Case Study: Acute Severe Asthma - Health Variations 3, Spring 2018
VerifiedAdded on 2023/06/03
|9
|2109
|319
Case Study
AI Summary
This case study provides a comprehensive analysis of acute severe asthma, exploring its causes, pathogenesis, clinical manifestations, and management strategies. It delves into the inflammatory processes and environmental factors contributing to asthma, highlighting the significance of clinical examinations, diagnostic procedures, and potential complications. The study further outlines high-priority nursing strategies for diagnosing and managing asthma, emphasizing the importance of clinical history, allergy analysis, and differential diagnoses. It details the pharmacological interventions, including bronchodilators and corticosteroids, and immediate management protocols for acute severe asthma, stressing the necessity of maintaining oxygen saturation and administering appropriate medications while monitoring patient progress. The case study concludes by referencing relevant research, offering a thorough understanding of acute severe asthma and its clinical management.
Running head: CASE STUDY: ACUTE SEVERE ASTHMA 1
Case study: acute severe asthma
Name:
Institution:
Case study: acute severe asthma
Name:
Institution:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
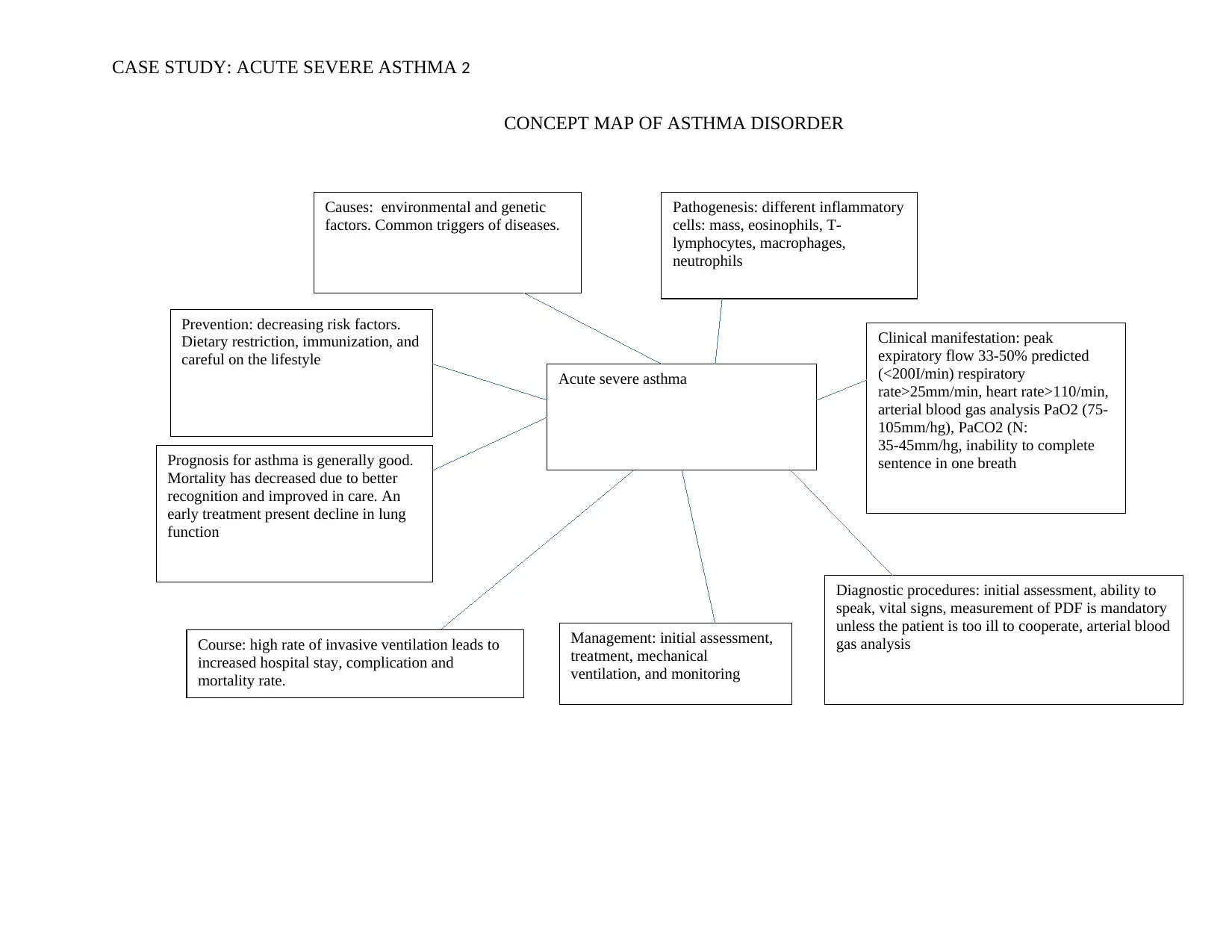
Acute severe asthma
Clinical manifestation: peak
expiratory flow 33-50% predicted
(<200I/min) respiratory
rate>25mm/min, heart rate>110/min,
arterial blood gas analysis PaO2 (75-
105mm/hg), PaCO2 (N:
35-45mm/hg, inability to complete
sentence in one breath
Diagnostic procedures: initial assessment, ability to
speak, vital signs, measurement of PDF is mandatory
unless the patient is too ill to cooperate, arterial blood
gas analysis
Pathogenesis: different inflammatory
cells: mass, eosinophils, T-
lymphocytes, macrophages,
neutrophils
Causes: environmental and genetic
factors. Common triggers of diseases.
