The Use of Biochemical Markers for Nasogastric Tube Placement
VerifiedAdded on 2023/01/16
|9
|1917
|31
Essay
AI Summary
This essay critically analyzes the use of biochemical markers, specifically pH testing and bilirubin levels, to determine the correct placement of nasogastric tubes in adult patients within hospital settings. The essay begins by establishing the clinical importance of accurate tube placement to prevent complications and improve patient outcomes, highlighting the role of nurses in this process. It then presents a PICO table outlining the patient population, intervention, comparison, and outcomes related to this clinical question. A literature search strategy is described, focusing on randomized control trials and systematic reviews published between 2010 and 2018. The essay then examines the findings of relevant studies, with a primary focus on Fernandez et al. (2010), which supports the use of biochemical markers, particularly the combined use of pH and bilirubin, as a reliable bedside method for verifying tube placement. It also acknowledges the limitations of pH testing, such as the influence of antacid medications and continuous feeding, while referencing other supporting studies and alternative methods like x-ray and ultrasound. The essay concludes that the combination of pH testing and bilirubin remains the best option for bedside testing, emphasizing the need for empowering practitioners with practical skills to enhance the effectiveness of this method and minimize patient exposure to radiation.

Running head: NASOGASTRIC TUBE IN ADULT PATIENTS
1
The use of biochemical markers for determining the correct placement of nasogastric tube in
adult patients in hospital settings?
Student’s Name
University
1
The use of biochemical markers for determining the correct placement of nasogastric tube in
adult patients in hospital settings?
Student’s Name
University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NASOGASTRIC TUBE IN ADULT PATIENTS 2
The use of biochemical markers for determining the correct placement of nasogastric tube
in adult patients in hospital settings?
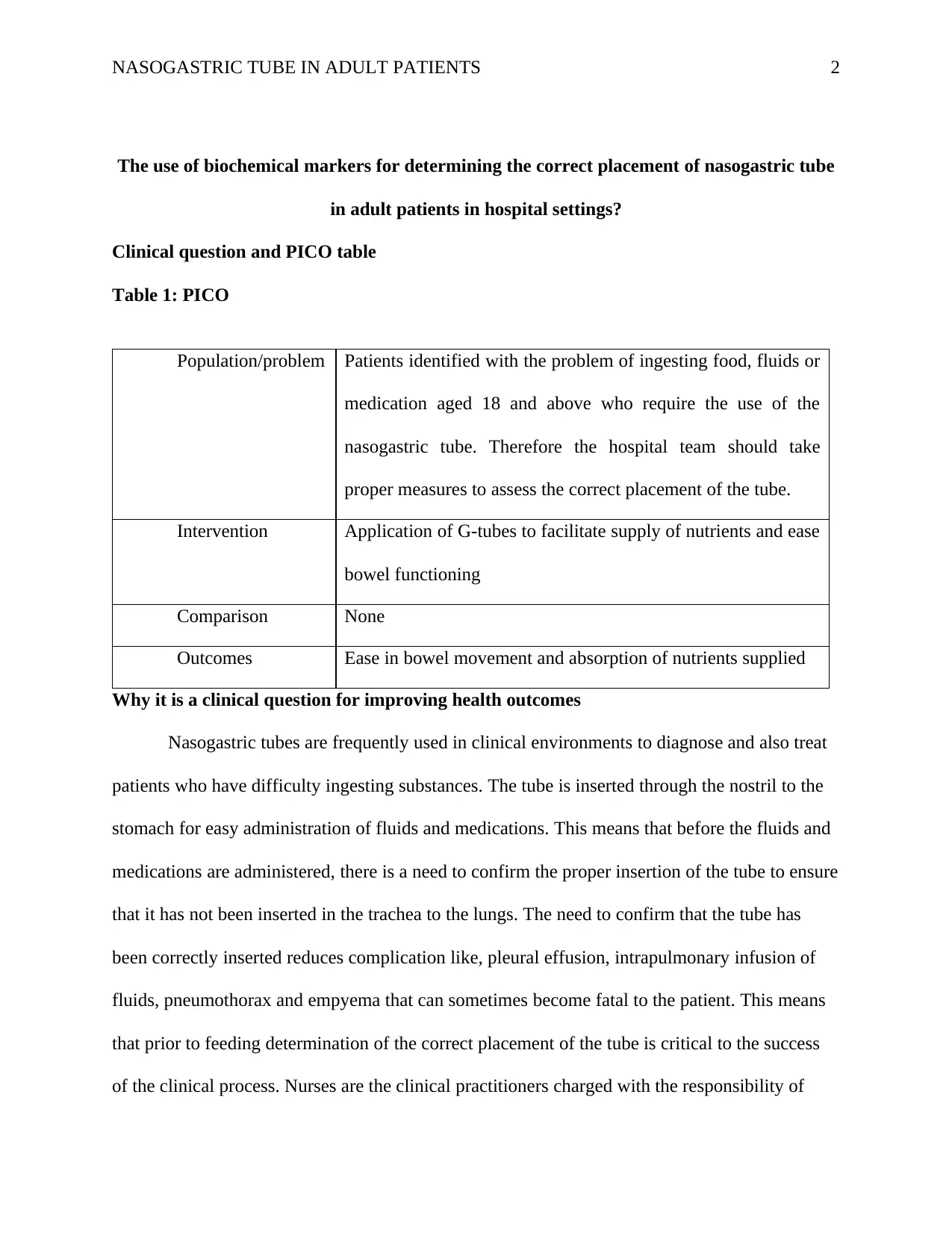
Clinical question and PICO table
Table 1: PICO
Population/problem Patients identified with the problem of ingesting food, fluids or
medication aged 18 and above who require the use of the
nasogastric tube. Therefore the hospital team should take
proper measures to assess the correct placement of the tube.
