Healthcare Risk Analysis Report: Bonded Medical Program (BMP)
VerifiedAdded on 2022/09/15
|5
|1174
|12
Report
AI Summary
This report presents a risk analysis of the Bonded Medical Program (BMP) in Australia, a government initiative designed to address workforce shortages in remote and rural areas. The analysis identifies the potential risks associated with the program, including student withdrawals, inadequate medical services, and reduced standards of care. It assesses the likelihood and impact of these risks, providing a risk matrix that evaluates each risk's level. The report highlights the challenges of attracting and retaining medical professionals in rural regions and the impact of the program's requirements on students' career ambitions and family options. To mitigate these risks, the report proposes management strategies such as providing scholarships, fostering positive attitudes towards rural practice, and offering legal advice to students. The analysis draws upon data from the Australian Bureau of Statistics and the Australian Institute of Health and Welfare to support its findings, offering recommendations to improve service delivery and the program's effectiveness.

Running head: BONDED MEDICAL PROGRAM 1
BONDED MEDICAL PROGRAM
Student’s Name
Institutional Affiliation
BONDED MEDICAL PROGRAM
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BONDED MEDICAL PROGRAM 2
Bonded Medical Program
Bonded medical program (BMP) is a proposed health system reform by the Australia
government where the graduate medical students are bounded by legal contracts to serve in
the remote, rural, and regional areas where there is a shortage in the workforce. On the other
hand, risk analysis is termed as the process of identifying and evaluating potential issues that
could negatively affect a project or business initiative from thriving.
Comprehensive Risk Estimation
An estimate of 20% of the population in Australia lives in the remote and rural regions.
These proportions of people face poor services in comparison to the people in the
metropolitan areas. In addition, the outer and inner regional communities have a high
incidence rate of chronic infections. There is a need for an increased medical workforce in the
