NUR341 Assessment 2: Analyzing Mr. Jungala's Healthcare Needs
VerifiedAdded on 2023/01/19
|10
|4564
|30
Report
AI Summary
This report, submitted as NUR341 Assessment 2, presents a comprehensive care plan for Mr. Willie Jungala, a 71-year-old patient admitted after a fall with a soft tissue injury to his right hip. The report is divided into three parts: assessment, planning and implementation, and a biopsychosocial approach. Part 1 details various assessments including alcohol withdrawal risk, cognitive function, falls risk, functional status, and nutritional needs, providing rationales for their relevance to Mr. Jungala's case. Part 2 focuses on the planning and implementation of nursing interventions, specifically addressing normal age-related changes, co-morbidities, acute illness and medications that contributed to the patient’s fall, with a focus on diabetes care and its integration into a comprehensive care plan. Part 3 emphasizes a biopsychosocial approach to care, considering the patient's physical, psychological, and social needs. The report uses evidence-based practice to tailor care to meet the patient's healthcare requirements, considering his medical history (hypertension, Type 2 diabetes, unstable angina), social situation, and cultural background, including his Aboriginal heritage. The report highlights the role of nurses in providing patient-centered care, promoting independence, and enhancing the patient's quality of life.
NUR341 Assessment 2
Mr Willie Jungala is a 71-year-old gentleman that has
been admitted to hospital post fall with soft tissue
injury to right hip.
History Assessment d
Patient profile Willie Jungala, 71-year-old man from Alice S
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich a
Landed on the floor on his right side. Follow
pain on movement and difficulty weight bea
tried to help him up but too painful, so they
Phx Hypertension, Type 2 Diabetes, Unstable A
Allergies Nil known allergies.
Medications
Aspirin 100mg mane
Perindopril 2mg mane
Metformin 1000mg TDS
GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 ti
Tobacco use
Non-smoker. Regular exposure to campfire
campfire burning - sit by campfire and enjoy
music.
Drug use Nil.
Home environment
Lives in town camp in house with extended
members staying at house: wife; daughter a
and her two toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daug
her two toddlers, has recently been diagnos
a few laughs help ease the stress.
Education Year 9 schooling.
Economic status Own land and house out bush but staying in
Ethnic background Aboriginal. Speaks Waramungu, Walpiri, Ea
Western Arrentre and English.
Religion/ spirituality Baptised Catholic by missionaries when you
funerals. Willie's spirit is strengthened by fa
Sexual practice Married. Been with wife for 51 years. Have
ADLs Independent.
IADLs
Does not drive any more due to decreased
Starting to get cataracts. Had glasses a few
well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with d
medical service if need to. Moves between
where he is staying at.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
1
Mr Willie Jungala is a 71-year-old gentleman that has
been admitted to hospital post fall with soft tissue
injury to right hip.
History Assessment d
Patient profile Willie Jungala, 71-year-old man from Alice S
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich a
Landed on the floor on his right side. Follow
pain on movement and difficulty weight bea
tried to help him up but too painful, so they
Phx Hypertension, Type 2 Diabetes, Unstable A
Allergies Nil known allergies.
Medications
Aspirin 100mg mane
Perindopril 2mg mane
Metformin 1000mg TDS
GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 ti
Tobacco use
Non-smoker. Regular exposure to campfire
campfire burning - sit by campfire and enjoy
music.
Drug use Nil.
Home environment
Lives in town camp in house with extended
members staying at house: wife; daughter a
and her two toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daug
her two toddlers, has recently been diagnos
a few laughs help ease the stress.
Education Year 9 schooling.
Economic status Own land and house out bush but staying in
Ethnic background Aboriginal. Speaks Waramungu, Walpiri, Ea
Western Arrentre and English.
Religion/ spirituality Baptised Catholic by missionaries when you
funerals. Willie's spirit is strengthened by fa
Sexual practice Married. Been with wife for 51 years. Have
ADLs Independent.
IADLs
Does not drive any more due to decreased
Starting to get cataracts. Had glasses a few
well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with d
medical service if need to. Moves between
where he is staying at.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
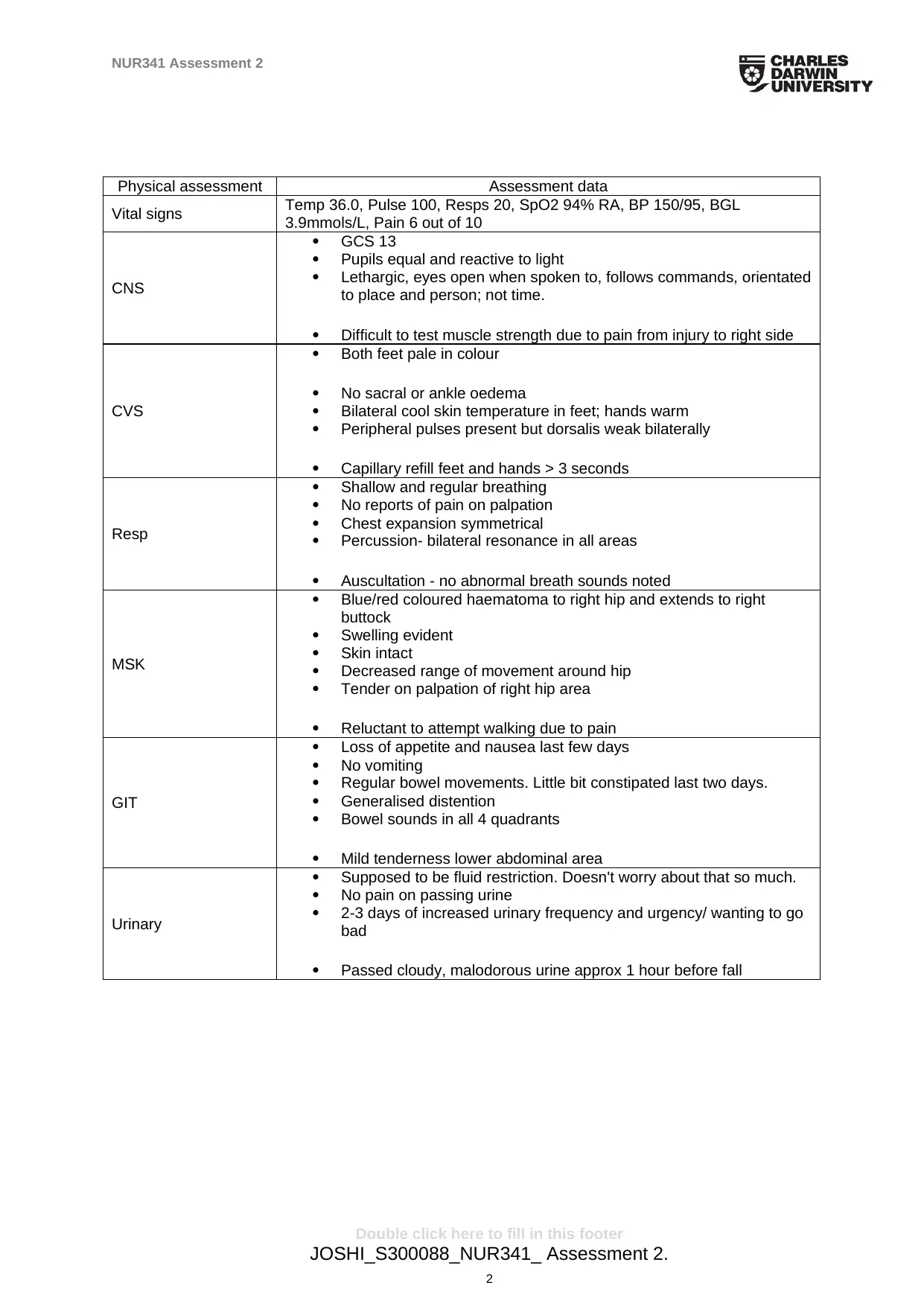
Physical assessment Assessment data
Vital signs Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95, BGL
3.9mmols/L, Pain 6 out of 10
CNS
GCS 13
Pupils equal and reactive to light
Lethargic, eyes open when spoken to, follows commands, orientated
to place and person; not time.
