Bio-psychosocial Model: Interventions & Social Prescribing in Nursing
VerifiedAdded on 2023/06/12
|10
|2446
|83
Essay
AI Summary
This essay provides a comprehensive overview of the bio-psychosocial model and its application in mental health nursing. It explains the three components of the model (biological, psychological, and social) and how they help nurses and midwives identify and assess factors contributing to mental health problems. The essay further elaborates on how these components can be used to plan interventions for individuals experiencing mental health issues, including cognitive-behavioral therapy and dual diagnosis treatment. Additionally, it illustrates the concept of social prescribing and how care nurses can engage in it to connect patients with community resources for emotional and practical support. The essay concludes by emphasizing the importance of the bio-psychosocial approach in understanding and addressing mental well-being difficulties within a broader socio-cultural context.
Mental health
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Content.
INTRODUCTION...........................................................................................................................1
MAIN BODY...................................................................................................................................1
Concept and components of the bio-psychosocial model............................................................1
How bio-psychosocial model help care nurses and practitioners to determine and access
factors that contributed to a person with mental well-being issues.............................................2
Planning of interventions with help of bio-psychosocial model for a person with mental well-
being issues..................................................................................................................................3
Illustrate social prescribing and how care nurses can engage in it..............................................3
CONCLUSION................................................................................................................................5
REFERENCES................................................................................................................................6
INTRODUCTION...........................................................................................................................1
MAIN BODY...................................................................................................................................1
Concept and components of the bio-psychosocial model............................................................1
How bio-psychosocial model help care nurses and practitioners to determine and access
factors that contributed to a person with mental well-being issues.............................................2
Planning of interventions with help of bio-psychosocial model for a person with mental well-
being issues..................................................................................................................................3
Illustrate social prescribing and how care nurses can engage in it..............................................3
CONCLUSION................................................................................................................................5
REFERENCES................................................................................................................................6

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRODUCTION
The concept of mental health generally refers to behavioral, cognitive as well as
emotional health. Its concept is all about how an individual can think, behave as well as can feel.
The term mental well-being sometimes can be used as the absence of mental disorders. The
conditions of mental well-being can affect the daily living functioning of an individual, physical
well-being, and relationships as well. The biopsychosocial model can effectively aid the care
nurses as well as care professionals to understand the interactions within psychosocial and
biological components of disease (Jorm, 2020). These are to enhance the dyadic relationship
among practitioners and their vulnerable patients as well as the effective multidisciplinary care
approaches within patient care. In this report, there is a discussion about the bio-psychosocial
models which are some essential perspectives in an individual’s life. As it can illustrate how a
seemingly healthy person can acquire a mental disorder as well as why a person is more prone to
mental distress or illness than other people. In this, there is also a discussion about the effective
bio-psychosocial models used by the care nurses to plan positive interventions for people who
are having mental well-being issues (Wiss, Schellenberger & Prelip, 2019).
MAIN BODY
Concept and components of the bio-psychosocial model.
