NUR4111: iSAP Framework Application: Annie's Safe Community Transition
VerifiedAdded on 2022/09/18
|8
|1904
|17
Homework Assignment
AI Summary
This assignment delves into a case study of Annie, a 69-year-old Indigenous woman with diabetes, hypertension, and chronic kidney problems, who requires a safe transition from acute care to the community. The assignment begins by defining discharge planning and discussing its importance in Annie's context, emphasizing its role in reducing hospital readmissions and ensuring medication adherence. It then identifies and discusses four key barriers to effective discharge planning, including communication gaps, lack of role clarity, resource limitations, and ineffective planning. The assignment outlines the key steps for planning and implementing safe transfer of care, emphasizing early risk assessment, individualized care plans, and the importance of communication with patients and their families. A concept map is constructed to illustrate a strengths-based, person-centered care plan. Finally, the assignment provides an evidence-based practice (EBP) rationale for the principles of cultural safety, health literacy, self-management, and access to services, drawing on the National Aboriginal and Torres Strait Islander Health Plan (2013–2023) and the National Strategic Framework for Chronic Conditions (2017) to support Annie's safe transition to community care.

Running Head: NURSING
NURSING
Student’s Name
Institutional Affiliation
Date
NURSING
Student’s Name
Institutional Affiliation
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
1. Define ‘discharge planning’ and discuss the importance of discharge planning and care
transition in relation to Annie’s needs. (approx. 100 words)
Discharge planning refers to the development of personal discharge plan proceeding to leaving
hospital to continue giving care to a patient (Shepperd, Lannin, Clemson, McCluskey, Cameron &
Barras, 2013). The importance of discharge planning to Annie who is diabetic ,has hypertension
and chronic kidney problems includes; it helps to lower down the readmission back to the hospital,
it helps Annie to recover from diabetes and kidney disease. The other importance is that it will help
her to ensure that there is a proper medication that adhered to and taken in appropriate doses for
quick recovery from diabetes hypertension and chronic kidney disease.
2. Discuss four known barriers to effective discharge planning in acute care services. (approx.
225 words)
Communication
Based on Hesselink, Zegers, Vernooij-Dassen, Barach, Kalkman, Flink & Suñol
(2014)Communication is one factor that's highly identified that influences the effective
discharge process. There is a communication gap found in the members. The concerned
team don't at many times inform the associated health services of the discharge plans.
Patients may sometimes be being ready medically for discharge but not in terms of
rehabilitation view. The concerned teams don't communicate the importance for patient
knowhow, for example, pharmacy education, anticoagulation clinics and nurse educator.
Lack of role clarity
Lack of clarity is another problem, and the people involved always suggest that it is
essential to have all the concerned parties to be engaged during discharge planning as
well as making precise clarified tasks (Wong, Yam, Cheung, Leung, Chan, Wong & Yeoh,
2011). It is not also clear as to who has the mandate to review the discharge plans, follow-
2
1. Define ‘discharge planning’ and discuss the importance of discharge planning and care
transition in relation to Annie’s needs. (approx. 100 words)
Discharge planning refers to the development of personal discharge plan proceeding to leaving
hospital to continue giving care to a patient (Shepperd, Lannin, Clemson, McCluskey, Cameron &
Barras, 2013). The importance of discharge planning to Annie who is diabetic ,has hypertension
and chronic kidney problems includes; it helps to lower down the readmission back to the hospital,
it helps Annie to recover from diabetes and kidney disease. The other importance is that it will help
her to ensure that there is a proper medication that adhered to and taken in appropriate doses for
quick recovery from diabetes hypertension and chronic kidney disease.
2. Discuss four known barriers to effective discharge planning in acute care services. (approx.
225 words)
Communication
Based on Hesselink, Zegers, Vernooij-Dassen, Barach, Kalkman, Flink & Suñol
(2014)Communication is one factor that's highly identified that influences the effective
discharge process. There is a communication gap found in the members. The concerned
team don't at many times inform the associated health services of the discharge plans.
Patients may sometimes be being ready medically for discharge but not in terms of
rehabilitation view. The concerned teams don't communicate the importance for patient
knowhow, for example, pharmacy education, anticoagulation clinics and nurse educator.
Lack of role clarity
Lack of clarity is another problem, and the people involved always suggest that it is
essential to have all the concerned parties to be engaged during discharge planning as
well as making precise clarified tasks (Wong, Yam, Cheung, Leung, Chan, Wong & Yeoh,
2011). It is not also clear as to who has the mandate to review the discharge plans, follow-
2
NURSING
up appointments, medications and the person involved to write the discharge summary.
