Systematic Review of Immunization Programs for Indigenous Australians
VerifiedAdded on 2023/06/05
|10
|2063
|81
Report
AI Summary
This report presents a systematic review of immunization programs targeting Indigenous communities in Australia, examining the impact of these programs on public health. The review synthesizes evidence from various databases, including PubMed, Scopus, and CINAHL, focusing on studies published from 2014 onwards. The report explores the motivation behind the review, which stems from the limited number of systematic analyses in this area, and aims to provide insights for future policy interventions. The methodology includes detailed search strategies and inclusion/exclusion criteria. The findings highlight the reduced burden of diseases and decreased hospital admission rates due to the National Immunization Program, while also pointing out existing gaps in immunization rates between Indigenous and non-Indigenous communities. The report identifies factors affecting immunization coverage, such as timeliness and healthcare provider identification of Aboriginal status, and emphasizes the need for interventions like personalized calendars to boost vaccination rates. It concludes with recommendations for further research and strategies to improve immunization programs within Indigenous communities.

RUNNING HEAD: HEALTH ADVANCEMENT AND PROMOTION 1
Health Advancement and Promotion
Name:
Institution:
Tutor:
Date:
Health Advancement and Promotion
Name:
Institution:
Tutor:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH ADVANCEMENT AND PROMOTION 2
Health advancement and Promotion
Title:
Immunization programs for the indigenous communities in Australia: A systematic
review
Introduction:
Evidence on the topic
Delayed vaccination as well as vaccine preventable communicable diseases still remain a
public health issue among the Aboriginal communities. The strategies to initiate the vaccination
coverage as well as timelines can be very resource intensive. The Aboriginal Medical Service
Sydney (AMSWS) in 2008-2009 came up with this low cost initiative to help boost childhood
immunization among the Aboriginal communities.
The National Immunization Program (NIP) provide extra immunization services to the
indigenous communities in Australia for free with the aim of protecting them against infections
(Collins et al., 2017). The extra immunizations provided are just an addition to the other routine
vaccines that are provided throughout the lives of children, adults, seniors as well as expectant
women in Australia.
It is recommended by the NIP that all children below five years among the Aboriginal
and Torres Islander people should receive the vaccines .There are different diseases that the
children should be immunized against and they include pneumococcal disease(Falster et al.,
2016). The NIP recommend that children between 12 and 18 months living in Queensland,
Health advancement and Promotion
Title:
Immunization programs for the indigenous communities in Australia: A systematic
review
Introduction:
Evidence on the topic
Delayed vaccination as well as vaccine preventable communicable diseases still remain a
public health issue among the Aboriginal communities. The strategies to initiate the vaccination
coverage as well as timelines can be very resource intensive. The Aboriginal Medical Service
Sydney (AMSWS) in 2008-2009 came up with this low cost initiative to help boost childhood
immunization among the Aboriginal communities.
The National Immunization Program (NIP) provide extra immunization services to the
indigenous communities in Australia for free with the aim of protecting them against infections
(Collins et al., 2017). The extra immunizations provided are just an addition to the other routine
vaccines that are provided throughout the lives of children, adults, seniors as well as expectant
women in Australia.
It is recommended by the NIP that all children below five years among the Aboriginal
and Torres Islander people should receive the vaccines .There are different diseases that the
children should be immunized against and they include pneumococcal disease(Falster et al.,
2016). The NIP recommend that children between 12 and 18 months living in Queensland,
HEALTH ADVANCEMENT AND PROMOTION 3
Northern Territory, Western Australia and South Australia should be immunized with the
additional booster dose of the pneumococcal vaccine.
The NIP also provide two doses of the Hepatitis A vaccine which is usually provided 6
months apart .It is recommended for children as from 12 months and should be provided to all
the indigenous communities children living in Queensland, Northern Territory, Western
Australia and the South Australia (Fathima et al., 2017). However, the age at which the
pneumococcal and the Hepatitis A vaccines are provided vary among the four regions. The Flu
vaccine is also provided by the NIP to all the Aboriginal and Torres Islander children between
the age of 6 months and 5 years.
Children between the age of 5 and 9 years are usually provided with catch up
vaccines .This are the routine vaccines that the children missed at a certain stage of their lives.
This is the same case for children between 10 and 15 years (Gidding et al., 2018) .Besides the
catch up vaccines to this age group, The Human papilloma virus, tetanus, diphtheria and the
whooping cough vaccines are also provided.
