NUR341 Assessment 2: Nursing Assessment and Care Plan for Mr. Jungala
VerifiedAdded on 2023/04/20
|14
|5124
|325
Report
AI Summary
This report presents a comprehensive nursing assessment and care plan for Mr. Willie Jungala, a 71-year-old male admitted to the hospital following a fall with a soft tissue injury to his right hip. The assessment encompasses a detailed patient history, including medical conditions such as hypertension, type 2 diabetes, and unstable angina, along with medication details, social history, and lifestyle factors. The report then delves into the specific assessments required, including alcohol withdrawal risk, cognitive function, fall risk, functional ability, and nutritional status, explaining the purpose of each assessment and its relevance to Mr. Jungala's condition. The document outlines the rationale for each assessment, detailing the tools and methods used to evaluate the patient's needs and potential risks. The assessment also addresses the importance of a person-centered care approach, considering the patient's individual needs and preferences. Furthermore, the report highlights the initial medical orders and nursing interventions, including vital sign monitoring, dietary considerations, and medication management. Overall, the report provides a thorough overview of the patient's condition, the assessment process, and the planned nursing care to ensure optimal patient outcomes.
NUR341 Assessment 2
Mr Willie Jungala is a 71-year-old gentleman that has
been admitted to hospital post fall with soft tissue
injury to right hip.
History Assessment data
Patient profile Willie Jungala, 71-year-old man from Alice Springs
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich and tripped on kids tonka truck.
Landed on the floor on his right side. Following fall, Willie was experiencing
pain on movement and difficulty weight bearing. Two teenage grandchildren
tried to help him up but too painful, so they called an ambulance.
Phx Hypertension, Type 2 Diabetes, Unstable Angina
Allergies Nil known allergies.
Medications
· Aspirin 100mg mane
· Perindopril 2mg mane
· Metformin 1000mg TDS
· GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 times per week.
Tobacco use
Non-smoker. Regular exposure to campfire smoke. Most nights have a
campfire burning - sit by campfire and enjoy the night 'yarning' or listening to
music.
Drug use Nil.
Home environment
Lives in town camp in house with extended family. Approximately 12 family
members staying at house: wife; daughter and her 4 teenage boys; daughter
and her two toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daughter that lives at home there with
her two toddlers, has recently been diagnosed with cancer. A few drinks and
a few laughs help ease the stress.
Education Year 9 schooling.
Economic status Own land and house out bush but staying in town for a while.
Ethnic background Aboriginal. Speaks Waramungu, Walpiri, Eastern and Central Arrente,
Western Arrentre and English.
Religion/ spirituality Baptised Catholic by missionaries when young. Only goes to church for
funerals. Willie's spirit is strengthened by family and country.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
1
Mr Willie Jungala is a 71-year-old gentleman that has
been admitted to hospital post fall with soft tissue
injury to right hip.
History Assessment data
Patient profile Willie Jungala, 71-year-old man from Alice Springs
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich and tripped on kids tonka truck.
Landed on the floor on his right side. Following fall, Willie was experiencing
pain on movement and difficulty weight bearing. Two teenage grandchildren
tried to help him up but too painful, so they called an ambulance.
Phx Hypertension, Type 2 Diabetes, Unstable Angina
Allergies Nil known allergies.
Medications
· Aspirin 100mg mane
· Perindopril 2mg mane
· Metformin 1000mg TDS
· GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 times per week.
Tobacco use
Non-smoker. Regular exposure to campfire smoke. Most nights have a
campfire burning - sit by campfire and enjoy the night 'yarning' or listening to
music.
Drug use Nil.
Home environment
Lives in town camp in house with extended family. Approximately 12 family
members staying at house: wife; daughter and her 4 teenage boys; daughter
and her two toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daughter that lives at home there with
her two toddlers, has recently been diagnosed with cancer. A few drinks and
a few laughs help ease the stress.
Education Year 9 schooling.
Economic status Own land and house out bush but staying in town for a while.
Ethnic background Aboriginal. Speaks Waramungu, Walpiri, Eastern and Central Arrente,
Western Arrentre and English.
Religion/ spirituality Baptised Catholic by missionaries when young. Only goes to church for
funerals. Willie's spirit is strengthened by family and country.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
Sexual practice Married. Been with wife for 51 years. Have one son and two daughters.
ADLs Independent.
IADLs
Does not drive any more due to decreased vision (diabetic retinopathy).
Starting to get cataracts. Had glasses a few years ago but they don't work so
well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with diabetic doctors/ clinics. Go to
medical service if need to. Moves between medical services depending on
where he is staying at.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
2
Sexual practice Married. Been with wife for 51 years. Have one son and two daughters.
ADLs Independent.
IADLs
Does not drive any more due to decreased vision (diabetic retinopathy).
