Detailed Analysis: Assessing Consciousness and Brain Function
VerifiedAdded on 2020/06/06
|10
|3834
|121
Report
AI Summary
This report provides a comprehensive overview of brain structure and function, covering the cerebrum, cerebellum, and brainstem components, including the twelve cranial nerves. It details the assessment process using the Glasgow Coma Scale (GCS), explaining its application, scoring, and significance in evaluating levels of consciousness. The report also addresses factors affecting consciousness, such as cerebral hemorrhage, liver disease, and brain tumors, alongside common disorders like acute bronchitis, and their management. Furthermore, it explores techniques for assessing eye movement, verbal response, and motor responses, emphasizing correct terminology and the prevention of complications. The report also discusses the crushing triad and signs of raised intracranial pressure, offering insights into nursing care and the importance of assessing respiratory rate, rhythm, depth, and other physiological parameters. The report concludes by highlighting the importance of monitoring the patient's mental status and provides a detailed understanding of various neurological conditions and their management.
Theory Make Up Time Sheet
1. Learning outcomes for the session Discuss the structure and function of the brain
Conduct an assessment using the Glasgow coma scale
Use the correct technique to assess eye movement, verbal response and motor responses Understand the significance of findings Identify the factors affecting conscious levels Know the correct terminology related to assessment and common disorders affecting level of
consciousness
Demonstrate knowledge and understanding of the principles of caring for someone who is unconscious
Write a care plan for a patient who is unconscious Identify clinical situations where the use of GCS is an appropriate means of assessment
2. Learning resources used to enable make up of study time missed
(please give full reference listing of evidence using “Cite them right”- for example, websites, journals, books used inclusive of
chapters and page numbers read) Discuss the structure and function of the brain
Cerebrum: It is the largest part of human brain. It is divided into four sections which are the frontal lobe,
parietal lobe, occipital lobe, and temporal lobe. It is associated with higher brain function such as thought and
action.
Cerebellum: The structure is associated with regulation and coordination of movement, posture, and balance.
The function is to receive information and coordinates voluntary movements (Geraghty. 2005).
Medulla oblongata: It is situated in the brain stem in front of cerebellum. It helps in regulate breathing,
digestion, sneezing, blood vessel function and swallowing.
Pons varolii: It is a portion of brain stem and is located above the Medulla oblongata. The function is to
connect lower and upper parts of brain.
Frontal lobe: The frontal lobe, the largest of the cerebral lobes, lies rostral to the central sulcus. Its function is
reasoning, planning, parts of speech, movement, emotions, and problem solving.
Hypothalamus: It is an integral part of the brain. The main function is to link the nervous system to the
endocrine system via the pituitary gland
Corpus callosum: It is located near the center of the brain. , this structure is the largest bundle of nerve fibers
that connects the left and right cerebral hemispheres, much like a bridge.
Thalamus: It is located above the brain stem between the cerebral cortex and the midbrain and has extensive
nerve connections to both.
1. Learning outcomes for the session Discuss the structure and function of the brain
Conduct an assessment using the Glasgow coma scale
Use the correct technique to assess eye movement, verbal response and motor responses Understand the significance of findings Identify the factors affecting conscious levels Know the correct terminology related to assessment and common disorders affecting level of
consciousness
Demonstrate knowledge and understanding of the principles of caring for someone who is unconscious
Write a care plan for a patient who is unconscious Identify clinical situations where the use of GCS is an appropriate means of assessment
2. Learning resources used to enable make up of study time missed
(please give full reference listing of evidence using “Cite them right”- for example, websites, journals, books used inclusive of
chapters and page numbers read) Discuss the structure and function of the brain
Cerebrum: It is the largest part of human brain. It is divided into four sections which are the frontal lobe,
parietal lobe, occipital lobe, and temporal lobe. It is associated with higher brain function such as thought and
action.
Cerebellum: The structure is associated with regulation and coordination of movement, posture, and balance.
The function is to receive information and coordinates voluntary movements (Geraghty. 2005).
Medulla oblongata: It is situated in the brain stem in front of cerebellum. It helps in regulate breathing,
digestion, sneezing, blood vessel function and swallowing.
Pons varolii: It is a portion of brain stem and is located above the Medulla oblongata. The function is to
connect lower and upper parts of brain.
Frontal lobe: The frontal lobe, the largest of the cerebral lobes, lies rostral to the central sulcus. Its function is
reasoning, planning, parts of speech, movement, emotions, and problem solving.
Hypothalamus: It is an integral part of the brain. The main function is to link the nervous system to the
endocrine system via the pituitary gland
Corpus callosum: It is located near the center of the brain. , this structure is the largest bundle of nerve fibers
that connects the left and right cerebral hemispheres, much like a bridge.
