Biomarker-Guided Antibiotic Stewardship in VAP: A Critical Report
VerifiedAdded on 2022/09/14
|10
|11013
|16
Report
AI Summary
The provided document is a research article published in The Lancet Respiratory Medicine, detailing the VAPrapid2 trial. This multicenter, randomized controlled trial investigated whether the measurement of IL-1β and IL-8 in bronchoalveolar lavage fluid could improve antibiotic stewardship in patients with clinically suspected ventilator-associated pneumonia in intensive care units (ICUs). The study included 210 patients across 24 ICUs in the UK, randomly assigned to either biomarker-guided antibiotic recommendations or routine antibiotic use. The primary outcome was antibiotic-free days. The trial found no significant difference in the primary outcome between the groups, suggesting that a rapid, highly sensitive rule-out test did not improve antibiotic stewardship due to established prescribing practices and reluctance for bronchoalveolar lavage. The study highlights the need to address prescribing culture and barriers to adopting new technologies to optimize antibiotic use in suspected ventilator-associated pneumonia. The trial was funded by the UK Department of Health and the Wellcome Trust.
182 www.thelancet.com/respiratory Vol 8 February 20
Articles
Lancet Respir Med 2020;
8: 182–91
Published Online
December 3, 2019
https://doi.org/10.1016/
S2213-2600(19)30367-4
SeeComment page 130
Translational and Clinical
Research Institute
(T P Hellyer PhD, A J Rostron PhD,
J Scott BSc, Prof A J Simpson PhD),
National Institute for Health
Research Newcastle In Vitro
Diagnostics Cooperative
(A J Allen PhD, Prof A J Simpson),
and Newcastle Clinical Trials
Unit (J Parker MClinRes,
S A Bowett PhD), Newcastle
University, Newcastle, UK;
The Wellcome-Wolfson Centre
for Experimental Medicine,
Queen’s University Belfast,
Belfast, UK
(Prof D F McAuley MD,
R McMullan MD,
L M Emerson MPH,
Prof B Blackwood PhD,
Prof C M O’Kane PhD);
Regional Intensive Care Unit
(Prof D F McAuley) and
Northern Ireland Clinical Trials
Unit (A Agus PhD, G Phair MSc),
The Royal Hospitals, Belfast,
UK; Anaesthesia, Critical Care
and Pain Medicine, University
of Edinburgh, Queen’s Medical
Research Institute, Edinburgh,
UK (Prof T S Walsh MD);
Intensive Care Unit, Royal
Infirmary of Edinburgh,
Edinburgh, UK (Prof T S Walsh,
K Kefala MD); Usher Institute,
University of Edinburgh,
Edinburgh, UK
(N Anderson PhD); Division of
Anaesthesia, Department of
Medicine, University of
Cambridge, Addenbrooke’s
Hospital, Cambridge, UK
(A Conway Morris PhD);
Department of Cancer and
Surgery, Imperial College
London, London, UK
Biomarker-guided antibiotic stewardship in sus
ventilator-associated pneumonia (VAPrapid2):
controlled trial and process evaluation
Thomas P Hellyer, Daniel F McAuley, Timothy S Walsh, Niall Anderson, Andrew Conway Morris, Suveer Singh, Pa
Gavin D Perkins, Ronan McMullan, Lydia M Emerson, Bronagh Blackwood, Stephen E Wright, Kallirroi Kefala, Ce
Simon V Baudouin, Ross L Paterson, Anthony J Rostron, Ashley Agus, Jonathan Bannard-Smith, Nicole M Robin, I
Christopher Bassford, Bryan Yates, Craig Spencer, Shondipon K Laha, Jonathan Hulme, Stephen Bonner, Vaness
Tina Van Den Broeck, Gert Boschman, DW James Keenan, Jonathan Scott, A Joy Allen, Glenn Phair, Jennie Parke
A John Simpson
Summary
Background Ventilator-associated pneumonia is the most common intensive care unit (I
accurate diagnosis remains difficult, leading to overuse of antibiotics. Low concentratio
bronchoalveolar lavage fluid have been validated as effective markers for exclusion of ventila
The VAPrapid2 trial aimed to determine whether measurement of bronchoalveolar lavage flui
effectively and safely improve antibiotic stewardship in patients with clinically suspected ven
Methods VAPrapid2 was a multicentre, randomised controlled trial in patients admitted to 24
Health Service hospital trusts across England, Scotland, and Northern Ireland. Patients were
and included if they were 18 years or older, intubated and mechanically ventilated for at leas
ventilator-associated pneumonia. Patients were randomly assigned (1:1) to biomarker-g
antibiotics (intervention group) or routine use of antibiotics (control group) using a web-base
hosted by Newcastle Clinical Trials Unit. Patients were randomised using randomly permuted
six and stratified by site, with allocation concealment. Clinicians were masked to patient assig
period until biomarker results were reported. Bronchoalveolar lavage was done in all patients
IL-1β and IL-8 rapidly determined in bronchoalveolar lavage fluid from patients randomised to
antibiotic recommendation group. If concentrations were below a previously validated cutoff,
that ventilator-associated pneumonia was unlikely and to consider discontinuing antibiotics.
use of antibiotics group received antibiotics according to usual practice at sites. Micro
bronchoalveolar lavage fluid from all patients and ventilator-associated pneumonia was
10⁴ colony forming units per mL of bronchoalveolar lavage fluid. The primary outcome
antibiotic-free days in the 7 days following bronchoalveolar lavage. Data were analysed on an
with an additional per-protocol analysis that excluded patients randomly assigned to t
defaulted to routine use of antibiotics because of failure to return an adequate bioma
process evaluation assessed factors influencing trial adoption, recruitment, and decisio
registered with ISRCTN, ISRCTN65937227, and ClinicalTrials.gov, NCT01972425.
Findings Between Nov 6, 2013, and Sept 13, 2016, 360 patients were screened for inclusion in
were ineligible, leaving 214 who were recruited to the study. Four patients were excluded bef
meaning that 210 patients were randomly assigned to biomarker-guided recommendation on
routine use of antibiotics (n=106). One patient in the biomarker-guided recommendation grou
the clinical team before bronchoscopy and so was excluded from the intention-to-treat
significant difference in the primary outcome of the distribution of antibiotic-free days
bronchoalveolar lavage in the intention-to-treat analysis (p=0·58). Bronchoalveolar lavag
small and transient increase in oxygen requirements. Established prescribing practices, reluc
lavage, and dependence on a chain of trial-related procedures emerged as factors that impair
Interpretation Antibiotic use remains high in patients with suspected ventilator-associat
stewardship was not improved by a rapid, highly sensitive rule-out test. Prescribing culture, r
performance, might explain this absence of effect.
Funding UK Department of Health and the Wellcome Trust.
Copyright © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article und
Articles
Lancet Respir Med 2020;
8: 182–91
Published Online
December 3, 2019
https://doi.org/10.1016/
S2213-2600(19)30367-4
SeeComment page 130
Translational and Clinical
Research Institute
(T P Hellyer PhD, A J Rostron PhD,
J Scott BSc, Prof A J Simpson PhD),
National Institute for Health
Research Newcastle In Vitro
Diagnostics Cooperative
(A J Allen PhD, Prof A J Simpson),
and Newcastle Clinical Trials
Unit (J Parker MClinRes,
S A Bowett PhD), Newcastle
University, Newcastle, UK;
The Wellcome-Wolfson Centre
for Experimental Medicine,
Queen’s University Belfast,
Belfast, UK
(Prof D F McAuley MD,
R McMullan MD,
L M Emerson MPH,
Prof B Blackwood PhD,
Prof C M O’Kane PhD);
Regional Intensive Care Unit
(Prof D F McAuley) and
Northern Ireland Clinical Trials
Unit (A Agus PhD, G Phair MSc),
The Royal Hospitals, Belfast,
UK; Anaesthesia, Critical Care
and Pain Medicine, University
of Edinburgh, Queen’s Medical
Research Institute, Edinburgh,
UK (Prof T S Walsh MD);
Intensive Care Unit, Royal
Infirmary of Edinburgh,
Edinburgh, UK (Prof T S Walsh,
K Kefala MD); Usher Institute,
University of Edinburgh,
Edinburgh, UK
(N Anderson PhD); Division of
Anaesthesia, Department of
Medicine, University of
Cambridge, Addenbrooke’s
Hospital, Cambridge, UK
(A Conway Morris PhD);
Department of Cancer and
Surgery, Imperial College
London, London, UK
Biomarker-guided antibiotic stewardship in sus
ventilator-associated pneumonia (VAPrapid2):
controlled trial and process evaluation
Thomas P Hellyer, Daniel F McAuley, Timothy S Walsh, Niall Anderson, Andrew Conway Morris, Suveer Singh, Pa
Gavin D Perkins, Ronan McMullan, Lydia M Emerson, Bronagh Blackwood, Stephen E Wright, Kallirroi Kefala, Ce
Simon V Baudouin, Ross L Paterson, Anthony J Rostron, Ashley Agus, Jonathan Bannard-Smith, Nicole M Robin, I
Christopher Bassford, Bryan Yates, Craig Spencer, Shondipon K Laha, Jonathan Hulme, Stephen Bonner, Vaness
Tina Van Den Broeck, Gert Boschman, DW James Keenan, Jonathan Scott, A Joy Allen, Glenn Phair, Jennie Parke
A John Simpson
Summary
Background Ventilator-associated pneumonia is the most common intensive care unit (I
accurate diagnosis remains difficult, leading to overuse of antibiotics. Low concentratio
bronchoalveolar lavage fluid have been validated as effective markers for exclusion of ventila
The VAPrapid2 trial aimed to determine whether measurement of bronchoalveolar lavage flui
effectively and safely improve antibiotic stewardship in patients with clinically suspected ven
Methods VAPrapid2 was a multicentre, randomised controlled trial in patients admitted to 24
Health Service hospital trusts across England, Scotland, and Northern Ireland. Patients were
and included if they were 18 years or older, intubated and mechanically ventilated for at leas
ventilator-associated pneumonia. Patients were randomly assigned (1:1) to biomarker-g
antibiotics (intervention group) or routine use of antibiotics (control group) using a web-base
hosted by Newcastle Clinical Trials Unit. Patients were randomised using randomly permuted
six and stratified by site, with allocation concealment. Clinicians were masked to patient assig
period until biomarker results were reported. Bronchoalveolar lavage was done in all patients
IL-1β and IL-8 rapidly determined in bronchoalveolar lavage fluid from patients randomised to
antibiotic recommendation group. If concentrations were below a previously validated cutoff,
that ventilator-associated pneumonia was unlikely and to consider discontinuing antibiotics.
use of antibiotics group received antibiotics according to usual practice at sites. Micro
bronchoalveolar lavage fluid from all patients and ventilator-associated pneumonia was
10⁴ colony forming units per mL of bronchoalveolar lavage fluid. The primary outcome
antibiotic-free days in the 7 days following bronchoalveolar lavage. Data were analysed on an
with an additional per-protocol analysis that excluded patients randomly assigned to t
defaulted to routine use of antibiotics because of failure to return an adequate bioma
process evaluation assessed factors influencing trial adoption, recruitment, and decisio
registered with ISRCTN, ISRCTN65937227, and ClinicalTrials.gov, NCT01972425.
Findings Between Nov 6, 2013, and Sept 13, 2016, 360 patients were screened for inclusion in
were ineligible, leaving 214 who were recruited to the study. Four patients were excluded bef
meaning that 210 patients were randomly assigned to biomarker-guided recommendation on
routine use of antibiotics (n=106). One patient in the biomarker-guided recommendation grou
the clinical team before bronchoscopy and so was excluded from the intention-to-treat
significant difference in the primary outcome of the distribution of antibiotic-free days
bronchoalveolar lavage in the intention-to-treat analysis (p=0·58). Bronchoalveolar lavag
small and transient increase in oxygen requirements. Established prescribing practices, reluc
lavage, and dependence on a chain of trial-related procedures emerged as factors that impair
Interpretation Antibiotic use remains high in patients with suspected ventilator-associat
stewardship was not improved by a rapid, highly sensitive rule-out test. Prescribing culture, r
performance, might explain this absence of effect.
