Analysis of Smoking Practices in Australia: A Report
VerifiedAdded on 2022/11/01
|21
|3638
|319
Report
AI Summary
This report provides a comprehensive analysis of smoking practices in Australia, examining the factors that influence smoking uptake and patterns within the population. It explores the health impacts of smoking on physical, mental, social, and emotional well-being, highlighting the disparities across different demographic groups, including indigenous Australians and those with mental health issues. The report investigates the level of awareness regarding smoking prevention and the effectiveness of government strategies, such as taxation, mass media campaigns, and legislative measures. It also discusses the limitations of existing research and suggests areas for future improvements, including addressing cultural behaviors, improving access to cessation support, and strengthening research on interventions for disadvantaged populations. The study utilizes both primary and secondary data, drawing from surveys, peer-reviewed journals, and government sources to provide a detailed overview of the issue, including an analysis of the smoking rates among various age groups and genders, and the impact of smoking on the Wellness Wheel, which encompasses various aspects of an individual's life.
Assignment on the Reasons
behind Prevalent Smoking
Practices in Australia
behind Prevalent Smoking
Practices in Australia
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction................................................................................................................................3
Aim of the Investigation.........................................................................................................4
Objectives of the Study..........................................................................................................4
Method of Inquiry......................................................................................................................5
Discussion and Conclusion......................................................................................................10
References................................................................................................................................14
Introduction................................................................................................................................3
Aim of the Investigation.........................................................................................................4
Objectives of the Study..........................................................................................................4
Method of Inquiry......................................................................................................................5
Discussion and Conclusion......................................................................................................10
References................................................................................................................................14
Introduction
The biggest factor causing death and decline in health in the Australian populace was credited
to tobacco smoking practices as of 2011, responsible for causing injuries and diseases to 9%
of total populace increasing their risks to cardiovascular diseases, respiratory and related
health issues affecting the physical, emotional, social and mental well-being of individuals
associated with present tobacco usage, past usage and to individuals with exposure to passive
smoking (USHHS 2014). Estimated reports suggested that tobacco smoking resulted in lung
cancer to 80% and was the root-causal factor of 75% of COPD cases, claiming over 15,000 of
Australians annually. Smoking also amounted to an economic expenditure of $31.5 billion in
2005 which raised the strategic preventable measures in Australia resulting in drastic
reductions in smoking rates in the present time (IGCD 2013). Strategies like advertisement
bans, indoor smoking bans, outdoor smoking bans, bans in plain packaging, increment in
prices, restricted sales to the minors, educational awareness generation and media based
campaigns on smoking and its detrimental efficacies have all worked towards reducing the
smoking rates in Australia (MCDS 2011). The National-Drug-Strategy-Household-Survey of
2010, recognised that there are lesser people taking up smoking aged 14 years or above in
present times as compared to that before, with 57.8% of non-smokers now in comparison to
the 49% of 1991 (Australian Institute of Health and Welfare, 2010). However, the smoking
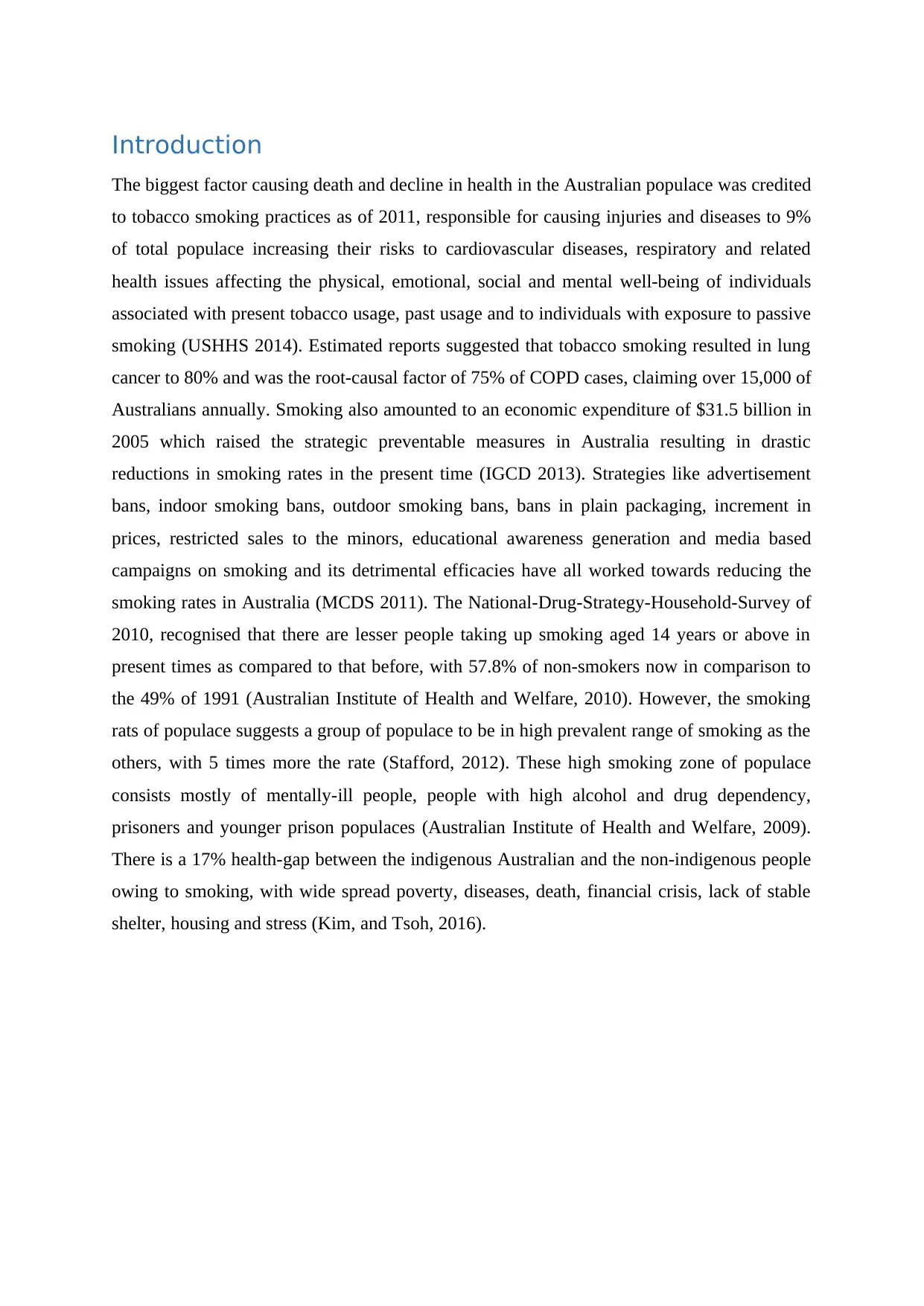
rats of populace suggests a group of populace to be in high prevalent range of smoking as the
others, with 5 times more the rate (Stafford, 2012). These high smoking zone of populace
