Detailed Discharge Planning Report: Angelo's Lewy Body Dementia Care
VerifiedAdded on 2021/04/17
|18
|5110
|447
Report
AI Summary
This report details the discharge plan for Angelo, a patient with Lewy Body Dementia (LBD). The plan emphasizes a holistic approach, considering Angelo's medical history, current health status, and social life. It highlights the importance of multidisciplinary team (MDT) collaboration, including nurses, doctors, therapists, and social workers, to ensure a smooth transition from hospital to home. The report underscores the significance of family involvement, patient education, and effective communication. It addresses the complexities of LBD, including potential challenges with medication and behavior, and emphasizes the need for long-term care, including support from social workers, carers, and community resources. The report also discusses the importance of assessing Angelo's needs, coordinating care, and making necessary arrangements for his safety and well-being, such as home modifications and medication management. The report highlights the need for a patient-centered approach, considering Angelo's preferences and ensuring his dignity and independence are maintained throughout the discharge process. The report references the Nursing and Midwifery Council's (NMC) professional code of conduct and the Data Protection Act to ensure patient confidentiality.
Discharge Plan
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction :
Main objective of this essay is to elaborate discharge planning for Angelo with focus on
medical history, health status and social life. This essay will include aspects like planning,
roles and responsibilities of each member of multidisciplinary team, incorporation of family
members of patient and social worker in discharge planning and importance of effective
communication. In this essay, potential and actual situations will be discussed for the
discharge of Angelo. Holistic assessment of patient’s needs and preferences should be
arranged for Angelo to return to his home and back to independence with minimal assistance.
Nursing and Midwifery Council's (NMC) professional code of conduct (2015) will be
followed throughout the discharge planning. According to Data Protection Act (1998) and the
Nursing and Midwifery Council (NMC 2015) all the information related to the patient will be
kept confidential. Usually discharge planning is initiated from admission of the patient and
there is a possibility of alteration depending on the outcome of patient’s recovery during his
stay in the hospital. It is important that Family and friends is incorporated in discharge
planning. Family members of the patient should be educated about the health status of the
patient, diagnostic results, dose and frequency of medication administration, adherence to
medication administration and diet. Family members need to be educated about the changes
to care plan ato aid smooth transition back to the community. Views and wishes of the patient
and family members need to be considered while designing discharge planning. The
multidisciplinary team involved should make sure that patient is medically fit, and all the
facilities are available for his discharge. Arrangements should be made for continuity of care
after discharge and carers will be involved to help Mr Davies with his activity of daily living
(ADL) should also twice a day. In the case of Mr Davies as he lives in a sheltered
accommodation, the security should also be involved for him to increase his frequency of
checking on Mr Davies. Therefore, in the case of Mr Davis, his Discharge planning is
complex and should patient and family centred (Heath et al., 2015; Orlu-Gul et al., 2014).
Discharge plan helps to ensure smooth and safe move of patient from hospital to home.
Discharge plan is an ongoing procedure for safe movement of the patient without any
complication from the hospital facility to the home or society. In psychiatric patient like
Angelo, there should be symptoms change for movement from hospital to society. Psychiatric
patients might develop stigma of rejection from the society, hence this stigma should be
addressed before discharge form the hospital. Assessment of the discharge should be based
on the requirements and needs of the patient after discharge. Based on these requirements and
2
Main objective of this essay is to elaborate discharge planning for Angelo with focus on
medical history, health status and social life. This essay will include aspects like planning,
roles and responsibilities of each member of multidisciplinary team, incorporation of family
members of patient and social worker in discharge planning and importance of effective
communication. In this essay, potential and actual situations will be discussed for the
discharge of Angelo. Holistic assessment of patient’s needs and preferences should be
arranged for Angelo to return to his home and back to independence with minimal assistance.
Nursing and Midwifery Council's (NMC) professional code of conduct (2015) will be
followed throughout the discharge planning. According to Data Protection Act (1998) and the
Nursing and Midwifery Council (NMC 2015) all the information related to the patient will be
kept confidential. Usually discharge planning is initiated from admission of the patient and
there is a possibility of alteration depending on the outcome of patient’s recovery during his
stay in the hospital. It is important that Family and friends is incorporated in discharge
planning. Family members of the patient should be educated about the health status of the
patient, diagnostic results, dose and frequency of medication administration, adherence to
medication administration and diet. Family members need to be educated about the changes
to care plan ato aid smooth transition back to the community. Views and wishes of the patient
and family members need to be considered while designing discharge planning. The
multidisciplinary team involved should make sure that patient is medically fit, and all the
facilities are available for his discharge. Arrangements should be made for continuity of care
after discharge and carers will be involved to help Mr Davies with his activity of daily living
(ADL) should also twice a day. In the case of Mr Davies as he lives in a sheltered
accommodation, the security should also be involved for him to increase his frequency of
checking on Mr Davies. Therefore, in the case of Mr Davis, his Discharge planning is
complex and should patient and family centred (Heath et al., 2015; Orlu-Gul et al., 2014).
Discharge plan helps to ensure smooth and safe move of patient from hospital to home.
Discharge plan is an ongoing procedure for safe movement of the patient without any
complication from the hospital facility to the home or society. In psychiatric patient like
Angelo, there should be symptoms change for movement from hospital to society. Psychiatric
patients might develop stigma of rejection from the society, hence this stigma should be
addressed before discharge form the hospital. Assessment of the discharge should be based
on the requirements and needs of the patient after discharge. Based on these requirements and
2
needs of the patient, few patients need simple and other need complex discharge process.
