Biology 1 CBB064: Reproductive System Assignment Tasks 1-4
VerifiedAdded on 2023/01/23
|17
|4097
|72
Homework Assignment
AI Summary
This biology assignment delves into the complexities of the human reproductive system. It begins with a comparative analysis of the male and female reproductive systems, detailing the structure and function of each organ. The assignment then explores the roles of key hormones like oestrogen, progesterone, and testosterone, and how they influence sexual development, the menstrual cycle, and pregnancy. It provides a comprehensive overview of the menstrual cycle, including the changes in the uterine lining and the hormonal control involved. Furthermore, the assignment explains the process of in vitro fertilization (IVF) and its application in cases of infertility, including fallopian tube blockage and endometriosis. It also covers the key stages of embryonic development from conception to week eight, including a detailed look at the placenta's function and the importance of avoiding alcohol during pregnancy. Finally, the assignment describes the hormonal control of both lactation and birth, comparing the roles of the hormones involved in each process.
Biology
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 1:
a)
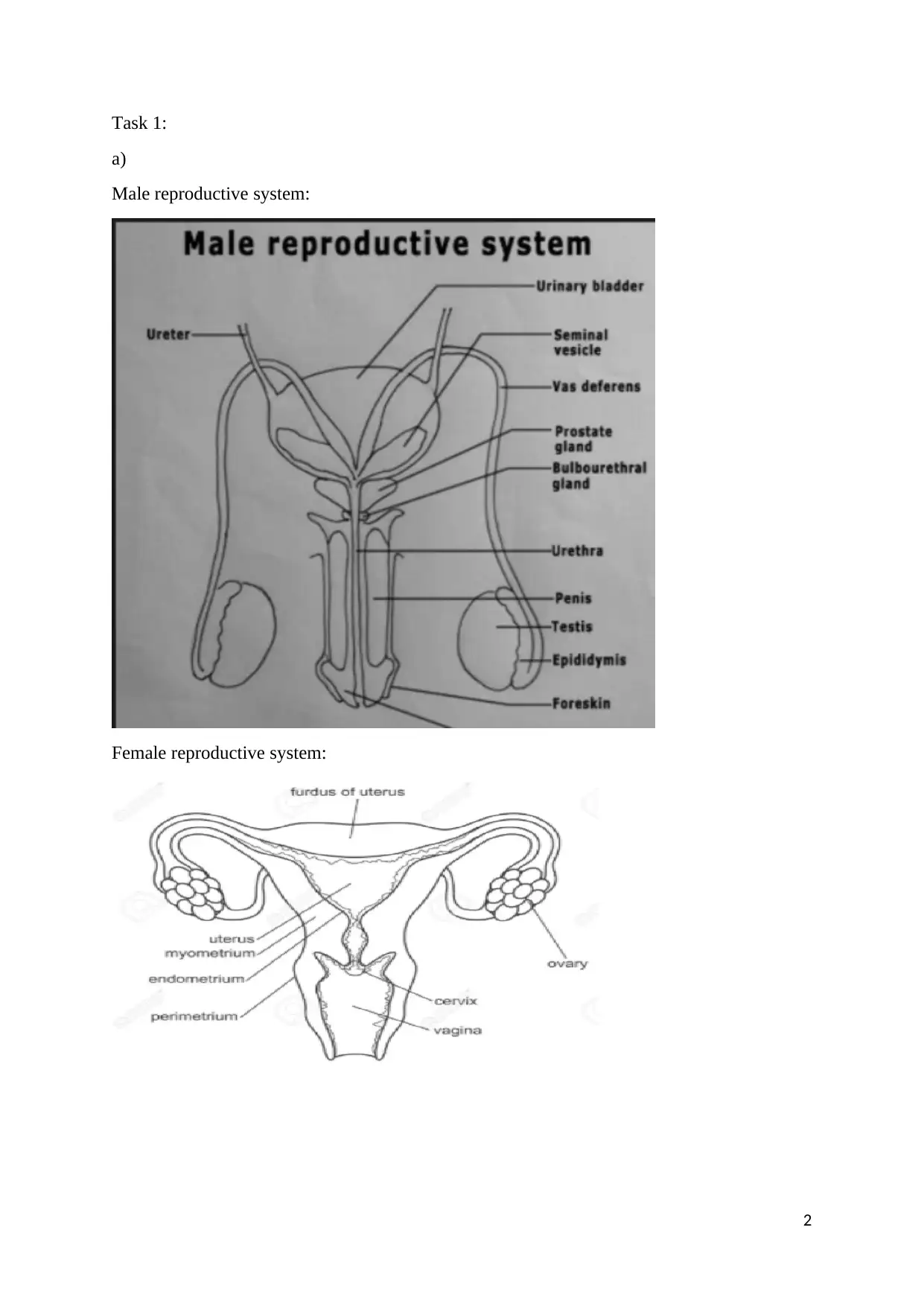
Male reproductive system:
Female reproductive system:
2
a)
Male reproductive system:
Female reproductive system:
2
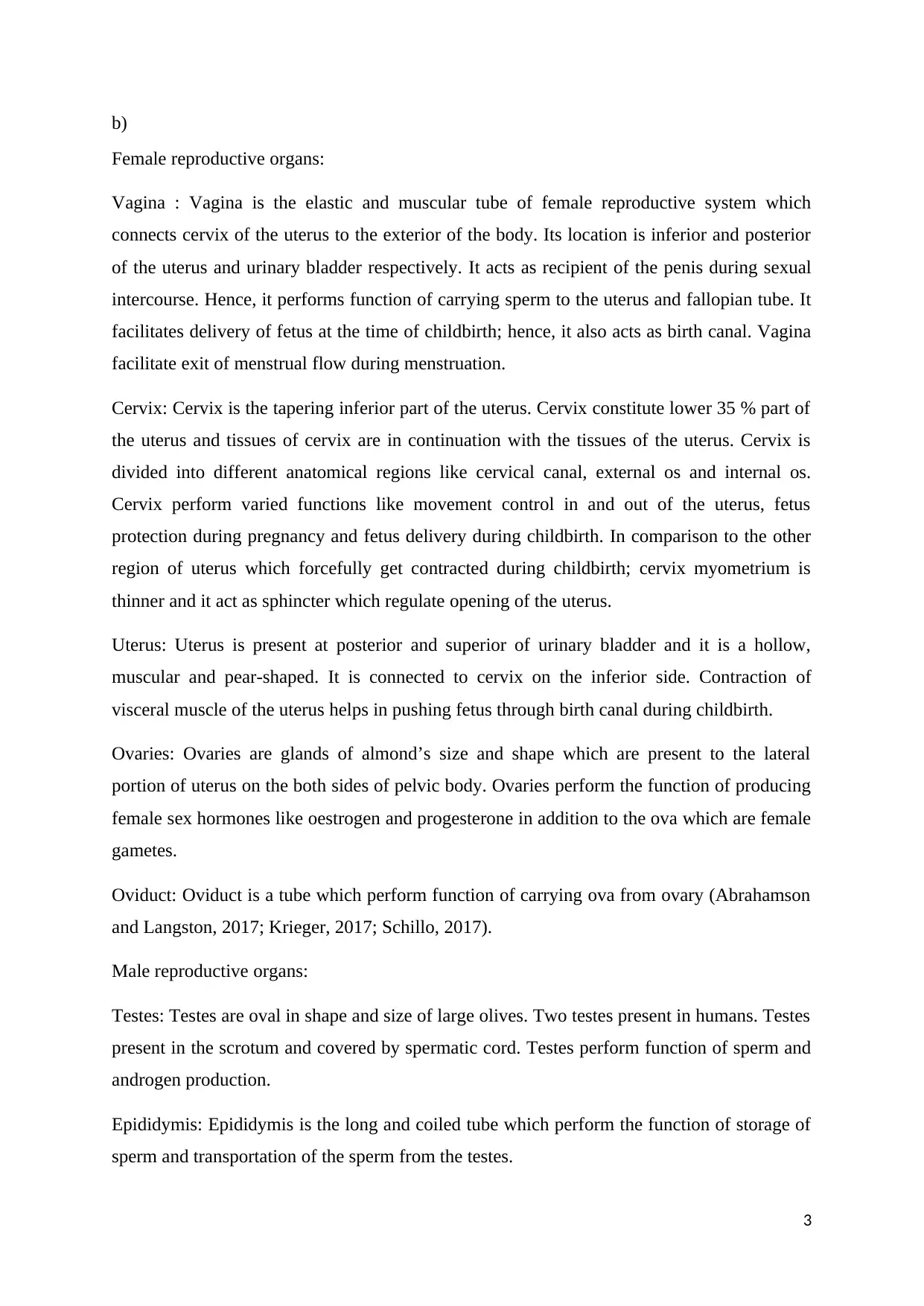
b)
Female reproductive organs:
Vagina : Vagina is the elastic and muscular tube of female reproductive system which
connects cervix of the uterus to the exterior of the body. Its location is inferior and posterior
of the uterus and urinary bladder respectively. It acts as recipient of the penis during sexual
intercourse. Hence, it performs function of carrying sperm to the uterus and fallopian tube. It
facilitates delivery of fetus at the time of childbirth; hence, it also acts as birth canal. Vagina
facilitate exit of menstrual flow during menstruation.
Cervix: Cervix is the tapering inferior part of the uterus. Cervix constitute lower 35 % part of
the uterus and tissues of cervix are in continuation with the tissues of the uterus. Cervix is
divided into different anatomical regions like cervical canal, external os and internal os.
Cervix perform varied functions like movement control in and out of the uterus, fetus
protection during pregnancy and fetus delivery during childbirth. In comparison to the other
region of uterus which forcefully get contracted during childbirth; cervix myometrium is
thinner and it act as sphincter which regulate opening of the uterus.
Uterus: Uterus is present at posterior and superior of urinary bladder and it is a hollow,
muscular and pear-shaped. It is connected to cervix on the inferior side. Contraction of
visceral muscle of the uterus helps in pushing fetus through birth canal during childbirth.