consists mostly of mentally-ill people, people with high alcohol and drug dependency,
prisoners and younger prison populaces (Australian Institute of Health and Welfare, 2009).
There is a 17% health-gap between the indigenous Australian and the non-indigenous people
owing to smoking, with wide spread poverty, diseases, death, financial crisis, lack of stable
shelter, housing and stress (Kim, and Tsoh, 2016).
The biggest factor causing death and decline in health in the Australian populace was credited
to tobacco smoking practices as of 2011, responsible for causing injuries and diseases to 9%
of total populace increasing their risks to cardiovascular diseases, respiratory and related
health issues affecting the physical, emotional, social and mental well-being of individuals
associated with present tobacco usage, past usage and to individuals with exposure to passive
smoking (USHHS 2014). Estimated reports suggested that tobacco smoking resulted in lung
cancer to 80% and was the root-causal factor of 75% of COPD cases, claiming over 15,000 of
Australians annually. Smoking also amounted to an economic expenditure of $31.5 billion in
2005 which raised the strategic preventable measures in Australia resulting in drastic
reductions in smoking rates in the present time (IGCD 2013). Strategies like advertisement
bans, indoor smoking bans, outdoor smoking bans, bans in plain packaging, increment in
prices, restricted sales to the minors, educational awareness generation and media based
campaigns on smoking and its detrimental efficacies have all worked towards reducing the
smoking rates in Australia (MCDS 2011). The National-Drug-Strategy-Household-Survey of
2010, recognised that there are lesser people taking up smoking aged 14 years or above in
present times as compared to that before, with 57.8% of non-smokers now in comparison to
the 49% of 1991 (Australian Institute of Health and Welfare, 2010). However, the smoking
rats of populace suggests a group of populace to be in high prevalent range of smoking as the
others, with 5 times more the rate (Stafford, 2012). These high smoking zone of populace
consists mostly of mentally-ill people, people with high alcohol and drug dependency,
prisoners and younger prison populaces (Australian Institute of Health and Welfare, 2009).
There is a 17% health-gap between the indigenous Australian and the non-indigenous people
owing to smoking, with wide spread poverty, diseases, death, financial crisis, lack of stable
shelter, housing and stress (Kim, and Tsoh, 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Table: Smoking rate amongst diverse groups in Australian populace
(Source: Www1.health.gov.au, 2019)
Aim of the Investigation
The present study focuses on the diverse health impacts affecting the Australian
demographics due to smoking practices. The study aims “to understand the factors which
influences smoking, the level of awareness generation and how the 4-components of human
health gets affected by smoking practices in the Australian population.”
For investigating upon the same, the study focused in primary and secondary data collection
means through quantitative data collection means in the form of surveys considering a sample
population of 22 respondents irrespective of their age, occupation and genders. The study
focused on secondary sources of peer-reviewed journals, literary works and articles published
in international forums and also relied on government sites for data collection. The significant
impacts of smoking, the demographics affected and the benefits of social and community
based health-care measures have also been elicited.
(Source: Www1.health.gov.au, 2019)
Aim of the Investigation
The present study focuses on the diverse health impacts affecting the Australian
demographics due to smoking practices. The study aims “to understand the factors which
influences smoking, the level of awareness generation and how the 4-components of human
health gets affected by smoking practices in the Australian population.”
For investigating upon the same, the study focused in primary and secondary data collection
means through quantitative data collection means in the form of surveys considering a sample
population of 22 respondents irrespective of their age, occupation and genders. The study
focused on secondary sources of peer-reviewed journals, literary works and articles published
in international forums and also relied on government sites for data collection. The significant
impacts of smoking, the demographics affected and the benefits of social and community
based health-care measures have also been elicited.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Objectives of the Study
On the basis of the aforementioned aim the investigation has been carried out relied on the
three objectives as detailed below, to help direct the investigation in the right track and for
efficient data analysis and interpretation.