Angelo require complex discharge process because he needs to receive care from district
nurses, general practitioner (GP), district nurses, and specialist nurse, community
psychiatrist, occupational therapist, physio therapist, social worker and carers (see table 1)
after discharge from the hospital. MDT for the discharge of Angelo should comprise of
nurse, doctor, care manager, occupational therapist, psychotherapist and discharge co-
coordinators (Day et al., 2009). The nurse in charge of the discharge must be able to liaise
with the social worker so that vital necessities and arrangements for Mr Angelo’s needs will
be communicated effectively to eradicate fail discharge (Tochimoto et al., 2015). ( I edited
this part and you can see how it makes sence) Angelo is awaiting discharge from the hospital
following Lewy body dementia. Lewy body dementia is the deposition of alpha-synuclein
proteins in the brain which are termed as Lewy bodies. It results in problems in thinking,
movement, behaviour, and mood. Lewy body dementia worsens condition of the patient
gradually. Hence, long term care need to be provided to John. Lewy body dementia can affect
patient both physically and mentally. It is evident in case of John also because he is being
experiencing fall and hallucination. Fall and hallucination indicates both physical and mental
impairment in John respectively. (Kosaka, 2016). From the reports and profile of Angelo, it
is evident that he received all the necessary care, attained satisfactory independence and he is
exhibiting good progress. There can be burden on the caregiver for the management of LBD
due to its complex nature. Hence, there should be incorporation of professionals from diverse
fields like medical, nursing, pharmacy and social (Heenan and Birrell, 2017). (whats the
relevance its repitition)
NMC Code of Professional Conduct (2015) was incorporated for independence,
empowerment and maintenance of Angelo. Angelo’s dignity should be considered and
community and social support should be provided to him after his discharge (see table 1)
(Burnard et al., 2004). (grammar is bad still you fail to read the guildlines and follow the step
no references to the table in the appendix)
Most of the patients with LBD are not responsive to antipsychotic medications, hence
discharge planners need to consider this before making discharge plan. Hence, neurologist
should be consulted and his input incorporated and follow up appointments need to be
arranged before Mr angelo is discharged (see table 1) Evidence based information related to
unresponsiveness of antipsychotic drugs for LBD patients should be shared with healthcare
providers (Boot et al., 2013) (what evidence please state and add reference). This information
3
Angelo require complex discharge process because he needs to receive care from district
nurses, general practitioner (GP), district nurses, and specialist nurse, community
psychiatrist, occupational therapist, physio therapist, social worker and carers (see table 1)
after discharge from the hospital. MDT for the discharge of Angelo should comprise of
nurse, doctor, care manager, occupational therapist, psychotherapist and discharge co-
coordinators (Day et al., 2009). The nurse in charge of the discharge must be able to liaise
with the social worker so that vital necessities and arrangements for Mr Angelo’s needs will
be communicated effectively to eradicate fail discharge (Tochimoto et al., 2015). ( I edited
this part and you can see how it makes sence) Angelo is awaiting discharge from the hospital
following Lewy body dementia. Lewy body dementia is the deposition of alpha-synuclein
proteins in the brain which are termed as Lewy bodies. It results in problems in thinking,
movement, behaviour, and mood. Lewy body dementia worsens condition of the patient
gradually. Hence, long term care need to be provided to John. Lewy body dementia can affect
patient both physically and mentally. It is evident in case of John also because he is being
experiencing fall and hallucination. Fall and hallucination indicates both physical and mental
impairment in John respectively. (Kosaka, 2016). From the reports and profile of Angelo, it
is evident that he received all the necessary care, attained satisfactory independence and he is
exhibiting good progress. There can be burden on the caregiver for the management of LBD
due to its complex nature. Hence, there should be incorporation of professionals from diverse
fields like medical, nursing, pharmacy and social (Heenan and Birrell, 2017). (whats the
relevance its repitition)
NMC Code of Professional Conduct (2015) was incorporated for independence,
empowerment and maintenance of Angelo. Angelo’s dignity should be considered and
community and social support should be provided to him after his discharge (see table 1)
(Burnard et al., 2004). (grammar is bad still you fail to read the guildlines and follow the step
no references to the table in the appendix)
Most of the patients with LBD are not responsive to antipsychotic medications, hence
discharge planners need to consider this before making discharge plan. Hence, neurologist
should be consulted and his input incorporated and follow up appointments need to be
arranged before Mr angelo is discharged (see table 1) Evidence based information related to
unresponsiveness of antipsychotic drugs for LBD patients should be shared with healthcare
providers (Boot et al., 2013) (what evidence please state and add reference). This information
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
should be provided to the family members and they should be educated about it (see table 1).
LBD patients like Angelo might experience sudden decline in the functioning and
unacceptable behaviour. Hence, this type of emergency can be tackled effectively by
providing this information to the family and carers that will be involved in his care while his
at home, Caregiver should control emotions while making discharge plan for LBD patient
like Angelo because there can be mixed emotions like loving, rewarding, anger and
impatience while providing care to the LBD patient. Caregiver might have changed
perception about Angelo due to his unacceptable behaviour due to LBD. Caregiver should
only focus on health issue of Angelo keeping aside feelings about Angelo (please elaborate I
don’t understand)(Cross et al., 2015).
There should be effective communication among members of MDT (multi-disciplinary team)
to ensure smooth transition and safe discharge to the society. A meeting should be arranged
involving the members of MDT team, family members and social worker to facilitate a
smooth discharge planning and implementation before Angelo is discharged from the
hospital. Effective communication can be helpful in making proper decisions for providing
care with the available resources. Angelo and family members need to communicate to the
MDT and influence decision making and proper person centered care that will meet all
Angelo’s needs (see table 1) (Pethybridge, 2004).
Angelo should be educated about the confusion and hallucination. MDT team should
convince him that there is no existence of genomes (what is the relevance). He is also
associated with conditions like Hypertension and Hyperlipidaemia. For these conditions, he
need to consume medicines on the regular basis. However, due to diseased condition, he
might forget to take medicines. Discharge co-ordinator should make all the arrangements to
monitor his medication consumption on regular basis. Since, he was staying alone at home
and falls occasionally, there should be arrangement for staying with him. Hence, there is
incorporation of occupational therapist. (good point but make it clear and use proper
grammar in this case say that’s why the occupational therapist will be involved to make sure
the house is safe for angelo to return back to by visiting his home and making sure all
equipments , wires, and harful stuff that will cause mr Davies harm will be removed, key safe
put in place , pendant alarm provided, just incase he falls so that help will come in time,
carers will come in 3 times a day to give him food and make sure he takes his medication and
also assist him with wash, shopping and cleaning the house, and helpwith his activity of daily
living)
4
LBD patients like Angelo might experience sudden decline in the functioning and
unacceptable behaviour. Hence, this type of emergency can be tackled effectively by
providing this information to the family and carers that will be involved in his care while his
at home, Caregiver should control emotions while making discharge plan for LBD patient
like Angelo because there can be mixed emotions like loving, rewarding, anger and
impatience while providing care to the LBD patient. Caregiver might have changed
perception about Angelo due to his unacceptable behaviour due to LBD. Caregiver should
only focus on health issue of Angelo keeping aside feelings about Angelo (please elaborate I
don’t understand)(Cross et al., 2015).
