Pediatric Anaphylaxis AEFI in Victoria, Australia: 2007-2013
VerifiedAdded on 2022/09/14
|6
|6284
|12
Report
AI Summary
This report presents a comprehensive analysis of pediatric anaphylaxis as an adverse event following immunization (AEFI) in Victoria, Australia, from 2007 to 2013. The study, based on data from the SAEFVIC surveillance system, applied the Brighton Collaboration case definition to classify and analyze anaphylactic events. The findings reveal an estimated incidence rate of anaphylaxis for DTaP vaccines of 0.36 cases per 100,000 doses and 1.25 per 100,000 doses for MMR vaccines. The majority of cases had rapid onset, but some developed symptoms beyond 30 minutes post-immunization. Intramuscular adrenaline was administered in most cases, with all patients making a full recovery. The study highlights the importance of diagnostic criteria in passive surveillance systems and emphasizes the need for healthcare professionals and parents to be aware of the potential for delayed onset of anaphylaxis following immunization.

Vaccine 33 (2015) 1602–1607
Contentslists available at ScienceDirect
Vaccine
j o u rn al h ome p a g e :w w w . e l s e v i e r . c o m / l o c a t e / v a c c i n e
Pediatric anaphylacticadverseevents following immunization in
Victoria, Australia from 2007 to 2013
Daryl R. Chenga,b,∗, Kirsten P. Perretta,c,d, Sharon Chood, Margie Danchina,c,e,
Jim P. Butteryf, Nigel W. Crawforda,e,f
a Departmentof GeneralMedicine,TheRoyal Children’sHospital,Melbourne,VIC, Australia
b JohnsHopkinsBloombergSchoolof Public Health,Baltimore,MD, USA
c Vaccineand ImmunisationResearchGroup(VIRGo),Murdoch ChildrensResearchInstituteand MelbourneSchoolof Populationand GlobalHealth,
TheUniversityof Melbourne,Melbourne,VIC, Australia
d Departmentof Allergyand Immunology,Royal Children’sHospital,Melbourne,VIC, Australia
e Departmentof Pediatrics,The Universityof Melbourne,Melbourne,VIC, Australia
f SAEFVIC,Murdoch Children’sResearchInstitute,Melbourne,VIC, Australia
a r t i c l e i n f o
Articlehistory:
Received10 November 2014
Receivedin revised form 3 February 2015
Accepted4 February 2015
Available online 16 February 2015
Keywords:
Anaphylaxis
Immunization
AEFI
Vaccine safety
a b s t r a c t
Background:Anaphylaxis is a rare life-threatening adverse event following immunization (AEFI). Vari-
ability in presentationcan make differentiation between anaphylaxisand other AEFI difficult. This study
summarizespediatricanaphylaxisAEFI reportedto an Australianstate-basedpassivesurveillancesystem.
Methods:All suspectedand reported pediatric (<18years)anaphylaxisAEFI notified to SAEFVIC (Surveil-
lance of Adverse Events Following Vaccination In the Community) Melbourne, Australia, between May
2007 to May 2013 were analyzed.Clinical descriptions of the AEFI, using the internationally recognized
Brighton Collaborationcasedefinition (BCCD)and final outcome were documented.
Results:93%(25/27) of AEFI classifiedas anaphylaxismet BCCD criteria, with 36%(9/25), assessedas the
highest level of diagnostic certainty (Level 1). Median age was 4.7 years (range 0.3–16.2); 48%of cases
were male. The vaccine antigens administered included: diphtheria, tetanus,acellular pertussis (DTaP)
alone or in combination vaccinescontaining other antigensin 11 of 25 cases(44%);and live attenuated
measlesmumps rubella (MMR) vaccinefor six (five also had other vaccinesconcomitantlyadministered).
The estimatedincidencerate of anaphylaxisfor DTaP vaccineswas 0.36 casesper 100,000doses,and 1.25
per 100,000 doses for MMR vaccines.The majority of caseshad rapid onset, but in 24%(6/25) of cases,
first symptomsof anaphylaxisdeveloped≥30min after immunization. In 60%(15/25) of cases,symptoms
resolved ≤60min of presentation.Intramuscular adrenaline was administered in 90%(18/25) of cases.
All casesmade a full recoverywith no sequelaeidentified.
Conclusion:This comprehensivecase series of pediatric anaphylaxisas an AEFI identified that diagnos-
tic criteria are useful when applied to a passive vaccine surveillance system when adequate clinical
information is available.Anaphylaxis as an AEFI is rare and usually begins within 30 min of vaccination.
However, healthcareprofessionalsand vaccinees/parentsshould be aware that onset of anaphylaxiscan
be delayedbeyond30 min following immunization and that medical attentionshould be soughtpromptly
if anaphylaxisis suspected.
© 2015 Elsevier Ltd. All rights reserved.
1. Introduction
Australia has a standardized childhood National Immunisa-
tion Program (NIP) schedule approved and reviewed on a regular
∗ Correspondingauthor at: The Royal Children’sHospital Melbourne, 50 Fleming-
ton Rd, Parkville, VIC 3052, Australia. Tel.: +619345 5522.
E-mail address:daryl.cheng@rch.org.au(D.R.Cheng).
basis by the Australian Technical Advisory Group on Immunisa-
tion (ATAGI) and authorized by the National Health and Medical
ResearchCouncil (NHMRC) [1]. It includes infant and early child-
hood immunization, as well as a secondaryschool (age12–16 years)
program for catch-up vaccines (Hepatitis B, Varicella) and new
vaccines(e.g.Human papillomavirus (HPV) vaccine introduced for
females in 2007; males in 2012) [2]. There are also specific special
risk groups with additional vaccine requirements (e.g. Aboriginal
and Torres St Islanders).
http://dx.doi.org/10.1016/j.vaccine.2015.02.008
0264-410X/©2015 Elsevier Ltd. All rights reserved.
Contentslists available at ScienceDirect
Vaccine
j o u rn al h ome p a g e :w w w . e l s e v i e r . c o m / l o c a t e / v a c c i n e
Pediatric anaphylacticadverseevents following immunization in
Victoria, Australia from 2007 to 2013
Daryl R. Chenga,b,∗, Kirsten P. Perretta,c,d, Sharon Chood, Margie Danchina,c,e,
Jim P. Butteryf, Nigel W. Crawforda,e,f
a Departmentof GeneralMedicine,TheRoyal Children’sHospital,Melbourne,VIC, Australia
b JohnsHopkinsBloombergSchoolof Public Health,Baltimore,MD, USA
c Vaccineand ImmunisationResearchGroup(VIRGo),Murdoch ChildrensResearchInstituteand MelbourneSchoolof Populationand GlobalHealth,
TheUniversityof Melbourne,Melbourne,VIC, Australia
d Departmentof Allergyand Immunology,Royal Children’sHospital,Melbourne,VIC, Australia
e Departmentof Pediatrics,The Universityof Melbourne,Melbourne,VIC, Australia
f SAEFVIC,Murdoch Children’sResearchInstitute,Melbourne,VIC, Australia
a r t i c l e i n f o
Articlehistory:
Received10 November 2014
Receivedin revised form 3 February 2015
Accepted4 February 2015
Available online 16 February 2015
Keywords:
Anaphylaxis
Immunization
AEFI
Vaccine safety
a b s t r a c t
Background:Anaphylaxis is a rare life-threatening adverse event following immunization (AEFI). Vari-
ability in presentationcan make differentiation between anaphylaxisand other AEFI difficult. This study
summarizespediatricanaphylaxisAEFI reportedto an Australianstate-basedpassivesurveillancesystem.
Methods:All suspectedand reported pediatric (<18years)anaphylaxisAEFI notified to SAEFVIC (Surveil-
lance of Adverse Events Following Vaccination In the Community) Melbourne, Australia, between May
2007 to May 2013 were analyzed.Clinical descriptions of the AEFI, using the internationally recognized
Brighton Collaborationcasedefinition (BCCD)and final outcome were documented.
Results:93%(25/27) of AEFI classifiedas anaphylaxismet BCCD criteria, with 36%(9/25), assessedas the
highest level of diagnostic certainty (Level 1). Median age was 4.7 years (range 0.3–16.2); 48%of cases
were male. The vaccine antigens administered included: diphtheria, tetanus,acellular pertussis (DTaP)
alone or in combination vaccinescontaining other antigensin 11 of 25 cases(44%);and live attenuated
measlesmumps rubella (MMR) vaccinefor six (five also had other vaccinesconcomitantlyadministered).
The estimatedincidencerate of anaphylaxisfor DTaP vaccineswas 0.36 casesper 100,000doses,and 1.25
per 100,000 doses for MMR vaccines.The majority of caseshad rapid onset, but in 24%(6/25) of cases,
first symptomsof anaphylaxisdeveloped≥30min after immunization. In 60%(15/25) of cases,symptoms
resolved ≤60min of presentation.Intramuscular adrenaline was administered in 90%(18/25) of cases.
All casesmade a full recoverywith no sequelaeidentified.
Conclusion:This comprehensivecase series of pediatric anaphylaxisas an AEFI identified that diagnos-
tic criteria are useful when applied to a passive vaccine surveillance system when adequate clinical
information is available.Anaphylaxis as an AEFI is rare and usually begins within 30 min of vaccination.
However, healthcareprofessionalsand vaccinees/parentsshould be aware that onset of anaphylaxiscan
be delayedbeyond30 min following immunization and that medical attentionshould be soughtpromptly
if anaphylaxisis suspected.
© 2015 Elsevier Ltd. All rights reserved.
1. Introduction
Australia has a standardized childhood National Immunisa-
tion Program (NIP) schedule approved and reviewed on a regular
∗ Correspondingauthor at: The Royal Children’sHospital Melbourne, 50 Fleming-
ton Rd, Parkville, VIC 3052, Australia. Tel.: +619345 5522.