Ovaries: Ovaries are glands of almond’s size and shape which are present to the lateral
portion of uterus on the both sides of pelvic body. Ovaries perform the function of producing
female sex hormones like oestrogen and progesterone in addition to the ova which are female
gametes.
Oviduct: Oviduct is a tube which perform function of carrying ova from ovary (Abrahamson
and Langston, 2017; Krieger, 2017; Schillo, 2017).
Male reproductive organs:
Testes: Testes are oval in shape and size of large olives. Two testes present in humans. Testes
present in the scrotum and covered by spermatic cord. Testes perform function of sperm and
androgen production.
Epididymis: Epididymis is the long and coiled tube which perform the function of storage of
sperm and transportation of the sperm from the testes.
3
Female reproductive organs:
Vagina : Vagina is the elastic and muscular tube of female reproductive system which
connects cervix of the uterus to the exterior of the body. Its location is inferior and posterior
of the uterus and urinary bladder respectively. It acts as recipient of the penis during sexual
intercourse. Hence, it performs function of carrying sperm to the uterus and fallopian tube. It
facilitates delivery of fetus at the time of childbirth; hence, it also acts as birth canal. Vagina
facilitate exit of menstrual flow during menstruation.
Cervix: Cervix is the tapering inferior part of the uterus. Cervix constitute lower 35 % part of
the uterus and tissues of cervix are in continuation with the tissues of the uterus. Cervix is
divided into different anatomical regions like cervical canal, external os and internal os.
Cervix perform varied functions like movement control in and out of the uterus, fetus
protection during pregnancy and fetus delivery during childbirth. In comparison to the other
region of uterus which forcefully get contracted during childbirth; cervix myometrium is
thinner and it act as sphincter which regulate opening of the uterus.
Uterus: Uterus is present at posterior and superior of urinary bladder and it is a hollow,
muscular and pear-shaped. It is connected to cervix on the inferior side. Contraction of
visceral muscle of the uterus helps in pushing fetus through birth canal during childbirth.
Ovaries: Ovaries are glands of almond’s size and shape which are present to the lateral
portion of uterus on the both sides of pelvic body. Ovaries perform the function of producing
female sex hormones like oestrogen and progesterone in addition to the ova which are female
gametes.
Oviduct: Oviduct is a tube which perform function of carrying ova from ovary (Abrahamson
and Langston, 2017; Krieger, 2017; Schillo, 2017).
Male reproductive organs:
Testes: Testes are oval in shape and size of large olives. Two testes present in humans. Testes
present in the scrotum and covered by spermatic cord. Testes perform function of sperm and
androgen production.
