Biochemistry: Analysis of Blood Transfusion, Grouping and Reactions
VerifiedAdded on 2021/04/21
|25
|3894
|169
Homework Assignment
AI Summary
This biochemistry assignment comprehensively explores blood grouping and transfusion. It begins with an analysis of ABO blood group testing, including agglutination results and the use of enhancement solutions like LISS and PEG. The assignment delves into the causes of false positive and false negative results in ABO blood grouping, such as Rouleaux formation and inadequate antibody ratios. It then discusses the role of antisera in blood grouping, including color coding conventions and preservation methods. The assignment also covers the management of patients with autoimmune hemolytic anemia (AIHA) and the challenges in finding compatible blood, along with the different techniques used for compatibility testing. Furthermore, it details the clinical symptoms of mismatched blood transfusions, such as fever, back pain, and potential complications affecting organs. The assignment also addresses transfusion-related acute lung injury (TRALI) and other transfusion reactions, outlining their detection, investigation, and management. Finally, the assignment analyzes antibody screening and the importance of matching blood groups before transfusion, emphasizing the clinical significance of various antibodies and the potential for haemolytic reactions. References are provided throughout the document.

Running head: BIOCHEMISTRY
Transfusion, Transplantation and Specialist Biochemistry
Name of the Student
Name of the University
Author Note
Transfusion, Transplantation and Specialist Biochemistry
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BIOCHEMISTRY
Part 1: ABO Blood Group Test
Answer 1
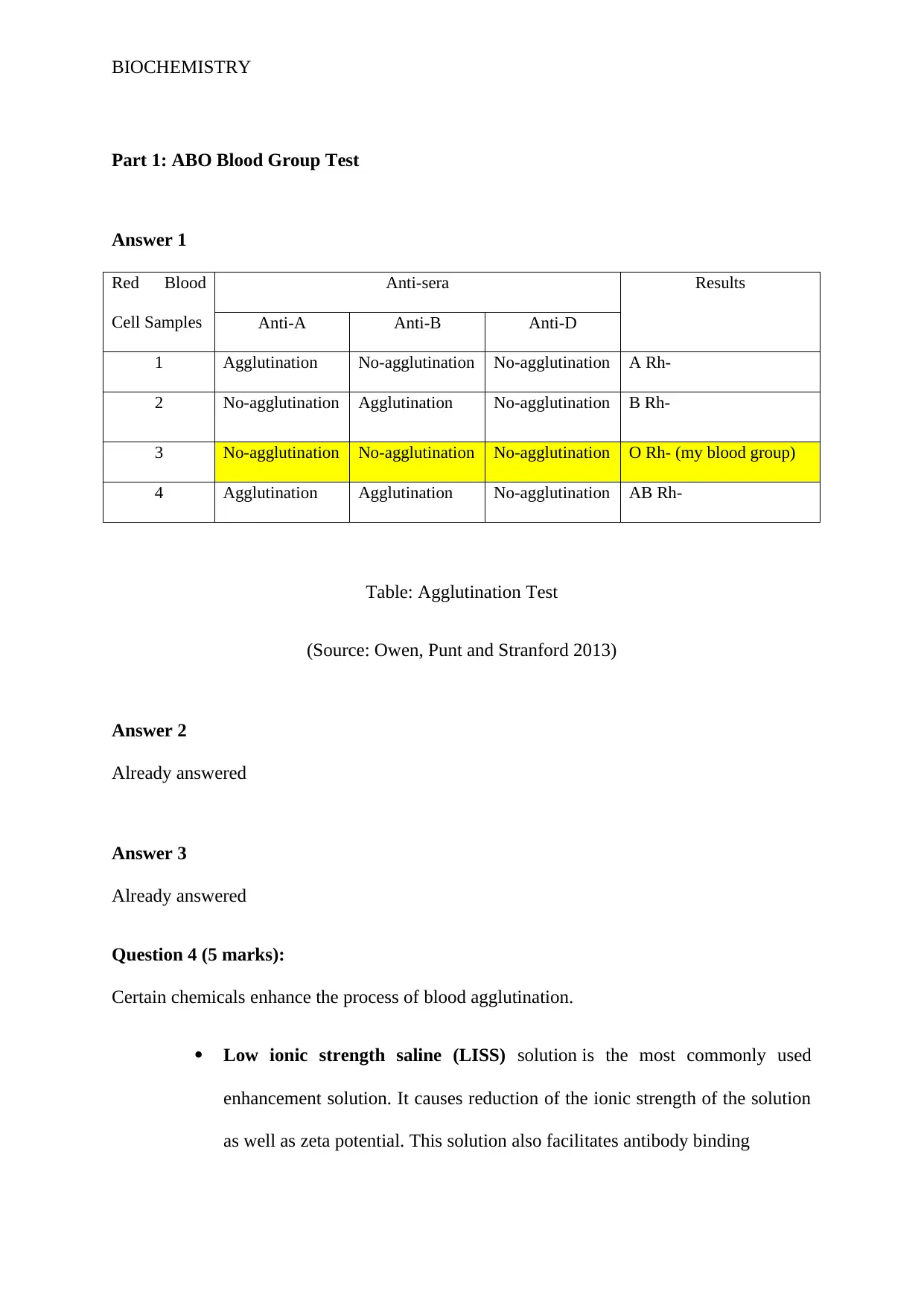
Red Blood
Cell Samples
Anti-sera Results
Anti-A Anti-B Anti-D
1 Agglutination No-agglutination No-agglutination A Rh-
2 No-agglutination Agglutination No-agglutination B Rh-
3 No-agglutination No-agglutination No-agglutination O Rh- (my blood group)
4 Agglutination Agglutination No-agglutination AB Rh-
Table: Agglutination Test
(Source: Owen, Punt and Stranford 2013)
Answer 2
Already answered
Answer 3
Already answered
Question 4 (5 marks):
Certain chemicals enhance the process of blood agglutination.