Prevention: decreasing risk factors.
Dietary restriction, immunization, and
careful on the lifestyle
Prognosis for asthma is generally good.
Mortality has decreased due to better
recognition and improved in care. An
early treatment present decline in lung
function
Course: high rate of invasive ventilation leads to
increased hospital stay, complication and
mortality rate.
Management: initial assessment,
treatment, mechanical
ventilation, and monitoring
CASE STUDY: ACUTE SEVERE ASTHMA 2
CONCEPT MAP OF ASTHMA DISORDER
Clinical manifestation: peak
expiratory flow 33-50% predicted
(<200I/min) respiratory
rate>25mm/min, heart rate>110/min,
arterial blood gas analysis PaO2 (75-
105mm/hg), PaCO2 (N:
35-45mm/hg, inability to complete
sentence in one breath
Diagnostic procedures: initial assessment, ability to
speak, vital signs, measurement of PDF is mandatory
unless the patient is too ill to cooperate, arterial blood
gas analysis
Pathogenesis: different inflammatory
cells: mass, eosinophils, T-
lymphocytes, macrophages,
neutrophils
Causes: environmental and genetic
factors. Common triggers of diseases.
Prevention: decreasing risk factors.
Dietary restriction, immunization, and
careful on the lifestyle
Prognosis for asthma is generally good.
Mortality has decreased due to better
recognition and improved in care. An
early treatment present decline in lung
function
Course: high rate of invasive ventilation leads to
increased hospital stay, complication and
mortality rate.
Management: initial assessment,
treatment, mechanical
ventilation, and monitoring
CASE STUDY: ACUTE SEVERE ASTHMA 2
CONCEPT MAP OF ASTHMA DISORDER
CASE STUDY: ACUTE SEVERE ASTHMA 3
Question 1
Asthma is a common prolonged syndrome of the lung air route that comprises a sophisticated link of airflow block, bronchial
hyperresponsiveness and an underlying infection. The illness can extremely vary on different patients. Prolonged signs of disease can
arise from bronchospasm or patient’s reaction during the bronchodilator treatment. Chronic and acute tenderness can upset the air
corridor capacity, airflow and also fundamental bronchial hyperresponsiveness, which improves vulnerability to bronchospasm. Thus,
asthma is a long-lasting inflammatory illness of an airway in which numerous cells and cellular features play a role, specifically;
eosinophils, mast cells, T lymphocytes, neutrophils, macrophages, and epithelial cells. This swelling causes regular incidents of
breathlessness, coughing, and stiffness of chest. Hence, the events are linked with extensive but mutable airflow hitch that is
commonly flexible either with treatment or spontaneously (Carr, Berdnikovs, Simon, Bochner & Rosenwasser, 2016, pp. pp. 21).
The main causes of an inflammatory process which make individuals to became vulnerable to its impact is hotly debated topic
among scholars. The appearance of asthma is an interactive yet multifaceted procedure that relies on the interaction between the
environmental exposures and host elements predominantly heredities that happen at an imperative time in the expansion of the
immune structure. Host dynamics include inborn resistance, sex, and genetics while ecological aspects comprise respiratory
infections, allergens, and other environmental exposures such as pollution and lifestyle (Saint, Semple, Sinha & Hawcutt, 2018, pp.
210).