rural areas of Australia due to the large poor health conditions of the people.
Majority of the Australians living in remote and rural regions often travel for a long
distance in order to access medical services. Similarly, on the basis of 2005-2010 AIHW
survey, 57% of people who live in the remote areas tend to move in the regions that are less
remote to be able to obtain proper medical services in the situations of chronic infection such
as end-stage renal disease (ESRD) (Australian Institute of Health and Welfare, 2016).
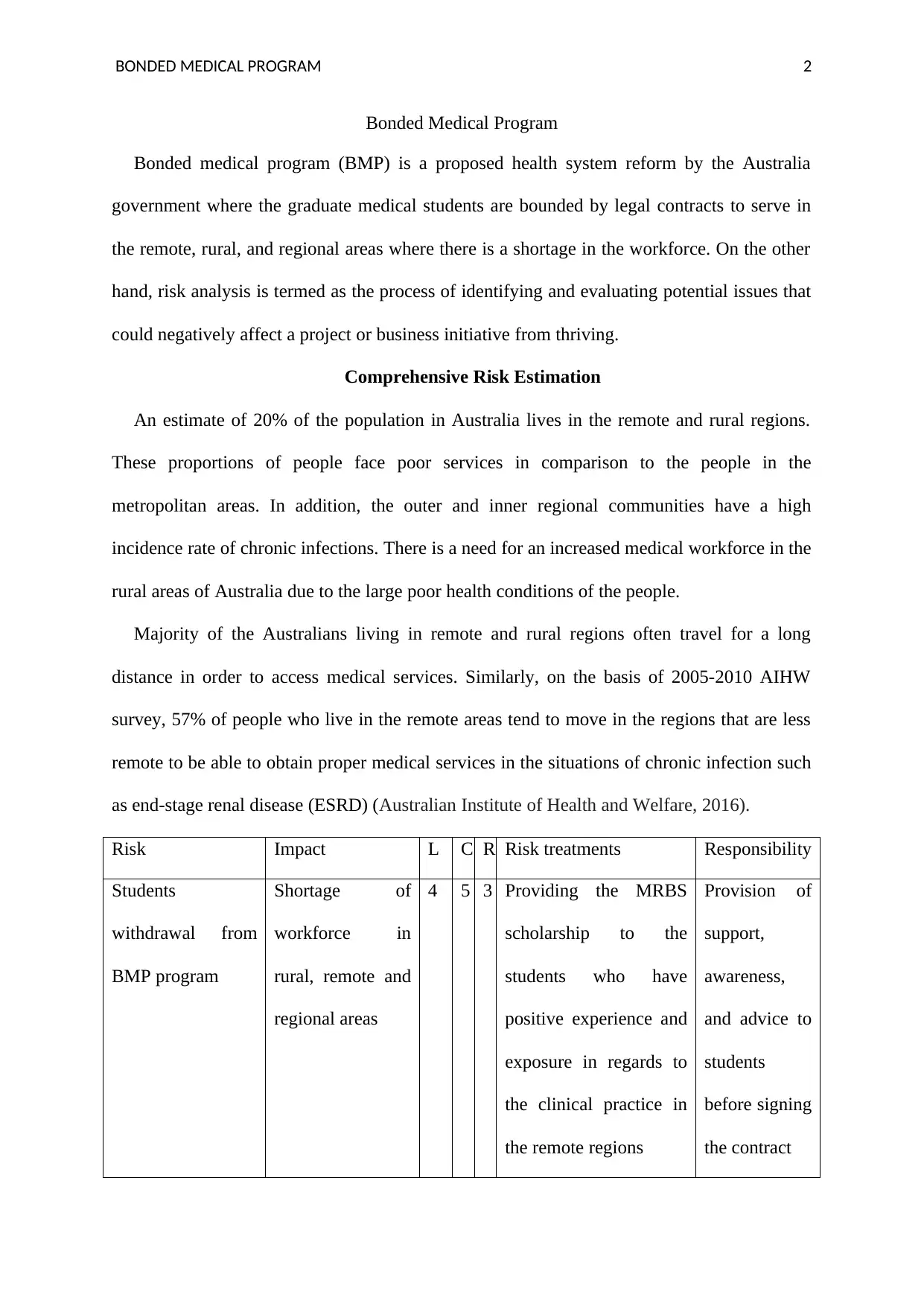
Risk Impact L C R Risk treatments Responsibility
Students
withdrawal from
BMP program
Shortage of
workforce in
rural, remote and
regional areas
4 5 3 Providing the MRBS
scholarship to the
students who have
positive experience and
exposure in regards to
the clinical practice in
the remote regions
Provision of
support,
awareness,
and advice to
students
before signing
the contract
Bonded Medical Program
Bonded medical program (BMP) is a proposed health system reform by the Australia
government where the graduate medical students are bounded by legal contracts to serve in
the remote, rural, and regional areas where there is a shortage in the workforce. On the other
hand, risk analysis is termed as the process of identifying and evaluating potential issues that
could negatively affect a project or business initiative from thriving.
Comprehensive Risk Estimation
An estimate of 20% of the population in Australia lives in the remote and rural regions.
These proportions of people face poor services in comparison to the people in the
metropolitan areas. In addition, the outer and inner regional communities have a high
incidence rate of chronic infections. There is a need for an increased medical workforce in the
rural areas of Australia due to the large poor health conditions of the people.
Majority of the Australians living in remote and rural regions often travel for a long
distance in order to access medical services. Similarly, on the basis of 2005-2010 AIHW
survey, 57% of people who live in the remote areas tend to move in the regions that are less
remote to be able to obtain proper medical services in the situations of chronic infection such
as end-stage renal disease (ESRD) (Australian Institute of Health and Welfare, 2016).
