Analyzing Value-Based Healthcare Reform in Australia: A Report
VerifiedAdded on 2023/06/04
|18
|4867
|385
Report
AI Summary
This report examines the role of health economics in managing chronic diseases within the Australian healthcare system. It highlights the increasing demand for chronic disease care due to an aging population and lifestyle changes, emphasizing the need for healthcare reform. The study analyzes the effectiveness of health economics in mitigating chronic disease issues, the importance of healthcare reform systems, and ten guiding principles for developing a sustainable chronic healthcare setting. It further discusses market concentration, supply chain importance, demand for healthcare facilities, demographic influences, and regulatory authority. The report concludes with recommendations for addressing key problems in the Australian healthcare setting and promoting financial sustainability in chronic healthcare, offering valuable insights for policymakers and healthcare professionals. Desklib offers a platform to explore similar solved assignments and reports.
HEALTH ECONOMICS
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Executive Summary
The study has unfolded the importance of health economics in nursing healthcare settings on
chronic disease. The context of the analysis of the importance of health economics is a
chronic disease. Chronic disease is in high demand among both the urban and rural
population in Australia. People are easily affected by chronic disease. The study has analysed
that the effectiveness of health economics has the ability to mitigate the chronic disease issue
from Australia. The importance of healthcare reform system has been analysed in the study
on rational perspective. Ten guiding principles of healthcare reform system has been analysed
in the study to develop the present chronic healthcare setting in Australia. Additionally,
market concentration, the importance of supply chain in the chronic healthcare setting,
demand of healthcare facility from the disease, demand for the volume of healthcare setting
and the importance of demography and regulatory authority has been described in précised
manner. The recommendation part has located the key problems in the healthcare setting of
Australia and has provided four specific recommendations for each issue. The concluding
part has summarised the whole discussion and located an overall recommendation on the
development of chronic healthcare setting in Australia keeping alignment to the financial
capability of the target population.
1 | P a g e
The study has unfolded the importance of health economics in nursing healthcare settings on
chronic disease. The context of the analysis of the importance of health economics is a
chronic disease. Chronic disease is in high demand among both the urban and rural
population in Australia. People are easily affected by chronic disease. The study has analysed
that the effectiveness of health economics has the ability to mitigate the chronic disease issue
from Australia. The importance of healthcare reform system has been analysed in the study
on rational perspective. Ten guiding principles of healthcare reform system has been analysed
in the study to develop the present chronic healthcare setting in Australia. Additionally,
market concentration, the importance of supply chain in the chronic healthcare setting,
demand of healthcare facility from the disease, demand for the volume of healthcare setting
and the importance of demography and regulatory authority has been described in précised
manner. The recommendation part has located the key problems in the healthcare setting of
Australia and has provided four specific recommendations for each issue. The concluding
part has summarised the whole discussion and located an overall recommendation on the
development of chronic healthcare setting in Australia keeping alignment to the financial
capability of the target population.
1 | P a g e
Table of Contents
Executive Summary...................................................................................................................1
Introduction................................................................................................................................3
Health care reform system.........................................................................................................3
Guiding principles of the health care reforms............................................................................5
Analysis......................................................................................................................................8
Market concentration.............................................................................................................8
The elasticity of the supply chain...........................................................................................9
Elasticity of demand...............................................................................................................9
The need for volume..............................................................................................................9
Population demography’s.....................................................................................................10
Risk transfer.........................................................................................................................10
Regulatory Authority...........................................................................................................10
Execution of the health reform framework..........................................................................10
Recommendation......................................................................................................................11
Conclusion................................................................................................................................12
Reference List..........................................................................................................................14
2 | P a g e
Executive Summary...................................................................................................................1
Introduction................................................................................................................................3
Health care reform system.........................................................................................................3
Guiding principles of the health care reforms............................................................................5
Analysis......................................................................................................................................8
Market concentration.............................................................................................................8
The elasticity of the supply chain...........................................................................................9
Elasticity of demand...............................................................................................................9
The need for volume..............................................................................................................9
Population demography’s.....................................................................................................10
Risk transfer.........................................................................................................................10
Regulatory Authority...........................................................................................................10
Execution of the health reform framework..........................................................................10
Recommendation......................................................................................................................11
Conclusion................................................................................................................................12
Reference List..........................................................................................................................14
2 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Introduction
Health economics is a study that allows a systematic identification of the healthcare problems
through its economic value for the treatment of chronic disease. The healthcare system is
moved away by the traditional approach and in terms of measuring its volume and output
which is needed to be resolved through effective cost measurement to provide quality care to
the patients suffering from chronic disease. This theory aims to develop a behavioural
understanding of both public and private healthcare providers. Moreover, the decision-
making process of healthcare policies is standardized with the effective implementation of
health economics at the chronic healthcare setting. It is notable that the evaluation of health
care economics on chronic disease has become so popular in the present Australia society.
