Acute Respiratory Distress: Asthma Exacerbation Case Study Report
VerifiedAdded on 2023/06/10
|12
|3331
|496
Report
AI Summary
This report presents a case study of a 66-year-old man, Harry, admitted to the hospital with acute respiratory distress due to asthma exacerbation. The report delves into the patient's history, including his smoking habit and past prescriptions, and details his current health problem, including the use of the ABCDE approach for assessment. It explores the underlying pathophysiology of acute respiratory failure, differentiating between type 1 and type 2 respiratory failures, and discussing the role of factors such as bronchospasm and inflammation. The report also outlines ethical considerations and provides a detailed discussion of interventions, including supplemental oxygen, non-invasive positive pressure ventilation (NIPPV), mechanical ventilation, and antibiotic treatment, to manage the patient's condition effectively. The report concludes by summarizing the key aspects of the case and emphasizing the importance of understanding pathophysiology for effective patient care.

Running head: EXACERBATION OF ASTHMA
Exacerbation of asthma
Name of the student
University name
Author’s note
Exacerbation of asthma
Name of the student
University name
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1
EXACERBATION OF ASTHMA
Table of Contents
Introduction................................................................................................................................2
Brief summary of the patient’s current health problem.............................................................2
Relevant history and specific early management plan...............................................................4
Ethical requirements...................................................................................................................5
Explanation of underlying pathophysiology related to acute respiratory failure.......................5
Interventions...............................................................................................................................7
Conclusion..................................................................................................................................8
References..................................................................................................................................9
EXACERBATION OF ASTHMA
Table of Contents
Introduction................................................................................................................................2
Brief summary of the patient’s current health problem.............................................................2
Relevant history and specific early management plan...............................................................4
Ethical requirements...................................................................................................................5
Explanation of underlying pathophysiology related to acute respiratory failure.......................5
Interventions...............................................................................................................................7
Conclusion..................................................................................................................................8
References..................................................................................................................................9
2
EXACERBATION OF ASTHMA
Introduction
The current assignment focuses upon understanding the deep seated pathophysiology
associated acute respiratory distress or failure. In this respect, developing a knowledge
regarding the pathophysiology can help in the development of effective preventive measures
as well as design a sound care plan. The pathophysiology here mainly focuses upon the
aetiology and the causes of a disease. Therefore, understanding the pathophysiology helps in
understanding the origin as well as identifies the genetic roots for the development of a
disease within the patient population (Villar et al. 2014). It has been observed that most of the
times the environment along with the genetic factors contributes towards the development of
a disease (Khemani et al. 2015). Therefore, a detailed knowledge of the pathophysiology
helps to take into consideration all these factors and the different levels of expression
produced by them. In the current study, a particular case study has been taken into
consideration. Based upon the conditions and the symptoms presented by the patient, the
underlying pathophsyiology has been accessed.
Brief summary of the patient’s current health problem
Here, the patient is a 66 year old man Harry suffering from acute respiratory distress
owing to which he had been admitted to the hospital. The respiratory distress emerged due to
exacerbation of asthmatic conditions within the patient. As mentioned by Pediatric Acute
Lung Injury Consensus Conference Group (2015), the falling of the SpO2 below 90% for
longer periods of time could lead to medical emergency as the patient is unable to respire
normally. In case the patient is left untreated for longer periods of time it could lead to
respiratory failure and eventually death (Mac Sweeney and McAuley 2016). As mentioned by
Lemiale et al. (2015), with failure of the respiratory system, the neurological system will fail
and the mental status of the patient deteriorates.
EXACERBATION OF ASTHMA
Introduction
The current assignment focuses upon understanding the deep seated pathophysiology
associated acute respiratory distress or failure. In this respect, developing a knowledge
regarding the pathophysiology can help in the development of effective preventive measures
as well as design a sound care plan. The pathophysiology here mainly focuses upon the
aetiology and the causes of a disease. Therefore, understanding the pathophysiology helps in
understanding the origin as well as identifies the genetic roots for the development of a
disease within the patient population (Villar et al. 2014). It has been observed that most of the
times the environment along with the genetic factors contributes towards the development of
a disease (Khemani et al. 2015). Therefore, a detailed knowledge of the pathophysiology
helps to take into consideration all these factors and the different levels of expression
produced by them. In the current study, a particular case study has been taken into
consideration. Based upon the conditions and the symptoms presented by the patient, the
underlying pathophsyiology has been accessed.
Brief summary of the patient’s current health problem
Here, the patient is a 66 year old man Harry suffering from acute respiratory distress
owing to which he had been admitted to the hospital. The respiratory distress emerged due to
exacerbation of asthmatic conditions within the patient. As mentioned by Pediatric Acute
Lung Injury Consensus Conference Group (2015), the falling of the SpO2 below 90% for
longer periods of time could lead to medical emergency as the patient is unable to respire
normally. In case the patient is left untreated for longer periods of time it could lead to
respiratory failure and eventually death (Mac Sweeney and McAuley 2016). As mentioned by
Lemiale et al. (2015), with failure of the respiratory system, the neurological system will fail
and the mental status of the patient deteriorates.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
EXACERBATION OF ASTHMA
Here, the patient Harry was diagnosed with PaO2 less than 60 mm of Hg without
elevated CO2 level. In this respect, urgent resuscitation had to be provided to the patient,
which involves airway control, ventilator management and stabilization of the circulation. In
this respect, a therapeutic plan needs to be developed for the patient based on informed
clinical and laboratory examination (Pediatric Acute Lung Injury Consensus Conference
Group 2015). The laboratory examination confirmed exacerbation of asthma within the
patient. The tests which were conducted upon the patients were a chest x- ray followed by a
sputum tests. The chest x-ray depicted shrunken alveoli which signified the presence of
chronic respiratory distress within the patient, whereas the sputum test signified the presence
of viral infection. The viral infection further worsened the asthmatic conditions of the patient
(Lemiale et al. 2015).