Difficult to test muscle strength due to pain from injury to right side
CVS
Both feet pale in colour
No sacral or ankle oedema
Bilateral cool skin temperature in feet; hands warm
Peripheral pulses present but dorsalis weak bilaterally
Capillary refill feet and hands > 3 seconds
Resp
Shallow and regular breathing
No reports of pain on palpation
Chest expansion symmetrical
Percussion- bilateral resonance in all areas
Auscultation - no abnormal breath sounds noted
MSK
Blue/red coloured haematoma to right hip and extends to right
buttock
Swelling evident
Skin intact
Decreased range of movement around hip
Tender on palpation of right hip area
Reluctant to attempt walking due to pain
GIT
Loss of appetite and nausea last few days
No vomiting
Regular bowel movements. Little bit constipated last two days.
Generalised distention
Bowel sounds in all 4 quadrants
Mild tenderness lower abdominal area
Urinary
Supposed to be fluid restriction. Doesn't worry about that so much.
No pain on passing urine
2-3 days of increased urinary frequency and urgency/ wanting to go
bad
Passed cloudy, malodorous urine approx 1 hour before fall
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
2
Physical assessment Assessment data
Vital signs Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95, BGL
3.9mmols/L, Pain 6 out of 10
CNS
GCS 13
Pupils equal and reactive to light
Lethargic, eyes open when spoken to, follows commands, orientated
to place and person; not time.
Difficult to test muscle strength due to pain from injury to right side
CVS
Both feet pale in colour
No sacral or ankle oedema
Bilateral cool skin temperature in feet; hands warm
Peripheral pulses present but dorsalis weak bilaterally
Capillary refill feet and hands > 3 seconds
Resp
Shallow and regular breathing
No reports of pain on palpation
Chest expansion symmetrical
Percussion- bilateral resonance in all areas
Auscultation - no abnormal breath sounds noted
MSK
Blue/red coloured haematoma to right hip and extends to right
buttock
Swelling evident
Skin intact
Decreased range of movement around hip
Tender on palpation of right hip area
Reluctant to attempt walking due to pain
GIT
Loss of appetite and nausea last few days
No vomiting
Regular bowel movements. Little bit constipated last two days.
Generalised distention
Bowel sounds in all 4 quadrants
Mild tenderness lower abdominal area
Urinary
Supposed to be fluid restriction. Doesn't worry about that so much.
No pain on passing urine
2-3 days of increased urinary frequency and urgency/ wanting to go
bad
Passed cloudy, malodorous urine approx 1 hour before fall
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
2
NUR341 Assessment 2
Part 1: Assessment (1000 words)
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or the purpose of
these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
Alcohol withdrawal risk assessment is considered by Morley et al. (2016) as one of
the most significant steps in fostering early identification of alcohol withdrawal
syndrome. Alcohol withdrawal syndrome encompasses the unpleasant mental and
physical indications that are manifested after alcohol cessation. Such symptoms tend
to deviate from minimal tremors, to hallucinations and in adverse conditions,
convulsions may manifest. Lappin et al. (2018) demystify that repetitive withdrawal
episodes act as essential contributors to the advancement of alcohol dependence,
and the detrimental health consequences associated with drinking. In early stages,
alcohol withdrawal symptom among elderly patients manifests in the form
hyperactivity, headaches, tremors and autonomic presentations. Lee et al. (2016)
consider the four-item Fast Alcohol Screening Tool (FAST) as the most effective tool
in the process of assessing alcohol withdrawal symptoms among elderly patients.
A review of Mr. Jungala’s case study reveals the manifestation of a wider
range of alcohol withdrawal symptoms. For instance, Mr. Jungala is described as a
social man who reports 2 to 3 mid-strength beers about 2 to 3 times on a weekly
basis. Lappin et al. (2018) recommend that an individual should take no more than
two standard alcoholic drinks on a daily basis. The fact that Mr. Jungala consumes 2
to 3 mid-strength beers about 2 to 3 times on a weekly basis reveals that he is not a
heavy user despite the fact that his daily consumption may be above the
recommended limit. Mr. Jungala considers taking a few drinks as a strategy of
easing the stress associated with his daughter’s recent cancer diagnosis.
Cognitive assessment
Cognitive assessments in clinical settings are conducted with the aim of evaluating
the essential aspects of an individual’s brain function. According to Herath et al.
(2016), effective cognitive assessment calls for proper inclusion of the information
needed to establish the most effective intervention for the patient under
consideration. On the other hand, Lappin et al. (2018) explain that the process aims
at fostering the integration of data gathered from the processes of observing the
client, talking to the assigned carers and from the results acquired from the
assessment tool. As such, the tools applied in cognitive evaluations tend to vet
essential aspects of brain function such as the ability and level of concentration,
memory status, reasoning capabilities, language and processing speed. Morley et al.
(2016) recommend the Wonderlic test as the most effective tool of assessing one’s
cognitive abilities.
Based on the case study, Mr. Jungala does not present with notable
challenges in his cognitive function. However, there is a possibility that stressful
conditions such as his daughter’s recent cancer diagnosis and his position as a
diabetic could expose Mr. Jungala to the vulnerabilities of acquiring cognitive
disorders. According to Clarke et al. (2016), diabetes imposes detrimental effects on
an individual’s cognitive function in the domains of abstract reasoning, memory and
behavioural speed as a result of poor metabolic control and severity of automatic
and peripheral neuropathy.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
3
Part 1: Assessment (1000 words)
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or the purpose of
these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
Alcohol withdrawal risk assessment is considered by Morley et al. (2016) as one of
the most significant steps in fostering early identification of alcohol withdrawal
syndrome. Alcohol withdrawal syndrome encompasses the unpleasant mental and
physical indications that are manifested after alcohol cessation. Such symptoms tend
to deviate from minimal tremors, to hallucinations and in adverse conditions,
convulsions may manifest. Lappin et al. (2018) demystify that repetitive withdrawal
episodes act as essential contributors to the advancement of alcohol dependence,
and the detrimental health consequences associated with drinking. In early stages,
alcohol withdrawal symptom among elderly patients manifests in the form
hyperactivity, headaches, tremors and autonomic presentations. Lee et al. (2016)
consider the four-item Fast Alcohol Screening Tool (FAST) as the most effective tool
in the process of assessing alcohol withdrawal symptoms among elderly patients.
A review of Mr. Jungala’s case study reveals the manifestation of a wider
range of alcohol withdrawal symptoms. For instance, Mr. Jungala is described as a
social man who reports 2 to 3 mid-strength beers about 2 to 3 times on a weekly
basis. Lappin et al. (2018) recommend that an individual should take no more than
two standard alcoholic drinks on a daily basis. The fact that Mr. Jungala consumes 2
to 3 mid-strength beers about 2 to 3 times on a weekly basis reveals that he is not a
heavy user despite the fact that his daily consumption may be above the
recommended limit. Mr. Jungala considers taking a few drinks as a strategy of
easing the stress associated with his daughter’s recent cancer diagnosis.