E-mail address:daryl.cheng@rch.org.au(D.R.Cheng).
basis by the Australian Technical Advisory Group on Immunisa-
tion (ATAGI) and authorized by the National Health and Medical
ResearchCouncil (NHMRC) [1]. It includes infant and early child-
hood immunization, as well as a secondaryschool (age12–16 years)
program for catch-up vaccines (Hepatitis B, Varicella) and new
vaccines(e.g.Human papillomavirus (HPV) vaccine introduced for
females in 2007; males in 2012) [2]. There are also specific special
risk groups with additional vaccine requirements (e.g. Aboriginal
and Torres St Islanders).
http://dx.doi.org/10.1016/j.vaccine.2015.02.008
0264-410X/©2015 Elsevier Ltd. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
D.R.Chenget al. / Vaccine33 (2015)1602–1607 1603
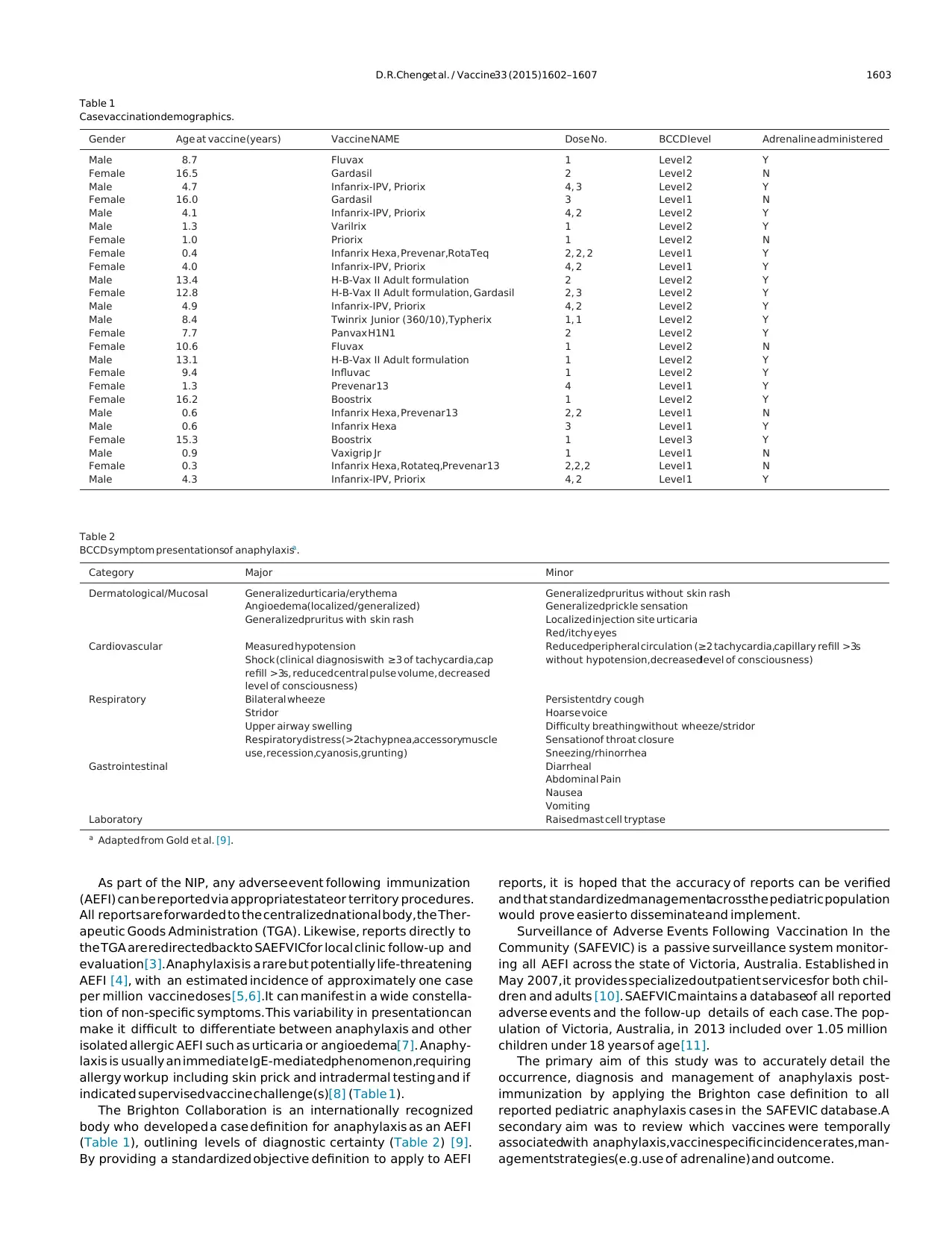
Table 1
Casevaccination demographics.
Gender Age at vaccine(years) Vaccine NAME Dose No. BCCD level Adrenaline administered
Male 8.7 Fluvax 1 Level 2 Y
Female 16.5 Gardasil 2 Level 2 N
Male 4.7 Infanrix-IPV, Priorix 4, 3 Level 2 Y
Female 16.0 Gardasil 3 Level 1 N
Male 4.1 Infanrix-IPV, Priorix 4, 2 Level 2 Y
Male 1.3 Varilrix 1 Level 2 Y
Female 1.0 Priorix 1 Level 2 N
Female 0.4 Infanrix Hexa, Prevenar,RotaTeq 2, 2, 2 Level 1 Y
Female 4.0 Infanrix-IPV, Priorix 4, 2 Level 1 Y
Male 13.4 H-B-Vax II Adult formulation 2 Level 2 Y
Female 12.8 H-B-Vax II Adult formulation, Gardasil 2, 3 Level 2 Y
Male 4.9 Infanrix-IPV, Priorix 4, 2 Level 2 Y
Male 8.4 Twinrix Junior (360/10),Typherix 1, 1 Level 2 Y
Female 7.7 Panvax H1N1 2 Level 2 Y
Female 10.6 Fluvax 1 Level 2 N
Male 13.1 H-B-Vax II Adult formulation 1 Level 2 Y
Female 9.4 Influvac 1 Level 2 Y
Female 1.3 Prevenar 13 4 Level 1 Y
Female 16.2 Boostrix 1 Level 2 Y
Male 0.6 Infanrix Hexa, Prevenar13 2, 2 Level 1 N
Male 0.6 Infanrix Hexa 3 Level 1 Y
Female 15.3 Boostrix 1 Level 3 Y
Male 0.9 Vaxigrip Jr 1 Level 1 N
Female 0.3 Infanrix Hexa, Rotateq,Prevenar13 2,2,2 Level 1 N
Male 4.3 Infanrix-IPV, Priorix 4, 2 Level 1 Y
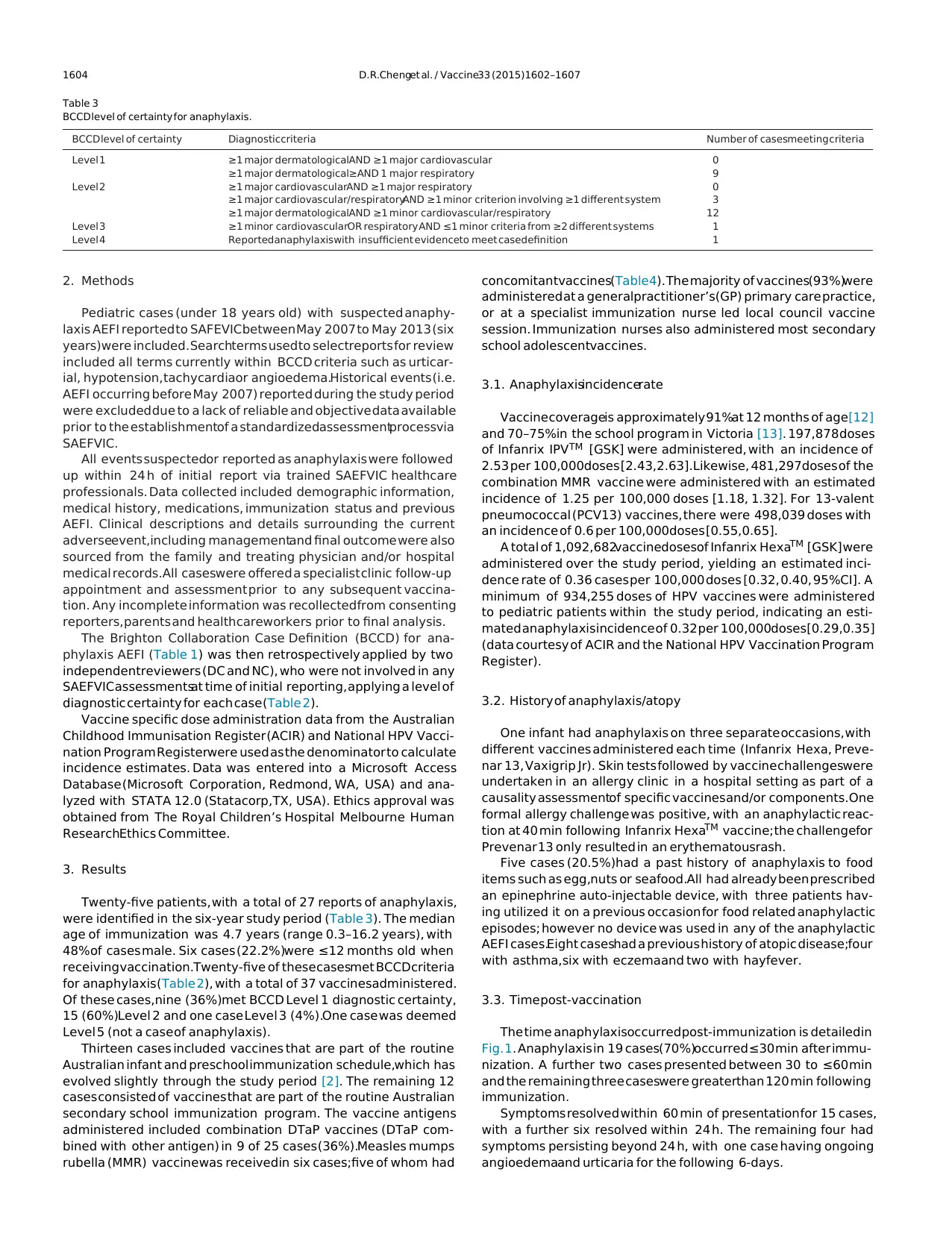
Table 2
BCCD symptom presentationsof anaphylaxisa.
Category Major Minor
Dermatological/Mucosal Generalizedurticaria/erythema
Angioedema(localized/generalized)
Generalizedpruritus with skin rash
Generalizedpruritus without skin rash
Generalizedprickle sensation
Localized injection site urticaria
Red/itchy eyes
Cardiovascular Measured hypotension
Shock (clinical diagnosiswith ≥3 of tachycardia,cap
refill >3s, reducedcentral pulse volume, decreased
level of consciousness)
Reducedperipheral circulation (≥2 tachycardia,capillary refill >3s
without hypotension,decreasedlevel of consciousness)
Respiratory Bilateral wheeze
Stridor
Upper airway swelling
Respiratorydistress(>2tachypnea,accessorymuscle
use, recession,cyanosis,grunting)
Persistentdry cough
Hoarse voice
Difficulty breathingwithout wheeze/stridor
Sensationof throat closure
Sneezing/rhinorrhea
Gastrointestinal Diarrheal
Abdominal Pain
Nausea
Vomiting
Laboratory Raisedmast cell tryptase
a Adapted from Gold et al. [9].