There should be effective communication among members of MDT (multi-disciplinary team)
to ensure smooth transition and safe discharge to the society. A meeting should be arranged
involving the members of MDT team, family members and social worker to facilitate a
smooth discharge planning and implementation before Angelo is discharged from the
hospital. Effective communication can be helpful in making proper decisions for providing
care with the available resources. Angelo and family members need to communicate to the
MDT and influence decision making and proper person centered care that will meet all
Angelo’s needs (see table 1) (Pethybridge, 2004).
Angelo should be educated about the confusion and hallucination. MDT team should
convince him that there is no existence of genomes (what is the relevance). He is also
associated with conditions like Hypertension and Hyperlipidaemia. For these conditions, he
need to consume medicines on the regular basis. However, due to diseased condition, he
might forget to take medicines. Discharge co-ordinator should make all the arrangements to
monitor his medication consumption on regular basis. Since, he was staying alone at home
and falls occasionally, there should be arrangement for staying with him. Hence, there is
incorporation of occupational therapist. (good point but make it clear and use proper
grammar in this case say that’s why the occupational therapist will be involved to make sure
the house is safe for angelo to return back to by visiting his home and making sure all
equipments , wires, and harful stuff that will cause mr Davies harm will be removed, key safe
put in place , pendant alarm provided, just incase he falls so that help will come in time,
carers will come in 3 times a day to give him food and make sure he takes his medication and
also assist him with wash, shopping and cleaning the house, and helpwith his activity of daily
living)
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Patient participation in the hospital discharge can be helpful in establishing safe care. It can
be helpful in improving patient satisfaction and reducing risk of hospital readmissions.
Effective patient and family members participation can be achieved by integrated and co-
ordinated care provide by MDT. Angelo should receive continued care after discharge, his
social needs to be identified and holistic care needs to be provided to Angelo. Holistic care
will include is social well-being, psychological, (list the holistic care) to Angelo should be
provided for giving not only medical care but also to improve well being of Angelo (see table
2) (Dyrstad et al., 2015).
Long-term care (LTC) is necessary for Angelo because providing care to the patients like
Angelo by social workers and carers for the longer duration would be difficult (a sheer
contast you said its necessary , so give rational). Long-term care can provide care based on
the individuals needs. Physical, mental and social well being of the patient like Angelo can be
achieved through long-term care. Long term care not only consider therapeutic care but also
other aspects like activities of daily living (ADL). ADL include bathing, toilet use, dressing
and grooming, moving about and eating. LTC is necessary for Angelo to keep him healthy, to
maintain his wellbeing and to protect him from injury. LTC can also be helpful for Angelo
for improving access to care. Social support groups and family members should play
significant role in improving access to care for Angelo because Angelo could be more
accessible to these groups after discharge to provide LTC (this is repition but if it must be
used in this contest then explain why clearly). It is evident that LBD patients face problems in
terms of ADL and access to care. Challenges in care also need to be considered while
providing LTC to Angelo. LBD is complicated with multiple symptoms. Hence, physician
should consider only prominent symptoms which are more disturbing to Angelo (McKeith et
al., 2009). There might be disagreement between caregiver and Angelo. Angelo might
experience hallucination, however caregiver might not be agreed with him on his
hallucinating state. Hallucination might be more disturbing to Angelo, however; caregiver
might not consider as a serious issue for Angelo. On the other side, caregiver might be more
concerned about the fluctuating memory of Angelo due to his confused state. In LTC, open
discussion should occur between Angelo and caregiver because in LBD, medications useful
for one symptom can exaggerate another symptom. LTC is not feasible for LBD patients in
the hospital premises because hospital management try to avoid hospitalisation of LBD
patients for longer duration. Due to consumption of neuroleptics, there might be behavioural
manifestations in LBD patients and it can lead to adverse effects. Hence, effective discharge
5
be helpful in improving patient satisfaction and reducing risk of hospital readmissions.
Effective patient and family members participation can be achieved by integrated and co-
ordinated care provide by MDT. Angelo should receive continued care after discharge, his
social needs to be identified and holistic care needs to be provided to Angelo. Holistic care
will include is social well-being, psychological, (list the holistic care) to Angelo should be
provided for giving not only medical care but also to improve well being of Angelo (see table
2) (Dyrstad et al., 2015).
Long-term care (LTC) is necessary for Angelo because providing care to the patients like
Angelo by social workers and carers for the longer duration would be difficult (a sheer
contast you said its necessary , so give rational). Long-term care can provide care based on
the individuals needs. Physical, mental and social well being of the patient like Angelo can be
achieved through long-term care. Long term care not only consider therapeutic care but also
other aspects like activities of daily living (ADL). ADL include bathing, toilet use, dressing
and grooming, moving about and eating. LTC is necessary for Angelo to keep him healthy, to
maintain his wellbeing and to protect him from injury. LTC can also be helpful for Angelo
for improving access to care. Social support groups and family members should play
significant role in improving access to care for Angelo because Angelo could be more
accessible to these groups after discharge to provide LTC (this is repition but if it must be
used in this contest then explain why clearly). It is evident that LBD patients face problems in
terms of ADL and access to care. Challenges in care also need to be considered while
providing LTC to Angelo. LBD is complicated with multiple symptoms. Hence, physician
should consider only prominent symptoms which are more disturbing to Angelo (McKeith et
al., 2009). There might be disagreement between caregiver and Angelo. Angelo might
experience hallucination, however caregiver might not be agreed with him on his
hallucinating state. Hallucination might be more disturbing to Angelo, however; caregiver
might not consider as a serious issue for Angelo. On the other side, caregiver might be more
concerned about the fluctuating memory of Angelo due to his confused state. In LTC, open
discussion should occur between Angelo and caregiver because in LBD, medications useful
for one symptom can exaggerate another symptom. LTC is not feasible for LBD patients in
the hospital premises because hospital management try to avoid hospitalisation of LBD
patients for longer duration. Due to consumption of neuroleptics, there might be behavioural
manifestations in LBD patients and it can lead to adverse effects. Hence, effective discharge
5
plan should be implemented for Angelo for timely discharge and arrangements should be
made for LTC at home. Accessibility of Angelo for the outpatient physicians should be
improved to avoid unnecessary hospitalisation (Blanc et al., 2017).