Cognitive assessment
Cognitive assessments in clinical settings are conducted with the aim of evaluating
the essential aspects of an individual’s brain function. According to Herath et al.
(2016), effective cognitive assessment calls for proper inclusion of the information
needed to establish the most effective intervention for the patient under
consideration. On the other hand, Lappin et al. (2018) explain that the process aims
at fostering the integration of data gathered from the processes of observing the
client, talking to the assigned carers and from the results acquired from the
assessment tool. As such, the tools applied in cognitive evaluations tend to vet
essential aspects of brain function such as the ability and level of concentration,
memory status, reasoning capabilities, language and processing speed. Morley et al.
(2016) recommend the Wonderlic test as the most effective tool of assessing one’s
cognitive abilities.
Based on the case study, Mr. Jungala does not present with notable
challenges in his cognitive function. However, there is a possibility that stressful
conditions such as his daughter’s recent cancer diagnosis and his position as a
diabetic could expose Mr. Jungala to the vulnerabilities of acquiring cognitive
disorders. According to Clarke et al. (2016), diabetes imposes detrimental effects on
an individual’s cognitive function in the domains of abstract reasoning, memory and
behavioural speed as a result of poor metabolic control and severity of automatic
and peripheral neuropathy.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
Falls assessment
Falls assessment plays a significant role in fostering ample examination of the
extents to which a particular patient is exposed to the vulnerabilities of acquiring
injuries derived from falls. According to Ejupi et al. (2016), exposure to walking and
jogging among elderly people increases their risks of falling. On the other hand, the
scholars explain that an increase in an individual’s levels of physical activity
decreases the risk of falls while increasing the risks of being exposed to serious
injuries. Houry et al. (2016) reveal that falls among elderly people aged less than 75
years are highly associated with extrinsic factors. The researchers reveal that the
Morse Fall Scale is widely applied as a simplified and rapid tool of evaluating a
patient’s degree of exposure to the risk of falling based on its position as a less
complicated instrument that takes less than 3 minutes to evaluate a patient.
Mr. Jungala reveals that his fall was as a result of his movements at home.
Following the fall, Mr. Jungala has experienced pains whenever he moves as well as
difficulties in weight bearing. Mr. Jungala’s age is one of the greatest contributors of
the fall he encountered. According to Houry et al. (2016), the natural ageing process
exposes older adults to the vulnerabilities of falls. The researchers explain that falls
are common among older adults who present with other chronic health conditions
such as diabetes and cardiovascular ailments. The fact that Mr. Jungala is diabetic,
hypertensive and suffers from unstable angina reveals his susceptibility to falls.
Functional assessment
Functional assessment proceeds with the aim of assessing a patent’s level of frailty.
Lappin et al. (2018) explain that comprehensive functional assessments are
conducted to determine the efficacy of the present and future healthcare needs of a
frail patient. According to Ejupi et al. (2016), frailty is a common phenomenon
presented by older adults which interferes with their cognitive and physical attributes.
The researchers explain that older adults residing outside healthcare institutions
must be availed with necessary assistances when undertaking heir day to day
activities whenever they are faced with cognitive deterioration and/or decrements in
their levels of outside mobility. Geriatric assessment is considered by Ejupi et al.
(2016) as one of the most effective tools of evaluating a patient’s level of cognitive
function as it inculcates a multidisciplinary approach.
Mr. Jungala presents with conditions such as reluctance in his attempts of
walking as a result of the pain felt, decreased hip movements, and blue/red
hematoma on the right hip that extends to the buttock region. According to Stone et
al. (2015), most of the frail elderly patients present with multiple health care needs.
For instance, Mr. Jungala is diabetic, hypertensive and suffers from unstable angina.
Such conditions act as active contributors to the patient’s current state.
Nutritional assessment
Nutritional assessment proceeds with the aim of conducting a broad analysis of the
objective and subjective clinical information on the efficacy of an individual’s dietary
intakes, medication, and lifestyle. Lappin et al. (2018) explain that the consumption
of a well balanced diet plays a significant role in helping elder adults to remain
healthy as they age. However, poor nutrition eposes older patients to the
vulnerabilities of chronic health conditions such as cardiovascular diseases, and
diabetes. The ‘Malnutrition Universal Screening Tool’ is widely applied as an
instrument of undertaking nutritional assessments based on its efficacy as a reliable,
valid and easy to apply equipment in clinical settings.
Mr. Jungala’s medical history reveals that the patient is restricted to a diabetic
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
4
Falls assessment
Falls assessment plays a significant role in fostering ample examination of the
extents to which a particular patient is exposed to the vulnerabilities of acquiring
injuries derived from falls. According to Ejupi et al. (2016), exposure to walking and
jogging among elderly people increases their risks of falling. On the other hand, the
scholars explain that an increase in an individual’s levels of physical activity
decreases the risk of falls while increasing the risks of being exposed to serious
injuries. Houry et al. (2016) reveal that falls among elderly people aged less than 75
years are highly associated with extrinsic factors. The researchers reveal that the
Morse Fall Scale is widely applied as a simplified and rapid tool of evaluating a
patient’s degree of exposure to the risk of falling based on its position as a less
complicated instrument that takes less than 3 minutes to evaluate a patient.
Mr. Jungala reveals that his fall was as a result of his movements at home.
Following the fall, Mr. Jungala has experienced pains whenever he moves as well as
difficulties in weight bearing. Mr. Jungala’s age is one of the greatest contributors of
the fall he encountered. According to Houry et al. (2016), the natural ageing process
exposes older adults to the vulnerabilities of falls. The researchers explain that falls
are common among older adults who present with other chronic health conditions
such as diabetes and cardiovascular ailments. The fact that Mr. Jungala is diabetic,
hypertensive and suffers from unstable angina reveals his susceptibility to falls.
Functional assessment
Functional assessment proceeds with the aim of assessing a patent’s level of frailty.
Lappin et al. (2018) explain that comprehensive functional assessments are
conducted to determine the efficacy of the present and future healthcare needs of a
frail patient. According to Ejupi et al. (2016), frailty is a common phenomenon
presented by older adults which interferes with their cognitive and physical attributes.
The researchers explain that older adults residing outside healthcare institutions
must be availed with necessary assistances when undertaking heir day to day
activities whenever they are faced with cognitive deterioration and/or decrements in
their levels of outside mobility. Geriatric assessment is considered by Ejupi et al.
(2016) as one of the most effective tools of evaluating a patient’s level of cognitive
function as it inculcates a multidisciplinary approach.
Mr. Jungala presents with conditions such as reluctance in his attempts of
walking as a result of the pain felt, decreased hip movements, and blue/red
hematoma on the right hip that extends to the buttock region. According to Stone et
al. (2015), most of the frail elderly patients present with multiple health care needs.
For instance, Mr. Jungala is diabetic, hypertensive and suffers from unstable angina.
Such conditions act as active contributors to the patient’s current state.
