Sustainability and Value-Based Care in Australian Health System
VerifiedAdded on 2023/06/03
|19
|5288
|485
Report
AI Summary
This report provides an overview of health economics and comparative health systems, with a focus on the Australian healthcare system. It begins by defining healthcare systems and value-based care, contrasting it with the traditional fee-for-service model. The report then maps and evaluates the sustainability of the Australian healthcare system, considering factors such as increasing technology costs, market concentration, the need for volume, an aging population, and increased chronic diseases. It also discusses the principles of value-based healthcare as outlined by the Australian Charter of Healthcare Rights, including the right to access, respect, and high-quality care. The report concludes with recommendations for improving the sustainability of the Australian healthcare system, emphasizing the need for fiscal responsibility, technological advancements, and a focus on patient-centered care.

Running head: HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Health economics and comparative Health systems
Name of the student
Name of the University
Author Note
Health economics and comparative Health systems
Name of the student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Executive Summary:
Healthcare system represents the method through which an economy finances, organises and
delivers its health care facilities to a large number of populations. This system access various
issues related to stakeholders, expenditures as well as resources that include facilities and
healthcare workers. The chief focus of healthcare system is to develop the health condition of
people through an effective and successive way applying available resources of the society.
Value-based care represents the healthcare philosophy that can be obtained when
professionals consider the quality related to care. This care is provided to people
intentionally. Thus, the entire outcome depends on cost-efficiency. Thus, in this modern
model, doctors as well as specialists consider data with evidence for giving best practices at
the time of treating patients. However, traditional healthcare represents the environment,
where physicians consider the number of services they provide. In this system, physicians
consider the number of procedures that they order for applying reimbursement. This system is
known as “fee-for-service” (FFS) related to reimbursement model. To understand this
situation in practical field, this paper considers health scenario of Australia. The chief
purpose of this report is to mapping and evaluating the sustainability of healthcare system in
this country. In conclusion, it can be said that health care system is an essential factor of an
economy for serving its large number of population. The Australian Charter of Healthcare
Rights has also provided some principles describing about rights of patients under the health
care system of the country. For helping people to obtain value-based services, Charter has
provided some principles related to right to access, right to receive respects and right to
receive care with high quality. Some other principles have been described as well. After
discussing these principles, the paper has considered about sustainability issues related to the
health care service.
Executive Summary:
Healthcare system represents the method through which an economy finances, organises and
delivers its health care facilities to a large number of populations. This system access various
issues related to stakeholders, expenditures as well as resources that include facilities and
healthcare workers. The chief focus of healthcare system is to develop the health condition of
people through an effective and successive way applying available resources of the society.
Value-based care represents the healthcare philosophy that can be obtained when
professionals consider the quality related to care. This care is provided to people
intentionally. Thus, the entire outcome depends on cost-efficiency. Thus, in this modern
model, doctors as well as specialists consider data with evidence for giving best practices at
the time of treating patients. However, traditional healthcare represents the environment,
where physicians consider the number of services they provide. In this system, physicians
consider the number of procedures that they order for applying reimbursement. This system is
known as “fee-for-service” (FFS) related to reimbursement model. To understand this
situation in practical field, this paper considers health scenario of Australia. The chief
purpose of this report is to mapping and evaluating the sustainability of healthcare system in
this country. In conclusion, it can be said that health care system is an essential factor of an
economy for serving its large number of population. The Australian Charter of Healthcare
Rights has also provided some principles describing about rights of patients under the health
care system of the country. For helping people to obtain value-based services, Charter has
provided some principles related to right to access, right to receive respects and right to
receive care with high quality. Some other principles have been described as well. After
discussing these principles, the paper has considered about sustainability issues related to the
health care service.
2HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Table of Contents
Introduction:...............................................................................................................................3
Principles based on value-based healthcare system:..................................................................4
Sustainability of healthcare service:...........................................................................................7
Increasing cost of technology:...............................................................................................7
Market concentration:............................................................................................................9
The need for volume:.............................................................................................................9
The aging population:..........................................................................................................10
Increased chronic diseases:..................................................................................................11
Recommendations:...................................................................................................................11
Conclusion:..............................................................................................................................13
References:...............................................................................................................................15
Table of Contents
Introduction:...............................................................................................................................3
Principles based on value-based healthcare system:..................................................................4
Sustainability of healthcare service:...........................................................................................7
Increasing cost of technology:...............................................................................................7
Market concentration:............................................................................................................9
The need for volume:.............................................................................................................9
The aging population:..........................................................................................................10
Increased chronic diseases:..................................................................................................11
Recommendations:...................................................................................................................11
Conclusion:..............................................................................................................................13
References:...............................................................................................................................15
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Introduction:
Healthcare system represents the method through which an economy finances,
organises and delivers its health care facilities to a large number of populations. This system
access various issues related to stakeholders, expenditures as well as resources that include
facilities and healthcare workers. The chief focus of healthcare system is to develop the
health condition of people through an effective and successive way applying available
resources of the society. Since the beginning of 21st century, accessing healthcare system has
become an important issue for the government of any country. This system has been
considered as a special good, which is required to maintain human rights. Therefore, an
analysis of healthcare systems considers value creation (Sweeney, Danaher & McColl-
Kennedy, 2015). In modern world, healthcare system follows value-based care considering
health outcomes, experience of care and efficient and effective care depending on costs.
Previously, this healthcare system was depended on traditional approach, where value was
measured in terms of volume or output depending on costs. Value-based care represents the
healthcare philosophy that can be obtained when professionals consider the quality related to
care. This care is provided to people intentionally (Scott, Liu & Yong, 2018). Thus, the entire
outcome depends on cost-efficiency. Thus, in this modern model, doctors as well as
specialists consider data with evidence for giving best practices at the time of treating
patients. On the contrary, traditional healthcare represents the environment, where physicians
consider the number of services they provide (Bal et al., 2016). In this system, physicians
consider the number of procedures that they order for applying reimbursement. This system is
known as “fee-for-service” (FFS) related to reimbursement model.
Thus, according to some researchers, the model of FFS payment related to healthcare
is a cost-driving model that increases costs of healthcare services (Sanders et al., 2016). The
model does this in order to encourage and incentivise physicians to use expensive services.
Introduction:
Healthcare system represents the method through which an economy finances,
organises and delivers its health care facilities to a large number of populations. This system
access various issues related to stakeholders, expenditures as well as resources that include
facilities and healthcare workers. The chief focus of healthcare system is to develop the
health condition of people through an effective and successive way applying available
resources of the society. Since the beginning of 21st century, accessing healthcare system has
become an important issue for the government of any country. This system has been
considered as a special good, which is required to maintain human rights. Therefore, an
analysis of healthcare systems considers value creation (Sweeney, Danaher & McColl-
Kennedy, 2015). In modern world, healthcare system follows value-based care considering
health outcomes, experience of care and efficient and effective care depending on costs.
Previously, this healthcare system was depended on traditional approach, where value was
measured in terms of volume or output depending on costs. Value-based care represents the
healthcare philosophy that can be obtained when professionals consider the quality related to
care. This care is provided to people intentionally (Scott, Liu & Yong, 2018). Thus, the entire
outcome depends on cost-efficiency. Thus, in this modern model, doctors as well as
specialists consider data with evidence for giving best practices at the time of treating
patients. On the contrary, traditional healthcare represents the environment, where physicians
consider the number of services they provide (Bal et al., 2016). In this system, physicians
consider the number of procedures that they order for applying reimbursement. This system is
known as “fee-for-service” (FFS) related to reimbursement model.
Thus, according to some researchers, the model of FFS payment related to healthcare
is a cost-driving model that increases costs of healthcare services (Sanders et al., 2016). The
model does this in order to encourage and incentivise physicians to use expensive services.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Therefore, this model influences volume of the services and does not consider quality. To
understand this situation in practical field, this paper considers health scenario of Australia.
The chief purpose of this report is to mapping and evaluating the sustainability of healthcare
system in this country. To discuss further, this paper will discuss about the healthcare system
of this country. After that, some principles will be provided that can guide this specified
system reform of Australia. Following to this, a discussion will be done on sustainability of
healthcare system based on some relevant data. At the end, the report intends to provide
proper recommendations and conclusions based on the entire discussion.
Principles based on value-based healthcare system:
According to the Organisation for Economic Co-operation and Development (OECD),
Australia provides the best healthcare system to people. However, the system experiences
huge pressure for changing requirement of healthcare, for instance, increasing demand as
well as costs, complex conditions of health and inequalities in healthcare (Richardson, Joshy
& D'Este, 2018). The Australian Safety and Quality Framework for Health Care have
provided a vision describing a high-quality care with safety for Australian people. To achieve
this vision, the organisation has set some actions as well. This framework of actions identifies
three chief principles for providing healthcare with standard quality. These principles state
that care needs to be consumer centred, organised for safety and driven for information
(Meurk et al., 2018). Australian Health Care Reform Alliance takes some principles for
developing healthcare facilities of the country. These principles are as follows:
Policies, services as well as programs depending on evidences
Community engagement depending on ongoing and meaningful process
Social determinants related to health perspective
Health system based on strong sector of primary health care
Health workforce considering skilled and flexible workers with greatest potential
Therefore, this model influences volume of the services and does not consider quality. To
understand this situation in practical field, this paper considers health scenario of Australia.