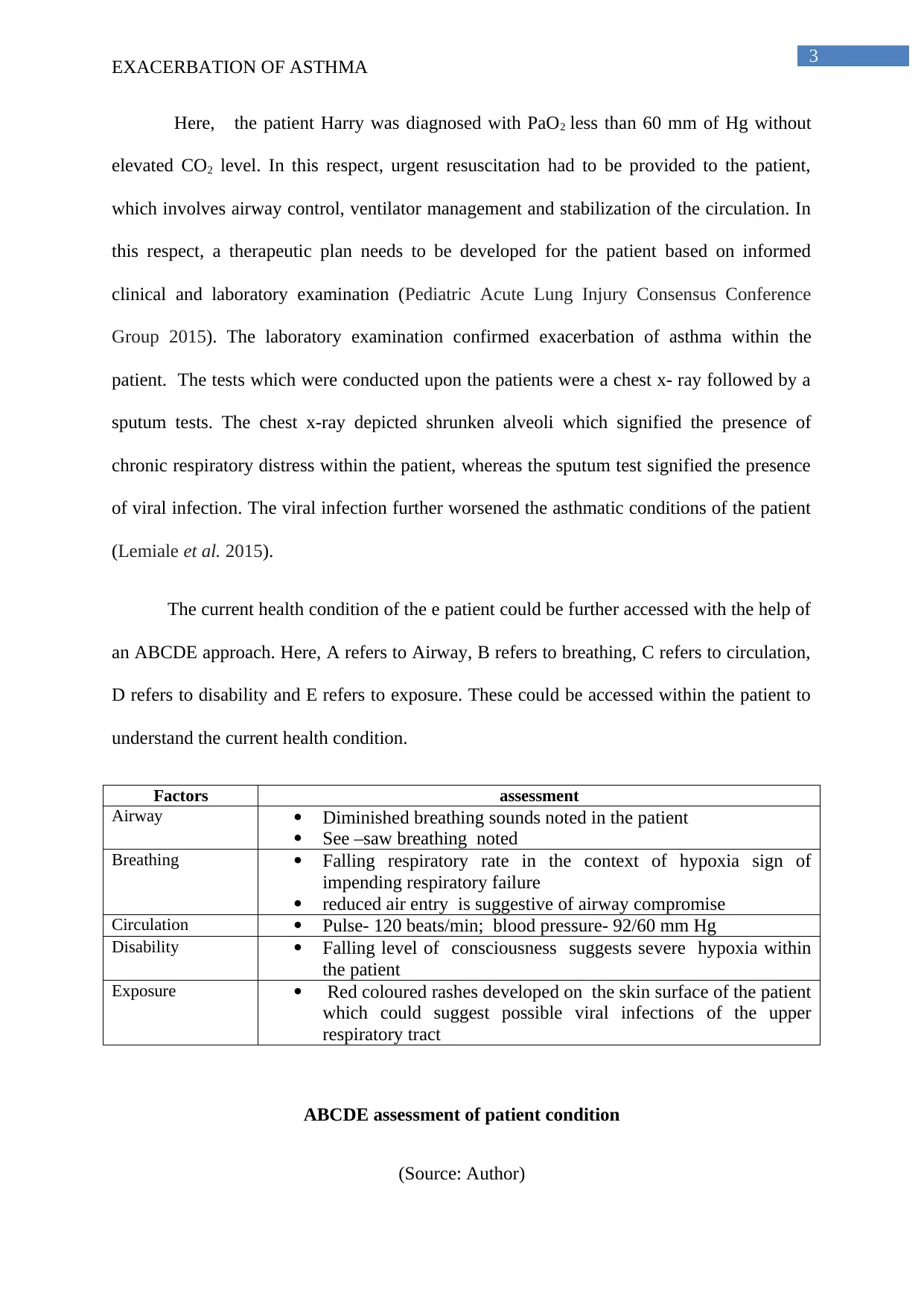
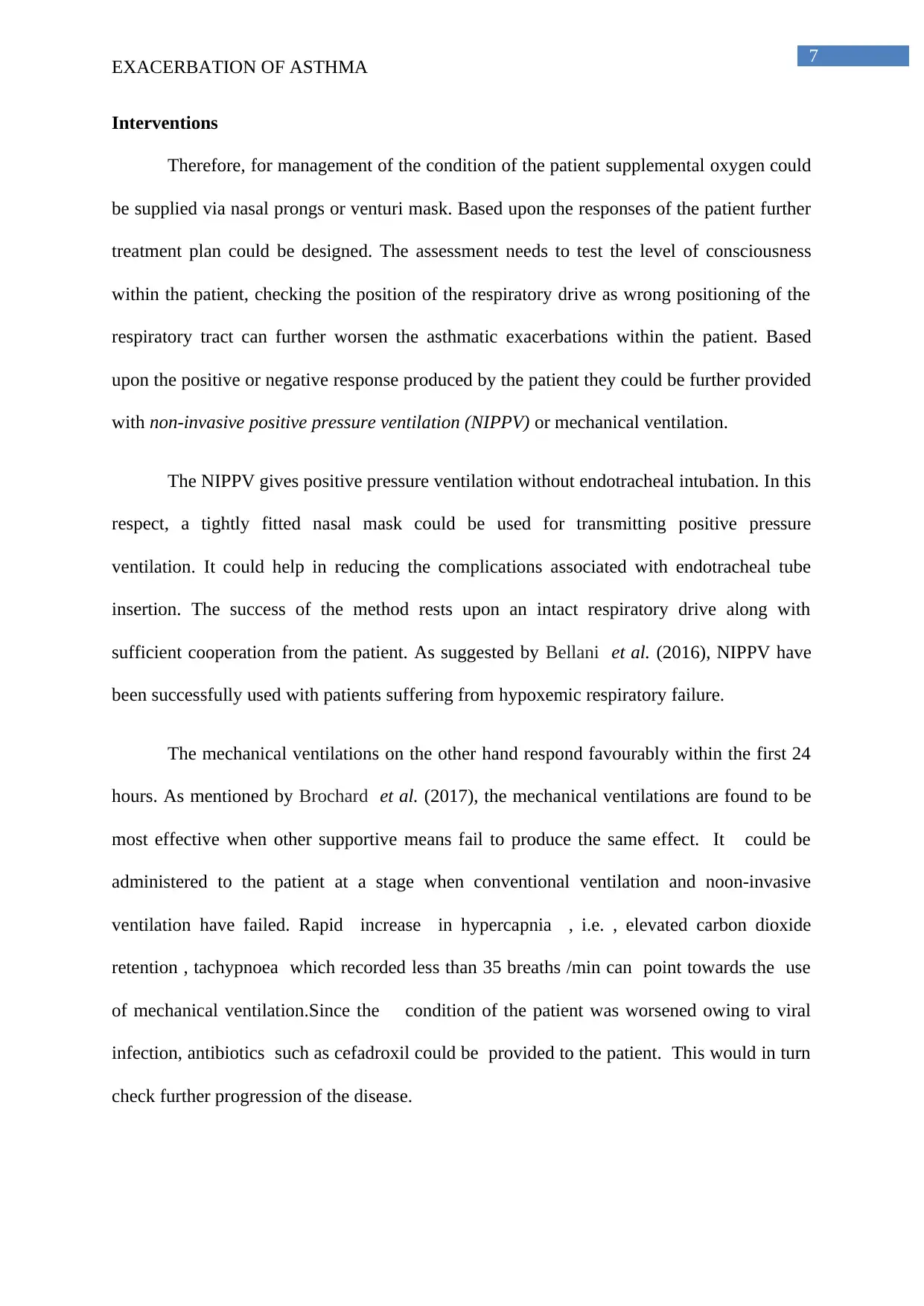
The current health condition of the e patient could be further accessed with the help of
an ABCDE approach. Here, A refers to Airway, B refers to breathing, C refers to circulation,
D refers to disability and E refers to exposure. These could be accessed within the patient to
understand the current health condition.
Factors assessment
Airway Diminished breathing sounds noted in the patient
See –saw breathing noted
Breathing Falling respiratory rate in the context of hypoxia sign of
impending respiratory failure
reduced air entry is suggestive of airway compromise
Circulation Pulse- 120 beats/min; blood pressure- 92/60 mm Hg
Disability Falling level of consciousness suggests severe hypoxia within
the patient
Exposure Red coloured rashes developed on the skin surface of the patient
which could suggest possible viral infections of the upper
respiratory tract
ABCDE assessment of patient condition
(Source: Author)
EXACERBATION OF ASTHMA
Here, the patient Harry was diagnosed with PaO2 less than 60 mm of Hg without
elevated CO2 level. In this respect, urgent resuscitation had to be provided to the patient,
which involves airway control, ventilator management and stabilization of the circulation. In
this respect, a therapeutic plan needs to be developed for the patient based on informed
clinical and laboratory examination (Pediatric Acute Lung Injury Consensus Conference
Group 2015). The laboratory examination confirmed exacerbation of asthma within the
patient. The tests which were conducted upon the patients were a chest x- ray followed by a
sputum tests. The chest x-ray depicted shrunken alveoli which signified the presence of
chronic respiratory distress within the patient, whereas the sputum test signified the presence
of viral infection. The viral infection further worsened the asthmatic conditions of the patient
(Lemiale et al. 2015).
The current health condition of the e patient could be further accessed with the help of
an ABCDE approach. Here, A refers to Airway, B refers to breathing, C refers to circulation,
D refers to disability and E refers to exposure. These could be accessed within the patient to
understand the current health condition.