The technological capacity of the healthcare resources is the key source of discussion of
healthcare economics. The demand for public healthcare doer chronic diseases is gradually
increasing over the years. Thus, to keep sustainability with the increase of healthcare demand
in chronic disease, the requirement of health economics is also increasing potentially. The
need for financial resources has become impactful on availing healthcare services. The
ultimate aim of the economic evaluation of chronic healthcare is to assist the decision-making
process for the policymakers for the treatment of the patients suffering from chronic disease.
The chronic healthcare decision and values have become more explicit to sustain cost and
benefit with equal balance. This study will unfold the ethical principles of chronic healthcare
principles. Ten principles will be discussed for a better understanding to provide cost
effective treatment to the patients suffering from chronic disease. The importance of market
concentration along with the capability of the supply chain in chronic health care economics
will also be discussed in the study. The importance of elasticity, volume and the demographic
population will be discussed in the context of chronic health economics to resolve the chronic
healthcare disease. The associated risk factors will be analysed and probable regulatory
authority to mitigate the chronic healthcare risks and financial risks will be discussed. The
execution of the overall chronic healthcare framework will be analysed followed by some key
recommendations for the development of chronic healthcare issues keeping sustainability
with the health economics. The concluding part of the study will summarise the whole
discussion and will outline an overall recommendation.
3 | P a g e
Health economics is a study that allows a systematic identification of the healthcare problems
through its economic value for the treatment of chronic disease. The healthcare system is
moved away by the traditional approach and in terms of measuring its volume and output
which is needed to be resolved through effective cost measurement to provide quality care to
the patients suffering from chronic disease. This theory aims to develop a behavioural
understanding of both public and private healthcare providers. Moreover, the decision-
making process of healthcare policies is standardized with the effective implementation of
health economics at the chronic healthcare setting. It is notable that the evaluation of health
care economics on chronic disease has become so popular in the present Australia society.
The technological capacity of the healthcare resources is the key source of discussion of
healthcare economics. The demand for public healthcare doer chronic diseases is gradually
increasing over the years. Thus, to keep sustainability with the increase of healthcare demand
in chronic disease, the requirement of health economics is also increasing potentially. The
need for financial resources has become impactful on availing healthcare services. The
ultimate aim of the economic evaluation of chronic healthcare is to assist the decision-making
process for the policymakers for the treatment of the patients suffering from chronic disease.
The chronic healthcare decision and values have become more explicit to sustain cost and
benefit with equal balance. This study will unfold the ethical principles of chronic healthcare
principles. Ten principles will be discussed for a better understanding to provide cost
effective treatment to the patients suffering from chronic disease. The importance of market
concentration along with the capability of the supply chain in chronic health care economics
will also be discussed in the study. The importance of elasticity, volume and the demographic
population will be discussed in the context of chronic health economics to resolve the chronic
healthcare disease. The associated risk factors will be analysed and probable regulatory
authority to mitigate the chronic healthcare risks and financial risks will be discussed. The
execution of the overall chronic healthcare framework will be analysed followed by some key