Starting to get cataracts. Had glasses a few years ago but they don't work so
well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with diabetic doctors/ clinics. Go to
medical service if need to. Moves between medical services depending on
where he is staying at.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
2
NUR341 Assessment 2
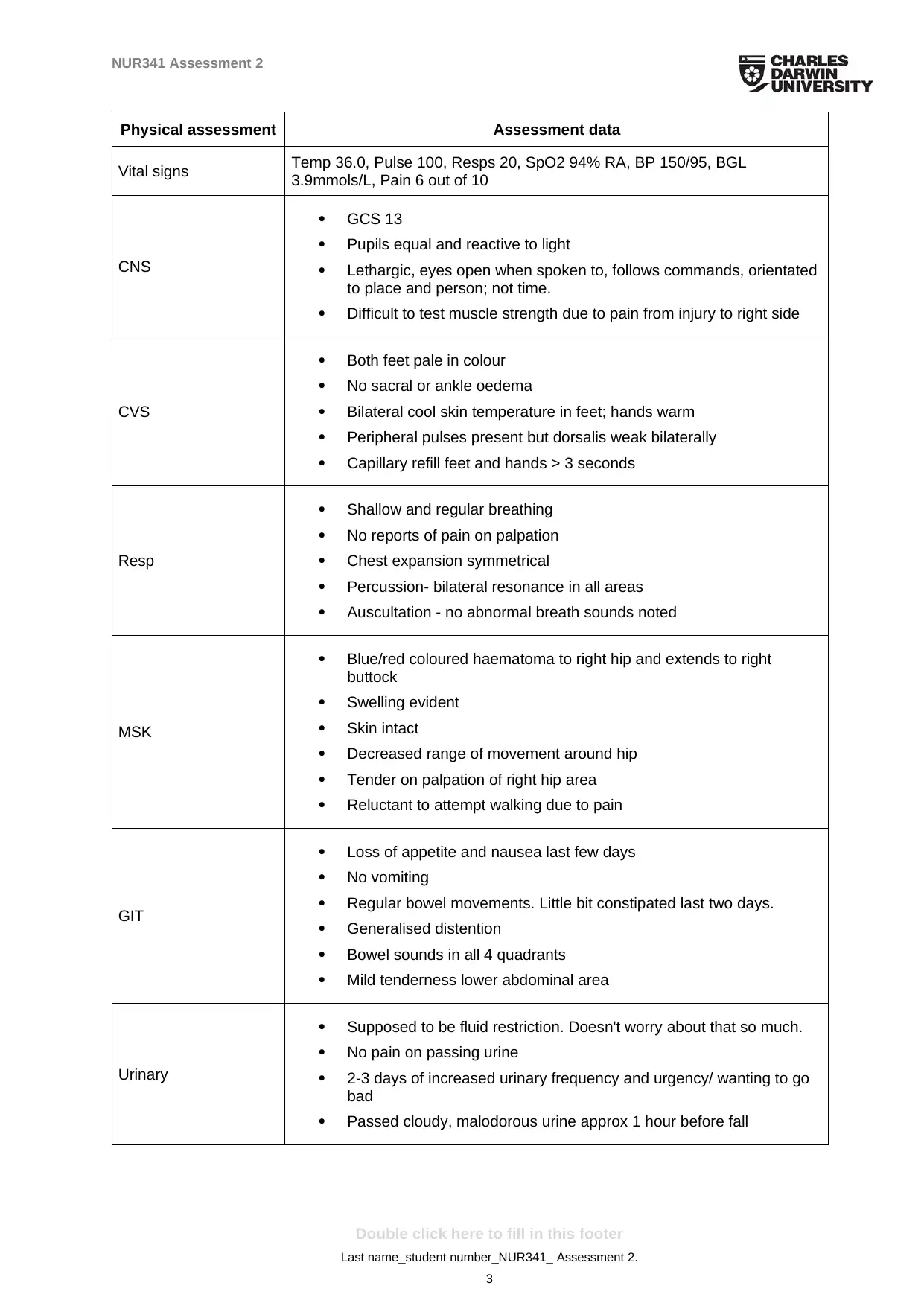
Physical assessment Assessment data
Vital signs Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95, BGL
3.9mmols/L, Pain 6 out of 10
CNS
· GCS 13
· Pupils equal and reactive to light
· Lethargic, eyes open when spoken to, follows commands, orientated
to place and person; not time.
· Difficult to test muscle strength due to pain from injury to right side
CVS
· Both feet pale in colour
· No sacral or ankle oedema
· Bilateral cool skin temperature in feet; hands warm
· Peripheral pulses present but dorsalis weak bilaterally
· Capillary refill feet and hands > 3 seconds
Resp
· Shallow and regular breathing
· No reports of pain on palpation
· Chest expansion symmetrical
· Percussion- bilateral resonance in all areas
· Auscultation - no abnormal breath sounds noted
MSK
· Blue/red coloured haematoma to right hip and extends to right
buttock
· Swelling evident
· Skin intact
· Decreased range of movement around hip
· Tender on palpation of right hip area
· Reluctant to attempt walking due to pain
GIT
· Loss of appetite and nausea last few days
· No vomiting
· Regular bowel movements. Little bit constipated last two days.
· Generalised distention
· Bowel sounds in all 4 quadrants
· Mild tenderness lower abdominal area
Urinary
· Supposed to be fluid restriction. Doesn't worry about that so much.
· No pain on passing urine
· 2-3 days of increased urinary frequency and urgency/ wanting to go
bad
· Passed cloudy, malodorous urine approx 1 hour before fall
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
3
Physical assessment Assessment data
Vital signs Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95, BGL
3.9mmols/L, Pain 6 out of 10
CNS
· GCS 13
· Pupils equal and reactive to light
· Lethargic, eyes open when spoken to, follows commands, orientated
to place and person; not time.
· Difficult to test muscle strength due to pain from injury to right side
CVS
· Both feet pale in colour
· No sacral or ankle oedema
· Bilateral cool skin temperature in feet; hands warm
· Peripheral pulses present but dorsalis weak bilaterally
· Capillary refill feet and hands > 3 seconds
Resp
· Shallow and regular breathing
· No reports of pain on palpation
· Chest expansion symmetrical
· Percussion- bilateral resonance in all areas
· Auscultation - no abnormal breath sounds noted
MSK
· Blue/red coloured haematoma to right hip and extends to right
buttock
· Swelling evident
· Skin intact
· Decreased range of movement around hip
· Tender on palpation of right hip area
· Reluctant to attempt walking due to pain
GIT
· Loss of appetite and nausea last few days
· No vomiting
· Regular bowel movements. Little bit constipated last two days.
· Generalised distention
· Bowel sounds in all 4 quadrants
· Mild tenderness lower abdominal area
Urinary
· Supposed to be fluid restriction. Doesn't worry about that so much.