Factors assessment
Airway Diminished breathing sounds noted in the patient
See –saw breathing noted
Breathing Falling respiratory rate in the context of hypoxia sign of
impending respiratory failure
reduced air entry is suggestive of airway compromise
Circulation Pulse- 120 beats/min; blood pressure- 92/60 mm Hg
Disability Falling level of consciousness suggests severe hypoxia within
the patient
Exposure Red coloured rashes developed on the skin surface of the patient
which could suggest possible viral infections of the upper
respiratory tract
ABCDE assessment of patient condition
(Source: Author)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
EXACERBATION OF ASTHMA
Relevant history and specific early management plan
The patient is a 66 years man suffering from asthma and had a past history of
smoking. The patient was a native of the Queensland region Australia and worked as a civil
engineer in a construction unit. The habit of smoking along with the dust emitted from the
factory further worsened the health condition of the patient. Harry reported that he had been
prescribed by his doctor a number of corticosteroids, which could be inhaled for relieving
the conditions of asthma within the patient. Some of these medications are- fluticasone,
budesonide, flunisolide, mometasone etc. The patient reported that he would often require the
help of nebulizers for dealing with respiratory distress. The patient had been previously
admitted to the hospital on several occasions owing to shortness of breath. Some of the
medications which had been previously suggested to the patient are Salmeterol which are
long acting beta agonists. These are known to open the airways in the patient. However, as
argued by Frat et al. (2015), the salmeterol may increase the severe asthma attack. Hence,
the medicined need to be provided in combination with corticosteroids. Additionally,
bronchodilators such as ipratropium have been seen to relax the airways and make breathing
easier.
Therefore, some of the initial care plan which could be used to support the treatment
and care of the patient were use of bronchodilators, corticosteroids inhalers. On initial
admissions, some of the preliminary care strategies which could be provided to the patient are
providing the patient with mechanical ventilation (Brochard et al. 2017). For the purpose of
which an endotracheal tube could be placed through the mouth or the nose of the patient.
Regular blood pressure should be monitored within the patient looking for orthostatic
changes (Scaravilli et al. 2015). Blood tests could be performed for monitoring oxygen
levels.
EXACERBATION OF ASTHMA
Relevant history and specific early management plan
The patient is a 66 years man suffering from asthma and had a past history of
smoking. The patient was a native of the Queensland region Australia and worked as a civil
engineer in a construction unit. The habit of smoking along with the dust emitted from the
factory further worsened the health condition of the patient. Harry reported that he had been
prescribed by his doctor a number of corticosteroids, which could be inhaled for relieving
the conditions of asthma within the patient. Some of these medications are- fluticasone,
budesonide, flunisolide, mometasone etc. The patient reported that he would often require the
help of nebulizers for dealing with respiratory distress. The patient had been previously
admitted to the hospital on several occasions owing to shortness of breath. Some of the
medications which had been previously suggested to the patient are Salmeterol which are
long acting beta agonists. These are known to open the airways in the patient. However, as
argued by Frat et al. (2015), the salmeterol may increase the severe asthma attack. Hence,
the medicined need to be provided in combination with corticosteroids. Additionally,
bronchodilators such as ipratropium have been seen to relax the airways and make breathing
easier.
Therefore, some of the initial care plan which could be used to support the treatment
and care of the patient were use of bronchodilators, corticosteroids inhalers. On initial
admissions, some of the preliminary care strategies which could be provided to the patient are
providing the patient with mechanical ventilation (Brochard et al. 2017). For the purpose of
which an endotracheal tube could be placed through the mouth or the nose of the patient.
Regular blood pressure should be monitored within the patient looking for orthostatic
changes (Scaravilli et al. 2015). Blood tests could be performed for monitoring oxygen
levels.
5
EXACERBATION OF ASTHMA
Ethical requirements
While understanding the pathophsyiology of a patient a number of ethical
considerations need to be taken into consideration. For instance, at no stage during the study
the exact details of the participants could be leaked out. For the public presentation of the
study, the name of the participants needs to be changed as using the exact details of the
participants could lead to legal breaches.
Explanation of underlying pathophysiology related to acute respiratory failure
Asthma is a common respiratory condition which is commonly characterised by
shortness of breath or difficulty in breathing within the patient. Asthma is characterised by an
increased sensitivity of the lower airways to irritants and allergens, which could lead to
bronchospasm characterised by inflammation and narrowing of the arterioles (Bellani et al.
2016). Some of the associated asthmatic complications which obstructs the normal passage
of air through the lungs are-bronchospasm, edema of inner lining of the airways, increased
secretion of mucous which blocks the small airways. The asthma patients usually suffer
from periodic attacks, which are accompanied with very few or no signs and symptoms
(Ranieri et al. 2016).
In this respect, a prolonged life threatening attack could lead to the development of
status asthmaticus within the patient (Lee et al. 2015). It is often characterise by a stage
when the patients respond to neither oxygen nor medication. Under such conditions, the
patients require immediate transport to the hospital. The respiratory distress often results in
altered mental awareness within the patient. As suggested by Schmidt et al. (2014), the upper
respiratory tract infections are often accompanied by fever, allergic reactions such as
sneezing, redness of eye, chests tightness running nose etc. It is often accompanied by
tachycardia and tachypnea , where the tachycardia resembles heart rate greater than 120
EXACERBATION OF ASTHMA
Ethical requirements
While understanding the pathophsyiology of a patient a number of ethical
considerations need to be taken into consideration. For instance, at no stage during the study
the exact details of the participants could be leaked out. For the public presentation of the
study, the name of the participants needs to be changed as using the exact details of the
participants could lead to legal breaches.