Epididymis: Epididymis is the long and coiled tube which perform the function of storage of
sperm and transportation of the sperm from the testes.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Vas deferens:
Vas deferens is the long and muscular tube which extends from the epididymis to the pelvic
cavity. Vas deferens perform the function of transportation of mature sperm to the urethra
which helps in ejaculation of sperm.
Ejaculatory ducts: Ejaculatory ducts are the paired structure which formed through union of
vas deferens and duct of the seminal vesicle. Ejaculatory duct plays role in the emission stage
of the ejaculation of semen in which contractions of different organs like prostate gland, the
seminal vesicles, the bulbourethral gland and the vas deferens impulses secretions in to the
prostatic urethra.
Urethra: Urethra is a narrow and fibromuscular tube which transports semen from the
ejaculatory duct to outside the body.
Penis: Penis reaches its full-size during puberty which is made up of different parts like glans,
Corpus cavernosum and Corpus spongiosum. Penis perform the function of sexual
intercourse and ejaculation of semen.
Accessory glands: Male reproductive system contain accessory glands like seminal vesicles,
prostate gland, and the bulbourethral glands. These accessory glands contain secretory fluids
which enter urethra (Abrahamson and Langston, 2017; Krieger, 2017; Schillo, 2017).
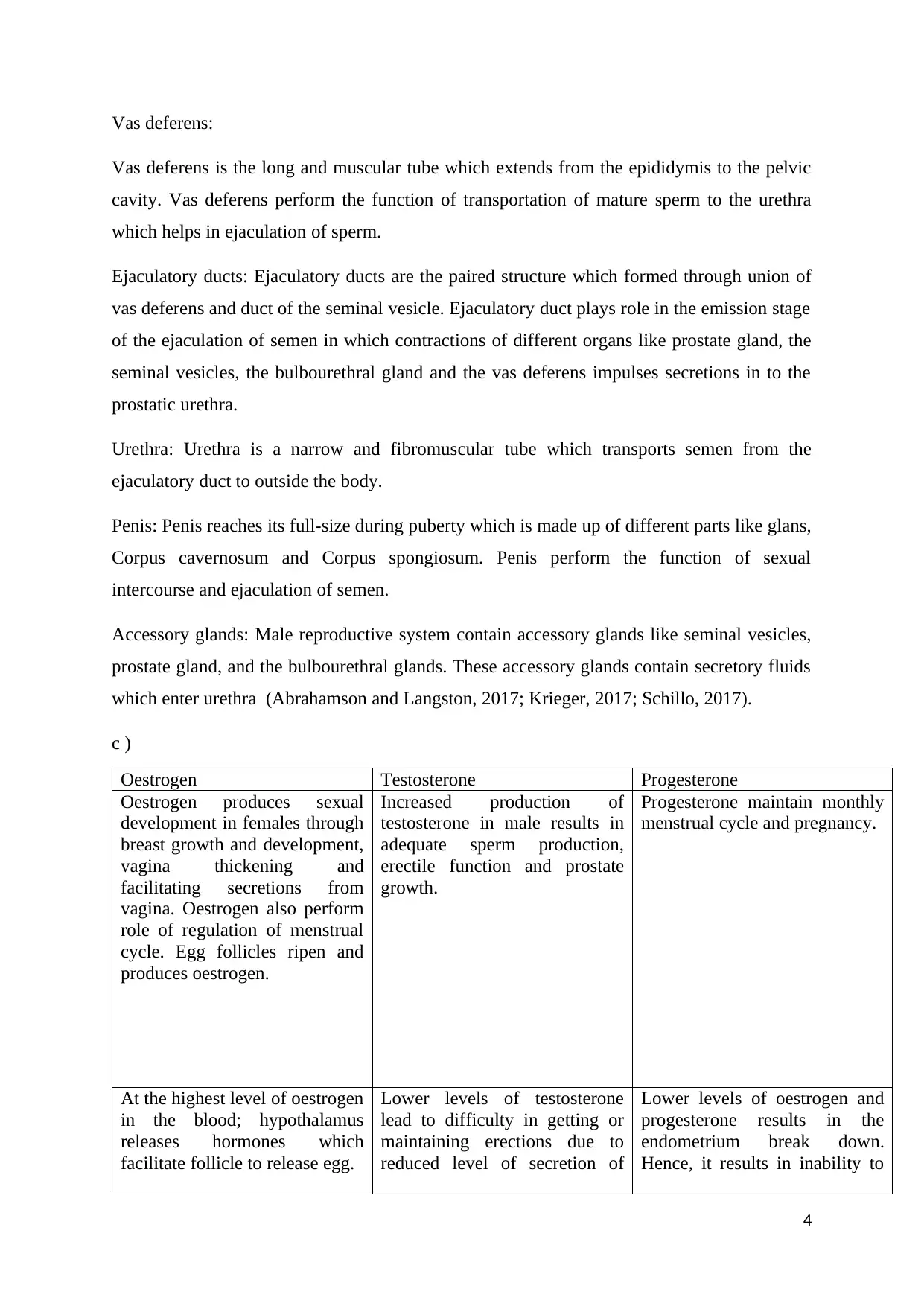
c )
Oestrogen Testosterone Progesterone
Oestrogen produces sexual
development in females through
breast growth and development,
vagina thickening and
facilitating secretions from
vagina. Oestrogen also perform
role of regulation of menstrual
cycle. Egg follicles ripen and
produces oestrogen.
Increased production of
testosterone in male results in
adequate sperm production,
erectile function and prostate
growth.
Progesterone maintain monthly
menstrual cycle and pregnancy.
At the highest level of oestrogen
in the blood; hypothalamus
releases hormones which
facilitate follicle to release egg.
Lower levels of testosterone
lead to difficulty in getting or
maintaining erections due to
reduced level of secretion of
Lower levels of oestrogen and
progesterone results in the
endometrium break down.
Hence, it results in inability to
4
Vas deferens is the long and muscular tube which extends from the epididymis to the pelvic
cavity. Vas deferens perform the function of transportation of mature sperm to the urethra
which helps in ejaculation of sperm.
Ejaculatory ducts: Ejaculatory ducts are the paired structure which formed through union of
vas deferens and duct of the seminal vesicle. Ejaculatory duct plays role in the emission stage
of the ejaculation of semen in which contractions of different organs like prostate gland, the
seminal vesicles, the bulbourethral gland and the vas deferens impulses secretions in to the
prostatic urethra.