Risk Impact L C R Risk treatments Responsibility
Students
withdrawal from
BMP program
Shortage of
workforce in
rural, remote and
regional areas
4 5 3 Providing the MRBS
scholarship to the
students who have
positive experience and
exposure in regards to
the clinical practice in
the remote regions
Provision of
support,
awareness,
and advice to
students
before signing
the contract
BONDED MEDICAL PROGRAM 3
Risk likelihood
There is a possible likelihood of the risk being realized due to an insufficient workforce in
the rural regions. Therefore, there is a developed need to progressively assess this medical
program in order to improve service delivery. According to the 2015 AIHW health workforce
analysis, the number of medical experts working per person in the cities is 4.1 per 1000 in
comparison to 2.5 per 1000 in the remote and rural (Australian Bureau of Statistics, 2015).
From the survey, it was valid that with an increase in the level of remoteness, the number of
medical specialists declined. Inadequate medical services attributed to the fact that people in
remote regions of Australia have a minimal likelihood to access hospital procedures and
routine screening programs.
Impact
The numbers of students who complete the BMP program or Medical Bonded Rural
Scholarship (MBRS) reduce due to withdrawals, which are a breach of contract. Thus
according to the Australian Institute of Health and Welfare (AIHW) survey in 2017, there
were a total of 414 withdrawals, 151 undertaking rural return of service (RoS) with only 9
participants completing the program. The majority of the students who withdrew from the
program believed that RoS limited their family options and career ambitions in regard to
education and employment.
Risk level
There was a high-risk level of the program due to compliant from the doctors in the
remote and rural training association on the reduced standards of care in the rural regions if
the students remain in the program unwillingly (Walters et al., 2016). Some of the students
have preconceived attitudes and ideas in regards to working in rural regions, which may
hinder the delivery of medical services to the community. Additionally, some of them feel
Risk likelihood
There is a possible likelihood of the risk being realized due to an insufficient workforce in
the rural regions. Therefore, there is a developed need to progressively assess this medical
program in order to improve service delivery. According to the 2015 AIHW health workforce
analysis, the number of medical experts working per person in the cities is 4.1 per 1000 in
comparison to 2.5 per 1000 in the remote and rural (Australian Bureau of Statistics, 2015).
From the survey, it was valid that with an increase in the level of remoteness, the number of
medical specialists declined. Inadequate medical services attributed to the fact that people in
remote regions of Australia have a minimal likelihood to access hospital procedures and
routine screening programs.
Impact
The numbers of students who complete the BMP program or Medical Bonded Rural
Scholarship (MBRS) reduce due to withdrawals, which are a breach of contract. Thus
according to the Australian Institute of Health and Welfare (AIHW) survey in 2017, there
were a total of 414 withdrawals, 151 undertaking rural return of service (RoS) with only 9
participants completing the program. The majority of the students who withdrew from the
program believed that RoS limited their family options and career ambitions in regard to
education and employment.
Risk level
There was a high-risk level of the program due to compliant from the doctors in the
remote and rural training association on the reduced standards of care in the rural regions if
the students remain in the program unwillingly (Walters et al., 2016). Some of the students
have preconceived attitudes and ideas in regards to working in rural regions, which may
hinder the delivery of medical services to the community. Additionally, some of them feel
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BONDED MEDICAL PROGRAM 4
isolated in the rural regions and are have been kept away from their close family members
and friends; thus, the level of service delivery will decline to heighten the risk. Lack of rural
experience and the high workload that the medical professions encounter make them be
reluctant in their service delivery. This is because they cannot cope up with the huge number
of patients who require treatment due to their low number of inadequate medical resources.
Management Plan
To reduce the number of withdrawals from the program, it is essential to adopt measures
such as providing the MRBS scholarship to the students who have positive experience and
exposure in regards to the clinical practice in the remote regions (Grobler, Marais &
Mabunda, 2015). Moreover, encouraging the students who have been admitted to the
program to be positive and avoid negative sentiments in regards to rural experience.