Adults among the indigenous communities are also not exempted from the catch up
vaccines. Adults between the age of 15 and 49 years receive the catch up vaccine from the NIP.
Some of the vaccines at this group include flu (Influenza) for people above 15 years (Hendry et
al., 2018). Pneumococcal vaccine is also provided to people within this age group. Those adults
above 50 years within the Aboriginal and Torres Islander people are also immunized against the
pneumococcal disease.
Northern Territory, Western Australia and South Australia should be immunized with the
additional booster dose of the pneumococcal vaccine.
The NIP also provide two doses of the Hepatitis A vaccine which is usually provided 6
months apart .It is recommended for children as from 12 months and should be provided to all
the indigenous communities children living in Queensland, Northern Territory, Western
Australia and the South Australia (Fathima et al., 2017). However, the age at which the
pneumococcal and the Hepatitis A vaccines are provided vary among the four regions. The Flu
vaccine is also provided by the NIP to all the Aboriginal and Torres Islander children between
the age of 6 months and 5 years.
Children between the age of 5 and 9 years are usually provided with catch up
vaccines .This are the routine vaccines that the children missed at a certain stage of their lives.
This is the same case for children between 10 and 15 years (Gidding et al., 2018) .Besides the
catch up vaccines to this age group, The Human papilloma virus, tetanus, diphtheria and the
whooping cough vaccines are also provided.
Adults among the indigenous communities are also not exempted from the catch up
vaccines. Adults between the age of 15 and 49 years receive the catch up vaccine from the NIP.
Some of the vaccines at this group include flu (Influenza) for people above 15 years (Hendry et
al., 2018). Pneumococcal vaccine is also provided to people within this age group. Those adults
above 50 years within the Aboriginal and Torres Islander people are also immunized against the
pneumococcal disease.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH ADVANCEMENT AND PROMOTION 4
What motivated this review?
There are several studies on the immunization programs among the Aboriginal and
Torres Islander people of Australia .However, there are very few systematic reviews and this was
the driving force behind my study. This is to ensure that there is comprehending of how the
immunization services are carried out among the indigenous communities in Australia. The
systematic review would also provide an insight for the future policy makers to target the
indigenous communities for future interventions.
Methods:
Search strategy
Data sources: I used the five major electronic databases that include PubMed, Scopus,
CINAHL, Google scholar and the web of science. The databases were searched for English
journals or articles on the immunization /vaccination programs among the Aboriginal and Torres
Islander People of Australia for a period between 2014 up to date. To seek additional materials,
the google website was also used.
Search terms/keywords: The main search term used was “Immunization” OR “Vaccination”
and then the subsequent searches involved the Aboriginal and the Torres Islander people of
Australia, immunization practices in Australia etc.
Inclusion/exclusion criteria
All the articles that mentioned immunization or vaccination among the indigenous
communities in Australia were considered.
What motivated this review?
There are several studies on the immunization programs among the Aboriginal and
Torres Islander people of Australia .However, there are very few systematic reviews and this was
the driving force behind my study. This is to ensure that there is comprehending of how the
immunization services are carried out among the indigenous communities in Australia. The
systematic review would also provide an insight for the future policy makers to target the
indigenous communities for future interventions.
Methods:
Search strategy
Data sources: I used the five major electronic databases that include PubMed, Scopus,
CINAHL, Google scholar and the web of science. The databases were searched for English
journals or articles on the immunization /vaccination programs among the Aboriginal and Torres
Islander People of Australia for a period between 2014 up to date. To seek additional materials,
the google website was also used.
Search terms/keywords: The main search term used was “Immunization” OR “Vaccination”
and then the subsequent searches involved the Aboriginal and the Torres Islander people of
Australia, immunization practices in Australia etc.
Inclusion/exclusion criteria
All the articles that mentioned immunization or vaccination among the indigenous
communities in Australia were considered.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH ADVANCEMENT AND PROMOTION 5
Those Articles the mentioned immunization/vaccination among the indigenous
communities in Australia in exceptionally difficult circumstances like vaccination and the
prevalence of HIV were excluded. Those that mentioned vaccination in comparison with
nutrition were also excluded.
Immunization/vaccination programs were defined by the both the young and adults
immunization indicators as stipulated by the WHO/UNICEF.