Explanation of underlying pathophysiology related to acute respiratory failure
Asthma is a common respiratory condition which is commonly characterised by
shortness of breath or difficulty in breathing within the patient. Asthma is characterised by an
increased sensitivity of the lower airways to irritants and allergens, which could lead to
bronchospasm characterised by inflammation and narrowing of the arterioles (Bellani et al.
2016). Some of the associated asthmatic complications which obstructs the normal passage
of air through the lungs are-bronchospasm, edema of inner lining of the airways, increased
secretion of mucous which blocks the small airways. The asthma patients usually suffer
from periodic attacks, which are accompanied with very few or no signs and symptoms
(Ranieri et al. 2016).
In this respect, a prolonged life threatening attack could lead to the development of
status asthmaticus within the patient (Lee et al. 2015). It is often characterise by a stage
when the patients respond to neither oxygen nor medication. Under such conditions, the
patients require immediate transport to the hospital. The respiratory distress often results in
altered mental awareness within the patient. As suggested by Schmidt et al. (2014), the upper
respiratory tract infections are often accompanied by fever, allergic reactions such as
sneezing, redness of eye, chests tightness running nose etc. It is often accompanied by
tachycardia and tachypnea , where the tachycardia resembles heart rate greater than 120
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
EXACERBATION OF ASTHMA
breaths per minute. In this respect, falling of the partial pressure of oxygen below 90% for
prolonged periods of time could signify the need for immediate hospitalization, as it could
lead to respiratory failure within the patient (Neto et al. 2015).
In the present scenario, the exacerbation of asthma leads to an acute respiratory
failure within the patient. The failure of the respiratory system could be referred to as a
condition where adequate gas exchange cannot be maintained. As mentioned by Amato et al.
(2015), the patient looses the ability to ventilate adequately. Here, the respiratory failure
could be divided into two significant types such as type 1 and type 2. The type 1 respiratory
failure is defined by PaO2 of <60 mm Hg and normal or low PaCO2. On the other hand, type
2 respiratory failure is defined by PaO2 of <60 mm Hg and PaCO2 of >45 mm Hg. It has
been seen that hypoxemia and hypercarbic conditions often co-exist. The type 1 respiratory
failure can occur due to a number of causes such as – chronic bronchitis, pneumonia,
pulmonary edema, pnemothorax and pneumoconiosis etc. On the other hand, the type 2
respiratory failure could be accounted to a number of causes such as – emphysema, asthma,
pulmonary edema, infections caused by foreign bodies etc (Brochard et al. 2017).
The respiratory failure could be further classified into acute respiratory failure and
chronic respiratory failure. It could be characterised by acute deterioration in an individual
with significant hypercarbic respiratory failure. One of the most common causes of type 2
respiratory failure is pulmonary disorder (Neto et al. 2015). The hypoxemia that develops
slowly over the years produces little effects within the patients. The diagnosis could be done
by arterial blood gas analysis. The assessment of ph helps in measuring the degree of acute
versus chronic respiratory failure (Frat et al. 2015). However, at any stage the falling of the
partial pressure of oxygen below 90% should be taken as a pivotal sign.
EXACERBATION OF ASTHMA
breaths per minute. In this respect, falling of the partial pressure of oxygen below 90% for
prolonged periods of time could signify the need for immediate hospitalization, as it could
lead to respiratory failure within the patient (Neto et al. 2015).
In the present scenario, the exacerbation of asthma leads to an acute respiratory
failure within the patient. The failure of the respiratory system could be referred to as a
condition where adequate gas exchange cannot be maintained. As mentioned by Amato et al.
(2015), the patient looses the ability to ventilate adequately. Here, the respiratory failure
could be divided into two significant types such as type 1 and type 2. The type 1 respiratory
failure is defined by PaO2 of <60 mm Hg and normal or low PaCO2. On the other hand, type
2 respiratory failure is defined by PaO2 of <60 mm Hg and PaCO2 of >45 mm Hg. It has
been seen that hypoxemia and hypercarbic conditions often co-exist. The type 1 respiratory
failure can occur due to a number of causes such as – chronic bronchitis, pneumonia,
pulmonary edema, pnemothorax and pneumoconiosis etc. On the other hand, the type 2
respiratory failure could be accounted to a number of causes such as – emphysema, asthma,
pulmonary edema, infections caused by foreign bodies etc (Brochard et al. 2017).