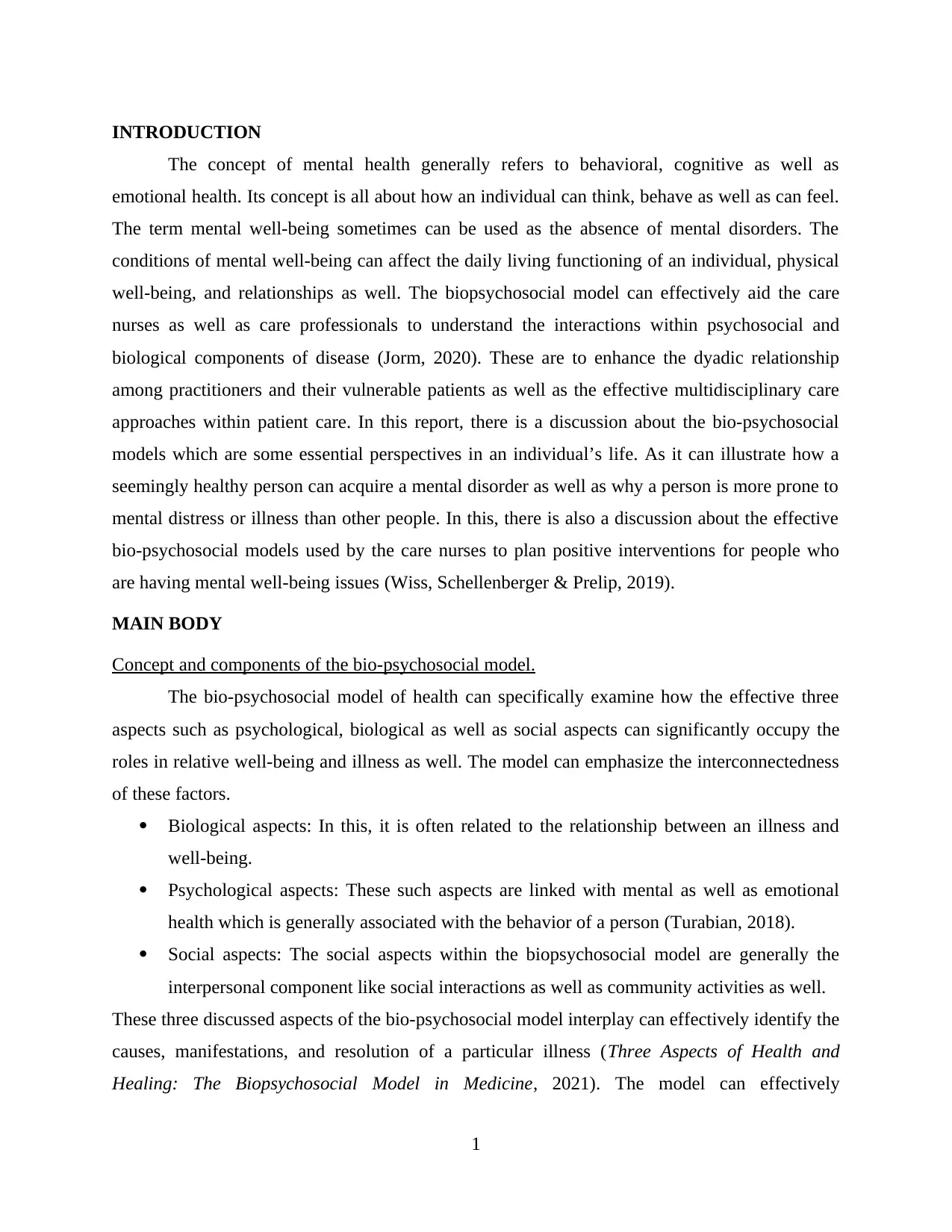
The bio-psychosocial model of health can specifically examine how the effective three
aspects such as psychological, biological as well as social aspects can significantly occupy the
roles in relative well-being and illness as well. The model can emphasize the interconnectedness
of these factors.
Biological aspects: In this, it is often related to the relationship between an illness and
well-being.
Psychological aspects: These such aspects are linked with mental as well as emotional
health which is generally associated with the behavior of a person (Turabian, 2018).
Social aspects: The social aspects within the biopsychosocial model are generally the
interpersonal component like social interactions as well as community activities as well.
These three discussed aspects of the bio-psychosocial model interplay can effectively identify the
causes, manifestations, and resolution of a particular illness (Three Aspects of Health and
Healing: The Biopsychosocial Model in Medicine, 2021). The model can effectively
1
The concept of mental health generally refers to behavioral, cognitive as well as
emotional health. Its concept is all about how an individual can think, behave as well as can feel.
The term mental well-being sometimes can be used as the absence of mental disorders. The
conditions of mental well-being can affect the daily living functioning of an individual, physical
well-being, and relationships as well. The biopsychosocial model can effectively aid the care
nurses as well as care professionals to understand the interactions within psychosocial and
biological components of disease (Jorm, 2020). These are to enhance the dyadic relationship
among practitioners and their vulnerable patients as well as the effective multidisciplinary care
approaches within patient care. In this report, there is a discussion about the bio-psychosocial
models which are some essential perspectives in an individual’s life. As it can illustrate how a
seemingly healthy person can acquire a mental disorder as well as why a person is more prone to
mental distress or illness than other people. In this, there is also a discussion about the effective
bio-psychosocial models used by the care nurses to plan positive interventions for people who
are having mental well-being issues (Wiss, Schellenberger & Prelip, 2019).