Funding UK Department of Health and the Wellcome Trust.
Copyright © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article und
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Articles
www.thelancet.com/respiratory Vol 8 February 2020 183
(S Singh PhD); Division of
Infection Immunity and
Respiratory Medicine,
Manchester National Institute
for Health Research Biomedica
Research Centre, University of
Manchester, Manchester, UK
(Prof P Dark PhD); Integrated
Critical Care Unit, Sunderland
Royal Hospital, City Hospitals
Sunderland NHS Foundation
Trust, Sunderland, UK
(A I Roy MBChB, A J Rostron);
Warwick Medical School,
University of Warwick,
Coventry, UK
(Prof G D Perkins MD); Intensive
Care Unit, Heartlands Hospital
University Hospitals
Birmingham NHS Foundation
Trust, Birmingham, UK
(Prof G D Perkins); Integrated
Critical Care Unit, Freeman
Hospital (S E Wright MBChB)
and Intensive Care Unit, Royal
Victoria Infirmary
(S V Baudouin MD), Newcastle
upon Tyne Hospitals NHS
Foundation Trust, Newcastle,
UK; Intensive Care Unit,
Western General Hospital,
Edinburgh, UK
(R L Paterson MD); Intensive
Care Unit, Manchester Royal
Infirmary, Manchester
University NHS Foundation
Trust, Manchester, UK
(J Bannard-Smith MBChB);
Intensive Care Unit, Countess
of Chester NHS Foundation
Trust, Chester, UK
(N M Robin MBChB); Institute
of Ageing and Chronic Disease
University of Liverpool,
Liverpool, UK
(Prof I D Welters PhD); Intensive
Care Unit, University Hospital
Coventry, University Hospitals
Coventry and Warwickshire
NHS Trust, Coventry, UK
(C Bassford PhD); Intensive Care
Unit, Northumbria Specialist
Emergency Care Hospital,
Cramlington, UK
(B Yates MBBS); Intensive Care
Unit, Preston Royal Hospital,
Lancashire Teaching Hospitals
NHS Foundation Trust,
Preston, UK (C Spencer MBChB,
S K Laha MA); Intensive Care
Unit, Sandwell General
Hospital, Sandwell and
West Birmingham Hospitals
NHS Trust, West Bromwich, UK
(J Hulme MD); Intensive Care
Unit, James Cook University
Hospital, South Tees Hospitals
NHS Foundation Trust,
Middlesbrough, UK
(Prof S Bonner FFICM); Intensive
Care Unit, Queen Elizabeth
Introduction
Ventilator-associated pneumonia is the most common
infection acquired in intensive care units (ICUs),1 and is
associatedwith substantialmortality,particu larlyin
the ageing ICU population.2 Broad-spectrum antibiotic
use is recommended in suspected ventilator-associated
pneumonia.3,4 However,diag nosisof this infection
remains notoriously difficult, and pulmonary infection is
typically confirmed in only 20–60% of suspected cases.5
Consequently,antibioticsare overusedfor suspected
ventilator-associatedpneumonia,potentiallyexposing
patients to adverse effects, detracting from alternative
causes of respiratory compromise, increasing costs, and
driving emergence of antimicrobial resistance.5
Point prevalence studies suggest that 70% of patients
in the ICU receive antibiotics.6 The association between
increased antibiotic use and emergence of antimicrobial
resistance in ICUs is well established.7 In the setting
of hospital-acquired pneumonia, adherence to guide-
lines that promote broad-spectrum empirical antibiotics
has been associatedwith adverseoutcomes.8 This
background has driven a need to rationalise antibiotic
prescribing in ICUs.
Rapid diagnostic tests with the capacity to rule out
ventilator-associatedpneumoniamight presentearly
opportunitiesto optimiseantibioticprescriptionand
decrease antibiotic use. Among protein-based biomarkers,
only a combination of low IL-1β and IL-8 concentrations
in bronchoalveolar lavage fluid has been validated in a
multicentresetting in suspectedventilator-asso ciated
pneumonia.9,10
The VAPrapid2 trial aimed to determinewhether
measurement of bronchoalveolar lavage fluid IL-1β and
IL-8 could improve antibiotic stewardshipwithout
compromisingpatientsafetyin suspectedventilator-
associated pneumonia. In keeping with expert guidance
on analysis of complex interventions,11 a process eva-
luation study was embedded in this trial.
Methods
Study design and participants
VAPrapid2 was a multicentre, randomised controlled
trial in patients admitted to the ICU with suspected
ventilator-associated pneumonia. The trial was done in
24 ICUs from 17 National Health Service (NHS) hospital
trusts across England, Scotland, and Northern Ireland.
Research in context
Evidence before this study
We searched Medline between Jan 1, 1996, and April 30, 2019,
with the MeSH terms “Pneumonia”; “Pneumonia, bacterial”;
“Pneumonia, Ventilator-Associated”; “Respiratory Tract
Infections”; “Biomarkers”; “Protein Precursors”; and “Anti-
bacterial Agents”. Although several trials investigated the role
of procalcitonin in reducing antibiotic use in lower respiratory
tract infections, to our knowledge, few trials have been done in
patients with ventilator-associated pneumonia. A multicentre
trial of a procalcitonin-guided intervention to discontinue
antibiotics in patients with ventilator-associated pneumonia
reported a significant improvement in antibiotic-free days at
28 days. However, the duration of antibiotics in both the
intervention and the control groups of the trial were longer
than the 8-day duration recommended in international
guidelines. A further single-centre trial used a combination of
the Clinical Pulmonary Infection Score and procalcitonin to
guide antibiotic discontinuation in patients who had already
completed 7 days of antibiotic therapy. Although patients in
the procalcitonin group had more antibiotic-free days at
28 days versus the control group, the duration of antibiotics in
both groups was longer than 8 days. These studies focused on
discontinuation of antibiotics once empirical treatment was
established. To our knowledge, there are no published trials in
which antibiotic stewardship is based on early exclusion of
ventilator-associated pneumonia.
Added value of this study
To our knowledge, VAPrapid2 is the first trial to use a validated
biomarker in a cohort of patients with clinically suspected
ventilator-associated pneumonia, with an aim to determine
whether early exclusion of ventilator-associated pneumonia
could improve antibiotic stewardship. Furthermore, our trial
included a process evaluation that aimed to understand clinical
behaviours and implementation of the trial protocol. This trial
showed that, although the biomarker test could accurately
exclude ventilator-associated pneumonia, the trial
recommendation regarding antibiotic discontinuation was
seldom followed by clinicians, resulting in no difference in
antibiotic use between the intervention and control groups.
The results of this trial highlight entrenched behaviours in
antibiotic prescribing practice and barriers to adopting new,
unfamiliar technologies.
Implications of all the available evidence
Previous trials of procalcitonin have influenced the duration of
antibiotic treatment in patients with ventilator-associated
pneumonia. However, most patients with suspected ventilator-
associated pneumonia do not actually have it, subjecting them
to unnecessary antibiotic treatment while the true cause of
respiratory compromise potentially goes untreated. Avoiding
antibiotic use in such patients remains an important goal for
antibiotic stewardship in intensive care units. The VAPrapid2
trial showed no influence on antibiotic prescribing practices in
this patient group. Future studies should differentiate
suspected from confirmed ventilator-associated pneumonia,
aim to reduce antibiotics in patients who do not have
confirmed infection, and dissect complex mechanisms that
influence prescribing practices.
www.thelancet.com/respiratory Vol 8 February 2020 183
(S Singh PhD); Division of
Infection Immunity and
Respiratory Medicine,
Manchester National Institute
for Health Research Biomedica
Research Centre, University of
Manchester, Manchester, UK
(Prof P Dark PhD); Integrated
Critical Care Unit, Sunderland
Royal Hospital, City Hospitals
Sunderland NHS Foundation
Trust, Sunderland, UK
(A I Roy MBChB, A J Rostron);
Warwick Medical School,
University of Warwick,
Coventry, UK
(Prof G D Perkins MD); Intensive
Care Unit, Heartlands Hospital
University Hospitals
Birmingham NHS Foundation
Trust, Birmingham, UK
(Prof G D Perkins); Integrated
Critical Care Unit, Freeman
Hospital (S E Wright MBChB)
and Intensive Care Unit, Royal
Victoria Infirmary
(S V Baudouin MD), Newcastle
upon Tyne Hospitals NHS
Foundation Trust, Newcastle,
UK; Intensive Care Unit,
Western General Hospital,
Edinburgh, UK
(R L Paterson MD); Intensive
Care Unit, Manchester Royal
Infirmary, Manchester
University NHS Foundation
Trust, Manchester, UK
(J Bannard-Smith MBChB);
Intensive Care Unit, Countess
of Chester NHS Foundation
Trust, Chester, UK
(N M Robin MBChB); Institute
of Ageing and Chronic Disease
University of Liverpool,
Liverpool, UK
(Prof I D Welters PhD); Intensive
Care Unit, University Hospital
Coventry, University Hospitals
Coventry and Warwickshire
NHS Trust, Coventry, UK
(C Bassford PhD); Intensive Care
Unit, Northumbria Specialist
Emergency Care Hospital,
Cramlington, UK
(B Yates MBBS); Intensive Care
Unit, Preston Royal Hospital,
Lancashire Teaching Hospitals
NHS Foundation Trust,
Preston, UK (C Spencer MBChB,
S K Laha MA); Intensive Care
Unit, Sandwell General
Hospital, Sandwell and
West Birmingham Hospitals
NHS Trust, West Bromwich, UK
(J Hulme MD); Intensive Care
Unit, James Cook University
Hospital, South Tees Hospitals
NHS Foundation Trust,
Middlesbrough, UK
(Prof S Bonner FFICM); Intensive
Care Unit, Queen Elizabeth
Introduction
Ventilator-associated pneumonia is the most common
infection acquired in intensive care units (ICUs),1 and is
associatedwith substantialmortality,particu larlyin
the ageing ICU population.2 Broad-spectrum antibiotic
use is recommended in suspected ventilator-associated
pneumonia.3,4 However,diag nosisof this infection
remains notoriously difficult, and pulmonary infection is
typically confirmed in only 20–60% of suspected cases.5
Consequently,antibioticsare overusedfor suspected
ventilator-associatedpneumonia,potentiallyexposing
patients to adverse effects, detracting from alternative
causes of respiratory compromise, increasing costs, and
driving emergence of antimicrobial resistance.5
Point prevalence studies suggest that 70% of patients
in the ICU receive antibiotics.6 The association between
increased antibiotic use and emergence of antimicrobial
resistance in ICUs is well established.7 In the setting
of hospital-acquired pneumonia, adherence to guide-
lines that promote broad-spectrum empirical antibiotics
has been associatedwith adverseoutcomes.8 This
background has driven a need to rationalise antibiotic
prescribing in ICUs.
Rapid diagnostic tests with the capacity to rule out
ventilator-associatedpneumoniamight presentearly
opportunitiesto optimiseantibioticprescriptionand
decrease antibiotic use. Among protein-based biomarkers,
only a combination of low IL-1β and IL-8 concentrations
in bronchoalveolar lavage fluid has been validated in a
multicentresetting in suspectedventilator-asso ciated
pneumonia.9,10
The VAPrapid2 trial aimed to determinewhether
measurement of bronchoalveolar lavage fluid IL-1β and
IL-8 could improve antibiotic stewardshipwithout
compromisingpatientsafetyin suspectedventilator-
associated pneumonia. In keeping with expert guidance
on analysis of complex interventions,11 a process eva-
luation study was embedded in this trial.
Methods
Study design and participants
VAPrapid2 was a multicentre, randomised controlled
trial in patients admitted to the ICU with suspected
ventilator-associated pneumonia. The trial was done in
24 ICUs from 17 National Health Service (NHS) hospital
trusts across England, Scotland, and Northern Ireland.