The respiratory failure could be further classified into acute respiratory failure and
chronic respiratory failure. It could be characterised by acute deterioration in an individual
with significant hypercarbic respiratory failure. One of the most common causes of type 2
respiratory failure is pulmonary disorder (Neto et al. 2015). The hypoxemia that develops
slowly over the years produces little effects within the patients. The diagnosis could be done
by arterial blood gas analysis. The assessment of ph helps in measuring the degree of acute
versus chronic respiratory failure (Frat et al. 2015). However, at any stage the falling of the
partial pressure of oxygen below 90% should be taken as a pivotal sign.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
EXACERBATION OF ASTHMA
Interventions
Therefore, for management of the condition of the patient supplemental oxygen could
be supplied via nasal prongs or venturi mask. Based upon the responses of the patient further
treatment plan could be designed. The assessment needs to test the level of consciousness
within the patient, checking the position of the respiratory drive as wrong positioning of the
respiratory tract can further worsen the asthmatic exacerbations within the patient. Based
upon the positive or negative response produced by the patient they could be further provided
with non-invasive positive pressure ventilation (NIPPV) or mechanical ventilation.
The NIPPV gives positive pressure ventilation without endotracheal intubation. In this
respect, a tightly fitted nasal mask could be used for transmitting positive pressure
ventilation. It could help in reducing the complications associated with endotracheal tube
insertion. The success of the method rests upon an intact respiratory drive along with
sufficient cooperation from the patient. As suggested by Bellani et al. (2016), NIPPV have
been successfully used with patients suffering from hypoxemic respiratory failure.
The mechanical ventilations on the other hand respond favourably within the first 24
hours. As mentioned by Brochard et al. (2017), the mechanical ventilations are found to be
most effective when other supportive means fail to produce the same effect. It could be
administered to the patient at a stage when conventional ventilation and noon-invasive
ventilation have failed. Rapid increase in hypercapnia , i.e. , elevated carbon dioxide
retention , tachypnoea which recorded less than 35 breaths /min can point towards the use
of mechanical ventilation.Since the condition of the patient was worsened owing to viral
infection, antibiotics such as cefadroxil could be provided to the patient. This would in turn
check further progression of the disease.
EXACERBATION OF ASTHMA
Interventions
Therefore, for management of the condition of the patient supplemental oxygen could
be supplied via nasal prongs or venturi mask. Based upon the responses of the patient further
treatment plan could be designed. The assessment needs to test the level of consciousness
within the patient, checking the position of the respiratory drive as wrong positioning of the
respiratory tract can further worsen the asthmatic exacerbations within the patient. Based
upon the positive or negative response produced by the patient they could be further provided
with non-invasive positive pressure ventilation (NIPPV) or mechanical ventilation.
The NIPPV gives positive pressure ventilation without endotracheal intubation. In this
respect, a tightly fitted nasal mask could be used for transmitting positive pressure
ventilation. It could help in reducing the complications associated with endotracheal tube
insertion. The success of the method rests upon an intact respiratory drive along with
sufficient cooperation from the patient. As suggested by Bellani et al. (2016), NIPPV have
been successfully used with patients suffering from hypoxemic respiratory failure.
The mechanical ventilations on the other hand respond favourably within the first 24
hours. As mentioned by Brochard et al. (2017), the mechanical ventilations are found to be
most effective when other supportive means fail to produce the same effect. It could be
administered to the patient at a stage when conventional ventilation and noon-invasive
ventilation have failed. Rapid increase in hypercapnia , i.e. , elevated carbon dioxide
retention , tachypnoea which recorded less than 35 breaths /min can point towards the use
of mechanical ventilation.Since the condition of the patient was worsened owing to viral
infection, antibiotics such as cefadroxil could be provided to the patient. This would in turn
check further progression of the disease.
8
EXACERBATION OF ASTHMA
Conclusion
The current assignment focuses upon the aspect of pathophysiology identification and
delivery of effective care and treatment to a patient suffering from acute respiratory failure.
Here, the patient suffers from asthma which has worsened leading to complications such as
acute respiratory distress and failure within the patient.
Therefore, a number of effective assessment patterns have been discussed over here
such as the ABCDE assessment. It helps in understanding the present symptoms expressed by
the patient which could be further related with the underlying pathophysiology. In this
respect, understanding the past history of the patient is also important in designing of an
effective care Plan. The pathophysiology have been further discussed with reference to the
interventions and methods which could be used for treating the conditions of the patient.
Therefore, in order to reduce the incidences of acute respiratory failure it is important to
know the underlying causes, which could be used to design effective intervention strategies.
EXACERBATION OF ASTHMA
Conclusion
The current assignment focuses upon the aspect of pathophysiology identification and
delivery of effective care and treatment to a patient suffering from acute respiratory failure.
Here, the patient suffers from asthma which has worsened leading to complications such as
acute respiratory distress and failure within the patient.
Therefore, a number of effective assessment patterns have been discussed over here
such as the ABCDE assessment. It helps in understanding the present symptoms expressed by
the patient which could be further related with the underlying pathophysiology. In this
respect, understanding the past history of the patient is also important in designing of an
effective care Plan. The pathophysiology have been further discussed with reference to the
interventions and methods which could be used for treating the conditions of the patient.
Therefore, in order to reduce the incidences of acute respiratory failure it is important to
know the underlying causes, which could be used to design effective intervention strategies.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
EXACERBATION OF ASTHMA
References
Amato, M.B., Meade, M.O., Slutsky, A.S., Brochard, L., Costa, E.L., Schoenfeld, D.A.,
Stewart, T.E., Briel, M., Talmor, D., Mercat, A. and Richard, J.C.M., 2015. Driving pressure
and survival in the acute respiratory distress syndrome. New England Journal of
Medicine, 372(8), pp.747-755.