Lack of resources
According to Okoniewska, Santana, Groshaus, Stajkovic, Cowles, Chakrovorty, & Ghali
(2015) lack of resources is a vital issue concerning achieving an effective discharge plan.
Most of the members are thought not only to lack resources allocated to acute care but
also the community care as limiting enough follow-up care. Sometimes the problem is
excellent outside the hospital than inside the hospital.
Ineffective planning
These can lead to delayed discharge which results to accumulation in hospitals. This
causes overcrowding of patients since the beds are minimal.
3. Summarise in your own words and in dot point format the key steps
for planning and implementing safe transfer of care as outlined in Transfer of care from acute
inpatient services (2014). (approx. 225 words)
According to McKenna, Furness, Dhital, Ennis, Houghton, Lupson & Toomey
(2014)
Any preparation for the transfer of care is to start before admission planned and
immediately, the patients must undergo discharge risk assessment in twenty-four
hours of access.
A known date in which the transfer is done should be known earlier or soon as
possible after acute patients are admitted to make sure there are predictability and
accuracy. The individual patients must have their discharge plan or the transfer
care plan.
The duty of implementing and coordinating patients discharge is supposed to be
3
up appointments, medications and the person involved to write the discharge summary.
Lack of resources
According to Okoniewska, Santana, Groshaus, Stajkovic, Cowles, Chakrovorty, & Ghali
(2015) lack of resources is a vital issue concerning achieving an effective discharge plan.
Most of the members are thought not only to lack resources allocated to acute care but
also the community care as limiting enough follow-up care. Sometimes the problem is
excellent outside the hospital than inside the hospital.
Ineffective planning
These can lead to delayed discharge which results to accumulation in hospitals. This
causes overcrowding of patients since the beds are minimal.
3. Summarise in your own words and in dot point format the key steps
for planning and implementing safe transfer of care as outlined in Transfer of care from acute
inpatient services (2014). (approx. 225 words)
According to McKenna, Furness, Dhital, Ennis, Houghton, Lupson & Toomey
(2014)
Any preparation for the transfer of care is to start before admission planned and
immediately, the patients must undergo discharge risk assessment in twenty-four
hours of access.
A known date in which the transfer is done should be known earlier or soon as
possible after acute patients are admitted to make sure there are predictability and
accuracy. The individual patients must have their discharge plan or the transfer
care plan.
The duty of implementing and coordinating patients discharge is supposed to be
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING
done by a specified team or person.
The group that is responsible for coordinating patient discharge or the transfer
case should liaise with the individual patient and the caretakers to make them
ready for the release.
The handover of the care plan is supposed to be advanced and implemented when
there is a consultation with two parties or people that must be involved, and they
include the patient, cares or the family members. Families or the caretakers must
understand every phase of transfer of care plan.
Any transfer of case summary must be started immediately, and development
must be done throughout the patient admission
A transfer of care specification is supposed to be completed for all patients
proceeding to discharge or transfer of care. Transfer of patient details must
conform with the principles of privacy as dictated by health records act 2001 and in
the information privacy act of the year 2000
Those patients with a higher risk of being admitted should be known and plan to
reduce the chances of implementation of readmission.
When transferring patients from one medical care to another, Victorian quality
council inter hospital transfer patient form must be used.
The community services are supposed to be made when there is the completion of
risk assessment or the patient to be referred to appropriate healthcare.
When the patient is discharged, it is vital to engage the so-called community
support services.
There must be the permanence of medication supervision must be well maintained
and approve done to the patient transfer of care.
