
exhaustion and apathy are likely to get exacerbated. Furthermore, there will be complete loss of
the ability to speak, and the patient will become completely bedridden, and was unable to feed
herself. One of the major techniques that will be used in planning her end-of-life daily care is
related to maintenance of a routine.
Effective comfort care was provided to the patient in a way that made the caregivers
display essential skills to assess the facial expressions, reactions and movement. In addition to
providing good physical support, the spiritual and emotional distress of the patients was also
addressed. This was achieved by creating provisions for counseling, in addition to administration
of SSRIs. Furthermore, respite care was also provided, in combination with grief support for the
family members. They were also responsible for monitoring the patient to view any adverse
effects of the medicines on patient health. Supplementary oxygen delivery also proved beneficial
during the advanced stage, which in turn helped in treating respiratory distress (22).
GP letter
Dr. Borgart (Hyopothetical)
system to reduce feelings of pain (19). It primarily interacts with the μ-opioid receptors that are
located distinctly in the hypothalamus, thalamus, amygdala, putamen and nucleus caudatus (20).
Upon binding to the receptors, morphine has proved successful in initiating sedation and
analgesia. Keeping in consideration the health status of the patient, a low dose of morphine was
prescribed for Amy. Further evidences suggest that morphine creates little or no effect on the
survival rate of a patient in palliative care settings (21). However, care was taken to prevent
overdose of the drug, in order to eliminate risks of respiratory distress or asphyxia. During
transition of the patient to the end-stage of the condition, symptoms related to severe pain,
exhaustion and apathy are likely to get exacerbated. Furthermore, there will be complete loss of
the ability to speak, and the patient will become completely bedridden, and was unable to feed
herself. One of the major techniques that will be used in planning her end-of-life daily care is
related to maintenance of a routine.
Effective comfort care was provided to the patient in a way that made the caregivers
display essential skills to assess the facial expressions, reactions and movement. In addition to
providing good physical support, the spiritual and emotional distress of the patients was also
addressed. This was achieved by creating provisions for counseling, in addition to administration
of SSRIs. Furthermore, respite care was also provided, in combination with grief support for the
family members. They were also responsible for monitoring the patient to view any adverse
effects of the medicines on patient health. Supplementary oxygen delivery also proved beneficial
during the advanced stage, which in turn helped in treating respiratory distress (22).
GP letter
Dr. Borgart (Hyopothetical)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
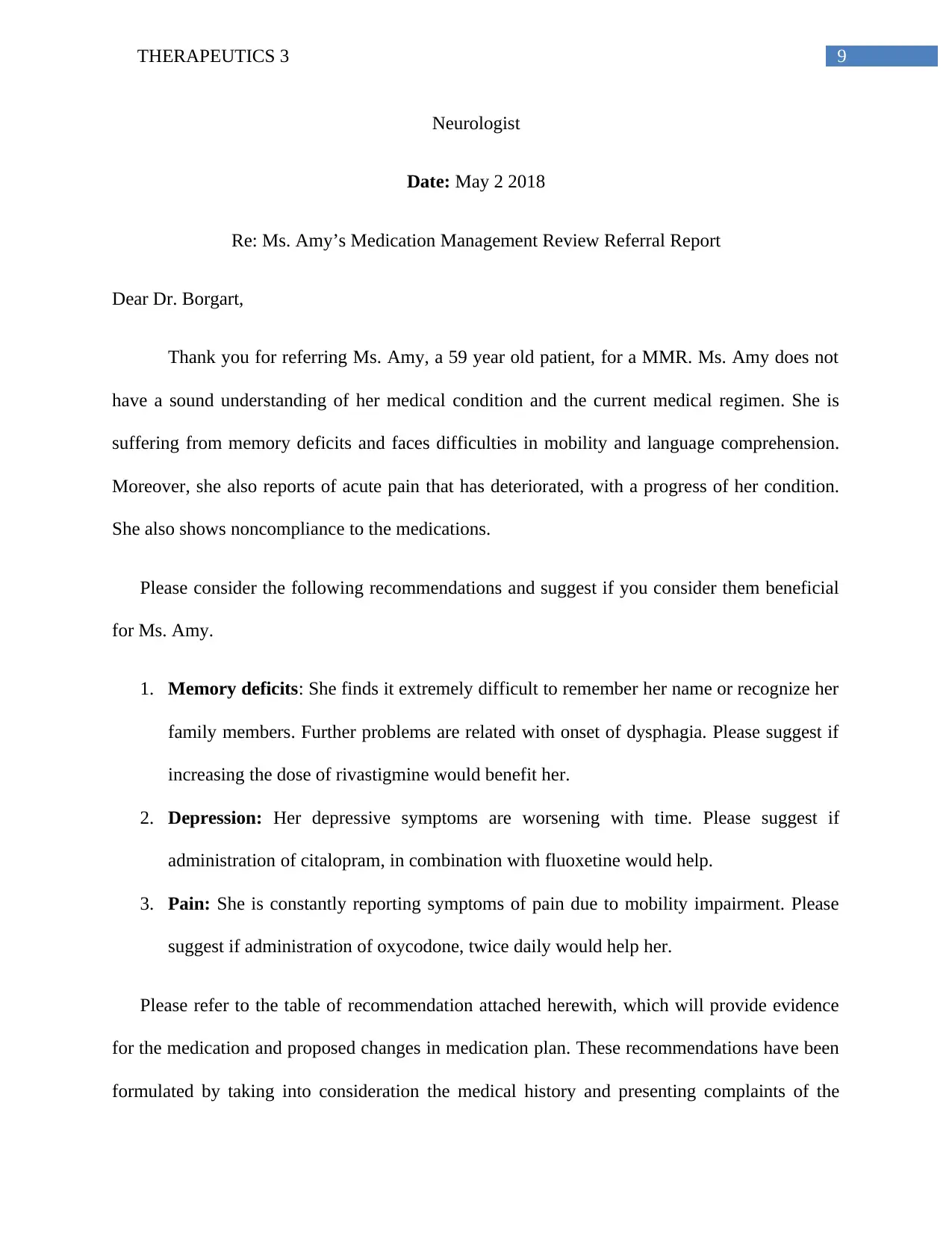
9THERAPEUTICS 3
Neurologist
Date: May 2 2018
Re: Ms. Amy’s Medication Management Review Referral Report