Thalamus: It is located above the brain stem between the cerebral cortex and the midbrain and has extensive
nerve connections to both.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Theory Make Up Time Sheet
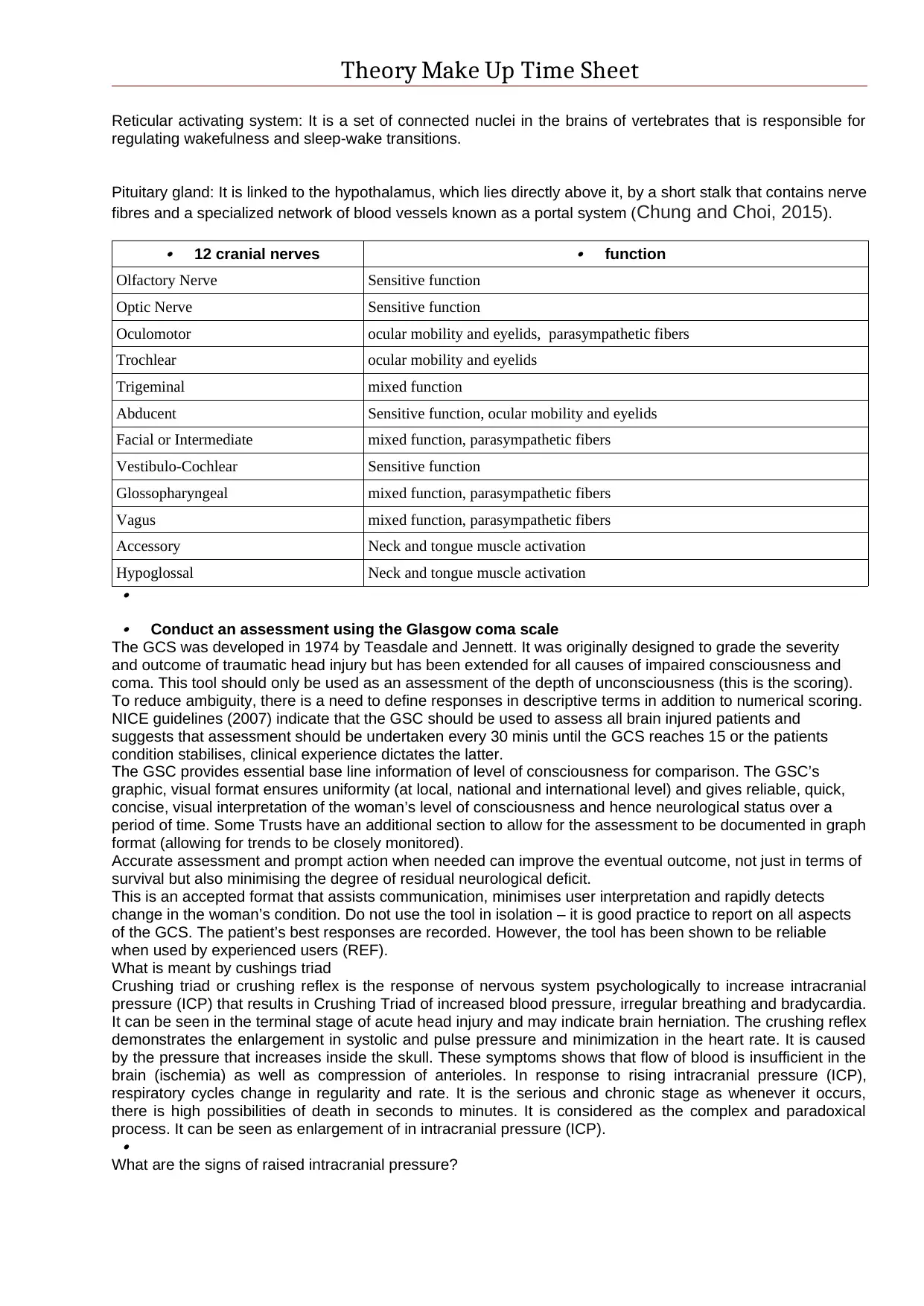
Reticular activating system: It is a set of connected nuclei in the brains of vertebrates that is responsible for
regulating wakefulness and sleep-wake transitions.
Pituitary gland: It is linked to the hypothalamus, which lies directly above it, by a short stalk that contains nerve
fibres and a specialized network of blood vessels known as a portal system (Chung and Choi, 2015). 12 cranial nerves
function
Olfactory Nerve Sensitive function
Optic Nerve Sensitive function
Oculomotor ocular mobility and eyelids, parasympathetic fibers
Trochlear ocular mobility and eyelids
Trigeminal mixed function
Abducent Sensitive function, ocular mobility and eyelids
Facial or Intermediate mixed function, parasympathetic fibers
Vestibulo-Cochlear Sensitive function
Glossopharyngeal mixed function, parasympathetic fibers
Vagus mixed function, parasympathetic fibers
Accessory Neck and tongue muscle activation
Hypoglossal Neck and tongue muscle activation
Conduct an assessment using the Glasgow coma scale
The GCS was developed in 1974 by Teasdale and Jennett. It was originally designed to grade the severity
and outcome of traumatic head injury but has been extended for all causes of impaired consciousness and
coma. This tool should only be used as an assessment of the depth of unconsciousness (this is the scoring).
To reduce ambiguity, there is a need to define responses in descriptive terms in addition to numerical scoring.
NICE guidelines (2007) indicate that the GSC should be used to assess all brain injured patients and
suggests that assessment should be undertaken every 30 minis until the GCS reaches 15 or the patients
condition stabilises, clinical experience dictates the latter.
The GSC provides essential base line information of level of consciousness for comparison. The GSC’s
graphic, visual format ensures uniformity (at local, national and international level) and gives reliable, quick,
concise, visual interpretation of the woman’s level of consciousness and hence neurological status over a
period of time. Some Trusts have an additional section to allow for the assessment to be documented in graph
format (allowing for trends to be closely monitored).
Accurate assessment and prompt action when needed can improve the eventual outcome, not just in terms of
survival but also minimising the degree of residual neurological deficit.
This is an accepted format that assists communication, minimises user interpretation and rapidly detects
change in the woman’s condition. Do not use the tool in isolation – it is good practice to report on all aspects
of the GCS. The patient’s best responses are recorded. However, the tool has been shown to be reliable
when used by experienced users (REF).