Research in context
Evidence before this study
We searched Medline between Jan 1, 1996, and April 30, 2019,
with the MeSH terms “Pneumonia”; “Pneumonia, bacterial”;
“Pneumonia, Ventilator-Associated”; “Respiratory Tract
Infections”; “Biomarkers”; “Protein Precursors”; and “Anti-
bacterial Agents”. Although several trials investigated the role
of procalcitonin in reducing antibiotic use in lower respiratory
tract infections, to our knowledge, few trials have been done in
patients with ventilator-associated pneumonia. A multicentre
trial of a procalcitonin-guided intervention to discontinue
antibiotics in patients with ventilator-associated pneumonia
reported a significant improvement in antibiotic-free days at
28 days. However, the duration of antibiotics in both the
intervention and the control groups of the trial were longer
than the 8-day duration recommended in international
guidelines. A further single-centre trial used a combination of
the Clinical Pulmonary Infection Score and procalcitonin to
guide antibiotic discontinuation in patients who had already
completed 7 days of antibiotic therapy. Although patients in
the procalcitonin group had more antibiotic-free days at
28 days versus the control group, the duration of antibiotics in
both groups was longer than 8 days. These studies focused on
discontinuation of antibiotics once empirical treatment was
established. To our knowledge, there are no published trials in
which antibiotic stewardship is based on early exclusion of
ventilator-associated pneumonia.
Added value of this study
To our knowledge, VAPrapid2 is the first trial to use a validated
biomarker in a cohort of patients with clinically suspected
ventilator-associated pneumonia, with an aim to determine
whether early exclusion of ventilator-associated pneumonia
could improve antibiotic stewardship. Furthermore, our trial
included a process evaluation that aimed to understand clinical
behaviours and implementation of the trial protocol. This trial
showed that, although the biomarker test could accurately
exclude ventilator-associated pneumonia, the trial
recommendation regarding antibiotic discontinuation was
seldom followed by clinicians, resulting in no difference in
antibiotic use between the intervention and control groups.
The results of this trial highlight entrenched behaviours in
antibiotic prescribing practice and barriers to adopting new,
unfamiliar technologies.
Implications of all the available evidence
Previous trials of procalcitonin have influenced the duration of
antibiotic treatment in patients with ventilator-associated
pneumonia. However, most patients with suspected ventilator-
associated pneumonia do not actually have it, subjecting them
to unnecessary antibiotic treatment while the true cause of
respiratory compromise potentially goes untreated. Avoiding
antibiotic use in such patients remains an important goal for
antibiotic stewardship in intensive care units. The VAPrapid2
trial showed no influence on antibiotic prescribing practices in
this patient group. Future studies should differentiate
suspected from confirmed ventilator-associated pneumonia,
aim to reduce antibiotics in patients who do not have
confirmed infection, and dissect complex mechanisms that
influence prescribing practices.
Articles
184 www.thelancet.com/respiratory Vol 8 February 20
Hospital, Gateshead NHS
Foundation Trust, Gateshead,
UK (V Linnett MBBS); Intensive
Care Unit, Russells Hall
Hospital, Dudley Group NHS
Foundation Trust, Dudley, UK
(J Sonksen MBChB); and Becton
Dickinson Biosciences Europe,
Erembodegem, Belgium
(T Van Den Broeck PhD,
G Boschman PhD,
D W J Keenan BSc)
Correspondence to:
Prof A John Simpson,
Translational and Clinical
Research Institute, Newcastle
University, Newcastle NE2 4HH,
UK
j.simpson@ncl.ac.uk
See Onlinefor appendix
Patients were screened for eligibility on weekdays and
included if they were aged 18 years or older, intubated
and mechanically ventilated for at least 48 h, and had
suspected ventilator-associated pneumonia. Criteria for
suspected ventilator-associated pneumonia were new or
worsening chest radiographic (x-ray or chest CT) alveolar
changesplus at least two of the following: body
temperature less than 35°C or greater than 38°C, white
cell count less than 4 × 10⁹/L or greater than 11 × 10⁹/L,
and purulent tracheal secretions.5 Additionally, clinicians
had to con sidereligible patientsunlikely to have
extrapulmonary infection requiring antibiotic treatment
(ie, early discontinuationof antibioticswould be
appropriateif ventilator-associatedpneumonia was
confidently excluded).
Patients were excluded if they fulfilled the criteria
predicting poor tolerance of bronchoscopy and broncho-
alveolar lavage: PaO2 less than 8 kPa on FiO2 greater
than 0·7, positive end-expiratory pressure greater than
15 cmH2O, peak airway pressure greater than 35 cmH2O,
heart rate greater than 140 beats per minute, mean
arterial pressure less than 65 mm Hg, bleeding diathesis
(platelet count <20 × 10⁹/L or international normalised
ratio >3), intracranial pressure greater than 20 mm Hg,
and ICU consultantconsideredbronchoscopyand
bronchoalveolar lavage to be unsafe for the patient.
The research protocol was approved by the England and
Northern Ireland (13/LO/065) and Scotland (13/SS/0074)
National Research Ethics Service committees, and the trial
protocol has been published previously.12 Patients or their
relatives or representatives gave written informed consent
for inclusion in the study.
Randomisation and masking
Patientswere randomlyassigned(1:1)to biomarker-
guided recommendationon antibiotics(intervention
group) or routine use of antibiotics(controlgroup)
using a web-basedrandomisationservicehostedby
Newcastle Clinical Trials Unit (NCTU). Randomisation
was triggered by the technician receiving each patient’s
bronchoalveolar lavage fluid sample. The randomisation
sequence was generated by the trial statistician using
Sealed Envelope.Patients were randomisedusing
randomlypermuted blocks ofsize fourand six and
stratified by site, with allocation concealment. Participants
underwent the same clinical procedures up to the point
biomarker results were returned to the clinical service
for the intervention group. Therefore, there was an initial
period of double-blinding until test results were com-
municated to clini cians. As such, clinicians and research
nurses were masked until the biomarker results became
available.
Procedures
Investigators were asked to record a clinical opinion on
the pre-testprobabilityof ventilator-associatedpneu-
monia in randomly assigned patients—high, medium,
or low. A protocolised bronchoscopy and bronchoalveola
lavage was arranged for all randomly assigned patients
using a 120 mL lavage with 0·9% saline.10 Samples were
transportedat 4°C to one of six testinglaboratories
(appendix p 5), with a transport time of up to 1·5 h.
IL-1β and IL-8 in bronchoalveolar lavage fluid wer
measured by cytometric bead array using Accuri C6 flow
cytometers (Becton Dickinson Biosciences; San Jose, CA
USA). IL-1β and IL-8 concentrations in bronchoalveolar
lavagefluid were enteredinto a previouslyderived
equation for the exclusion of ventilator-associated pneu
monia,10 and an automated calculation was made av
able to the laboratory staff processing bronchoalveo
lavage fluid samples. Instructions were communicate
to clinicians by telephoneimmediatelyafter results
became available. For patients randomly assigned t
the biomarker-guided group, the instruction relayed
clinicians was either, “Biomarker result above cutoff
Ventilator-associatedpneumoniacannotbe excluded,
consider continuing antibiotics,” or “Biomarker resul
below cutoff. The negative predictive value is 1 an
ventilator-associatedpneumonia is very unlikely.
Consider discontinuation of antibiotics.” For patients
randomlyassignedto routine use of antibioticsthe
instruction given to clinicians was, “Patient in routin
use of antibiotics group.” If assays did not meet internal
quality control criteria, clinicians were advised to defaul
to routine care. The median negative predictive val
previously calculated for the combination of IL-1β a
IL-8 was 1·0 (95% CI 0·92–1·0).10
We defined confirmed ventilator-associated pneumoni
as growth of a potentially pathogenic organism of at lea
10⁴ colony forming units (CFU) per mL of broncho-
alveolar lavage fluid.13Microbiology testing was done in
accredited NHS or Public Health England microbiology
laboratories. Standard operating procedures for sem
quan titative culture were done in accordance with
2012 UK Standardsfor MicrobiologyInvestigation,
issued by the Health Protection Agency. This strate
allowed samples to be quantified as having no gro
1–10 CFU/mL, 10–10² CFU/mL, 10²–10³ CFU/mL,
10³–10⁴ CFU/mL, 10⁴–10⁵ CFU/mL, and so on, allowing
simple and clear demarcationof bacteriagrown at
10⁴ CFU/mL or more (ventilator-associated pneumonia)
and less than 10⁴ CFU/mL.
Investigators visited all ICUs before recruitment com-
menced, providing educational sessions on the diagnos
performance of the biomarkers and on the trial int
vention. Key components of trial design were reinforced
through regular communication. Additional training was
done in testing laboratories with respect to laborato
processes and biomarker measurement. Before the
commenced, clinicians were again made aware of t
biomarkertest and were encouragedto follow the
biomarker-guided recommendations. However, antibiot
use decisions were not mandated and were at clinicians
discretion.
For more on Sealed Envelope
see www.sealedenvelope.com
184 www.thelancet.com/respiratory Vol 8 February 20
Hospital, Gateshead NHS
Foundation Trust, Gateshead,
UK (V Linnett MBBS); Intensive
Care Unit, Russells Hall
Hospital, Dudley Group NHS
Foundation Trust, Dudley, UK
(J Sonksen MBChB); and Becton
Dickinson Biosciences Europe,
Erembodegem, Belgium
(T Van Den Broeck PhD,
G Boschman PhD,
D W J Keenan BSc)
Correspondence to:
Prof A John Simpson,
Translational and Clinical
Research Institute, Newcastle
University, Newcastle NE2 4HH,
UK
j.simpson@ncl.ac.uk
See Onlinefor appendix
Patients were screened for eligibility on weekdays and
included if they were aged 18 years or older, intubated
and mechanically ventilated for at least 48 h, and had
suspected ventilator-associated pneumonia. Criteria for
suspected ventilator-associated pneumonia were new or
worsening chest radiographic (x-ray or chest CT) alveolar
changesplus at least two of the following: body
temperature less than 35°C or greater than 38°C, white
cell count less than 4 × 10⁹/L or greater than 11 × 10⁹/L,
and purulent tracheal secretions.5 Additionally, clinicians
had to con sidereligible patientsunlikely to have
extrapulmonary infection requiring antibiotic treatment
(ie, early discontinuationof antibioticswould be
appropriateif ventilator-associatedpneumonia was
confidently excluded).
Patients were excluded if they fulfilled the criteria
predicting poor tolerance of bronchoscopy and broncho-
alveolar lavage: PaO2 less than 8 kPa on FiO2 greater
than 0·7, positive end-expiratory pressure greater than
15 cmH2O, peak airway pressure greater than 35 cmH2O,
heart rate greater than 140 beats per minute, mean
arterial pressure less than 65 mm Hg, bleeding diathesis
(platelet count <20 × 10⁹/L or international normalised
ratio >3), intracranial pressure greater than 20 mm Hg,
and ICU consultantconsideredbronchoscopyand
bronchoalveolar lavage to be unsafe for the patient.
The research protocol was approved by the England and
Northern Ireland (13/LO/065) and Scotland (13/SS/0074)
National Research Ethics Service committees, and the trial
protocol has been published previously.12 Patients or their
relatives or representatives gave written informed consent
for inclusion in the study.
Randomisation and masking
Patientswere randomlyassigned(1:1)to biomarker-
guided recommendationon antibiotics(intervention
group) or routine use of antibiotics(controlgroup)
using a web-basedrandomisationservicehostedby
Newcastle Clinical Trials Unit (NCTU). Randomisation
was triggered by the technician receiving each patient’s
bronchoalveolar lavage fluid sample. The randomisation
sequence was generated by the trial statistician using
Sealed Envelope.Patients were randomisedusing
randomlypermuted blocks ofsize fourand six and
stratified by site, with allocation concealment. Participants
underwent the same clinical procedures up to the point
biomarker results were returned to the clinical service
for the intervention group. Therefore, there was an initial
period of double-blinding until test results were com-
municated to clini cians. As such, clinicians and research
nurses were masked until the biomarker results became
available.