Nutritional assessment
Nutritional assessment proceeds with the aim of conducting a broad analysis of the
objective and subjective clinical information on the efficacy of an individual’s dietary
intakes, medication, and lifestyle. Lappin et al. (2018) explain that the consumption
of a well balanced diet plays a significant role in helping elder adults to remain
healthy as they age. However, poor nutrition eposes older patients to the
vulnerabilities of chronic health conditions such as cardiovascular diseases, and
diabetes. The ‘Malnutrition Universal Screening Tool’ is widely applied as an
instrument of undertaking nutritional assessments based on its efficacy as a reliable,
valid and easy to apply equipment in clinical settings.
Mr. Jungala’s medical history reveals that the patient is restricted to a diabetic
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

NUR341 Assessment 2
diet. On the other hand, there are tendencies that the patient likes consuming junks.
Such a notion is attributed to the fact that Mr. Jungala was going to the kitchen to
make a sandwich on the day when he encountered the fall. Lappin et al. (2018)
explain that poor nutrition and lack of enough physical exercise among adult patients
are the major causes of health problems among elderly patients.
Part 2: Plan and implementation (500 words)
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and medications may have
contributed to his fall. Choose one factor and outline your nursing actions and referrals you would
execute; include rationales for same.
Mr. Jungala’s care plan will be customized to meet his healthcare needs as an
inpatient. A diabetes care plan will be initiated with the aim of ensuring that Mr.
Jungala’s blood sugar level is maintained while encouraging the patient to participate
in physical activity. According to Houry et al. (2016), effective adoption of diabetes
care plans plays a significant role in ensuring that patients are well guided to their
food intake and physical exercise schedules while providing a greater control of their
self-care. Considering Mr. Jungala’s economic position, a diabetes care pathway will
be initiated to foster the provision of better care services at a reduced cost. As a
consequence, Mr. Jungala will be exposed to a strict diabetic diet with physical
exercise to manage his condition. Makizako et al. (2015) explain that care pathways
play a significant role in improving patient outcomes at a reduced cost by allowing for
timely decision-making, escalation of remedies, and appropriate follow-up. Specific
to the patient’s hypertensive condition will be the institutionalization of lifestyle
modifications. Feinkohl et al. (2015) explain that poor eating behaviours, stress, and
lack of physical exercise act as significant contributors to hypertensive conditions. As
such, Mr. Jungala’s care plan will include regular physical exercises in the form of
walking, reducing the levels of intake of alcoholic drinks, increasing the intake of
potassium rich foods, reducing caffeine intake, and learning the most effective
strategies of managing the stressful vents presented by her daughter’s recent
diagnosis with cancer. Specific to Mr. Jungala’s chronic renal failure will be an
intensive glycemic control aimed at delaying the advancement of micro-albuminuria.
According to Feinkohl et al. (2015), intensive glycemic control plays a significant role
in establishing a balance with the challenges associated severe blood sugar levels.
The care plan will play a central role in fostering effective patient centred care with
the inclusion of a multidisciplinary perspective.
The care plan will heavily rely on referrals targeting an occupational therapist,
a nutritionist, and an optometrist. The nutritionist will be incorporated to assess the
client’s nutritional requirements while developing the most effective food plan for Mr.
Jungala. According to Lee et al. (2016), nutritionists must establish a collaborative
framework with physicians and the assigned carers to ensure that the meal plans
advanced meet the medical and nutritional needs of the patient. However, an
optometrist will be included in Mr. Jungala’s care plan to avail the patient with eye
care. According to Herath et al. (2016), optometrists play a significant role in
fostering vision training and correction. An occupational therapist will be incorporated
in Mr. Jungala’s care plan to guide him in his efforts of improving his ability to
undertake tasks. Lastly, a social worker will be included to ensure that Mr. Jungala is
presented with an ample coping environment to manage his stress and anxieties.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
5
diet. On the other hand, there are tendencies that the patient likes consuming junks.
Such a notion is attributed to the fact that Mr. Jungala was going to the kitchen to
make a sandwich on the day when he encountered the fall. Lappin et al. (2018)
explain that poor nutrition and lack of enough physical exercise among adult patients
are the major causes of health problems among elderly patients.
Part 2: Plan and implementation (500 words)
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and medications may have
contributed to his fall. Choose one factor and outline your nursing actions and referrals you would
execute; include rationales for same.
Mr. Jungala’s care plan will be customized to meet his healthcare needs as an
inpatient. A diabetes care plan will be initiated with the aim of ensuring that Mr.
Jungala’s blood sugar level is maintained while encouraging the patient to participate
in physical activity. According to Houry et al. (2016), effective adoption of diabetes
care plans plays a significant role in ensuring that patients are well guided to their
food intake and physical exercise schedules while providing a greater control of their
self-care. Considering Mr. Jungala’s economic position, a diabetes care pathway will
be initiated to foster the provision of better care services at a reduced cost. As a
consequence, Mr. Jungala will be exposed to a strict diabetic diet with physical
exercise to manage his condition. Makizako et al. (2015) explain that care pathways
play a significant role in improving patient outcomes at a reduced cost by allowing for
timely decision-making, escalation of remedies, and appropriate follow-up. Specific
to the patient’s hypertensive condition will be the institutionalization of lifestyle
modifications. Feinkohl et al. (2015) explain that poor eating behaviours, stress, and
lack of physical exercise act as significant contributors to hypertensive conditions. As
such, Mr. Jungala’s care plan will include regular physical exercises in the form of
walking, reducing the levels of intake of alcoholic drinks, increasing the intake of
potassium rich foods, reducing caffeine intake, and learning the most effective
strategies of managing the stressful vents presented by her daughter’s recent
diagnosis with cancer. Specific to Mr. Jungala’s chronic renal failure will be an
intensive glycemic control aimed at delaying the advancement of micro-albuminuria.
According to Feinkohl et al. (2015), intensive glycemic control plays a significant role
in establishing a balance with the challenges associated severe blood sugar levels.
The care plan will play a central role in fostering effective patient centred care with
the inclusion of a multidisciplinary perspective.
The care plan will heavily rely on referrals targeting an occupational therapist,
a nutritionist, and an optometrist. The nutritionist will be incorporated to assess the
client’s nutritional requirements while developing the most effective food plan for Mr.