Minimization of stigmatization, negative sentiments, and thoughts will enhance a genuine
desire and positive attitude of the students who would wish to join the program (Playford,
Ngo, Gupta & Puddey, 2017).
BMP is a legitimate agreement; thus it is essential for the students to receive a piece of
legal advice before taking part in the signing of the contract. Therefore bonded medical
doctors and students require extensive support and awareness when in search of a career and
legal planning advice. Since accessibility, cost, and limited knowledge can be a potential
barrier (Calder et al., 2018).
isolated in the rural regions and are have been kept away from their close family members
and friends; thus, the level of service delivery will decline to heighten the risk. Lack of rural
experience and the high workload that the medical professions encounter make them be
reluctant in their service delivery. This is because they cannot cope up with the huge number
of patients who require treatment due to their low number of inadequate medical resources.
Management Plan
To reduce the number of withdrawals from the program, it is essential to adopt measures
such as providing the MRBS scholarship to the students who have positive experience and
exposure in regards to the clinical practice in the remote regions (Grobler, Marais &
Mabunda, 2015). Moreover, encouraging the students who have been admitted to the
program to be positive and avoid negative sentiments in regards to rural experience.
Minimization of stigmatization, negative sentiments, and thoughts will enhance a genuine
desire and positive attitude of the students who would wish to join the program (Playford,
Ngo, Gupta & Puddey, 2017).
BMP is a legitimate agreement; thus it is essential for the students to receive a piece of
legal advice before taking part in the signing of the contract. Therefore bonded medical
doctors and students require extensive support and awareness when in search of a career and
legal planning advice. Since accessibility, cost, and limited knowledge can be a potential
barrier (Calder et al., 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BONDED MEDICAL PROGRAM 5
References
Australian Bureau of Statistics. (2015). National health survey: First results, 2014–15. ABS
Cat. No. 4364.0. 55.001).
Australian Institute of Health and Welfare. (2016). Admitted patient care 2014–15:
Australian hospital statistics. Health services series no 68, Cat. no. HSE 172.
Calder, R., Glover, J., Buckley, J., McNeil, J., Harris, B., & Lindberg, R. (2018). Better data
for better decisions: The Case for an Australian Health Survey.
Grobler, L., Marais, B. J., & Mabunda, S. (2015). Interventions for increasing the proportion
of health professionals practising in rural and other underserved areas. Cochrane database
of systematic reviews, (6).
Playford, D., Ngo, H., Gupta, S., & Puddey, I. B. (2017). Opting for rural practice: the
influence of medical student origin, intention and immersion experience. Medical Journal
of Australia, 207(4), 154-158.
Walters, L., Seal, A., McGirr, J., Stewart, R., DeWitt, D., & Playford, D. (2016). Effect of
medical student preference on rural clinical school experience and rural career
intentions. Rural and remote health, 16(4).
References
Australian Bureau of Statistics. (2015). National health survey: First results, 2014–15. ABS
Cat. No. 4364.0. 55.001).
Australian Institute of Health and Welfare. (2016). Admitted patient care 2014–15:
Australian hospital statistics. Health services series no 68, Cat. no. HSE 172.
Calder, R., Glover, J., Buckley, J., McNeil, J., Harris, B., & Lindberg, R. (2018). Better data
for better decisions: The Case for an Australian Health Survey.
Grobler, L., Marais, B. J., & Mabunda, S. (2015). Interventions for increasing the proportion
of health professionals practising in rural and other underserved areas. Cochrane database
of systematic reviews, (6).
Playford, D., Ngo, H., Gupta, S., & Puddey, I. B. (2017). Opting for rural practice: the
influence of medical student origin, intention and immersion experience. Medical Journal
of Australia, 207(4), 154-158.
Walters, L., Seal, A., McGirr, J., Stewart, R., DeWitt, D., & Playford, D. (2016). Effect of
medical student preference on rural clinical school experience and rural career
intentions. Rural and remote health, 16(4).
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