Procedures
Investigators were asked to record a clinical opinion on
the pre-testprobabilityof ventilator-associatedpneu-
monia in randomly assigned patients—high, medium,
or low. A protocolised bronchoscopy and bronchoalveola
lavage was arranged for all randomly assigned patients
using a 120 mL lavage with 0·9% saline.10 Samples were
transportedat 4°C to one of six testinglaboratories
(appendix p 5), with a transport time of up to 1·5 h.
IL-1β and IL-8 in bronchoalveolar lavage fluid wer
measured by cytometric bead array using Accuri C6 flow
cytometers (Becton Dickinson Biosciences; San Jose, CA
USA). IL-1β and IL-8 concentrations in bronchoalveolar
lavagefluid were enteredinto a previouslyderived
equation for the exclusion of ventilator-associated pneu
monia,10 and an automated calculation was made av
able to the laboratory staff processing bronchoalveo
lavage fluid samples. Instructions were communicate
to clinicians by telephoneimmediatelyafter results
became available. For patients randomly assigned t
the biomarker-guided group, the instruction relayed
clinicians was either, “Biomarker result above cutoff
Ventilator-associatedpneumoniacannotbe excluded,
consider continuing antibiotics,” or “Biomarker resul
below cutoff. The negative predictive value is 1 an
ventilator-associatedpneumonia is very unlikely.
Consider discontinuation of antibiotics.” For patients
randomlyassignedto routine use of antibioticsthe
instruction given to clinicians was, “Patient in routin
use of antibiotics group.” If assays did not meet internal
quality control criteria, clinicians were advised to defaul
to routine care. The median negative predictive val
previously calculated for the combination of IL-1β a
IL-8 was 1·0 (95% CI 0·92–1·0).10
We defined confirmed ventilator-associated pneumoni
as growth of a potentially pathogenic organism of at lea
10⁴ colony forming units (CFU) per mL of broncho-
alveolar lavage fluid.13Microbiology testing was done in
accredited NHS or Public Health England microbiology
laboratories. Standard operating procedures for sem
quan titative culture were done in accordance with
2012 UK Standardsfor MicrobiologyInvestigation,
issued by the Health Protection Agency. This strate
allowed samples to be quantified as having no gro
1–10 CFU/mL, 10–10² CFU/mL, 10²–10³ CFU/mL,
10³–10⁴ CFU/mL, 10⁴–10⁵ CFU/mL, and so on, allowing
simple and clear demarcationof bacteriagrown at
10⁴ CFU/mL or more (ventilator-associated pneumonia)
and less than 10⁴ CFU/mL.
Investigators visited all ICUs before recruitment com-
menced, providing educational sessions on the diagnos
performance of the biomarkers and on the trial int
vention. Key components of trial design were reinforced
through regular communication. Additional training was
done in testing laboratories with respect to laborato
processes and biomarker measurement. Before the
commenced, clinicians were again made aware of t
biomarkertest and were encouragedto follow the
biomarker-guided recommendations. However, antibiot
use decisions were not mandated and were at clinicians
discretion.
For more on Sealed Envelope
see www.sealedenvelope.com
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Articles
www.thelancet.com/respiratory Vol 8 February 2020 185
A process evaluation was done with interviews of clinical
staff and research staff (eg, site principal investigator,
consultants, research nurses, and ward manager) in the
following three phases: pre-trial (in month 1 of sites
joining the trial; exploring routine diagnosis and
management of ventilator-associated pneumonia), mid-
trial (once a site was involved in the trial for at least 1 year;
exploring intervention quality, attitudes to the trial, and
barriers or facilitators to suc cessful trial delivery), and late-
trial, with purposive sampling of nine sites based on pre-
trial and mid-trial results (in the final 3 months of the
intervention period in June to Augsust, 2016; exploring
local factors determining recruitment). Interviews were
done by LME. Further details are in the appendix (p 4).
Outcomes
The primary outcome was the distribution of antibiotic-
free days in the 7 days following bronchoalveolar lavage.
Antibiotic-free days were handled as an integer, with
patients classified in one of eight categories (0–7 antibiotic-
free days, inclusive).
Predefined secondary outcomes were antibiotic-free
days at days 14 and 28, antibiotic days at days 7, 14, and
28, ventilator-free days at 28 days, 28-day mortality and
ICU mortality,sequentialorgan failure assessment
(SOFA) score at days 3, 7 and 14, duration of critical care
(level 2 and level 3 care) and hospital stay, antibiotic-
associated infections (Clostridium difficile and meticillin-
resistant Staphylococcus aureus) up to hospital discharge,
death, or 56 days, antibiotic-resistant pathogens (resistant
to two or more antibiotics) cultured up to hospital dis-
charge, death, or 56 days, and health-care resource use
calculated from length of critical care and hospital stay
up to discharge, death, or 56 days. When considering
outcomes at days 7, 14, and 28, antibiotics refers to all
antibiotics given for treatment of infection; prophylactic
antibiotics were not considered.
Since adverse clinical events are common in ICUs, the
trial protocolmandatedreportingof adverseevents
within 2 h of bronchoscopy. Clinical team members
reported any further events after 2 h if they were con-
sidered clinically significant or related to the trial.
Statistical analysis
Full statistical methods were outlined in a Statistical
Analysis Plan before the close of recruitment. Sample
size was based on the change in frequency distribution
of antibiotic-free days in the 7 days following broncho-
alveolar lavage. Models of change in distribution are
outlined in the trial protocol.12 We deemed effect sizes
in the region 0·07–0·08 to be of a clinically relevant
magnitude.These effect sizes representan approx -
imate change in median antibiotic-free days from 0
(IQR 0·0–2·5) to 1·5 (0·0–3·5). There fore, we proposed
a recruitment target of 90 patients per group, with an α
of 0·05 and β of 0·20. Allowing for attrition of 14·3%,
the target sample size was 210 patients. The primary
analysis was done on the intention-to-treat population.
We analysedthe primary outcomeby χ² test on a
2 × 8 table of trial group versus antibiotic-free days.
Sensitivity analyses were done using a discrete-time
Cox proportionalhazards model with centre and
randomisation group as covariates, censored for death
or end of follow-up at 7 days. We did a further sensitivity
analysis, redefining antibiotic-freedays as zero if
death occurred within 7 days, as a more conservative
approach.
We analysed secondary outcomes using Cox propor-
tional hazards models, logistic regression, linear regres-
sion, or Poisson regression as appropriate (see appendix
p 4). Planned subgroup analyses included a per-protocol
analysis, clinician assessment of likelihood of ventilator-
associated pneumonia, and admission category (medical,
surgical caused by trauma or head injury, and other
surgical). We excluded patients randomly assigned to the
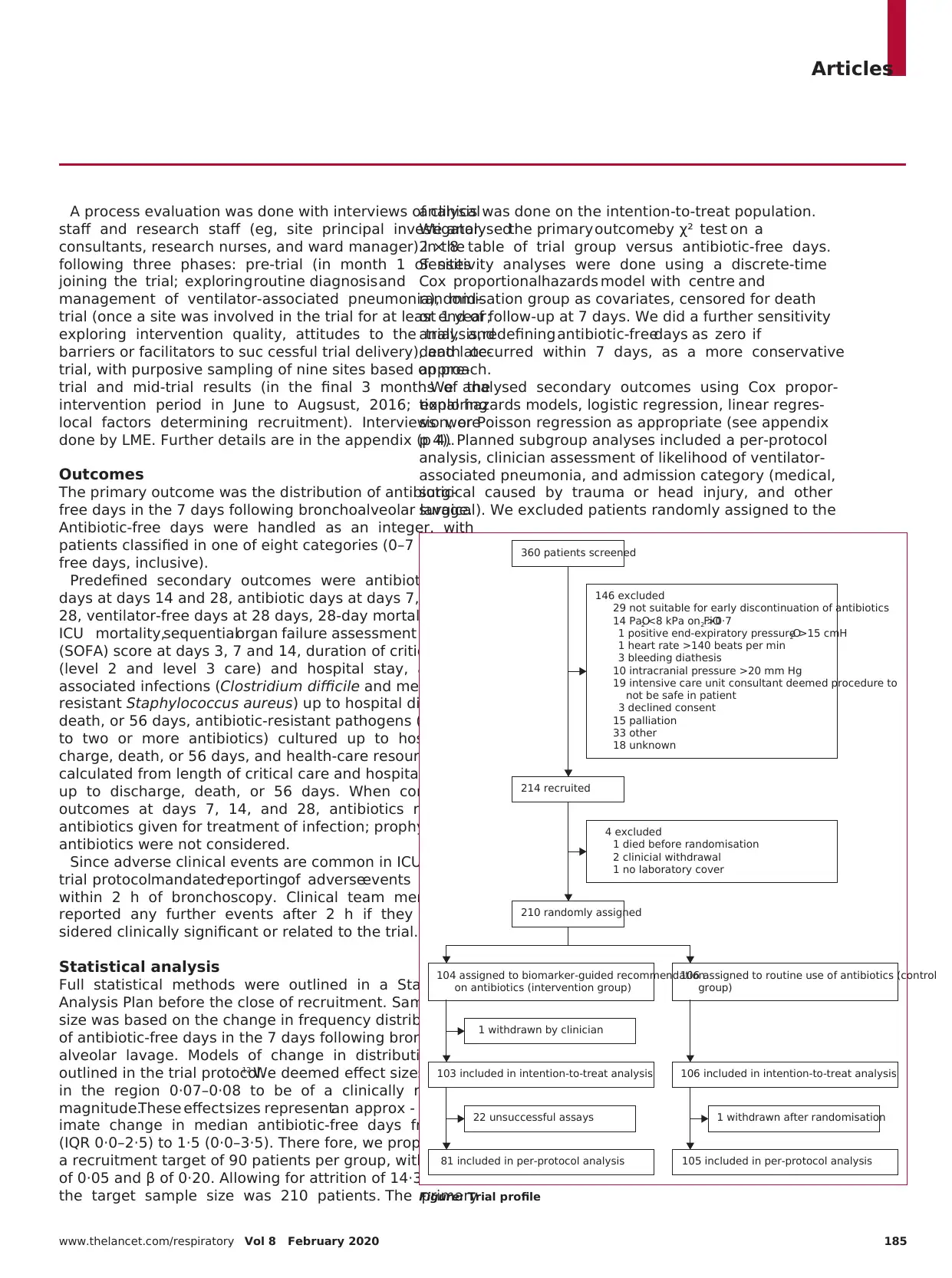
Figure: Trial profile
1 withdrawn by clinician
104 assigned to biomarker-guided recommendation
on antibiotics (intervention group)
103 included in intention-to-treat analysis
81 included in per-protocol analysis
22 unsuccessful assays
106 assigned to routine use of antibiotics (control
group)
106 included in intention-to-treat analysis
105 included in per-protocol analysis
1 withdrawn after randomisation
210 randomly assigned
214 recruited
360 patients screened
4 excluded
1 died before randomisation
2 clinicial withdrawal
1 no laboratory cover
146 excluded
29 not suitable for early discontinuation of antibiotics
14 PaO2 <8 kPa on FiO2 >0·7
1 positive end-expiratory pressure >15 cmH2O
1 heart rate >140 beats per min
3 bleeding diathesis
10 intracranial pressure >20 mm Hg
19 intensive care unit consultant deemed procedure to
not be safe in patient
3 declined consent
15 palliation
33 other
18 unknown
www.thelancet.com/respiratory Vol 8 February 2020 185
A process evaluation was done with interviews of clinical
staff and research staff (eg, site principal investigator,
consultants, research nurses, and ward manager) in the
following three phases: pre-trial (in month 1 of sites
joining the trial; exploring routine diagnosis and
management of ventilator-associated pneumonia), mid-
trial (once a site was involved in the trial for at least 1 year;
exploring intervention quality, attitudes to the trial, and
barriers or facilitators to suc cessful trial delivery), and late-
trial, with purposive sampling of nine sites based on pre-
trial and mid-trial results (in the final 3 months of the
intervention period in June to Augsust, 2016; exploring
local factors determining recruitment). Interviews were
done by LME. Further details are in the appendix (p 4).