What is meant by cushings triad
Crushing triad or crushing reflex is the response of nervous system psychologically to increase intracranial
pressure (ICP) that results in Crushing Triad of increased blood pressure, irregular breathing and bradycardia.
It can be seen in the terminal stage of acute head injury and may indicate brain herniation. The crushing reflex
demonstrates the enlargement in systolic and pulse pressure and minimization in the heart rate. It is caused
by the pressure that increases inside the skull. These symptoms shows that flow of blood is insufficient in the
brain (ischemia) as well as compression of anterioles. In response to rising intracranial pressure (ICP),
respiratory cycles change in regularity and rate. It is the serious and chronic stage as whenever it occurs,
there is high possibilities of death in seconds to minutes. It is considered as the complex and paradoxical
process. It can be seen as enlargement of in intracranial pressure (ICP).
What are the signs of raised intracranial pressure?
Reticular activating system: It is a set of connected nuclei in the brains of vertebrates that is responsible for
regulating wakefulness and sleep-wake transitions.
Pituitary gland: It is linked to the hypothalamus, which lies directly above it, by a short stalk that contains nerve
fibres and a specialized network of blood vessels known as a portal system (Chung and Choi, 2015). 12 cranial nerves
function
Olfactory Nerve Sensitive function
Optic Nerve Sensitive function
Oculomotor ocular mobility and eyelids, parasympathetic fibers
Trochlear ocular mobility and eyelids
Trigeminal mixed function
Abducent Sensitive function, ocular mobility and eyelids
Facial or Intermediate mixed function, parasympathetic fibers
Vestibulo-Cochlear Sensitive function
Glossopharyngeal mixed function, parasympathetic fibers
Vagus mixed function, parasympathetic fibers
Accessory Neck and tongue muscle activation
Hypoglossal Neck and tongue muscle activation
Conduct an assessment using the Glasgow coma scale
The GCS was developed in 1974 by Teasdale and Jennett. It was originally designed to grade the severity
and outcome of traumatic head injury but has been extended for all causes of impaired consciousness and
coma. This tool should only be used as an assessment of the depth of unconsciousness (this is the scoring).
To reduce ambiguity, there is a need to define responses in descriptive terms in addition to numerical scoring.
NICE guidelines (2007) indicate that the GSC should be used to assess all brain injured patients and
suggests that assessment should be undertaken every 30 minis until the GCS reaches 15 or the patients
condition stabilises, clinical experience dictates the latter.
The GSC provides essential base line information of level of consciousness for comparison. The GSC’s
graphic, visual format ensures uniformity (at local, national and international level) and gives reliable, quick,
concise, visual interpretation of the woman’s level of consciousness and hence neurological status over a
period of time. Some Trusts have an additional section to allow for the assessment to be documented in graph
format (allowing for trends to be closely monitored).
Accurate assessment and prompt action when needed can improve the eventual outcome, not just in terms of
survival but also minimising the degree of residual neurological deficit.
This is an accepted format that assists communication, minimises user interpretation and rapidly detects
change in the woman’s condition. Do not use the tool in isolation – it is good practice to report on all aspects
of the GCS. The patient’s best responses are recorded. However, the tool has been shown to be reliable
when used by experienced users (REF).
What is meant by cushings triad
Crushing triad or crushing reflex is the response of nervous system psychologically to increase intracranial
pressure (ICP) that results in Crushing Triad of increased blood pressure, irregular breathing and bradycardia.
It can be seen in the terminal stage of acute head injury and may indicate brain herniation. The crushing reflex
demonstrates the enlargement in systolic and pulse pressure and minimization in the heart rate. It is caused
by the pressure that increases inside the skull. These symptoms shows that flow of blood is insufficient in the
brain (ischemia) as well as compression of anterioles. In response to rising intracranial pressure (ICP),
respiratory cycles change in regularity and rate. It is the serious and chronic stage as whenever it occurs,
there is high possibilities of death in seconds to minutes. It is considered as the complex and paradoxical
process. It can be seen as enlargement of in intracranial pressure (ICP).
What are the signs of raised intracranial pressure?
Theory Make Up Time Sheet
Intracranial pressure is the sudden rise in the pressure around the head and brain. There are various signs
that can be observed in an individual regarding the intracranial pressure. One can be suffered from severe
headaches frequently. Nausea and vomiting are the two other signs that can be observed in an individual. The
blood pressure is increased and it impacts negatively on the health of human being, Further, an individual
remains confused about time location and people. Double vision can be observed and pupils doesn't respond
to the change in light. Shallow breathing, seizures, loss of consciousness and coma are other signs and
symptoms of intracranial pressure. These signs could show other chronic situations other than increased
intracranial pressure such as brain tumor, stroke and head injury. Constant enlargement in intracranial
pressure is considered as life threatening and it requires emergency medical help. Identify the factors affecting conscious levels cerebral haemorrhage : a very basic cause of it is the brain trauma in which the brain is affected to a
much level. So, it causes unconsciousness.
liver disease : There is a decline in brain function because of which the hepatic encephalopathy occurs
which further causes liver diseases.
brain tumor : The cells of the brain have been damaged because of which brain tumor
uremia, or end-stage kidney failure.
heart disease : As heart is directly connected to the brain, so there are chances of it getting
unconscious.
dementia, such as Alzheimer's disease : As in case of dementia, the person starts losing the level of
understanding and concentrating because it directly affects the brain. So, the proper process of sending
and receiving messages does not take place well, so it affects on the consciousness of the person.