Question 1
Asthma is a common prolonged syndrome of the lung air route that comprises a sophisticated link of airflow block, bronchial
hyperresponsiveness and an underlying infection. The illness can extremely vary on different patients. Prolonged signs of disease can
arise from bronchospasm or patient’s reaction during the bronchodilator treatment. Chronic and acute tenderness can upset the air
corridor capacity, airflow and also fundamental bronchial hyperresponsiveness, which improves vulnerability to bronchospasm. Thus,
asthma is a long-lasting inflammatory illness of an airway in which numerous cells and cellular features play a role, specifically;
eosinophils, mast cells, T lymphocytes, neutrophils, macrophages, and epithelial cells. This swelling causes regular incidents of
breathlessness, coughing, and stiffness of chest. Hence, the events are linked with extensive but mutable airflow hitch that is
commonly flexible either with treatment or spontaneously (Carr, Berdnikovs, Simon, Bochner & Rosenwasser, 2016, pp. pp. 21).
The main causes of an inflammatory process which make individuals to became vulnerable to its impact is hotly debated topic
among scholars. The appearance of asthma is an interactive yet multifaceted procedure that relies on the interaction between the
environmental exposures and host elements predominantly heredities that happen at an imperative time in the expansion of the
immune structure. Host dynamics include inborn resistance, sex, and genetics while ecological aspects comprise respiratory
infections, allergens, and other environmental exposures such as pollution and lifestyle (Saint, Semple, Sinha & Hawcutt, 2018, pp.
210).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASE STUDY: ACUTE SEVERE ASTHMA 4
Hyperinflated lungs happen when air gets stuck in the organ and causes the organ to overinflate. Hyperinflated lungs can be
instigated by a blockage in the air ways or by air sacs that are less variable, which interfere with the discharge of air from the lungs.
Hyperinflated lungs are frequently seen in individuals with chronic obstructive pulmonary disease, a disorder that comprises
emphysema. Definite lung difficulties such as cystic fibrosis and asthma also can cause hyperinflation (Memon, Parkash, Khan, Gowa
& Bai, 2016, pp .243).
It is worth noting that only small percentage of patients which have historical asthma disorders. Wheezing can occurs in some
patients, particularly during the exacerbations. Sometimes severe asthma can present severely with the respiratory disease or abrupt
start of shortness of breath. Important clinical examinations are tachypnea ( rapid breathing ), prolonged phase of respiration,
hyperinflation where the chest may become barrel-shaped owing to air catching, wheezing a musical sort sound received through the
stethoscope) is hardly present, and sign of heart failure such has peripheral oedema (swelling) may be present in progressive illness.
In order to diagnose the acute asthma and examine it severity, several tests should be done including blood gas tests and chest x-ray
(Saint, Semple, Sinha & Hawcutt, 2018, pp. 213).
Smith shows symptoms of the diseases with an incapability to speak a sentence in one breath, reduced breath sounds and
prevalent wheeze which are some of the symptoms of the Asthma. Another test such as chest x-ray proves a positive test for the
disease as it shows inflated lungs. Also, the arterial blood gas examination to measure oxygen interchange shows some deficient such
as lower or equal to the 60mmHg PaO2 despite supplemental oxygen at 60.
Hyperinflated lungs happen when air gets stuck in the organ and causes the organ to overinflate. Hyperinflated lungs can be
instigated by a blockage in the air ways or by air sacs that are less variable, which interfere with the discharge of air from the lungs.
Hyperinflated lungs are frequently seen in individuals with chronic obstructive pulmonary disease, a disorder that comprises
emphysema. Definite lung difficulties such as cystic fibrosis and asthma also can cause hyperinflation (Memon, Parkash, Khan, Gowa
& Bai, 2016, pp .243).
It is worth noting that only small percentage of patients which have historical asthma disorders. Wheezing can occurs in some
patients, particularly during the exacerbations. Sometimes severe asthma can present severely with the respiratory disease or abrupt
start of shortness of breath. Important clinical examinations are tachypnea ( rapid breathing ), prolonged phase of respiration,
hyperinflation where the chest may become barrel-shaped owing to air catching, wheezing a musical sort sound received through the
stethoscope) is hardly present, and sign of heart failure such has peripheral oedema (swelling) may be present in progressive illness.
In order to diagnose the acute asthma and examine it severity, several tests should be done including blood gas tests and chest x-ray
(Saint, Semple, Sinha & Hawcutt, 2018, pp. 213).