· No pain on passing urine
· 2-3 days of increased urinary frequency and urgency/ wanting to go
bad
· Passed cloudy, malodorous urine approx 1 hour before fall
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

NUR341 Assessment 2
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
4
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

NUR341 Assessment 2
Part 1: Assessment
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or the purpose of
these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
In accordance to the information provided about the patient, it can be said that Mr. Willie
Jungala consumes alcohol occasionally. The frequency of his alcohol consumption has been
mentioned as 2 to 3 beers, 2 to 3 times per week. Clearly, the consumption level exceeds the
recommended limit of healthy consumption of alcohol by the Australian National Guidelines
for Alcohol consumption which is equivalent to only 375ml of alcohol consumption
(Australian drinking guidelines - FARE , 2019). However, considering Mr. Jungala’s medical
history of Diabetes, Hypertension as well as unstable Angina, it is recommended that the
patient must go through an alcohol assessment. The purpose of the alcohol withdrawal risk
assessment is to evaluate the possible physical health effects that could be triggered upon
initiating alcohol withdrawal. According to CIWA-Ar for Alcohol Withdrawal- MDCalc
(2019), withdrawal occurs in a characteristic drug dependent manner in individuals who
abruptly reduce or stop alcohol use. In order to manage withdrawal in the patient, it is
important to evaluate the dependence on alcohol abuse. The primary goal of conducting the
assessment is to devise appropriate measures so as to encourage withdrawal without affecting
the physical health of the patient adversely. To conduct the assessment, the nursing
professional would need to ask a number of questions related to the areas of nausea or
vomiting tendency, tremor, paroxysmal sweats, anxiety, agitation, tactile disturbances,
auditory disturbances, visual disturbances, headache/fullness in head, and orientation or
clouding of sensorium. On the basis of the responses acquired from the patient, the nurse
would score the patient’s dependence behavior on a scale of low, moderate and high. As per
the score, adequate pharmacological as well as non-pharmacological interventions would be
taken to manage the symptoms of the patient.
Cognitive assessment
On the basis of the patient’s general information provided, it can be said that the patient’s
cognitive functioning is within the normal range. It should also be noted that the patient is
able to perform his activities of daily living without assistance. However, it has been
mentioned that the patient feels stressed at time and consumes alcohol to relieve himself of
stress. This suggests the existence of a condition known as dual diagnosis. Research studies
suggests that stress or depression often triggers substance abuse which ultimately leads to the
emergence of mental health issues (Kaufman, 2018). At the same time, on account of the
advanced age of the patient, it is important to access that whether or not the patient could
potentially develop dementia or delirium. Therefore, conducting a cognitive assessment of the
patient is important. The cognitive assessment would be conducted by means of the Mental
state evaluation assessment. The mental state evaluation assessment helps in accessing a
number of factors such as general appearance, level of consciousness, mood and behavior,
orientation to time and place, memory, insight and judgment, language and speech,
knowledge and vocabulary as well as sensory and motor skills. The assessment of these
factors can help in determining whether or not the patient is suffering from any mental health
issues. Also, in order to access the dementia risk, the patient would be assessed on the basis of
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
5
Part 1: Assessment
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or the purpose of
these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
In accordance to the information provided about the patient, it can be said that Mr. Willie
Jungala consumes alcohol occasionally. The frequency of his alcohol consumption has been
mentioned as 2 to 3 beers, 2 to 3 times per week. Clearly, the consumption level exceeds the
recommended limit of healthy consumption of alcohol by the Australian National Guidelines
for Alcohol consumption which is equivalent to only 375ml of alcohol consumption
(Australian drinking guidelines - FARE , 2019). However, considering Mr. Jungala’s medical
history of Diabetes, Hypertension as well as unstable Angina, it is recommended that the
patient must go through an alcohol assessment. The purpose of the alcohol withdrawal risk
assessment is to evaluate the possible physical health effects that could be triggered upon
initiating alcohol withdrawal. According to CIWA-Ar for Alcohol Withdrawal- MDCalc
(2019), withdrawal occurs in a characteristic drug dependent manner in individuals who
abruptly reduce or stop alcohol use. In order to manage withdrawal in the patient, it is
important to evaluate the dependence on alcohol abuse. The primary goal of conducting the
assessment is to devise appropriate measures so as to encourage withdrawal without affecting
the physical health of the patient adversely. To conduct the assessment, the nursing
professional would need to ask a number of questions related to the areas of nausea or
vomiting tendency, tremor, paroxysmal sweats, anxiety, agitation, tactile disturbances,
auditory disturbances, visual disturbances, headache/fullness in head, and orientation or
clouding of sensorium. On the basis of the responses acquired from the patient, the nurse
would score the patient’s dependence behavior on a scale of low, moderate and high. As per
the score, adequate pharmacological as well as non-pharmacological interventions would be
taken to manage the symptoms of the patient.
Cognitive assessment
On the basis of the patient’s general information provided, it can be said that the patient’s
cognitive functioning is within the normal range. It should also be noted that the patient is
able to perform his activities of daily living without assistance. However, it has been
mentioned that the patient feels stressed at time and consumes alcohol to relieve himself of
stress. This suggests the existence of a condition known as dual diagnosis. Research studies
suggests that stress or depression often triggers substance abuse which ultimately leads to the
emergence of mental health issues (Kaufman, 2018). At the same time, on account of the
advanced age of the patient, it is important to access that whether or not the patient could
potentially develop dementia or delirium. Therefore, conducting a cognitive assessment of the
patient is important. The cognitive assessment would be conducted by means of the Mental
state evaluation assessment. The mental state evaluation assessment helps in accessing a
number of factors such as general appearance, level of consciousness, mood and behavior,
orientation to time and place, memory, insight and judgment, language and speech,
knowledge and vocabulary as well as sensory and motor skills. The assessment of these
factors can help in determining whether or not the patient is suffering from any mental health
issues. Also, in order to access the dementia risk, the patient would be assessed on the basis of
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
5

NUR341 Assessment 2
the Geriatric depression scale. The rationale for the use of the Geriatric depression scale can
be backed by the findings of evidence based studies which suggest that advancing age marks
the onset of insecurities and depression among the elderly.