Outcomes
The primary outcome was the distribution of antibiotic-
free days in the 7 days following bronchoalveolar lavage.
Antibiotic-free days were handled as an integer, with
patients classified in one of eight categories (0–7 antibiotic-
free days, inclusive).
Predefined secondary outcomes were antibiotic-free
days at days 14 and 28, antibiotic days at days 7, 14, and
28, ventilator-free days at 28 days, 28-day mortality and
ICU mortality,sequentialorgan failure assessment
(SOFA) score at days 3, 7 and 14, duration of critical care
(level 2 and level 3 care) and hospital stay, antibiotic-
associated infections (Clostridium difficile and meticillin-
resistant Staphylococcus aureus) up to hospital discharge,
death, or 56 days, antibiotic-resistant pathogens (resistant
to two or more antibiotics) cultured up to hospital dis-
charge, death, or 56 days, and health-care resource use
calculated from length of critical care and hospital stay
up to discharge, death, or 56 days. When considering
outcomes at days 7, 14, and 28, antibiotics refers to all
antibiotics given for treatment of infection; prophylactic
antibiotics were not considered.
Since adverse clinical events are common in ICUs, the
trial protocolmandatedreportingof adverseevents
within 2 h of bronchoscopy. Clinical team members
reported any further events after 2 h if they were con-
sidered clinically significant or related to the trial.
Statistical analysis
Full statistical methods were outlined in a Statistical
Analysis Plan before the close of recruitment. Sample
size was based on the change in frequency distribution
of antibiotic-free days in the 7 days following broncho-
alveolar lavage. Models of change in distribution are
outlined in the trial protocol.12 We deemed effect sizes
in the region 0·07–0·08 to be of a clinically relevant
magnitude.These effect sizes representan approx -
imate change in median antibiotic-free days from 0
(IQR 0·0–2·5) to 1·5 (0·0–3·5). There fore, we proposed
a recruitment target of 90 patients per group, with an α
of 0·05 and β of 0·20. Allowing for attrition of 14·3%,
the target sample size was 210 patients. The primary
analysis was done on the intention-to-treat population.
We analysedthe primary outcomeby χ² test on a
2 × 8 table of trial group versus antibiotic-free days.
Sensitivity analyses were done using a discrete-time
Cox proportionalhazards model with centre and
randomisation group as covariates, censored for death
or end of follow-up at 7 days. We did a further sensitivity
analysis, redefining antibiotic-freedays as zero if
death occurred within 7 days, as a more conservative
approach.
We analysed secondary outcomes using Cox propor-
tional hazards models, logistic regression, linear regres-
sion, or Poisson regression as appropriate (see appendix
p 4). Planned subgroup analyses included a per-protocol
analysis, clinician assessment of likelihood of ventilator-
associated pneumonia, and admission category (medical,
surgical caused by trauma or head injury, and other
surgical). We excluded patients randomly assigned to the
Figure: Trial profile
1 withdrawn by clinician
104 assigned to biomarker-guided recommendation
on antibiotics (intervention group)
103 included in intention-to-treat analysis
81 included in per-protocol analysis
22 unsuccessful assays
106 assigned to routine use of antibiotics (control
group)
106 included in intention-to-treat analysis
105 included in per-protocol analysis
1 withdrawn after randomisation
210 randomly assigned
214 recruited
360 patients screened
4 excluded
1 died before randomisation
2 clinicial withdrawal
1 no laboratory cover
146 excluded
29 not suitable for early discontinuation of antibiotics
14 PaO2 <8 kPa on FiO2 >0·7
1 positive end-expiratory pressure >15 cmH2O
1 heart rate >140 beats per min
3 bleeding diathesis
10 intracranial pressure >20 mm Hg
19 intensive care unit consultant deemed procedure to
not be safe in patient
3 declined consent
15 palliation
33 other
18 unknown
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Articles
186 www.thelancet.com/respiratory Vol 8 February 20
interventiongroup who defaultedto routine use of
antibiotics from the per-protocol analysis because th
did not return a biomarker result.
We assessed the prevalence of missing data during a
masked review after database lock, which was judg
to be of sufficiently low frequency as to not requir
imputation for all variables. However, as prespecified in
the Statistical Analysis Plan, SOFA scores were based on
the last evaluable score. Unadjusted CIs and p values ar
reported for multiplicity.
The Newcastle upon Tyne Hospitals NHS Foundation
Trust acted as sponsor for the trial. Clinical trial manage
ment was providedby the NCTU. An independent
data monitoring and safety committee oversaw the trial
(appendix p 3).
Analyses were done with R version 3.3.2, with the
addition of the discSurv package (version 1.3.4). Th
study is registered with ISRCTN, ISRCTN65937227, and
ClinicalTrials.gov, NCT01972425.
Role of the funding source
The funder of the study had no role in study design, dat
collection, data analysis, data interpretation, or writing
the report. The corresponding author had full access to
all the data in the study and had final responsibility for
the decision to submit for publication.
Results
Between Nov 6, 2013, and Sept 13, 2016, 360 patients
screened for inclusion in the study. 146 patients w
ineligible, leaving 214 who were recruited to the st
Four patientswere excludedbefore randomisation,
meaning that 210 patients were randomly assigned
biomarker-guided recommendation on antibiotics (n=10
or routine use of antibiotics (n=106; figure). One patien
in the biomarker-guidedrecommendationgroup was
withdrawn by the clinical team once baseline data
collected but before bronchoscopy, so was excluded fro
the intention-to-treat analysis.
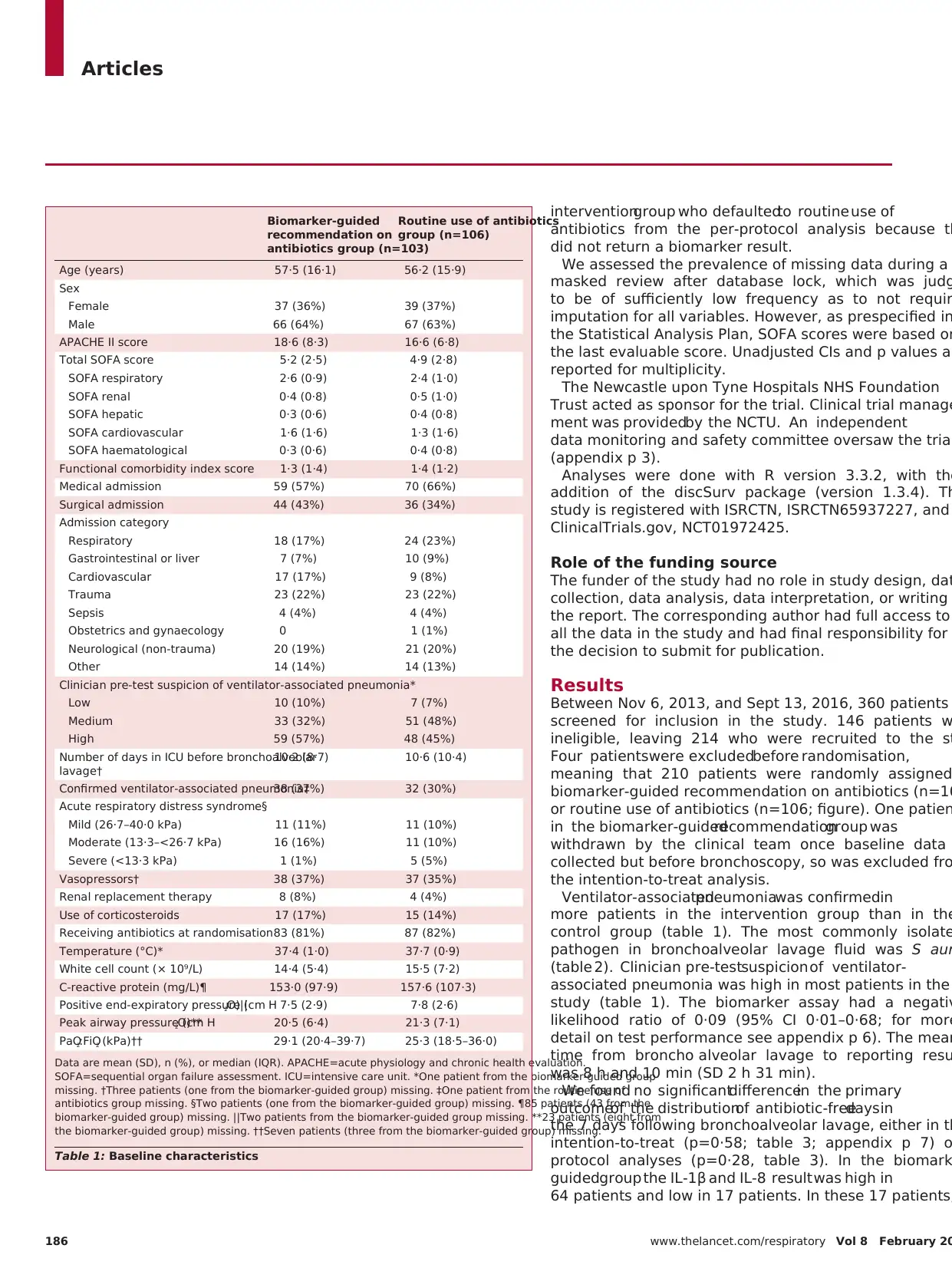
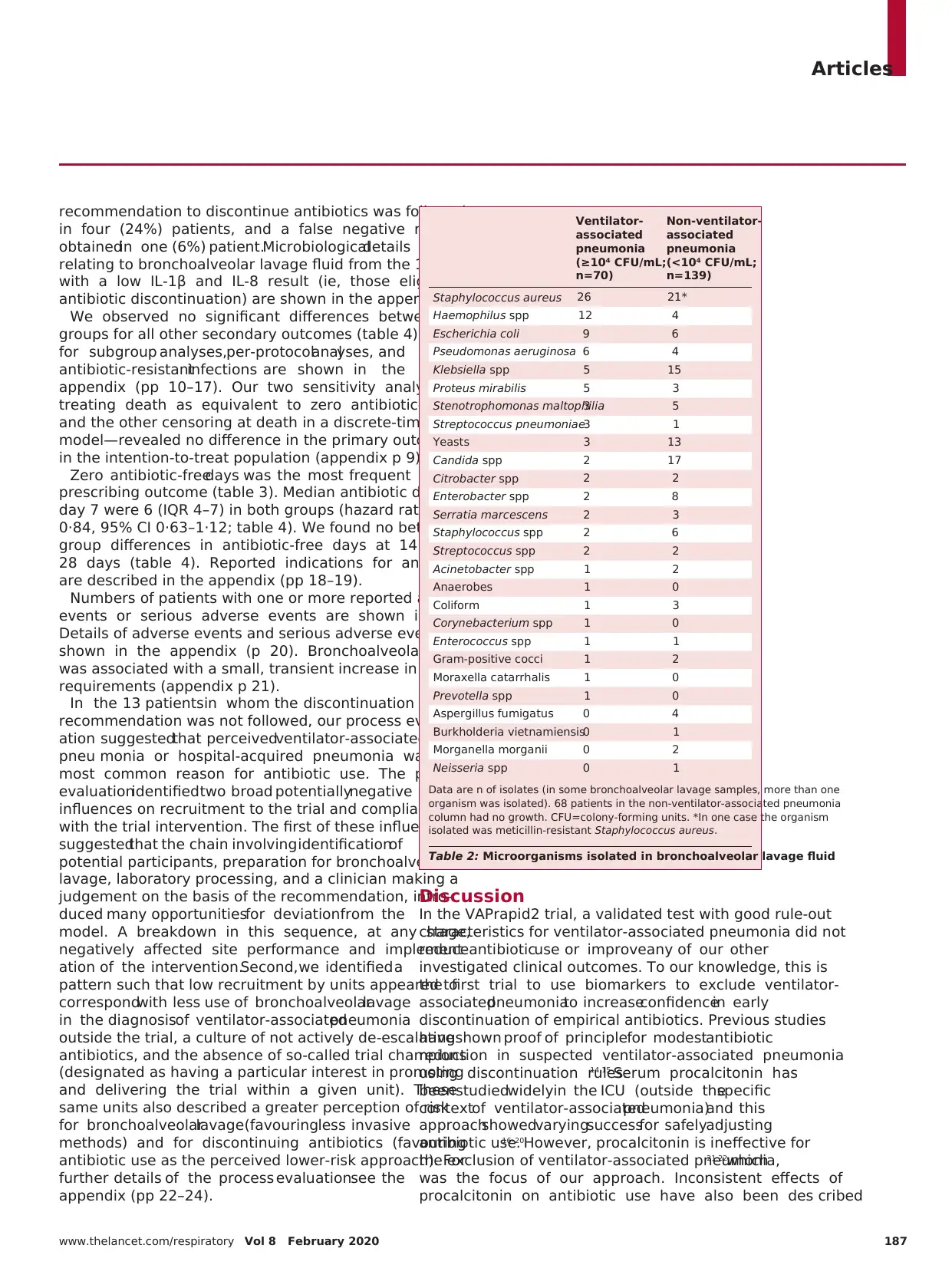
Ventilator-associatedpneumoniawas confirmedin
more patients in the intervention group than in the
control group (table 1). The most commonly isolate
pathogen in bronchoalveolar lavage fluid was S aur
(table 2). Clinician pre-testsuspicion of ventilator-
associated pneumonia was high in most patients in the
study (table 1). The biomarker assay had a negativ
likelihood ratio of 0·09 (95% CI 0·01–0·68; for more
detail on test performance see appendix p 6). The mean
time from broncho alveolar lavage to reporting resu
was 8 h and 10 min (SD 2 h 31 min).