Coordination is most important aspect in the discharge process. Nurse need to play both shift
discharge coordinator and full time discharge coordinator for Angelo. Discharge coordinators
should perform the tasks of communication, functioning of MDT and assessment. Expected
date of discharge for Angelo should be decided within 48 hours of admission to the hospital.
However, it is difficult to implement strictly based on the needs of the patient. Hospital
policy also need to be considered while deciding discharge date for Angelo (Lin et al., 2014).
Making decision on the date of discharge as early as possible would be helpful in the
preparation of discharge plan and its smooth implementation. However, date can be amended
based on the reassessment of the patient condition and progress with respect to clinical
management plan. Making decision on the date of discharge is based on the overall hospital
capacity, progress of clinical outcomes and patient’s expectations. For effective discharge
planning clinical management plan of Angelo should be reviewed on daily basis. Clinical
management plan can be reviewed by implementing review, action, progress (RAP). Timely
update of clinical management plan to MDT and Angelo is important aspect in discharge
planning (see table 2) (Mortenson and Bishop, 2016).
In discharge planning, attention should be given to prevent readmission of Angelo to the
hospital. Readmissions can be prevented by ensuring discharge checklist is completed,
ensuring Angelo or his family members understands about diagnosis, medication
consumption and side effects of medications, ensuring Angelo can visit GP after discharge
from the hospital and ensuring Angelo is satisfied with the discharge process. Empowerment
of Angelo and his family members in the discharge process is important aspect in discharge
process. Patient expectations, complexities and challenges need to be considered for the
empowerment of the patient. Medical and social care partners play significant role in the
empowerment of the patient (Russell et al., 2014). Clinical referrals are important for the
empowerment of patient. Empowerment can be achieved by providing support services like
intermediate care and dementia care to Angelo. Involvement of patient in the discharge plan
requires experience and patience. There should be operative discussion among patient, family
members, MDT, discharge co-ordinator and social workers for the empowerment of the
patient in the discharge process (Shepperd et al., 2013). Discharge checklist should be ready
48 hours prior to discharge. However, in most of the cases it is difficult to maintain same
6
made for LTC at home. Accessibility of Angelo for the outpatient physicians should be
improved to avoid unnecessary hospitalisation (Blanc et al., 2017).
Coordination is most important aspect in the discharge process. Nurse need to play both shift
discharge coordinator and full time discharge coordinator for Angelo. Discharge coordinators
should perform the tasks of communication, functioning of MDT and assessment. Expected
date of discharge for Angelo should be decided within 48 hours of admission to the hospital.
However, it is difficult to implement strictly based on the needs of the patient. Hospital
policy also need to be considered while deciding discharge date for Angelo (Lin et al., 2014).
Making decision on the date of discharge as early as possible would be helpful in the
preparation of discharge plan and its smooth implementation. However, date can be amended
based on the reassessment of the patient condition and progress with respect to clinical
management plan. Making decision on the date of discharge is based on the overall hospital
capacity, progress of clinical outcomes and patient’s expectations. For effective discharge
planning clinical management plan of Angelo should be reviewed on daily basis. Clinical
management plan can be reviewed by implementing review, action, progress (RAP). Timely
update of clinical management plan to MDT and Angelo is important aspect in discharge
planning (see table 2) (Mortenson and Bishop, 2016).
In discharge planning, attention should be given to prevent readmission of Angelo to the
hospital. Readmissions can be prevented by ensuring discharge checklist is completed,
ensuring Angelo or his family members understands about diagnosis, medication
consumption and side effects of medications, ensuring Angelo can visit GP after discharge
from the hospital and ensuring Angelo is satisfied with the discharge process. Empowerment
of Angelo and his family members in the discharge process is important aspect in discharge
process. Patient expectations, complexities and challenges need to be considered for the
empowerment of the patient. Medical and social care partners play significant role in the
empowerment of the patient (Russell et al., 2014). Clinical referrals are important for the
empowerment of patient. Empowerment can be achieved by providing support services like
intermediate care and dementia care to Angelo. Involvement of patient in the discharge plan
requires experience and patience. There should be operative discussion among patient, family
members, MDT, discharge co-ordinator and social workers for the empowerment of the
patient in the discharge process (Shepperd et al., 2013). Discharge checklist should be ready
48 hours prior to discharge. However, in most of the cases it is difficult to maintain same
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

checklist at the time of actual discharge. Primary and social care involvement is required for
preparing discharge checklist. Planning stage, pre-discharge and vital aspects of discharge
should not be missed from the checklist (see appendix 3) (Soong et al., 2013).
Conclusion:
Discharge planning can be a tough job in case of patients with complex discharge. Discharge
planning in case of Angelo is also a complex process. Effective discharge for Angelo can be
achieved by incorporation of different professionals of MDT. LTC should be considered in
the discharge process of Angelo. Planned discharge process proved to be useful in reducing
unnecessary readmissions. Effective communication among MDT, Angelo and family
members can provide person centred care to Angelo and also it can empower Angelo.
Effective discharge planning is necessary to ensure timely discharge and continuity of care.
Please review again and refer to the table, one which will explain with definition of the role
of the multidisciplinary team which will be involved, table two will be for discharge
planning, which will show assessment, goal, intervention and the rational. Please!!!!!!! I need
to pass that’s why I am paying for it.
7
preparing discharge checklist. Planning stage, pre-discharge and vital aspects of discharge
should not be missed from the checklist (see appendix 3) (Soong et al., 2013).
Conclusion:
Discharge planning can be a tough job in case of patients with complex discharge. Discharge
planning in case of Angelo is also a complex process. Effective discharge for Angelo can be
achieved by incorporation of different professionals of MDT. LTC should be considered in
the discharge process of Angelo. Planned discharge process proved to be useful in reducing
unnecessary readmissions. Effective communication among MDT, Angelo and family
members can provide person centred care to Angelo and also it can empower Angelo.
Effective discharge planning is necessary to ensure timely discharge and continuity of care.
Please review again and refer to the table, one which will explain with definition of the role
of the multidisciplinary team which will be involved, table two will be for discharge
planning, which will show assessment, goal, intervention and the rational. Please!!!!!!! I need
to pass that’s why I am paying for it.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Reference:
Blanc, F., Mahmoudi, R., Jonveaux, T., et al. (2017). Long-term cognitive outcome of
Alzheimer's disease and dementia with Lewy bodies: dual disease is worse. Alzheimer's
Research & Therapy, 9(1):47. doi: 10.1186/s13195-017-0272-8.