Dear Dr. Borgart,
Thank you for referring Ms. Amy, a 59 year old patient, for a MMR. Ms. Amy does not
have a sound understanding of her medical condition and the current medical regimen. She is
suffering from memory deficits and faces difficulties in mobility and language comprehension.
Moreover, she also reports of acute pain that has deteriorated, with a progress of her condition.
She also shows noncompliance to the medications.
Please consider the following recommendations and suggest if you consider them beneficial
for Ms. Amy.
1. Memory deficits: She finds it extremely difficult to remember her name or recognize her
family members. Further problems are related with onset of dysphagia. Please suggest if
increasing the dose of rivastigmine would benefit her.
2. Depression: Her depressive symptoms are worsening with time. Please suggest if
administration of citalopram, in combination with fluoxetine would help.
3. Pain: She is constantly reporting symptoms of pain due to mobility impairment. Please
suggest if administration of oxycodone, twice daily would help her.
Please refer to the table of recommendation attached herewith, which will provide evidence
for the medication and proposed changes in medication plan. These recommendations have been
formulated by taking into consideration the medical history and presenting complaints of the
Neurologist
Date: May 2 2018
Re: Ms. Amy’s Medication Management Review Referral Report
Dear Dr. Borgart,
Thank you for referring Ms. Amy, a 59 year old patient, for a MMR. Ms. Amy does not
have a sound understanding of her medical condition and the current medical regimen. She is
suffering from memory deficits and faces difficulties in mobility and language comprehension.
Moreover, she also reports of acute pain that has deteriorated, with a progress of her condition.
She also shows noncompliance to the medications.
Please consider the following recommendations and suggest if you consider them beneficial
for Ms. Amy.
1. Memory deficits: She finds it extremely difficult to remember her name or recognize her
family members. Further problems are related with onset of dysphagia. Please suggest if
increasing the dose of rivastigmine would benefit her.
2. Depression: Her depressive symptoms are worsening with time. Please suggest if
administration of citalopram, in combination with fluoxetine would help.
3. Pain: She is constantly reporting symptoms of pain due to mobility impairment. Please
suggest if administration of oxycodone, twice daily would help her.
Please refer to the table of recommendation attached herewith, which will provide evidence
for the medication and proposed changes in medication plan. These recommendations have been
formulated by taking into consideration the medical history and presenting complaints of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10THERAPEUTICS 3
patient, in addition to the diagnostic results. An improvement in the patient’s condition would
require further amendments to the recommendations.
I look forward to receiving your suggestions. Please do not hesitate to contact me for
discussing any additional information.