recommendations for the development of chronic healthcare issues keeping sustainability
with the health economics. The concluding part of the study will summarise the whole
discussion and will outline an overall recommendation.
3 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health care reform system
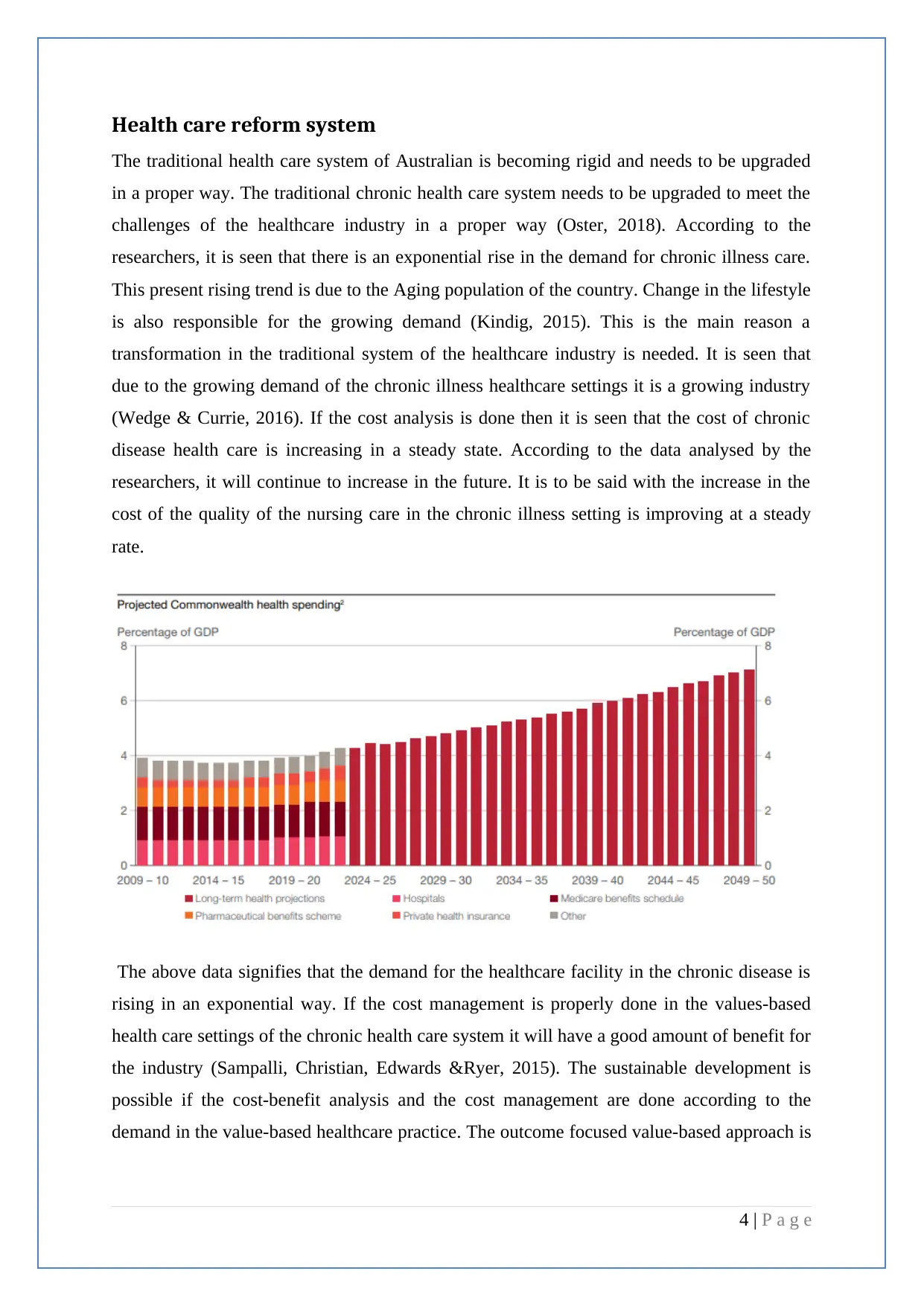
The traditional health care system of Australian is becoming rigid and needs to be upgraded
in a proper way. The traditional chronic health care system needs to be upgraded to meet the
challenges of the healthcare industry in a proper way (Oster, 2018). According to the
researchers, it is seen that there is an exponential rise in the demand for chronic illness care.
This present rising trend is due to the Aging population of the country. Change in the lifestyle
is also responsible for the growing demand (Kindig, 2015). This is the main reason a
transformation in the traditional system of the healthcare industry is needed. It is seen that
due to the growing demand of the chronic illness healthcare settings it is a growing industry
(Wedge & Currie, 2016). If the cost analysis is done then it is seen that the cost of chronic
disease health care is increasing in a steady state. According to the data analysed by the
researchers, it will continue to increase in the future. It is to be said with the increase in the
cost of the quality of the nursing care in the chronic illness setting is improving at a steady
rate.
The above data signifies that the demand for the healthcare facility in the chronic disease is
rising in an exponential way. If the cost management is properly done in the values-based
health care settings of the chronic health care system it will have a good amount of benefit for
the industry (Sampalli, Christian, Edwards &Ryer, 2015). The sustainable development is
possible if the cost-benefit analysis and the cost management are done according to the
demand in the value-based healthcare practice. The outcome focused value-based approach is
4 | P a g e
The traditional health care system of Australian is becoming rigid and needs to be upgraded
in a proper way. The traditional chronic health care system needs to be upgraded to meet the
challenges of the healthcare industry in a proper way (Oster, 2018). According to the
researchers, it is seen that there is an exponential rise in the demand for chronic illness care.
This present rising trend is due to the Aging population of the country. Change in the lifestyle
is also responsible for the growing demand (Kindig, 2015). This is the main reason a
transformation in the traditional system of the healthcare industry is needed. It is seen that
due to the growing demand of the chronic illness healthcare settings it is a growing industry
(Wedge & Currie, 2016). If the cost analysis is done then it is seen that the cost of chronic
disease health care is increasing in a steady state. According to the data analysed by the
researchers, it will continue to increase in the future. It is to be said with the increase in the
cost of the quality of the nursing care in the chronic illness setting is improving at a steady
rate.
The above data signifies that the demand for the healthcare facility in the chronic disease is
rising in an exponential way. If the cost management is properly done in the values-based
health care settings of the chronic health care system it will have a good amount of benefit for
the industry (Sampalli, Christian, Edwards &Ryer, 2015). The sustainable development is
possible if the cost-benefit analysis and the cost management are done according to the
demand in the value-based healthcare practice. The outcome focused value-based approach is
4 | P a g e
very much important for the healthcare industry (Davidsson, 2018). The main objectives of
the outcome based health care industry are as follows:
A nationally unified health system should be prevalent in case of handling the chronic
disease patients. Besides national unification, it must be controlled in the regional
base to serve according to the regional demands of the patient (Younossi& Henry,
2014).