The chief purpose of this report is to mapping and evaluating the sustainability of healthcare
system in this country. To discuss further, this paper will discuss about the healthcare system
of this country. After that, some principles will be provided that can guide this specified
system reform of Australia. Following to this, a discussion will be done on sustainability of
healthcare system based on some relevant data. At the end, the report intends to provide
proper recommendations and conclusions based on the entire discussion.
Principles based on value-based healthcare system:
According to the Organisation for Economic Co-operation and Development (OECD),
Australia provides the best healthcare system to people. However, the system experiences
huge pressure for changing requirement of healthcare, for instance, increasing demand as
well as costs, complex conditions of health and inequalities in healthcare (Richardson, Joshy
& D'Este, 2018). The Australian Safety and Quality Framework for Health Care have
provided a vision describing a high-quality care with safety for Australian people. To achieve
this vision, the organisation has set some actions as well. This framework of actions identifies
three chief principles for providing healthcare with standard quality. These principles state
that care needs to be consumer centred, organised for safety and driven for information
(Meurk et al., 2018). Australian Health Care Reform Alliance takes some principles for
developing healthcare facilities of the country. These principles are as follows:
Policies, services as well as programs depending on evidences
Community engagement depending on ongoing and meaningful process
Social determinants related to health perspective
Health system based on strong sector of primary health care
Health workforce considering skilled and flexible workers with greatest potential
5HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Focusing on wellness of people and addressing ill-health of people successfully
The Department of Health, under the Australian Government has taken some principles
for developing services of primary healthcare (Leslie, 2018). Some of these important
principles are:
1. To maximise participation, genuine community of local indigenous people are
engaged. This engagement will consider formal structure regarding control of
community. This can also involve practice and ethic involving community.
2. Another principle states about collaborative approaches for observing works of
primary healthcare services along with other sectors like housing. These healthcare
services can work with other community-based or other organisations of primary
healthcare service considering both public and private sectors (Health.gov.au, 2018).
Moreover, primary health care services work with other levels of system related with
health care, especially, hospitals and specialists.
3. The next principle states that programs of core healthcare provides long-term health
for the community considering mental as well as child health and detection of chronic
disease to work somewhere else under local priorities and local conditions.
4. The next principle is about evidence-based approaches that reflect an approach of
continuous quality improvement. These approaches also consider local government
for adapting local community to work somewhere else under local conditions as well
as priorities.
5. Other approach is based on a multidisciplinary team that chiefly involves the
employment of community members related to local Aboriginal and Torres Strait
Island. This approach also considers continuous process of training along with support
6. The next approach states to harmonise with local people of Aboriginal community in
their life.
Focusing on wellness of people and addressing ill-health of people successfully
The Department of Health, under the Australian Government has taken some principles
for developing services of primary healthcare (Leslie, 2018). Some of these important
principles are:
1. To maximise participation, genuine community of local indigenous people are
engaged. This engagement will consider formal structure regarding control of
community. This can also involve practice and ethic involving community.
2. Another principle states about collaborative approaches for observing works of
primary healthcare services along with other sectors like housing. These healthcare
services can work with other community-based or other organisations of primary
healthcare service considering both public and private sectors (Health.gov.au, 2018).
Moreover, primary health care services work with other levels of system related with
health care, especially, hospitals and specialists.
3. The next principle states that programs of core healthcare provides long-term health
for the community considering mental as well as child health and detection of chronic
disease to work somewhere else under local priorities and local conditions.
4. The next principle is about evidence-based approaches that reflect an approach of
continuous quality improvement. These approaches also consider local government
for adapting local community to work somewhere else under local conditions as well
as priorities.
5. Other approach is based on a multidisciplinary team that chiefly involves the
employment of community members related to local Aboriginal and Torres Strait
Island. This approach also considers continuous process of training along with support
6. The next approach states to harmonise with local people of Aboriginal community in
their life.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
7. The last principle states to provide secured as well as adequate resources to focus on
management. This principle also states to deliver non-acute care.