Low ionic strength saline (LISS) solution is the most commonly used
enhancement solution. It causes reduction of the ionic strength of the solution
as well as zeta potential. This solution also facilitates antibody binding
Part 1: ABO Blood Group Test
Answer 1
Red Blood
Cell Samples
Anti-sera Results
Anti-A Anti-B Anti-D
1 Agglutination No-agglutination No-agglutination A Rh-
2 No-agglutination Agglutination No-agglutination B Rh-
3 No-agglutination No-agglutination No-agglutination O Rh- (my blood group)
4 Agglutination Agglutination No-agglutination AB Rh-
Table: Agglutination Test
(Source: Owen, Punt and Stranford 2013)
Answer 2
Already answered
Answer 3
Already answered
Question 4 (5 marks):
Certain chemicals enhance the process of blood agglutination.
Low ionic strength saline (LISS) solution is the most commonly used
enhancement solution. It causes reduction of the ionic strength of the solution
as well as zeta potential. This solution also facilitates antibody binding
BIOCHEMISTRY
Using Polyethylene glycol (PEG) in the mixture draws the red blood cells
close to each other and antibodies by pushing out the water molecules. It is a
highly sensitive technique with high efficiency that enhances the aggregation
process, but other antibodies can also be concentrated, so it has to be made
sure that the mixture contains necessary antibody-antigens only.
Proteolyting enzymes (like, papain and ficin) can sometimes be
used fordenaturing some RBC antigens and removing negative charge from
RBC membrane surface. This helps in reduction of the zeta potential, drawing
in cells close, facilitating agglutination process. This is most effective for the
detection of Rh factor (Fernandes et al. 2011)
Question 5 (5 marks):
The discrepancies for the forward type ABO agglutination reaction are as follows-
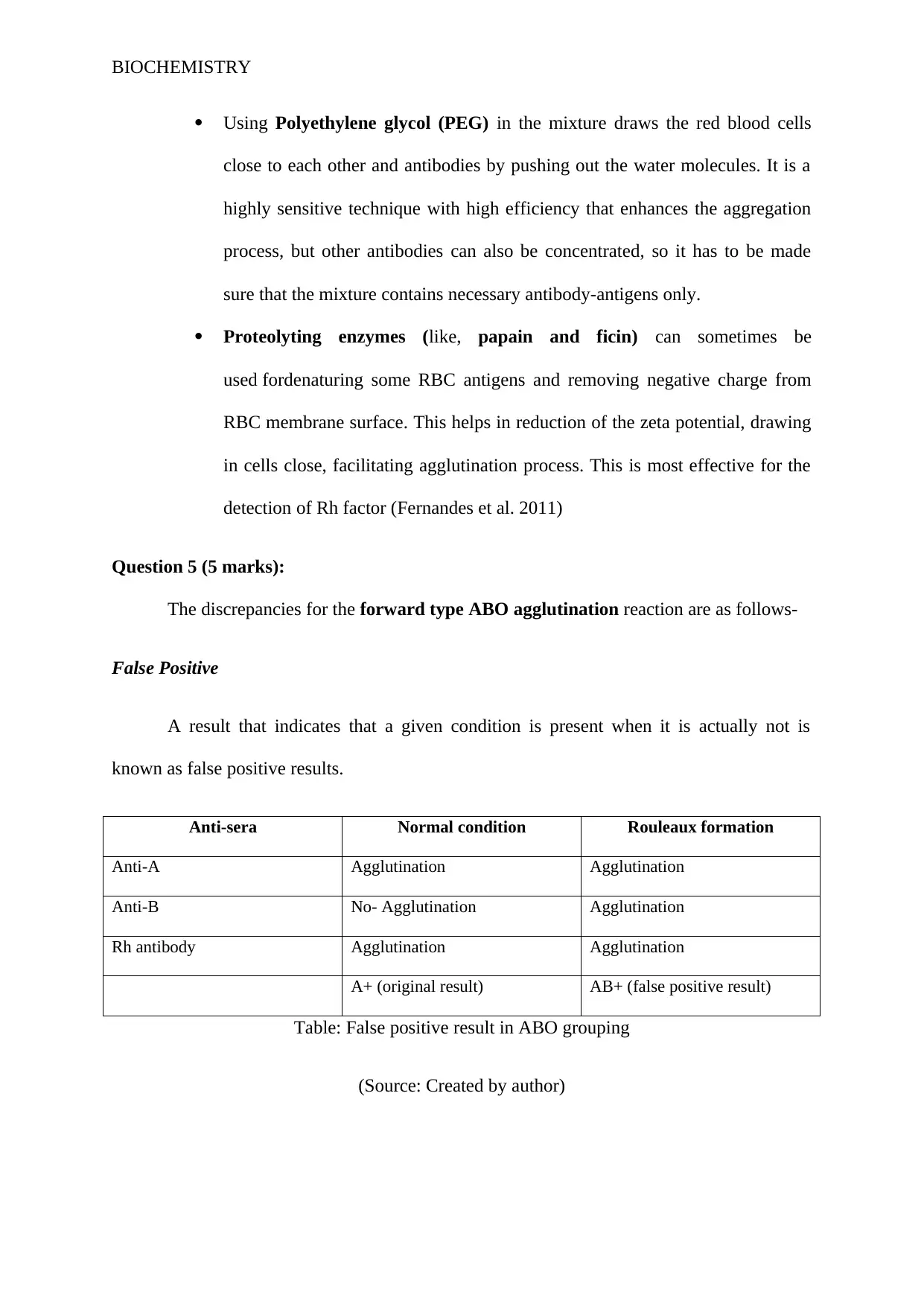
False Positive
A result that indicates that a given condition is present when it is actually not is
known as false positive results.