The different study characteristics such as the study design used were considered.
It is only the articles that were published in English that were considered for the
systematic review.
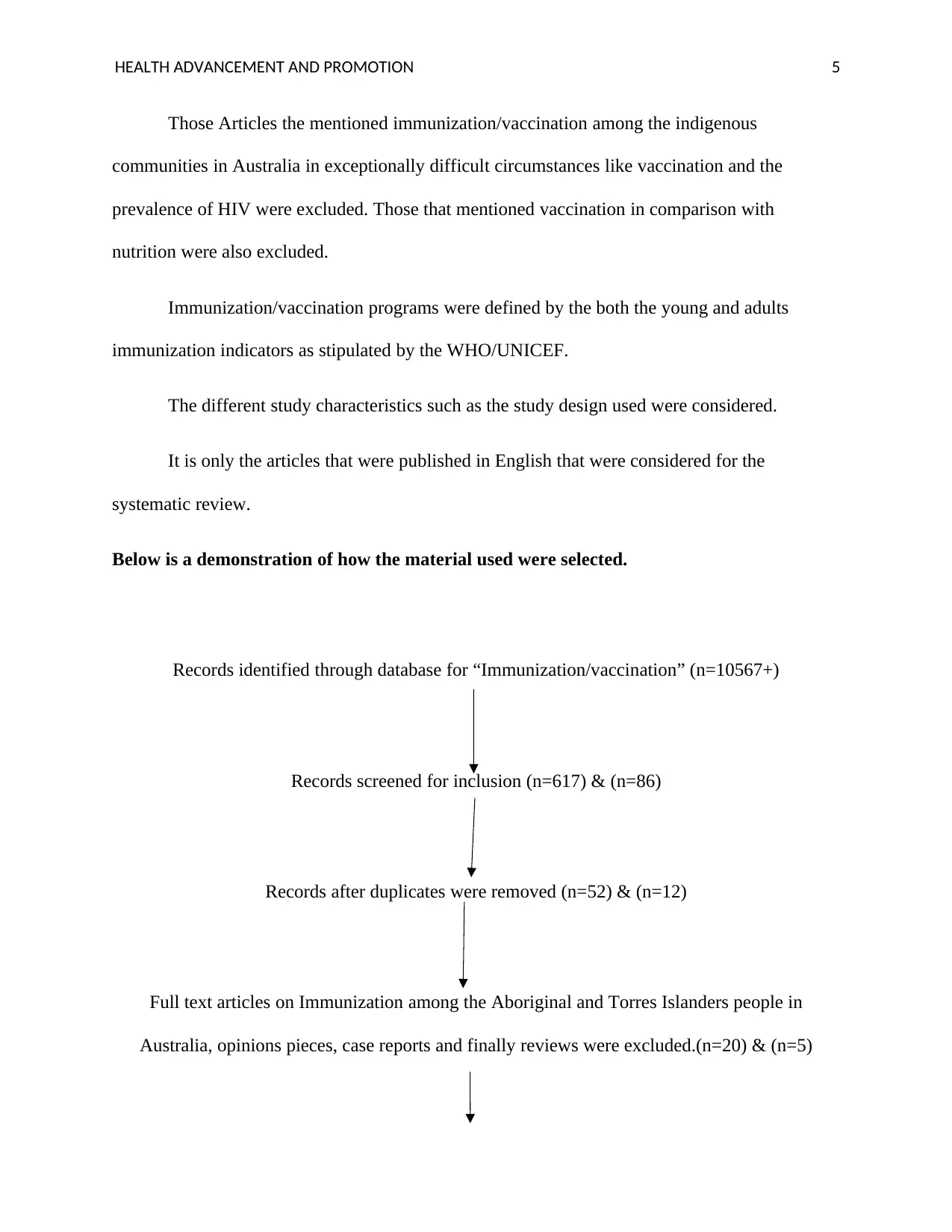
Below is a demonstration of how the material used were selected.
Records identified through database for “Immunization/vaccination” (n=10567+)
Records screened for inclusion (n=617) & (n=86)
Records after duplicates were removed (n=52) & (n=12)
Full text articles on Immunization among the Aboriginal and Torres Islanders people in
Australia, opinions pieces, case reports and finally reviews were excluded.(n=20) & (n=5)
Those Articles the mentioned immunization/vaccination among the indigenous
communities in Australia in exceptionally difficult circumstances like vaccination and the
prevalence of HIV were excluded. Those that mentioned vaccination in comparison with
nutrition were also excluded.