Bellani, G., Laffey, J.G., Pham, T., Fan, E., Brochard, L., Esteban, A., Gattinoni, L., Van
Haren, F., Larsson, A., McAuley, D.F. and Ranieri, M., 2016. Epidemiology, patterns of care,
and mortality for patients with acute respiratory distress syndrome in intensive care units in
50 countries. Jama, 315(8), pp.788-800.
Brochard, L., Slutsky, A. and Pesenti, A., 2017. Mechanical ventilation to minimize
progression of lung injury in acute respiratory failure. American journal of respiratory and
critical care medicine, 195(4), pp.438-442.
Brochard, L., Slutsky, A. and Pesenti, A., 2017. Mechanical ventilation to minimize
progression of lung injury in acute respiratory failure. American journal of respiratory and
critical care medicine, 195(4), pp.438-442.
Frat, J.P., Thille, A.W., Mercat, A., Girault, C., Ragot, S., Perbet, S., Prat, G., Boulain, T.,
Morawiec, E., Cottereau, A. and Devaquet, J., 2015. High-flow oxygen through nasal cannula
in acute hypoxemic respiratory failure. New England Journal of Medicine, 372(23), pp.2185-
2196.
Khemani, R.G., Smith, L.S., Zimmerman, J.J., Erickson, S. and Pediatric Acute Lung Injury
Consensus Conference Group, 2015. Pediatric acute respiratory distress syndrome: definition,
incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus
Conference. Pediatric Critical Care Medicine, 16(5_suppl), pp.S23-S40.
EXACERBATION OF ASTHMA
References
Amato, M.B., Meade, M.O., Slutsky, A.S., Brochard, L., Costa, E.L., Schoenfeld, D.A.,
Stewart, T.E., Briel, M., Talmor, D., Mercat, A. and Richard, J.C.M., 2015. Driving pressure
and survival in the acute respiratory distress syndrome. New England Journal of
Medicine, 372(8), pp.747-755.
Bellani, G., Laffey, J.G., Pham, T., Fan, E., Brochard, L., Esteban, A., Gattinoni, L., Van
Haren, F., Larsson, A., McAuley, D.F. and Ranieri, M., 2016. Epidemiology, patterns of care,
and mortality for patients with acute respiratory distress syndrome in intensive care units in
50 countries. Jama, 315(8), pp.788-800.
Brochard, L., Slutsky, A. and Pesenti, A., 2017. Mechanical ventilation to minimize
progression of lung injury in acute respiratory failure. American journal of respiratory and
critical care medicine, 195(4), pp.438-442.
Brochard, L., Slutsky, A. and Pesenti, A., 2017. Mechanical ventilation to minimize
progression of lung injury in acute respiratory failure. American journal of respiratory and
critical care medicine, 195(4), pp.438-442.
Frat, J.P., Thille, A.W., Mercat, A., Girault, C., Ragot, S., Perbet, S., Prat, G., Boulain, T.,
Morawiec, E., Cottereau, A. and Devaquet, J., 2015. High-flow oxygen through nasal cannula
in acute hypoxemic respiratory failure. New England Journal of Medicine, 372(23), pp.2185-
2196.
Khemani, R.G., Smith, L.S., Zimmerman, J.J., Erickson, S. and Pediatric Acute Lung Injury
Consensus Conference Group, 2015. Pediatric acute respiratory distress syndrome: definition,
incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus
Conference. Pediatric Critical Care Medicine, 16(5_suppl), pp.S23-S40.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
EXACERBATION OF ASTHMA
Lee, H.Y., Rhee, C.K. and Lee, J.W., 2015. Feasibility of high-flow nasal cannula oxygen
therapy for acute respiratory failure in patients with hematologic malignancies: a
retrospective single-center study. Journal of critical care, 30(4), pp.773-777.
Lemiale, V., Mokart, D., Resche-Rigon, M., Pène, F., Mayaux, J., Faucher, E., Nyunga, M.,
Girault, C., Perez, P., Guitton, C. and Ekpe, K., 2015. Effect of noninvasive ventilation vs
oxygen therapy on mortality among immunocompromised patients with acute respiratory
failure: a randomized clinical trial. Jama, 314(16), pp.1711-1719.
Lemiale, V., Resche-Rigon, M., Mokart, D., Pène, F., Rabbat, A., Kouatchet, A., Vincent, F.,
Bruneel, F., Nyunga, M., Lebert, C. and Perez, P., 2015. Acute respiratory failure in patients
with hematological malignancies: outcomes according to initial ventilation strategy. A groupe
de recherche respiratoire en réanimation onco-hématologique (Grrr-OH) study. Annals of
intensive care, 5(1), p.28.
Mac Sweeney, R. and McAuley, D.F., 2016. Acute respiratory distress syndrome. The
Lancet, 388(10058), pp.2416-2430.
Neto, A.S., Simonis, F.D., Barbas, C.S., Biehl, M., Determann, R.M., Elmer, J., Friedman,
G., Gajic, O., Goldstein, J.N., Linko, R. and De Oliveira, R.P., 2015. Lung-protective
ventilation with low tidal volumes and the occurrence of pulmonary complications in patients
without acute respiratory distress syndrome: a systematic review and individual patient data
analysis. Critical care medicine, 43(10), pp.2155-2163.