Falls assessment
As has already been mentioned in the case study, Mr. Jungala is 71 year old and his
presenting complaint is a soft tissue injury in the right hip region. It should be noted here that
the patient had encountered fall on account of tripping over on a toy of his grandson. This
suggests that the patient is susceptible to further falls in future. In addition to this, it should
also be noted here that the previous medical history of the patient suggests that the patient
suffers from Diabetic retinopathy, which means that the patient is unable to see clearly and
experiences blurred vision (Hewston & Deshpande, 2016). This further suggests that the
patient is at a high risk of encountering falls in future. Research studies suggest that advancing
age leads to degradation of muscular strength and the tensile strength of the bones which
increases the risk of encountering a fall (D’Silva et al., 2016). Therefore, on the basis of the
accumulated information, it is obvious that the patient is at a high risk of encountering fall in
future which could even lead to a serious fracture. Therefore, it is extremely important to
conduct a fall risk assessment. The use of the JHFRAT tool kit which is also known as the
John Hopkins Fall Risk Assessment Tool could help in accessing the risk of the patient to
encounter further falls in future. The purpose of conducting the risk assessment is to secure
the environment and at the same time lower the chances of encountering an episode of fall
which could lead to serious injuries or fracture.
Functional assessment
The case study suggests that the patient experiences no problems in addressing activities of
daily living. However, it should be noted in this context, that the patient has experienced an
episode of fall and complains of tremendous pain. On account of the pain, the patient’s ability
to address the activities of daily living can be restricted. Therefore, conducting a functional
assessment is extremely useful to assess the ability of the patient to address his activities of
daily living. As stated by Chiba et al.(2015), functional assessment critically identifies a
patient’s ability to perform activities of daily living as well as instrumental activities of daily
living and the level of conducting self-maintenance activities. It should be noted in this
context that the use of Katz index of independence in activities of daily living can help in
critically evaluating the areas where the patient would be needing assistance with his activities
of daily living (Soto-Varela et al., 2015). On the basis of the assessment evaluation,
appropriate intervention strategy can be planned and the patient can be offered home based
nursing care to help him with daily living activities such as washing, dressing or cooking. It
should be noted in this context that the Katz Index of Independence in activities of daily living
is generally referred to as Katz ADL and helps in conducting an appropriate functional
assessment of the patient to perform his activities of daily living independently without an
external assistance (Malara et al., 2014). The tool helps in identifying the issues that the
patients experience with daily living activities and helps in devising appropriate intervention
strategies. The index places the level of perfection in performing the activities under six
categories known as bathing, dressing, toileting, transferring, continence as well as feeding. A
score of 6 indicates no problems with ADLs, however, a score of 4 indicates mild problem
and that of 2 indicates major problems with ADLs.
Nutritional assessment
On the basis of the information provided about the patient in the case study, it should be
mentioned that the patient suffers from loss of appetite. Also, on the basis of the previous
medical history, it should be stated that patient suffers from Hypertension as well as Diabetes
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
6
the Geriatric depression scale. The rationale for the use of the Geriatric depression scale can
be backed by the findings of evidence based studies which suggest that advancing age marks
the onset of insecurities and depression among the elderly.
Falls assessment
As has already been mentioned in the case study, Mr. Jungala is 71 year old and his
presenting complaint is a soft tissue injury in the right hip region. It should be noted here that
the patient had encountered fall on account of tripping over on a toy of his grandson. This
suggests that the patient is susceptible to further falls in future. In addition to this, it should
also be noted here that the previous medical history of the patient suggests that the patient
suffers from Diabetic retinopathy, which means that the patient is unable to see clearly and
experiences blurred vision (Hewston & Deshpande, 2016). This further suggests that the
patient is at a high risk of encountering falls in future. Research studies suggest that advancing
age leads to degradation of muscular strength and the tensile strength of the bones which
increases the risk of encountering a fall (D’Silva et al., 2016). Therefore, on the basis of the
accumulated information, it is obvious that the patient is at a high risk of encountering fall in
future which could even lead to a serious fracture. Therefore, it is extremely important to
conduct a fall risk assessment. The use of the JHFRAT tool kit which is also known as the
John Hopkins Fall Risk Assessment Tool could help in accessing the risk of the patient to
encounter further falls in future. The purpose of conducting the risk assessment is to secure
the environment and at the same time lower the chances of encountering an episode of fall
which could lead to serious injuries or fracture.
Functional assessment
The case study suggests that the patient experiences no problems in addressing activities of
daily living. However, it should be noted in this context, that the patient has experienced an
episode of fall and complains of tremendous pain. On account of the pain, the patient’s ability
to address the activities of daily living can be restricted. Therefore, conducting a functional
assessment is extremely useful to assess the ability of the patient to address his activities of
daily living. As stated by Chiba et al.(2015), functional assessment critically identifies a
patient’s ability to perform activities of daily living as well as instrumental activities of daily
living and the level of conducting self-maintenance activities. It should be noted in this
context that the use of Katz index of independence in activities of daily living can help in
critically evaluating the areas where the patient would be needing assistance with his activities
of daily living (Soto-Varela et al., 2015). On the basis of the assessment evaluation,
appropriate intervention strategy can be planned and the patient can be offered home based
nursing care to help him with daily living activities such as washing, dressing or cooking. It
should be noted in this context that the Katz Index of Independence in activities of daily living
is generally referred to as Katz ADL and helps in conducting an appropriate functional
assessment of the patient to perform his activities of daily living independently without an
external assistance (Malara et al., 2014). The tool helps in identifying the issues that the
patients experience with daily living activities and helps in devising appropriate intervention
strategies. The index places the level of perfection in performing the activities under six
categories known as bathing, dressing, toileting, transferring, continence as well as feeding. A
score of 6 indicates no problems with ADLs, however, a score of 4 indicates mild problem
and that of 2 indicates major problems with ADLs.