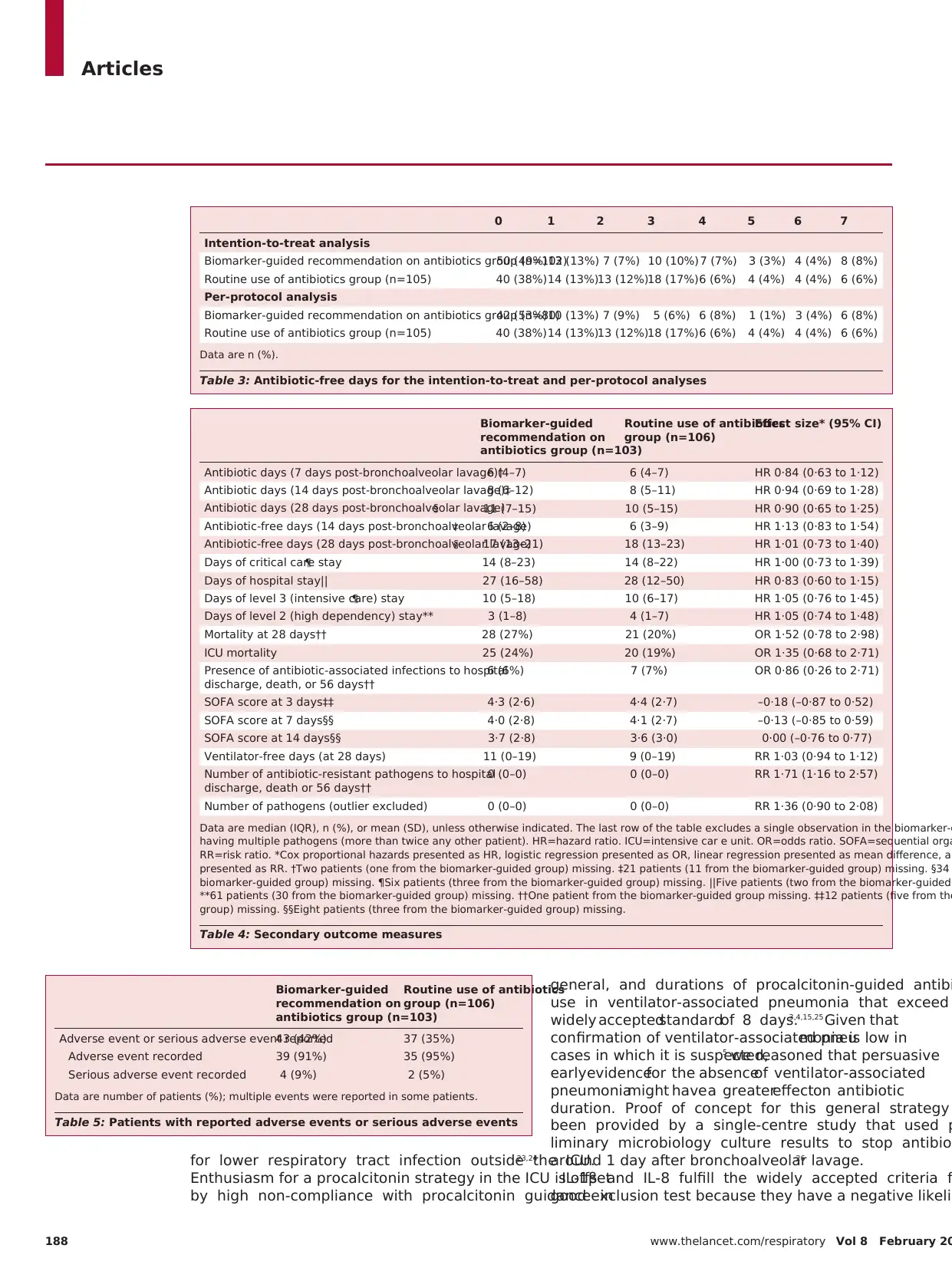
We found no significantdifferencein the primary
outcomeof the distributionof antibiotic-freedays in
the 7 days following bronchoalveolar lavage, either in th
intention-to-treat (p=0·58; table 3; appendix p 7) o
protocol analyses (p=0·28, table 3). In the biomark
guidedgroup the IL-1β and IL-8 result was high in
64 patients and low in 17 patients. In these 17 patients,
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Age (years) 57·5 (16·1) 56·2 (15·9)
Sex
Female 37 (36%) 39 (37%)
Male 66 (64%) 67 (63%)
APACHE II score 18·6 (8·3) 16·6 (6·8)
Total SOFA score 5·2 (2·5) 4·9 (2·8)
SOFA respiratory 2·6 (0·9) 2·4 (1·0)
SOFA renal 0·4 (0·8) 0·5 (1·0)
SOFA hepatic 0·3 (0·6) 0·4 (0·8)
SOFA cardiovascular 1·6 (1·6) 1·3 (1·6)
SOFA haematological 0·3 (0·6) 0·4 (0·8)
Functional comorbidity index score 1·3 (1·4) 1·4 (1·2)
Medical admission 59 (57%) 70 (66%)
Surgical admission 44 (43%) 36 (34%)
Admission category
Respiratory 18 (17%) 24 (23%)
Gastrointestinal or liver 7 (7%) 10 (9%)
Cardiovascular 17 (17%) 9 (8%)
Trauma 23 (22%) 23 (22%)
Sepsis 4 (4%) 4 (4%)
Obstetrics and gynaecology 0 1 (1%)
Neurological (non-trauma) 20 (19%) 21 (20%)
Other 14 (14%) 14 (13%)
Clinician pre-test suspicion of ventilator-associated pneumonia*
Low 10 (10%) 7 (7%)
Medium 33 (32%) 51 (48%)
High 59 (57%) 48 (45%)
Number of days in ICU before bronchoalveolar
lavage†
10·2 (8·7) 10·6 (10·4)
Confirmed ventilator-associated pneumonia‡38 (37%) 32 (30%)
Acute respiratory distress syndrome§
Mild (26·7–40·0 kPa) 11 (11%) 11 (10%)
Moderate (13·3–<26·7 kPa) 16 (16%) 11 (10%)
Severe (<13·3 kPa) 1 (1%) 5 (5%)
Vasopressors† 38 (37%) 37 (35%)
Renal replacement therapy 8 (8%) 4 (4%)
Use of corticosteroids 17 (17%) 15 (14%)
Receiving antibiotics at randomisation83 (81%) 87 (82%)
Temperature (°C)* 37·4 (1·0) 37·7 (0·9)
White cell count (× 10⁹/L) 14·4 (5·4) 15·5 (7·2)
C-reactive protein (mg/L)¶ 153·0 (97·9) 157·6 (107·3)
Positive end-expiratory pressure (cm H2O)|| 7·5 (2·9) 7·8 (2·6)
Peak airway pressure (cm H2O)** 20·5 (6·4) 21·3 (7·1)
PaO2:FiO2 (kPa)†† 29·1 (20·4–39·7) 25·3 (18·5–36·0)
Data are mean (SD), n (%), or median (IQR). APACHE=acute physiology and chronic health evaluation.
SOFA=sequential organ failure assessment. ICU=intensive care unit. *One patient from the biomarker-guided group
missing. †Three patients (one from the biomarker-guided group) missing. ‡One patient from the routine use of
antibiotics group missing. §Two patients (one from the biomarker-guided group) missing. ¶85 patients (43 from the
biomarker-guided group) missing. ||Two patients from the biomarker-guided group missing. **23 patients (eight from
the biomarker-guided group) missing. ††Seven patients (three from the biomarker-guided group) missing.
Table 1: Baseline characteristics
186 www.thelancet.com/respiratory Vol 8 February 20
interventiongroup who defaultedto routine use of
antibiotics from the per-protocol analysis because th
did not return a biomarker result.
We assessed the prevalence of missing data during a
masked review after database lock, which was judg
to be of sufficiently low frequency as to not requir
imputation for all variables. However, as prespecified in
the Statistical Analysis Plan, SOFA scores were based on
the last evaluable score. Unadjusted CIs and p values ar
reported for multiplicity.
The Newcastle upon Tyne Hospitals NHS Foundation
Trust acted as sponsor for the trial. Clinical trial manage
ment was providedby the NCTU. An independent
data monitoring and safety committee oversaw the trial
(appendix p 3).
Analyses were done with R version 3.3.2, with the
addition of the discSurv package (version 1.3.4). Th
study is registered with ISRCTN, ISRCTN65937227, and
ClinicalTrials.gov, NCT01972425.
Role of the funding source
The funder of the study had no role in study design, dat
collection, data analysis, data interpretation, or writing
the report. The corresponding author had full access to
all the data in the study and had final responsibility for
the decision to submit for publication.
Results
Between Nov 6, 2013, and Sept 13, 2016, 360 patients
screened for inclusion in the study. 146 patients w
ineligible, leaving 214 who were recruited to the st
Four patientswere excludedbefore randomisation,
meaning that 210 patients were randomly assigned
biomarker-guided recommendation on antibiotics (n=10
or routine use of antibiotics (n=106; figure). One patien
in the biomarker-guidedrecommendationgroup was
withdrawn by the clinical team once baseline data
collected but before bronchoscopy, so was excluded fro
the intention-to-treat analysis.
Ventilator-associatedpneumoniawas confirmedin
more patients in the intervention group than in the
control group (table 1). The most commonly isolate
pathogen in bronchoalveolar lavage fluid was S aur
(table 2). Clinician pre-testsuspicion of ventilator-
associated pneumonia was high in most patients in the
study (table 1). The biomarker assay had a negativ
likelihood ratio of 0·09 (95% CI 0·01–0·68; for more
detail on test performance see appendix p 6). The mean
time from broncho alveolar lavage to reporting resu
was 8 h and 10 min (SD 2 h 31 min).