Smith shows symptoms of the diseases with an incapability to speak a sentence in one breath, reduced breath sounds and
prevalent wheeze which are some of the symptoms of the Asthma. Another test such as chest x-ray proves a positive test for the
disease as it shows inflated lungs. Also, the arterial blood gas examination to measure oxygen interchange shows some deficient such
as lower or equal to the 60mmHg PaO2 despite supplemental oxygen at 60.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASE STUDY: ACUTE SEVERE ASTHMA 5
Some of the complications of severe acute asthma which is likely to develop are collapse lung (Pneumothorax), which can be
life-threatening in individuals who have severe disease, as the function of the lung is already comprised. It is uncommon but very
serious when it happens. Another complication is heart problems where the disease can increase the pressure in the arteries that
connect heart and lungs. This condition causes a state called cor pulmonate, in which a part of the heart expands and weakens. Smith
shows signs high-pressure recording to 150/85mm/hg higher than normal.
Question two
One of the high priority nursing strategies to diagnose Jackson Smith is clinical history. The content of detailed history taking
for the disease includes the nature, period and causes of signs. Age and circumstance of early beginning of indications, allergies and
comorbidities, family history, occupation, long-term medication, and exacerbations are some of crucial info. Looking at the first
clinical examination of a patient, the history is given that he had complications that had been diagnosed when he was two years old.
The second high priority nursing strategies are clinical examination. Allergy analysis should continuously be done (clinical past,
blood test). Typically, patient with acute asthma have previously had a basic evaluation of their illness. In the verification of the
diagnosis; if adverse asthma is assumed, differential diagnoses that may simulator asthma should primarily be ruled out. This is
because up to 40% of asthma patients smoke. Sub-acute reversibility analysis using total treatment should be done in addition to
critical reversibility testing to rule out the chronic obstructive pulmonary disease. If the prednisone treatment completely or largely
Some of the complications of severe acute asthma which is likely to develop are collapse lung (Pneumothorax), which can be
life-threatening in individuals who have severe disease, as the function of the lung is already comprised. It is uncommon but very
serious when it happens. Another complication is heart problems where the disease can increase the pressure in the arteries that
connect heart and lungs. This condition causes a state called cor pulmonate, in which a part of the heart expands and weakens. Smith
shows signs high-pressure recording to 150/85mm/hg higher than normal.
Question two
One of the high priority nursing strategies to diagnose Jackson Smith is clinical history. The content of detailed history taking
for the disease includes the nature, period and causes of signs. Age and circumstance of early beginning of indications, allergies and
comorbidities, family history, occupation, long-term medication, and exacerbations are some of crucial info. Looking at the first
clinical examination of a patient, the history is given that he had complications that had been diagnosed when he was two years old.
The second high priority nursing strategies are clinical examination. Allergy analysis should continuously be done (clinical past,
blood test). Typically, patient with acute asthma have previously had a basic evaluation of their illness. In the verification of the
diagnosis; if adverse asthma is assumed, differential diagnoses that may simulator asthma should primarily be ruled out. This is
because up to 40% of asthma patients smoke. Sub-acute reversibility analysis using total treatment should be done in addition to
critical reversibility testing to rule out the chronic obstructive pulmonary disease. If the prednisone treatment completely or largely
CASE STUDY: ACUTE SEVERE ASTHMA 6
reinstates lung function, COPD is improbable. A chest x-ray may be expedient as it can rule numerous differentials detects such as
malformation, tumours, pulmonary embolism, and dysplasia (George, Joshi, Concepcion & Lee, 2017, pp.40).
Both the clinical history and examination was done to the patient. His family was able to say that a patient has been diagnosed
with asthma when he was two years old. Even though the above is not a comprehensive part of the clinical history, it does form part of
the clinical history. Clinical examination is done to the patient. Some of the examinations include the checking of blood pressure,
respiratory and pulse rate, oxygen saturation, blood gas test, and chest x-ray which shown hyperinflated lungs. Also, the patient
showed severe dyspnea, which is an inability to speak a sentence in one breath and finally auscultation of lungs identified diminished
breath sounds and widespread wheeze.
Question 3a
The usual procedure of bronchoconstriction happens in reaction to straight parasympathetic stimulation. Antagonism of this
outcome is created by free mixing epinephrine that performs upon B-receptors. B-blockers such as atenolol have been well recognized
to induce spasms in asthmatic patients because they avert epinephrine from undertaking its business. B-Agonists such as salbutamol
are utilised to excite the similar receptors that epinephrine uses (B2) to cause bronchodilation (Inayat, Shah, Rahu & Sahito, 2017, pp.
102).