1. To determine the influential factors behind smoking.
2. To elucidate the level of awareness present in Australia and their effectiveness in
prevention of smoking
3. To determine the impact of smoking on the four components of human health –
mental, physical, social and physical.
Thus the investigation is based upon the following Research Questions:
1. What influences a person to start smoking?
2. Is there enough awareness to prevent people from smoking in Australia?
3. How does smoking affect the persons 4 components of health?
Method of Inquiry
The present study has been focused upon two methods of data collection, namely the primary
and the secondary method of data collection. The primary data collection procedure considers
22 Australian respondents irrespective of their age, gender, occupation or lifestyles. The
secondary data is obtained in the study from a collection of government sites, peer-reviewed
journal articles, and internationally acclaimed literary sources containing relevant data of
recent years ranging from 2009 to 2019.
Determining the influential factors behind smoking
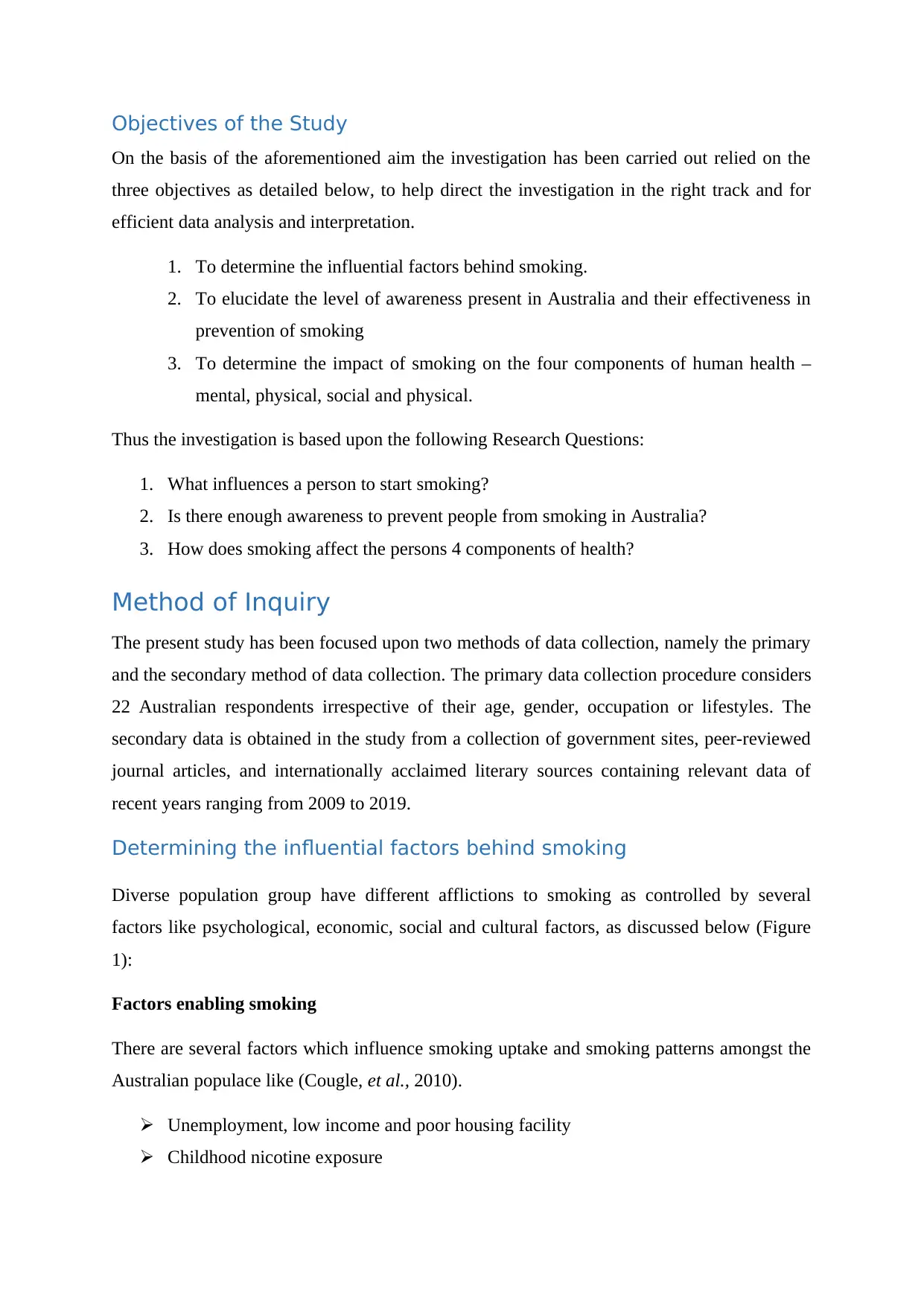
Diverse population group have different afflictions to smoking as controlled by several
factors like psychological, economic, social and cultural factors, as discussed below (Figure
1):
Factors enabling smoking
There are several factors which influence smoking uptake and smoking patterns amongst the
Australian populace like (Cougle, et al., 2010).
Unemployment, low income and poor housing facility
Childhood nicotine exposure
On the basis of the aforementioned aim the investigation has been carried out relied on the
three objectives as detailed below, to help direct the investigation in the right track and for
efficient data analysis and interpretation.