Boot, B. P, McDade, E. M., McGinnis, S. M., and Boeve, B. F. (2013). Treatment of
Dementia with Lewy Bodies. Current Treatment Options in Neurology, 15(6), 738–764.
Burnard, P., Christine, M. C., and Susan, S. (2004). Professional and Ethical Issues in
Nursing. Baillière Tindall.
Cross, N., Terpening, Z., Rogers, N.L., Naism et al. (2015). Napping in older people 'at risk'
of dementia: relationships with depression, cognition, medical burden and sleep quality.
Journal of Sleep Research, 24(5), pp. 494-502.
Day, M.R., McCarthy,G., and Coffey, A. (2009) Discharge planning: the role of the discharge
co-ordinator. Nursing Older People, 21, (1), pp. 26-31
Dyrstad, D.N., Laugaland, K.A., and Storm, M. (2015). An observational study of older
patients' participation in hospital admission and discharge--exploring patient and next of kin
perspectives. Journal of Clinical Nursing, 24(11-12), pp. 1693-706.
Greenhalgh, T. (2013). Primary Health Care: Theory and Practice. John Wiley & Sons.
Heenan, D., and Birrell, D. (2017). The Integration of Health and Social Care in the UK:
Policy and Practice. Macmillan International Higher Education.
Heath, H., Sturdy, D. and Cheesly, A. (2010) Discharge planning: A summary of the
Department of Health’s guidance Ready to go. Planning the discharge and the transfer of
patients from hospital and intermediate care. Harrow: RCN Publishing Company Ltd.
Housley, W. (2017). Interaction in Multidisciplinary Teams. Routledge.
Kosaka, K. (2016). Dementia with Lewy Bodies: Clinical and Biological Aspects. Springer.
Lin, R., Gallagher, R., Spinaze, M., et al. (2014). Effect of a patient-directed discharge letter
on patient understanding of their hospitalisation. Journal of Internal Medicine, 44(9), pp.
851-7.
McKeith, I. (2009). Top cited papers in International Psychogeriatrics: 1. Long-term use of
rivastigmine in patients with dementia with Lewy bodies: an open-label trial. International
Psychogeriatrics, 21(1), pp. 5-6.
Mortenson, W.B., and Bishop, A.M. (2016). Discharge Criteria and Follow-Up Support for
Dementia Care Units. Journal of Applied Gerontology, 35(3), pp. 321-30.
Orlu-Gul, M., Raimi-Abraham, B., Jamieson, E., Wei, L., Murray, M., Stawarz, K.,
Stegemann, S., Tuleu, C. and Smith, F.J. (2014) Public engagement workshop: How to
improve medicines for older people?. International journal of pharmaceutics, 459(1), pp.65-
69.
Pethybridge, J. How team working influences discharge planning from hospital: a study of
four multi-disciplinary teams in an acute hospital in England. Journal of Interprofessional
Care, 18(1), pp. 29-41.
8
Blanc, F., Mahmoudi, R., Jonveaux, T., et al. (2017). Long-term cognitive outcome of
Alzheimer's disease and dementia with Lewy bodies: dual disease is worse. Alzheimer's
Research & Therapy, 9(1):47. doi: 10.1186/s13195-017-0272-8.
Boot, B. P, McDade, E. M., McGinnis, S. M., and Boeve, B. F. (2013). Treatment of
Dementia with Lewy Bodies. Current Treatment Options in Neurology, 15(6), 738–764.
Burnard, P., Christine, M. C., and Susan, S. (2004). Professional and Ethical Issues in
Nursing. Baillière Tindall.
Cross, N., Terpening, Z., Rogers, N.L., Naism et al. (2015). Napping in older people 'at risk'
of dementia: relationships with depression, cognition, medical burden and sleep quality.
Journal of Sleep Research, 24(5), pp. 494-502.
Day, M.R., McCarthy,G., and Coffey, A. (2009) Discharge planning: the role of the discharge
co-ordinator. Nursing Older People, 21, (1), pp. 26-31
Dyrstad, D.N., Laugaland, K.A., and Storm, M. (2015). An observational study of older
patients' participation in hospital admission and discharge--exploring patient and next of kin
perspectives. Journal of Clinical Nursing, 24(11-12), pp. 1693-706.
Greenhalgh, T. (2013). Primary Health Care: Theory and Practice. John Wiley & Sons.
Heenan, D., and Birrell, D. (2017). The Integration of Health and Social Care in the UK:
Policy and Practice. Macmillan International Higher Education.
Heath, H., Sturdy, D. and Cheesly, A. (2010) Discharge planning: A summary of the
Department of Health’s guidance Ready to go. Planning the discharge and the transfer of
patients from hospital and intermediate care. Harrow: RCN Publishing Company Ltd.
Housley, W. (2017). Interaction in Multidisciplinary Teams. Routledge.
Kosaka, K. (2016). Dementia with Lewy Bodies: Clinical and Biological Aspects. Springer.
Lin, R., Gallagher, R., Spinaze, M., et al. (2014). Effect of a patient-directed discharge letter
on patient understanding of their hospitalisation. Journal of Internal Medicine, 44(9), pp.
851-7.
McKeith, I. (2009). Top cited papers in International Psychogeriatrics: 1. Long-term use of
rivastigmine in patients with dementia with Lewy bodies: an open-label trial. International
Psychogeriatrics, 21(1), pp. 5-6.
Mortenson, W.B., and Bishop, A.M. (2016). Discharge Criteria and Follow-Up Support for
Dementia Care Units. Journal of Applied Gerontology, 35(3), pp. 321-30.
Orlu-Gul, M., Raimi-Abraham, B., Jamieson, E., Wei, L., Murray, M., Stawarz, K.,
Stegemann, S., Tuleu, C. and Smith, F.J. (2014) Public engagement workshop: How to
improve medicines for older people?. International journal of pharmaceutics, 459(1), pp.65-
69.
Pethybridge, J. How team working influences discharge planning from hospital: a study of
four multi-disciplinary teams in an acute hospital in England. Journal of Interprofessional
Care, 18(1), pp. 29-41.
8
Russell, P., Hewage, U., and Thompson, C. (2014). Method for improving the quality of
discharge summaries written by a general medical team. Internal Medicine Journal, 44(3),
pp.298-301.