Urethra: Urethra is a narrow and fibromuscular tube which transports semen from the
ejaculatory duct to outside the body.
Penis: Penis reaches its full-size during puberty which is made up of different parts like glans,
Corpus cavernosum and Corpus spongiosum. Penis perform the function of sexual
intercourse and ejaculation of semen.
Accessory glands: Male reproductive system contain accessory glands like seminal vesicles,
prostate gland, and the bulbourethral glands. These accessory glands contain secretory fluids
which enter urethra (Abrahamson and Langston, 2017; Krieger, 2017; Schillo, 2017).
c )
Oestrogen Testosterone Progesterone
Oestrogen produces sexual
development in females through
breast growth and development,
vagina thickening and
facilitating secretions from
vagina. Oestrogen also perform
role of regulation of menstrual
cycle. Egg follicles ripen and
produces oestrogen.
Increased production of
testosterone in male results in
adequate sperm production,
erectile function and prostate
growth.
Progesterone maintain monthly
menstrual cycle and pregnancy.
At the highest level of oestrogen
in the blood; hypothalamus
releases hormones which
facilitate follicle to release egg.
Lower levels of testosterone
lead to difficulty in getting or
maintaining erections due to
reduced level of secretion of
Lower levels of oestrogen and
progesterone results in the
endometrium break down.
Hence, it results in inability to
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
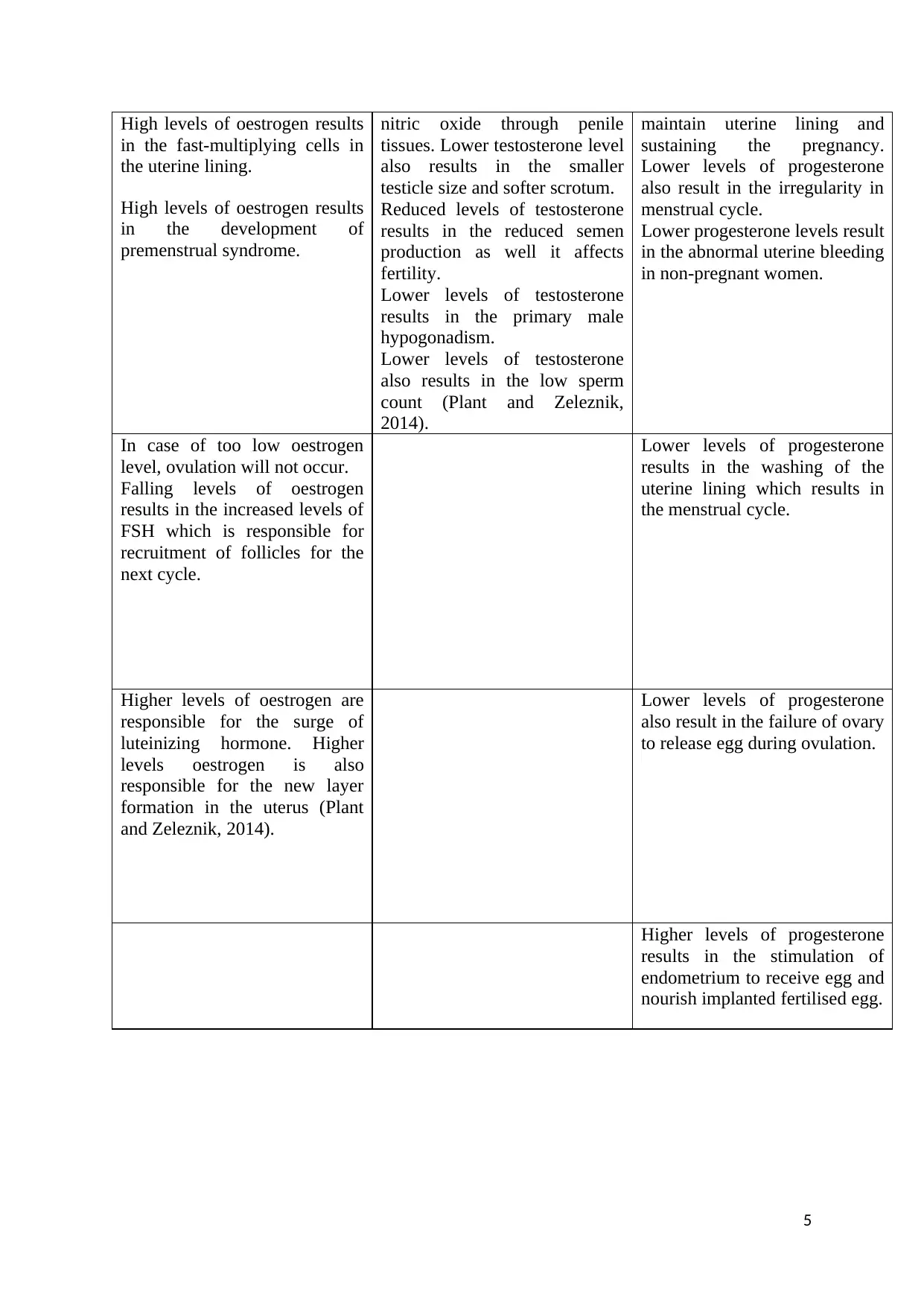
High levels of oestrogen results
in the fast-multiplying cells in
the uterine lining.
High levels of oestrogen results
in the development of
premenstrual syndrome.
nitric oxide through penile
tissues. Lower testosterone level
also results in the smaller
testicle size and softer scrotum.
Reduced levels of testosterone
results in the reduced semen
production as well it affects
fertility.
Lower levels of testosterone
results in the primary male
hypogonadism.
Lower levels of testosterone
also results in the low sperm
count (Plant and Zeleznik,
2014).
maintain uterine lining and
sustaining the pregnancy.
Lower levels of progesterone
also result in the irregularity in
menstrual cycle.
Lower progesterone levels result
in the abnormal uterine bleeding
in non-pregnant women.
In case of too low oestrogen
level, ovulation will not occur.
Falling levels of oestrogen
results in the increased levels of
FSH which is responsible for
recruitment of follicles for the
next cycle.
Lower levels of progesterone
results in the washing of the
uterine lining which results in
the menstrual cycle.
Higher levels of oestrogen are
responsible for the surge of
luteinizing hormone. Higher
levels oestrogen is also
responsible for the new layer
formation in the uterus (Plant
and Zeleznik, 2014).