1. To determine the influential factors behind smoking.
2. To elucidate the level of awareness present in Australia and their effectiveness in
prevention of smoking
3. To determine the impact of smoking on the four components of human health –
mental, physical, social and physical.
Thus the investigation is based upon the following Research Questions:
1. What influences a person to start smoking?
2. Is there enough awareness to prevent people from smoking in Australia?
3. How does smoking affect the persons 4 components of health?
Method of Inquiry
The present study has been focused upon two methods of data collection, namely the primary
and the secondary method of data collection. The primary data collection procedure considers
22 Australian respondents irrespective of their age, gender, occupation or lifestyles. The
secondary data is obtained in the study from a collection of government sites, peer-reviewed
journal articles, and internationally acclaimed literary sources containing relevant data of
recent years ranging from 2009 to 2019.
Determining the influential factors behind smoking
Diverse population group have different afflictions to smoking as controlled by several
factors like psychological, economic, social and cultural factors, as discussed below (Figure
1):
Factors enabling smoking
There are several factors which influence smoking uptake and smoking patterns amongst the
Australian populace like (Cougle, et al., 2010).
Unemployment, low income and poor housing facility
Childhood nicotine exposure
Economic stress
Depression and anxiety
Parental exposure and peer pressure
Intensive/targeted tobacco marketing
Low indoor working hours
Barriers faced in quitting tobacco
People are more adept in taking up tobacco than in refraining from it. This is further fuelled
by certain barriers which prevent the quitting of tobacco usage as discussed below (Rayson,
2011):
High nicotine dependency
Lower awareness generation
Lack of knowledge and misconceptions
Lack of knowledge on cessation services available
NRT therapy knowledge
Economic stress
Lack of family and peer support
Low confidence
Boredom
Equalising smoking as a “stress-bursting hobby”
Depression and anxiety
Parental exposure and peer pressure
Intensive/targeted tobacco marketing
Low indoor working hours
Barriers faced in quitting tobacco
People are more adept in taking up tobacco than in refraining from it. This is further fuelled
by certain barriers which prevent the quitting of tobacco usage as discussed below (Rayson,
2011):
High nicotine dependency
Lower awareness generation
Lack of knowledge and misconceptions
Lack of knowledge on cessation services available
NRT therapy knowledge
Economic stress
Lack of family and peer support
Low confidence
Boredom
Equalising smoking as a “stress-bursting hobby”
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Figure 1: Smoking enablers and quitting barriers in the disadvantaged populace
(Source: Www1.health.gov.au, 2019)
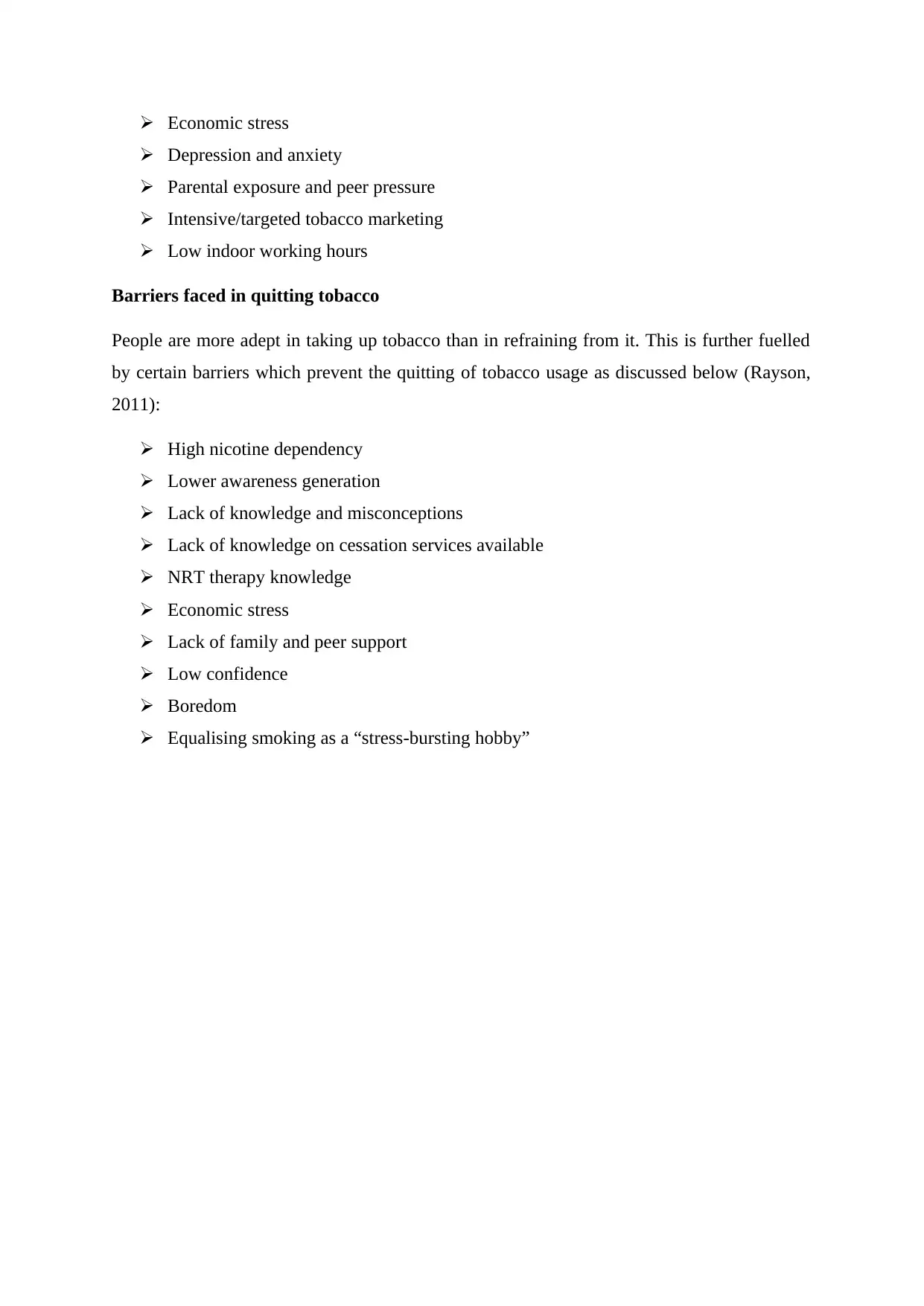
Elucidation on the level of awareness present in Australia and their
effectiveness in Smoking prevention
The Australian Government aims to reduce the disparity amongst the population groups
prone to smoking as is demonstrated in the National-Tobacco-Strategy (2012-18), which
focuses on the health and social inequalities of the high-prevalent zone. This has been one of
the targets amidst the 9 prior action arenas in order to reduce economic and health disparities
in the population (Siahpush, et al., 2010).