Shepperd, S., Lannin, N.A., Clemson, L.M., et al. (2013). Discharge planning from hospital
to home. Cochrane Database of Systematic Reviews, 31, (1):CD000313. doi:
10.1002/14651858.CD000313.
Soong, C., Daub, S., Lee, J., et al. (2013). Development of a checklist of safe discharge
practices for hospital patients. Journal of Hospital Medicine, 8(8), 444-9.
Tochimoto, S., Kitamura, M., Hino, S., and Kitamura, T. (2015). Predictors of home
discharge among patients hospitalized for behavioural and psychological symptoms of
dementia. Psychogeriatrics, 15(4), pp. 248-54.
Whitworth, H.B., and Whitworth, J. (2010). A Caregiver's Guide to Lewy Body Dementia.
Demos Medical Publishing.
Zun, L.S. (2013). Behavioral Emergencies for the Emergency Physician. Cambridge
University Press.
9
discharge summaries written by a general medical team. Internal Medicine Journal, 44(3),
pp.298-301.
Shepperd, S., Lannin, N.A., Clemson, L.M., et al. (2013). Discharge planning from hospital
to home. Cochrane Database of Systematic Reviews, 31, (1):CD000313. doi:
10.1002/14651858.CD000313.
Soong, C., Daub, S., Lee, J., et al. (2013). Development of a checklist of safe discharge
practices for hospital patients. Journal of Hospital Medicine, 8(8), 444-9.
Tochimoto, S., Kitamura, M., Hino, S., and Kitamura, T. (2015). Predictors of home
discharge among patients hospitalized for behavioural and psychological symptoms of
dementia. Psychogeriatrics, 15(4), pp. 248-54.
Whitworth, H.B., and Whitworth, J. (2010). A Caregiver's Guide to Lewy Body Dementia.
Demos Medical Publishing.
Zun, L.S. (2013). Behavioral Emergencies for the Emergency Physician. Cambridge
University Press.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
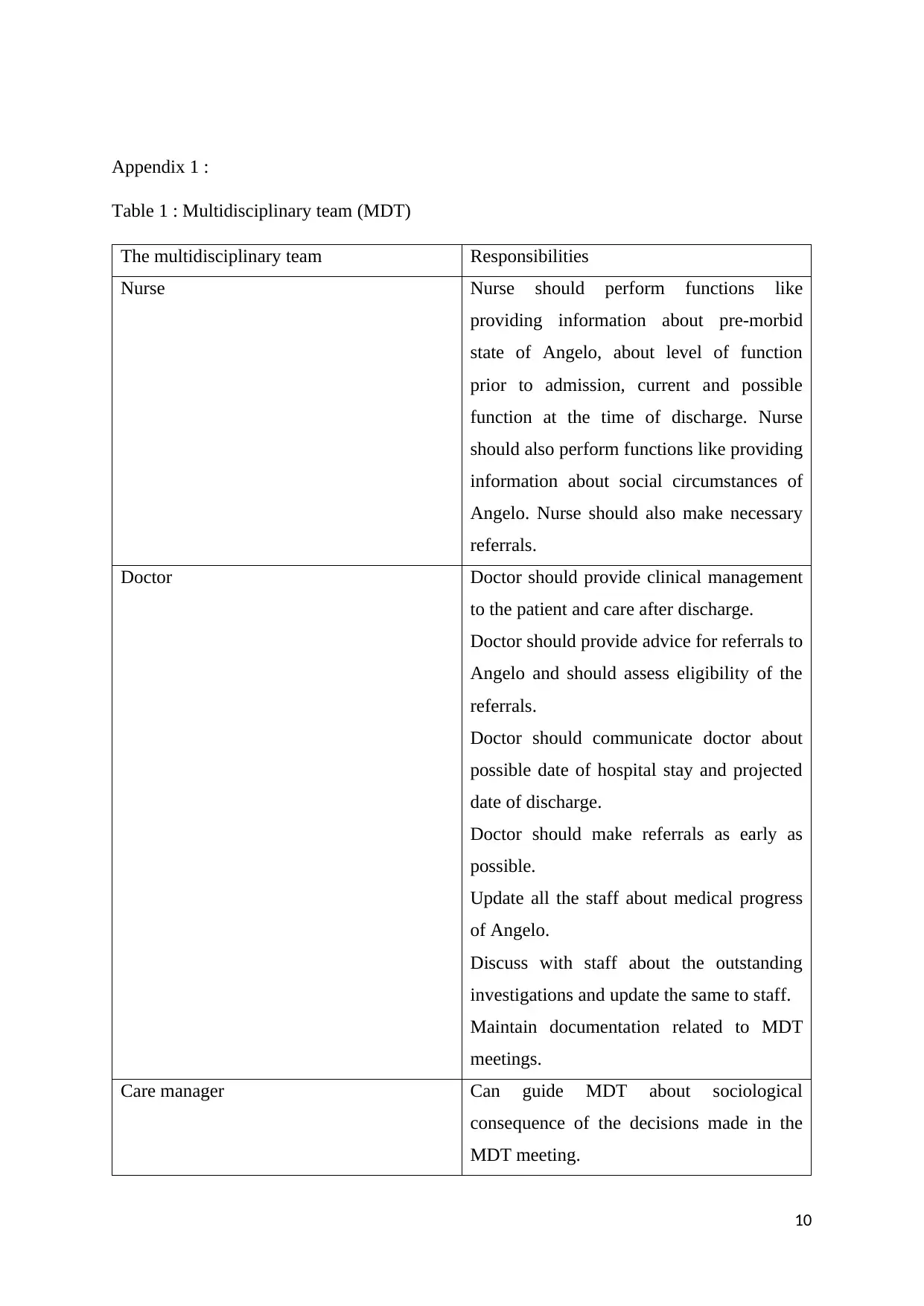
Appendix 1 :
Table 1 : Multidisciplinary team (MDT)
The multidisciplinary team Responsibilities
Nurse Nurse should perform functions like
providing information about pre-morbid
state of Angelo, about level of function
prior to admission, current and possible
function at the time of discharge. Nurse
should also perform functions like providing
information about social circumstances of
Angelo. Nurse should also make necessary
referrals.
Doctor Doctor should provide clinical management
to the patient and care after discharge.
Doctor should provide advice for referrals to
Angelo and should assess eligibility of the
referrals.
Doctor should communicate doctor about
possible date of hospital stay and projected
date of discharge.