Intervention Application of G-tubes to facilitate supply of nutrients and ease
bowel functioning
Comparison None
Outcomes Ease in bowel movement and absorption of nutrients supplied
Why it is a clinical question for improving health outcomes
Nasogastric tubes are frequently used in clinical environments to diagnose and also treat
patients who have difficulty ingesting substances. The tube is inserted through the nostril to the
stomach for easy administration of fluids and medications. This means that before the fluids and
medications are administered, there is a need to confirm the proper insertion of the tube to ensure
that it has not been inserted in the trachea to the lungs. The need to confirm that the tube has
been correctly inserted reduces complication like, pleural effusion, intrapulmonary infusion of
fluids, pneumothorax and empyema that can sometimes become fatal to the patient. This means
that prior to feeding determination of the correct placement of the tube is critical to the success
of the clinical process. Nurses are the clinical practitioners charged with the responsibility of
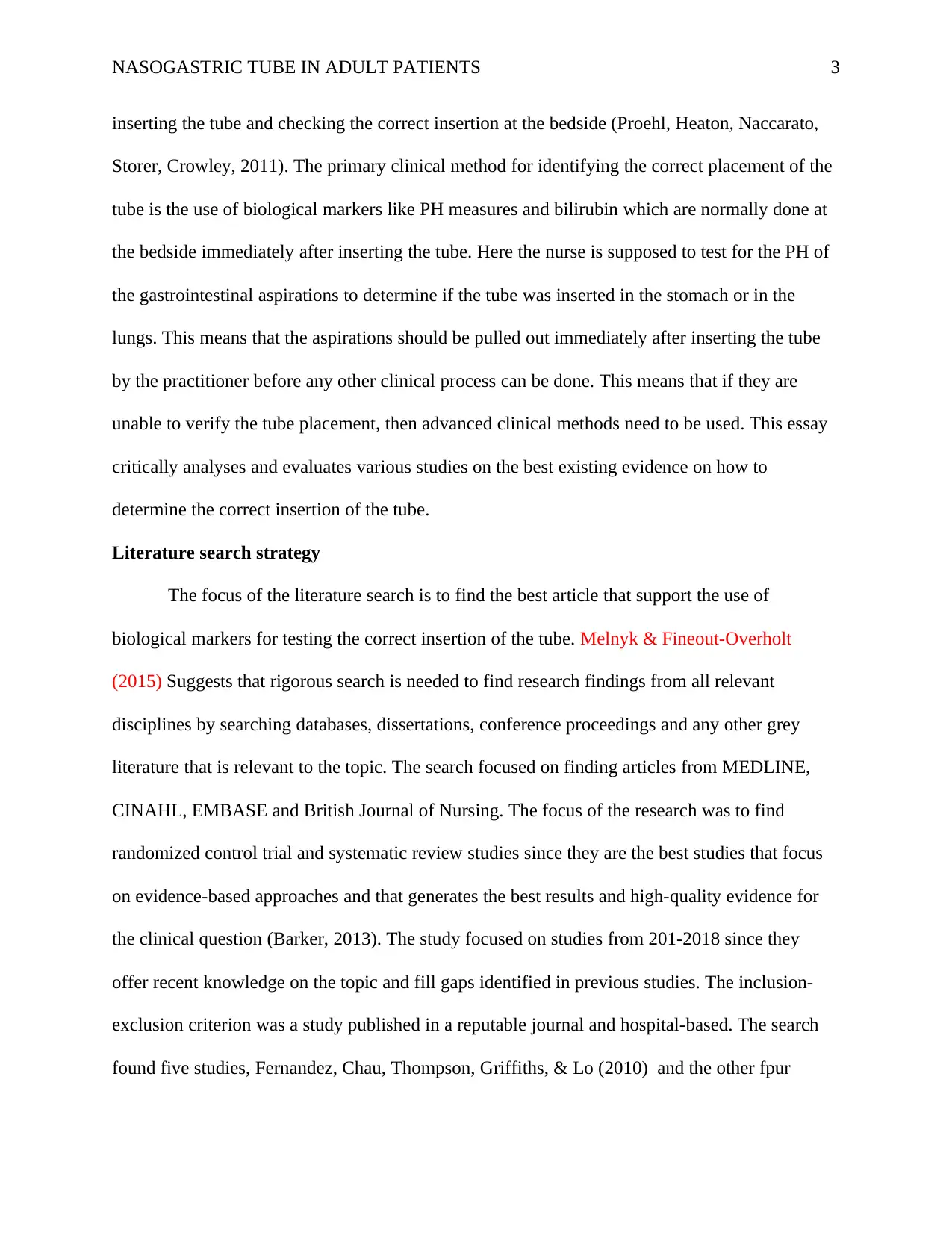
The use of biochemical markers for determining the correct placement of nasogastric tube
in adult patients in hospital settings?
Clinical question and PICO table
Table 1: PICO
Population/problem Patients identified with the problem of ingesting food, fluids or
medication aged 18 and above who require the use of the
nasogastric tube. Therefore the hospital team should take
proper measures to assess the correct placement of the tube.
Intervention Application of G-tubes to facilitate supply of nutrients and ease
bowel functioning
Comparison None
Outcomes Ease in bowel movement and absorption of nutrients supplied
Why it is a clinical question for improving health outcomes
Nasogastric tubes are frequently used in clinical environments to diagnose and also treat
patients who have difficulty ingesting substances. The tube is inserted through the nostril to the
stomach for easy administration of fluids and medications. This means that before the fluids and
medications are administered, there is a need to confirm the proper insertion of the tube to ensure
that it has not been inserted in the trachea to the lungs. The need to confirm that the tube has
been correctly inserted reduces complication like, pleural effusion, intrapulmonary infusion of
fluids, pneumothorax and empyema that can sometimes become fatal to the patient. This means
that prior to feeding determination of the correct placement of the tube is critical to the success
of the clinical process. Nurses are the clinical practitioners charged with the responsibility of
NASOGASTRIC TUBE IN ADULT PATIENTS 3
inserting the tube and checking the correct insertion at the bedside (Proehl, Heaton, Naccarato,