Some of the important components in case of value-based chronic health care reforms
are performance, information and reporting. These parameters should be properly
implemented in to make the reform cost efficient and outcome focused (Davidsson,
2018).
To meet this exponential demand for chronic illness health care an efficient health
force will be required to serve the nation with an outcome focused service.
To implement the values based health reform system the most important point that is
the funding. If there is no appropriate funding then the reforms will not be possible in
a proper way. It is very much important for the sustainability of the healthcare
industry to have proper amount of funding. Sustainable reforms help in enhancing the
quality and efficiency of the service given to the chronic healthcare patient in the
healthcare settings (Sampalli, Christian, Edwards &Ryer, 2015). It is possible to make
values-based reforms of the chronic disease healthcare settings following some
guiding principles. The principles will help to implement the health care reforms in
such a way that the sustainable development in the health care settings will be
possible (Wedge & Currie, 2016).
Guiding principles of the health care reforms
Due to the exponential increase in the demand of the chronic disease and primary care in
Australia, value-based medical reforms have become one of the essential needs. If the value-
based reforms in the chronic disease and primary care are performed then there will be
sustainable development of the healthcare industry (Kourlaba, Hillas, Vassilakopoulos &
Maniadakis, 2018). There are some guiding principles that help in the implementation of the
value-based guided reforms in the healthcare industry. The principles are as below:
Principle 1: A holistic view of well being of the patient
Principle 2: Service provided the centre with the patient and his family
5 | P a g e
the outcome based health care industry are as follows:
A nationally unified health system should be prevalent in case of handling the chronic
disease patients. Besides national unification, it must be controlled in the regional
base to serve according to the regional demands of the patient (Younossi& Henry,
2014).
Some of the important components in case of value-based chronic health care reforms
are performance, information and reporting. These parameters should be properly
implemented in to make the reform cost efficient and outcome focused (Davidsson,
2018).
To meet this exponential demand for chronic illness health care an efficient health
force will be required to serve the nation with an outcome focused service.
To implement the values based health reform system the most important point that is
the funding. If there is no appropriate funding then the reforms will not be possible in
a proper way. It is very much important for the sustainability of the healthcare
industry to have proper amount of funding. Sustainable reforms help in enhancing the
quality and efficiency of the service given to the chronic healthcare patient in the
healthcare settings (Sampalli, Christian, Edwards &Ryer, 2015). It is possible to make
values-based reforms of the chronic disease healthcare settings following some
guiding principles. The principles will help to implement the health care reforms in
such a way that the sustainable development in the health care settings will be
possible (Wedge & Currie, 2016).
Guiding principles of the health care reforms
Due to the exponential increase in the demand of the chronic disease and primary care in
Australia, value-based medical reforms have become one of the essential needs. If the value-
based reforms in the chronic disease and primary care are performed then there will be
sustainable development of the healthcare industry (Kourlaba, Hillas, Vassilakopoulos &
Maniadakis, 2018). There are some guiding principles that help in the implementation of the
value-based guided reforms in the healthcare industry. The principles are as below:
Principle 1: A holistic view of well being of the patient
Principle 2: Service provided the centre with the patient and his family
5 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Principle 3: Collaboration and continuous relationship
Principle 4: A holistic team-based approach
Principle 5: Shared decision making and engagement of patient care in a proper way.
Principle 6: Coordinating proper care across the chronic disease health care system.
Principle 7: Maintenance of equitability, affordability in the appropriate care of the
patient
Principle 8: an Evidenced base system with quality care and improvement
Principle 9: Efficient workforce and infrastructure to support the quality care.
Principle 10: Proper funding to make the reform sustainable for the feature.
Principle 1: A holistic view of the wellbeing of the patient
According to the principle, the fundamental aim is to provide a holistic care for the
chronic healthcare patient in a proper way. The total health care system should be
patient oriented. The problems of the patient should be dealt with the highest priority
(Mozaffari, Peyrovi, & Nayeri, 2015). According to this principle, there are broader
views which should be attended if the holistic transformation of patient-centric
healthcare is to be attended. This transformation in the healthcare industry includes
the emotional spiritual and economical attributes. Community culture and patient-
centric approach should be taken to have a holistic transformation (Ali, Marhemat,
Sara, & Hamid, 2015).The Cross Sectoral relationship and economical components
should be considered properly during the value-based transformation in the healthcare
settings.
Principle 2: Service provided centring the patient and his family
This principle depicts that patient should be at the middle of every transforming steps.
The chronic disease healthcare setting should be totally patient-centric. It explains that
chronic health care setting should be person oriented (Chiara, 2018). The social and
cultural and economic background of the patients should be acknowledged for the
holistic development of the care settings. The patient's preferences should be
comprehended and respected in a proper manner (Patton & Dalton, 2015). It is said
that the patient should be the partners in care planning and design. According to the
Australian Commission on safety and quality in health service standard consumers
can be made partners in the implementation of the value-based transformation through
proper cost management (Chiara, 2018).