Lower levels of progesterone
also result in the failure of ovary
to release egg during ovulation.
Higher levels of progesterone
results in the stimulation of
endometrium to receive egg and
nourish implanted fertilised egg.
5
in the fast-multiplying cells in
the uterine lining.
High levels of oestrogen results
in the development of
premenstrual syndrome.
nitric oxide through penile
tissues. Lower testosterone level
also results in the smaller
testicle size and softer scrotum.
Reduced levels of testosterone
results in the reduced semen
production as well it affects
fertility.
Lower levels of testosterone
results in the primary male
hypogonadism.
Lower levels of testosterone
also results in the low sperm
count (Plant and Zeleznik,
2014).
maintain uterine lining and
sustaining the pregnancy.
Lower levels of progesterone
also result in the irregularity in
menstrual cycle.
Lower progesterone levels result
in the abnormal uterine bleeding
in non-pregnant women.
In case of too low oestrogen
level, ovulation will not occur.
Falling levels of oestrogen
results in the increased levels of
FSH which is responsible for
recruitment of follicles for the
next cycle.
Lower levels of progesterone
results in the washing of the
uterine lining which results in
the menstrual cycle.
Higher levels of oestrogen are
responsible for the surge of
luteinizing hormone. Higher
levels oestrogen is also
responsible for the new layer
formation in the uterus (Plant
and Zeleznik, 2014).
Lower levels of progesterone
also result in the failure of ovary
to release egg during ovulation.
Higher levels of progesterone
results in the stimulation of
endometrium to receive egg and
nourish implanted fertilised egg.
5
Higher levels of progesterone
counteract effects of oestrogen
due to reduction in the levels of
oestrogen.
Higher levels of progesterone
also result in the vaginal dryness
and breast tenderness.
Higher levels of progesterone
also result in the ovarian cysts
(White, Harrison, and
Mehlmann, 2018).
6
counteract effects of oestrogen
due to reduction in the levels of
oestrogen.
Higher levels of progesterone
also result in the vaginal dryness
and breast tenderness.
Higher levels of progesterone
also result in the ovarian cysts
(White, Harrison, and
Mehlmann, 2018).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Task 2:
Several changes occur in uterine lining (endometrium) during menstrual cycle. Uterus
comprises of innermost glandular layer which is known as endometrium. During menstrual
cycle, endometrium gets thickened and it gets blood vessel rich tissue lining. Thickening of
the uterus is the appropriate milieu for the implantation of the blastocyst after its entry into
the uterus. During menstrual cycle, body initiate ovulation. There is gradual rise in the
oestrogen, which indicate initiation of follicular or proliferation phase of the menstrual cycle.
Consequently, there is slowing of the blood discharge which results in stopping response to
hormone and consequently there is thickening and proliferation of uterus. Increase in the
levels of oestrogen results in the growth of endometrium and myometrium of the uterus. It
stimulates endometrial cells for the generation of progesterone receptors which is helpful in
priming the endometrium for the late proliferative and luteal phase. Higher levels of
oestrogen are responsible for the formation of newer layer of endometrium in the uterus
which is known as proliferative endometrium (Pope and Wurlitzer, 2017; Gravelle and
Gravelle, 2017).
Follicle-stimulating hormone (FSH) reaches its peak level in the first week of the follicular
phase. Rush of LH triggers ovulation. Abrupt change in level of hormone during ovulation
results in the slight alteration in the endometrium which lead to midcycle blood flow. After
completion of ovulation, progesterone initiates its action. Alteration in endometrium occur to
form secondary lining which makes endometrium ready for implantation of embryo which is
helpful in establishing pregnancy. After implantation of blastocyst, uterine lining remains as
the decidua which become part of placenta which is helpful in providing support and
protecting embryo during gestation. Decrease in the levels of progesterone and oestrogen
results in the shedding in endometrial lining and egg in menstruation. Death of corpus luteum
is mainly responsible for the reduced levels of progesterone and oestrogen which lead to the
termination of luteal phase. Raised levels of FSH are mainly responsible for the follicles
recruitment for next cycle (Pope and Wurlitzer, 2017; Gravelle and Gravelle, 2017).
Normal menstrual discharge can occur, even if, there is no ovulation. This phase is termed as
anovulatory cycle. Follicular development might initiate; however, it might not get
completed, even though oestrogen stimulate the uterine lining. In the secretory phase of the
menstrual cycle, uterine lining secrets different chemicals which perform different functions
like supporting early pregnancy or break down and shedding of endometrial lining, if
pregnancy does not occur (Gruhn and Kazer, 2013).
7
Several changes occur in uterine lining (endometrium) during menstrual cycle. Uterus
comprises of innermost glandular layer which is known as endometrium. During menstrual
cycle, endometrium gets thickened and it gets blood vessel rich tissue lining. Thickening of
the uterus is the appropriate milieu for the implantation of the blastocyst after its entry into
the uterus. During menstrual cycle, body initiate ovulation. There is gradual rise in the
oestrogen, which indicate initiation of follicular or proliferation phase of the menstrual cycle.
Consequently, there is slowing of the blood discharge which results in stopping response to
hormone and consequently there is thickening and proliferation of uterus. Increase in the
levels of oestrogen results in the growth of endometrium and myometrium of the uterus. It
stimulates endometrial cells for the generation of progesterone receptors which is helpful in
priming the endometrium for the late proliferative and luteal phase. Higher levels of
oestrogen are responsible for the formation of newer layer of endometrium in the uterus
which is known as proliferative endometrium (Pope and Wurlitzer, 2017; Gravelle and
Gravelle, 2017).
Follicle-stimulating hormone (FSH) reaches its peak level in the first week of the follicular
phase. Rush of LH triggers ovulation. Abrupt change in level of hormone during ovulation
results in the slight alteration in the endometrium which lead to midcycle blood flow. After
completion of ovulation, progesterone initiates its action. Alteration in endometrium occur to
form secondary lining which makes endometrium ready for implantation of embryo which is
helpful in establishing pregnancy. After implantation of blastocyst, uterine lining remains as
the decidua which become part of placenta which is helpful in providing support and
protecting embryo during gestation. Decrease in the levels of progesterone and oestrogen
results in the shedding in endometrial lining and egg in menstruation. Death of corpus luteum
is mainly responsible for the reduced levels of progesterone and oestrogen which lead to the
termination of luteal phase. Raised levels of FSH are mainly responsible for the follicles
recruitment for next cycle (Pope and Wurlitzer, 2017; Gravelle and Gravelle, 2017).