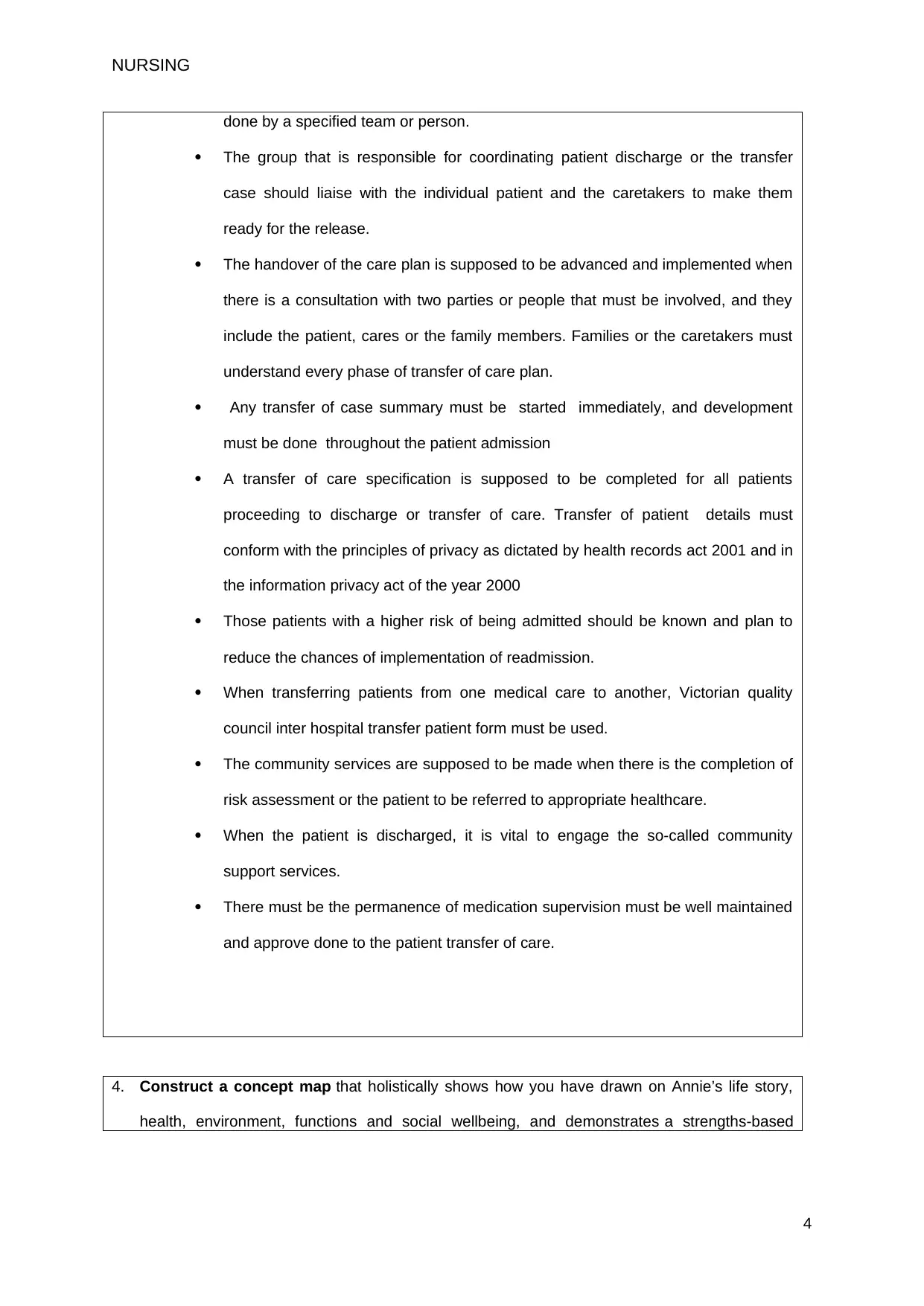
4. Construct a concept map that holistically shows how you have drawn on Annie’s life story,
health, environment, functions and social wellbeing, and demonstrates a strengths-based
4
done by a specified team or person.
The group that is responsible for coordinating patient discharge or the transfer
case should liaise with the individual patient and the caretakers to make them
ready for the release.
The handover of the care plan is supposed to be advanced and implemented when
there is a consultation with two parties or people that must be involved, and they
include the patient, cares or the family members. Families or the caretakers must
understand every phase of transfer of care plan.
Any transfer of case summary must be started immediately, and development
must be done throughout the patient admission
A transfer of care specification is supposed to be completed for all patients
proceeding to discharge or transfer of care. Transfer of patient details must
conform with the principles of privacy as dictated by health records act 2001 and in
the information privacy act of the year 2000
Those patients with a higher risk of being admitted should be known and plan to
reduce the chances of implementation of readmission.
When transferring patients from one medical care to another, Victorian quality
council inter hospital transfer patient form must be used.
The community services are supposed to be made when there is the completion of
risk assessment or the patient to be referred to appropriate healthcare.
When the patient is discharged, it is vital to engage the so-called community
support services.
There must be the permanence of medication supervision must be well maintained
and approve done to the patient transfer of care.