The Australian Charter of Healthcare Rights states about the rights of patients and other
people, who use health care system of Australia (Morris, Moore & Bismark, 2018). These
rights are required to make sure that where and when the government is providing care with
high quality and safety. The Charter has recognised that people providing and receiving care
have significant role to achieve healthcare rights. The Charter helps patients, families and
consumers, services and cares to obtain health care through understanding their rights for
obtaining the service (Neil, Murphy & Chapman, 2018). These rights also help people to
work together for gaining a high quality and safe health system. In this context, some guiding
principles are provided. Charter has applied these principles in the health care system of the
country.
1. Each people have the right to access health care. For Charter, this right is essential.
2. Australian society consists with people of different cultures and life style. Charter
respects these differences. All patients have the right to receive respect, consideration
and respect.
3. The government of Australia has done many international agreements related to
human rights. This helps to identify right of every people to obtain higher standard for
physical and mental health. Thus, each patient has the right to receive high quality
care and safe medical treatment.
4. The Charter will inform patients about services, options and treatments along with
costs in a clear and open way.
5. All patients have the right to include decisions and choices for getting care.
6. Each patient has the right to keep his or her personal information private and
confidential.
7. The last principle states to provide secured as well as adequate resources to focus on
management. This principle also states to deliver non-acute care.
The Australian Charter of Healthcare Rights states about the rights of patients and other
people, who use health care system of Australia (Morris, Moore & Bismark, 2018). These
rights are required to make sure that where and when the government is providing care with
high quality and safety. The Charter has recognised that people providing and receiving care
have significant role to achieve healthcare rights. The Charter helps patients, families and
consumers, services and cares to obtain health care through understanding their rights for
obtaining the service (Neil, Murphy & Chapman, 2018). These rights also help people to
work together for gaining a high quality and safe health system. In this context, some guiding
principles are provided. Charter has applied these principles in the health care system of the
country.
1. Each people have the right to access health care. For Charter, this right is essential.
2. Australian society consists with people of different cultures and life style. Charter
respects these differences. All patients have the right to receive respect, consideration
and respect.
3. The government of Australia has done many international agreements related to
human rights. This helps to identify right of every people to obtain higher standard for