Nutritional assessment
On the basis of the information provided about the patient in the case study, it should be
mentioned that the patient suffers from loss of appetite. Also, on the basis of the previous
medical history, it should be stated that patient suffers from Hypertension as well as Diabetes
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

NUR341 Assessment 2
which suggests that the patient must consume a balanced diet so as to avoid the physiological
imbalance of the blood sugar or the blood pressure level. It is extremely important to conduct
a nutritional assessment of the patient so as to identify clinically if the patient suffers from
malnutrition and at the same time monitor the nutritional status of the patient so as to ensure
that the patient consumes an appropriate diet that does not interfere with the normal blood
glucose or blood pressure level of the patient. The nutritional assessment of the patient can be
conducted by investigating the nutrition history and at the same time conducting a physical
assessment. Typically factors such as observing the general skin, nails, eyes, mouth, hair,
head and neck, MSK, CNS, peripheral vaculature and abdomen can help in conducting a
general physical assessment of the patient. In addition to this, counting anthropometric
measurements such as estimating the height, weight, BMI, waist circumference, hip ratio,
skinfold thickness, mid arm and mid arm muscular circumferences can help in assessing
whether or not the patient is susceptible to suffer from obesity (D’Silva et al., 2016; Abd-El-
Gawad et al., 2014). Therefore, the pateint’s nutritional assessment can be conducted by
means of a nutritional health checklist.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
7
which suggests that the patient must consume a balanced diet so as to avoid the physiological
imbalance of the blood sugar or the blood pressure level. It is extremely important to conduct
a nutritional assessment of the patient so as to identify clinically if the patient suffers from
malnutrition and at the same time monitor the nutritional status of the patient so as to ensure
that the patient consumes an appropriate diet that does not interfere with the normal blood
glucose or blood pressure level of the patient. The nutritional assessment of the patient can be
conducted by investigating the nutrition history and at the same time conducting a physical
assessment. Typically factors such as observing the general skin, nails, eyes, mouth, hair,
head and neck, MSK, CNS, peripheral vaculature and abdomen can help in conducting a
general physical assessment of the patient. In addition to this, counting anthropometric
measurements such as estimating the height, weight, BMI, waist circumference, hip ratio,
skinfold thickness, mid arm and mid arm muscular circumferences can help in assessing
whether or not the patient is susceptible to suffer from obesity (D’Silva et al., 2016; Abd-El-
Gawad et al., 2014). Therefore, the pateint’s nutritional assessment can be conducted by
means of a nutritional health checklist.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

NUR341 Assessment 2
Part 2: Plan and implementation
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and medications may have
contributed to his fall. Choose one factor and outline your nursing actions and referrals you would
execute; include rationales for same.
On the basis of the background information provided, it can be mentioned that the patient’s
Diabetic retinopathy might have been one potential cause that led to the fall. Diabetes
retinopathy interferes with normal vision and causes blurred vision. It can be said that on
account of the inability of Mr. Jungula to see clearly, he tripped over his grandson’s toy and
experienced a fall. In addition to this, the provided medical information of the patient also
suggests that the patient has developed cataracts and was recommended to use glasses which
do not work anymore. Therefore, the patient is susceptible to experience recurrent episodes of
fall on account of not being able to see clearly. In addition to this, the patient reports to relive
stress by consuming alcohol and states that he consumes 2-3 beers, two to three times a week.
Consumption of alcohol would trigger dizziness which could further increase the risk of
encountering another fall. Therefore, the nursing plan for Mr. Jungula would comprise of
reducing the risks of recurrent falls. In order to ensure the same, the nursing actions that
would be adapted would comprise of conducting a thorough fall risk assessment and then
adapting strategies to secure the environment (Soto-Varela et al., 2015). This would be done
by educating the patient as well as the family members to ensure that the home environment
avoids clustering of furniture and has sufficient light so as to ensure that Mr. Jungula is able
to see clearly. Further, the family members would also be educated to ensure that the floor is
dry and does not contain loose rugs and scattered toys which could increase the probability of
tripping and falling. The patient would be referred to an ophthalmologist. The rationale for
the same being offering assistance with a cataract surgery, so as to ensure that patient is able
to see clearly and does not encounter another subsequent fall. The nursing action for the
referral would comprise of educating the patient and the family members about the need to
get a cataract surgery done and providing them information about ophthalmologists who
would be able to conduct the surgery. In addition to this, the patient would also be referred to
a veteran alcohol withdrawal social group. The rationale for the same being that the
dependence on alcohol exceeds the normal permissible limits and this could interfere with the
normal blood glucose as well as blood pressure level of the patient and at the same time could
also lead to another fall (Hewston & Deshpande, 2016). The support group would make use
of appropriate counseling and intervention strategies to address the alcohol abuse issues and
would help in maintain a sound physical health (Kuerbis et al., 2014). At the same time,
secondary nursing actions would comprise of assisting the patient to use comfortable
footwear and administering proper medication in consultation with the physician to ensure
pain relief. Therefore, it can be mentioned that the primary goal would be to educate the
family members of the patient to secure the home environment and make referral to an
ophthalmologist so as to ensure clear vision after getting a cataract surgery. The secondary
nursing actions would comprise of assisting the patient with comfortable footwear and
reducing the alcohol dependence to prevent dizziness and loss of clear vision.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
8
Part 2: Plan and implementation
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and medications may have
contributed to his fall. Choose one factor and outline your nursing actions and referrals you would
execute; include rationales for same.
On the basis of the background information provided, it can be mentioned that the patient’s
Diabetic retinopathy might have been one potential cause that led to the fall. Diabetes
retinopathy interferes with normal vision and causes blurred vision. It can be said that on
account of the inability of Mr. Jungula to see clearly, he tripped over his grandson’s toy and
experienced a fall. In addition to this, the provided medical information of the patient also
suggests that the patient has developed cataracts and was recommended to use glasses which
do not work anymore. Therefore, the patient is susceptible to experience recurrent episodes of
fall on account of not being able to see clearly. In addition to this, the patient reports to relive
stress by consuming alcohol and states that he consumes 2-3 beers, two to three times a week.