Immunization/vaccination programs were defined by the both the young and adults
immunization indicators as stipulated by the WHO/UNICEF.
The different study characteristics such as the study design used were considered.
It is only the articles that were published in English that were considered for the
systematic review.
Below is a demonstration of how the material used were selected.
Records identified through database for “Immunization/vaccination” (n=10567+)
Records screened for inclusion (n=617) & (n=86)
Records after duplicates were removed (n=52) & (n=12)
Full text articles on Immunization among the Aboriginal and Torres Islanders people in
Australia, opinions pieces, case reports and finally reviews were excluded.(n=20) & (n=5)
HEALTH ADVANCEMENT AND PROMOTION 6
Studies included in the review 7 were cohort studies, 18 were cross-sectional studies and 7 were
mixed methods for determining immunization among the indigenous communities in Australia.
Results:
Summary evidence from the reviewed studies
Conclusion:
Conclusion from the evidence
Immunization among the Aboriginal communities is quite evident due to the reduced
burden of diseases as well as a decreased rate in the hospital admission rates since the
introduction of the National Immunization Program (Jayasinghe et al., 2015). According to
studies, the hospital admission rates have dropped from 28% to only 6% in the past decade.
However, the studies have found out that there exists a very wide gap in the rates of
immunization between the indigenous and the non-indigenous communities. By the time the
children are two years, the gap widens further and this implies delays in immunization among the
Aboriginal communities (Lotter, Regan, Thomas, Effler, & Mak, 2017). The delays makes the
children vulnerable to diseases that can be prevented through vaccination.
Children are however not exclusively protected until they complete the recommended
childhood vaccinations at 4 years of age. At the moment, the studies found out that 94-95% of
Aboriginal children who are above 4 years are considered fully vaccinated.
The rates of immunization are generally improving but the studies established that there
are some factors that affect the immunization coverage rates among the Aboriginals (Pearce,
Marshall, Bedford, & Lynch, 2015). Some of the factors include timeliness as well as
Studies included in the review 7 were cohort studies, 18 were cross-sectional studies and 7 were
mixed methods for determining immunization among the indigenous communities in Australia.
Results:
Summary evidence from the reviewed studies
Conclusion:
Conclusion from the evidence
Immunization among the Aboriginal communities is quite evident due to the reduced
burden of diseases as well as a decreased rate in the hospital admission rates since the
introduction of the National Immunization Program (Jayasinghe et al., 2015). According to
studies, the hospital admission rates have dropped from 28% to only 6% in the past decade.
However, the studies have found out that there exists a very wide gap in the rates of
immunization between the indigenous and the non-indigenous communities. By the time the
children are two years, the gap widens further and this implies delays in immunization among the
Aboriginal communities (Lotter, Regan, Thomas, Effler, & Mak, 2017). The delays makes the
children vulnerable to diseases that can be prevented through vaccination.
Children are however not exclusively protected until they complete the recommended
childhood vaccinations at 4 years of age. At the moment, the studies found out that 94-95% of
Aboriginal children who are above 4 years are considered fully vaccinated.
The rates of immunization are generally improving but the studies established that there
are some factors that affect the immunization coverage rates among the Aboriginals (Pearce,
Marshall, Bedford, & Lynch, 2015). Some of the factors include timeliness as well as
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH ADVANCEMENT AND PROMOTION 7
identification of the Aboriginal status among the different healthcare providers (Reekie et al.,
2018) .Immunization rates have shown reduction in the rates of preventable diseases among the
Aboriginal children in Australia and there should be different strategies to make it better.
Use of personalized calendars can boost the timelines of vaccination among the
Aboriginal children.This is accoding to the AMSWS tool.This is a very cost effective tool and it
also seems practical and effective in improving early childhood vaccination among the
Aboriginal communities in Australia.This program should therefore be supported by the
Australian Government.
Study objectives from the evidence:
The main objective from the evidence was to improve vaccination or immunization
among the indigenous communities in Australia.
To educate these communities on the importance of immunization
To train different healthcare professionals on how to conduct
immunization and how to handle potential resistance from certain sections of the
community.
To collaborate with different stakeholders such as the government, the
community and other organizations to fully implement immunization programs among
the Aboriginal and Torres Islander people.