Jungala. According to Lee et al. (2016), nutritionists must establish a collaborative
framework with physicians and the assigned carers to ensure that the meal plans
advanced meet the medical and nutritional needs of the patient. However, an
optometrist will be included in Mr. Jungala’s care plan to avail the patient with eye
care. According to Herath et al. (2016), optometrists play a significant role in
fostering vision training and correction. An occupational therapist will be incorporated
in Mr. Jungala’s care plan to guide him in his efforts of improving his ability to
undertake tasks. Lastly, a social worker will be included to ensure that Mr. Jungala is
presented with an ample coping environment to manage his stress and anxieties.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
5
NUR341 Assessment 2
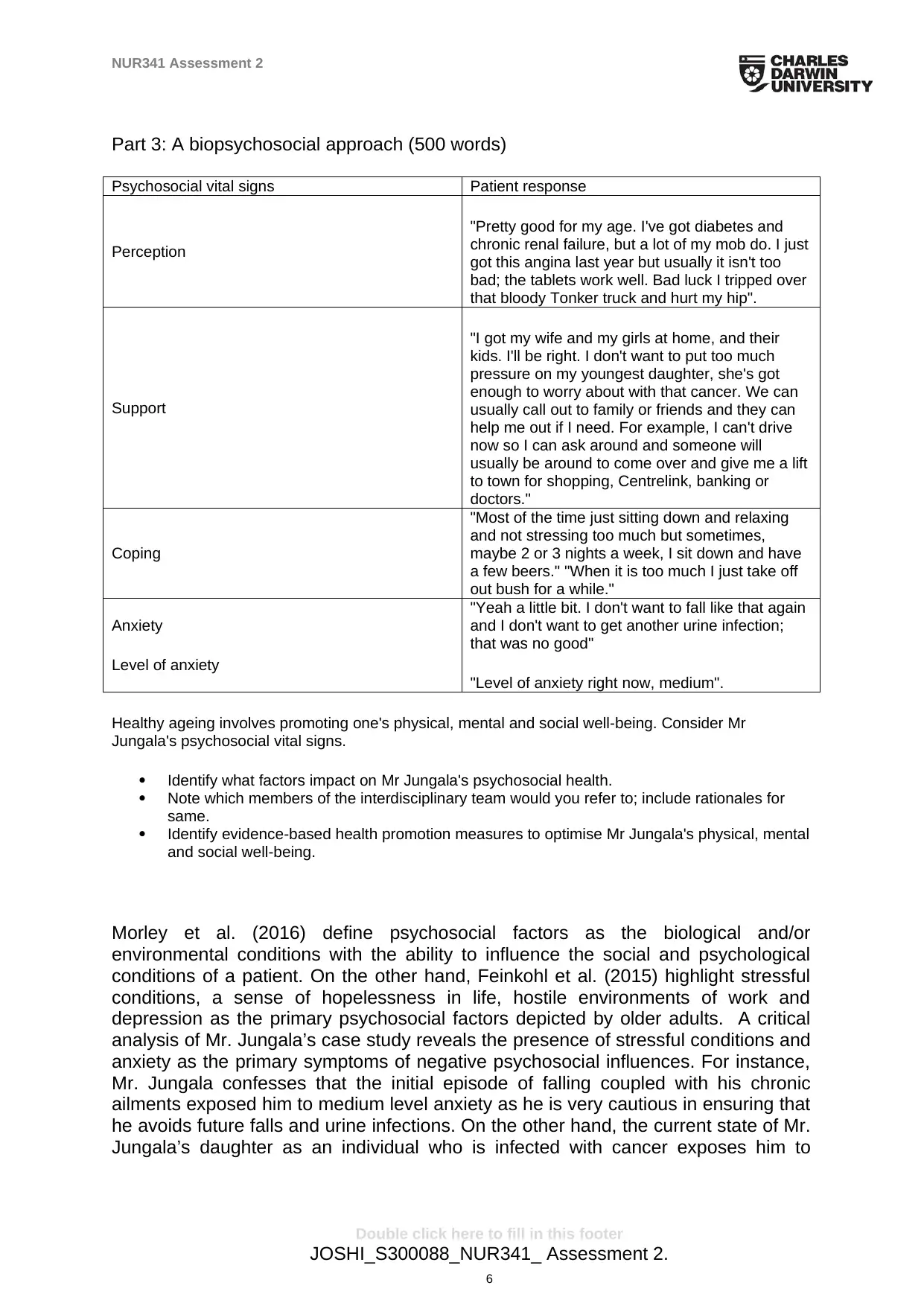
Part 3: A biopsychosocial approach (500 words)
Psychosocial vital signs Patient response
Perception
"Pretty good for my age. I've got diabetes and
chronic renal failure, but a lot of my mob do. I just
got this angina last year but usually it isn't too
bad; the tablets work well. Bad luck I tripped over
that bloody Tonker truck and hurt my hip".
Support
"I got my wife and my girls at home, and their
kids. I'll be right. I don't want to put too much
pressure on my youngest daughter, she's got
enough to worry about with that cancer. We can
usually call out to family or friends and they can
help me out if I need. For example, I can't drive
now so I can ask around and someone will
usually be around to come over and give me a lift
to town for shopping, Centrelink, banking or
doctors."
Coping
"Most of the time just sitting down and relaxing
and not stressing too much but sometimes,
maybe 2 or 3 nights a week, I sit down and have
a few beers." "When it is too much I just take off
out bush for a while."
Anxiety
Level of anxiety
"Yeah a little bit. I don't want to fall like that again
and I don't want to get another urine infection;
that was no good"
"Level of anxiety right now, medium".
Healthy ageing involves promoting one's physical, mental and social well-being. Consider Mr
Jungala's psychosocial vital signs.
Identify what factors impact on Mr Jungala's psychosocial health.
Note which members of the interdisciplinary team would you refer to; include rationales for
same.
Identify evidence-based health promotion measures to optimise Mr Jungala's physical, mental
and social well-being.
Morley et al. (2016) define psychosocial factors as the biological and/or
environmental conditions with the ability to influence the social and psychological
conditions of a patient. On the other hand, Feinkohl et al. (2015) highlight stressful
conditions, a sense of hopelessness in life, hostile environments of work and
depression as the primary psychosocial factors depicted by older adults. A critical
analysis of Mr. Jungala’s case study reveals the presence of stressful conditions and
anxiety as the primary symptoms of negative psychosocial influences. For instance,
Mr. Jungala confesses that the initial episode of falling coupled with his chronic
ailments exposed him to medium level anxiety as he is very cautious in ensuring that
he avoids future falls and urine infections. On the other hand, the current state of Mr.
Jungala’s daughter as an individual who is infected with cancer exposes him to
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
6
Part 3: A biopsychosocial approach (500 words)
Psychosocial vital signs Patient response
Perception
"Pretty good for my age. I've got diabetes and
chronic renal failure, but a lot of my mob do. I just
got this angina last year but usually it isn't too
bad; the tablets work well. Bad luck I tripped over
that bloody Tonker truck and hurt my hip".
Support
"I got my wife and my girls at home, and their
kids. I'll be right. I don't want to put too much
pressure on my youngest daughter, she's got
enough to worry about with that cancer. We can
usually call out to family or friends and they can
help me out if I need. For example, I can't drive
now so I can ask around and someone will
usually be around to come over and give me a lift
to town for shopping, Centrelink, banking or
doctors."
Coping
"Most of the time just sitting down and relaxing
and not stressing too much but sometimes,
maybe 2 or 3 nights a week, I sit down and have
a few beers." "When it is too much I just take off
out bush for a while."
Anxiety
Level of anxiety
"Yeah a little bit. I don't want to fall like that again
and I don't want to get another urine infection;
that was no good"
"Level of anxiety right now, medium".
Healthy ageing involves promoting one's physical, mental and social well-being. Consider Mr
Jungala's psychosocial vital signs.
Identify what factors impact on Mr Jungala's psychosocial health.
Note which members of the interdisciplinary team would you refer to; include rationales for
same.
Identify evidence-based health promotion measures to optimise Mr Jungala's physical, mental
and social well-being.
Morley et al. (2016) define psychosocial factors as the biological and/or
environmental conditions with the ability to influence the social and psychological
conditions of a patient. On the other hand, Feinkohl et al. (2015) highlight stressful
conditions, a sense of hopelessness in life, hostile environments of work and
depression as the primary psychosocial factors depicted by older adults. A critical
analysis of Mr. Jungala’s case study reveals the presence of stressful conditions and
anxiety as the primary symptoms of negative psychosocial influences. For instance,
Mr. Jungala confesses that the initial episode of falling coupled with his chronic
ailments exposed him to medium level anxiety as he is very cautious in ensuring that
he avoids future falls and urine infections. On the other hand, the current state of Mr.