4. Construct a concept map that holistically shows how you have drawn on Annie’s life story,
health, environment, functions and social wellbeing, and demonstrates a strengths-based
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
person-centred care plan to improving her situation. (approx. 125 words)
5. Provide an EBP rationale for the following PHC principles for Annie’s safe transition to
community care. The rationale should include strategies from the National Aboriginal and
Torres Strait Islander Health Plan (2013–2023) and the National Strategic Framework for
Chronic Conditions, 2017. (approx. total 450 words (approx. 158 words for each PHC principle)
o cultural safety
o health literacy and self-management (for practical reasons these two principles
have been combined)
o access to services
CULTURAL SAFETY
From Department of Health (2015) Cultural safety aims at addressing the inequality of
power distribution in health services. Providing a community with a conducive environment
to share their concerns on cultural practices helps in identifying areas of improving
services. Culture influences a person's decisions on when and why they should seek health
5
person-centred care plan to improving her situation. (approx. 125 words)
5. Provide an EBP rationale for the following PHC principles for Annie’s safe transition to
community care. The rationale should include strategies from the National Aboriginal and
Torres Strait Islander Health Plan (2013–2023) and the National Strategic Framework for
Chronic Conditions, 2017. (approx. total 450 words (approx. 158 words for each PHC principle)
o cultural safety
o health literacy and self-management (for practical reasons these two principles
have been combined)
o access to services
CULTURAL SAFETY
From Department of Health (2015) Cultural safety aims at addressing the inequality of
power distribution in health services. Providing a community with a conducive environment
to share their concerns on cultural practices helps in identifying areas of improving
services. Culture influences a person's decisions on when and why they should seek health
5
NURSING
services, accept treatments, adhere to treatment and follow up and successful prevention
and health promotional strategies (Department of Health, 2015). Since Annie is so
passionate about the aboriginal community, she influenced by their culture and decided to
the local hospital. To ensure culturally safe and appropriate services: people provided must
communicate in respect and create good relationships, be flexible to meet local wants and
health workforce should be increased. The community leaders should advocate for
sustainable and quality culture safety to address chronic conditions. Health care education
is needed to improve the social capability of health care workers.
HEALTH LITERACY AND SELF MANAGEMENT
Health literacy is a point at which specific individuals can process, obtain and understand
essential health services and information required to make significant health decisions
(Australian Health Ministers' Advisory Council, 2017). Self-management is the ability of a
person to take responsibilities of his or her wellbeing and behaviour. Health literacy is
essential as it affects and empowers a person's capacity to make the best decisions about
their health care and health and take the best actions. Self-management is the central part
of ideal care for the chronic case because the patient can set appropriate goals to their
social and health needs. The patients can discuss treatment preferences and set the
individual quality of life purposes. Annie had no information on how to manage diabetes on
her own and was always supported by local aboriginal health service. People should have
relevant and sufficient information about their conditions and how to manage it.
ACCESS TO SERVICES
Accessible services are those that are affordable, appropriate, acceptable and physically
available (Australian Health Ministers' Advisory Council, 2017). Access is limited by
economic and physical barriers and lack of knowledge of how, where to get health
services. Patients with chronic conditions need the right care from the right team and the
right place and time. Accessible health services allow culturally safe, appropriate and
quality care that meets the needs of the patients. Access also improves a person's health
literacy and helps individuals navigate health systems. Annie, who has diabetes and
chronic kidney disease, is indigenous and was not familiar with hospitals. She lacked
6
services, accept treatments, adhere to treatment and follow up and successful prevention
and health promotional strategies (Department of Health, 2015). Since Annie is so
passionate about the aboriginal community, she influenced by their culture and decided to
the local hospital. To ensure culturally safe and appropriate services: people provided must
communicate in respect and create good relationships, be flexible to meet local wants and
health workforce should be increased. The community leaders should advocate for
sustainable and quality culture safety to address chronic conditions. Health care education
is needed to improve the social capability of health care workers.
HEALTH LITERACY AND SELF MANAGEMENT
Health literacy is a point at which specific individuals can process, obtain and understand
essential health services and information required to make significant health decisions
(Australian Health Ministers' Advisory Council, 2017). Self-management is the ability of a
person to take responsibilities of his or her wellbeing and behaviour. Health literacy is
essential as it affects and empowers a person's capacity to make the best decisions about
their health care and health and take the best actions. Self-management is the central part
of ideal care for the chronic case because the patient can set appropriate goals to their
social and health needs. The patients can discuss treatment preferences and set the
individual quality of life purposes. Annie had no information on how to manage diabetes on
her own and was always supported by local aboriginal health service. People should have
relevant and sufficient information about their conditions and how to manage it.