We found no significantdifferencein the primary
outcomeof the distributionof antibiotic-freedays in
the 7 days following bronchoalveolar lavage, either in th
intention-to-treat (p=0·58; table 3; appendix p 7) o
protocol analyses (p=0·28, table 3). In the biomark
guidedgroup the IL-1β and IL-8 result was high in
64 patients and low in 17 patients. In these 17 patients,
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Age (years) 57·5 (16·1) 56·2 (15·9)
Sex
Female 37 (36%) 39 (37%)
Male 66 (64%) 67 (63%)
APACHE II score 18·6 (8·3) 16·6 (6·8)
Total SOFA score 5·2 (2·5) 4·9 (2·8)
SOFA respiratory 2·6 (0·9) 2·4 (1·0)
SOFA renal 0·4 (0·8) 0·5 (1·0)
SOFA hepatic 0·3 (0·6) 0·4 (0·8)
SOFA cardiovascular 1·6 (1·6) 1·3 (1·6)
SOFA haematological 0·3 (0·6) 0·4 (0·8)
Functional comorbidity index score 1·3 (1·4) 1·4 (1·2)
Medical admission 59 (57%) 70 (66%)
Surgical admission 44 (43%) 36 (34%)
Admission category
Respiratory 18 (17%) 24 (23%)
Gastrointestinal or liver 7 (7%) 10 (9%)
Cardiovascular 17 (17%) 9 (8%)
Trauma 23 (22%) 23 (22%)
Sepsis 4 (4%) 4 (4%)
Obstetrics and gynaecology 0 1 (1%)
Neurological (non-trauma) 20 (19%) 21 (20%)
Other 14 (14%) 14 (13%)
Clinician pre-test suspicion of ventilator-associated pneumonia*
Low 10 (10%) 7 (7%)
Medium 33 (32%) 51 (48%)
High 59 (57%) 48 (45%)
Number of days in ICU before bronchoalveolar
lavage†
10·2 (8·7) 10·6 (10·4)
Confirmed ventilator-associated pneumonia‡38 (37%) 32 (30%)
Acute respiratory distress syndrome§
Mild (26·7–40·0 kPa) 11 (11%) 11 (10%)
Moderate (13·3–<26·7 kPa) 16 (16%) 11 (10%)
Severe (<13·3 kPa) 1 (1%) 5 (5%)
Vasopressors† 38 (37%) 37 (35%)
Renal replacement therapy 8 (8%) 4 (4%)
Use of corticosteroids 17 (17%) 15 (14%)
Receiving antibiotics at randomisation83 (81%) 87 (82%)
Temperature (°C)* 37·4 (1·0) 37·7 (0·9)
White cell count (× 10⁹/L) 14·4 (5·4) 15·5 (7·2)
C-reactive protein (mg/L)¶ 153·0 (97·9) 157·6 (107·3)
Positive end-expiratory pressure (cm H2O)|| 7·5 (2·9) 7·8 (2·6)
Peak airway pressure (cm H2O)** 20·5 (6·4) 21·3 (7·1)
PaO2:FiO2 (kPa)†† 29·1 (20·4–39·7) 25·3 (18·5–36·0)
Data are mean (SD), n (%), or median (IQR). APACHE=acute physiology and chronic health evaluation.
SOFA=sequential organ failure assessment. ICU=intensive care unit. *One patient from the biomarker-guided group
missing. †Three patients (one from the biomarker-guided group) missing. ‡One patient from the routine use of
antibiotics group missing. §Two patients (one from the biomarker-guided group) missing. ¶85 patients (43 from the
biomarker-guided group) missing. ||Two patients from the biomarker-guided group missing. **23 patients (eight from
the biomarker-guided group) missing. ††Seven patients (three from the biomarker-guided group) missing.
Table 1: Baseline characteristics
Articles
www.thelancet.com/respiratory Vol 8 February 2020 187
recommendation to discontinue antibiotics was followed
in four (24%) patients, and a false negative result was
obtainedin one (6%) patient.Microbiologicaldetails
relating to bronchoalveolar lavage fluid from the 17 patients
with a low IL-1β and IL-8 result (ie, those eligible for
antibiotic discontinuation) are shown in the appendix (p 8).
We observed no significant differences between the
groups for all other secondary outcomes (table 4). Results
for subgroup analyses,per-protocolanalyses, and
antibiotic-resistantinfections are shown in the
appendix (pp 10–17). Our two sensitivity analyses—one
treating death as equivalent to zero antibiotic-free days
and the other censoring at death in a discrete-time Cox
model—revealed no difference in the primary outcome
in the intention-to-treat population (appendix p 9).
Zero antibiotic-freedays was the most frequent
prescribing outcome (table 3). Median antibiotic days at
day 7 were 6 (IQR 4–7) in both groups (hazard ratio [HR]
0·84, 95% CI 0·63–1·12; table 4). We found no between-
group differences in antibiotic-free days at 14 days or
28 days (table 4). Reported indications for antibiotics
are described in the appendix (pp 18–19).
Numbers of patients with one or more reported adverse
events or serious adverse events are shown in table 5.
Details of adverse events and serious adverse events are
shown in the appendix (p 20). Bronchoalveolar lavage
was associated with a small, transient increase in oxygen
requirements (appendix p 21).
In the 13 patientsin whom the discontinuation
recommendation was not followed, our process evalu-
ation suggestedthat perceivedventilator-associated
pneu monia or hospital-acquired pneumonia was the
most common reason for antibiotic use. The process
evaluationidentifiedtwo broad potentiallynegative
influences on recruitment to the trial and compliance
with the trial intervention. The first of these influences
suggestedthat the chain involving identificationof
potential participants, preparation for bronchoalveolar
lavage, laboratory processing, and a clinician making a
judgement on the basis of the recommendation, intro-
duced many opportunitiesfor deviationfrom the
model. A breakdown in this sequence, at any stage,
negatively affected site performance and implement-
ation of the intervention.Second, we identified a
pattern such that low recruitment by units appeared to
correspondwith less use of bronchoalveolarlavage
in the diagnosisof ventilator-associatedpneumonia
outside the trial, a culture of not actively de-escalating
antibiotics, and the absence of so-called trial champions
(designated as having a particular interest in promoting
and delivering the trial within a given unit). These
same units also described a greater perception of risk
for bronchoalveolarlavage(favouringless invasive
methods) and for discontinuing antibiotics (favouring
antibiotic use as the perceived lower-risk approach). For
further details of the process evaluationsee the
appendix (pp 22–24).
Discussion
In the VAPrapid2 trial, a validated test with good rule-out
characteristics for ventilator-associated pneumonia did not
reduceantibioticuse or improveany of our other
investigated clinical outcomes. To our knowledge, this is
the first trial to use biomarkers to exclude ventilator-
associatedpneumoniato increaseconfidencein early
discontinuation of empirical antibiotics. Previous studies
have shown proof of principlefor modestantibiotic
reduction in suspected ventilator-associated pneumonia
using discontinuation rules.14,15 Serum procalcitonin has
been studiedwidelyin the ICU (outside thespecific
contextof ventilator-associatedpneumonia)and this
approachshowedvaryingsuccessfor safelyadjusting
antibiotic use.16–20However, procalcitonin is ineffective for
the exclusion of ventilator-associated pneumonia,21,22which
was the focus of our approach. Inconsistent effects of
procalcitonin on antibiotic use have also been des cribed
Ventilator-
associated
pneumonia
(≥10⁴ CFU/mL;
n=70)
Non-ventilator-
associated
pneumonia
(<10⁴ CFU/mL;
n=139)
Staphylococcus aureus 26 21*
Haemophilus spp 12 4
Escherichia coli 9 6
Pseudomonas aeruginosa 6 4
Klebsiella spp 5 15
Proteus mirabilis 5 3
Stenotrophomonas maltophilia3 5
Streptococcus pneumoniae3 1
Yeasts 3 13
Candida spp 2 17
Citrobacter spp 2 2
Enterobacter spp 2 8
Serratia marcescens 2 3
Staphylococcus spp 2 6
Streptococcus spp 2 2
Acinetobacter spp 1 2
Anaerobes 1 0
Coliform 1 3
Corynebacterium spp 1 0
Enterococcus spp 1 1
Gram-positive cocci 1 2
Moraxella catarrhalis 1 0
Prevotella spp 1 0
Aspergillus fumigatus 0 4
Burkholderia vietnamiensis0 1
Morganella morganii 0 2
Neisseria spp 0 1
Data are n of isolates (in some bronchoalveolar lavage samples, more than one
organism was isolated). 68 patients in the non-ventilator-associated pneumonia
column had no growth. CFU=colony-forming units. *In one case the organism
isolated was meticillin-resistant Staphylococcus aureus.
Table 2: Microorganisms isolated in bronchoalveolar lavage fluid
www.thelancet.com/respiratory Vol 8 February 2020 187
recommendation to discontinue antibiotics was followed
in four (24%) patients, and a false negative result was
obtainedin one (6%) patient.Microbiologicaldetails
relating to bronchoalveolar lavage fluid from the 17 patients
with a low IL-1β and IL-8 result (ie, those eligible for
antibiotic discontinuation) are shown in the appendix (p 8).
We observed no significant differences between the
groups for all other secondary outcomes (table 4). Results
for subgroup analyses,per-protocolanalyses, and
antibiotic-resistantinfections are shown in the
appendix (pp 10–17). Our two sensitivity analyses—one
treating death as equivalent to zero antibiotic-free days
and the other censoring at death in a discrete-time Cox
model—revealed no difference in the primary outcome
in the intention-to-treat population (appendix p 9).
Zero antibiotic-freedays was the most frequent
prescribing outcome (table 3). Median antibiotic days at
day 7 were 6 (IQR 4–7) in both groups (hazard ratio [HR]
0·84, 95% CI 0·63–1·12; table 4). We found no between-
group differences in antibiotic-free days at 14 days or
28 days (table 4). Reported indications for antibiotics
are described in the appendix (pp 18–19).
Numbers of patients with one or more reported adverse
events or serious adverse events are shown in table 5.
Details of adverse events and serious adverse events are
shown in the appendix (p 20). Bronchoalveolar lavage
was associated with a small, transient increase in oxygen
requirements (appendix p 21).
In the 13 patientsin whom the discontinuation
recommendation was not followed, our process evalu-
ation suggestedthat perceivedventilator-associated
pneu monia or hospital-acquired pneumonia was the
most common reason for antibiotic use. The process
evaluationidentifiedtwo broad potentiallynegative
influences on recruitment to the trial and compliance
with the trial intervention. The first of these influences
suggestedthat the chain involving identificationof
potential participants, preparation for bronchoalveolar
lavage, laboratory processing, and a clinician making a
judgement on the basis of the recommendation, intro-
duced many opportunitiesfor deviationfrom the
model. A breakdown in this sequence, at any stage,
negatively affected site performance and implement-
ation of the intervention.Second, we identified a
pattern such that low recruitment by units appeared to
correspondwith less use of bronchoalveolarlavage
in the diagnosisof ventilator-associatedpneumonia
outside the trial, a culture of not actively de-escalating
antibiotics, and the absence of so-called trial champions
(designated as having a particular interest in promoting
and delivering the trial within a given unit). These
same units also described a greater perception of risk
for bronchoalveolarlavage(favouringless invasive
methods) and for discontinuing antibiotics (favouring
antibiotic use as the perceived lower-risk approach). For
further details of the process evaluationsee the
appendix (pp 22–24).
Discussion
In the VAPrapid2 trial, a validated test with good rule-out
characteristics for ventilator-associated pneumonia did not
reduceantibioticuse or improveany of our other
investigated clinical outcomes. To our knowledge, this is
the first trial to use biomarkers to exclude ventilator-
associatedpneumoniato increaseconfidencein early
discontinuation of empirical antibiotics. Previous studies
have shown proof of principlefor modestantibiotic
reduction in suspected ventilator-associated pneumonia
using discontinuation rules.14,15 Serum procalcitonin has
been studiedwidelyin the ICU (outside thespecific
contextof ventilator-associatedpneumonia)and this
approachshowedvaryingsuccessfor safelyadjusting
antibiotic use.16–20However, procalcitonin is ineffective for
the exclusion of ventilator-associated pneumonia,21,22which
was the focus of our approach. Inconsistent effects of
procalcitonin on antibiotic use have also been des cribed
Ventilator-
associated
pneumonia
(≥10⁴ CFU/mL;
n=70)
Non-ventilator-
associated
pneumonia
(<10⁴ CFU/mL;
n=139)
Staphylococcus aureus 26 21*
Haemophilus spp 12 4
Escherichia coli 9 6
Pseudomonas aeruginosa 6 4
Klebsiella spp 5 15
Proteus mirabilis 5 3
Stenotrophomonas maltophilia3 5
Streptococcus pneumoniae3 1
Yeasts 3 13
Candida spp 2 17
Citrobacter spp 2 2
Enterobacter spp 2 8
Serratia marcescens 2 3
Staphylococcus spp 2 6
Streptococcus spp 2 2
Acinetobacter spp 1 2
Anaerobes 1 0
Coliform 1 3
Corynebacterium spp 1 0
Enterococcus spp 1 1
Gram-positive cocci 1 2
Moraxella catarrhalis 1 0
Prevotella spp 1 0
Aspergillus fumigatus 0 4
Burkholderia vietnamiensis0 1
Morganella morganii 0 2
Neisseria spp 0 1
Data are n of isolates (in some bronchoalveolar lavage samples, more than one
organism was isolated). 68 patients in the non-ventilator-associated pneumonia
column had no growth. CFU=colony-forming units. *In one case the organism
isolated was meticillin-resistant Staphylococcus aureus.