Jungala’s daughter as an individual who is infected with cancer exposes him to
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
stressful moments. The patient considers taking a few drinks as a strategy of easing
the stress associated with his daughter’s recent cancer diagnosis. Despite the
negative effects presented by Mr. Jungala’s environment, the client considers his
family and friends as a major source of strength. For instance, Mr. Jungala finds
solace from the fact that most of his friends suffer from similar ailments such as
chronic renal failures and diabetes. Similarly, the patient boasts of the supportive
environment provided by his wife, children, grandchildren and friends. The
presences of such positive social ties have played an effective role in ensuring that
Mr. Jungala is presented with an enabling environment.
Mr. Jungala will be referred to a social worker and an occupational therapist
as the primary members of the interdisciplinary team to offer ample guidance and
interventions for his psychosocial challenges. Stone et al. (2015) explain that there
are tendencies that some injuries incurred may act as significant contributors to the
stressful conditions experienced by elderly patients. Such a premise explains the
importance of including an occupational therapist in the treatment plan of Mr.
Jungala. However, the scholars reveal that some psychosocial challenges occur as a
result of the detrimental factors presented by a patient’s social environment. A critical
analysis of Mr. Jungala’s condition reveals that her daughter’s recent diagnosis of
cancer has played an active role in increasing his anxieties. As such, a social worker
will be incorporated to avail the most effective coping mechanisms aimed at
minimizing alcohol use.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
7
stressful moments. The patient considers taking a few drinks as a strategy of easing
the stress associated with his daughter’s recent cancer diagnosis. Despite the
negative effects presented by Mr. Jungala’s environment, the client considers his
family and friends as a major source of strength. For instance, Mr. Jungala finds
solace from the fact that most of his friends suffer from similar ailments such as
chronic renal failures and diabetes. Similarly, the patient boasts of the supportive
environment provided by his wife, children, grandchildren and friends. The
presences of such positive social ties have played an effective role in ensuring that
Mr. Jungala is presented with an enabling environment.
Mr. Jungala will be referred to a social worker and an occupational therapist
as the primary members of the interdisciplinary team to offer ample guidance and
interventions for his psychosocial challenges. Stone et al. (2015) explain that there
are tendencies that some injuries incurred may act as significant contributors to the
stressful conditions experienced by elderly patients. Such a premise explains the
importance of including an occupational therapist in the treatment plan of Mr.
Jungala. However, the scholars reveal that some psychosocial challenges occur as a
result of the detrimental factors presented by a patient’s social environment. A critical
analysis of Mr. Jungala’s condition reveals that her daughter’s recent diagnosis of
cancer has played an active role in increasing his anxieties. As such, a social worker
will be incorporated to avail the most effective coping mechanisms aimed at
minimizing alcohol use.
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
References
Clarke, J., Proudfoot, J., & Ma, H. (2016). Mobile Phone and Web-based
Cognitive Behavior Therapy for Depressive Symptoms and Mental
Health Comorbidities in People Living With Diabetes: Results of a
Feasibility Study. JMIR Mental Health, 3(2), e23. doi: 10.2196/mental.5131
Ejupi, A., Gschwind, Y., Brodie, M., Zagler, W., Lord, S., & Delbaere, K. (2016).
Kinect-based choice reaching and stepping reaction time tests for
clinical and in-home assessment of fall risk in older people: a
prospective study. European Review Of Aging And Physical Activity,
13(1). doi: 10.1186/s11556-016-0162-2
Feinkohl, I., Price, J., Strachan, M., & Frier, B. (2015). The impact of diabetes
on cognitive decline: potential vascular, metabolic, and psychosocial
risk factors. Alzheimer's Research & Therapy, 7(1). doi: 10.1186/s13195-
015-0130-5
Herath, P., Cherbuin, N., Eramudugolla, R., & Anstey, K. (2016). The Effect of
Diabetes Medication on Cognitive Function: Evidence from the PATH
Through Life Study. Biomed Research International, 2016, 1-7. doi:
10.1155/2016/7208429
Houry, D., Florence, C., Baldwin, G., Stevens, J., & McClure, R. (2015). The
CDC Injury Center’s Response to the Growing Public Health Problem of
Falls Among Older Adults. American Journal Of Lifestyle Medicine,
10(1), 74-77. doi: 10.1177/1559827615600137
Lappin, J., Ayub, M., Rogers, D., Morgan, M., Kanyamibwa, J., & Shakeshaft, A.
(2018). Routine screening and related interventions significantly
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
8
References
Clarke, J., Proudfoot, J., & Ma, H. (2016). Mobile Phone and Web-based
Cognitive Behavior Therapy for Depressive Symptoms and Mental
Health Comorbidities in People Living With Diabetes: Results of a
Feasibility Study. JMIR Mental Health, 3(2), e23. doi: 10.2196/mental.5131
Ejupi, A., Gschwind, Y., Brodie, M., Zagler, W., Lord, S., & Delbaere, K. (2016).
Kinect-based choice reaching and stepping reaction time tests for
clinical and in-home assessment of fall risk in older people: a
prospective study. European Review Of Aging And Physical Activity,
13(1). doi: 10.1186/s11556-016-0162-2
Feinkohl, I., Price, J., Strachan, M., & Frier, B. (2015). The impact of diabetes
on cognitive decline: potential vascular, metabolic, and psychosocial
risk factors. Alzheimer's Research & Therapy, 7(1). doi: 10.1186/s13195-
015-0130-5
Herath, P., Cherbuin, N., Eramudugolla, R., & Anstey, K. (2016). The Effect of
Diabetes Medication on Cognitive Function: Evidence from the PATH
Through Life Study. Biomed Research International, 2016, 1-7. doi:
10.1155/2016/7208429
Houry, D., Florence, C., Baldwin, G., Stevens, J., & McClure, R. (2015). The
CDC Injury Center’s Response to the Growing Public Health Problem of
Falls Among Older Adults. American Journal Of Lifestyle Medicine,
10(1), 74-77. doi: 10.1177/1559827615600137
Lappin, J., Ayub, M., Rogers, D., Morgan, M., Kanyamibwa, J., & Shakeshaft, A.
(2018). Routine screening and related interventions significantly
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
8
NUR341 Assessment 2
improve the effectiveness of emergency department detection and
management of alcohol withdrawal syndrome. Emergency Medicine
Australasia, 30(5), 648-653. doi: 10.1111/1742-6723.12959
Lee, H., Ruggoo, V., & Graudins, A. (2015). Intrathecal Clonidine Pump Failure
Causing Acute Withdrawal Syndrome With ‘Stress-Induced’
Cardiomyopathy. Journal Of Medical Toxicology, 12(1), 134-138. doi:
10.1007/s13181-015-0505-9
Makizako, H., Shimada, H., Tsutsumimoto, K., Lee, S., Doi, T., & Nakakubo, S.