physical and mental health. Thus, each patient has the right to receive high quality
care and safe medical treatment.
4. The Charter will inform patients about services, options and treatments along with
costs in a clear and open way.
5. All patients have the right to include decisions and choices for getting care.
6. Each patient has the right to keep his or her personal information private and
confidential.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
The chief focus of these principles is to provide Australian citizens a value-based
medical facility. According to these principles, patients can access various services for
fulfilling their requirement related to healthcare. Under the professional care, patients receive
high-quality health services in a safe process provided by skilled physicians
(Safetyandquality.gov.au, 2018). The entire care process chiefly focuses to provide respects
to patients considering their cultural diversity. Moreover, patients receive facility to
communicate with the government for obtaining proper treatment. In this context, patients
can take decisions and choices regarding their planning for health service. Each patient has
the opportunity keep his or her personal information as private and confidential.
Sustainability of healthcare service:
Increasing cost of technology:
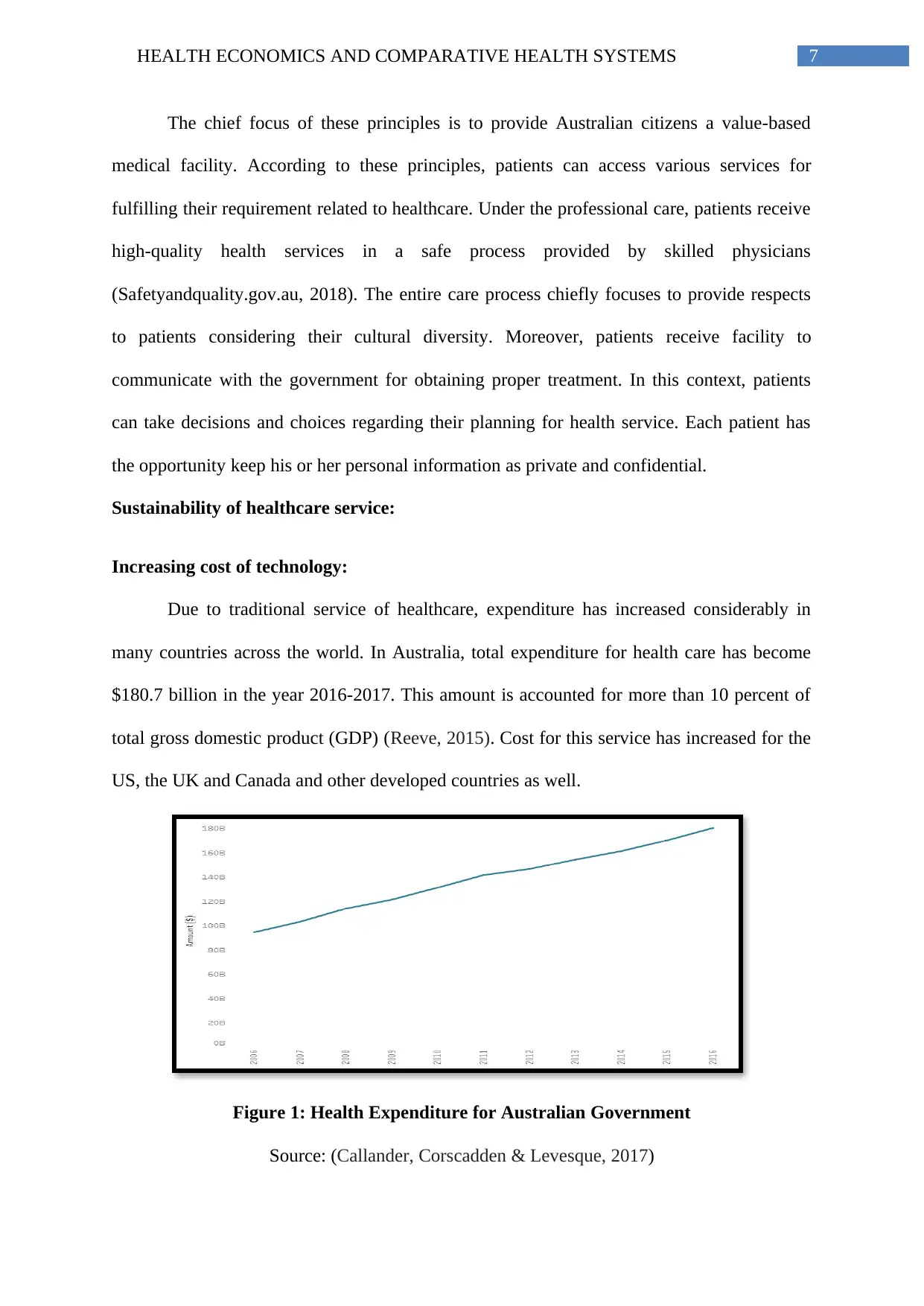
Due to traditional service of healthcare, expenditure has increased considerably in
many countries across the world. In Australia, total expenditure for health care has become
$180.7 billion in the year 2016-2017. This amount is accounted for more than 10 percent of
total gross domestic product (GDP) (Reeve, 2015). Cost for this service has increased for the
US, the UK and Canada and other developed countries as well.
Figure 1: Health Expenditure for Australian Government
Source: (Callander, Corscadden & Levesque, 2017)
The chief focus of these principles is to provide Australian citizens a value-based
medical facility. According to these principles, patients can access various services for
fulfilling their requirement related to healthcare. Under the professional care, patients receive
high-quality health services in a safe process provided by skilled physicians
(Safetyandquality.gov.au, 2018). The entire care process chiefly focuses to provide respects
to patients considering their cultural diversity. Moreover, patients receive facility to
communicate with the government for obtaining proper treatment. In this context, patients
can take decisions and choices regarding their planning for health service. Each patient has
the opportunity keep his or her personal information as private and confidential.
Sustainability of healthcare service:
Increasing cost of technology:
Due to traditional service of healthcare, expenditure has increased considerably in
many countries across the world. In Australia, total expenditure for health care has become
$180.7 billion in the year 2016-2017. This amount is accounted for more than 10 percent of
total gross domestic product (GDP) (Reeve, 2015). Cost for this service has increased for the
US, the UK and Canada and other developed countries as well.