Further research:
There is need for further intervention studies to be conducted so as to provide further
evidence concerning the best strategies that should be employed to encourage more aboriginal
identification of the Aboriginal status among the different healthcare providers (Reekie et al.,
2018) .Immunization rates have shown reduction in the rates of preventable diseases among the
Aboriginal children in Australia and there should be different strategies to make it better.
Use of personalized calendars can boost the timelines of vaccination among the
Aboriginal children.This is accoding to the AMSWS tool.This is a very cost effective tool and it
also seems practical and effective in improving early childhood vaccination among the
Aboriginal communities in Australia.This program should therefore be supported by the
Australian Government.
Study objectives from the evidence:
The main objective from the evidence was to improve vaccination or immunization
among the indigenous communities in Australia.
To educate these communities on the importance of immunization
To train different healthcare professionals on how to conduct
immunization and how to handle potential resistance from certain sections of the
community.
To collaborate with different stakeholders such as the government, the
community and other organizations to fully implement immunization programs among
the Aboriginal and Torres Islander people.
Further research:
There is need for further intervention studies to be conducted so as to provide further
evidence concerning the best strategies that should be employed to encourage more aboriginal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTH ADVANCEMENT AND PROMOTION 8
and Torres islander people to be vaccinated against most of the preventable infections in
Australia.
and Torres islander people to be vaccinated against most of the preventable infections in
Australia.
HEALTH ADVANCEMENT AND PROMOTION 9
References
Collins, D. A., Hoskins, A., Snelling, T., Senasinghe, K., Bowman, J., Stemberger, N. A., …
Lehmann, D. (2017). Predictors of pneumococcal carriage and the effect of the 13-
valent pneumococcal conjugate vaccination in the Western Australian Aboriginal
population. Pneumonia, 9(1). doi:10.1186/s41479-017-0038-x
Falster, K., Banks, E., Lujic, S., Falster, M., Lynch, J., Zwi, K., … Jorm, L. (2016).
Inequalities in pediatric avoidable hospitalizations between Aboriginal and non-
Aboriginal children in Australia: a population data linkage study. BMC Pediatrics,
16(1). doi:10.1186/s12887-016-0706-7
Fathima, P., Blyth, C. C., Lehmann, D., Lim, F. J., Abdalla, T., De Klerk, N., &
Moore, H. C. (2017). The Impact of Pneumococcal Vaccination on Bacterial and
Viral Pneumonia in Western Australian Children: Record Linkage Cohort Study of
469589 Births, 1996–2012. Clinical Infectious Diseases, 66(7), 1075-1085.
doi:10.1093/cid/cix923
Gidding, H., McCallum, L., Fathima, P., Moore, H., Snelling, T., Blyth, C., … McIntyre, P.
(2018). Effectiveness of a 3 + 0 pneumococcal conjugate vaccine schedule against
invasive pneumococcal disease among a birth cohort of 1.4 million children in
Australia. Vaccine, 36(19), 2650-2656. doi:10.1016/j.vaccine.2018.03.058
Hendry, A. J., Beard, F. H., Dey, A., Meijer, D., Campbell-Lloyd, S., Clark, K. K., …
Sheppeard, V. (2018). Closing the vaccination coverage gap in New South Wales: the
Aboriginal Immunisation Healthcare Worker Program. The Medical Journal of
Australia, 209(1), 24-28. doi:10.5694/mja18.00063
Jayasinghe, S., Chiu, C., Menzies, R., Lehmann, D., Cook, H., Giele, C., … McIntyre, P.
(2015). Evaluation of impact of 23 valent pneumococcal polysaccharide vaccine
References
Collins, D. A., Hoskins, A., Snelling, T., Senasinghe, K., Bowman, J., Stemberger, N. A., …
Lehmann, D. (2017). Predictors of pneumococcal carriage and the effect of the 13-
valent pneumococcal conjugate vaccination in the Western Australian Aboriginal
population. Pneumonia, 9(1). doi:10.1186/s41479-017-0038-x
Falster, K., Banks, E., Lujic, S., Falster, M., Lynch, J., Zwi, K., … Jorm, L. (2016).