Pediatric Acute Lung Injury Consensus Conference Group, 2015. Pediatric acute respiratory
distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury
Consensus Conference. Pediatric critical care medicine: a journal of the Society of Critical
EXACERBATION OF ASTHMA
Lee, H.Y., Rhee, C.K. and Lee, J.W., 2015. Feasibility of high-flow nasal cannula oxygen
therapy for acute respiratory failure in patients with hematologic malignancies: a
retrospective single-center study. Journal of critical care, 30(4), pp.773-777.
Lemiale, V., Mokart, D., Resche-Rigon, M., Pène, F., Mayaux, J., Faucher, E., Nyunga, M.,
Girault, C., Perez, P., Guitton, C. and Ekpe, K., 2015. Effect of noninvasive ventilation vs
oxygen therapy on mortality among immunocompromised patients with acute respiratory
failure: a randomized clinical trial. Jama, 314(16), pp.1711-1719.
Lemiale, V., Resche-Rigon, M., Mokart, D., Pène, F., Rabbat, A., Kouatchet, A., Vincent, F.,
Bruneel, F., Nyunga, M., Lebert, C. and Perez, P., 2015. Acute respiratory failure in patients
with hematological malignancies: outcomes according to initial ventilation strategy. A groupe
de recherche respiratoire en réanimation onco-hématologique (Grrr-OH) study. Annals of
intensive care, 5(1), p.28.
Mac Sweeney, R. and McAuley, D.F., 2016. Acute respiratory distress syndrome. The
Lancet, 388(10058), pp.2416-2430.
Neto, A.S., Simonis, F.D., Barbas, C.S., Biehl, M., Determann, R.M., Elmer, J., Friedman,
G., Gajic, O., Goldstein, J.N., Linko, R. and De Oliveira, R.P., 2015. Lung-protective
ventilation with low tidal volumes and the occurrence of pulmonary complications in patients
without acute respiratory distress syndrome: a systematic review and individual patient data
analysis. Critical care medicine, 43(10), pp.2155-2163.
Pediatric Acute Lung Injury Consensus Conference Group, 2015. Pediatric acute respiratory
distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury
Consensus Conference. Pediatric critical care medicine: a journal of the Society of Critical
11
EXACERBATION OF ASTHMA
Care Medicine and the World Federation of Pediatric Intensive and Critical Care
Societies, 16(5), p.428.
Ranieri, V.M., Suter, P.M., Tortorella, C., De Tullio, R., Dayer, J.M., Brienza, A., Bruno, F.
and Slutsky, A.S., 2016. Effect of mechanical ventilation on inflammatory mediators in
patients with acute respiratory distress syndrome: a randomized controlled
trial. Jama, 282(1), pp.54-61.
Scaravilli, V., Grasselli, G., Castagna, L., Zanella, A., Isgrò, S., Lucchini, A., Patroniti, N.,
Bellani, G. and Pesenti, A., 2015. Prone positioning improves oxygenation in spontaneously
breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective
study. Journal of critical care, 30(6), pp.1390-1394.
Schmidt, M., Bailey, M., Sheldrake, J., Hodgson, C., Aubron, C., Rycus, P.T., Scheinkestel,
C., Cooper, D.J., Brodie, D., Pellegrino, V. and Combes, A., 2014. Predicting survival after
extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory
Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. American journal
of respiratory and critical care medicine, 189(11), pp.1374-1382.
Villar, J., Sulemanji, D. and Kacmarek, R.M., 2014. The acute respiratory distress syndrome:
incidence and mortality, has it changed?. Current opinion in critical care, 20(1), pp.3-9.
EXACERBATION OF ASTHMA
Care Medicine and the World Federation of Pediatric Intensive and Critical Care
Societies, 16(5), p.428.
Ranieri, V.M., Suter, P.M., Tortorella, C., De Tullio, R., Dayer, J.M., Brienza, A., Bruno, F.
and Slutsky, A.S., 2016. Effect of mechanical ventilation on inflammatory mediators in
patients with acute respiratory distress syndrome: a randomized controlled
trial. Jama, 282(1), pp.54-61.
Scaravilli, V., Grasselli, G., Castagna, L., Zanella, A., Isgrò, S., Lucchini, A., Patroniti, N.,
Bellani, G. and Pesenti, A., 2015. Prone positioning improves oxygenation in spontaneously
breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective
study. Journal of critical care, 30(6), pp.1390-1394.
Schmidt, M., Bailey, M., Sheldrake, J., Hodgson, C., Aubron, C., Rycus, P.T., Scheinkestel,
C., Cooper, D.J., Brodie, D., Pellegrino, V. and Combes, A., 2014. Predicting survival after
extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory
Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. American journal
of respiratory and critical care medicine, 189(11), pp.1374-1382.
Villar, J., Sulemanji, D. and Kacmarek, R.M., 2014. The acute respiratory distress syndrome:
incidence and mortality, has it changed?. Current opinion in critical care, 20(1), pp.3-9.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