Anti-sera Normal condition Rouleaux formation
Anti-A Agglutination Agglutination
Anti-B No- Agglutination Agglutination
Rh antibody Agglutination Agglutination
A+ (original result) AB+ (false positive result)
Table: False positive result in ABO grouping
(Source: Created by author)
Using Polyethylene glycol (PEG) in the mixture draws the red blood cells
close to each other and antibodies by pushing out the water molecules. It is a
highly sensitive technique with high efficiency that enhances the aggregation
process, but other antibodies can also be concentrated, so it has to be made
sure that the mixture contains necessary antibody-antigens only.
Proteolyting enzymes (like, papain and ficin) can sometimes be
used fordenaturing some RBC antigens and removing negative charge from
RBC membrane surface. This helps in reduction of the zeta potential, drawing
in cells close, facilitating agglutination process. This is most effective for the
detection of Rh factor (Fernandes et al. 2011)
Question 5 (5 marks):
The discrepancies for the forward type ABO agglutination reaction are as follows-
False Positive
A result that indicates that a given condition is present when it is actually not is
known as false positive results.
Anti-sera Normal condition Rouleaux formation
Anti-A Agglutination Agglutination
Anti-B No- Agglutination Agglutination
Rh antibody Agglutination Agglutination
A+ (original result) AB+ (false positive result)
Table: False positive result in ABO grouping
(Source: Created by author)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BIOCHEMISTRY
The main cause behind the appearance of false positive reaction in ABO blood
grouping is Rouleaux formation, marginal drying, little drops of blood and contamination. In
Rouleaux formation, the RBC’s have stacked together in long chains and this occurs with the
increase in the amount of serum proteins with a special mention to globulins and fibrinogen.
This long chain RBCs tend to sediment rapidly and this precipitated form of RBC appears to
be like agglutination complex and hence giving rise to false positive results. The appearance
of false positive results in Rouleaux formation is common during infectious conditions,
increase in the ration of RBC: plasma volume (hypovolemia or anemia) and other
inflammatory or connective tissue disorders (Kwaan 2010).
False Negative
When the test results indicates that sample do not contain any faulty gene or evidence
of infectious disease however, the actual scenario different, then it is known as false positive
results (Tyagi and Tyagi 2013). The main causes behind the appearance of false negative
results in ABO blood grouping is early evaluation, inadequate antigen:antibody ration and
use of expired test reagents. According toTyagi and Tyagi (2013), the test analysis is
considered false negative when: the subgroups of A or B are weak, the test subject has
recently undergone O blood group transfusion, unmatched bone marrow or stem cell
transplant and compounds and subject’s blood contains substances neutralizing anti-A or
anti-B antibodies.Tyagi and Tyagi (2013), have further opined that the test analysis is
considered a false negative reaction when: the antibodies are absent or low in number,
subject is an infant or elderly, subject is undergoing immune-suppressed condition, presence
of Intravenous fluid in blood and subject has recently undergone wrong blood transfusion.
The main cause behind the appearance of false positive reaction in ABO blood
grouping is Rouleaux formation, marginal drying, little drops of blood and contamination. In
Rouleaux formation, the RBC’s have stacked together in long chains and this occurs with the
increase in the amount of serum proteins with a special mention to globulins and fibrinogen.
This long chain RBCs tend to sediment rapidly and this precipitated form of RBC appears to
be like agglutination complex and hence giving rise to false positive results. The appearance
of false positive results in Rouleaux formation is common during infectious conditions,
increase in the ration of RBC: plasma volume (hypovolemia or anemia) and other
inflammatory or connective tissue disorders (Kwaan 2010).
False Negative
When the test results indicates that sample do not contain any faulty gene or evidence
of infectious disease however, the actual scenario different, then it is known as false positive
results (Tyagi and Tyagi 2013). The main causes behind the appearance of false negative
results in ABO blood grouping is early evaluation, inadequate antigen:antibody ration and
use of expired test reagents. According toTyagi and Tyagi (2013), the test analysis is
considered false negative when: the subgroups of A or B are weak, the test subject has
recently undergone O blood group transfusion, unmatched bone marrow or stem cell
transplant and compounds and subject’s blood contains substances neutralizing anti-A or
anti-B antibodies.Tyagi and Tyagi (2013), have further opined that the test analysis is
considered a false negative reaction when: the antibodies are absent or low in number,
subject is an infant or elderly, subject is undergoing immune-suppressed condition, presence
of Intravenous fluid in blood and subject has recently undergone wrong blood transfusion.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

BIOCHEMISTRY
Question 6
Antisera are employed in ABO blood grouping in order to determine which antigens
are present on the red blood cells. The blood test employing antisera and patient’s RBC is
called front cell group or blood grouping. Government of UK further opined that no
colouring agent should be added to the reagents for blood group serology. The exceptions
are: polyspecific anti-human globulin reagents can be coloured green, anti-A may be
coloured blue and anti-B yellow. UK Government Department of Health (2015) further stated
that the colourant should interfere interfere with the observation of the test results. These
antisera are obtained via the process of plasmapheresis from the donors whose blood is
stimulated with soluable antigens. According to the standard convention set by the
government of UK, the anti-sera are colour coded for proper detection and differentiation
(Plasma Tech 2017).