Yours faithfully,
(Name and date)
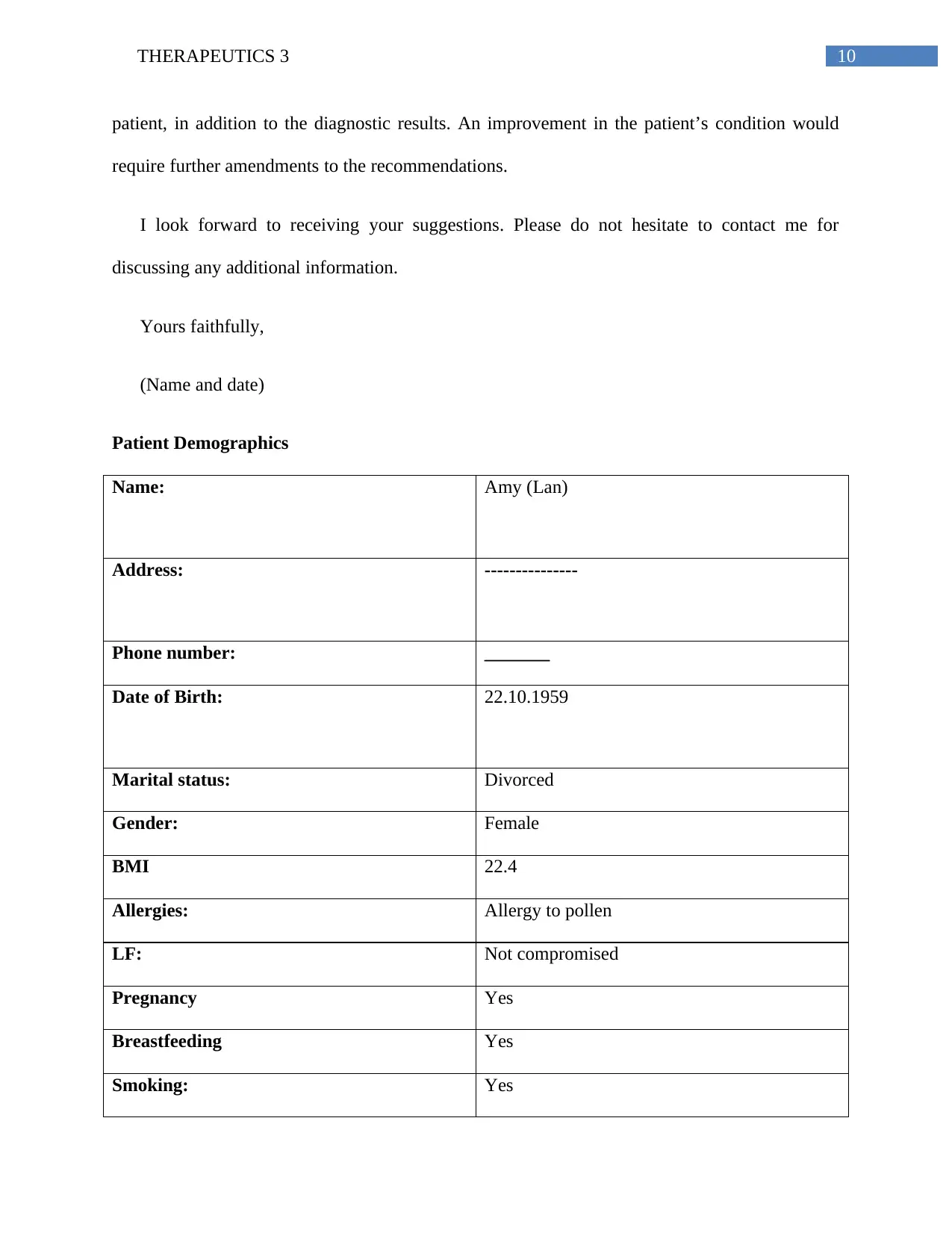
Patient Demographics
Name: Amy (Lan)
Address: ---------------
Phone number: _______
Date of Birth: 22.10.1959
Marital status: Divorced
Gender: Female
BMI 22.4
Allergies: Allergy to pollen
LF: Not compromised
Pregnancy Yes
Breastfeeding Yes
Smoking: Yes
patient, in addition to the diagnostic results. An improvement in the patient’s condition would
require further amendments to the recommendations.
I look forward to receiving your suggestions. Please do not hesitate to contact me for
discussing any additional information.