The working procedures
Government strategies impacting the entire population have shown a positive impact in
reducing smoking tendencies amongst diverse socio-economic groups, through tax increment,
mass media awareness and legislative measures (Durkin, et al., 2011).
(Source: Www1.health.gov.au, 2019)
Elucidation on the level of awareness present in Australia and their
effectiveness in Smoking prevention
The Australian Government aims to reduce the disparity amongst the population groups
prone to smoking as is demonstrated in the National-Tobacco-Strategy (2012-18), which
focuses on the health and social inequalities of the high-prevalent zone. This has been one of
the targets amidst the 9 prior action arenas in order to reduce economic and health disparities
in the population (Siahpush, et al., 2010).
The working procedures
Government strategies impacting the entire population have shown a positive impact in
reducing smoking tendencies amongst diverse socio-economic groups, through tax increment,
mass media awareness and legislative measures (Durkin, et al., 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Tax increment on tobacco prices is a means of population intervention policy helped
to reduce health-inequalities in smoking. This has reduced tobacco consumption
(Chaloupka, et al., 2011).
Anti-smoking campaign promoted through mass-media has increased help-seeking
behaviour via Quitline calls, increased intentions of quitting, ceased smoking rates.
Legislation promoting smoke-free practices has also increased quit tendencies and
attempts reducing consumption, in workplaces, and public places, discouraging
smoking amongst low SES and high SES group individuals.
Strategies adopted across populations have reduced young-adolescents from smoking
amongst all groups particularly the low socio-economic category.
Promises
All these are playing a positive role in encouraging development of cessation services, anti-
smoking therapies and treatments supporting the cultural and social settings on smokers
amongst all groups.
Figure 2: Summary of tobacco strategy across Australian impacting low-income groups
to reduce health-inequalities in smoking. This has reduced tobacco consumption
(Chaloupka, et al., 2011).
Anti-smoking campaign promoted through mass-media has increased help-seeking
behaviour via Quitline calls, increased intentions of quitting, ceased smoking rates.
Legislation promoting smoke-free practices has also increased quit tendencies and
attempts reducing consumption, in workplaces, and public places, discouraging
smoking amongst low SES and high SES group individuals.
Strategies adopted across populations have reduced young-adolescents from smoking
amongst all groups particularly the low socio-economic category.
Promises
All these are playing a positive role in encouraging development of cessation services, anti-
smoking therapies and treatments supporting the cultural and social settings on smokers
amongst all groups.