Anti-sera Colour
Anti-A Blue
Anti-B Yellow
Anti-A,B (from group O people) Colourless (as no dye is added)
Table: Colour coding of the antisera
(Source: Plasma Tech 2017)
Colour coded Anti A and anti B antisera contains 0.1% of sodium azide as
preservative and this helps in the preservation of the anti-sera for at least two years from the
date of manufacture (Plasma Tech 2017).
Question 6
Antisera are employed in ABO blood grouping in order to determine which antigens
are present on the red blood cells. The blood test employing antisera and patient’s RBC is
called front cell group or blood grouping. Government of UK further opined that no
colouring agent should be added to the reagents for blood group serology. The exceptions
are: polyspecific anti-human globulin reagents can be coloured green, anti-A may be
coloured blue and anti-B yellow. UK Government Department of Health (2015) further stated
that the colourant should interfere interfere with the observation of the test results. These
antisera are obtained via the process of plasmapheresis from the donors whose blood is
stimulated with soluable antigens. According to the standard convention set by the
government of UK, the anti-sera are colour coded for proper detection and differentiation
(Plasma Tech 2017).
Anti-sera Colour
Anti-A Blue
Anti-B Yellow
Anti-A,B (from group O people) Colourless (as no dye is added)
Table: Colour coding of the antisera
(Source: Plasma Tech 2017)
Colour coded Anti A and anti B antisera contains 0.1% of sodium azide as
preservative and this helps in the preservation of the anti-sera for at least two years from the
date of manufacture (Plasma Tech 2017).
BIOCHEMISTRY
Question 7 (2marks):
The blood group from the given diagram seems to be O+ as agglutination did not occur after
adding anti-A sera and anti-B sera. Rh test showed positive results of agglutination against
anti-D serum (Owen, Punt and Stranford 2013).
Question 8
Already answere
Question 9 (14 marks):
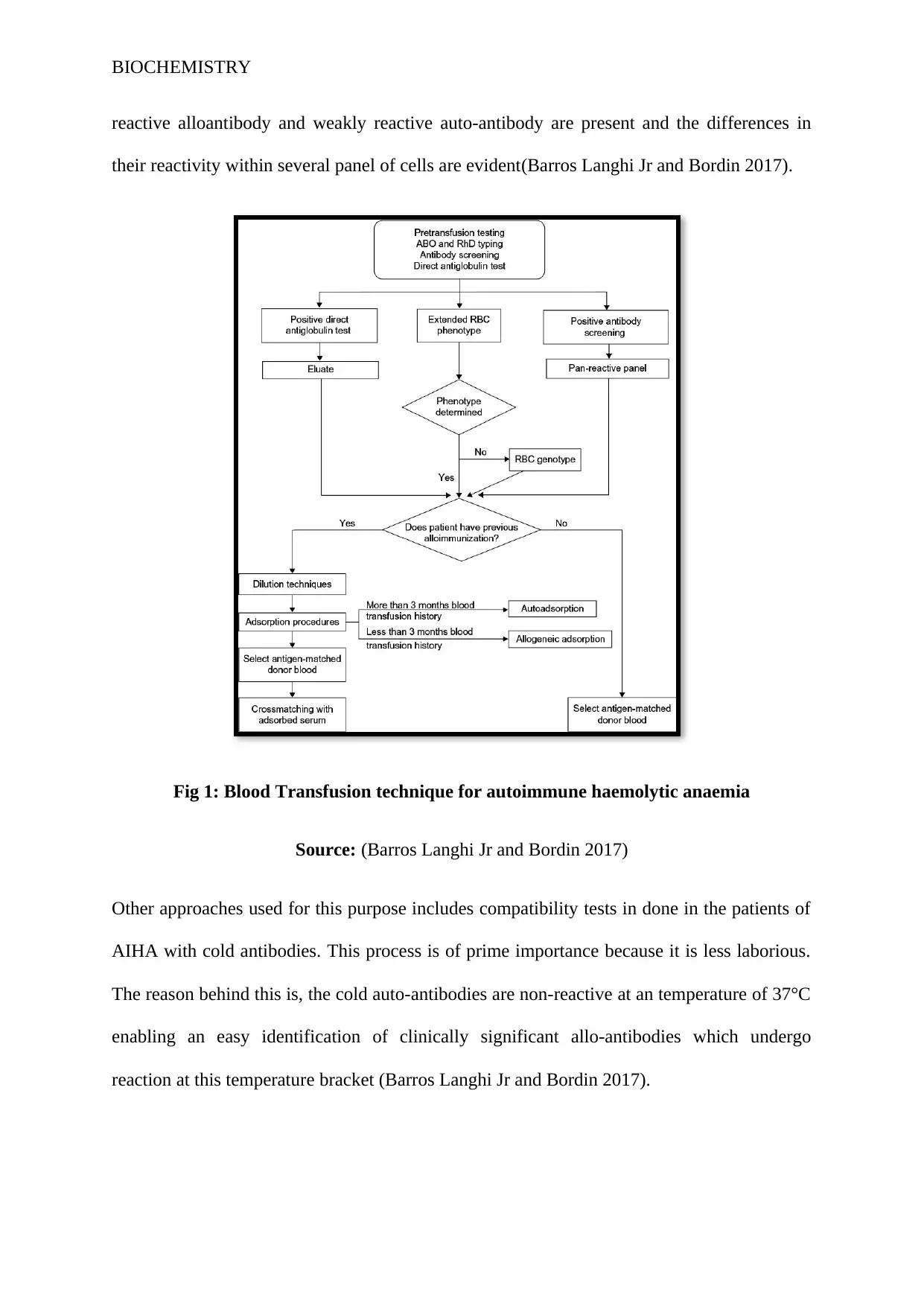
Patients suffering from autoimmune haemolytic anaemia (AIHA) frequently develop
anaemia of significant severity and hence require blood transfusion. However, it is almost
impossible to find compatible blood group because the autoantibody present in the patient's
serum tend to react with nearly all the normal red blood cells. Furthermore, the auto-
antibodies may overshadow the presence of red blood cell alloantibody which is capable of
generating haemolytic transfusion reaction(Petz 2004). Standardmanagement of patient
withAIHA under clinical setting demands special compatibility test in transfusion laboratory.