6 | P a g e
Principle 4: A holistic team-based approach
Principle 5: Shared decision making and engagement of patient care in a proper way.
Principle 6: Coordinating proper care across the chronic disease health care system.
Principle 7: Maintenance of equitability, affordability in the appropriate care of the
patient
Principle 8: an Evidenced base system with quality care and improvement
Principle 9: Efficient workforce and infrastructure to support the quality care.
Principle 10: Proper funding to make the reform sustainable for the feature.
Principle 1: A holistic view of the wellbeing of the patient
According to the principle, the fundamental aim is to provide a holistic care for the
chronic healthcare patient in a proper way. The total health care system should be
patient oriented. The problems of the patient should be dealt with the highest priority
(Mozaffari, Peyrovi, & Nayeri, 2015). According to this principle, there are broader
views which should be attended if the holistic transformation of patient-centric
healthcare is to be attended. This transformation in the healthcare industry includes
the emotional spiritual and economical attributes. Community culture and patient-
centric approach should be taken to have a holistic transformation (Ali, Marhemat,
Sara, & Hamid, 2015).The Cross Sectoral relationship and economical components
should be considered properly during the value-based transformation in the healthcare
settings.
Principle 2: Service provided centring the patient and his family
This principle depicts that patient should be at the middle of every transforming steps.
The chronic disease healthcare setting should be totally patient-centric. It explains that
chronic health care setting should be person oriented (Chiara, 2018). The social and
cultural and economic background of the patients should be acknowledged for the
holistic development of the care settings. The patient's preferences should be
comprehended and respected in a proper manner (Patton & Dalton, 2015). It is said
that the patient should be the partners in care planning and design. According to the
Australian Commission on safety and quality in health service standard consumers
can be made partners in the implementation of the value-based transformation through
proper cost management (Chiara, 2018).
6 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Principle 3: Collaboration and continuous relationship
There should be a proper collaboration between the departments in implementing the
transformation needed for the healthcare purpose. In this principle, it is said that the
relationship between the patient and the chronic healthcare team should be longitudinal in
nature (Markowski&Dabhilkar, 2016). To provide the optimum care in the chronic illness
care setting through proper cost benefit analysis is the main aim. By nurturing the health
and economic relationship between the medical professionals and the patient's holistic
transformation can be possible (Yan, 2017). Through this holistic approach sustainable
development in the chronic illness care setting is possible.
Principle 4: A holistic team-based approach
A holistic team-based approach is very much essential to implement the transformation in
a proper way. The accountability of the medical professionals towards the chronic
healthcare patient should be increased (Huljev&Pandak, 2016). A holistic team-based
approach will optimize resource use and decrease the overall cost. Through proper
funding and capacity building training, it should be implemented. A holistic team-based
approach will help to achieve sustainable development in the transformation of chronic
disease healthcare settings (Dyess, 2015).
Principle 5: Shared decision making and engagement of patient care in a proper
way
This principle depicts the proper capacity building of the employees through proper
training. Investment is also required that will enable the training to be conducted. It helps
in enhancing the quality of service in emergency situations (Rehman, 2016). Decision-
making process is enhanced through a proper capacity building. Documentation of
chronic healthcare reports should be done in a proper way. Consent should be taken from
the patient before starting the treatment procedure (Tappet al., 2016).
Principle 6: Coordinating proper care across the chronic disease health care
system.
Proper coordination is one of the most essential parameters needed for the sustainability
of the transformation in the healthcare sector. Pro activeness enhances the coordinated
7 | P a g e
There should be a proper collaboration between the departments in implementing the
transformation needed for the healthcare purpose. In this principle, it is said that the
relationship between the patient and the chronic healthcare team should be longitudinal in
nature (Markowski&Dabhilkar, 2016). To provide the optimum care in the chronic illness
care setting through proper cost benefit analysis is the main aim. By nurturing the health
and economic relationship between the medical professionals and the patient's holistic
transformation can be possible (Yan, 2017). Through this holistic approach sustainable
development in the chronic illness care setting is possible.
Principle 4: A holistic team-based approach
A holistic team-based approach is very much essential to implement the transformation in
a proper way. The accountability of the medical professionals towards the chronic
healthcare patient should be increased (Huljev&Pandak, 2016). A holistic team-based
approach will optimize resource use and decrease the overall cost. Through proper
funding and capacity building training, it should be implemented. A holistic team-based
approach will help to achieve sustainable development in the transformation of chronic
disease healthcare settings (Dyess, 2015).
Principle 5: Shared decision making and engagement of patient care in a proper
way
This principle depicts the proper capacity building of the employees through proper
training. Investment is also required that will enable the training to be conducted. It helps
in enhancing the quality of service in emergency situations (Rehman, 2016). Decision-
making process is enhanced through a proper capacity building. Documentation of
chronic healthcare reports should be done in a proper way. Consent should be taken from
the patient before starting the treatment procedure (Tappet al., 2016).