Figure 1: Health Expenditure for Australian Government
Source: (Callander, Corscadden & Levesque, 2017)
8HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
In most of the developed countries, debates have been occurred for more expenditure
merits and health care. In this context, some economists have argued that through spending
more than USD1000 for each person in every year, healthcare can provide only marginal
benefits in healthcare services. This is because most of the health care services in these
countries have been constructed already. In the same year, health care expenditure for each
person in Australia was more than $7400 (Mantilla Herrera et al., 2018). On the contrary,
supporters have argued that marginal benefits generating from extra expenditure of health is
essential. This helps wealthy nations to reduce small risks related to ill health of people to
very small one. This process, in turn, helps developed countries to shift their health care
services from increasing longevity to developing life quality. Others have argued that extra
spending on healthcare services can exceed costs, as higher expenditure depending on
technology has developed health accessibility among people. This implies that modern
technology can help people to obtain new treatment facilities with modern technologies
(Harris et al., 2017). However, it is essential for any government to maintain fiscal
sustainability without doing much change in taxes or increasing public debt of the nation. To
reduce this increasing cost in health care service, the government of this country can take
various steps to improve sustainability. For doing so, the Australian government has intended
to do small reforms in this specific sector. Some of these chief mechanisms applied by the
Australian government are as follow:
Determining the best intervening way of health care facilities, funded by the
government
Changing the paying process of health care providers
Charging costs on each person; and
Developing competitions among various health care service providers (1)
In most of the developed countries, debates have been occurred for more expenditure
merits and health care. In this context, some economists have argued that through spending
more than USD1000 for each person in every year, healthcare can provide only marginal
benefits in healthcare services. This is because most of the health care services in these
countries have been constructed already. In the same year, health care expenditure for each
person in Australia was more than $7400 (Mantilla Herrera et al., 2018). On the contrary,
supporters have argued that marginal benefits generating from extra expenditure of health is
essential. This helps wealthy nations to reduce small risks related to ill health of people to
very small one. This process, in turn, helps developed countries to shift their health care
services from increasing longevity to developing life quality. Others have argued that extra
spending on healthcare services can exceed costs, as higher expenditure depending on
technology has developed health accessibility among people. This implies that modern
technology can help people to obtain new treatment facilities with modern technologies
(Harris et al., 2017). However, it is essential for any government to maintain fiscal
sustainability without doing much change in taxes or increasing public debt of the nation. To
reduce this increasing cost in health care service, the government of this country can take
various steps to improve sustainability. For doing so, the Australian government has intended
to do small reforms in this specific sector. Some of these chief mechanisms applied by the
Australian government are as follow:
Determining the best intervening way of health care facilities, funded by the
government
Changing the paying process of health care providers
Charging costs on each person; and
Developing competitions among various health care service providers (1)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Market concentration:
Competition among health professionals is an important factor. Geographical area or
insurers do not restrict the Australian market for general practitioners (GPs). Instead of this,
patients can select GP based on some factors like convenience, waiting times and reputation
along with pocket costs (Elliott et al., 2017). According to a report of IBIS World, the
Australian market of GPs can experience moderate competition. According to their analysis,
each GP operates within confined area and consequently they do not possess larger share of
market. In other words, it can be said that these market experience have less concentrated
market. However, this concentration has developed for normal practice sector due to
increasing number of large medical practices (Macpherson, O’Donnell, Godden & O’Neill,
2018). These services have offered health services by large number. Moreover, private sector
of health insurance experiences restricted competition due to high market concentration. This
happens because the number of private health insurance funds is very limited.
The need for volume:
Total process through health care providers obtain their payment has become an
important issue in the context of heath care expenditure. Some methods provide incentives
for providing over service while others provide comparatively less incentives to deliver care
with high quality. In recent years, the country depends heavily on this payment method (Dixit
& Sambasivan, 2018). The World Health Organisation has considered this process as least
effective to reduce expenditure growth. This is because fee-for-service payments and activity-
based funding (ABF) give enough incentives to increase the volume regarding care delivered
and other expenses. In this context, it needs to mention that the volume based on provided
health care services as well as the price paid by government determines total health care
expenditure. This implies that the government is trying to reduce the public expenditure
growth that can be done by slow growth in volume regarding services provided (Hay et al.,
Market concentration:
Competition among health professionals is an important factor. Geographical area or
insurers do not restrict the Australian market for general practitioners (GPs). Instead of this,
patients can select GP based on some factors like convenience, waiting times and reputation
along with pocket costs (Elliott et al., 2017). According to a report of IBIS World, the
Australian market of GPs can experience moderate competition. According to their analysis,
each GP operates within confined area and consequently they do not possess larger share of
market. In other words, it can be said that these market experience have less concentrated
market. However, this concentration has developed for normal practice sector due to
increasing number of large medical practices (Macpherson, O’Donnell, Godden & O’Neill,
2018). These services have offered health services by large number. Moreover, private sector
of health insurance experiences restricted competition due to high market concentration. This
happens because the number of private health insurance funds is very limited.