It is equally important that the doctors understand the mechanism of compatibility tests.
Provided accurate compatibility tests are done, the proper indications for transfusion in
patients with AIHA are not highly different from anaemic patients devoidof AIHA. Proper
communication between doctors and pathologists are crucial to review the importance of
transfusion reaction and subsequent compatibility test methods employed to detect the
optimal unit of RBCs for transfusion(Petz 2004).
Numerous approaches are used to detect the safe and the most compatible RBC units
for blood transfusion in patients with AIHA. Dilution technique is used only during the
emergency because this technique is relatively easy. Dilution is used when the strongly
Question 7 (2marks):
The blood group from the given diagram seems to be O+ as agglutination did not occur after
adding anti-A sera and anti-B sera. Rh test showed positive results of agglutination against
anti-D serum (Owen, Punt and Stranford 2013).
Question 8
Already answere
Question 9 (14 marks):
Patients suffering from autoimmune haemolytic anaemia (AIHA) frequently develop
anaemia of significant severity and hence require blood transfusion. However, it is almost
impossible to find compatible blood group because the autoantibody present in the patient's
serum tend to react with nearly all the normal red blood cells. Furthermore, the auto-
antibodies may overshadow the presence of red blood cell alloantibody which is capable of
generating haemolytic transfusion reaction(Petz 2004). Standardmanagement of patient
withAIHA under clinical setting demands special compatibility test in transfusion laboratory.
It is equally important that the doctors understand the mechanism of compatibility tests.
Provided accurate compatibility tests are done, the proper indications for transfusion in
patients with AIHA are not highly different from anaemic patients devoidof AIHA. Proper
communication between doctors and pathologists are crucial to review the importance of
transfusion reaction and subsequent compatibility test methods employed to detect the
optimal unit of RBCs for transfusion(Petz 2004).
Numerous approaches are used to detect the safe and the most compatible RBC units
for blood transfusion in patients with AIHA. Dilution technique is used only during the
emergency because this technique is relatively easy. Dilution is used when the strongly
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BIOCHEMISTRY
reactive alloantibody and weakly reactive auto-antibody are present and the differences in
their reactivity within several panel of cells are evident(Barros Langhi Jr and Bordin 2017).
Fig 1: Blood Transfusion technique for autoimmune haemolytic anaemia
Source: (Barros Langhi Jr and Bordin 2017)
Other approaches used for this purpose includes compatibility tests in done in the patients of
AIHA with cold antibodies. This process is of prime importance because it is less laborious.
The reason behind this is, the cold auto-antibodies are non-reactive at an temperature of 37°C
enabling an easy identification of clinically significant allo-antibodies which undergo
reaction at this temperature bracket (Barros Langhi Jr and Bordin 2017).
reactive alloantibody and weakly reactive auto-antibody are present and the differences in
their reactivity within several panel of cells are evident(Barros Langhi Jr and Bordin 2017).
Fig 1: Blood Transfusion technique for autoimmune haemolytic anaemia
Source: (Barros Langhi Jr and Bordin 2017)
Other approaches used for this purpose includes compatibility tests in done in the patients of
AIHA with cold antibodies. This process is of prime importance because it is less laborious.
The reason behind this is, the cold auto-antibodies are non-reactive at an temperature of 37°C
enabling an easy identification of clinically significant allo-antibodies which undergo
reaction at this temperature bracket (Barros Langhi Jr and Bordin 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BIOCHEMISTRY
References
Barros, M., Langhi Jr, D. and Bordin, J. (2017). Autoimmune hemolyticanemia: transfusion
challenges and solutions. International Journal of Clinical Transfusion Medicine, Volume 5,
pp.9-18.
Fernandes, H.P., Cesar, C.L. and Barjas-Castro, M.D.L., 2011. Electrical properties of the red
blood cell membrane and immunohematological investigation. Revistabrasileira de
hematologia e hemoterapia, 33(4), pp.297-301.