Storer, Crowley, 2011). The primary clinical method for identifying the correct placement of the
tube is the use of biological markers like PH measures and bilirubin which are normally done at
the bedside immediately after inserting the tube. Here the nurse is supposed to test for the PH of
the gastrointestinal aspirations to determine if the tube was inserted in the stomach or in the
lungs. This means that the aspirations should be pulled out immediately after inserting the tube
by the practitioner before any other clinical process can be done. This means that if they are
unable to verify the tube placement, then advanced clinical methods need to be used. This essay
critically analyses and evaluates various studies on the best existing evidence on how to
determine the correct insertion of the tube.
Literature search strategy
The focus of the literature search is to find the best article that support the use of
biological markers for testing the correct insertion of the tube. Melnyk & Fineout-Overholt
(2015) Suggests that rigorous search is needed to find research findings from all relevant
disciplines by searching databases, dissertations, conference proceedings and any other grey
literature that is relevant to the topic. The search focused on finding articles from MEDLINE,
CINAHL, EMBASE and British Journal of Nursing. The focus of the research was to find
randomized control trial and systematic review studies since they are the best studies that focus
on evidence-based approaches and that generates the best results and high-quality evidence for
the clinical question (Barker, 2013). The study focused on studies from 201-2018 since they
offer recent knowledge on the topic and fill gaps identified in previous studies. The inclusion-
exclusion criterion was a study published in a reputable journal and hospital-based. The search
found five studies, Fernandez, Chau, Thompson, Griffiths, & Lo (2010) and the other fpur
inserting the tube and checking the correct insertion at the bedside (Proehl, Heaton, Naccarato,
Storer, Crowley, 2011). The primary clinical method for identifying the correct placement of the
tube is the use of biological markers like PH measures and bilirubin which are normally done at
the bedside immediately after inserting the tube. Here the nurse is supposed to test for the PH of
the gastrointestinal aspirations to determine if the tube was inserted in the stomach or in the
lungs. This means that the aspirations should be pulled out immediately after inserting the tube
by the practitioner before any other clinical process can be done. This means that if they are
unable to verify the tube placement, then advanced clinical methods need to be used. This essay
critically analyses and evaluates various studies on the best existing evidence on how to
determine the correct insertion of the tube.