Doctor should make referrals as early as
possible.
Update all the staff about medical progress
of Angelo.
Discuss with staff about the outstanding
investigations and update the same to staff.
Maintain documentation related to MDT
meetings.
Care manager Can guide MDT about sociological
consequence of the decisions made in the
MDT meeting.
10
Table 1 : Multidisciplinary team (MDT)
The multidisciplinary team Responsibilities
Nurse Nurse should perform functions like
providing information about pre-morbid
state of Angelo, about level of function
prior to admission, current and possible
function at the time of discharge. Nurse
should also perform functions like providing
information about social circumstances of
Angelo. Nurse should also make necessary
referrals.
Doctor Doctor should provide clinical management
to the patient and care after discharge.
Doctor should provide advice for referrals to
Angelo and should assess eligibility of the
referrals.
Doctor should communicate doctor about
possible date of hospital stay and projected
date of discharge.
Doctor should make referrals as early as
possible.
Update all the staff about medical progress
of Angelo.
Discuss with staff about the outstanding
investigations and update the same to staff.
Maintain documentation related to MDT
meetings.
Care manager Can guide MDT about sociological
consequence of the decisions made in the
MDT meeting.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
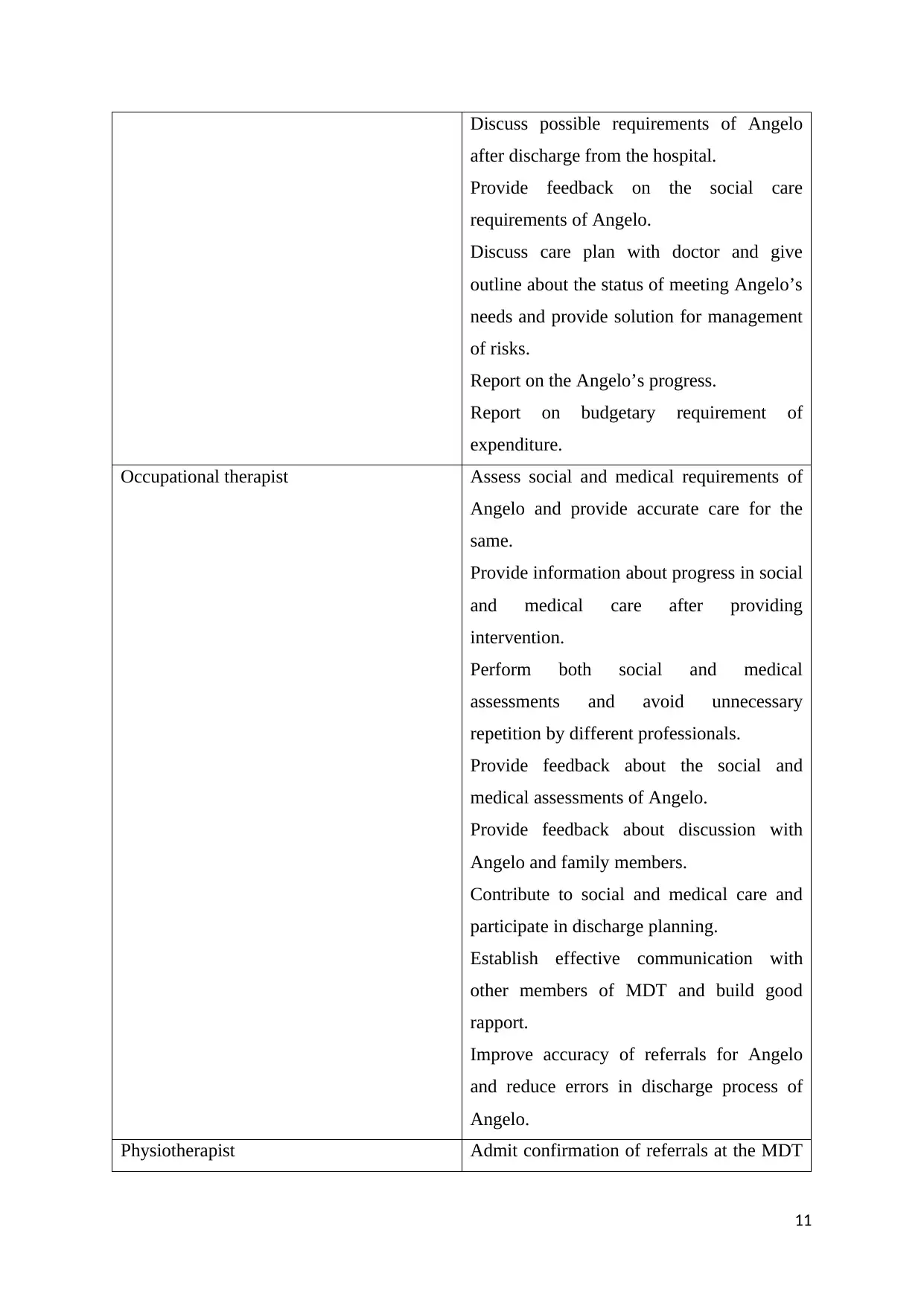
Discuss possible requirements of Angelo
after discharge from the hospital.
Provide feedback on the social care
requirements of Angelo.
Discuss care plan with doctor and give
outline about the status of meeting Angelo’s
needs and provide solution for management
of risks.
Report on the Angelo’s progress.
Report on budgetary requirement of
expenditure.
Occupational therapist Assess social and medical requirements of
Angelo and provide accurate care for the
same.
Provide information about progress in social
and medical care after providing
intervention.
Perform both social and medical
assessments and avoid unnecessary
repetition by different professionals.
Provide feedback about the social and
medical assessments of Angelo.
Provide feedback about discussion with
Angelo and family members.
Contribute to social and medical care and
participate in discharge planning.
Establish effective communication with
other members of MDT and build good
rapport.
Improve accuracy of referrals for Angelo
and reduce errors in discharge process of
Angelo.
Physiotherapist Admit confirmation of referrals at the MDT
11
after discharge from the hospital.
Provide feedback on the social care
requirements of Angelo.
Discuss care plan with doctor and give
outline about the status of meeting Angelo’s
needs and provide solution for management
of risks.
Report on the Angelo’s progress.
Report on budgetary requirement of
expenditure.
Occupational therapist Assess social and medical requirements of
Angelo and provide accurate care for the
same.
Provide information about progress in social
and medical care after providing
intervention.