Principle 6: Coordinating proper care across the chronic disease health care
system.
Proper coordination is one of the most essential parameters needed for the sustainability
of the transformation in the healthcare sector. Pro activeness enhances the coordinated
7 | P a g e
care among the chronic healthcare patients (Kim, 2014). It helps to develop interpersonal
relation among medical professionals in giving quality service in economic manner.
Principle 7: Maintenance of equitability, affordability in the appropriate care of the
patient
This is another major reason for the reforms. There is not much lack of equitable
distribution of appropriate care and sustainable cost. This can be implemented by proper
economic reforms of the settings (Warshaw, 2015). It is one of the most essential
requirements that must be fulfilled in chronic disease care settings.
Principle 8: the Evidenced base system with quality care and improvement
There should be more practice of evidence-based nursing. This will improve the quality
care received by the chronic healthcare patient. Through evidence-based nursing and
equitable distribution of quality care and proper cost management the main
transformation can be in the chronic illness care settings (Hamer, 2013).
Principle 9: Efficient workforce and infrastructure to support the quality care.
Proper funding should be provided for the capacity building of the workforce. The proper
capacity building of the workforce will help to enable the transformation. Infrastructure
development is also essential (Hamer, 2013). The infrastructure should be upgraded with
the installation of the modern equipment of nursing assessments. Steady funding from the
government agencies is required for the sustainability of the transformation (Kim, 2014).
Principle 10: Proper funding to make the reform sustainable for the feature.
Principle 10 is almost the same as principal 9. It states that for the sustainability of the
transformation a steady funding source is required.
8 | P a g e
relation among medical professionals in giving quality service in economic manner.
Principle 7: Maintenance of equitability, affordability in the appropriate care of the
patient
This is another major reason for the reforms. There is not much lack of equitable
distribution of appropriate care and sustainable cost. This can be implemented by proper
economic reforms of the settings (Warshaw, 2015). It is one of the most essential
requirements that must be fulfilled in chronic disease care settings.
Principle 8: the Evidenced base system with quality care and improvement
There should be more practice of evidence-based nursing. This will improve the quality
care received by the chronic healthcare patient. Through evidence-based nursing and
equitable distribution of quality care and proper cost management the main
transformation can be in the chronic illness care settings (Hamer, 2013).
Principle 9: Efficient workforce and infrastructure to support the quality care.
Proper funding should be provided for the capacity building of the workforce. The proper
capacity building of the workforce will help to enable the transformation. Infrastructure
development is also essential (Hamer, 2013). The infrastructure should be upgraded with
the installation of the modern equipment of nursing assessments. Steady funding from the
government agencies is required for the sustainability of the transformation (Kim, 2014).
Principle 10: Proper funding to make the reform sustainable for the feature.
Principle 10 is almost the same as principal 9. It states that for the sustainability of the
transformation a steady funding source is required.
8 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Analysis
Market concentration
The evaluation of health economics for chronic disease care in Australia is helpful to
understand the present care setting. Additionally, the comparison of the chronic disease care
setting between Australia and the international market is effective in planning for care
programs (Brunt&Bowblis, 2016). Thus, on the theory of market concentration, the
objectives of chronic disease care in Australia healthcare setting are :
To provide ethically integrated care at a low cost
To provide evidence care practice to the patients suffering from chronic disease
To bring the financially backward patients under national free health check-up skims
To utilise the government resources for the treatment of patients suffering from
chronic disease.
The elasticity of the supply chain
The supply chain in the Australian chronic healthcare setting has the effectiveness to provide
efficient care service to the patients. The cost of the supply chain in the chronic healthcare
setting in Australia is second largest (Jia, 2017). It is presumed that the supply chain cost
would surpass the labour cost by 2022. The present trend of Australian healthcare supply
chain is centralised and customer specific. The effective policies taken by the decision
makers are helpful to reduce the supply chain cost in Australia (Johnson & Miller, 2018).
Elasticity of demand
The growing number of chronic disease in Australia is the key reason for the increase in
demand for cost-effective healthcare services in Australia. The patients require ethical care,
potentially developed care plans and effective health care policies(Brunt &Bowblis, 2016).
The reasons for elasticity in demand are :
Advancements in the chronic care treatments in Australia
Self-management policies, regular visits and follow up treatments by healthcare
professionals
The easy availability of medical services through effective marketing policies, low
pricing, long trading house and quality treatment
9 | P a g e
Market concentration
The evaluation of health economics for chronic disease care in Australia is helpful to
understand the present care setting. Additionally, the comparison of the chronic disease care
setting between Australia and the international market is effective in planning for care
programs (Brunt&Bowblis, 2016). Thus, on the theory of market concentration, the
objectives of chronic disease care in Australia healthcare setting are :
To provide ethically integrated care at a low cost
To provide evidence care practice to the patients suffering from chronic disease
To bring the financially backward patients under national free health check-up skims
To utilise the government resources for the treatment of patients suffering from
chronic disease.