As part of the NIP, any adverse event following immunization
(AEFI) can be reported via appropriatestateor territory procedures.
All reports are forwarded to the centralizednational body, the Ther-
apeutic Goods Administration (TGA). Likewise, reports directly to
the TGA are redirectedbackto SAEFVICfor local clinic follow-up and
evaluation[3]. Anaphylaxis is a rare but potentially life-threatening
AEFI [4], with an estimated incidence of approximately one case
per million vaccine doses [5,6].It can manifest in a wide constella-
tion of non-specific symptoms. This variability in presentation can
make it difficult to differentiate between anaphylaxis and other
isolated allergic AEFI such as urticaria or angioedema[7]. Anaphy-
laxis is usually an immediate IgE-mediatedphenomenon,requiring
allergy workup including skin prick and intradermal testing and if
indicated supervised vaccine challenge(s)[8] (Table 1).
The Brighton Collaboration is an internationally recognized
body who developed a case definition for anaphylaxis as an AEFI
(Table 1), outlining levels of diagnostic certainty (Table 2) [9].
By providing a standardized objective definition to apply to AEFI
reports, it is hoped that the accuracy of reports can be verified
and that standardizedmanagementacrossthe pediatric population
would prove easier to disseminate and implement.
Surveillance of Adverse Events Following Vaccination In the
Community (SAFEVIC) is a passive surveillance system monitor-
ing all AEFI across the state of Victoria, Australia. Established in
May 2007, it provides specialized outpatient servicesfor both chil-
dren and adults [10]. SAEFVIC maintains a databaseof all reported
adverse events and the follow-up details of each case. The pop-
ulation of Victoria, Australia, in 2013 included over 1.05 million
children under 18 years of age [11].
The primary aim of this study was to accurately detail the
occurrence, diagnosis and management of anaphylaxis post-
immunization by applying the Brighton case definition to all
reported pediatric anaphylaxis cases in the SAFEVIC database.A
secondary aim was to review which vaccines were temporally
associatedwith anaphylaxis,vaccinespecific incidence rates,man-
agementstrategies(e.g.use of adrenaline) and outcome.
Table 1
Casevaccination demographics.
Gender Age at vaccine(years) Vaccine NAME Dose No. BCCD level Adrenaline administered
Male 8.7 Fluvax 1 Level 2 Y
Female 16.5 Gardasil 2 Level 2 N
Male 4.7 Infanrix-IPV, Priorix 4, 3 Level 2 Y
Female 16.0 Gardasil 3 Level 1 N
Male 4.1 Infanrix-IPV, Priorix 4, 2 Level 2 Y
Male 1.3 Varilrix 1 Level 2 Y
Female 1.0 Priorix 1 Level 2 N
Female 0.4 Infanrix Hexa, Prevenar,RotaTeq 2, 2, 2 Level 1 Y
Female 4.0 Infanrix-IPV, Priorix 4, 2 Level 1 Y
Male 13.4 H-B-Vax II Adult formulation 2 Level 2 Y
Female 12.8 H-B-Vax II Adult formulation, Gardasil 2, 3 Level 2 Y
Male 4.9 Infanrix-IPV, Priorix 4, 2 Level 2 Y
Male 8.4 Twinrix Junior (360/10),Typherix 1, 1 Level 2 Y
Female 7.7 Panvax H1N1 2 Level 2 Y
Female 10.6 Fluvax 1 Level 2 N
Male 13.1 H-B-Vax II Adult formulation 1 Level 2 Y
Female 9.4 Influvac 1 Level 2 Y
Female 1.3 Prevenar 13 4 Level 1 Y
Female 16.2 Boostrix 1 Level 2 Y
Male 0.6 Infanrix Hexa, Prevenar13 2, 2 Level 1 N
Male 0.6 Infanrix Hexa 3 Level 1 Y
Female 15.3 Boostrix 1 Level 3 Y
Male 0.9 Vaxigrip Jr 1 Level 1 N
Female 0.3 Infanrix Hexa, Rotateq,Prevenar13 2,2,2 Level 1 N
Male 4.3 Infanrix-IPV, Priorix 4, 2 Level 1 Y
Table 2
BCCD symptom presentationsof anaphylaxisa.
Category Major Minor
Dermatological/Mucosal Generalizedurticaria/erythema
Angioedema(localized/generalized)
Generalizedpruritus with skin rash
Generalizedpruritus without skin rash
Generalizedprickle sensation
Localized injection site urticaria
Red/itchy eyes
Cardiovascular Measured hypotension
Shock (clinical diagnosiswith ≥3 of tachycardia,cap
refill >3s, reducedcentral pulse volume, decreased
level of consciousness)
Reducedperipheral circulation (≥2 tachycardia,capillary refill >3s
without hypotension,decreasedlevel of consciousness)
Respiratory Bilateral wheeze
Stridor
Upper airway swelling
Respiratorydistress(>2tachypnea,accessorymuscle
use, recession,cyanosis,grunting)
Persistentdry cough
Hoarse voice
Difficulty breathingwithout wheeze/stridor
Sensationof throat closure
Sneezing/rhinorrhea
Gastrointestinal Diarrheal
Abdominal Pain
Nausea
Vomiting
Laboratory Raisedmast cell tryptase
a Adapted from Gold et al. [9].
As part of the NIP, any adverse event following immunization
(AEFI) can be reported via appropriatestateor territory procedures.
All reports are forwarded to the centralizednational body, the Ther-
apeutic Goods Administration (TGA). Likewise, reports directly to
the TGA are redirectedbackto SAEFVICfor local clinic follow-up and
evaluation[3]. Anaphylaxis is a rare but potentially life-threatening
AEFI [4], with an estimated incidence of approximately one case
per million vaccine doses [5,6].It can manifest in a wide constella-
tion of non-specific symptoms. This variability in presentation can
make it difficult to differentiate between anaphylaxis and other
isolated allergic AEFI such as urticaria or angioedema[7]. Anaphy-
laxis is usually an immediate IgE-mediatedphenomenon,requiring
allergy workup including skin prick and intradermal testing and if
indicated supervised vaccine challenge(s)[8] (Table 1).
The Brighton Collaboration is an internationally recognized
body who developed a case definition for anaphylaxis as an AEFI
(Table 1), outlining levels of diagnostic certainty (Table 2) [9].
By providing a standardized objective definition to apply to AEFI
reports, it is hoped that the accuracy of reports can be verified
and that standardizedmanagementacrossthe pediatric population
would prove easier to disseminate and implement.
Surveillance of Adverse Events Following Vaccination In the
Community (SAFEVIC) is a passive surveillance system monitor-
ing all AEFI across the state of Victoria, Australia. Established in
May 2007, it provides specialized outpatient servicesfor both chil-
dren and adults [10]. SAEFVIC maintains a databaseof all reported
adverse events and the follow-up details of each case. The pop-
ulation of Victoria, Australia, in 2013 included over 1.05 million
children under 18 years of age [11].
The primary aim of this study was to accurately detail the
occurrence, diagnosis and management of anaphylaxis post-
immunization by applying the Brighton case definition to all
reported pediatric anaphylaxis cases in the SAFEVIC database.A
secondary aim was to review which vaccines were temporally
associatedwith anaphylaxis,vaccinespecific incidence rates,man-
agementstrategies(e.g.use of adrenaline) and outcome.
1604 D.R.Chenget al. / Vaccine33 (2015)1602–1607
Table 3
BCCD level of certainty for anaphylaxis.
BCCD level of certainty Diagnosticcriteria Number of casesmeeting criteria
Level 1 ≥1 major dermatologicalAND ≥1 major cardiovascular 0
≥1 major dermatological≥AND 1 major respiratory 9
Level 2 ≥1 major cardiovascularAND ≥1 major respiratory 0
≥1 major cardiovascular/respiratoryAND ≥1 minor criterion involving ≥1 different system 3
≥1 major dermatologicalAND ≥1 minor cardiovascular/respiratory 12
Level 3 ≥1 minor cardiovascularOR respiratory AND ≤1 minor criteria from ≥2 different systems 1
Level 4 Reportedanaphylaxiswith insufficient evidenceto meet casedefinition 1
2. Methods
Pediatric cases (under 18 years old) with suspected anaphy-
laxis AEFI reported to SAFEVICbetween May 2007 to May 2013 (six
years)were included. Searchterms used to selectreports for review
included all terms currently within BCCD criteria such as urticar-
ial, hypotension, tachycardiaor angioedema.Historical events (i.e.
AEFI occurring before May 2007) reported during the study period
were excluded due to a lack of reliable and objective data available
prior to the establishmentof a standardizedassessmentprocessvia
SAEFVIC.
All events suspectedor reported as anaphylaxis were followed
up within 24 h of initial report via trained SAEFVIC healthcare
professionals. Data collected included demographic information,
medical history, medications, immunization status and previous
AEFI. Clinical descriptions and details surrounding the current
adverseevent,including managementand final outcome were also
sourced from the family and treating physician and/or hospital
medical records.All caseswere offered a specialist clinic follow-up
appointment and assessment prior to any subsequent vaccina-
tion. Any incomplete information was recollectedfrom consenting
reporters, parents and healthcareworkers prior to final analysis.
The Brighton Collaboration Case Definition (BCCD) for ana-
phylaxis AEFI (Table 1) was then retrospectively applied by two
independentreviewers (DC and NC), who were not involved in any
SAEFVIC assessmentsat time of initial reporting, applying a level of
diagnostic certainty for each case (Table 2).
Vaccine specific dose administration data from the Australian
Childhood Immunisation Register (ACIR) and National HPV Vacci-
nation Program Registerwere used as the denominator to calculate
incidence estimates. Data was entered into a Microsoft Access
Database (Microsoft Corporation, Redmond, WA, USA) and ana-
lyzed with STATA 12.0 (Statacorp,TX, USA). Ethics approval was
obtained from The Royal Children’s Hospital Melbourne Human
ResearchEthics Committee.