Literature search strategy
The focus of the literature search is to find the best article that support the use of
biological markers for testing the correct insertion of the tube. Melnyk & Fineout-Overholt
(2015) Suggests that rigorous search is needed to find research findings from all relevant
disciplines by searching databases, dissertations, conference proceedings and any other grey
literature that is relevant to the topic. The search focused on finding articles from MEDLINE,
CINAHL, EMBASE and British Journal of Nursing. The focus of the research was to find
randomized control trial and systematic review studies since they are the best studies that focus
on evidence-based approaches and that generates the best results and high-quality evidence for
the clinical question (Barker, 2013). The study focused on studies from 201-2018 since they
offer recent knowledge on the topic and fill gaps identified in previous studies. The inclusion-
exclusion criterion was a study published in a reputable journal and hospital-based. The search
found five studies, Fernandez, Chau, Thompson, Griffiths, & Lo (2010) and the other fpur
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NASOGASTRIC TUBE IN ADULT PATIENTS 4
supporting studies were Boeykens, Steeman, & Duysburgh (2014), Chan, Tan, Jabin, Lee, &
Ang (2012), Tho, Mordiffi, Ang, & Chen (2011) and Rowat, Graham, & Dennis (2018).
Explanation of the article and comparison with other articles in the search
The study that was relevant was Fernandez, Chau, Thompson, Griffiths, & Lo (2010)
which presents the use of biochemical markers to confirm the correct placement of the tube.
Since the focus of the topic is the use of biological markers for testing the correct placement of
the tube, then this study offers the best evidence to support this topic. This study proposes the
use of biochemical makers rather than other radioactive methods like x-ray and ultrasound as the
primary method of verifying the correct placement of the tube. This study proposes the use of
PH and bilirubin to confirm the correct placement of the tube. According to the study, the
accuracy of the biochemical markers is increased if the PH and bilirubin methods are combined
since it increases the prediction accuracy to 98.3%. This means that after the PH test has been
done, the bilirubin test is used to differentiate between gastric and intestinal tube placement thus
increasing the likelihood of the results. The verification is based on the contingent of successful
aspiration of fluids from the gastric or intestines so that the PH can be tested.
This method offers the best results since other studies like the ones by Boeykens,
Steeman, & Duysburgh (2014), Chan, Tan, Jabin, Lee, & Ang (2012) and Tho, Mordiffi, Ang, &
Chen (2011) that support the use of PH testing as the primary bedside method for confirming the
correct placement of the tube. This means that the practitioner needs to ensure that the PH
method has first been used to test the intestinal and gastric aspirations to determine the position
of the tube. This method has been attributed to its clinical effects due to the reduced risk of
radiations that can affect the patient and cause other secondary long-term effects. This means
supporting studies were Boeykens, Steeman, & Duysburgh (2014), Chan, Tan, Jabin, Lee, &
Ang (2012), Tho, Mordiffi, Ang, & Chen (2011) and Rowat, Graham, & Dennis (2018).
Explanation of the article and comparison with other articles in the search
The study that was relevant was Fernandez, Chau, Thompson, Griffiths, & Lo (2010)
which presents the use of biochemical markers to confirm the correct placement of the tube.
Since the focus of the topic is the use of biological markers for testing the correct placement of
the tube, then this study offers the best evidence to support this topic. This study proposes the
use of biochemical makers rather than other radioactive methods like x-ray and ultrasound as the
primary method of verifying the correct placement of the tube. This study proposes the use of
PH and bilirubin to confirm the correct placement of the tube. According to the study, the
accuracy of the biochemical markers is increased if the PH and bilirubin methods are combined
since it increases the prediction accuracy to 98.3%. This means that after the PH test has been
done, the bilirubin test is used to differentiate between gastric and intestinal tube placement thus
increasing the likelihood of the results. The verification is based on the contingent of successful
aspiration of fluids from the gastric or intestines so that the PH can be tested.