Ipratropium bromide antagonizes the activities of acetylcholine at the parasympathetic, postganglionic and effector-cell
junction. When breathed in, it fixes competitively to cholinergic receptors in the bronchial smooth muscle and thus hindering the
reinstates lung function, COPD is improbable. A chest x-ray may be expedient as it can rule numerous differentials detects such as
malformation, tumours, pulmonary embolism, and dysplasia (George, Joshi, Concepcion & Lee, 2017, pp.40).
Both the clinical history and examination was done to the patient. His family was able to say that a patient has been diagnosed
with asthma when he was two years old. Even though the above is not a comprehensive part of the clinical history, it does form part of
the clinical history. Clinical examination is done to the patient. Some of the examinations include the checking of blood pressure,
respiratory and pulse rate, oxygen saturation, blood gas test, and chest x-ray which shown hyperinflated lungs. Also, the patient
showed severe dyspnea, which is an inability to speak a sentence in one breath and finally auscultation of lungs identified diminished
breath sounds and widespread wheeze.
Question 3a
The usual procedure of bronchoconstriction happens in reaction to straight parasympathetic stimulation. Antagonism of this
outcome is created by free mixing epinephrine that performs upon B-receptors. B-blockers such as atenolol have been well recognized
to induce spasms in asthmatic patients because they avert epinephrine from undertaking its business. B-Agonists such as salbutamol
are utilised to excite the similar receptors that epinephrine uses (B2) to cause bronchodilation (Inayat, Shah, Rahu & Sahito, 2017, pp.
102).
Ipratropium bromide antagonizes the activities of acetylcholine at the parasympathetic, postganglionic and effector-cell
junction. When breathed in, it fixes competitively to cholinergic receptors in the bronchial smooth muscle and thus hindering the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASE STUDY: ACUTE SEVERE ASTHMA 7
bronchoconstrictors action of the acetylcholine-mediated vagal impulses. Thus, vagal tone reserve leads to dilation of the large central
airways resulting in bronchodilation (Inayat, Shah, Rahu & Sahito, 2017, pp. 104).
.
Corticosteroids such as hydrocortisone reverse the mucosal edema, minimizing vascular permeability by vasoconstriction, and
inhibiting the release of LTC 4 and LTD4.
Question 3b
Immediate management is required in case of acute severe asthma
Oxygen to maintain SpO2 94-98% should be maintained. Salbutamol 5mg through an oxygen-driven nebulizer, ipratropium
bromide 0.5 mg through an oxygen-driven nebulizer, and hydrocortisone IV 100mg should be administered. However, no sedatives of
any sort but chest radiograph only if pneumothorax or association are alleged (Kulkarni, Akwei, Luyt, Gaillard & Mulla, 2015, pp.
2473).
If life-threatening sorts are existent, confer with senior health care providers. Add IV magnesium sulphate 1.-2g infusion over
20minutes and provide nebulized beta2 agonist more regularly such as salbutamol up to every 15-30mnutes or 10mg continuously
hours.
bronchoconstrictors action of the acetylcholine-mediated vagal impulses. Thus, vagal tone reserve leads to dilation of the large central
airways resulting in bronchodilation (Inayat, Shah, Rahu & Sahito, 2017, pp. 104).
.
Corticosteroids such as hydrocortisone reverse the mucosal edema, minimizing vascular permeability by vasoconstriction, and
inhibiting the release of LTC 4 and LTD4.
Question 3b
Immediate management is required in case of acute severe asthma
Oxygen to maintain SpO2 94-98% should be maintained. Salbutamol 5mg through an oxygen-driven nebulizer, ipratropium
bromide 0.5 mg through an oxygen-driven nebulizer, and hydrocortisone IV 100mg should be administered. However, no sedatives of
any sort but chest radiograph only if pneumothorax or association are alleged (Kulkarni, Akwei, Luyt, Gaillard & Mulla, 2015, pp.
2473).
If life-threatening sorts are existent, confer with senior health care providers. Add IV magnesium sulphate 1.-2g infusion over
20minutes and provide nebulized beta2 agonist more regularly such as salbutamol up to every 15-30mnutes or 10mg continuously
hours.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASE STUDY: ACUTE SEVERE ASTHMA 8
If the patient is improving, oxygen should be maintained between SpO2 94-98%. Prednisolone oral 40-50 each day and
nebulized Beta2 agonist and ipratropium 4- hours ought to be administered. If the patient is not progressing after 15-30 minutes,
continuous steroids and oxygen administration should follow. Give nebulized beta2 agonist more frequently such as salbutamol up to
every 15-30 minutes and continues ipratropium 0.5mg 4-6 hours until a patient improves.