Normal menstrual discharge can occur, even if, there is no ovulation. This phase is termed as
anovulatory cycle. Follicular development might initiate; however, it might not get
completed, even though oestrogen stimulate the uterine lining. In the secretory phase of the
menstrual cycle, uterine lining secrets different chemicals which perform different functions
like supporting early pregnancy or break down and shedding of endometrial lining, if
pregnancy does not occur (Gruhn and Kazer, 2013).
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
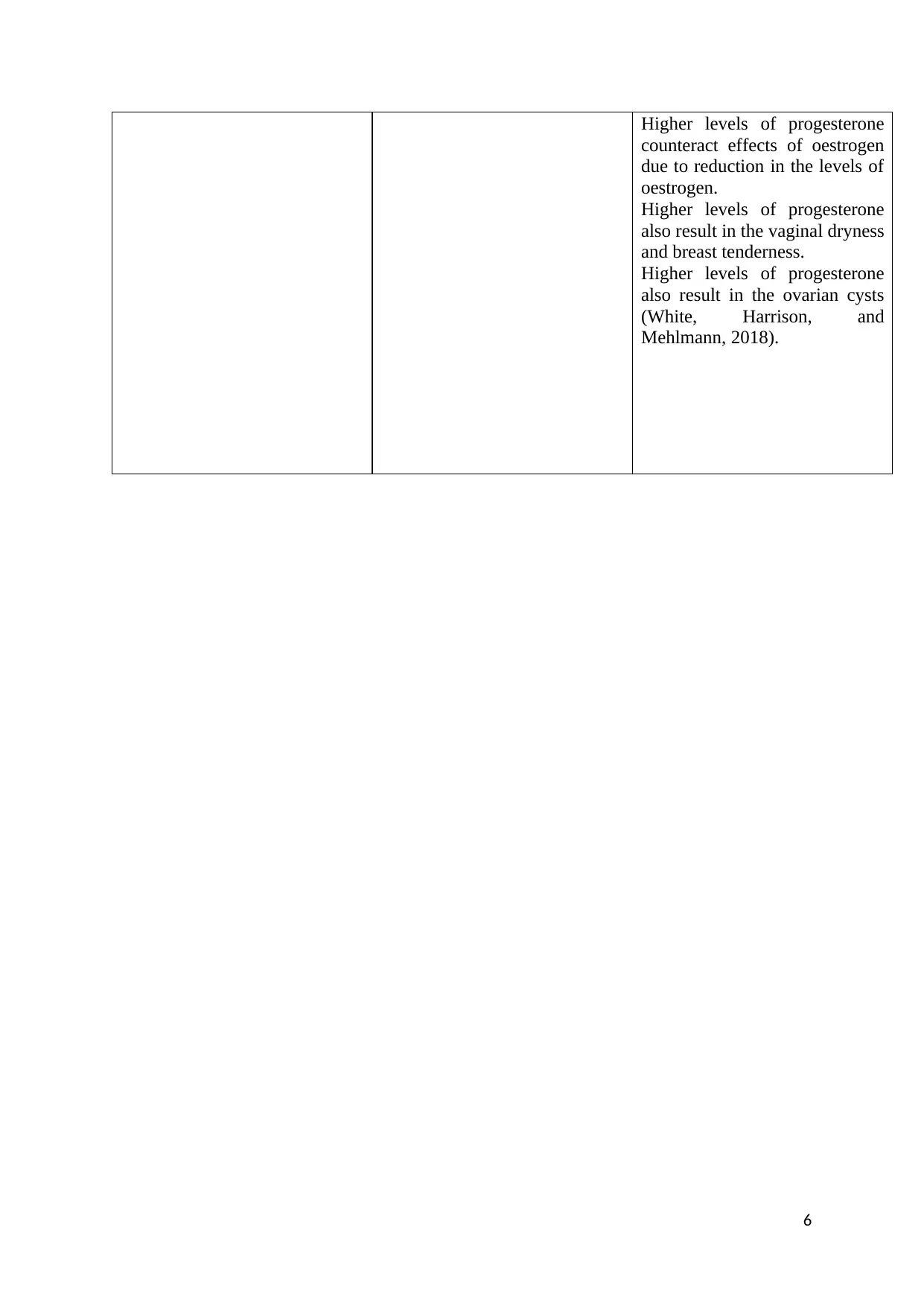
Task 3 :
a ) Pathway for sperm from testes to uterine tube
b ) Pathway for ovum from ovary to uterus.
c) Endometriosis is a condition which can affect fertility. Laparoscopic surgery is useful in
treating this condition and increase probability of conceiving with IVF. It has been reported
that IVF treatment increases the chances of pregnancy by 20 to 40 % in within three months
in the patients with endometriosis. Both fresh and frozen embryos can be used in the IVF
treatment. During IVF procedure, mature eggs from the ovaries gathered and fertilised with
sperm in the laboratory. Fertilised egg which is called as embryo is implanted in the uterus.
Riya is associated with fallopian tube blockage. Hence, it is problematic to get eggs fertilised
or embryo to get travelled to uterus. Riya is associated with endometriosis. Usually in
endometriosis; functioning of ovaries, uterus and fallopian tubes get affected. In case of Riya,
functioning of fallopian tubes get affected. Surgery is not useful in cases of blockade
8
Ovary – Immature eggs stored,
ovulation
Fallopian tubes – Fertilization
Uterus – Implantation
a ) Pathway for sperm from testes to uterine tube
b ) Pathway for ovum from ovary to uterus.
c) Endometriosis is a condition which can affect fertility. Laparoscopic surgery is useful in
treating this condition and increase probability of conceiving with IVF. It has been reported
that IVF treatment increases the chances of pregnancy by 20 to 40 % in within three months
in the patients with endometriosis. Both fresh and frozen embryos can be used in the IVF
treatment. During IVF procedure, mature eggs from the ovaries gathered and fertilised with
sperm in the laboratory. Fertilised egg which is called as embryo is implanted in the uterus.