This method offers the best results since other studies like the ones by Boeykens,
Steeman, & Duysburgh (2014), Chan, Tan, Jabin, Lee, & Ang (2012) and Tho, Mordiffi, Ang, &
Chen (2011) that support the use of PH testing as the primary bedside method for confirming the
correct placement of the tube. This means that the practitioner needs to ensure that the PH
method has first been used to test the intestinal and gastric aspirations to determine the position
of the tube. This method has been attributed to its clinical effects due to the reduced risk of
radiations that can affect the patient and cause other secondary long-term effects. This means
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NASOGASTRIC TUBE IN ADULT PATIENTS 5
that education and empowerment of nurses are critical in ensuring that the practitioner accurately
analyses and tests the aspirated contents of the patient.
Despite the reliability of the PH method, another study by Rowat, Graham, & Dennis
(2018) suggests that the reliability of this method is depended on the aspiration of
gastrointestinal fluids that can be used to test the position of the tube. Thus care needs to be
observed when obtaining the aspirations of the patient to avoid variability between the methods
and the sample. Sometimes if the PH patient is using antacid medications and also received
continuous feeding, it may be difficult to assess the placement of the tube using the PH method.
This calls for the use of the bilirubin test and if the results are still not clear, then the practitioner
can use x-ray and ultrasound methods to confirm the placement of the tube. This means that
other clinical signs can be used to increase the outcome of the results like the visual analysis of
the aspiration to ensure the validity of the results.
Conclusion
Therefore, the combination of PH testing and bilirubin method are the best options for
testing the correct placement of the tube since they reduce exposure to radiation. Despite the fact
that there are other methods for testing the correct insertion of the tube-like x-ray and ultrasound,
the bedside method of PH and bilirubin remains the primary one since the practitioner can only
use other methods if the primary method has been ineffective. Thus to increase the outcome of
this method, practitioners need to be empowered with the practical testing skills to increase the
applicability of the method. This essay concludes that the PH and bilirubin methods remain the
bedside tests for determining the correct placement of the nasogastric tube to minimize the
complications that are related to wrong placement. Thus clinicians are only supposed to use other
that education and empowerment of nurses are critical in ensuring that the practitioner accurately
analyses and tests the aspirated contents of the patient.
Despite the reliability of the PH method, another study by Rowat, Graham, & Dennis
(2018) suggests that the reliability of this method is depended on the aspiration of
gastrointestinal fluids that can be used to test the position of the tube. Thus care needs to be
observed when obtaining the aspirations of the patient to avoid variability between the methods
and the sample. Sometimes if the PH patient is using antacid medications and also received
continuous feeding, it may be difficult to assess the placement of the tube using the PH method.
This calls for the use of the bilirubin test and if the results are still not clear, then the practitioner
can use x-ray and ultrasound methods to confirm the placement of the tube. This means that
other clinical signs can be used to increase the outcome of the results like the visual analysis of
the aspiration to ensure the validity of the results.
Conclusion
Therefore, the combination of PH testing and bilirubin method are the best options for
testing the correct placement of the tube since they reduce exposure to radiation. Despite the fact
that there are other methods for testing the correct insertion of the tube-like x-ray and ultrasound,
the bedside method of PH and bilirubin remains the primary one since the practitioner can only
use other methods if the primary method has been ineffective. Thus to increase the outcome of
this method, practitioners need to be empowered with the practical testing skills to increase the
applicability of the method. This essay concludes that the PH and bilirubin methods remain the
bedside tests for determining the correct placement of the nasogastric tube to minimize the
complications that are related to wrong placement. Thus clinicians are only supposed to use other
NASOGASTRIC TUBE IN ADULT PATIENTS 6
secondary methods like xi-ray and ultrasound if the primary method has not been effective in
verifying the correct insertion of the tube.
secondary methods like xi-ray and ultrasound if the primary method has not been effective in
verifying the correct insertion of the tube.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

NASOGASTRIC TUBE IN ADULT PATIENTS 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NASOGASTRIC TUBE IN ADULT PATIENTS 8
References
Barker, J. (2013). Evidence-Based Practice for Nurses. London: Sage.
Boeykens, K., Steeman, E., & Duysburgh, I. (2014). Reliability of pH measurement and the
auscultatory method to confirm the position of a nasogastric tube. International Journal
of Nursing Studies, 51(11), 1427-1433.