MAIN BODY
Concept and components of the bio-psychosocial model.
The bio-psychosocial model of health can specifically examine how the effective three
aspects such as psychological, biological as well as social aspects can significantly occupy the
roles in relative well-being and illness as well. The model can emphasize the interconnectedness
of these factors.
Biological aspects: In this, it is often related to the relationship between an illness and
well-being.
Psychological aspects: These such aspects are linked with mental as well as emotional
health which is generally associated with the behavior of a person (Turabian, 2018).
Social aspects: The social aspects within the biopsychosocial model are generally the
interpersonal component like social interactions as well as community activities as well.
These three discussed aspects of the bio-psychosocial model interplay can effectively identify the
causes, manifestations, and resolution of a particular illness (Three Aspects of Health and
Healing: The Biopsychosocial Model in Medicine, 2021). The model can effectively
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
acknowledge the episodes of stress as well as reduced mental well-being that can contribute to a
disorder within the human body (Davison & Cooke, 2014).
How bio-psychosocial model help care nurses and practitioners determine and access factors that
contributed to a person with mental well-being issues.
The concept of the bio-psychosocial model within the healthcare organization can play an
essential role. The model can help the care nurses as well as practitioners to efficiently
understand the effective interactions between both psychosocial and biological components of
the disease ("My mental health", 2020). These can be done to enhance the more effective
relationships between the vulnerable patients and care nurses or practitioners as well as the
multidisciplinary care team in the care of vulnerable patients.
Planning of interventions with help of a bio-psychosocial model for a person with mental well-
being issues.
With help of the bio-psychosocial model can help to plan the intervention for a person
with mental well-being health issues. In this, mental well-being conditions are generally the
leading causes of disability across the world. The effective intervention for these such conditions
2
disorder within the human body (Davison & Cooke, 2014).
How bio-psychosocial model help care nurses and practitioners determine and access factors that
contributed to a person with mental well-being issues.
The concept of the bio-psychosocial model within the healthcare organization can play an
essential role. The model can help the care nurses as well as practitioners to efficiently
understand the effective interactions between both psychosocial and biological components of
the disease ("My mental health", 2020). These can be done to enhance the more effective
relationships between the vulnerable patients and care nurses or practitioners as well as the
multidisciplinary care team in the care of vulnerable patients.
Planning of interventions with help of a bio-psychosocial model for a person with mental well-
being issues.
With help of the bio-psychosocial model can help to plan the intervention for a person
with mental well-being health issues. In this, mental well-being conditions are generally the
leading causes of disability across the world. The effective intervention for these such conditions
2
can have a key role in their care treatment, although the applicability of the findings to some
pathetic resource settings can be difficult or challenging (Goetz et al., 2015). The bio-
psychosocial interventions to treat mental health issues among people can involve such as
structured counseling, case management, enhancement of motivation, effective coordination to
care, psychotherapy and relapse prevention, and many more. In addition to this, another main
intervention that is specifically used to treat mental health issues is as mentioned below:
Cognitive-behavioral therapy: The therapy is generally a form of psychological care treatment
that has been exhibited to be effective for various or a variety of issues consisting of anxiety,
depression, alcohol abuse, and many more. It is considered that cognitive-behavioral therapy
leads to a specific enhancement in functioning as well as quality of the life as well. Cognitive
therapy mainly includes the efforts to alter the thinking patterns of an individual such as it can
aid in learning to recognize an individual's distortion in a thinking pattern which can create
issues and then re-evaluate them in light of reality as well. In addition to this, the therapy can
effectively provide knowledge to use problem-solving skills so that people with mental health
issues can effectively overcome their issues appropriately (What is Cognitive Behavioral
Therapy? 2017).