et al. (2015). Social Frailty in Community-Dwelling Older Adults as a Risk
Factor for Disability. Journal Of The American Medical Directors
Association, 16(11), 1003.e7-1003.e11. doi: 10.1016/j.jamda.2015.08.023
Morley, K., Logge, W., Pearson, S., Baillie, A., & Haber, P. (2016). National
trends in alcohol pharmacotherapy: Findings from an Australian claims
database. Drug And Alcohol Dependence, 166, 254-257. doi:
10.1016/j.drugalcdep.2016.06.027
Stone, E., Skubic, M., Rantz, M., Abbott, C., & Miller, S. (2015). Average in-home
gait speed: Investigation of a new metric for mobility and fall risk
assessment of elders. Gait & Posture, 41(1), 57-62. doi:
10.1016/j.gaitpost.2014.08.019
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
9
improve the effectiveness of emergency department detection and
management of alcohol withdrawal syndrome. Emergency Medicine
Australasia, 30(5), 648-653. doi: 10.1111/1742-6723.12959
Lee, H., Ruggoo, V., & Graudins, A. (2015). Intrathecal Clonidine Pump Failure
Causing Acute Withdrawal Syndrome With ‘Stress-Induced’
Cardiomyopathy. Journal Of Medical Toxicology, 12(1), 134-138. doi:
10.1007/s13181-015-0505-9
Makizako, H., Shimada, H., Tsutsumimoto, K., Lee, S., Doi, T., & Nakakubo, S.
et al. (2015). Social Frailty in Community-Dwelling Older Adults as a Risk
Factor for Disability. Journal Of The American Medical Directors
Association, 16(11), 1003.e7-1003.e11. doi: 10.1016/j.jamda.2015.08.023
Morley, K., Logge, W., Pearson, S., Baillie, A., & Haber, P. (2016). National
trends in alcohol pharmacotherapy: Findings from an Australian claims
database. Drug And Alcohol Dependence, 166, 254-257. doi:
10.1016/j.drugalcdep.2016.06.027
Stone, E., Skubic, M., Rantz, M., Abbott, C., & Miller, S. (2015). Average in-home
gait speed: Investigation of a new metric for mobility and fall risk
assessment of elders. Gait & Posture, 41(1), 57-62. doi:
10.1016/j.gaitpost.2014.08.019
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
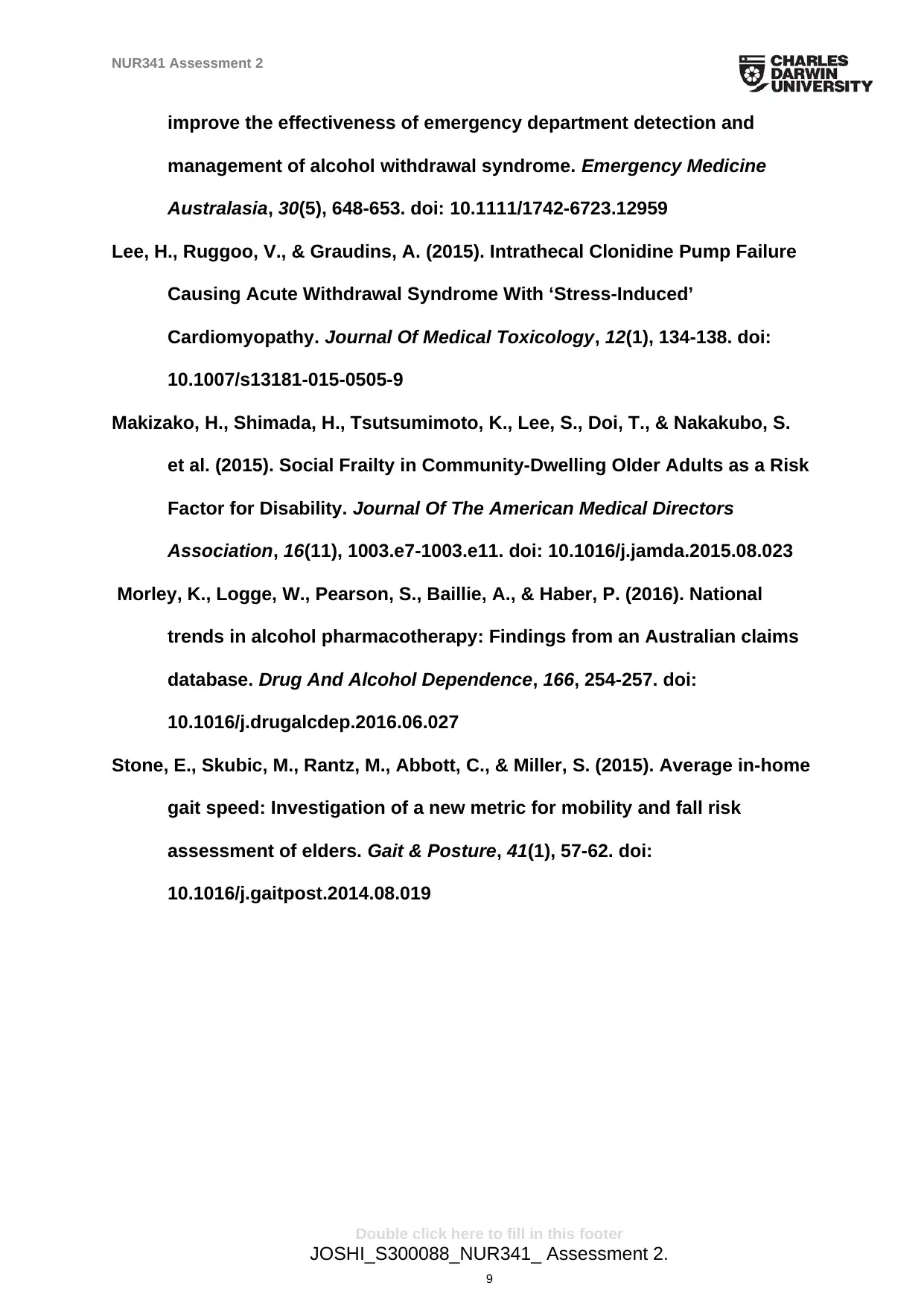
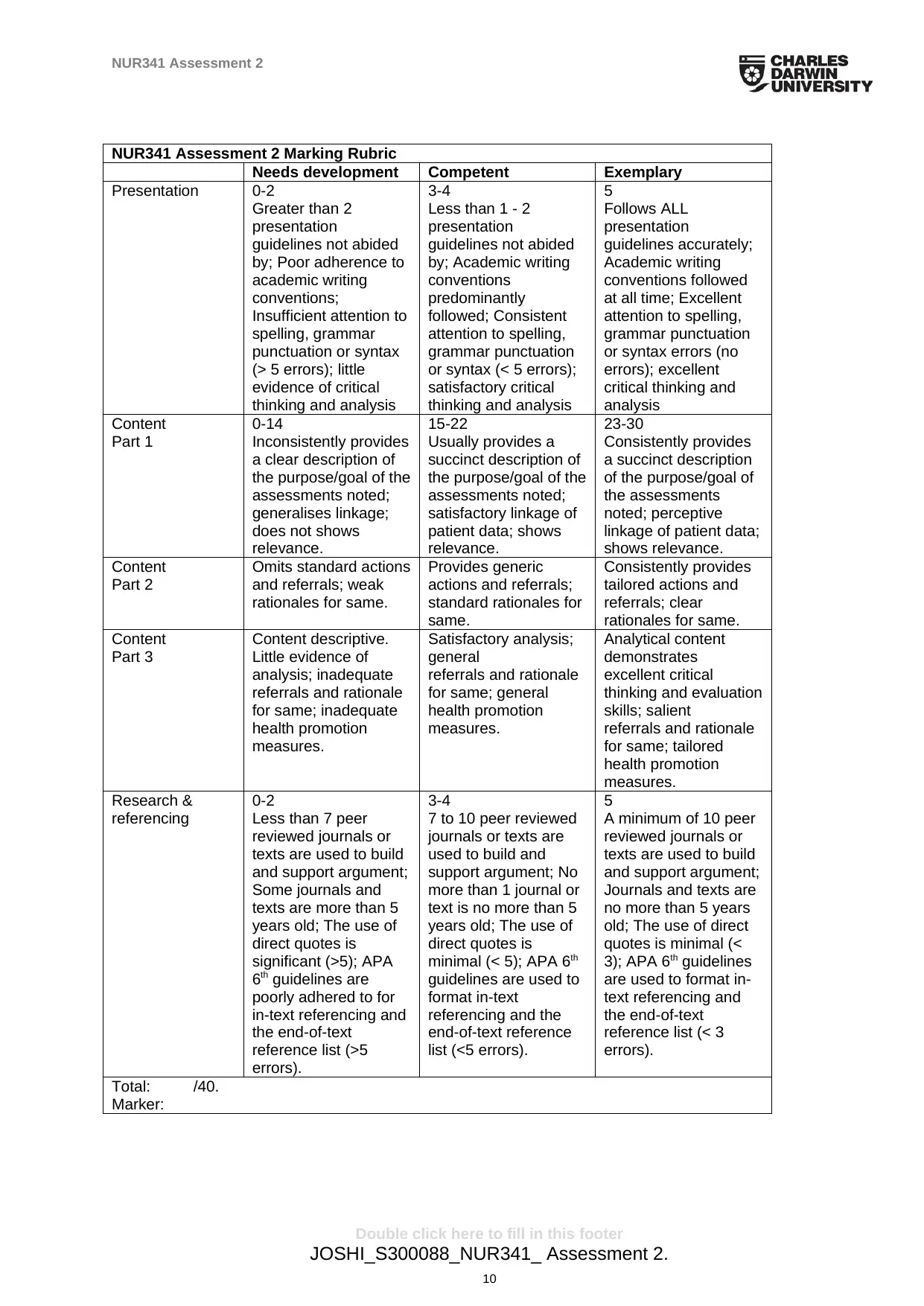
NUR341 Assessment 2 Marking Rubric
Needs development Competent Exemplary
Presentation 0-2
Greater than 2
presentation
guidelines not abided
by; Poor adherence to
academic writing
conventions;
Insufficient attention to
spelling, grammar
punctuation or syntax
(> 5 errors); little
evidence of critical
thinking and analysis
3-4
Less than 1 - 2
presentation
guidelines not abided
by; Academic writing
conventions
predominantly
followed; Consistent
attention to spelling,
grammar punctuation
or syntax (< 5 errors);
satisfactory critical
thinking and analysis
5
Follows ALL
presentation
guidelines accurately;
Academic writing
conventions followed
at all time; Excellent
attention to spelling,
grammar punctuation
or syntax errors (no
errors); excellent
critical thinking and
analysis
Content
Part 1
0-14
Inconsistently provides
a clear description of
the purpose/goal of the
assessments noted;
generalises linkage;
does not shows
relevance.
15-22
Usually provides a
succinct description of
the purpose/goal of the
assessments noted;
satisfactory linkage of
patient data; shows
relevance.
23-30
Consistently provides
a succinct description
of the purpose/goal of
the assessments
noted; perceptive
linkage of patient data;
shows relevance.
Content
Part 2
Omits standard actions
and referrals; weak
rationales for same.
Provides generic
actions and referrals;
standard rationales for
same.
Consistently provides
tailored actions and
referrals; clear
rationales for same.
Content
Part 3
Content descriptive.
Little evidence of
analysis; inadequate
referrals and rationale
for same; inadequate
health promotion
measures.
Satisfactory analysis;
general
referrals and rationale
for same; general
health promotion
measures.
Analytical content
demonstrates
excellent critical
thinking and evaluation
skills; salient
referrals and rationale
for same; tailored
health promotion