Consumption of alcohol would trigger dizziness which could further increase the risk of
encountering another fall. Therefore, the nursing plan for Mr. Jungula would comprise of
reducing the risks of recurrent falls. In order to ensure the same, the nursing actions that
would be adapted would comprise of conducting a thorough fall risk assessment and then
adapting strategies to secure the environment (Soto-Varela et al., 2015). This would be done
by educating the patient as well as the family members to ensure that the home environment
avoids clustering of furniture and has sufficient light so as to ensure that Mr. Jungula is able
to see clearly. Further, the family members would also be educated to ensure that the floor is
dry and does not contain loose rugs and scattered toys which could increase the probability of
tripping and falling. The patient would be referred to an ophthalmologist. The rationale for
the same being offering assistance with a cataract surgery, so as to ensure that patient is able
to see clearly and does not encounter another subsequent fall. The nursing action for the
referral would comprise of educating the patient and the family members about the need to
get a cataract surgery done and providing them information about ophthalmologists who
would be able to conduct the surgery. In addition to this, the patient would also be referred to
a veteran alcohol withdrawal social group. The rationale for the same being that the
dependence on alcohol exceeds the normal permissible limits and this could interfere with the
normal blood glucose as well as blood pressure level of the patient and at the same time could
also lead to another fall (Hewston & Deshpande, 2016). The support group would make use
of appropriate counseling and intervention strategies to address the alcohol abuse issues and
would help in maintain a sound physical health (Kuerbis et al., 2014). At the same time,
secondary nursing actions would comprise of assisting the patient to use comfortable
footwear and administering proper medication in consultation with the physician to ensure
pain relief. Therefore, it can be mentioned that the primary goal would be to educate the
family members of the patient to secure the home environment and make referral to an
ophthalmologist so as to ensure clear vision after getting a cataract surgery. The secondary
nursing actions would comprise of assisting the patient with comfortable footwear and
reducing the alcohol dependence to prevent dizziness and loss of clear vision.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
8
NUR341 Assessment 2
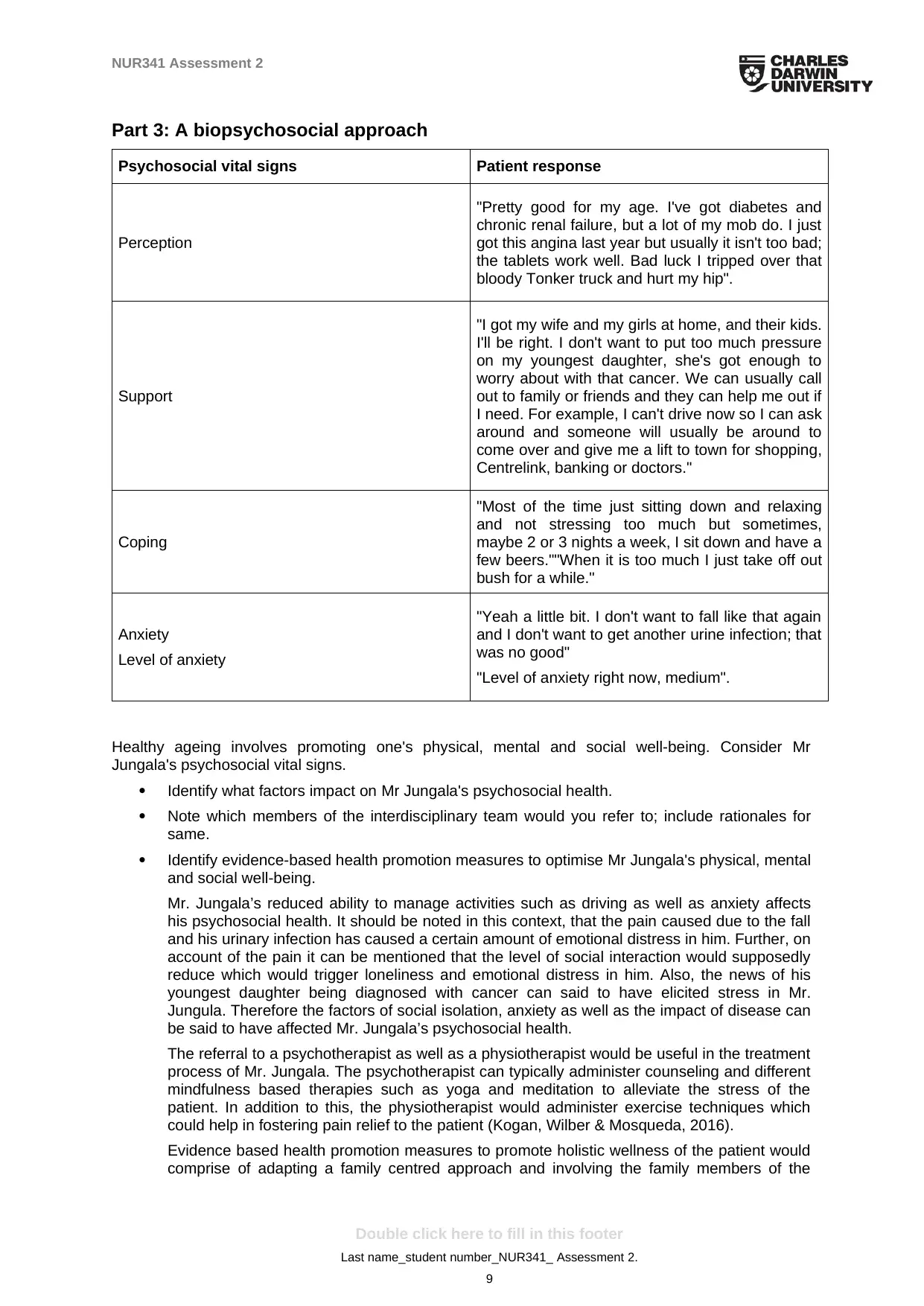
Part 3: A biopsychosocial approach
Psychosocial vital signs Patient response
Perception
"Pretty good for my age. I've got diabetes and
chronic renal failure, but a lot of my mob do. I just
got this angina last year but usually it isn't too bad;
the tablets work well. Bad luck I tripped over that
bloody Tonker truck and hurt my hip".
Support
"I got my wife and my girls at home, and their kids.
I'll be right. I don't want to put too much pressure
on my youngest daughter, she's got enough to
worry about with that cancer. We can usually call
out to family or friends and they can help me out if
I need. For example, I can't drive now so I can ask
around and someone will usually be around to
come over and give me a lift to town for shopping,
Centrelink, banking or doctors."
Coping
"Most of the time just sitting down and relaxing
and not stressing too much but sometimes,
maybe 2 or 3 nights a week, I sit down and have a
few beers.""When it is too much I just take off out
bush for a while."
Anxiety
Level of anxiety
"Yeah a little bit. I don't want to fall like that again
and I don't want to get another urine infection; that
was no good"
"Level of anxiety right now, medium".