Perform both social and medical
assessments and avoid unnecessary
repetition by different professionals.
Provide feedback about the social and
medical assessments of Angelo.
Provide feedback about discussion with
Angelo and family members.
Contribute to social and medical care and
participate in discharge planning.
Establish effective communication with
other members of MDT and build good
rapport.
Improve accuracy of referrals for Angelo
and reduce errors in discharge process of
Angelo.
Physiotherapist Admit confirmation of referrals at the MDT
11
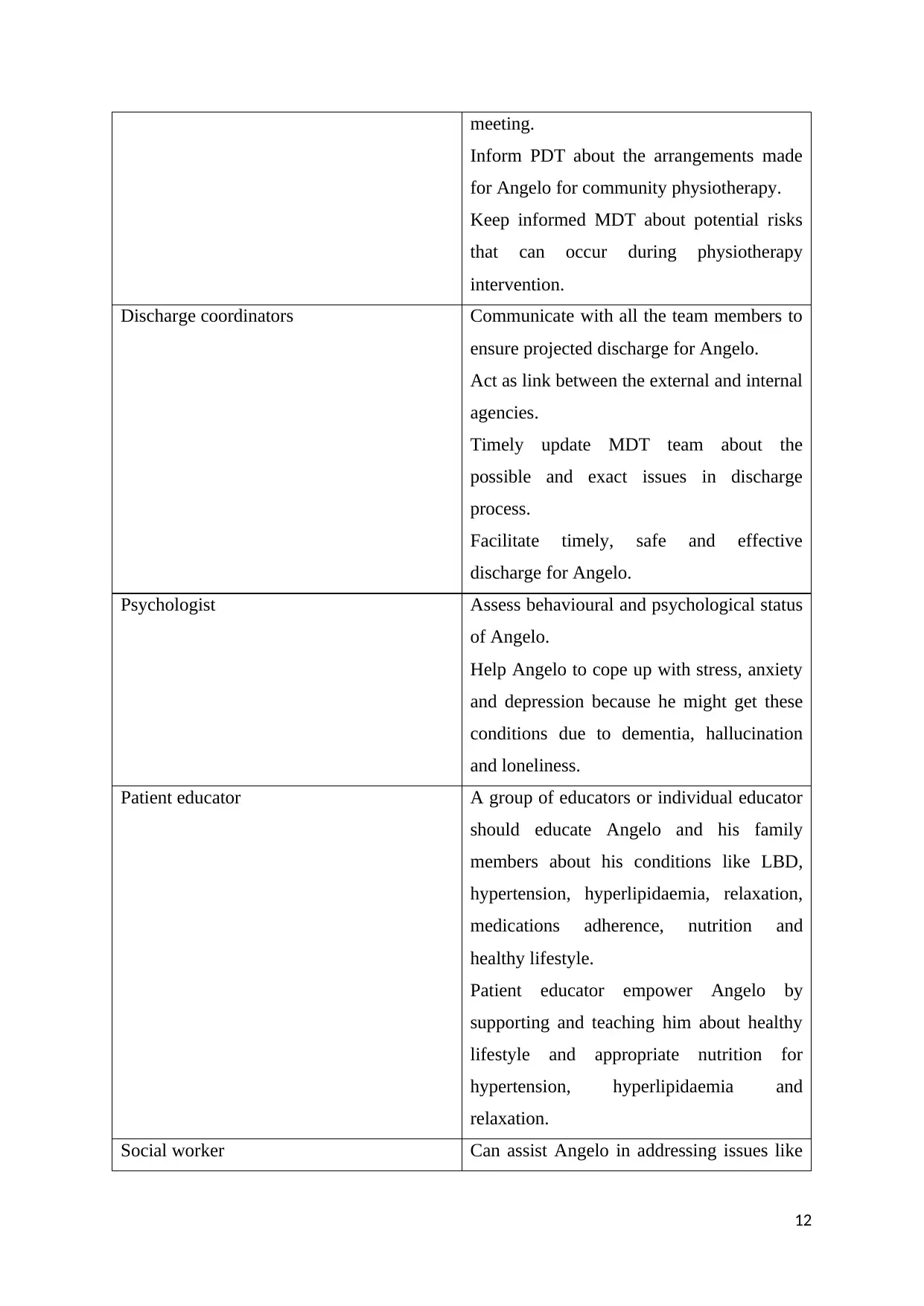
meeting.
Inform PDT about the arrangements made
for Angelo for community physiotherapy.
Keep informed MDT about potential risks
that can occur during physiotherapy
intervention.
Discharge coordinators Communicate with all the team members to
ensure projected discharge for Angelo.
Act as link between the external and internal
agencies.
Timely update MDT team about the
possible and exact issues in discharge
process.
Facilitate timely, safe and effective
discharge for Angelo.
Psychologist Assess behavioural and psychological status
of Angelo.
Help Angelo to cope up with stress, anxiety
and depression because he might get these
conditions due to dementia, hallucination
and loneliness.
Patient educator A group of educators or individual educator
should educate Angelo and his family
members about his conditions like LBD,
hypertension, hyperlipidaemia, relaxation,
medications adherence, nutrition and
healthy lifestyle.
Patient educator empower Angelo by
supporting and teaching him about healthy
lifestyle and appropriate nutrition for
hypertension, hyperlipidaemia and
relaxation.
Social worker Can assist Angelo in addressing issues like
12
Inform PDT about the arrangements made
for Angelo for community physiotherapy.
Keep informed MDT about potential risks
that can occur during physiotherapy
intervention.
Discharge coordinators Communicate with all the team members to
ensure projected discharge for Angelo.
Act as link between the external and internal
agencies.
Timely update MDT team about the
possible and exact issues in discharge
process.
Facilitate timely, safe and effective
discharge for Angelo.
Psychologist Assess behavioural and psychological status
of Angelo.
Help Angelo to cope up with stress, anxiety
and depression because he might get these
conditions due to dementia, hallucination
and loneliness.
Patient educator A group of educators or individual educator
should educate Angelo and his family
members about his conditions like LBD,
hypertension, hyperlipidaemia, relaxation,
medications adherence, nutrition and
healthy lifestyle.
Patient educator empower Angelo by
supporting and teaching him about healthy
lifestyle and appropriate nutrition for
hypertension, hyperlipidaemia and
relaxation.
Social worker Can assist Angelo in addressing issues like
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