3. Results
Twenty-five patients, with a total of 27 reports of anaphylaxis,
were identified in the six-year study period (Table 3). The median
age of immunization was 4.7 years (range 0.3–16.2 years), with
48%of cases male. Six cases (22.2%)were ≤12 months old when
receiving vaccination.Twenty-five of these casesmet BCCDcriteria
for anaphylaxis (Table 2), with a total of 37 vaccinesadministered.
Of these cases,nine (36%)met BCCD Level 1 diagnostic certainty,
15 (60%)Level 2 and one case Level 3 (4%).One case was deemed
Level 5 (not a case of anaphylaxis).
Thirteen cases included vaccines that are part of the routine
Australian infant and preschool immunization schedule,which has
evolved slightly through the study period [2]. The remaining 12
cases consisted of vaccines that are part of the routine Australian
secondary school immunization program. The vaccine antigens
administered included combination DTaP vaccines (DTaP com-
bined with other antigen) in 9 of 25 cases (36%).Measles mumps
rubella (MMR) vaccinewas receivedin six cases;five of whom had
concomitantvaccines(Table4). The majority of vaccines(93%)were
administered at a generalpractitioner’s(GP) primary care practice,
or at a specialist immunization nurse led local council vaccine
session. Immunization nurses also administered most secondary
school adolescentvaccines.
3.1. Anaphylaxisincidencerate
Vaccine coverageis approximately 91%at 12 months of age[12]
and 70–75%in the school program in Victoria [13]. 197,878 doses
of Infanrix IPVTM [GSK] were administered, with an incidence of
2.53 per 100,000doses [2.43,2.63].Likewise, 481,297doses of the
combination MMR vaccine were administered with an estimated
incidence of 1.25 per 100,000 doses [1.18, 1.32]. For 13-valent
pneumococcal (PCV13) vaccines, there were 498,039 doses with
an incidence of 0.6 per 100,000doses [0.55,0.65].
A total of 1,092,682vaccinedosesof Infanrix HexaTM [GSK] were
administered over the study period, yielding an estimated inci-
dence rate of 0.36 cases per 100,000 doses [0.32, 0.40, 95%CI]. A
minimum of 934,255 doses of HPV vaccines were administered
to pediatric patients within the study period, indicating an esti-
mated anaphylaxisincidence of 0.32 per 100,000doses[0.29,0.35]
(data courtesy of ACIR and the National HPV Vaccination Program
Register).
3.2. History of anaphylaxis/atopy
One infant had anaphylaxis on three separate occasions, with
different vaccines administered each time (Infanrix Hexa, Preve-
nar 13, Vaxigrip Jr). Skin tests followed by vaccine challengeswere
undertaken in an allergy clinic in a hospital setting as part of a
causality assessmentof specific vaccinesand/or components.One
formal allergy challenge was positive, with an anaphylactic reac-
tion at 40 min following Infanrix HexaTM vaccine; the challengefor
Prevenar 13 only resulted in an erythematousrash.
Five cases (20.5%)had a past history of anaphylaxis to food
items such as egg,nuts or seafood.All had already been prescribed
an epinephrine auto-injectable device, with three patients hav-
ing utilized it on a previous occasion for food related anaphylactic
episodes; however no device was used in any of the anaphylactic
AEFI cases.Eight caseshad a previous history of atopic disease;four
with asthma,six with eczemaand two with hayfever.
3.3. Time post-vaccination
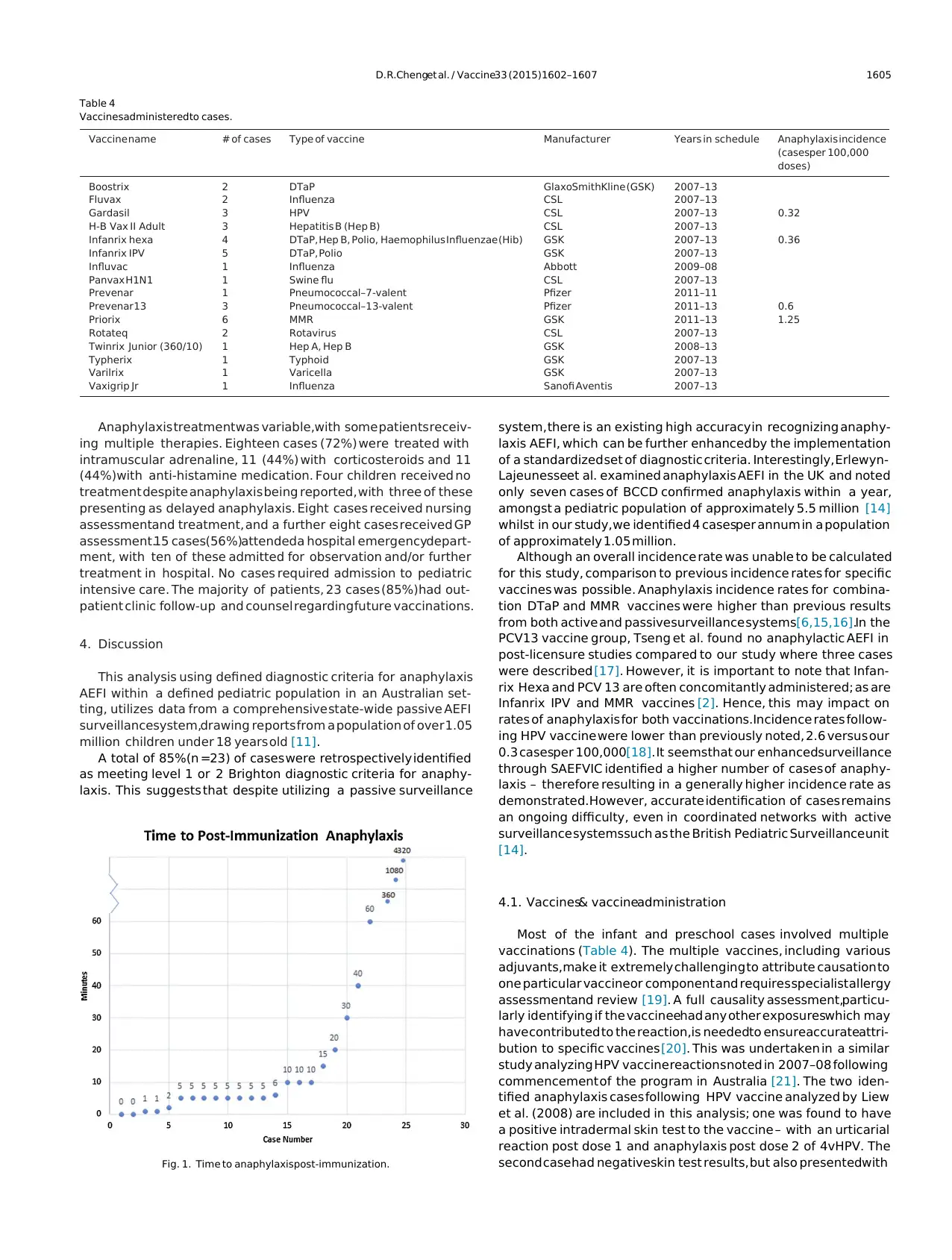
The time anaphylaxisoccurred post-immunization is detailedin
Fig. 1. Anaphylaxis in 19 cases(70%)occurred ≤30 min after immu-
nization. A further two cases presented between 30 to ≤60 min
and the remaining three caseswere greaterthan 120 min following
immunization.
Symptoms resolved within 60 min of presentation for 15 cases,
with a further six resolved within 24 h. The remaining four had
symptoms persisting beyond 24 h, with one case having ongoing
angioedemaand urticaria for the following 6-days.
Table 3
BCCD level of certainty for anaphylaxis.
BCCD level of certainty Diagnosticcriteria Number of casesmeeting criteria
Level 1 ≥1 major dermatologicalAND ≥1 major cardiovascular 0
≥1 major dermatological≥AND 1 major respiratory 9
Level 2 ≥1 major cardiovascularAND ≥1 major respiratory 0
≥1 major cardiovascular/respiratoryAND ≥1 minor criterion involving ≥1 different system 3
≥1 major dermatologicalAND ≥1 minor cardiovascular/respiratory 12
Level 3 ≥1 minor cardiovascularOR respiratory AND ≤1 minor criteria from ≥2 different systems 1
Level 4 Reportedanaphylaxiswith insufficient evidenceto meet casedefinition 1
2. Methods
Pediatric cases (under 18 years old) with suspected anaphy-
laxis AEFI reported to SAFEVICbetween May 2007 to May 2013 (six
years)were included. Searchterms used to selectreports for review
included all terms currently within BCCD criteria such as urticar-
ial, hypotension, tachycardiaor angioedema.Historical events (i.e.
AEFI occurring before May 2007) reported during the study period
were excluded due to a lack of reliable and objective data available
prior to the establishmentof a standardizedassessmentprocessvia
SAEFVIC.
All events suspectedor reported as anaphylaxis were followed
up within 24 h of initial report via trained SAEFVIC healthcare
professionals. Data collected included demographic information,
medical history, medications, immunization status and previous
AEFI. Clinical descriptions and details surrounding the current
adverseevent,including managementand final outcome were also
sourced from the family and treating physician and/or hospital
medical records.All caseswere offered a specialist clinic follow-up
appointment and assessment prior to any subsequent vaccina-
tion. Any incomplete information was recollectedfrom consenting
reporters, parents and healthcareworkers prior to final analysis.
The Brighton Collaboration Case Definition (BCCD) for ana-
phylaxis AEFI (Table 1) was then retrospectively applied by two
independentreviewers (DC and NC), who were not involved in any
SAEFVIC assessmentsat time of initial reporting, applying a level of
diagnostic certainty for each case (Table 2).
Vaccine specific dose administration data from the Australian
Childhood Immunisation Register (ACIR) and National HPV Vacci-
nation Program Registerwere used as the denominator to calculate
incidence estimates. Data was entered into a Microsoft Access
Database (Microsoft Corporation, Redmond, WA, USA) and ana-
lyzed with STATA 12.0 (Statacorp,TX, USA). Ethics approval was
obtained from The Royal Children’s Hospital Melbourne Human
ResearchEthics Committee.
3. Results
Twenty-five patients, with a total of 27 reports of anaphylaxis,
were identified in the six-year study period (Table 3). The median
age of immunization was 4.7 years (range 0.3–16.2 years), with
48%of cases male. Six cases (22.2%)were ≤12 months old when
receiving vaccination.Twenty-five of these casesmet BCCDcriteria
for anaphylaxis (Table 2), with a total of 37 vaccinesadministered.