Healthy ageing involves promoting one's physical, mental and social well-being. Consider Mr
Jungala's psychosocial vital signs.
· Identify what factors impact on Mr Jungala's psychosocial health.
· Note which members of the interdisciplinary team would you refer to; include rationales for
same.
· Identify evidence-based health promotion measures to optimise Mr Jungala's physical, mental
and social well-being.
Mr. Jungala’s reduced ability to manage activities such as driving as well as anxiety affects
his psychosocial health. It should be noted in this context, that the pain caused due to the fall
and his urinary infection has caused a certain amount of emotional distress in him. Further, on
account of the pain it can be mentioned that the level of social interaction would supposedly
reduce which would trigger loneliness and emotional distress in him. Also, the news of his
youngest daughter being diagnosed with cancer can said to have elicited stress in Mr.
Jungula. Therefore the factors of social isolation, anxiety as well as the impact of disease can
be said to have affected Mr. Jungala’s psychosocial health.
The referral to a psychotherapist as well as a physiotherapist would be useful in the treatment
process of Mr. Jungala. The psychotherapist can typically administer counseling and different
mindfulness based therapies such as yoga and meditation to alleviate the stress of the
patient. In addition to this, the physiotherapist would administer exercise techniques which
could help in fostering pain relief to the patient (Kogan, Wilber & Mosqueda, 2016).
Evidence based health promotion measures to promote holistic wellness of the patient would
comprise of adapting a family centred approach and involving the family members of the
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
9
Part 3: A biopsychosocial approach
Psychosocial vital signs Patient response
Perception
"Pretty good for my age. I've got diabetes and
chronic renal failure, but a lot of my mob do. I just
got this angina last year but usually it isn't too bad;
the tablets work well. Bad luck I tripped over that
bloody Tonker truck and hurt my hip".
Support
"I got my wife and my girls at home, and their kids.
I'll be right. I don't want to put too much pressure
on my youngest daughter, she's got enough to
worry about with that cancer. We can usually call
out to family or friends and they can help me out if
I need. For example, I can't drive now so I can ask
around and someone will usually be around to
come over and give me a lift to town for shopping,
Centrelink, banking or doctors."
Coping
"Most of the time just sitting down and relaxing
and not stressing too much but sometimes,
maybe 2 or 3 nights a week, I sit down and have a
few beers.""When it is too much I just take off out
bush for a while."
Anxiety
Level of anxiety
"Yeah a little bit. I don't want to fall like that again
and I don't want to get another urine infection; that
was no good"
"Level of anxiety right now, medium".
Healthy ageing involves promoting one's physical, mental and social well-being. Consider Mr
Jungala's psychosocial vital signs.
· Identify what factors impact on Mr Jungala's psychosocial health.
· Note which members of the interdisciplinary team would you refer to; include rationales for
same.
· Identify evidence-based health promotion measures to optimise Mr Jungala's physical, mental
and social well-being.
Mr. Jungala’s reduced ability to manage activities such as driving as well as anxiety affects
his psychosocial health. It should be noted in this context, that the pain caused due to the fall
and his urinary infection has caused a certain amount of emotional distress in him. Further, on
account of the pain it can be mentioned that the level of social interaction would supposedly
reduce which would trigger loneliness and emotional distress in him. Also, the news of his
youngest daughter being diagnosed with cancer can said to have elicited stress in Mr.
Jungula. Therefore the factors of social isolation, anxiety as well as the impact of disease can
be said to have affected Mr. Jungala’s psychosocial health.
The referral to a psychotherapist as well as a physiotherapist would be useful in the treatment
process of Mr. Jungala. The psychotherapist can typically administer counseling and different
mindfulness based therapies such as yoga and meditation to alleviate the stress of the
patient. In addition to this, the physiotherapist would administer exercise techniques which
could help in fostering pain relief to the patient (Kogan, Wilber & Mosqueda, 2016).
Evidence based health promotion measures to promote holistic wellness of the patient would
comprise of adapting a family centred approach and involving the family members of the
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

NUR341 Assessment 2
patient in the care process (Douglas et al., 2014). Shared decision making along with the
consideration of the personal preference of both the patient as well as the family members
would help in fostering holistic wellness and recovery. In addition to this, the nurse would
place the patient at the heart of the care process and deliver patient centred care for a
positive and effective recovery. Research studies suggest that involving the family members
in the decision making process can help in improving patient outcome (Douglas et al., 2014;
Kogan, Wilber & Mosqueda, 2016). Further, the care professionals must ensure a culturally
safe care delivery and make sure that the culture and spiritual specific preferences of the
patient as well as the family members is adequately addressed. This would be done by
making referral to an aboriginal care professional who would be able to converse with the
patient in the similar language and at the same time the gender specific requirement of the
patient would also be considered so as to ensure that the patient is satisfied with the devised
set of intervention strategies (Giger, 2016). Therefore, it can be expected that upon using the
principles of cultural safety and trans-cultural nursing, the patient would experience improved
health outcome.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
10
patient in the care process (Douglas et al., 2014). Shared decision making along with the
consideration of the personal preference of both the patient as well as the family members
would help in fostering holistic wellness and recovery. In addition to this, the nurse would
place the patient at the heart of the care process and deliver patient centred care for a
positive and effective recovery. Research studies suggest that involving the family members
in the decision making process can help in improving patient outcome (Douglas et al., 2014;
Kogan, Wilber & Mosqueda, 2016). Further, the care professionals must ensure a culturally
safe care delivery and make sure that the culture and spiritual specific preferences of the
patient as well as the family members is adequately addressed. This would be done by
making referral to an aboriginal care professional who would be able to converse with the
patient in the similar language and at the same time the gender specific requirement of the
patient would also be considered so as to ensure that the patient is satisfied with the devised
set of intervention strategies (Giger, 2016). Therefore, it can be expected that upon using the
principles of cultural safety and trans-cultural nursing, the patient would experience improved
health outcome.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
References
Abd-El-Gawad, W. M., Abou-Hashem, R. M., El Maraghy, M. O., & Amin, G. E. (2014).