Nursing: repeat measurement of PEF 15-minutes after preliminary treatment and oximeter measurement ought to be
maintained at SpO2 94-98%. One should repeat blood gas measurement after one-hour starting from initial treatment. Finally, chart
PEF earlier and after providing Beta2 agonists and at least four times daily during the hospice stay.
If the patient is improving, oxygen should be maintained between SpO2 94-98%. Prednisolone oral 40-50 each day and
nebulized Beta2 agonist and ipratropium 4- hours ought to be administered. If the patient is not progressing after 15-30 minutes,
continuous steroids and oxygen administration should follow. Give nebulized beta2 agonist more frequently such as salbutamol up to
every 15-30 minutes and continues ipratropium 0.5mg 4-6 hours until a patient improves.
Nursing: repeat measurement of PEF 15-minutes after preliminary treatment and oximeter measurement ought to be
maintained at SpO2 94-98%. One should repeat blood gas measurement after one-hour starting from initial treatment. Finally, chart
PEF earlier and after providing Beta2 agonists and at least four times daily during the hospice stay.
CASE STUDY: ACUTE SEVERE ASTHMA 9
References
Carr, T. F., Berdnikovs, S., Simon, H. U., Bochner, B. S., & Rosenwasser, L. J. (2016). Eosinophilic bioactivities in severe
asthma. World Allergy Organization Journal, 9(1), 21.
George, M., Joshi, S. V., Concepcion, E., & Lee, H. (2017). Paradoxical bronchospasm from benzalkonium chloride (BAC)
preservative in albuterol nebulizer solution in a patient with acute severe asthma. A case report and literature review of airway
effects of BAC. Respiratory medicine case reports, 21, 39-41.
Inayat, N., Shah, R. H., Rahu, Q. A., & Sahito, R. (2017). Nebulized Salbutamol with and without Ipratropium Bromide in the
treatment of acute Severe Asthma. Pakistan Journal of Chest Medicine, 22(3), 102-6.
Kulkarni, H., Akwei, S., Luyt, D. K., Gaillard, E. A., & Mulla, H. (2015). Cardiac Troponin I Levels in Children with Acute Severe
Asthma Treated with IV Salbutamol. Lung Dis Treat, 1(102), 2472-1018.
Memon, B. N., Parkash, A., Khan, K. M. A., Gowa, M. A., & Bai, C. (2016). Response to nebulized salbutamol versus combination
with ipratropium bromide in children with acute severe asthma. JPMA. The Journal of the Pakistan Medical
Association, 66(3), 243-246.
Saint, G. L., Semple, M. G., Sinha, I., & Hawcutt, D. B. (2018). Optimizing the Dosing of Intravenous Theophylline in Acute Severe
Asthma in Children. Pediatric Drugs, 20(3), 209-214.
References
Carr, T. F., Berdnikovs, S., Simon, H. U., Bochner, B. S., & Rosenwasser, L. J. (2016). Eosinophilic bioactivities in severe
asthma. World Allergy Organization Journal, 9(1), 21.
George, M., Joshi, S. V., Concepcion, E., & Lee, H. (2017). Paradoxical bronchospasm from benzalkonium chloride (BAC)
preservative in albuterol nebulizer solution in a patient with acute severe asthma. A case report and literature review of airway
effects of BAC. Respiratory medicine case reports, 21, 39-41.
Inayat, N., Shah, R. H., Rahu, Q. A., & Sahito, R. (2017). Nebulized Salbutamol with and without Ipratropium Bromide in the
treatment of acute Severe Asthma. Pakistan Journal of Chest Medicine, 22(3), 102-6.
Kulkarni, H., Akwei, S., Luyt, D. K., Gaillard, E. A., & Mulla, H. (2015). Cardiac Troponin I Levels in Children with Acute Severe
Asthma Treated with IV Salbutamol. Lung Dis Treat, 1(102), 2472-1018.
Memon, B. N., Parkash, A., Khan, K. M. A., Gowa, M. A., & Bai, C. (2016). Response to nebulized salbutamol versus combination
with ipratropium bromide in children with acute severe asthma. JPMA. The Journal of the Pakistan Medical
Association, 66(3), 243-246.
Saint, G. L., Semple, M. G., Sinha, I., & Hawcutt, D. B. (2018). Optimizing the Dosing of Intravenous Theophylline in Acute Severe
Asthma in Children. Pediatric Drugs, 20(3), 209-214.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