Of these cases,nine (36%)met BCCD Level 1 diagnostic certainty,
15 (60%)Level 2 and one case Level 3 (4%).One case was deemed
Level 5 (not a case of anaphylaxis).
Thirteen cases included vaccines that are part of the routine
Australian infant and preschool immunization schedule,which has
evolved slightly through the study period [2]. The remaining 12
cases consisted of vaccines that are part of the routine Australian
secondary school immunization program. The vaccine antigens
administered included combination DTaP vaccines (DTaP com-
bined with other antigen) in 9 of 25 cases (36%).Measles mumps
rubella (MMR) vaccinewas receivedin six cases;five of whom had
concomitantvaccines(Table4). The majority of vaccines(93%)were
administered at a generalpractitioner’s(GP) primary care practice,
or at a specialist immunization nurse led local council vaccine
session. Immunization nurses also administered most secondary
school adolescentvaccines.
3.1. Anaphylaxisincidencerate
Vaccine coverageis approximately 91%at 12 months of age[12]
and 70–75%in the school program in Victoria [13]. 197,878 doses
of Infanrix IPVTM [GSK] were administered, with an incidence of
2.53 per 100,000doses [2.43,2.63].Likewise, 481,297doses of the
combination MMR vaccine were administered with an estimated
incidence of 1.25 per 100,000 doses [1.18, 1.32]. For 13-valent
pneumococcal (PCV13) vaccines, there were 498,039 doses with
an incidence of 0.6 per 100,000doses [0.55,0.65].
A total of 1,092,682vaccinedosesof Infanrix HexaTM [GSK] were
administered over the study period, yielding an estimated inci-
dence rate of 0.36 cases per 100,000 doses [0.32, 0.40, 95%CI]. A
minimum of 934,255 doses of HPV vaccines were administered
to pediatric patients within the study period, indicating an esti-
mated anaphylaxisincidence of 0.32 per 100,000doses[0.29,0.35]
(data courtesy of ACIR and the National HPV Vaccination Program
Register).
3.2. History of anaphylaxis/atopy
One infant had anaphylaxis on three separate occasions, with
different vaccines administered each time (Infanrix Hexa, Preve-
nar 13, Vaxigrip Jr). Skin tests followed by vaccine challengeswere
undertaken in an allergy clinic in a hospital setting as part of a
causality assessmentof specific vaccinesand/or components.One
formal allergy challenge was positive, with an anaphylactic reac-
tion at 40 min following Infanrix HexaTM vaccine; the challengefor
Prevenar 13 only resulted in an erythematousrash.
Five cases (20.5%)had a past history of anaphylaxis to food
items such as egg,nuts or seafood.All had already been prescribed
an epinephrine auto-injectable device, with three patients hav-
ing utilized it on a previous occasion for food related anaphylactic
episodes; however no device was used in any of the anaphylactic
AEFI cases.Eight caseshad a previous history of atopic disease;four
with asthma,six with eczemaand two with hayfever.
3.3. Time post-vaccination
The time anaphylaxisoccurred post-immunization is detailedin
Fig. 1. Anaphylaxis in 19 cases(70%)occurred ≤30 min after immu-
nization. A further two cases presented between 30 to ≤60 min
and the remaining three caseswere greaterthan 120 min following
immunization.
Symptoms resolved within 60 min of presentation for 15 cases,
with a further six resolved within 24 h. The remaining four had
symptoms persisting beyond 24 h, with one case having ongoing
angioedemaand urticaria for the following 6-days.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
D.R.Chenget al. / Vaccine33 (2015)1602–1607 1605
Table 4
Vaccinesadministeredto cases.
Vaccine name # of cases Type of vaccine Manufacturer Years in schedule Anaphylaxis incidence
(casesper 100,000
doses)
Boostrix 2 DTaP GlaxoSmithKline (GSK) 2007–13
Fluvax 2 Influenza CSL 2007–13
Gardasil 3 HPV CSL 2007–13 0.32
H-B Vax II Adult 3 Hepatitis B (Hep B) CSL 2007–13
Infanrix hexa 4 DTaP, Hep B, Polio, Haemophilus Influenzae (Hib) GSK 2007–13 0.36
Infanrix IPV 5 DTaP, Polio GSK 2007–13
Influvac 1 Influenza Abbott 2009–08
Panvax H1N1 1 Swine flu CSL 2007–13
Prevenar 1 Pneumococcal–7-valent Pfizer 2011–11
Prevenar 13 3 Pneumococcal–13-valent Pfizer 2011–13 0.6
Priorix 6 MMR GSK 2011–13 1.25
Rotateq 2 Rotavirus CSL 2007–13
Twinrix Junior (360/10) 1 Hep A, Hep B GSK 2008–13
Typherix 1 Typhoid GSK 2007–13
Varilrix 1 Varicella GSK 2007–13
Vaxigrip Jr 1 Influenza Sanofi Aventis 2007–13
Anaphylaxis treatmentwas variable,with some patients receiv-
ing multiple therapies. Eighteen cases (72%) were treated with
intramuscular adrenaline, 11 (44%) with corticosteroids and 11
(44%)with anti-histamine medication. Four children received no
treatment despite anaphylaxis being reported, with three of these
presenting as delayed anaphylaxis. Eight cases received nursing
assessmentand treatment, and a further eight cases received GP
assessment.15 cases(56%)attendeda hospital emergencydepart-
ment, with ten of these admitted for observation and/or further
treatment in hospital. No cases required admission to pediatric
intensive care. The majority of patients, 23 cases (85%)had out-
patient clinic follow-up and counsel regarding future vaccinations.
4. Discussion
This analysis using defined diagnostic criteria for anaphylaxis
AEFI within a defined pediatric population in an Australian set-
ting, utilizes data from a comprehensive state-wide passive AEFI
surveillancesystem,drawing reports from a population of over 1.05
million children under 18 years old [11].
A total of 85%(n =23) of cases were retrospectively identified
as meeting level 1 or 2 Brighton diagnostic criteria for anaphy-
laxis. This suggests that despite utilizing a passive surveillance
Fig. 1. Time to anaphylaxispost-immunization.
system, there is an existing high accuracy in recognizing anaphy-
laxis AEFI, which can be further enhanced by the implementation
of a standardized set of diagnostic criteria. Interestingly, Erlewyn-
Lajeunesseet al. examined anaphylaxis AEFI in the UK and noted
only seven cases of BCCD confirmed anaphylaxis within a year,
amongst a pediatric population of approximately 5.5 million [14]
whilst in our study,we identified 4 casesper annum in a population
of approximately 1.05 million.
Although an overall incidence rate was unable to be calculated
for this study, comparison to previous incidence rates for specific
vaccines was possible. Anaphylaxis incidence rates for combina-
tion DTaP and MMR vaccines were higher than previous results
from both active and passivesurveillance systems[6,15,16].In the
PCV13 vaccine group, Tseng et al. found no anaphylactic AEFI in
post-licensure studies compared to our study where three cases
were described [17]. However, it is important to note that Infan-
rix Hexa and PCV 13 are often concomitantly administered; as are
Infanrix IPV and MMR vaccines [2]. Hence, this may impact on
rates of anaphylaxis for both vaccinations.Incidence rates follow-
ing HPV vaccine were lower than previously noted, 2.6 versus our
0.3 casesper 100,000[18]. It seemsthat our enhancedsurveillance
through SAEFVIC identified a higher number of cases of anaphy-
laxis – therefore resulting in a generally higher incidence rate as
demonstrated.However, accurate identification of cases remains
an ongoing difficulty, even in coordinated networks with active
surveillance systemssuch as the British Pediatric Surveillanceunit
[14].
4.1. Vaccines& vaccineadministration
Most of the infant and preschool cases involved multiple
vaccinations (Table 4). The multiple vaccines, including various
adjuvants,make it extremely challenging to attribute causation to
one particular vaccineor component and requires specialist allergy
assessmentand review [19]. A full causality assessment,particu-
larly identifying if the vaccineehad any other exposureswhich may
have contributed to the reaction,is neededto ensureaccurateattri-
bution to specific vaccines [20]. This was undertaken in a similar
study analyzing HPV vaccine reactions noted in 2007–08 following
commencement of the program in Australia [21]. The two iden-
tified anaphylaxis cases following HPV vaccine analyzed by Liew
et al. (2008) are included in this analysis; one was found to have
a positive intradermal skin test to the vaccine – with an urticarial
reaction post dose 1 and anaphylaxis post dose 2 of 4vHPV. The
second casehad negativeskin test results, but also presentedwith
Table 4
Vaccinesadministeredto cases.
Vaccine name # of cases Type of vaccine Manufacturer Years in schedule Anaphylaxis incidence
(casesper 100,000
doses)
Boostrix 2 DTaP GlaxoSmithKline (GSK) 2007–13
Fluvax 2 Influenza CSL 2007–13
Gardasil 3 HPV CSL 2007–13 0.32
H-B Vax II Adult 3 Hepatitis B (Hep B) CSL 2007–13
Infanrix hexa 4 DTaP, Hep B, Polio, Haemophilus Influenzae (Hib) GSK 2007–13 0.36
Infanrix IPV 5 DTaP, Polio GSK 2007–13
Influvac 1 Influenza Abbott 2009–08
Panvax H1N1 1 Swine flu CSL 2007–13
Prevenar 1 Pneumococcal–7-valent Pfizer 2011–11
Prevenar 13 3 Pneumococcal–13-valent Pfizer 2011–13 0.6
Priorix 6 MMR GSK 2011–13 1.25
Rotateq 2 Rotavirus CSL 2007–13
Twinrix Junior (360/10) 1 Hep A, Hep B GSK 2008–13
Typherix 1 Typhoid GSK 2007–13
Varilrix 1 Varicella GSK 2007–13
Vaxigrip Jr 1 Influenza Sanofi Aventis 2007–13
Anaphylaxis treatmentwas variable,with some patients receiv-
ing multiple therapies. Eighteen cases (72%) were treated with
intramuscular adrenaline, 11 (44%) with corticosteroids and 11
(44%)with anti-histamine medication. Four children received no
treatment despite anaphylaxis being reported, with three of these
presenting as delayed anaphylaxis. Eight cases received nursing
assessmentand treatment, and a further eight cases received GP
assessment.15 cases(56%)attendeda hospital emergencydepart-
ment, with ten of these admitted for observation and/or further
treatment in hospital. No cases required admission to pediatric
intensive care. The majority of patients, 23 cases (85%)had out-
patient clinic follow-up and counsel regarding future vaccinations.