Brun, P.-M., Chenaitia, H., Lablanche, C., Pradel, A.-L., Denile, C., Bessereau, J., & Melaine, R.
(2014). 2-Point Ultrasonography to Confirm Correct Position of the Gastric Tube in
Prehospital Setting. Military Medicine, 179(9), 959–963.
Chan, E., Tan, S., Jabin, K., Lee, L., & Ang, C. (2012). Nasogastric feeding practices: A survey
using clinical scenarios, , 49 (3), pp. International Journal of Nursing Studies, 49(3),
310-319.
Fernandez, R., Chau, J., Thompson, D., Griffiths, R., & Lo, H. (2010). Accuracy of biochemical
markers for predicting nasogastric tube placement in adults—A systematic review of
diagnostic studies. International Journal of Nursing Studies, 47(8), 1037-1046.
Melnyk, B. M., & Fineout-Overholt, E. (2015). Evidence-Based Practice in Nursing &
Healthcare: A Guide to Best Practice (3rd ed.). Philadephia: Wolters Kluwer.
Proehl, J., Heaton, K., Naccarato, M., Crowley, M., Storer, A., Moretz, J., & Li, S. (2011).
Emergency Nursing Resource: Gastric Tube Placement Verification . Journal of
Emergency Nursing, 37(4), 357-362.
Rowat, A. M., Graham, C., & Dennis, M. (2018). Study to determine the likely accuracy of pH
testing to confirm nasogastric tube placement. BMJ Open Gastroenterology, 5(1).
References
Barker, J. (2013). Evidence-Based Practice for Nurses. London: Sage.
Boeykens, K., Steeman, E., & Duysburgh, I. (2014). Reliability of pH measurement and the
auscultatory method to confirm the position of a nasogastric tube. International Journal
of Nursing Studies, 51(11), 1427-1433.
Brun, P.-M., Chenaitia, H., Lablanche, C., Pradel, A.-L., Denile, C., Bessereau, J., & Melaine, R.
(2014). 2-Point Ultrasonography to Confirm Correct Position of the Gastric Tube in
Prehospital Setting. Military Medicine, 179(9), 959–963.
Chan, E., Tan, S., Jabin, K., Lee, L., & Ang, C. (2012). Nasogastric feeding practices: A survey
using clinical scenarios, , 49 (3), pp. International Journal of Nursing Studies, 49(3),
310-319.
Fernandez, R., Chau, J., Thompson, D., Griffiths, R., & Lo, H. (2010). Accuracy of biochemical
markers for predicting nasogastric tube placement in adults—A systematic review of
diagnostic studies. International Journal of Nursing Studies, 47(8), 1037-1046.
Melnyk, B. M., & Fineout-Overholt, E. (2015). Evidence-Based Practice in Nursing &
Healthcare: A Guide to Best Practice (3rd ed.). Philadephia: Wolters Kluwer.
Proehl, J., Heaton, K., Naccarato, M., Crowley, M., Storer, A., Moretz, J., & Li, S. (2011).
Emergency Nursing Resource: Gastric Tube Placement Verification . Journal of
Emergency Nursing, 37(4), 357-362.
Rowat, A. M., Graham, C., & Dennis, M. (2018). Study to determine the likely accuracy of pH
testing to confirm nasogastric tube placement. BMJ Open Gastroenterology, 5(1).
NASOGASTRIC TUBE IN ADULT PATIENTS 9
Taylor, S., Allan, K., Mcwilliam, H., Manara, A., Brown, J., Toher, D., & Rayner, W. (2014).
Confirming nasogastric tube position with electromagnetic tracking versus pH or X-ray
and tube radio-opacity. British Journal of Nursing, 23(7).
Tho, P., Mordiffi, S., Ang, E., & Chen, H. (2011). Implementation of the evidence review on
best practice for confirming the correct placement of nasogastric tube in patients in an
acute care hospital. International Journal of Evidence-Based Healthcare, 12(2), 51-60.
Taylor, S., Allan, K., Mcwilliam, H., Manara, A., Brown, J., Toher, D., & Rayner, W. (2014).
Confirming nasogastric tube position with electromagnetic tracking versus pH or X-ray
and tube radio-opacity. British Journal of Nursing, 23(7).
Tho, P., Mordiffi, S., Ang, E., & Chen, H. (2011). Implementation of the evidence review on
best practice for confirming the correct placement of nasogastric tube in patients in an
acute care hospital. International Journal of Evidence-Based Healthcare, 12(2), 51-60.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