Figure 2: Summary of tobacco strategy across Australian impacting low-income groups
(Source: Tobaccoinaustralia.org.au, 2019)
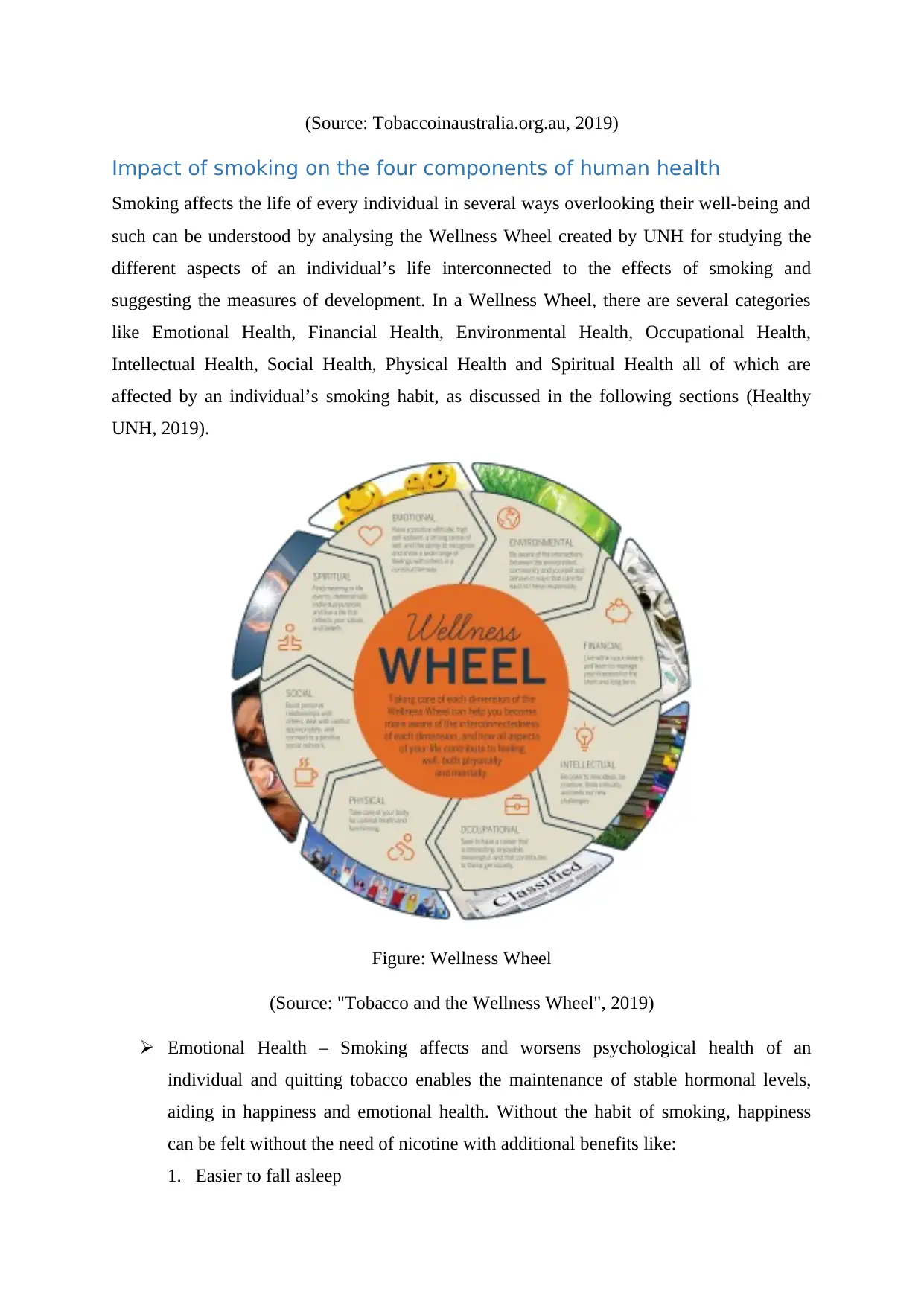
Impact of smoking on the four components of human health
Smoking affects the life of every individual in several ways overlooking their well-being and
such can be understood by analysing the Wellness Wheel created by UNH for studying the
different aspects of an individual’s life interconnected to the effects of smoking and
suggesting the measures of development. In a Wellness Wheel, there are several categories
like Emotional Health, Financial Health, Environmental Health, Occupational Health,
Intellectual Health, Social Health, Physical Health and Spiritual Health all of which are
affected by an individual’s smoking habit, as discussed in the following sections (Healthy
UNH, 2019).
Figure: Wellness Wheel
(Source: "Tobacco and the Wellness Wheel", 2019)
Emotional Health – Smoking affects and worsens psychological health of an
individual and quitting tobacco enables the maintenance of stable hormonal levels,
aiding in happiness and emotional health. Without the habit of smoking, happiness
can be felt without the need of nicotine with additional benefits like:
1. Easier to fall asleep
Impact of smoking on the four components of human health
Smoking affects the life of every individual in several ways overlooking their well-being and
such can be understood by analysing the Wellness Wheel created by UNH for studying the
different aspects of an individual’s life interconnected to the effects of smoking and
suggesting the measures of development. In a Wellness Wheel, there are several categories
like Emotional Health, Financial Health, Environmental Health, Occupational Health,
Intellectual Health, Social Health, Physical Health and Spiritual Health all of which are
affected by an individual’s smoking habit, as discussed in the following sections (Healthy
UNH, 2019).
Figure: Wellness Wheel
(Source: "Tobacco and the Wellness Wheel", 2019)
Emotional Health – Smoking affects and worsens psychological health of an
individual and quitting tobacco enables the maintenance of stable hormonal levels,
aiding in happiness and emotional health. Without the habit of smoking, happiness
can be felt without the need of nicotine with additional benefits like:
1. Easier to fall asleep
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2. Lesser anxiety
3. Lessened depression
4. Reduced Post-Traumatic-Stress Disorder
Physical Health – Smoking prevents preventable death rates, with even a single
cigarette affecting the mind and body driving it to detrimental conditions, affecting
even the infrequent smokers. Quitting tobacco helps in the following ways:
1. Lesser sick day
2. Decrement of cancer
3. Decreased heart diseases and strokes
4. Decreased emphysema and bronchitis
5. Increased development to medication
6. Decreased headache, arthritis, back aches and vision problems
7. Increased fertility and healing processes
Mental Health – Smoking causes memory dysfunctions in adults, affecting the
prefrontal cortex development in adolescents. The brain development trajectory is
affected which deters functioning of pre-frontal cortex in addicted teenagers.