4. Discussion
This analysis using defined diagnostic criteria for anaphylaxis
AEFI within a defined pediatric population in an Australian set-
ting, utilizes data from a comprehensive state-wide passive AEFI
surveillancesystem,drawing reports from a population of over 1.05
million children under 18 years old [11].
A total of 85%(n =23) of cases were retrospectively identified
as meeting level 1 or 2 Brighton diagnostic criteria for anaphy-
laxis. This suggests that despite utilizing a passive surveillance
Fig. 1. Time to anaphylaxispost-immunization.
system, there is an existing high accuracy in recognizing anaphy-
laxis AEFI, which can be further enhanced by the implementation
of a standardized set of diagnostic criteria. Interestingly, Erlewyn-
Lajeunesseet al. examined anaphylaxis AEFI in the UK and noted
only seven cases of BCCD confirmed anaphylaxis within a year,
amongst a pediatric population of approximately 5.5 million [14]
whilst in our study,we identified 4 casesper annum in a population
of approximately 1.05 million.
Although an overall incidence rate was unable to be calculated
for this study, comparison to previous incidence rates for specific
vaccines was possible. Anaphylaxis incidence rates for combina-
tion DTaP and MMR vaccines were higher than previous results
from both active and passivesurveillance systems[6,15,16].In the
PCV13 vaccine group, Tseng et al. found no anaphylactic AEFI in
post-licensure studies compared to our study where three cases
were described [17]. However, it is important to note that Infan-
rix Hexa and PCV 13 are often concomitantly administered; as are
Infanrix IPV and MMR vaccines [2]. Hence, this may impact on
rates of anaphylaxis for both vaccinations.Incidence rates follow-
ing HPV vaccine were lower than previously noted, 2.6 versus our
0.3 casesper 100,000[18]. It seemsthat our enhancedsurveillance
through SAEFVIC identified a higher number of cases of anaphy-
laxis – therefore resulting in a generally higher incidence rate as
demonstrated.However, accurate identification of cases remains
an ongoing difficulty, even in coordinated networks with active
surveillance systemssuch as the British Pediatric Surveillanceunit
[14].
4.1. Vaccines& vaccineadministration
Most of the infant and preschool cases involved multiple
vaccinations (Table 4). The multiple vaccines, including various
adjuvants,make it extremely challenging to attribute causation to
one particular vaccineor component and requires specialist allergy
assessmentand review [19]. A full causality assessment,particu-
larly identifying if the vaccineehad any other exposureswhich may
have contributed to the reaction,is neededto ensureaccurateattri-
bution to specific vaccines [20]. This was undertaken in a similar
study analyzing HPV vaccine reactions noted in 2007–08 following
commencement of the program in Australia [21]. The two iden-
tified anaphylaxis cases following HPV vaccine analyzed by Liew
et al. (2008) are included in this analysis; one was found to have
a positive intradermal skin test to the vaccine – with an urticarial
reaction post dose 1 and anaphylaxis post dose 2 of 4vHPV. The
second casehad negativeskin test results, but also presentedwith
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1606 D.R.Chenget al. / Vaccine33 (2015)1602–1607
an urticarial reaction post dose 1 and anaphylaxis post dose 2 of
4vHPV.
It is probable that the infant who had multiple presentationsof
anaphylaxis was not classical immunoglobulin-E (IgE) mediated,
with IgG and other inflammatory pathways postulated [22]. This
hypothesis of non-IgE pathways, is further supported by the four
cases of anaphylaxis presenting >60min after vaccination; this is
consistent with previous studies indicating that a delayed non-IgE
mediated reaction or an IgE mediated reaction from exposure to
another allergen after immunization are the most likely explana-
tions for delayed anaphylaxis presentation [6,21].
4.2. Medical & allergichistory
It is also important to consider AEFI in the context of back-
ground rates of conditions that may be assessedincorrectly as an
AEFI. SAEFVIC has reviewed the backgroundrates of certain condi-
tions in Victoria which are commonly attributed to vaccineAEFIs –
specifically in relation to HPV vaccine introduction in males [23].
For example, both allergies and anaphylaxis are increasing
across westernized and urbanized populations, with some of the
highest rates (up to 10% of 12 month olds have egg allergy) of
both conditions identified in the authors’stateof Victoria, Australia
[24]. However, although 19%(n =5) of patients in this study had a
proven food allergy, anaphylaxis incidence rates for vaccineswere
still extremely low, suggestingminimal correlation. Furthermore,
although a history of atopic disease (32%)was more common in
the study than the general population (16.6%)[5], there was no
correlation with a definitive clinical outcome.
The evidence to support the link between atopic history
and increased risk of anaphylaxis AEFI is mixed [25]. Gruber
et al. demonstrated that there was no identifiable link between
occurrenceor severity of atopic diseaseand early childhood immu-
nization. Cumulativevaccinedoseswere shown to slightly decrease
the severity of atopic dermatitis, thought to be secondary to vac-
cine antigen“education”of the immune systemand shifting it away
from a Th2 immune response [26]. This corresponds to previous
findings investigating risk factors for anaphylaxis in combination
MMR vaccines[27].
4.3. Futurepractice
Whilst the BCCDcriteria provides a standardizedcasedefinition
to aid in the diagnosis of anaphylaxis,its clinical application in the
field can be difficult [9]. Passive surveillance systems are mostly
utilized by health professionals,but can also include reports from
community membersand parents.The availability or knowledge of
specific criteria is variable,resulting in a wide rangeof clinical data.
Where possible,SAEFVICcontactsall serious adversereporters and
vaccines for serious AEFI such as anaphylaxis.This enhanced pas-
sive surveillance data will improve on the capacity to categorize
anaphylaxis and make an accuratediagnosis.
Healthcare professionals reported all our SAEFVIC cases,some
of whom were familiar with BCCD criteria. Nonetheless, two
distinct patterns emerged suggesting clinical difficulty with the
application of BCCD. Each case involved at least a dermatolog-
ical or respiratory symptom – suggesting that these symptoms
were likely the most easily diagnosed or recognized,especially in
the community setting. Secondly, there was a relative dearth of
cardiovascular symptoms, with only three minor cardiovascular
symptoms reported in total. The definition of clinical cardiac symp-
toms requires both clinical assessmentand measurementsof blood
pressure,heart rate and capillary refill. The lack of available equip-
ment or awareness of these symptoms could have contributed to
the difficulty of determining and thus recording cardiovascular
symptoms in a community setting.
Application of the Brighton criteria to specific AEFI of inter-
est has been identified as a challenge [9]. The development of a
prospectivechecklist and glossaryof terms that could be instituted
state-wide where pediatric immunization is delivered would be
ideal to ensure uniform reporting.
Current practice guidelines suggestthat patients are observed
for at least 15 min for any adverse reaction [1]; the timing of our
cases would indicate that there is a possibility of missing ana-
phylactic episodes.Patients who have had a previous anaphylactic
reaction should have a specialized assessmentas detailed above.
This includes a discussion regarding risks and benefits of immu-
nization as anaphylaxis is usually considered a contraindication
to further vaccine doses. Close observation in a hospital setting is
required. Future vaccinations with the same vaccines are usually
contraindicatedif a true anaphylacticAEFI has been confirmed and
the antigen identified [28]. This is not the case for isolated hyper-
sensitivity reactions such as urticaria; thus it is paramount that
casesare correctly classifiedto ensureappropriate follow-up in the
future.
The managementof anaphylaxisshould always err on the side of
caution, even if it is not immediately clear whether BCCD criteria
are met but the patient is clinically compromised. Intramuscular
adrenalineis first line treatmentand should be given if indicated,as
was the casein the majority of thesecases.Adrenaline has minimal
side effects,including in caseswhich on later review are considered
not to be anaphylaxis.
5. Limitations
The use of a passive surveillance system and potential under-
reporting of AEFI, incomplete data of all vaccines administered
acrossthe study period (2007–2013),the ever-changingAustralian
immunization schedule,the large number of unique vaccines and
multiple time points involved (e.g. some vaccines are three-dose
schedules) means that true overall AEFI incidence rates are dif-
ficult to determine. Nonetheless, the comprehensive dataset and
robust reporting process employed by SAEFVIC coupled with inci-
dence rates of certain specific vaccines and data regarding overall
coverageof routine vaccinesincreasethe reliability of findings.
Diagnosis of anaphylaxis in the study is dependent on BCCD
criteria, which may overestimate numbers of cases. The validity
of the diagnostic criteria has been demonstrated in other studies
[18,29]. Care needs to be taken when drawing conclusions from
the above data, especially if estimating rates and trends or deter-
mining safetyof individual vaccines.The number of adverseevents
reported to SAEFVIC may reflect somewhat on the number of doses
of a specific vaccine administered, but interpreting safety trends
with a rare adverseeventlike anaphylaxisis complex. Another lim-
itation of this study is the analysis of allergy testing (if applicable)
for allergy casesidentified.This was beyondthe scopeof this report,
with further researchdetailing our vaccinechallengesin confirmed
casesof anaphylaxis to be detailed in future publications.
6. Conclusion
This is a comprehensive case series of a serious AEFI, anaphy-
laxis, in the pediatric population. We identified 27 cases, with
approximately 90%receiving adrenaline and no serious sequelae
identified. Diagnosticcriteria are useful but can be difficult to apply
in a passive vaccine surveillance system,with the main limitation
being a lack of information on cardiovascular status. Healthcare
professionals and vaccinees/parentsshould be aware that onset of
anaphylaxiscan be delayedmore than 30 min following immuniza-
tion and prompt administration of adrenaline is recommended if
the diagnosis is considered.
an urticarial reaction post dose 1 and anaphylaxis post dose 2 of
4vHPV.
It is probable that the infant who had multiple presentationsof
anaphylaxis was not classical immunoglobulin-E (IgE) mediated,
with IgG and other inflammatory pathways postulated [22]. This
hypothesis of non-IgE pathways, is further supported by the four
cases of anaphylaxis presenting >60min after vaccination; this is
consistent with previous studies indicating that a delayed non-IgE
mediated reaction or an IgE mediated reaction from exposure to
another allergen after immunization are the most likely explana-
tions for delayed anaphylaxis presentation [6,21].
4.2. Medical & allergichistory
It is also important to consider AEFI in the context of back-
ground rates of conditions that may be assessedincorrectly as an
AEFI. SAEFVIC has reviewed the backgroundrates of certain condi-
tions in Victoria which are commonly attributed to vaccineAEFIs –
specifically in relation to HPV vaccine introduction in males [23].