The validity of Geriatric Nutrition Risk Index: simple tool for prediction of
nutritional-related complication of hospitalized elderly patients. Comparison with
Mini Nutritional Assessment. Clinical nutrition, 33(6), 1108-1116.
Australian drinking guidelines - FARE (2019). Australian drinking guidelines - FARE.
[online] FARE. Available at: http://fare.org.au/resources/australian-drinking-
guidelines/ [Accessed 27 Apr. 2019].
Chiba, Y., Kimbara, Y., Kodera, R., Tsuboi, Y., Sato, K., Tamura, Y., ... & Araki, A. (2015).
Risk factors associated with falls in elderly patients with type 2 diabetes. Journal of
diabetes and its complications, 29(7), 898-902.
CIWA-Ar for Alcohol Withdrawal - MDCalc (2019). CIWA-Ar for Alcohol Withdrawal -
MDCalc. [online] Mdcalc.com. Available at: https://www.mdcalc.com/ciwa-ar-
alcohol-withdrawal [Accessed 27 Apr. 2019].
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-Pollara, M.,
Lauderdale, J., ... & Purnell, L. (2014). Guidelines for implementing culturally
competent nursing care. Journal of Transcultural Nursing, 25(2), 109-121.
D'Silva, L. J., Lin, J., Staecker, H., Whitney, S. L., & Kluding, P. M. (2016). Impact of
diabetic complications on balance and falls: contribution of the vestibular
system. Physical therapy, 96(3), 400-409.
Giger, J. N. (2016). Transcultural Nursing-E-Book: Assessment and Intervention. Elsevier
Health Sciences.
Hewston, P., & Deshpande, N. (2016). Falls and balance impairments in older adults with
type 2 diabetes: thinking beyond diabetic peripheral neuropathy. Canadian journal of
diabetes, 40(1), 6-9.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
11
References
Abd-El-Gawad, W. M., Abou-Hashem, R. M., El Maraghy, M. O., & Amin, G. E. (2014).
The validity of Geriatric Nutrition Risk Index: simple tool for prediction of
nutritional-related complication of hospitalized elderly patients. Comparison with
Mini Nutritional Assessment. Clinical nutrition, 33(6), 1108-1116.
Australian drinking guidelines - FARE (2019). Australian drinking guidelines - FARE.
[online] FARE. Available at: http://fare.org.au/resources/australian-drinking-
guidelines/ [Accessed 27 Apr. 2019].
Chiba, Y., Kimbara, Y., Kodera, R., Tsuboi, Y., Sato, K., Tamura, Y., ... & Araki, A. (2015).
Risk factors associated with falls in elderly patients with type 2 diabetes. Journal of
diabetes and its complications, 29(7), 898-902.
CIWA-Ar for Alcohol Withdrawal - MDCalc (2019). CIWA-Ar for Alcohol Withdrawal -
MDCalc. [online] Mdcalc.com. Available at: https://www.mdcalc.com/ciwa-ar-
alcohol-withdrawal [Accessed 27 Apr. 2019].
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-Pollara, M.,
Lauderdale, J., ... & Purnell, L. (2014). Guidelines for implementing culturally
competent nursing care. Journal of Transcultural Nursing, 25(2), 109-121.
D'Silva, L. J., Lin, J., Staecker, H., Whitney, S. L., & Kluding, P. M. (2016). Impact of
diabetic complications on balance and falls: contribution of the vestibular
system. Physical therapy, 96(3), 400-409.
Giger, J. N. (2016). Transcultural Nursing-E-Book: Assessment and Intervention. Elsevier
Health Sciences.
Hewston, P., & Deshpande, N. (2016). Falls and balance impairments in older adults with
type 2 diabetes: thinking beyond diabetic peripheral neuropathy. Canadian journal of
diabetes, 40(1), 6-9.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
11
NUR341 Assessment 2
Kaufman, A. S. (2018). Contemporary intellectual assessment: Theories, tests, and issues.
Guilford Publications.
Kogan, A. C., Wilber, K., & Mosqueda, L. (2016). Person‐centered care for older adults with
chronic conditions and functional impairment: A systematic literature review. Journal
of the American Geriatrics Society, 64(1), e1-e7.
Kuerbis, A., Sacco, P., Blazer, D. G., & Moore, A. A. (2014). Substance abuse among older
adults. Clinics in geriatric medicine, 30(3), 629-654.
Malara, A., Sgrò, G., Caruso, C., Ceravolo, F., Curinga, G., Renda, G. F., ... & Rispoli, V.
(2014). Relationship between cognitive impairment and nutritional assessment on
functional status in Calabrian long-term-care. Clinical interventions in aging, 9, 105.
Soto-Varela, A., Faraldo-García, A., Rossi-Izquierdo, M., Lirola-Delgado, A., Vaamonde-
Sánchez-Andrade, I., del-Río-Valeiras, M., ... & Santos-Pérez, S. (2015). Can we
predict the risk of falls in elderly patients with instability?. Auris Nasus Larynx, 42(1),
8-14.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
12
Kaufman, A. S. (2018). Contemporary intellectual assessment: Theories, tests, and issues.
Guilford Publications.
Kogan, A. C., Wilber, K., & Mosqueda, L. (2016). Person‐centered care for older adults with
chronic conditions and functional impairment: A systematic literature review. Journal
of the American Geriatrics Society, 64(1), e1-e7.
Kuerbis, A., Sacco, P., Blazer, D. G., & Moore, A. A. (2014). Substance abuse among older
adults. Clinics in geriatric medicine, 30(3), 629-654.
Malara, A., Sgrò, G., Caruso, C., Ceravolo, F., Curinga, G., Renda, G. F., ... & Rispoli, V.
(2014). Relationship between cognitive impairment and nutritional assessment on
functional status in Calabrian long-term-care. Clinical interventions in aging, 9, 105.
Soto-Varela, A., Faraldo-García, A., Rossi-Izquierdo, M., Lirola-Delgado, A., Vaamonde-
Sánchez-Andrade, I., del-Río-Valeiras, M., ... & Santos-Pérez, S. (2015). Can we
predict the risk of falls in elderly patients with instability?. Auris Nasus Larynx, 42(1),
8-14.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