Dual diagnosis care treatment: In history, the mental well-being services and drugs misuse
treatment were split. It generally has been created a group of people who specifically decline via
the cracks, it is because they required parts to every care treatment modality. The people having
mental health issues who are receiving the care treatment only address half the issues, that
frequently led to relapse (Inpatient Dual Diagnosis Treatment Centers: Are They for Me? 2022).
The biopsychosocial model consists that psychological (emotions, thoughts, and behaviors)
and social (for example, socio-economic, cultural, and socio-environmental) elements that can
play a specific and positive role in the well-being and illness of a person. In addition, the
multidisciplinary approaches to the care management of acute illness, for example supporting the
patients to manage the illness. Enhancing the pain-coping sources and decreasing the disabilities
and patient emotional distress associated with pain can be executed via various effective self-
regulatory, cognitive, and behavioral techniques (Biopsychosocial model of illnesses in primary
care, 2018).
3
pathetic resource settings can be difficult or challenging (Goetz et al., 2015). The bio-
psychosocial interventions to treat mental health issues among people can involve such as
structured counseling, case management, enhancement of motivation, effective coordination to
care, psychotherapy and relapse prevention, and many more. In addition to this, another main
intervention that is specifically used to treat mental health issues is as mentioned below:
Cognitive-behavioral therapy: The therapy is generally a form of psychological care treatment
that has been exhibited to be effective for various or a variety of issues consisting of anxiety,
depression, alcohol abuse, and many more. It is considered that cognitive-behavioral therapy
leads to a specific enhancement in functioning as well as quality of the life as well. Cognitive
therapy mainly includes the efforts to alter the thinking patterns of an individual such as it can
aid in learning to recognize an individual's distortion in a thinking pattern which can create
issues and then re-evaluate them in light of reality as well. In addition to this, the therapy can
effectively provide knowledge to use problem-solving skills so that people with mental health
issues can effectively overcome their issues appropriately (What is Cognitive Behavioral
Therapy? 2017).
Dual diagnosis care treatment: In history, the mental well-being services and drugs misuse
treatment were split. It generally has been created a group of people who specifically decline via
the cracks, it is because they required parts to every care treatment modality. The people having
mental health issues who are receiving the care treatment only address half the issues, that
frequently led to relapse (Inpatient Dual Diagnosis Treatment Centers: Are They for Me? 2022).
The biopsychosocial model consists that psychological (emotions, thoughts, and behaviors)
and social (for example, socio-economic, cultural, and socio-environmental) elements that can
play a specific and positive role in the well-being and illness of a person. In addition, the
multidisciplinary approaches to the care management of acute illness, for example supporting the
patients to manage the illness. Enhancing the pain-coping sources and decreasing the disabilities
and patient emotional distress associated with pain can be executed via various effective self-
regulatory, cognitive, and behavioral techniques (Biopsychosocial model of illnesses in primary
care, 2018).
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Illustrate social prescribing and how care nurses can engage in it.
The term “social prescribing” is generally a pathway for the local agencies to refer
individuals to link a worker. In this, associating the workers can provide a person time,
concentrate on what things can matter to a person as well as can take a holistic approach towards
the well-being and health of a person. It can help to connect the people to the groups within
communities as well as a statutory service for both emotional as well as practical support. In this,
the social prescribing generally works for a broad variety of people such as those with one or
more long-term conditions, a person who specifically requires encouragement with their mental
well-being, the person who is isolated, the person who involves more complex needs that can
make influence over the health (Social prescribing, 2022).
Social prescribing can allow the well-being care professionals to refer vulnerable patients
to a broad range of local non-medical services which can offer empowerment as well as support
for emotional, social as well as practical requirements. Most of the clinical commissioning
groups as well as the local government organizations are already investing in schemes of social
prescribing, that can run in mainly voluntary settings. The schemes involved are healthy
4
The term “social prescribing” is generally a pathway for the local agencies to refer
individuals to link a worker. In this, associating the workers can provide a person time,
concentrate on what things can matter to a person as well as can take a holistic approach towards
the well-being and health of a person. It can help to connect the people to the groups within
communities as well as a statutory service for both emotional as well as practical support. In this,
the social prescribing generally works for a broad variety of people such as those with one or
more long-term conditions, a person who specifically requires encouragement with their mental
well-being, the person who is isolated, the person who involves more complex needs that can
make influence over the health (Social prescribing, 2022).