ACCESS TO SERVICES
Accessible services are those that are affordable, appropriate, acceptable and physically
available (Australian Health Ministers' Advisory Council, 2017). Access is limited by
economic and physical barriers and lack of knowledge of how, where to get health
services. Patients with chronic conditions need the right care from the right team and the
right place and time. Accessible health services allow culturally safe, appropriate and
quality care that meets the needs of the patients. Access also improves a person's health
literacy and helps individuals navigate health systems. Annie, who has diabetes and
chronic kidney disease, is indigenous and was not familiar with hospitals. She lacked
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING
knowledge about how and where to get excellent health services. The national framework
suggests that information on how to access healthcare services is provided and available
in time to all people, even those in remote areas. The technology is used to broaden
access to health services which are digital health options and telehealth.
References
Aberdeen, S. (2015). Concept mapping: a tool for improving patient care. Nursing Standard
(2014+), 29(48), 49.
Department of Health. (2015). Implementation plan for the national aboriginal and torres
strait islander health plan 2013–2023. Commonwealth of Australia.
Australian Health Ministers' Advisory Council. (2017). National strategic framework for
chronic conditions.
McKenna, B., Furness, T., Dhital, D., Ennis, G., Houghton, J., Lupson, C., & Toomey, N.
(2014). Recovery-oriented care in acute inpatient mental health settings: An
exploratory study. Issues in Mental Health Nursing, 35(7), 526-532.
Okoniewska, B., Santana, M. J., Groshaus, H., Stajkovic, S., Cowles, J., Chakrovorty, D., &
Ghali, W. A. (2015). Barriers to discharge in an acute care medical teaching unit: a
qualitative analysis of health providers’ perceptions. Journal of multidisciplinary
healthcare, 8, 83.
Wong, E. L., Yam, C. H., Cheung, A. W., Leung, M. C., Chan, F. W., Wong, F. Y., & Yeoh,
E. K. (2011). Barriers to effective discharge planning: a qualitative study
investigating the perspectives of frontline healthcare professionals. BMC health
services research, 11(1), 242.
7
knowledge about how and where to get excellent health services. The national framework
suggests that information on how to access healthcare services is provided and available
in time to all people, even those in remote areas. The technology is used to broaden
access to health services which are digital health options and telehealth.
References
Aberdeen, S. (2015). Concept mapping: a tool for improving patient care. Nursing Standard
(2014+), 29(48), 49.
Department of Health. (2015). Implementation plan for the national aboriginal and torres
strait islander health plan 2013–2023. Commonwealth of Australia.
Australian Health Ministers' Advisory Council. (2017). National strategic framework for
chronic conditions.
McKenna, B., Furness, T., Dhital, D., Ennis, G., Houghton, J., Lupson, C., & Toomey, N.
(2014). Recovery-oriented care in acute inpatient mental health settings: An
exploratory study. Issues in Mental Health Nursing, 35(7), 526-532.
Okoniewska, B., Santana, M. J., Groshaus, H., Stajkovic, S., Cowles, J., Chakrovorty, D., &
Ghali, W. A. (2015). Barriers to discharge in an acute care medical teaching unit: a
qualitative analysis of health providers’ perceptions. Journal of multidisciplinary
healthcare, 8, 83.
Wong, E. L., Yam, C. H., Cheung, A. W., Leung, M. C., Chan, F. W., Wong, F. Y., & Yeoh,
E. K. (2011). Barriers to effective discharge planning: a qualitative study
investigating the perspectives of frontline healthcare professionals. BMC health
services research, 11(1), 242.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

NURSING
Hesselink, G., Zegers, M., Vernooij-Dassen, M., Barach, P., Kalkman, C., Flink, M., ... &
Suñol, R. (2014). Improving patient discharge and reducing hospital readmissions
by using Intervention Mapping. BMC health services research, 14(1), 389.
Shepperd, S., Lannin, N. A., Clemson, L. M., McCluskey, A., Cameron, I. D., & Barras, S. L.
(2013). Discharge planning from hospital to home. Cochrane database of
systematic reviews, (1).
8
Hesselink, G., Zegers, M., Vernooij-Dassen, M., Barach, P., Kalkman, C., Flink, M., ... &
Suñol, R. (2014). Improving patient discharge and reducing hospital readmissions
by using Intervention Mapping. BMC health services research, 14(1), 389.
Shepperd, S., Lannin, N. A., Clemson, L. M., McCluskey, A., Cameron, I. D., & Barras, S. L.
(2013). Discharge planning from hospital to home. Cochrane database of
systematic reviews, (1).
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