Kwaan, H.C., 2010. Role of plasma proteins in whole blood viscosity: a brief clinical
review. Clinical hemorheology and microcirculation, 44(3), pp.167-176.
Owen, J.A., Punt, J. and Stranford, S.A., 2013. Kuby immunology (pp. 427-444). New York:
WH Freeman.
Petz, L.D., 2004. A physician's guide to transfusion in autoimmune haemolytic
anaemia. British journal of haematology, 124(6), pp.712-716.
Plasma Tech., 2017. Blood Grouping Antisera. Accessed on: 22March. 2018. Retrieved from:
http://plasmatec.co.uk/blood-grouping-antisera/
Torres, R., Kenney, B. and Tormey, C. (2012). Diagnosis, Treatment, and Reporting of
Adverse Effects of Transfusion. Laboratory Medicine, 43(5), pp.217-231.
Tyagi, S. and Tyagi, A., 2013. Possible correlation of transfusion transmitted diseases with
Rh type and ABO blood group system. Journal of clinical and diagnostic research:
JCDR, 7(9), p.1930.
References
Barros, M., Langhi Jr, D. and Bordin, J. (2017). Autoimmune hemolyticanemia: transfusion
challenges and solutions. International Journal of Clinical Transfusion Medicine, Volume 5,
pp.9-18.
Fernandes, H.P., Cesar, C.L. and Barjas-Castro, M.D.L., 2011. Electrical properties of the red
blood cell membrane and immunohematological investigation. Revistabrasileira de
hematologia e hemoterapia, 33(4), pp.297-301.
Kwaan, H.C., 2010. Role of plasma proteins in whole blood viscosity: a brief clinical
review. Clinical hemorheology and microcirculation, 44(3), pp.167-176.
Owen, J.A., Punt, J. and Stranford, S.A., 2013. Kuby immunology (pp. 427-444). New York:
WH Freeman.
Petz, L.D., 2004. A physician's guide to transfusion in autoimmune haemolytic
anaemia. British journal of haematology, 124(6), pp.712-716.
Plasma Tech., 2017. Blood Grouping Antisera. Accessed on: 22March. 2018. Retrieved from:
http://plasmatec.co.uk/blood-grouping-antisera/
Torres, R., Kenney, B. and Tormey, C. (2012). Diagnosis, Treatment, and Reporting of
Adverse Effects of Transfusion. Laboratory Medicine, 43(5), pp.217-231.
Tyagi, S. and Tyagi, A., 2013. Possible correlation of transfusion transmitted diseases with
Rh type and ABO blood group system. Journal of clinical and diagnostic research:
JCDR, 7(9), p.1930.
BIOCHEMISTRY
Column agglutination technology:
Question 10:
Results not provided for interpretation.
Question 11 (15 marks):
Blood transfusions are generally provided to patients who have encountered severe blood loss
which cannot be compensated naturally. It is important to match the blood group before
administering a transfusion procedure; otherwise the patient might suffer a biochemical
reaction against the transfusion. In extreme cases, mismatched blood transfusion causes harm
to lungs, kidney and liver.
The clinical symptoms that can arise from mismatched blood transfusion are as follows-
back ache
dark colouration of urine
sudden tremors in the body
losing consciousness
light-headedness
feverish symptoms
flank ache
experiencing skin flush
breathlessness
itchy sensation
The cause of mismatched blood transfusion reaction is due to the fact that the recipient’s
immune system recognizes the donor’s blood as foreign antigen and starts to produces
antibodies against them. This kind of repercussion is termed as haemolytic anaemia.
Another possible causation of transfusion reaction is development of an allergic cascade
in the patient’s blood which can be prevented by administration of anti-histamines.
Column agglutination technology:
Question 10:
Results not provided for interpretation.
Question 11 (15 marks):
Blood transfusions are generally provided to patients who have encountered severe blood loss
which cannot be compensated naturally. It is important to match the blood group before
administering a transfusion procedure; otherwise the patient might suffer a biochemical
reaction against the transfusion. In extreme cases, mismatched blood transfusion causes harm
to lungs, kidney and liver.
The clinical symptoms that can arise from mismatched blood transfusion are as follows-
back ache
dark colouration of urine
sudden tremors in the body
losing consciousness
light-headedness
feverish symptoms
flank ache
experiencing skin flush
breathlessness
itchy sensation
The cause of mismatched blood transfusion reaction is due to the fact that the recipient’s
immune system recognizes the donor’s blood as foreign antigen and starts to produces
antibodies against them. This kind of repercussion is termed as haemolytic anaemia.
Another possible causation of transfusion reaction is development of an allergic cascade
in the patient’s blood which can be prevented by administration of anti-histamines.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BIOCHEMISTRY
Patients are also sometimes observed to undergo transfusion reaction if the blood
provided was previously contaminated with bacteria causing the patient to undergo septic
shock.
Transmission associated cardiac overload (TACO) is another form of blood
transfusion reaction occurring when the patient is provided excess amounts of transfused
blood. This causes the circulatory system to become overloaded and pumping of blood
becomes difficult (Magee et al. 2012).