The need for volume:
Total process through health care providers obtain their payment has become an
important issue in the context of heath care expenditure. Some methods provide incentives
for providing over service while others provide comparatively less incentives to deliver care
with high quality. In recent years, the country depends heavily on this payment method (Dixit
& Sambasivan, 2018). The World Health Organisation has considered this process as least
effective to reduce expenditure growth. This is because fee-for-service payments and activity-
based funding (ABF) give enough incentives to increase the volume regarding care delivered
and other expenses. In this context, it needs to mention that the volume based on provided
health care services as well as the price paid by government determines total health care
expenditure. This implies that the government is trying to reduce the public expenditure
growth that can be done by slow growth in volume regarding services provided (Hay et al.,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
2017). However, in practical field, the government experiences difficulties to design,
implement policy solutions to cover up these objectives. However, reducing or slowing the
expenditure related to health care is not a policy problem only. Thus, this cannot be solved
with the help of technical solutions, as it is a political problem. One of the chief reasons is
that to implement slow growth of expenditure, government requires some policies. With the
help of these policies, the government can deduct unnecessary services of health. If
government reduces the need for volume regarding health care services then it may have
unfavourable effect on some outcomes relating to health care. This in turn may increase the
cost of care.
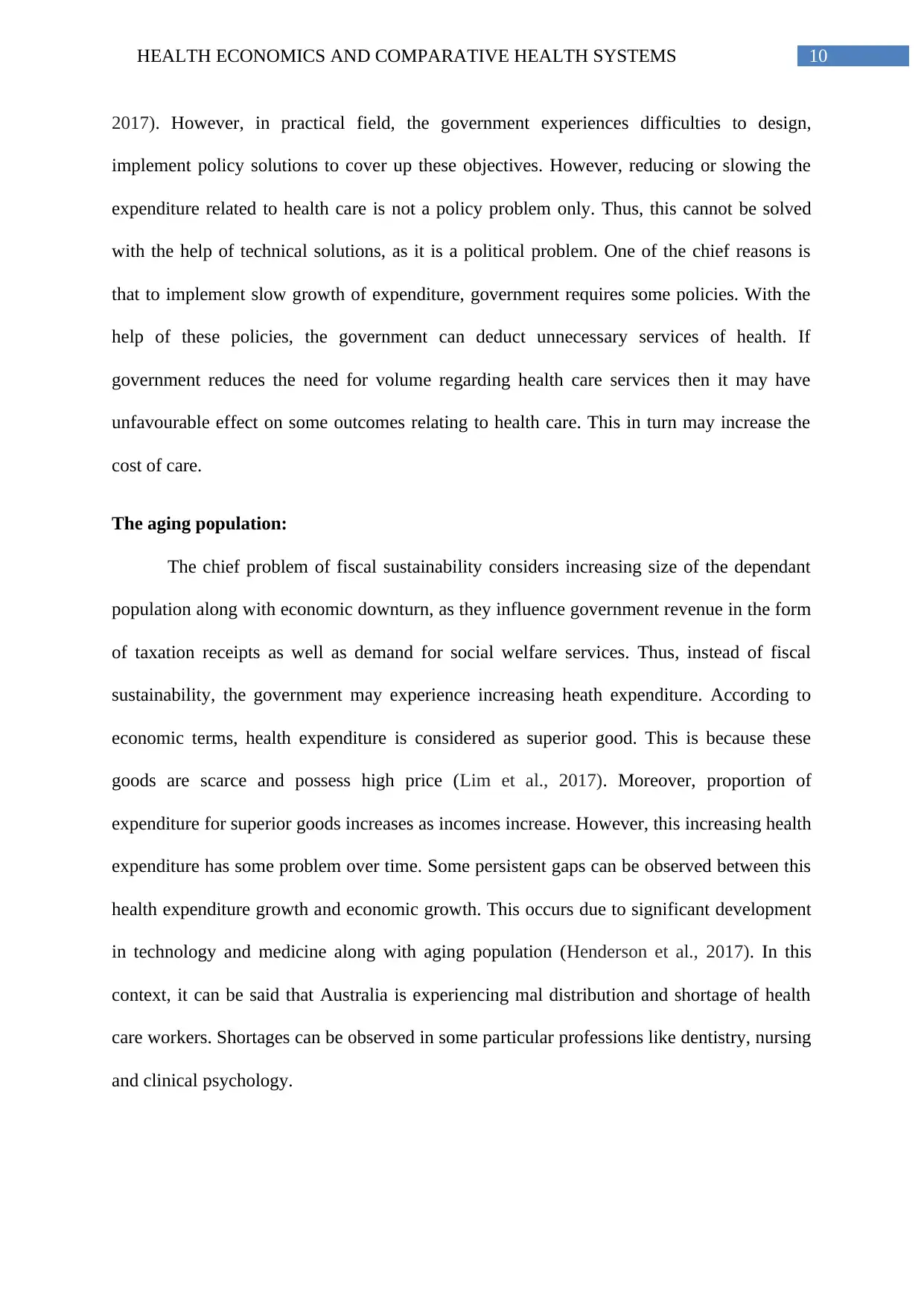
The aging population:
The chief problem of fiscal sustainability considers increasing size of the dependant
population along with economic downturn, as they influence government revenue in the form
of taxation receipts as well as demand for social welfare services. Thus, instead of fiscal
sustainability, the government may experience increasing heath expenditure. According to
economic terms, health expenditure is considered as superior good. This is because these
goods are scarce and possess high price (Lim et al., 2017). Moreover, proportion of
expenditure for superior goods increases as incomes increase. However, this increasing health
expenditure has some problem over time. Some persistent gaps can be observed between this
health expenditure growth and economic growth. This occurs due to significant development
in technology and medicine along with aging population (Henderson et al., 2017). In this
context, it can be said that Australia is experiencing mal distribution and shortage of health
care workers. Shortages can be observed in some particular professions like dentistry, nursing
and clinical psychology.