Yours faithfully,
(Name and date)
Patient Demographics
Name: Amy (Lan)
Address: ---------------
Phone number: _______
Date of Birth: 22.10.1959
Marital status: Divorced
Gender: Female
BMI 22.4
Allergies: Allergy to pollen
LF: Not compromised
Pregnancy Yes
Breastfeeding Yes
Smoking: Yes
11THERAPEUTICS 3
Alcohol: Occasionally
Carer details Nurse unit manager, family members, medical
interpreter
Treating Dr. details Neurologist
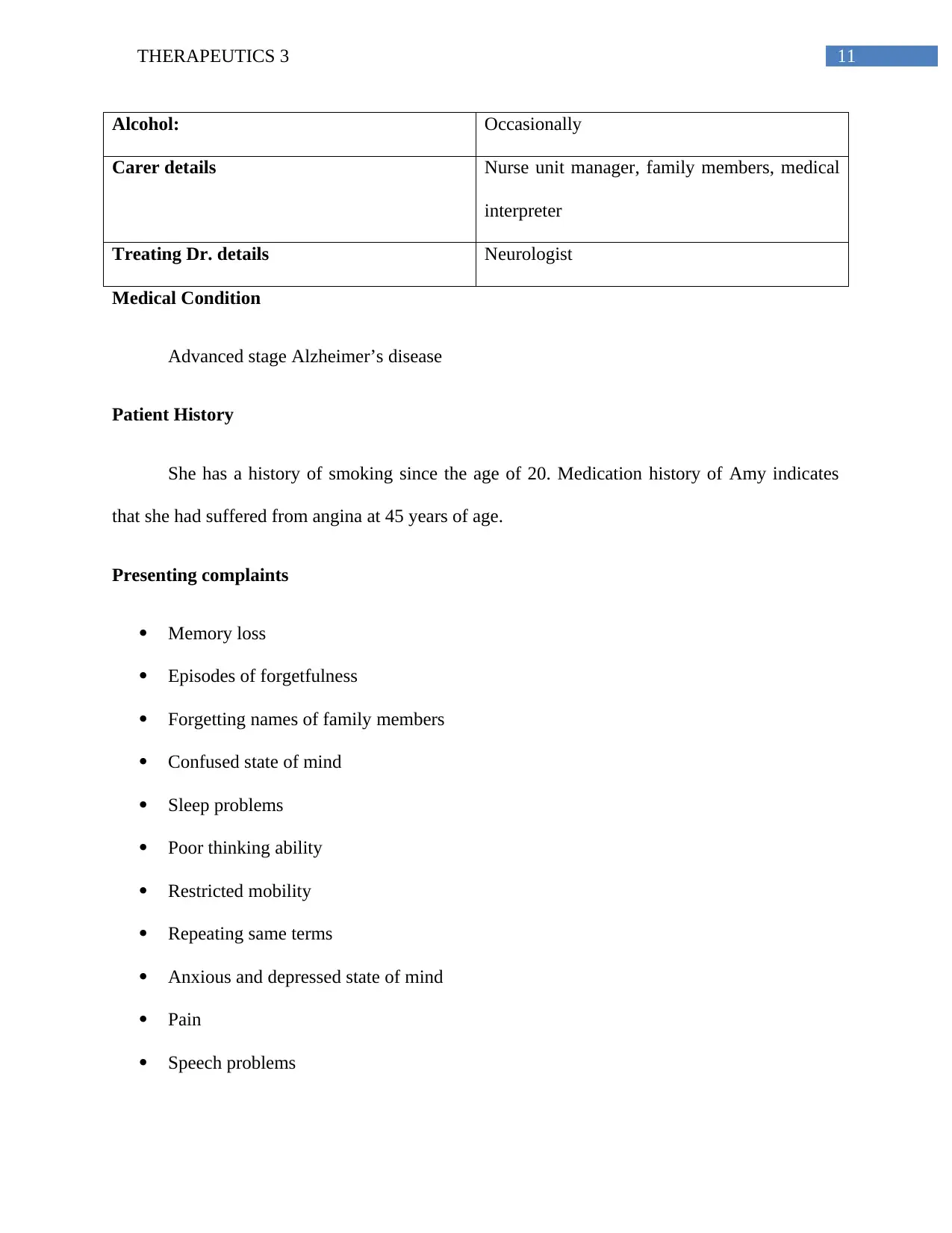
Medical Condition
Advanced stage Alzheimer’s disease
Patient History
She has a history of smoking since the age of 20. Medication history of Amy indicates
that she had suffered from angina at 45 years of age.
Presenting complaints
Memory loss
Episodes of forgetfulness
Forgetting names of family members
Confused state of mind
Sleep problems
Poor thinking ability
Restricted mobility
Repeating same terms
Anxious and depressed state of mind
Pain
Speech problems
Alcohol: Occasionally
Carer details Nurse unit manager, family members, medical
interpreter
Treating Dr. details Neurologist
Medical Condition
Advanced stage Alzheimer’s disease
Patient History
She has a history of smoking since the age of 20. Medication history of Amy indicates
that she had suffered from angina at 45 years of age.
Presenting complaints
Memory loss
Episodes of forgetfulness
Forgetting names of family members
Confused state of mind
Sleep problems
Poor thinking ability
Restricted mobility
Repeating same terms
Anxious and depressed state of mind
Pain
Speech problems
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