Use the correct technique to assess eye movement, verbal response and motor responses
Best eye response
This assesses the functioning of the brainstem and reticular activating system (RAS) and is not
always an indication of intact neurological functioning e.g. patients with persistent vegetative state will
open their eyes unconsciously. If eyes are open and no blinking is apparent, gently close the eyes
and observe if they open. Voluntary opening of the eyes will determine eye opening and intact brain
stem functioning (Royal Free Hospital Trust 2008).
Best verbal response
Provides information about the patient’s speech, comprehension and functioning areas of the higher,
cognitive centre of the brain. This category reflects the patient’s ability to articulate and express a
reply. And assess whether they are aware of themselves and their environment.
Best motor response
This tests the area of the brain that identifies sensory input and translates this into a motor response.
The intention is to determine the patient’s ability to obey a command to localise, and to withdraw or
assume abnormal body positions, in response to a pain stimulus. A deterioration of one point in the
motor response or an overall two point deterioration in the GCS score should be reported immediately
as this is clinically significant (NICE, 2003).
Know the correct terminology related to assessment and common disorders affecting level of
consciousness
What are the symptoms of acute bronchitis?
The symptoms of acute bronchitis are:
Fever
Wheezing
Chills
Sore Throat
Boday Aches
Chest Congestion
Shortness of breath
Cough
Discuss the management of this condition
In order to manage the acute bronchitis, an individual needs to consume fluids and must avoid taking caffeine
and alcohol. Further, he or she must take plenty of rest. An individual must Take over-the-counter pain
Intracranial pressure is the sudden rise in the pressure around the head and brain. There are various signs
that can be observed in an individual regarding the intracranial pressure. One can be suffered from severe
headaches frequently. Nausea and vomiting are the two other signs that can be observed in an individual. The
blood pressure is increased and it impacts negatively on the health of human being, Further, an individual
remains confused about time location and people. Double vision can be observed and pupils doesn't respond
to the change in light. Shallow breathing, seizures, loss of consciousness and coma are other signs and
symptoms of intracranial pressure. These signs could show other chronic situations other than increased
intracranial pressure such as brain tumor, stroke and head injury. Constant enlargement in intracranial
pressure is considered as life threatening and it requires emergency medical help. Identify the factors affecting conscious levels cerebral haemorrhage : a very basic cause of it is the brain trauma in which the brain is affected to a
much level. So, it causes unconsciousness.
liver disease : There is a decline in brain function because of which the hepatic encephalopathy occurs
which further causes liver diseases.
brain tumor : The cells of the brain have been damaged because of which brain tumor
uremia, or end-stage kidney failure.
heart disease : As heart is directly connected to the brain, so there are chances of it getting
unconscious.
dementia, such as Alzheimer's disease : As in case of dementia, the person starts losing the level of
understanding and concentrating because it directly affects the brain. So, the proper process of sending
and receiving messages does not take place well, so it affects on the consciousness of the person.
Use the correct technique to assess eye movement, verbal response and motor responses
Best eye response
This assesses the functioning of the brainstem and reticular activating system (RAS) and is not
always an indication of intact neurological functioning e.g. patients with persistent vegetative state will
open their eyes unconsciously. If eyes are open and no blinking is apparent, gently close the eyes
and observe if they open. Voluntary opening of the eyes will determine eye opening and intact brain
stem functioning (Royal Free Hospital Trust 2008).
Best verbal response
Provides information about the patient’s speech, comprehension and functioning areas of the higher,
cognitive centre of the brain. This category reflects the patient’s ability to articulate and express a
reply. And assess whether they are aware of themselves and their environment.
Best motor response
This tests the area of the brain that identifies sensory input and translates this into a motor response.
The intention is to determine the patient’s ability to obey a command to localise, and to withdraw or
assume abnormal body positions, in response to a pain stimulus. A deterioration of one point in the
motor response or an overall two point deterioration in the GCS score should be reported immediately
as this is clinically significant (NICE, 2003).
Know the correct terminology related to assessment and common disorders affecting level of
consciousness
What are the symptoms of acute bronchitis?
The symptoms of acute bronchitis are:
Fever
Wheezing
Chills
Sore Throat
Boday Aches
Chest Congestion
Shortness of breath
Cough
Discuss the management of this condition
In order to manage the acute bronchitis, an individual needs to consume fluids and must avoid taking caffeine
and alcohol. Further, he or she must take plenty of rest. An individual must Take over-the-counter pain
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Theory Make Up Time Sheet
relievers to reduce inflammation, ease pain, and lower your fever. Acetaminophen (Tylenol) also helps ease
pain and lower your fever. Taking cough medicines is recommended. Increasing humidity in home or using
humidifier will help in managing this condition effectively and efficeintlly.
How does the nurse help prevent complications from occurring with acute bronchitis?
The nurse will ask the patient about the symptoms and investigate the patient. This usually provides adequate
information to the nurse about the factors causing acute bronchitis. In some cases, the nurse might take a
chest X-ray to ensure that patient doesn't have pneumonia or another lung problem. By using nursing plan the
nurses than prepare and set the apparatus to make patient comfortable and aid in lowering his or her stress
level.
Rate: As in order to assess the efficiency of gas exchange, it is very important for healthcare
professional to seek the changes and transformations in the respiratory rates of patient
(Pasban-Noghabi and Memarian, 2016). By doing this, he or she will get a precise idea
about the respiratory rates. Only air delivered to the terminal bronchioles and alveoli is available
for gas exchange.