For example, both allergies and anaphylaxis are increasing
across westernized and urbanized populations, with some of the
highest rates (up to 10% of 12 month olds have egg allergy) of
both conditions identified in the authors’stateof Victoria, Australia
[24]. However, although 19%(n =5) of patients in this study had a
proven food allergy, anaphylaxis incidence rates for vaccineswere
still extremely low, suggestingminimal correlation. Furthermore,
although a history of atopic disease (32%)was more common in
the study than the general population (16.6%)[5], there was no
correlation with a definitive clinical outcome.
The evidence to support the link between atopic history
and increased risk of anaphylaxis AEFI is mixed [25]. Gruber
et al. demonstrated that there was no identifiable link between
occurrenceor severity of atopic diseaseand early childhood immu-
nization. Cumulativevaccinedoseswere shown to slightly decrease
the severity of atopic dermatitis, thought to be secondary to vac-
cine antigen“education”of the immune systemand shifting it away
from a Th2 immune response [26]. This corresponds to previous
findings investigating risk factors for anaphylaxis in combination
MMR vaccines[27].
4.3. Futurepractice
Whilst the BCCDcriteria provides a standardizedcasedefinition
to aid in the diagnosis of anaphylaxis,its clinical application in the
field can be difficult [9]. Passive surveillance systems are mostly
utilized by health professionals,but can also include reports from
community membersand parents.The availability or knowledge of
specific criteria is variable,resulting in a wide rangeof clinical data.
Where possible,SAEFVICcontactsall serious adversereporters and
vaccines for serious AEFI such as anaphylaxis.This enhanced pas-
sive surveillance data will improve on the capacity to categorize
anaphylaxis and make an accuratediagnosis.
Healthcare professionals reported all our SAEFVIC cases,some
of whom were familiar with BCCD criteria. Nonetheless, two
distinct patterns emerged suggesting clinical difficulty with the
application of BCCD. Each case involved at least a dermatolog-
ical or respiratory symptom – suggesting that these symptoms
were likely the most easily diagnosed or recognized,especially in
the community setting. Secondly, there was a relative dearth of
cardiovascular symptoms, with only three minor cardiovascular
symptoms reported in total. The definition of clinical cardiac symp-
toms requires both clinical assessmentand measurementsof blood
pressure,heart rate and capillary refill. The lack of available equip-
ment or awareness of these symptoms could have contributed to
the difficulty of determining and thus recording cardiovascular
symptoms in a community setting.
Application of the Brighton criteria to specific AEFI of inter-
est has been identified as a challenge [9]. The development of a
prospectivechecklist and glossaryof terms that could be instituted
state-wide where pediatric immunization is delivered would be
ideal to ensure uniform reporting.
Current practice guidelines suggestthat patients are observed
for at least 15 min for any adverse reaction [1]; the timing of our
cases would indicate that there is a possibility of missing ana-
phylactic episodes.Patients who have had a previous anaphylactic
reaction should have a specialized assessmentas detailed above.
This includes a discussion regarding risks and benefits of immu-
nization as anaphylaxis is usually considered a contraindication
to further vaccine doses. Close observation in a hospital setting is
required. Future vaccinations with the same vaccines are usually
contraindicatedif a true anaphylacticAEFI has been confirmed and
the antigen identified [28]. This is not the case for isolated hyper-
sensitivity reactions such as urticaria; thus it is paramount that
casesare correctly classifiedto ensureappropriate follow-up in the
future.
The managementof anaphylaxisshould always err on the side of
caution, even if it is not immediately clear whether BCCD criteria
are met but the patient is clinically compromised. Intramuscular
adrenalineis first line treatmentand should be given if indicated,as
was the casein the majority of thesecases.Adrenaline has minimal
side effects,including in caseswhich on later review are considered
not to be anaphylaxis.
5. Limitations
The use of a passive surveillance system and potential under-
reporting of AEFI, incomplete data of all vaccines administered
acrossthe study period (2007–2013),the ever-changingAustralian
immunization schedule,the large number of unique vaccines and
multiple time points involved (e.g. some vaccines are three-dose
schedules) means that true overall AEFI incidence rates are dif-
ficult to determine. Nonetheless, the comprehensive dataset and
robust reporting process employed by SAEFVIC coupled with inci-
dence rates of certain specific vaccines and data regarding overall
coverageof routine vaccinesincreasethe reliability of findings.
Diagnosis of anaphylaxis in the study is dependent on BCCD
criteria, which may overestimate numbers of cases. The validity
of the diagnostic criteria has been demonstrated in other studies
[18,29]. Care needs to be taken when drawing conclusions from
the above data, especially if estimating rates and trends or deter-
mining safetyof individual vaccines.The number of adverseevents
reported to SAEFVIC may reflect somewhat on the number of doses
of a specific vaccine administered, but interpreting safety trends
with a rare adverseeventlike anaphylaxisis complex. Another lim-
itation of this study is the analysis of allergy testing (if applicable)
for allergy casesidentified.This was beyondthe scopeof this report,
with further researchdetailing our vaccinechallengesin confirmed
casesof anaphylaxis to be detailed in future publications.
6. Conclusion
This is a comprehensive case series of a serious AEFI, anaphy-
laxis, in the pediatric population. We identified 27 cases, with
approximately 90%receiving adrenaline and no serious sequelae
identified. Diagnosticcriteria are useful but can be difficult to apply
in a passive vaccine surveillance system,with the main limitation
being a lack of information on cardiovascular status. Healthcare
professionals and vaccinees/parentsshould be aware that onset of
anaphylaxiscan be delayedmore than 30 min following immuniza-
tion and prompt administration of adrenaline is recommended if
the diagnosis is considered.

D.R.Chenget al. / Vaccine33 (2015)1602–1607 1607
Acknowledgements
Neal Halsey, Mandira Hiremath, Alissa McMinn for assistance
and advice in the study. We also thank the staff at ACIR and the
National HPV Vaccination Program Register for assistancein data
provision for the study.
Conflict of interest:The authors wish to confirm that there are
no known conflicts of interest associatedwith this publication and
there has been no significant financial support for this work that
could have influenced its outcome.
We confirm that the manuscript has been read and approved
by all named authors and that there are no other persons who
satisfied the criteria for authorship but are not listed. We further
confirm that the order of authors listed in the manuscript has been
approved by all of us. DC was the coordinating author, responsible
for design of the study, data collection and data analysis as well
as writing and finalizing the manuscript for submission. NC was
responsible for conceptualization of the study, data analysis and
writing/editing/finalizing the manuscript. KP, SC, MD and JB were
responsible for writing/editing the manuscript.
All authors confirm that they have given due consideration to
the protection of intellectual property associated with this work
and that there are no impediments to publication, including the
timing of publication, with respect to intellectual property. In so
doing we confirm that we have followed the regulations of our
institutions concerning intellectual property.
References
[1] National Health and Medical Research Council (NHMRC). The Australian
Immunisation Handbook. 10th ed. Canberra: Commonwealth of Australia;
2013.
[2] Department of Health, State Government of Victoria, Australia. Immun-
isation Schedule Victoria. 2014. Available at: http://www.health.vic.gov.au/
immunisation/factsheets/schedule-victoria.htm,accessed1 August 2014.
[3] Clothier HJ, Crawford NW, Kempe A, Buttery JP. Surveillanceof adverseevents
following immunisation: the model of SAEFVIC,Victoria. Commun Dis Intell Q
Rep 2011;35:294–8.
[4] RuggebergJU, Gold MS, Bayas JM, Blum MD, Bonhoeffer J, Friedlander S, et al.
Anaphylaxis: case definition and guidelines for data collection, analysis, and
presentationof immunization safetydata.Vaccine 2007;25:5675–84.
[5] Bohlke K, Davis RL, Marcy SM, Braun MM, DeStefano F, Black SB, et al.
Risk of anaphylaxis after vaccination of children and adolescents.Pediatrics
2003;112:815–20.
[6] Patja A, Davidkin I, Kurki T, Kallio MJ, Valle M, Peltola H. Seriousadverseevents
after measles–mumps–rubellavaccinationduring a fourteen-yearprospective
follow-up. Pediatr Infect Dis J 2000;19:1127–34.
[7] Caubet JC, Siegrist CA, Eigenmann PA. Allergic reactions and vaccines: distin-
guishing true and false reactions.Rev Med Suisse2009;5:416–9.
[8] Gold M. A clinical approach to investigationof suspectedvaccineanaphylaxis.
Curr Allergy Clin Immunol 2012;25:68–70.
[9] Gold MS, Gidudu J, Erlewyn-LajeunesseM, Law B. Brighton CollaborationWork-
ing Group on A. Can the Brighton Collaboration case definitions be used to
improve the quality of AdverseEventFollowing Immunization (AEFI) reporting.
Anaphylaxis as a casestudy. Vaccine 2010;28:4487–98.
[10] Clothier HJ, Crawford NW, Kempe A, Buttery JP. Surveillanceof adverseevents
following immunisation: The model of SAEFVIC Victoria. Commun Dis Intell Q
Rep 2011;35:294–8.
[11] Australian Bureau of Statistics (ABS). Population by Age and Sex, Regions of
Australia,2013.In: Australian Bureauof Statistics.Canberra:Australian Bureau
of Statistics;2014.
[12] National Centre for Immunisations Researchand Surveillance(NCIRS). Child-
hood Immunisation Coverageestimates.NCIRS,2013.
[13] Brotherton JM, Deeks SL, Campbell-Lloyd S, Misrachi A, Passaris I, Peterson
K, et al. Interim estimates of human papillomavirus vaccination coveragein
the school-based program in Australia. Communicable DiseasesIntelligence
2008;32:457–61.
[14] Erlewyn-LajeunesseM, Hunt LP, Heath PT, Finn A. Anaphylaxis as an adverse
eventfollowing immunisation in the UK and Ireland. Archiv DiseaseChildhood
2012;97:487–90.
[15] D’SouzaRM, Campbell-Lloyd S, Isaacs D, Gold M, BurgessM, Turnbull F, et al.
Adverse Events Following Immunisation associatedwith the 1998 Australian
Measles Control Campaign.In: Department of Health and Ageing AG, editor.
CommunicableDiseasesIntelligence2000,pp. 27–33.
[16] Nakayama T, Onoda K. Vaccine adverse events reported in post-marketing
study of the Kitasato Institute from 1994 to 2004.Vaccine 2007;25:570–6.