Riya is associated with fallopian tube blockage. Hence, it is problematic to get eggs fertilised
or embryo to get travelled to uterus. Riya is associated with endometriosis. Usually in
endometriosis; functioning of ovaries, uterus and fallopian tubes get affected. In case of Riya,
functioning of fallopian tubes get affected. Surgery is not useful in cases of blockade
8
Ovary – Immature eggs stored,
ovulation
Fallopian tubes – Fertilization
Uterus – Implantation
fallopian tubes because it can increase risk of ectopic surgery because during surgery part of
the fallopian tube need to be removed. Hence, IVF need to be carried out in Riya, instead of
surgery. Since, fallopian tube blockage lead to difficulty in movement of fertilised egg to the
uterus. IVF is the invasive procedure hence; embryo is directly inserted into women’s uterus
(Leeton, 2013; Gardner and Simón, 2017). IVF would be helpful in case of Riya to fertilise
egg outside and insert it in her uterus. Whole procedure of IVF in Riya can be completed in
five steps like stimulation, egg retrieval, insemination, embryo culture and transfer. All these
steps are useful in the collection of eggs from the Riya and collection of semen from her
husband and culturing it in vitro. Produced embryo is get inserted into uterus through vagina
and cervix. Thus, there are chances of eliminating infertility in Riya through IVF (Leeton,
2013; Gardner and Simón, 2017).
Task 4 :
First 8 weeks of the human development after fertilisation is called as embryonic period. This
period is also known as organogenic period because during this period maximum number of
organs in the embryo starts developing. Embryonic stage is divided into 23 Carnegie stages.
Week Image Description
Week 1 In week 1, four Carnegie
stages occur. These four
stages are stage 1
corresponds to oocyte,
spermatozoa and
fertilization. Stage 2, 3
and 4 of week corresponds
to zygote, morula and
blastocyst respectively.
Week 2 of the pregnancy
is usually life changing
week. In week 2 ovulation
occurs and union of egg
and sperm results in the
initiation of the
pregnancy. Week 2
comprises of stage 5 and
9
the fallopian tube need to be removed. Hence, IVF need to be carried out in Riya, instead of
surgery. Since, fallopian tube blockage lead to difficulty in movement of fertilised egg to the
uterus. IVF is the invasive procedure hence; embryo is directly inserted into women’s uterus
(Leeton, 2013; Gardner and Simón, 2017). IVF would be helpful in case of Riya to fertilise
egg outside and insert it in her uterus. Whole procedure of IVF in Riya can be completed in
five steps like stimulation, egg retrieval, insemination, embryo culture and transfer. All these
steps are useful in the collection of eggs from the Riya and collection of semen from her
husband and culturing it in vitro. Produced embryo is get inserted into uterus through vagina
and cervix. Thus, there are chances of eliminating infertility in Riya through IVF (Leeton,
2013; Gardner and Simón, 2017).
Task 4 :
First 8 weeks of the human development after fertilisation is called as embryonic period. This
period is also known as organogenic period because during this period maximum number of
organs in the embryo starts developing. Embryonic stage is divided into 23 Carnegie stages.
Week Image Description
Week 1 In week 1, four Carnegie
stages occur. These four
stages are stage 1
corresponds to oocyte,
spermatozoa and
fertilization. Stage 2, 3
and 4 of week corresponds
to zygote, morula and
blastocyst respectively.
Week 2 of the pregnancy
is usually life changing
week. In week 2 ovulation
occurs and union of egg
and sperm results in the
initiation of the
pregnancy. Week 2
comprises of stage 5 and
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6. In this week
implantation and
blastocyst differentiation
occurs. Blastocyst
differentiation results in
the early embryonic and
placental forming
structures.
Week 3 Week 3 comprise of
Carnegie stage 7,8 and 9.
During 3 week, baby is a
tiny ball which is termed
as blastocyst. Blastocyst is
made of numerous
hundred cells which
undergoes multiplication
very quickly. During this
week, conceptus cells
contribute to placental
membrane and early
placenta. During this
week, trophoblast cells
remain invading uterine
wall as a part of early
placentation. Gastrulation
get converted into
bilaminar embryo into
trilamilar embryo.
10
implantation and
blastocyst differentiation
occurs. Blastocyst
differentiation results in
the early embryonic and
placental forming
structures.
Week 3 Week 3 comprise of
Carnegie stage 7,8 and 9.
During 3 week, baby is a
tiny ball which is termed
as blastocyst. Blastocyst is
made of numerous
hundred cells which
undergoes multiplication
very quickly. During this
week, conceptus cells
contribute to placental
membrane and early
placenta. During this
week, trophoblast cells
remain invading uterine
wall as a part of early
placentation. Gastrulation