(Needs citation)
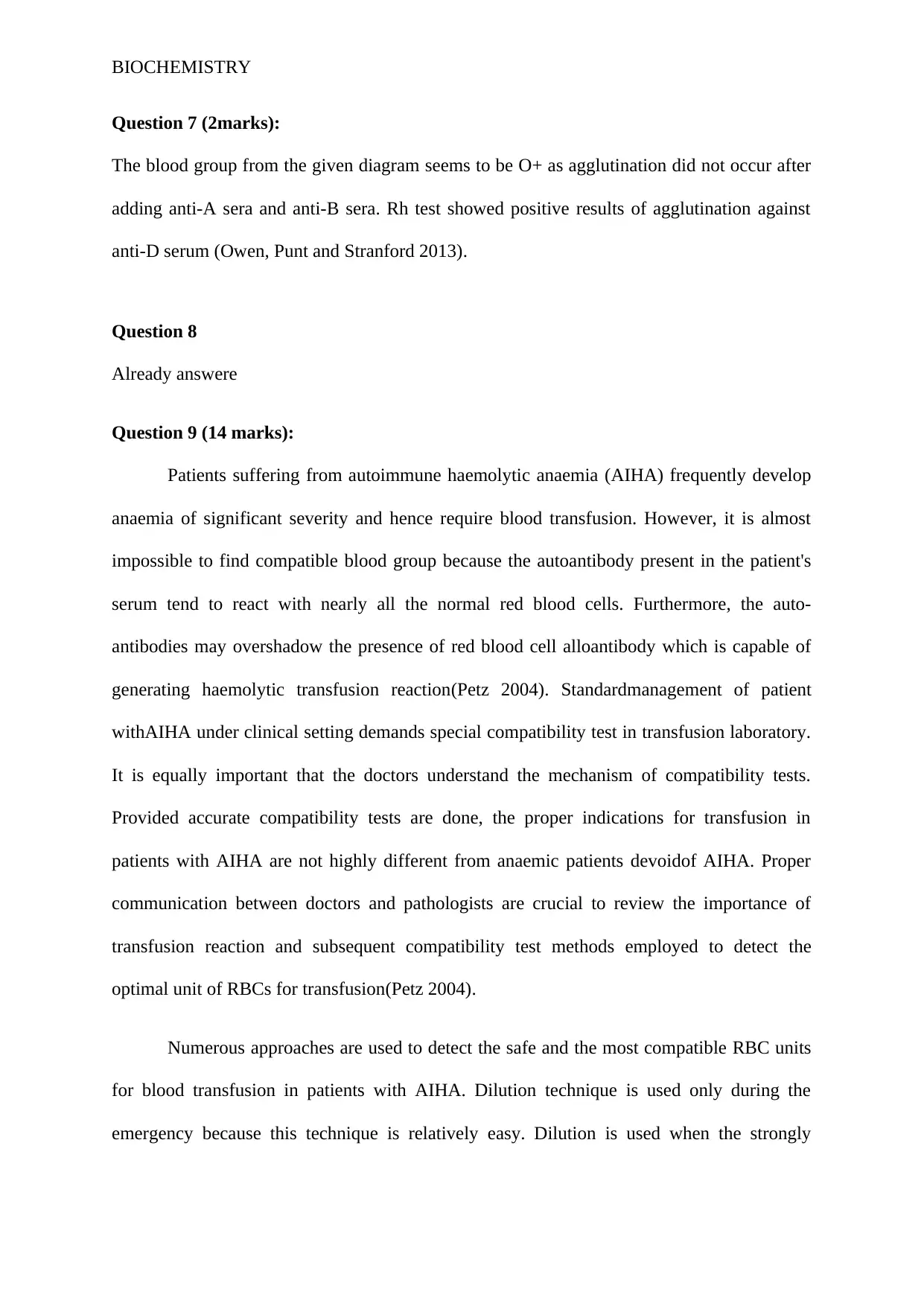
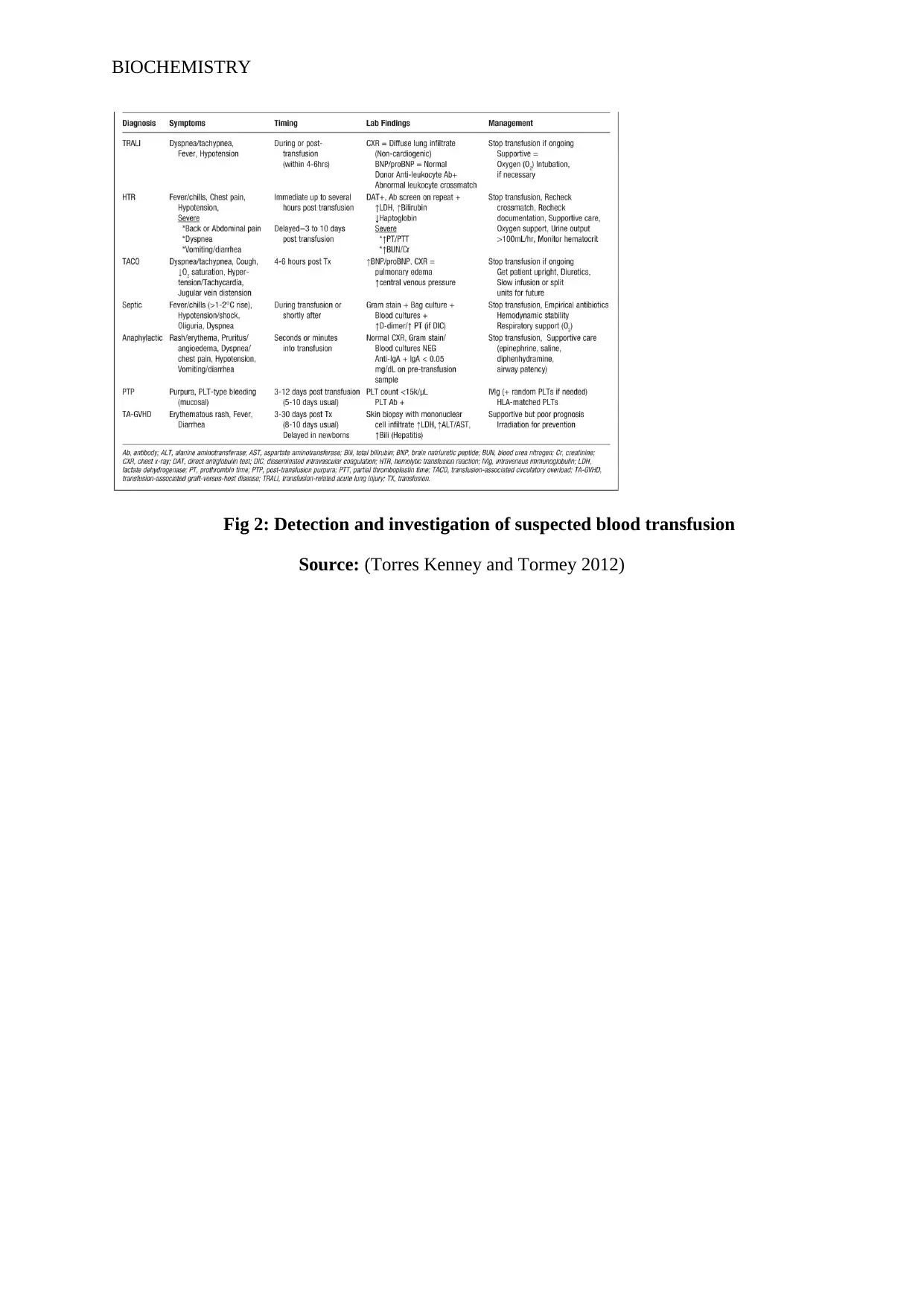
Question 12 (15marks):
Transfusion related acute injury (TRALI) can be seen after transfusion, by checking chest x-
ray (CXR), and vitals. Transfusion needs to be stopped and supportive oxygen needs to be
commenced. In haemolytic transfusion reaction; fever, chills and hypotension occurs
immediately after wrong transfusion. Blood cross match needs to be checked and oxygen
support is commenced along with urine output checking. If patient is seen to go into septic
shock, then suitable histamines and vasodilators are to be administered to maintain
hemodynamic stability as well as respiratory support needs to be provided. In case of
anaphylactic shock, epinephrine, saline and diphenhydramine are provided along with airway
supply. If transmission associated graft versus host disease (TA-GVD) is noticed, supportive
prognosis and mild irradiation may be commenced. The table below provides a brief
description of the haemolytic transfusion reactions Fig 2.
Patients are also sometimes observed to undergo transfusion reaction if the blood
provided was previously contaminated with bacteria causing the patient to undergo septic
shock.
Transmission associated cardiac overload (TACO) is another form of blood
transfusion reaction occurring when the patient is provided excess amounts of transfused
blood. This causes the circulatory system to become overloaded and pumping of blood
becomes difficult (Magee et al. 2012).
(Needs citation)
Question 12 (15marks):
Transfusion related acute injury (TRALI) can be seen after transfusion, by checking chest x-
ray (CXR), and vitals. Transfusion needs to be stopped and supportive oxygen needs to be
commenced. In haemolytic transfusion reaction; fever, chills and hypotension occurs