Inequalities in pediatric avoidable hospitalizations between Aboriginal and non-
Aboriginal children in Australia: a population data linkage study. BMC Pediatrics,
16(1). doi:10.1186/s12887-016-0706-7
Fathima, P., Blyth, C. C., Lehmann, D., Lim, F. J., Abdalla, T., De Klerk, N., &
Moore, H. C. (2017). The Impact of Pneumococcal Vaccination on Bacterial and
Viral Pneumonia in Western Australian Children: Record Linkage Cohort Study of
469589 Births, 1996–2012. Clinical Infectious Diseases, 66(7), 1075-1085.
doi:10.1093/cid/cix923
Gidding, H., McCallum, L., Fathima, P., Moore, H., Snelling, T., Blyth, C., … McIntyre, P.
(2018). Effectiveness of a 3 + 0 pneumococcal conjugate vaccine schedule against
invasive pneumococcal disease among a birth cohort of 1.4 million children in
Australia. Vaccine, 36(19), 2650-2656. doi:10.1016/j.vaccine.2018.03.058
Hendry, A. J., Beard, F. H., Dey, A., Meijer, D., Campbell-Lloyd, S., Clark, K. K., …
Sheppeard, V. (2018). Closing the vaccination coverage gap in New South Wales: the
Aboriginal Immunisation Healthcare Worker Program. The Medical Journal of
Australia, 209(1), 24-28. doi:10.5694/mja18.00063
Jayasinghe, S., Chiu, C., Menzies, R., Lehmann, D., Cook, H., Giele, C., … McIntyre, P.
(2015). Evaluation of impact of 23 valent pneumococcal polysaccharide vaccine
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH ADVANCEMENT AND PROMOTION
10
following 7 valent pneumococcal conjugate vaccine in Australian Indigenous
children. Vaccine, 33(48), 6666-6674. doi:10.1016/j.vaccine.2015.10.089
Lotter, K., Regan, A. K., Thomas, T., Effler, P. V., & Mak, D. B. (2017). Antenatal influenza
and pertussis vaccine uptake among Aboriginal mothers in Western Australia.
Australian and New Zealand Journal of Obstetrics and Gynaecology, 58(4), 417-424.
doi:10.1111/ajo.12739
Pearce, A., Marshall, H., Bedford, H., & Lynch, J. (2015). Barriers to childhood
immunisation: Findings from the Longitudinal Study of Australian Children. Vaccine,
33(29), 3377-3383. doi:10.1016/j.vaccine.2015.04.089
Reekie, J., Kaldor, J., Mak, D., Ward, J., Donovan, B., Hocking, J., … Liu, B. (2018). Long-
term impact of childhood hepatitis B vaccination programs on prevalence among
Aboriginal and non-Aboriginal women giving birth in Western Australia. Vaccine,
36(23), 3296-3300. doi:10.1016/j.vaccine.2018.04.057
Verdon, S., & McLeod, S. (2015). Indigenous Language Learning and Maintenance Among
Young Australian Aboriginal and Torres Strait Islander Children. International
Journal of Early Childhood, 47(1), 153-170. doi:10.1007/s13158-015-0131-3
10
following 7 valent pneumococcal conjugate vaccine in Australian Indigenous
children. Vaccine, 33(48), 6666-6674. doi:10.1016/j.vaccine.2015.10.089
Lotter, K., Regan, A. K., Thomas, T., Effler, P. V., & Mak, D. B. (2017). Antenatal influenza
and pertussis vaccine uptake among Aboriginal mothers in Western Australia.
Australian and New Zealand Journal of Obstetrics and Gynaecology, 58(4), 417-424.
doi:10.1111/ajo.12739
Pearce, A., Marshall, H., Bedford, H., & Lynch, J. (2015). Barriers to childhood
immunisation: Findings from the Longitudinal Study of Australian Children. Vaccine,
33(29), 3377-3383. doi:10.1016/j.vaccine.2015.04.089
Reekie, J., Kaldor, J., Mak, D., Ward, J., Donovan, B., Hocking, J., … Liu, B. (2018). Long-
term impact of childhood hepatitis B vaccination programs on prevalence among
Aboriginal and non-Aboriginal women giving birth in Western Australia. Vaccine,
36(23), 3296-3300. doi:10.1016/j.vaccine.2018.04.057
Verdon, S., & McLeod, S. (2015). Indigenous Language Learning and Maintenance Among
Young Australian Aboriginal and Torres Strait Islander Children. International
Journal of Early Childhood, 47(1), 153-170. doi:10.1007/s13158-015-0131-3
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