Rhythm: Rhythm is the pattern in which an individual breath in each and every situation. In order
to assess the rhythm in gas exchange process, the healthcare professional needs to consider the
pulmonary function, ventilation and carbon dioxide production.
Depth: The depth is assessed in the gas exchange process as it is very important for the
healthcare professionals to seek the information about the density in patient breathing.
Work of breathing: Work of breathing (WOB) is the energy expended to inhale and
exhale a breathing gas. It is assessed in gas exchange process to assess the
respiratory volume and time.
Posture: It is significance to assess the prone posture as it have number of effects on gas
exchange both under normal conditions and in patients with ARDS.
Skin colour: Cutaneous respiration may be the sole method of gas exchange, or may accompany
other forms, such as ventilation. It impacts on the skin and outer integument.
Symmetry of chest movement: Decreased chest expansion resulting from substernal goiter is
Bryson's sign. Symmetric but increased expansion suggests paralysis of the diaphragm with
compensatory intercostal contractions (Fukumoto and et.al., 2016). Asymmetric expansion
suggests pneumonia, a large pleural effusion, rib fracture, or pneumothorax.
Deformities of chest: Chest Wall Deformities. Chest wall deformities, such as kyphoscoliosis,
result in hypoventilation that is caused by a decrease in chest wall compliance from the restriction
of the chest wall due to the abnormal spinal curvature.
Pain: It is important and essential to monitor the pain of patient during gas exchange process. An
anaerobic process can take place in human muscle tissue, producing lactic acid—something so
painful that it feels as though vinegar itself
Mental status: It is significant to assess and check the mental status of the patient. If patient is not
mentally prepared, the process of gas exchange will not become possible.
Cough: It is important for the health care professional to monitor the cough in the patient in gas
exchange process. As it is the chronic disease, it cannot be ignored. Understand the significance of findings
relievers to reduce inflammation, ease pain, and lower your fever. Acetaminophen (Tylenol) also helps ease
pain and lower your fever. Taking cough medicines is recommended. Increasing humidity in home or using
humidifier will help in managing this condition effectively and efficeintlly.
How does the nurse help prevent complications from occurring with acute bronchitis?
The nurse will ask the patient about the symptoms and investigate the patient. This usually provides adequate
information to the nurse about the factors causing acute bronchitis. In some cases, the nurse might take a
chest X-ray to ensure that patient doesn't have pneumonia or another lung problem. By using nursing plan the
nurses than prepare and set the apparatus to make patient comfortable and aid in lowering his or her stress
level.
Rate: As in order to assess the efficiency of gas exchange, it is very important for healthcare
professional to seek the changes and transformations in the respiratory rates of patient
(Pasban-Noghabi and Memarian, 2016). By doing this, he or she will get a precise idea
about the respiratory rates. Only air delivered to the terminal bronchioles and alveoli is available
for gas exchange.
Rhythm: Rhythm is the pattern in which an individual breath in each and every situation. In order
to assess the rhythm in gas exchange process, the healthcare professional needs to consider the
pulmonary function, ventilation and carbon dioxide production.
Depth: The depth is assessed in the gas exchange process as it is very important for the
healthcare professionals to seek the information about the density in patient breathing.
Work of breathing: Work of breathing (WOB) is the energy expended to inhale and
exhale a breathing gas. It is assessed in gas exchange process to assess the
respiratory volume and time.
Posture: It is significance to assess the prone posture as it have number of effects on gas
exchange both under normal conditions and in patients with ARDS.
Skin colour: Cutaneous respiration may be the sole method of gas exchange, or may accompany
other forms, such as ventilation. It impacts on the skin and outer integument.
Symmetry of chest movement: Decreased chest expansion resulting from substernal goiter is
Bryson's sign. Symmetric but increased expansion suggests paralysis of the diaphragm with
compensatory intercostal contractions (Fukumoto and et.al., 2016). Asymmetric expansion
suggests pneumonia, a large pleural effusion, rib fracture, or pneumothorax.
Deformities of chest: Chest Wall Deformities. Chest wall deformities, such as kyphoscoliosis,
result in hypoventilation that is caused by a decrease in chest wall compliance from the restriction
of the chest wall due to the abnormal spinal curvature.
Pain: It is important and essential to monitor the pain of patient during gas exchange process. An
anaerobic process can take place in human muscle tissue, producing lactic acid—something so
painful that it feels as though vinegar itself
Mental status: It is significant to assess and check the mental status of the patient. If patient is not
mentally prepared, the process of gas exchange will not become possible.
Cough: It is important for the health care professional to monitor the cough in the patient in gas
exchange process. As it is the chronic disease, it cannot be ignored. Understand the significance of findings
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
From the findings it can be understood that the structure of brain is divided into several
component and each component has different role and functions. In order to assess
those functions I have analysed the concept diligently. This provides me an idea to how
to deal with problem and generate adequate solutions. There is huge importance for
these findings as this will help me in my future research projects. Furthermore, I have
analysed 12 cranial nerves and assess their functions. These will help me in developing
the understanding of the topic and I will be able to perform better and efficient. I have
conducted an assessment using Glassgow comma scale which was developed by
Teasdale and Jennett. It was originally designed to grade the severity and outcome of
traumatic head injury but has been extended for all causes of impaired consciousness
and coma. This tool should only be used as an assessment of the depth of
unconsciousness (this is the scoring). To reduce ambiguity, there is a need to define
responses in descriptive terms in addition to numerical scoring. Crushing triad or
crushing reflex is the response of nervous system psychologically to increase
intracranial pressure (ICP) that results in Crushing Triad of increased blood pressure,
irregular breathing and bradycardia. It can be seen in the terminal stage of acute head
injury and may indicate brain herniation. The crushing reflex demonstrates the
enlargement in systolic and pulse pressure and minimization in the heart rate. Thus,
from the above research, the outcome I generate is very significant for my future
researches. In this way I will be able to accomplish the aim and objectives of the my
research.