Social Health – Smoking can be passive smoking and active smoking, and with the
majorities of public joints accepting mild smoking practices, passive smoking is a
common menace affecting children and a large varieties of population negating their
health. These involuntary smoke inhalation increases toxins from building up in the
body causing health problems like:
1. Increased respiratory infection like pneumonia and bronchitis
2. Increased and severe asthma
3. Heart diseases
4. Heart strokes
5. Respiratory tract infections
6. Lung cancer
3. Lessened depression
4. Reduced Post-Traumatic-Stress Disorder
Physical Health – Smoking prevents preventable death rates, with even a single
cigarette affecting the mind and body driving it to detrimental conditions, affecting
even the infrequent smokers. Quitting tobacco helps in the following ways:
1. Lesser sick day
2. Decrement of cancer
3. Decreased heart diseases and strokes
4. Decreased emphysema and bronchitis
5. Increased development to medication
6. Decreased headache, arthritis, back aches and vision problems
7. Increased fertility and healing processes
Mental Health – Smoking causes memory dysfunctions in adults, affecting the
prefrontal cortex development in adolescents. The brain development trajectory is
affected which deters functioning of pre-frontal cortex in addicted teenagers.
Social Health – Smoking can be passive smoking and active smoking, and with the
majorities of public joints accepting mild smoking practices, passive smoking is a
common menace affecting children and a large varieties of population negating their
health. These involuntary smoke inhalation increases toxins from building up in the
body causing health problems like:
1. Increased respiratory infection like pneumonia and bronchitis
2. Increased and severe asthma
3. Heart diseases
4. Heart strokes
5. Respiratory tract infections
6. Lung cancer