Social prescribing can allow the well-being care professionals to refer vulnerable patients
to a broad range of local non-medical services which can offer empowerment as well as support
for emotional, social as well as practical requirements. Most of the clinical commissioning
groups as well as the local government organizations are already investing in schemes of social
prescribing, that can run in mainly voluntary settings. The schemes involved are healthy
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
exercise/eating, ballet for all age groups, and many more. In addition to this, the link care
workers can work with the people to produce an effective personalized plan to allow the people
to maintain their well-being and stay healthy (LEKA et al., 2018). The concept of social
prescribing is generally more than a method of signposting, but instead, a person can be helped
to take specific action steps to seek out empowerment as well as can engage with the societies
(Kim & Park, 2019).
CONCLUSION
From the above discussion, it is concluded that the bio-psychosocial approach has
generally imparted an avoid of profoundly established characteristics of a western folk model
like the body-mind can split as well as made an essential conceptual contribution to
understanding the mental well-being difficulties in a broader area. The bio-psychosocial
approaches generally play a central role that both the central beliefs as well as care practices can
play in understanding mental well-being difficulties. In this, it can aid facilitate a concentration
on specific idioms of distress which are greatly associated with enhancing the effective
interventions for mental well-being issues in various socio-cultural contexts well. It is analyzed
by the study that the bio-psychosocial model generally stresses a complex combination of both
psychological and biological aspects of medicine. The primary healthcare professionals and care
nurses can use the biopsychosocial model to enhance the clinical results, via producing an
awareness of the specific interactions within psychological, biological, and socio-cultural
components and to enhance the self-management of the disorders of patients through dual
relationships and a multidisciplinary approach of patient care.
5
workers can work with the people to produce an effective personalized plan to allow the people
to maintain their well-being and stay healthy (LEKA et al., 2018). The concept of social
prescribing is generally more than a method of signposting, but instead, a person can be helped
to take specific action steps to seek out empowerment as well as can engage with the societies
(Kim & Park, 2019).
CONCLUSION
From the above discussion, it is concluded that the bio-psychosocial approach has
generally imparted an avoid of profoundly established characteristics of a western folk model
like the body-mind can split as well as made an essential conceptual contribution to
understanding the mental well-being difficulties in a broader area. The bio-psychosocial
approaches generally play a central role that both the central beliefs as well as care practices can
play in understanding mental well-being difficulties. In this, it can aid facilitate a concentration
on specific idioms of distress which are greatly associated with enhancing the effective
interventions for mental well-being issues in various socio-cultural contexts well. It is analyzed
by the study that the bio-psychosocial model generally stresses a complex combination of both
psychological and biological aspects of medicine. The primary healthcare professionals and care
nurses can use the biopsychosocial model to enhance the clinical results, via producing an
awareness of the specific interactions within psychological, biological, and socio-cultural
components and to enhance the self-management of the disorders of patients through dual
relationships and a multidisciplinary approach of patient care.
5
REFERENCES
Books and Journals:
Cénat, J. M., Mukunzi, J. N., Noorishad, P. G., Rousseau, C., Derivois, D., & Bukaka, J. (2020).
A systematic review of mental health programs among populations affected by the Ebola
virus disease. Journal of Psychosomatic Research, 131, 109966.
Friedman, S. M., Mulhausen, P., Cleveland, M. L., Coll, P. P., Daniel, K. M., Hayward, A. D., ...
& White, H. K. (2019). Healthy aging: American Geriatrics Society white paper
executive summary. Journal of the American Geriatrics Society, 67(1), 17-20.
Jara‐Ogeda, R., Leyton, D., & Grandón, P. (2022). Stigmatization of people diagnosed with a
mental disorder in secondary mental health centers in Chile: An ethnographic
study. Journal of Community Psychology.