get converted into
bilaminar embryo into
trilamilar embryo.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
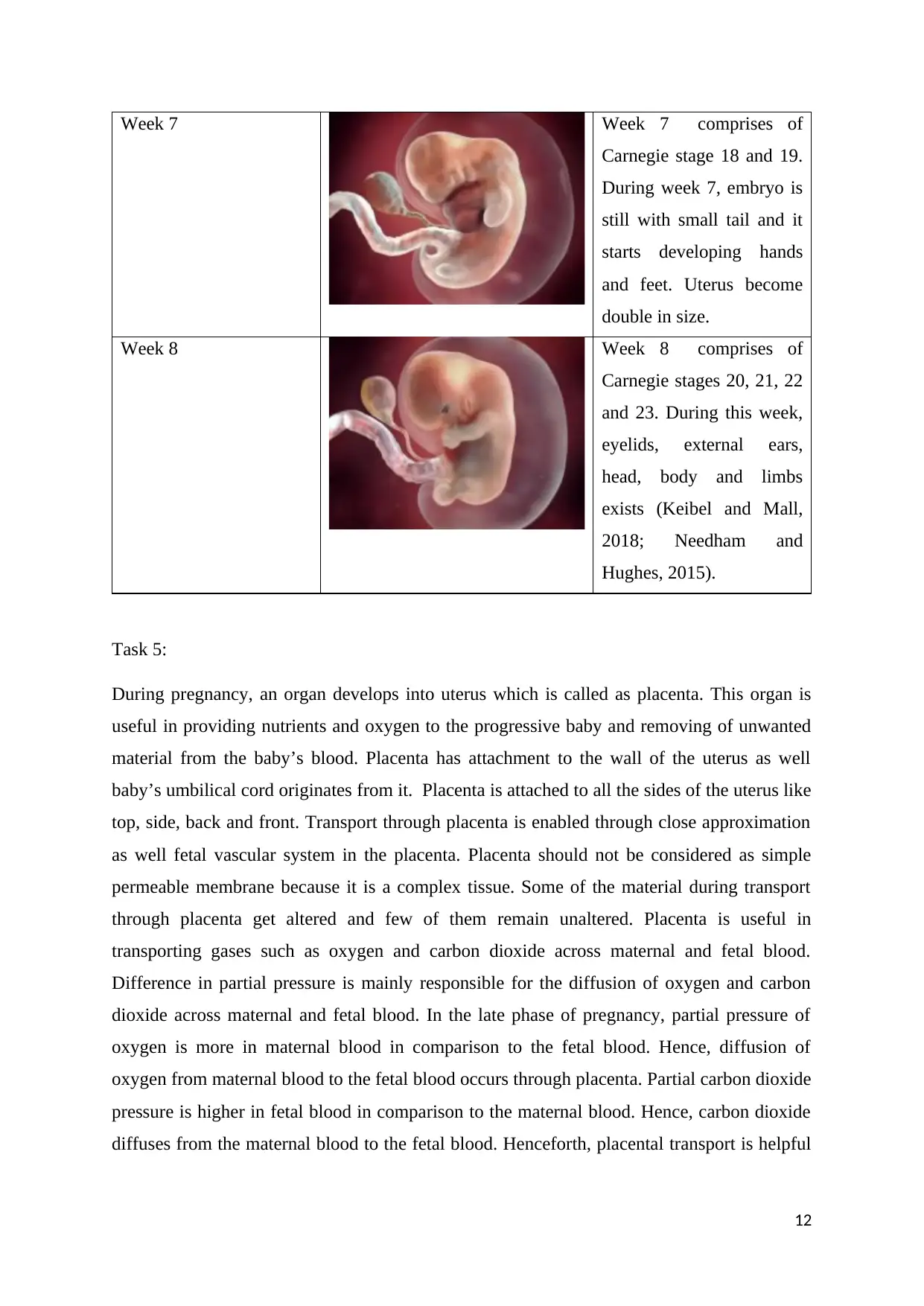
Week 4 Week 4 comprises of
Carnegie stages 10, 11, 12
and 13. In deep uterus,
two layered embryo is
present and primitive
placenta remain
developing.
Organogenesis initiated in
this week from the
trilaminar embryo.
Sensory placodes and limb
buds start appearing on
embryo surface. Within
embryo, circulatory,
digestive, urogenital and
nervous system begin to
develop.
Week 5 Week 5 comprises of
Carnegie stages 14 and 15.
This week is called as
organogenic period
because during this period,
maximum organs in the
embryo starts developing.
Week 6 Week 6 comprises of
Carnegie stages 16 and 17.
During this week, baby’s
nose, mouth and ears start
developing.
11
Carnegie stages 10, 11, 12
and 13. In deep uterus,
two layered embryo is
present and primitive
placenta remain
developing.
Organogenesis initiated in
this week from the
trilaminar embryo.
Sensory placodes and limb
buds start appearing on
embryo surface. Within
embryo, circulatory,
digestive, urogenital and
nervous system begin to
develop.
Week 5 Week 5 comprises of
Carnegie stages 14 and 15.
This week is called as
organogenic period
because during this period,
maximum organs in the
embryo starts developing.
Week 6 Week 6 comprises of
Carnegie stages 16 and 17.
During this week, baby’s
nose, mouth and ears start
developing.
11
Week 7 Week 7 comprises of
Carnegie stage 18 and 19.
During week 7, embryo is
still with small tail and it
starts developing hands
and feet. Uterus become
double in size.
Week 8 Week 8 comprises of
Carnegie stages 20, 21, 22
and 23. During this week,
eyelids, external ears,
head, body and limbs
exists (Keibel and Mall,
2018; Needham and
Hughes, 2015).
Task 5:
During pregnancy, an organ develops into uterus which is called as placenta. This organ is
useful in providing nutrients and oxygen to the progressive baby and removing of unwanted
material from the baby’s blood. Placenta has attachment to the wall of the uterus as well
baby’s umbilical cord originates from it. Placenta is attached to all the sides of the uterus like
top, side, back and front. Transport through placenta is enabled through close approximation
as well fetal vascular system in the placenta. Placenta should not be considered as simple
permeable membrane because it is a complex tissue. Some of the material during transport
through placenta get altered and few of them remain unaltered. Placenta is useful in
transporting gases such as oxygen and carbon dioxide across maternal and fetal blood.
Difference in partial pressure is mainly responsible for the diffusion of oxygen and carbon
dioxide across maternal and fetal blood. In the late phase of pregnancy, partial pressure of
oxygen is more in maternal blood in comparison to the fetal blood. Hence, diffusion of
oxygen from maternal blood to the fetal blood occurs through placenta. Partial carbon dioxide
pressure is higher in fetal blood in comparison to the maternal blood. Hence, carbon dioxide
diffuses from the maternal blood to the fetal blood. Henceforth, placental transport is helpful
12
Carnegie stage 18 and 19.
During week 7, embryo is
still with small tail and it
starts developing hands
and feet. Uterus become
double in size.
Week 8 Week 8 comprises of
Carnegie stages 20, 21, 22
and 23. During this week,
eyelids, external ears,
head, body and limbs
exists (Keibel and Mall,
2018; Needham and
Hughes, 2015).
Task 5:
During pregnancy, an organ develops into uterus which is called as placenta. This organ is
useful in providing nutrients and oxygen to the progressive baby and removing of unwanted
material from the baby’s blood. Placenta has attachment to the wall of the uterus as well
baby’s umbilical cord originates from it. Placenta is attached to all the sides of the uterus like
top, side, back and front. Transport through placenta is enabled through close approximation
as well fetal vascular system in the placenta. Placenta should not be considered as simple
permeable membrane because it is a complex tissue. Some of the material during transport
through placenta get altered and few of them remain unaltered. Placenta is useful in
transporting gases such as oxygen and carbon dioxide across maternal and fetal blood.
Difference in partial pressure is mainly responsible for the diffusion of oxygen and carbon
dioxide across maternal and fetal blood. In the late phase of pregnancy, partial pressure of
oxygen is more in maternal blood in comparison to the fetal blood. Hence, diffusion of
oxygen from maternal blood to the fetal blood occurs through placenta. Partial carbon dioxide
pressure is higher in fetal blood in comparison to the maternal blood. Hence, carbon dioxide
diffuses from the maternal blood to the fetal blood. Henceforth, placental transport is helpful
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