Understanding of principles of caring for someone who is unconscious
One should be efficient enough to understand the way in which the person
should be treated and given care, who is unconscious. There are some factors that
need to eb considered in such cases are patience, supportive nature etc. As when the
person is unconscious, it is obvious enough that they won't be present in their mental
state, so it is better to deal with patience and love because at this state, love, care and
support are only factors that work.
Write a care plan for a patient who is unconscious
Assessment: For the care to be effective, a nurse should perform frequent, systematic and
objective assessment on the comatose client. During the first few hours of coma, neurologic
assessment is to be done as often as every 15 minutes (Shields, 2015).
Physical Assessment: For physical assessment GCS will be used and the scores are described
below:
1. Eye opening
1
component and each component has different role and functions. In order to assess
those functions I have analysed the concept diligently. This provides me an idea to how
to deal with problem and generate adequate solutions. There is huge importance for
these findings as this will help me in my future research projects. Furthermore, I have
analysed 12 cranial nerves and assess their functions. These will help me in developing
the understanding of the topic and I will be able to perform better and efficient. I have
conducted an assessment using Glassgow comma scale which was developed by
Teasdale and Jennett. It was originally designed to grade the severity and outcome of
traumatic head injury but has been extended for all causes of impaired consciousness
and coma. This tool should only be used as an assessment of the depth of
unconsciousness (this is the scoring). To reduce ambiguity, there is a need to define
responses in descriptive terms in addition to numerical scoring. Crushing triad or
crushing reflex is the response of nervous system psychologically to increase
intracranial pressure (ICP) that results in Crushing Triad of increased blood pressure,
irregular breathing and bradycardia. It can be seen in the terminal stage of acute head
injury and may indicate brain herniation. The crushing reflex demonstrates the
enlargement in systolic and pulse pressure and minimization in the heart rate. Thus,
from the above research, the outcome I generate is very significant for my future
researches. In this way I will be able to accomplish the aim and objectives of the my
research.
Understanding of principles of caring for someone who is unconscious
One should be efficient enough to understand the way in which the person
should be treated and given care, who is unconscious. There are some factors that
need to eb considered in such cases are patience, supportive nature etc. As when the
person is unconscious, it is obvious enough that they won't be present in their mental
state, so it is better to deal with patience and love because at this state, love, care and
support are only factors that work.
Write a care plan for a patient who is unconscious
Assessment: For the care to be effective, a nurse should perform frequent, systematic and
objective assessment on the comatose client. During the first few hours of coma, neurologic
assessment is to be done as often as every 15 minutes (Shields, 2015).
Physical Assessment: For physical assessment GCS will be used and the scores are described
below:
1. Eye opening
1
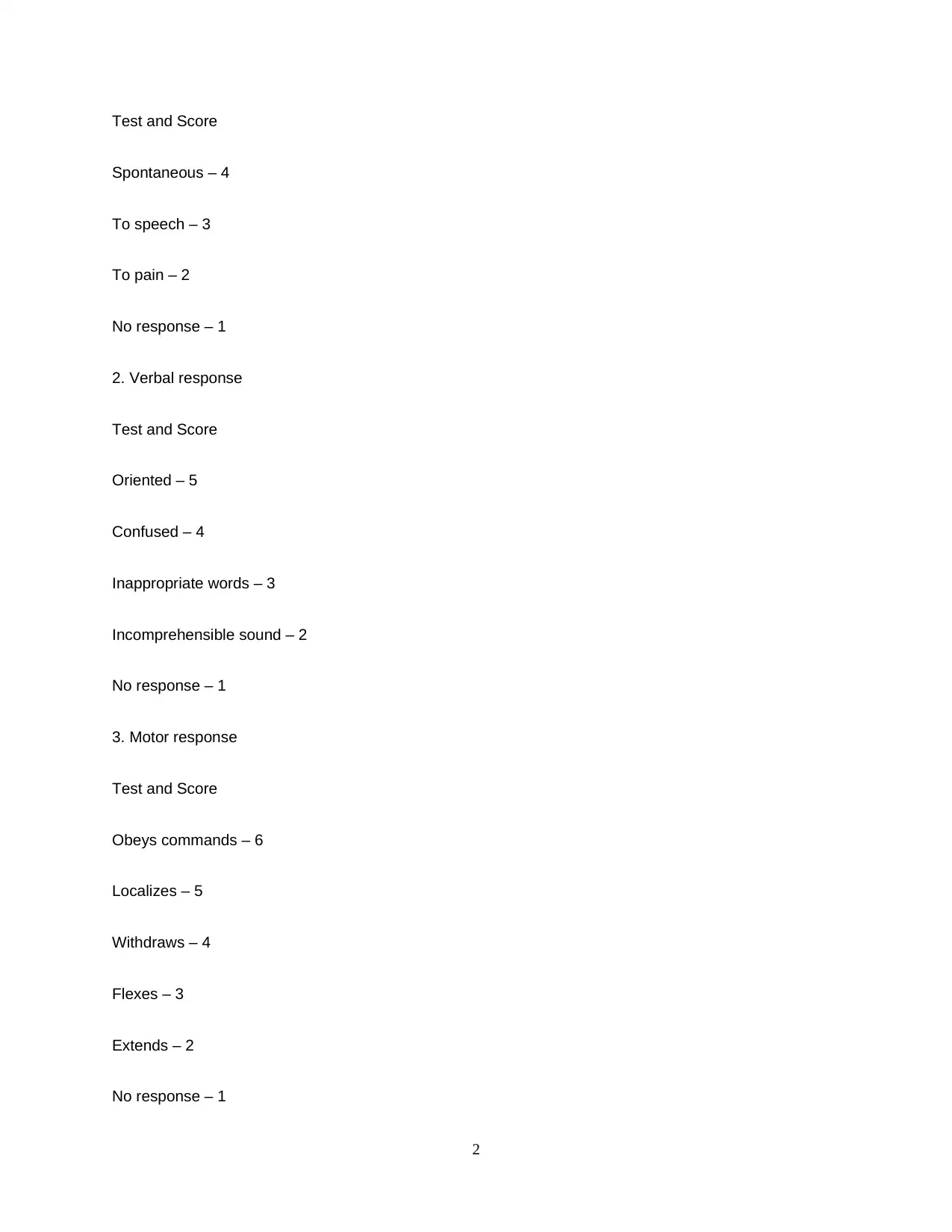
Test and Score
Spontaneous – 4
To speech – 3
To pain – 2
No response – 1
2. Verbal response
Test and Score
Oriented – 5
Confused – 4
Inappropriate words – 3
Incomprehensible sound – 2
No response – 1
3. Motor response
Test and Score
Obeys commands – 6
Localizes – 5
Withdraws – 4
Flexes – 3
Extends – 2
No response – 1
2
Spontaneous – 4
To speech – 3
To pain – 2
No response – 1
2. Verbal response
Test and Score
Oriented – 5
Confused – 4
Inappropriate words – 3
Incomprehensible sound – 2
No response – 1
3. Motor response
Test and Score
Obeys commands – 6
Localizes – 5
Withdraws – 4
Flexes – 3
Extends – 2
No response – 1
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Thus, the client’s response is rated on a scale from 3 to 15. A score of 3 indicates severe neurologic
impairment. A score of 15 indicates that the client is fully responsive (Rys and et.al., 2015). A score