immediately after wrong transfusion. Blood cross match needs to be checked and oxygen
support is commenced along with urine output checking. If patient is seen to go into septic
shock, then suitable histamines and vasodilators are to be administered to maintain
hemodynamic stability as well as respiratory support needs to be provided. In case of
anaphylactic shock, epinephrine, saline and diphenhydramine are provided along with airway
supply. If transmission associated graft versus host disease (TA-GVD) is noticed, supportive
prognosis and mild irradiation may be commenced. The table below provides a brief
description of the haemolytic transfusion reactions Fig 2.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BIOCHEMISTRY
Fig 2: Detection and investigation of suspected blood transfusion
Source: (Torres Kenney and Tormey 2012)
Fig 2: Detection and investigation of suspected blood transfusion
Source: (Torres Kenney and Tormey 2012)
BIOCHEMISTRY
References:
Magee, B.A., Martin, J., Cole, M.P., Morris, K.G. and Courtney, A.E., 2012. Effects of HLA-
matched blood transfusion for patients awaiting renal
transplantation. Transplantation, 94(11), pp.1111-1116.
Torres, R., Kenney, B. and Tormey, C. (2012). Diagnosis, Treatment, and Reporting of
Adverse Effects of Transfusion. Laboratory Medicine, 43(5), pp.217-231.
References:
Magee, B.A., Martin, J., Cole, M.P., Morris, K.G. and Courtney, A.E., 2012. Effects of HLA-
matched blood transfusion for patients awaiting renal
transplantation. Transplantation, 94(11), pp.1111-1116.
Torres, R., Kenney, B. and Tormey, C. (2012). Diagnosis, Treatment, and Reporting of
Adverse Effects of Transfusion. Laboratory Medicine, 43(5), pp.217-231.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 25
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