The elasticity of the supply chain
The supply chain in the Australian chronic healthcare setting has the effectiveness to provide
efficient care service to the patients. The cost of the supply chain in the chronic healthcare
setting in Australia is second largest (Jia, 2017). It is presumed that the supply chain cost
would surpass the labour cost by 2022. The present trend of Australian healthcare supply
chain is centralised and customer specific. The effective policies taken by the decision
makers are helpful to reduce the supply chain cost in Australia (Johnson & Miller, 2018).
Elasticity of demand
The growing number of chronic disease in Australia is the key reason for the increase in
demand for cost-effective healthcare services in Australia. The patients require ethical care,
potentially developed care plans and effective health care policies(Brunt &Bowblis, 2016).
The reasons for elasticity in demand are :
Advancements in the chronic care treatments in Australia
Self-management policies, regular visits and follow up treatments by healthcare
professionals
The easy availability of medical services through effective marketing policies, low
pricing, long trading house and quality treatment
9 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The need for volume
There is a vast requirement of expanding the volume of chronic healthcare services on
Australia. It is notable that Australia has only 3.4 active physicians per 1000 patients and 3.7
hospital bed for per 1000 chronic disease patients. Thus, the volume must be increasingly
focusing on cultural response, the direction of the goal, healthcare promotion, self-
management and evidence-based and it must be cost effective (Johnson & Miller, 2018).
Population demography’s
The effective chronic healthcare policies must be aligned with the demography of Australia.
The diversified population in Australia have their specific healthcare preferences
(Provenzano, 2016). The demographical chronic healthcare services include cultural respect,
person-centred care and systematic approach to each of the patient (Jia, 2017). Moreover, the
chronic patients under the poverty level must get free of cost health care check-up and must
be included under national healthcare skims.
Risk transfer
The economic risk factors associated with the Australian chronic healthcare setting are lack
of resources, the inefficiency of the caregivers, lack of effective evidence-based practices and
economic discrimination in the healthcare setting. These barriers must be broken with
immediate priority(Warshaw, 2015).
Regulatory Authority
The regulatory authorities of chronic health care diseases under Australian health economics
system are:
Australian Commission for Safety and Quality in Healthcare(ACSQH)
Australian Healthcare Reform Alliance (AHRA)
Australian Health Practitioner Regulatory Agency (AHPRA)
Australian Institute for Patient and Family Centred Care (AIPFCC)
Execution of the health reform framework
The chronic health reform framework in Australia is supervised under the leadership of
National Primary Healthcare Strategy skim. The effective execution of this healthcare reform
10 | P a g e
There is a vast requirement of expanding the volume of chronic healthcare services on
Australia. It is notable that Australia has only 3.4 active physicians per 1000 patients and 3.7
hospital bed for per 1000 chronic disease patients. Thus, the volume must be increasingly
focusing on cultural response, the direction of the goal, healthcare promotion, self-
management and evidence-based and it must be cost effective (Johnson & Miller, 2018).
Population demography’s
The effective chronic healthcare policies must be aligned with the demography of Australia.
The diversified population in Australia have their specific healthcare preferences
(Provenzano, 2016). The demographical chronic healthcare services include cultural respect,
person-centred care and systematic approach to each of the patient (Jia, 2017). Moreover, the
chronic patients under the poverty level must get free of cost health care check-up and must
be included under national healthcare skims.
Risk transfer
The economic risk factors associated with the Australian chronic healthcare setting are lack
of resources, the inefficiency of the caregivers, lack of effective evidence-based practices and
economic discrimination in the healthcare setting. These barriers must be broken with
immediate priority(Warshaw, 2015).