less than 7 require frequent assessment.
Planning: In the planning phase, the nurses will prepare the action plan and schedule at what time the
medication will be given to the patient. Planning is very important and essential for the nurses as it will
help them providing the right guidance.
Interventions: Assess predisposing factors to pain. Monitor vital signs. Conduct diversion activities, offer
other comfort measures. Provide peaceful calm environment.
Rationale: To know the etiology of the unconsciousness. These are usually altered when one in pain
(Wang and et.al., 2016). To divert patient attention while in pain.
Evaluation: After 2 hours of nursing intervention goal partially met.
Identify clinical situations where the use of GCS is an appropriate means of
assessment
GCS stands for Glasgow Coma Scale and was developed in 1974 by Teasdale and
Jennett. It was originally designed to grade the severity and outcome of traumatic head
injury but has been extended for all causes of impaired consciousness and coma. This
tool should only be used as an assessment of the depth of unconsciousness (this is the
scoring). To reduce ambiguity, there is a need to define responses in descriptive terms
in addition to numerical scoring (Wang and et.al., 2016). indicate that the GSC should
be used to assess all brain injured patients and suggests that assessment should be
undertaken every 30 minis until the GCS reaches 15 or the patients condition stabilizes,
clinical experience dictates the latter. Patients with brain injuries are assessed using the
Glasgow Coma Scale (GCS). This review evaluates the use of GCS scoring in medical
3
impairment. A score of 15 indicates that the client is fully responsive (Rys and et.al., 2015). A score
less than 7 require frequent assessment.
Planning: In the planning phase, the nurses will prepare the action plan and schedule at what time the
medication will be given to the patient. Planning is very important and essential for the nurses as it will
help them providing the right guidance.
Interventions: Assess predisposing factors to pain. Monitor vital signs. Conduct diversion activities, offer
other comfort measures. Provide peaceful calm environment.
Rationale: To know the etiology of the unconsciousness. These are usually altered when one in pain
(Wang and et.al., 2016). To divert patient attention while in pain.
Evaluation: After 2 hours of nursing intervention goal partially met.
Identify clinical situations where the use of GCS is an appropriate means of
assessment
GCS stands for Glasgow Coma Scale and was developed in 1974 by Teasdale and
Jennett. It was originally designed to grade the severity and outcome of traumatic head
injury but has been extended for all causes of impaired consciousness and coma. This
tool should only be used as an assessment of the depth of unconsciousness (this is the
scoring). To reduce ambiguity, there is a need to define responses in descriptive terms
in addition to numerical scoring (Wang and et.al., 2016). indicate that the GSC should
be used to assess all brain injured patients and suggests that assessment should be
undertaken every 30 minis until the GCS reaches 15 or the patients condition stabilizes,
clinical experience dictates the latter. Patients with brain injuries are assessed using the
Glasgow Coma Scale (GCS). This review evaluates the use of GCS scoring in medical
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
literature and identifies the reasons for inaccuracy. Thus, by using GCS, the nursing
and health care professionals can assessed injuries related with head and brain. It
helps the doctors to analyse and interprets the diagnosis and report and also helps
them to acqurie the information about the level of unconsciousness of the person. In this
ways, the GCS is used and it helps the doctors adequately. The GSC provides a
standardised consistent assessment of conscious level by evaluating three behavioural
responses: Eye opening (E); Verbal response (V); Motor response (M) (GCS). The rest
of the chart includes other observations that could help identify the cause of
neurological deterioration. Its reliability has been tested in that it can be used by
different assessors and still produces a consistent assessment, irrespective of the
assessor’s status . However, this is subject to observer variability and therefore clinical
decisions should not solely be based upon the GCS .