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
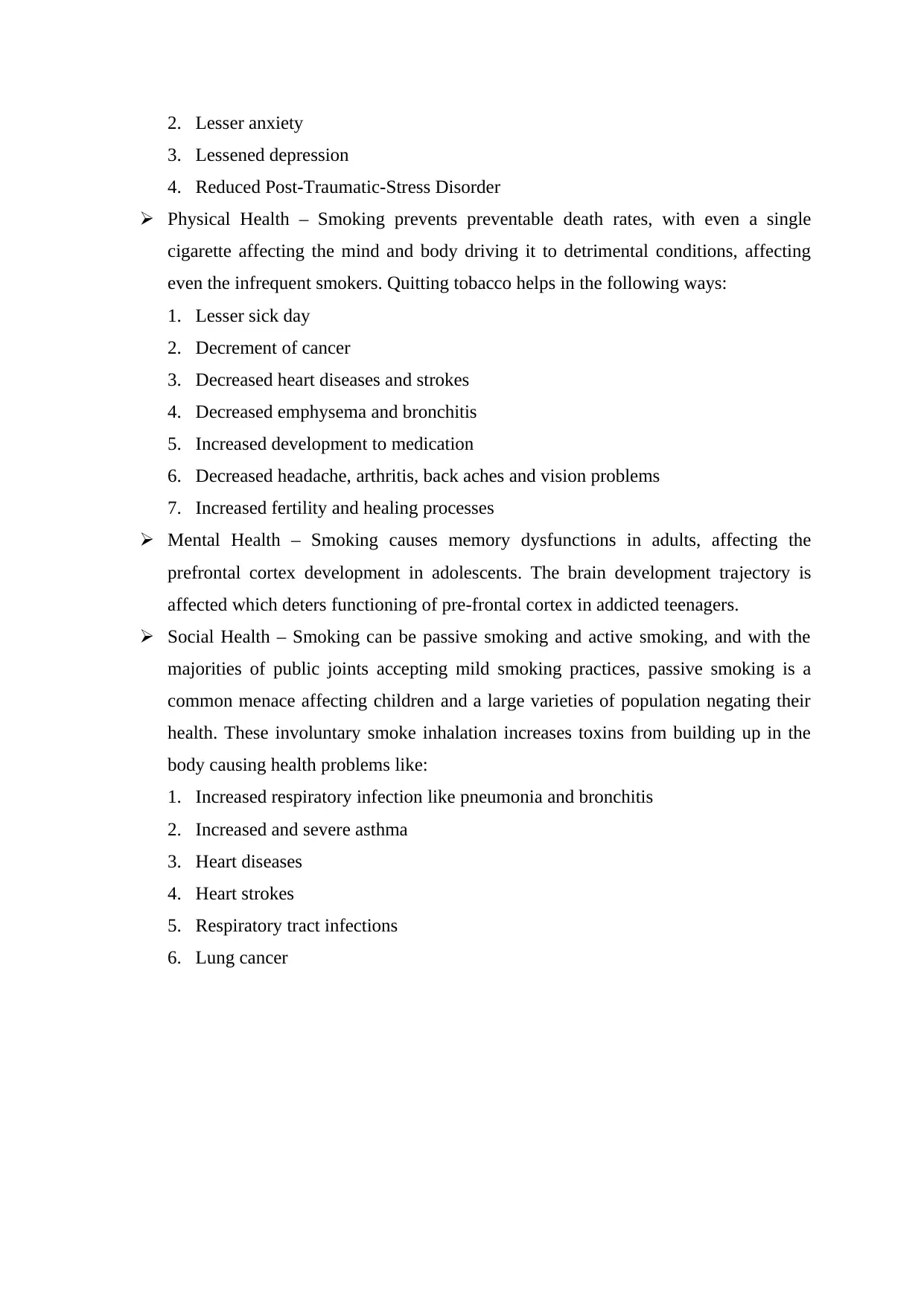
Discussion and Conclusion
(Source: Aihw.gov.au, 2019)
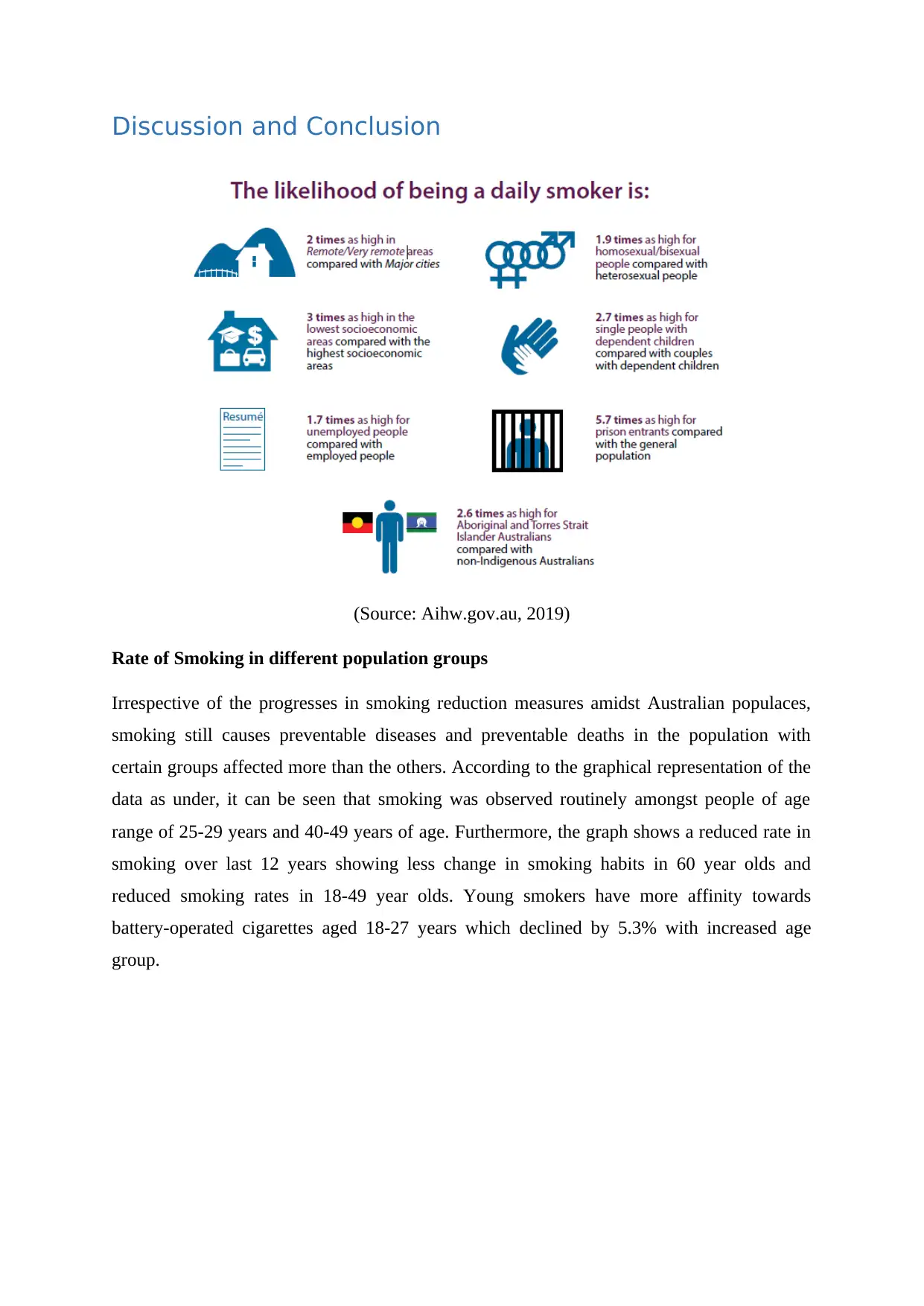
Rate of Smoking in different population groups
Irrespective of the progresses in smoking reduction measures amidst Australian populaces,
smoking still causes preventable diseases and preventable deaths in the population with
certain groups affected more than the others. According to the graphical representation of the
data as under, it can be seen that smoking was observed routinely amongst people of age
range of 25-29 years and 40-49 years of age. Furthermore, the graph shows a reduced rate in
smoking over last 12 years showing less change in smoking habits in 60 year olds and
reduced smoking rates in 18-49 year olds. Young smokers have more affinity towards
battery-operated cigarettes aged 18-27 years which declined by 5.3% with increased age
group.
(Source: Aihw.gov.au, 2019)
Rate of Smoking in different population groups
Irrespective of the progresses in smoking reduction measures amidst Australian populaces,
smoking still causes preventable diseases and preventable deaths in the population with
certain groups affected more than the others. According to the graphical representation of the
data as under, it can be seen that smoking was observed routinely amongst people of age
range of 25-29 years and 40-49 years of age. Furthermore, the graph shows a reduced rate in
smoking over last 12 years showing less change in smoking habits in 60 year olds and
reduced smoking rates in 18-49 year olds. Young smokers have more affinity towards
battery-operated cigarettes aged 18-27 years which declined by 5.3% with increased age
group.
Figure: Comparative analysis amongst smokers of different age groups in 2001 and 2013
(Source: Aihw.gov.au, 2019)
(Source: Aihw.gov.au, 2019)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