Kim, Y. K., & Park, S. C. (2019). Classification of psychiatric disorders. In Frontiers in
Psychiatry (pp. 17-25). Springer, Singapore.
Moe, J., Johnson, K., Park, K., & Finnerty, P. (2018). Integrated behavioral health and
counseling gender and sexual minority populations. Journal of LGBT Issues in
Counseling, 12(4), 215-229.
Jorm, A. (2020). We need to move from ‘mental health literacy’ to ‘mental health
action’. Mental Health &Amp; Prevention, 18, 200179.
https://doi.org/10.1016/j.mhp.2020.200179
Turabian, J. (2018). Gendering of Bio Psychosocial Model and General Practice. Journal Of
Women’S Health Care, 07(01). https://doi.org/10.4172/2167-0420.1000e131
My mental health. (2020), 10(4), 38-38. https://doi.org/10.7748/mhp.10.4.38.s35
Goetz, K., Berger, S., Gavartina, A., Zaroti, S., & Szecsenyi, J. (2015). How psychosocial factors
affect well-being of practice assistants at work in general medical care? – a questionnaire
survey. BMC Family Practice, 16(1). https://doi.org/10.1186/s12875-015-0366-y
LEKA, S., HASSARD, J., & YANAGIDA, A. (2018). Investigating the impact of psychosocial
risks and occupational stress on psychiatric hospital nurses' mental well-being in
Japan. Journal Of Psychiatric And Mental Health Nursing, 19(2), 123-131.
https://doi.org/10.1111/j.1365-2850.2011.01764.x
Davison, I., & Cooke, S. (2014). HOW NURSES' ATTITUDES AND ACTIONS CAN
INFLUENCE SHARED CARE. Journal Of Renal Care, 41(2), 96-103.
https://doi.org/10.1111/jorc.12105
Sliedrecht, W., de Waart, R., Witkiewitz, K., & Roozen, H. G. (2019). Alcohol use disorder
relapse factors: A systematic review. Psychiatry Research, 278, 97-115.
Smith, D. (2019). Reflecting on new models for osteopathy–it's time for change. International
Journal of Osteopathic Medicine, 31, 15-20.
Vella, S. A., Schweickle, M. J., Sutcliffe, J. T., & Swann, C. (2021). A systematic review and
meta-synthesis of mental health position statements in sport: Scope, quality and future
directions. Psychology of Sport and Exercise, 55, 101946.
Wiss, D. A., Schellenberger, M., & Prelip, M. L. (2019). Rapid assessment of nutrition services
in Los Angeles substance use disorder treatment centers. Journal of Community
Health, 44(1), 88-94.
Wong, J. J., Maddux, M., & Park, K. T. (2018). Mental health service needs in children and
adolescents with inflammatory bowel disease and other chronic gastrointestinal
disorders. Journal of Pediatric Gastroenterology and Nutrition, 67(3), 314-317.
6
Books and Journals:
Cénat, J. M., Mukunzi, J. N., Noorishad, P. G., Rousseau, C., Derivois, D., & Bukaka, J. (2020).
A systematic review of mental health programs among populations affected by the Ebola
virus disease. Journal of Psychosomatic Research, 131, 109966.
Friedman, S. M., Mulhausen, P., Cleveland, M. L., Coll, P. P., Daniel, K. M., Hayward, A. D., ...
& White, H. K. (2019). Healthy aging: American Geriatrics Society white paper
executive summary. Journal of the American Geriatrics Society, 67(1), 17-20.
Jara‐Ogeda, R., Leyton, D., & Grandón, P. (2022). Stigmatization of people diagnosed with a
mental disorder in secondary mental health centers in Chile: An ethnographic
study. Journal of Community Psychology.
Kim, Y. K., & Park, S. C. (2019). Classification of psychiatric disorders. In Frontiers in
Psychiatry (pp. 17-25). Springer, Singapore.
Moe, J., Johnson, K., Park, K., & Finnerty, P. (2018). Integrated behavioral health and
counseling gender and sexual minority populations. Journal of LGBT Issues in
Counseling, 12(4), 215-229.