Regulatory Authority
The regulatory authorities of chronic health care diseases under Australian health economics
system are:
Australian Commission for Safety and Quality in Healthcare(ACSQH)
Australian Healthcare Reform Alliance (AHRA)
Australian Health Practitioner Regulatory Agency (AHPRA)
Australian Institute for Patient and Family Centred Care (AIPFCC)
Execution of the health reform framework
The chronic health reform framework in Australia is supervised under the leadership of
National Primary Healthcare Strategy skim. The effective execution of this healthcare reform
10 | P a g e
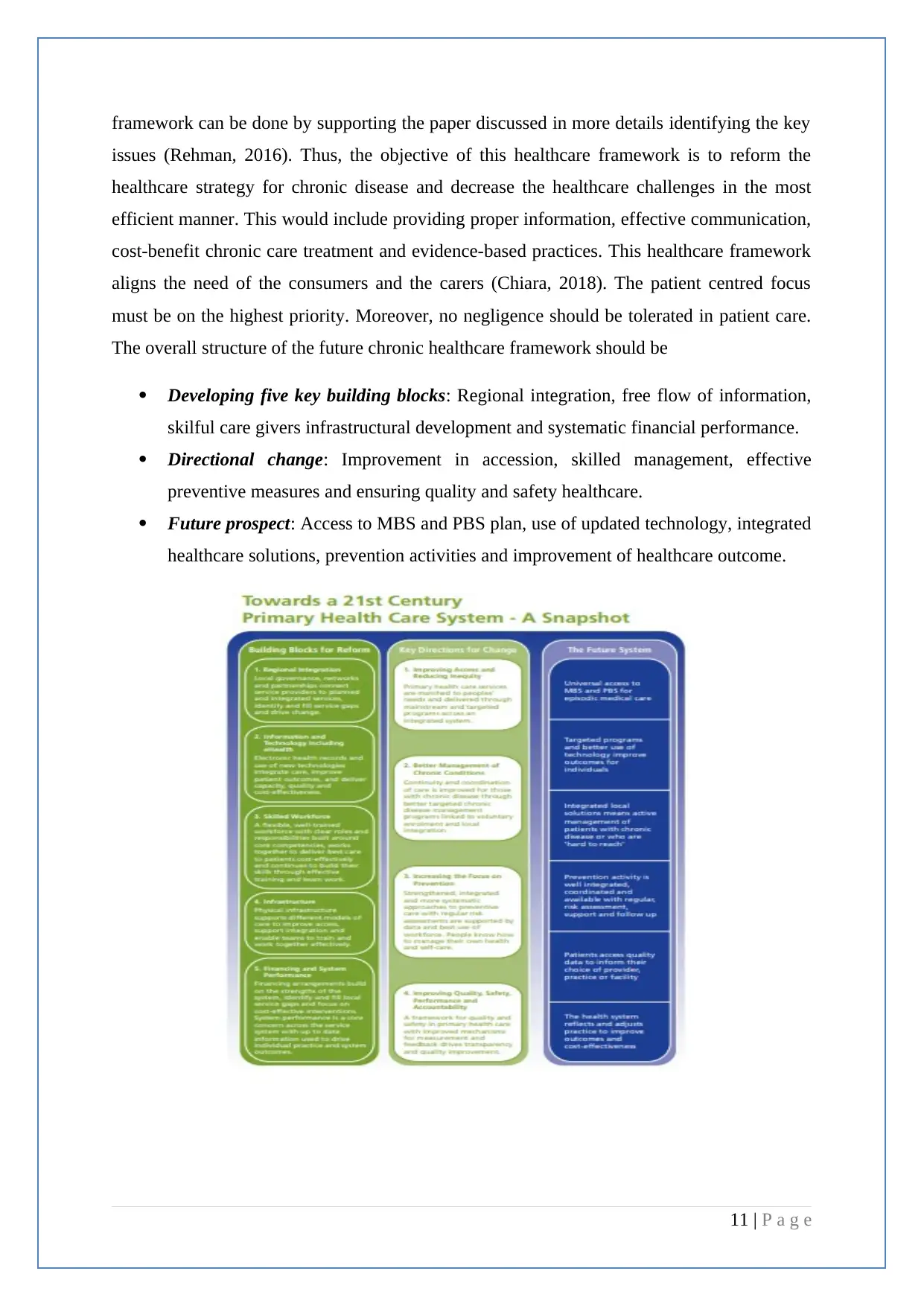
framework can be done by supporting the paper discussed in more details identifying the key
issues (Rehman, 2016). Thus, the objective of this healthcare framework is to reform the
healthcare strategy for chronic disease and decrease the healthcare challenges in the most
efficient manner. This would include providing proper information, effective communication,
cost-benefit chronic care treatment and evidence-based practices. This healthcare framework
aligns the need of the consumers and the carers (Chiara, 2018). The patient centred focus
must be on the highest priority. Moreover, no negligence should be tolerated in patient care.
The overall structure of the future chronic healthcare framework should be
Developing five key building blocks: Regional integration, free flow of information,
skilful care givers infrastructural development and systematic financial performance.
Directional change: Improvement in accession, skilled management, effective
preventive measures and ensuring quality and safety healthcare.
Future prospect: Access to MBS and PBS plan, use of updated technology, integrated
healthcare solutions, prevention activities and improvement of healthcare outcome.
11 | P a g e
issues (Rehman, 2016). Thus, the objective of this healthcare framework is to reform the
healthcare strategy for chronic disease and decrease the healthcare challenges in the most
efficient manner. This would include providing proper information, effective communication,
cost-benefit chronic care treatment and evidence-based practices. This healthcare framework
aligns the need of the consumers and the carers (Chiara, 2018). The patient centred focus
must be on the highest priority. Moreover, no negligence should be tolerated in patient care.
The overall structure of the future chronic healthcare framework should be
Developing five key building blocks: Regional integration, free flow of information,
skilful care givers infrastructural development and systematic financial performance.
Directional change: Improvement in accession, skilled management, effective
preventive measures and ensuring quality and safety healthcare.
Future prospect: Access to MBS and PBS plan, use of updated technology, integrated
healthcare solutions, prevention activities and improvement of healthcare outcome.
11 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