[17] Tseng HF, Sy LS, Liu IL, Qian L, Marcy SM, Weintraub E, et al. Postlicensure
surveillancefor pre-specifiedadverseeventsfollowing the 13-valent pneumo-
coccal conjugatevaccinein children. Vaccine 2013;31:2578–83.
[18] Brotherton JM, Gold MS, Kemp AS, McIntyre PB, BurgessMA, Campbell-LloydS,
et al. Anaphylaxis following quadrivalent human papillomavirus vaccination.
CMAJ: Can Med Assoc J 2008;179:525–33.
[19] Halsey NA, Edwards KM, Dekker CL, Klein NP, Baxter R, Larussa P, et al.
Algorithm to assesscausalityafter individual adverseeventsfollowing immun-
izations. Vaccine 2012;30:5791–8.
[20] Tozzi AE, Asturias EJ, BalakrishnanMR, HalseyNA, Law B, ZuberPL. Assessment
of causalityof individual adverseeventsfollowing immunization (AEFI): a WHO
tool for global use. Vaccine 2013;31:5041–6.
[21] Liew WK, Crawford N, Tang ML, Buttery J, Royle J, Gold M, et al. Hypersen-
sitivity reactions to human papillomavirus vaccine in Australian schoolgirls:
retrospectivecohort study. BMJ 2008;337:a2642.
[22] Khodoun MV, Mercatili P, Orekov T, Finkelman FD. Basophilsand macrophages
both contribute to IgG-mediatedanaphylaxis.J Immunol 2009;182:36.7.
[23] Clothier HJ, Lee KJ, SundararajanV, Buttery JP, Crawford NW. Human papillo-
mavirus vaccine in boys: backgroundrates of potential adverseevents.Med J
Aust 2013;198:554–8.
[24] Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al.
Prevalenceof challenge-provenIgE-mediated food allergy using population-
basedsampling and predeterminedchallengecriteria in infants. J Allergy Clin
Immunol 2011;127:668–76.
[25] Terhune TD, Deth RC. How aluminum adjuvants could promote and enhance
non-targetIgE synthesisin a genetically-vulnerablesub-population.J Immuno-
toxicol 2013;10:210–22.
[26] Gruber C, Warner J, Hill D, BauchauV, Group ES. Early atopic diseaseand early
childhood immunization – is there a link. Allergy 2008;63:1464–72.
[27] BonhoefferJ, Heininger U. Adverseeventsfollowing immunization: perception
and evidence.Curr Opin Infect Dis 2007;20:237–46.
[28] Crawford NW, Buttery JP. Adverse events following immunizations: fact and
fiction. Paediatr Child Health 2013;23:121–4.
[29] Erlewyn-Lajeunesse M, Dymond S, Slade I, Mansfield HL, Fish R, Jones O,
et al. Diagnostic utility of two case definitions for anaphylaxis. Drug Safety
2010;33:57–64.
Acknowledgements
Neal Halsey, Mandira Hiremath, Alissa McMinn for assistance
and advice in the study. We also thank the staff at ACIR and the
National HPV Vaccination Program Register for assistancein data
provision for the study.
Conflict of interest:The authors wish to confirm that there are
no known conflicts of interest associatedwith this publication and
there has been no significant financial support for this work that
could have influenced its outcome.
We confirm that the manuscript has been read and approved
by all named authors and that there are no other persons who
satisfied the criteria for authorship but are not listed. We further
confirm that the order of authors listed in the manuscript has been
approved by all of us. DC was the coordinating author, responsible
for design of the study, data collection and data analysis as well
as writing and finalizing the manuscript for submission. NC was
responsible for conceptualization of the study, data analysis and
writing/editing/finalizing the manuscript. KP, SC, MD and JB were
responsible for writing/editing the manuscript.
All authors confirm that they have given due consideration to
the protection of intellectual property associated with this work
and that there are no impediments to publication, including the
timing of publication, with respect to intellectual property. In so
doing we confirm that we have followed the regulations of our
institutions concerning intellectual property.
References
[1] National Health and Medical Research Council (NHMRC). The Australian
Immunisation Handbook. 10th ed. Canberra: Commonwealth of Australia;
2013.
[2] Department of Health, State Government of Victoria, Australia. Immun-
isation Schedule Victoria. 2014. Available at: http://www.health.vic.gov.au/
immunisation/factsheets/schedule-victoria.htm,accessed1 August 2014.
[3] Clothier HJ, Crawford NW, Kempe A, Buttery JP. Surveillanceof adverseevents
following immunisation: the model of SAEFVIC,Victoria. Commun Dis Intell Q
Rep 2011;35:294–8.
[4] RuggebergJU, Gold MS, Bayas JM, Blum MD, Bonhoeffer J, Friedlander S, et al.
Anaphylaxis: case definition and guidelines for data collection, analysis, and
presentationof immunization safetydata.Vaccine 2007;25:5675–84.
[5] Bohlke K, Davis RL, Marcy SM, Braun MM, DeStefano F, Black SB, et al.
Risk of anaphylaxis after vaccination of children and adolescents.Pediatrics
2003;112:815–20.
[6] Patja A, Davidkin I, Kurki T, Kallio MJ, Valle M, Peltola H. Seriousadverseevents
after measles–mumps–rubellavaccinationduring a fourteen-yearprospective
follow-up. Pediatr Infect Dis J 2000;19:1127–34.
[7] Caubet JC, Siegrist CA, Eigenmann PA. Allergic reactions and vaccines: distin-
guishing true and false reactions.Rev Med Suisse2009;5:416–9.
[8] Gold M. A clinical approach to investigationof suspectedvaccineanaphylaxis.
Curr Allergy Clin Immunol 2012;25:68–70.
[9] Gold MS, Gidudu J, Erlewyn-LajeunesseM, Law B. Brighton CollaborationWork-
ing Group on A. Can the Brighton Collaboration case definitions be used to
improve the quality of AdverseEventFollowing Immunization (AEFI) reporting.
Anaphylaxis as a casestudy. Vaccine 2010;28:4487–98.
[10] Clothier HJ, Crawford NW, Kempe A, Buttery JP. Surveillanceof adverseevents
following immunisation: The model of SAEFVIC Victoria. Commun Dis Intell Q
Rep 2011;35:294–8.
[11] Australian Bureau of Statistics (ABS). Population by Age and Sex, Regions of
Australia,2013.In: Australian Bureauof Statistics.Canberra:Australian Bureau
of Statistics;2014.
[12] National Centre for Immunisations Researchand Surveillance(NCIRS). Child-
hood Immunisation Coverageestimates.NCIRS,2013.
[13] Brotherton JM, Deeks SL, Campbell-Lloyd S, Misrachi A, Passaris I, Peterson
K, et al. Interim estimates of human papillomavirus vaccination coveragein
the school-based program in Australia. Communicable DiseasesIntelligence
2008;32:457–61.
[14] Erlewyn-LajeunesseM, Hunt LP, Heath PT, Finn A. Anaphylaxis as an adverse
eventfollowing immunisation in the UK and Ireland. Archiv DiseaseChildhood
2012;97:487–90.
[15] D’SouzaRM, Campbell-Lloyd S, Isaacs D, Gold M, BurgessM, Turnbull F, et al.
Adverse Events Following Immunisation associatedwith the 1998 Australian
Measles Control Campaign.In: Department of Health and Ageing AG, editor.
CommunicableDiseasesIntelligence2000,pp. 27–33.
[16] Nakayama T, Onoda K. Vaccine adverse events reported in post-marketing
study of the Kitasato Institute from 1994 to 2004.Vaccine 2007;25:570–6.
[17] Tseng HF, Sy LS, Liu IL, Qian L, Marcy SM, Weintraub E, et al. Postlicensure
surveillancefor pre-specifiedadverseeventsfollowing the 13-valent pneumo-
coccal conjugatevaccinein children. Vaccine 2013;31:2578–83.
[18] Brotherton JM, Gold MS, Kemp AS, McIntyre PB, BurgessMA, Campbell-LloydS,
et al. Anaphylaxis following quadrivalent human papillomavirus vaccination.
CMAJ: Can Med Assoc J 2008;179:525–33.
[19] Halsey NA, Edwards KM, Dekker CL, Klein NP, Baxter R, Larussa P, et al.
Algorithm to assesscausalityafter individual adverseeventsfollowing immun-
izations. Vaccine 2012;30:5791–8.
[20] Tozzi AE, Asturias EJ, BalakrishnanMR, HalseyNA, Law B, ZuberPL. Assessment
of causalityof individual adverseeventsfollowing immunization (AEFI): a WHO
tool for global use. Vaccine 2013;31:5041–6.
[21] Liew WK, Crawford N, Tang ML, Buttery J, Royle J, Gold M, et al. Hypersen-
sitivity reactions to human papillomavirus vaccine in Australian schoolgirls:
retrospectivecohort study. BMJ 2008;337:a2642.
[22] Khodoun MV, Mercatili P, Orekov T, Finkelman FD. Basophilsand macrophages
both contribute to IgG-mediatedanaphylaxis.J Immunol 2009;182:36.7.
[23] Clothier HJ, Lee KJ, SundararajanV, Buttery JP, Crawford NW. Human papillo-
mavirus vaccine in boys: backgroundrates of potential adverseevents.Med J
Aust 2013;198:554–8.
[24] Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al.
Prevalenceof challenge-provenIgE-mediated food allergy using population-
basedsampling and predeterminedchallengecriteria in infants. J Allergy Clin
Immunol 2011;127:668–76.
[25] Terhune TD, Deth RC. How aluminum adjuvants could promote and enhance
non-targetIgE synthesisin a genetically-vulnerablesub-population.J Immuno-
toxicol 2013;10:210–22.
[26] Gruber C, Warner J, Hill D, BauchauV, Group ES. Early atopic diseaseand early
childhood immunization – is there a link. Allergy 2008;63:1464–72.
[27] BonhoefferJ, Heininger U. Adverseeventsfollowing immunization: perception
and evidence.Curr Opin Infect Dis 2007;20:237–46.
[28] Crawford NW, Buttery JP. Adverse events following immunizations: fact and
fiction. Paediatr Child Health 2013;23:121–4.
[29] Erlewyn-Lajeunesse M, Dymond S, Slade I, Mansfield HL, Fish R, Jones O,
et al. Diagnostic utility of two case definitions for anaphylaxis. Drug Safety
2010;33:57–64.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.