measures.
Research &
referencing
0-2
Less than 7 peer
reviewed journals or
texts are used to build
and support argument;
Some journals and
texts are more than 5
years old; The use of
direct quotes is
significant (>5); APA
6th guidelines are
poorly adhered to for
in-text referencing and
the end-of-text
reference list (>5
errors).
3-4
7 to 10 peer reviewed
journals or texts are
used to build and
support argument; No
more than 1 journal or
text is no more than 5
years old; The use of
direct quotes is
minimal (< 5); APA 6th
guidelines are used to
format in-text
referencing and the
end-of-text reference
list (<5 errors).
5
A minimum of 10 peer
reviewed journals or
texts are used to build
and support argument;
Journals and texts are
no more than 5 years
old; The use of direct
quotes is minimal (<
3); APA 6th guidelines
are used to format in-
text referencing and
the end-of-text
reference list (< 3
errors).
Total: /40.
Marker:
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
10
NUR341 Assessment 2 Marking Rubric
Needs development Competent Exemplary
Presentation 0-2
Greater than 2
presentation
guidelines not abided
by; Poor adherence to
academic writing
conventions;
Insufficient attention to
spelling, grammar
punctuation or syntax
(> 5 errors); little
evidence of critical
thinking and analysis
3-4
Less than 1 - 2
presentation
guidelines not abided
by; Academic writing
conventions
predominantly
followed; Consistent
attention to spelling,
grammar punctuation
or syntax (< 5 errors);
satisfactory critical
thinking and analysis
5
Follows ALL
presentation
guidelines accurately;
Academic writing
conventions followed
at all time; Excellent
attention to spelling,
grammar punctuation
or syntax errors (no
errors); excellent
critical thinking and
analysis
Content
Part 1
0-14
Inconsistently provides
a clear description of
the purpose/goal of the
assessments noted;
generalises linkage;
does not shows
relevance.
15-22
Usually provides a
succinct description of
the purpose/goal of the
assessments noted;
satisfactory linkage of
patient data; shows
relevance.
23-30
Consistently provides
a succinct description
of the purpose/goal of
the assessments
noted; perceptive
linkage of patient data;
shows relevance.
Content
Part 2
Omits standard actions
and referrals; weak
rationales for same.
Provides generic
actions and referrals;
standard rationales for
same.
Consistently provides
tailored actions and
referrals; clear
rationales for same.
Content
Part 3
Content descriptive.
Little evidence of
analysis; inadequate
referrals and rationale
for same; inadequate
health promotion
measures.
Satisfactory analysis;
general
referrals and rationale
for same; general
health promotion
measures.
Analytical content
demonstrates
excellent critical
thinking and evaluation
skills; salient
referrals and rationale
for same; tailored
health promotion
measures.
Research &
referencing
0-2
Less than 7 peer
reviewed journals or
texts are used to build
and support argument;
Some journals and
texts are more than 5
years old; The use of
direct quotes is
significant (>5); APA
6th guidelines are
poorly adhered to for
in-text referencing and
the end-of-text
reference list (>5
errors).
3-4
7 to 10 peer reviewed
journals or texts are
used to build and
support argument; No
more than 1 journal or
text is no more than 5
years old; The use of
direct quotes is
minimal (< 5); APA 6th
guidelines are used to
format in-text
referencing and the
end-of-text reference
list (<5 errors).
5
A minimum of 10 peer
reviewed journals or
texts are used to build
and support argument;
Journals and texts are
no more than 5 years
old; The use of direct
quotes is minimal (<
3); APA 6th guidelines
are used to format in-
text referencing and
the end-of-text
reference list (< 3
errors).
Total: /40.
Marker:
Double click here to fill in this footer
JOSHI_S300088_NUR341_ Assessment 2.
10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