2017). However, in practical field, the government experiences difficulties to design,
implement policy solutions to cover up these objectives. However, reducing or slowing the
expenditure related to health care is not a policy problem only. Thus, this cannot be solved
with the help of technical solutions, as it is a political problem. One of the chief reasons is
that to implement slow growth of expenditure, government requires some policies. With the
help of these policies, the government can deduct unnecessary services of health. If
government reduces the need for volume regarding health care services then it may have
unfavourable effect on some outcomes relating to health care. This in turn may increase the
cost of care.
The aging population:
The chief problem of fiscal sustainability considers increasing size of the dependant
population along with economic downturn, as they influence government revenue in the form
of taxation receipts as well as demand for social welfare services. Thus, instead of fiscal
sustainability, the government may experience increasing heath expenditure. According to
economic terms, health expenditure is considered as superior good. This is because these
goods are scarce and possess high price (Lim et al., 2017). Moreover, proportion of
expenditure for superior goods increases as incomes increase. However, this increasing health
expenditure has some problem over time. Some persistent gaps can be observed between this
health expenditure growth and economic growth. This occurs due to significant development
in technology and medicine along with aging population (Henderson et al., 2017). In this
context, it can be said that Australia is experiencing mal distribution and shortage of health
care workers. Shortages can be observed in some particular professions like dentistry, nursing
and clinical psychology.
11HEALTH ECONOMICS AND COMPARATIVE HEALTH SYSTEMS
Figure 2: Increasing aging population in Australia
Source: (Nicholson et al., 2018)
Increased chronic diseases:
According to some health experts, fee-for-service cannot prevent and manage
increasing chronic diseases. They have stated that these services influence health
professionals to highlight on proper symptoms management instead of preventing disease
(Briggs, 2018). The Australian government has made some specific proposals of policies
based on co-payments that include issues of people, for instance a health Credit Card (Ball et
al., 2018). This has been done so that those people can pay health care without doing any
excess payments and reducing co-payments for chronic diseases.
Recommendations:
After discussing about the sustainability of value based health care model, the paper
can recommend some steps. By considering these steps, the government can efficiently
manage increasing health care expenditure. Firstly, expenditure has increased due to
technological costs. The government can spend more amounts in this sector for developing
life quality. However, it is also observed that higher expenditure for technology can also
Figure 2: Increasing aging population in Australia
Source: (Nicholson et al., 2018)
Increased chronic diseases:
According to some health experts, fee-for-service cannot prevent and manage
increasing chronic diseases. They have stated that these services influence health
professionals to highlight on proper symptoms management instead of preventing disease
(Briggs, 2018). The Australian government has made some specific proposals of policies
based on co-payments that include issues of people, for instance a health Credit Card (Ball et
al., 2018). This has been done so that those people can pay health care without doing any
excess payments and reducing co-payments for chronic diseases.
Recommendations:
After discussing about the sustainability of value based health care model, the paper
can recommend some steps. By considering these steps, the government can efficiently
manage increasing health care expenditure. Firstly, expenditure has increased due to
technological costs. The government can spend more amounts in this sector for developing
life quality. However, it is also observed that higher expenditure for technology can also
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