Jorm, A. (2020). We need to move from ‘mental health literacy’ to ‘mental health
action’. Mental Health &Amp; Prevention, 18, 200179.
https://doi.org/10.1016/j.mhp.2020.200179
Turabian, J. (2018). Gendering of Bio Psychosocial Model and General Practice. Journal Of
Women’S Health Care, 07(01). https://doi.org/10.4172/2167-0420.1000e131
My mental health. (2020), 10(4), 38-38. https://doi.org/10.7748/mhp.10.4.38.s35
Goetz, K., Berger, S., Gavartina, A., Zaroti, S., & Szecsenyi, J. (2015). How psychosocial factors
affect well-being of practice assistants at work in general medical care? – a questionnaire
survey. BMC Family Practice, 16(1). https://doi.org/10.1186/s12875-015-0366-y
LEKA, S., HASSARD, J., & YANAGIDA, A. (2018). Investigating the impact of psychosocial
risks and occupational stress on psychiatric hospital nurses' mental well-being in
Japan. Journal Of Psychiatric And Mental Health Nursing, 19(2), 123-131.
https://doi.org/10.1111/j.1365-2850.2011.01764.x
Davison, I., & Cooke, S. (2014). HOW NURSES' ATTITUDES AND ACTIONS CAN
INFLUENCE SHARED CARE. Journal Of Renal Care, 41(2), 96-103.
https://doi.org/10.1111/jorc.12105
Sliedrecht, W., de Waart, R., Witkiewitz, K., & Roozen, H. G. (2019). Alcohol use disorder
relapse factors: A systematic review. Psychiatry Research, 278, 97-115.
Smith, D. (2019). Reflecting on new models for osteopathy–it's time for change. International
Journal of Osteopathic Medicine, 31, 15-20.
Vella, S. A., Schweickle, M. J., Sutcliffe, J. T., & Swann, C. (2021). A systematic review and
meta-synthesis of mental health position statements in sport: Scope, quality and future
directions. Psychology of Sport and Exercise, 55, 101946.
Wiss, D. A., Schellenberger, M., & Prelip, M. L. (2019). Rapid assessment of nutrition services
in Los Angeles substance use disorder treatment centers. Journal of Community
Health, 44(1), 88-94.
Wong, J. J., Maddux, M., & Park, K. T. (2018). Mental health service needs in children and
adolescents with inflammatory bowel disease and other chronic gastrointestinal
disorders. Journal of Pediatric Gastroenterology and Nutrition, 67(3), 314-317.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Online:
Three Aspects of Health and Healing: The Bio-psychosocial Model in Medicine, 2021 [Online]
Available through: <https://surgery.wustl.edu/three-aspects-of-health-and-healing-the-
biopsychosocial-model/>
Social prescribing, 2022 [Online] Available through:
<https://www.rcn.org.uk/clinical-topics/public-health/self-care/social-prescribing>
What is Cognitive Behavioral Therapy?, 2017 [Online] Available through:
<https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral>
Inpatient Dual Diagnosis Treatment Centers: Are They for Me?, 2022 [Online] Available
through: <https://www.gbhoh.com/inpatient-dual-diagnosis-treatment-centers-are-they-for-me/>
Biopsychosocial model of illnesses in primary care, 2018 [Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069638/
7
Three Aspects of Health and Healing: The Bio-psychosocial Model in Medicine, 2021 [Online]
Available through: <https://surgery.wustl.edu/three-aspects-of-health-and-healing-the-
biopsychosocial-model/>
Social prescribing, 2022 [Online] Available through:
<https://www.rcn.org.uk/clinical-topics/public-health/self-care/social-prescribing>
What is Cognitive Behavioral Therapy?, 2017 [Online] Available through:
<https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral>
Inpatient Dual Diagnosis Treatment Centers: Are They for Me?, 2022 [Online] Available
through: <https://www.gbhoh.com/inpatient-dual-diagnosis-treatment-centers-are-they-for-me/>
Biopsychosocial model of illnesses in primary care, 2018 [Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069638/
7
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