3. Theory work produced to evidence learning. Tutor’s notes for the day are not acceptable.
(forexample: reflective report using a model of reflection, self assessment of learning and application to practice)
Geraghty, M. (2005), ‘Nursing the Unconscious Patient’, Nursing Standard, 20/1:54-64. This article
provides in depth information relating to the emergency care of the unconscious patient
Chung, M.J. and Choi, B.S., 2015. Study on the Nursing Practice Programs of the
Nurses in Small to Medium Sized Hospitals. Hospitals, 7(5).
Pasban-Noghabi, S. and Memarian, R., 2016. The Importance of Tools in Specific
Nursing Care in the Post-Anesthesia Care Unit (PACU). J Perioper Crit Intensive
Care Nurs, 2, p.131.
Wang, L.F., and et.al., 2016. Effect of comprehensive nursing intervention on
depression, anxiety and quality of life of infertility patients. Acta Med. Mediterr, 32,
pp.515-518.
4
and health care professionals can assessed injuries related with head and brain. It
helps the doctors to analyse and interprets the diagnosis and report and also helps
them to acqurie the information about the level of unconsciousness of the person. In this
ways, the GCS is used and it helps the doctors adequately. The GSC provides a
standardised consistent assessment of conscious level by evaluating three behavioural
responses: Eye opening (E); Verbal response (V); Motor response (M) (GCS). The rest
of the chart includes other observations that could help identify the cause of
neurological deterioration. Its reliability has been tested in that it can be used by
different assessors and still produces a consistent assessment, irrespective of the
assessor’s status . However, this is subject to observer variability and therefore clinical
decisions should not solely be based upon the GCS .
3. Theory work produced to evidence learning. Tutor’s notes for the day are not acceptable.
(forexample: reflective report using a model of reflection, self assessment of learning and application to practice)
Geraghty, M. (2005), ‘Nursing the Unconscious Patient’, Nursing Standard, 20/1:54-64. This article
provides in depth information relating to the emergency care of the unconscious patient
Chung, M.J. and Choi, B.S., 2015. Study on the Nursing Practice Programs of the
Nurses in Small to Medium Sized Hospitals. Hospitals, 7(5).
Pasban-Noghabi, S. and Memarian, R., 2016. The Importance of Tools in Specific
Nursing Care in the Post-Anesthesia Care Unit (PACU). J Perioper Crit Intensive
Care Nurs, 2, p.131.
Wang, L.F., and et.al., 2016. Effect of comprehensive nursing intervention on
depression, anxiety and quality of life of infertility patients. Acta Med. Mediterr, 32,
pp.515-518.
4
Rys, S., and et.al., 2015. Bridging the Gap Between Continuous Sedation Until Death
and Physician-Assisted Death: A Focus Group Study in Nursing Homes in
Flanders, Belgium. American Journal of Hospice and Palliative Medicine®, 32(4),
pp.407-416.
Shields, D., 2015. Intentionality in Healing—The Voices of Men in Nursing: A Grounded
Theory Investigation.
Kimura, A., 2017. Efficacy of Stroke Elderly with Unconsciousness Movement during
Non-REM Sleep on Vascular-Health in 5 Years. Archives of Physical Medicine and
Rehabilitation, 98(10), p.e64.
Fukumoto, M.,and et.al., 2016. Retrospective Analysis of Nursing Interventions and
Supportive Care for the Patients with AL Amyloidosis Receiving High-Dose
Melphalan and Autologous Stem-Cell Transplantation. Biology of Blood and
Marrow Transplantation, 22(3), pp.S447-S448.
Please attach/include your evidence of the theory you have made up to this form and then submit it to your Module Leader.
Please keep a copy of your form. The Module Leader will verify completion to the Programme Leader by forwarding the signed
form only to them.
Tutor to complete
4. Is work produced valid and authentic to meet learning outcomes of the session?
Yes No
If no, what further work is required to meet session’s outcomes?
5
and Physician-Assisted Death: A Focus Group Study in Nursing Homes in
Flanders, Belgium. American Journal of Hospice and Palliative Medicine®, 32(4),
pp.407-416.
Shields, D., 2015. Intentionality in Healing—The Voices of Men in Nursing: A Grounded
Theory Investigation.
Kimura, A., 2017. Efficacy of Stroke Elderly with Unconsciousness Movement during
Non-REM Sleep on Vascular-Health in 5 Years. Archives of Physical Medicine and
Rehabilitation, 98(10), p.e64.
Fukumoto, M.,and et.al., 2016. Retrospective Analysis of Nursing Interventions and
Supportive Care for the Patients with AL Amyloidosis Receiving High-Dose
Melphalan and Autologous Stem-Cell Transplantation. Biology of Blood and
Marrow Transplantation, 22(3), pp.S447-S448.
Please attach/include your evidence of the theory you have made up to this form and then submit it to your Module Leader.
Please keep a copy of your form. The Module Leader will verify completion to the Programme Leader by forwarding the signed
form only to them.
Tutor to complete
4. Is work produced valid and authentic to meet learning outcomes of the session?
Yes No
If no, what further work is required to meet session’s outcomes?
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Student signature: Module Leader signature:
(please state Student ID number, sign and date) (please sign and date)
6
(please state Student ID number, sign and date) (please sign and date)
6
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