Table 2: Microorganisms isolated in bronchoalveolar lavage fluid
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Articles
188 www.thelancet.com/respiratory Vol 8 February 20
for lower respiratory tract infection outside the ICU.23,24
Enthusiasm for a procalcitonin strategy in the ICU is offset
by high non-compliance with procalcitonin guidance in
general, and durations of procalcitonin-guided antibi
use in ventilator-associated pneumonia that exceed
widely acceptedstandardof 8 days.3,4,15,25 Given that
confirmation of ventilator-associated pneumonia is low in
cases in which it is suspected,5 we reasoned that persuasive
earlyevidencefor the absenceof ventilator-associated
pneumoniamight have a greatereffecton antibiotic
duration. Proof of concept for this general strategy
been provided by a single-centre study that used p
liminary microbiology culture results to stop antibio
around 1 day after bronchoalveolar lavage.26
IL-1β and IL-8 fulfill the widely accepted criteria f
good exclusion test because they have a negative likeli
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Effect size* (95% CI)
Antibiotic days (7 days post-bronchoalveolar lavage)†6 (4–7) 6 (4–7) HR 0·84 (0·63 to 1·12)
Antibiotic days (14 days post-bronchoalveolar lavage)‡8 (6–12) 8 (5–11) HR 0·94 (0·69 to 1·28)
Antibiotic days (28 days post-bronchoalveolar lavage)§ 11 (7–15) 10 (5–15) HR 0·90 (0·65 to 1·25)
Antibiotic-free days (14 days post-bronchoalveolar lavage)‡ 6 (2–8) 6 (3–9) HR 1·13 (0·83 to 1·54)
Antibiotic-free days (28 days post-bronchoalveolar lavage)§ 17 (13–21) 18 (13–23) HR 1·01 (0·73 to 1·40)
Days of critical care stay¶ 14 (8–23) 14 (8–22) HR 1·00 (0·73 to 1·39)
Days of hospital stay|| 27 (16–58) 28 (12–50) HR 0·83 (0·60 to 1·15)
Days of level 3 (intensive care) stay¶ 10 (5–18) 10 (6–17) HR 1·05 (0·76 to 1·45)
Days of level 2 (high dependency) stay** 3 (1–8) 4 (1–7) HR 1·05 (0·74 to 1·48)
Mortality at 28 days†† 28 (27%) 21 (20%) OR 1·52 (0·78 to 2·98)
ICU mortality 25 (24%) 20 (19%) OR 1·35 (0·68 to 2·71)
Presence of antibiotic-associated infections to hospital
discharge, death, or 56 days††
6 (6%) 7 (7%) OR 0·86 (0·26 to 2·71)
SOFA score at 3 days‡‡ 4·3 (2·6) 4·4 (2·7) –0·18 (–0·87 to 0·52)
SOFA score at 7 days§§ 4·0 (2·8) 4·1 (2·7) –0·13 (–0·85 to 0·59)
SOFA score at 14 days§§ 3·7 (2·8) 3·6 (3·0) 0·00 (–0·76 to 0·77)
Ventilator-free days (at 28 days) 11 (0–19) 9 (0–19) RR 1·03 (0·94 to 1·12)
Number of antibiotic-resistant pathogens to hospital
discharge, death or 56 days††
0 (0–0) 0 (0–0) RR 1·71 (1·16 to 2·57)
Number of pathogens (outlier excluded) 0 (0–0) 0 (0–0) RR 1·36 (0·90 to 2·08)
Data are median (IQR), n (%), or mean (SD), unless otherwise indicated. The last row of the table excludes a single observation in the biomarker-g
having multiple pathogens (more than twice any other patient). HR=hazard ratio. ICU=intensive car e unit. OR=odds ratio. SOFA=sequential orga
RR=risk ratio. *Cox proportional hazards presented as HR, logistic regression presented as OR, linear regression presented as mean difference, an
presented as RR. †Two patients (one from the biomarker-guided group) missing. ‡21 patients (11 from the biomarker-guided group) missing. §34
biomarker-guided group) missing. ¶Six patients (three from the biomarker-guided group) missing. ||Five patients (two from the biomarker-guided
**61 patients (30 from the biomarker-guided group) missing. ††One patient from the biomarker-guided group missing. ‡‡12 patients (five from the
group) missing. §§Eight patients (three from the biomarker-guided group) missing.
Table 4: Secondary outcome measures
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Adverse event or serious adverse event reported43 (42%) 37 (35%)
Adverse event recorded 39 (91%) 35 (95%)
Serious adverse event recorded 4 (9%) 2 (5%)
Data are number of patients (%); multiple events were reported in some patients.
Table 5: Patients with reported adverse events or serious adverse events
0 1 2 3 4 5 6 7
Intention-to-treat analysis
Biomarker-guided recommendation on antibiotics group (n=102)50 (49%)13 (13%) 7 (7%) 10 (10%)7 (7%) 3 (3%) 4 (4%) 8 (8%)
Routine use of antibiotics group (n=105) 40 (38%)14 (13%)13 (12%)18 (17%)6 (6%) 4 (4%) 4 (4%) 6 (6%)
Per-protocol analysis
Biomarker-guided recommendation on antibiotics group (n=80)42 (53%)10 (13%) 7 (9%) 5 (6%) 6 (8%) 1 (1%) 3 (4%) 6 (8%)
Routine use of antibiotics group (n=105) 40 (38%)14 (13%)13 (12%)18 (17%)6 (6%) 4 (4%) 4 (4%) 6 (6%)
Data are n (%).
Table 3: Antibiotic-free days for the intention-to-treat and per-protocol analyses
188 www.thelancet.com/respiratory Vol 8 February 20
for lower respiratory tract infection outside the ICU.23,24
Enthusiasm for a procalcitonin strategy in the ICU is offset
by high non-compliance with procalcitonin guidance in
general, and durations of procalcitonin-guided antibi
use in ventilator-associated pneumonia that exceed
widely acceptedstandardof 8 days.3,4,15,25 Given that
confirmation of ventilator-associated pneumonia is low in
cases in which it is suspected,5 we reasoned that persuasive
earlyevidencefor the absenceof ventilator-associated
pneumoniamight have a greatereffecton antibiotic
duration. Proof of concept for this general strategy
been provided by a single-centre study that used p
liminary microbiology culture results to stop antibio
around 1 day after bronchoalveolar lavage.26
IL-1β and IL-8 fulfill the widely accepted criteria f
good exclusion test because they have a negative likeli
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Effect size* (95% CI)
Antibiotic days (7 days post-bronchoalveolar lavage)†6 (4–7) 6 (4–7) HR 0·84 (0·63 to 1·12)
Antibiotic days (14 days post-bronchoalveolar lavage)‡8 (6–12) 8 (5–11) HR 0·94 (0·69 to 1·28)
Antibiotic days (28 days post-bronchoalveolar lavage)§ 11 (7–15) 10 (5–15) HR 0·90 (0·65 to 1·25)
Antibiotic-free days (14 days post-bronchoalveolar lavage)‡ 6 (2–8) 6 (3–9) HR 1·13 (0·83 to 1·54)
Antibiotic-free days (28 days post-bronchoalveolar lavage)§ 17 (13–21) 18 (13–23) HR 1·01 (0·73 to 1·40)
Days of critical care stay¶ 14 (8–23) 14 (8–22) HR 1·00 (0·73 to 1·39)
Days of hospital stay|| 27 (16–58) 28 (12–50) HR 0·83 (0·60 to 1·15)
Days of level 3 (intensive care) stay¶ 10 (5–18) 10 (6–17) HR 1·05 (0·76 to 1·45)
Days of level 2 (high dependency) stay** 3 (1–8) 4 (1–7) HR 1·05 (0·74 to 1·48)
Mortality at 28 days†† 28 (27%) 21 (20%) OR 1·52 (0·78 to 2·98)
ICU mortality 25 (24%) 20 (19%) OR 1·35 (0·68 to 2·71)
Presence of antibiotic-associated infections to hospital
discharge, death, or 56 days††
6 (6%) 7 (7%) OR 0·86 (0·26 to 2·71)
SOFA score at 3 days‡‡ 4·3 (2·6) 4·4 (2·7) –0·18 (–0·87 to 0·52)
SOFA score at 7 days§§ 4·0 (2·8) 4·1 (2·7) –0·13 (–0·85 to 0·59)
SOFA score at 14 days§§ 3·7 (2·8) 3·6 (3·0) 0·00 (–0·76 to 0·77)
Ventilator-free days (at 28 days) 11 (0–19) 9 (0–19) RR 1·03 (0·94 to 1·12)
Number of antibiotic-resistant pathogens to hospital
discharge, death or 56 days††
0 (0–0) 0 (0–0) RR 1·71 (1·16 to 2·57)
Number of pathogens (outlier excluded) 0 (0–0) 0 (0–0) RR 1·36 (0·90 to 2·08)
Data are median (IQR), n (%), or mean (SD), unless otherwise indicated. The last row of the table excludes a single observation in the biomarker-g
having multiple pathogens (more than twice any other patient). HR=hazard ratio. ICU=intensive car e unit. OR=odds ratio. SOFA=sequential orga
RR=risk ratio. *Cox proportional hazards presented as HR, logistic regression presented as OR, linear regression presented as mean difference, an
presented as RR. †Two patients (one from the biomarker-guided group) missing. ‡21 patients (11 from the biomarker-guided group) missing. §34
biomarker-guided group) missing. ¶Six patients (three from the biomarker-guided group) missing. ||Five patients (two from the biomarker-guided
**61 patients (30 from the biomarker-guided group) missing. ††One patient from the biomarker-guided group missing. ‡‡12 patients (five from the
group) missing. §§Eight patients (three from the biomarker-guided group) missing.
Table 4: Secondary outcome measures
Biomarker-guided
recommendation on
antibiotics group (n=103)
Routine use of antibiotics
group (n=106)
Adverse event or serious adverse event reported43 (42%) 37 (35%)
Adverse event recorded 39 (91%) 35 (95%)
Serious adverse event recorded 4 (9%) 2 (5%)
Data are number of patients (%); multiple events were reported in some patients.
Table 5: Patients with reported adverse events or serious adverse events
0 1 2 3 4 5 6 7
Intention-to-treat analysis
Biomarker-guided recommendation on antibiotics group (n=102)50 (49%)13 (13%) 7 (7%) 10 (10%)7 (7%) 3 (3%) 4 (4%) 8 (8%)
Routine use of antibiotics group (n=105) 40 (38%)14 (13%)13 (12%)18 (17%)6 (6%) 4 (4%) 4 (4%) 6 (6%)
Per-protocol analysis
Biomarker-guided recommendation on antibiotics group (n=80)42 (53%)10 (13%) 7 (9%) 5 (6%) 6 (8%) 1 (1%) 3 (4%) 6 (8%)
Routine use of antibiotics group (n=105) 40 (38%)14 (13%)13 (12%)18 (17%)6 (6%) 4 (4%) 4 (4%) 6 (6%)
Data are n (%).
Table 3: Antibiotic-free days for the intention-to-treat and per-protocol analyses
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
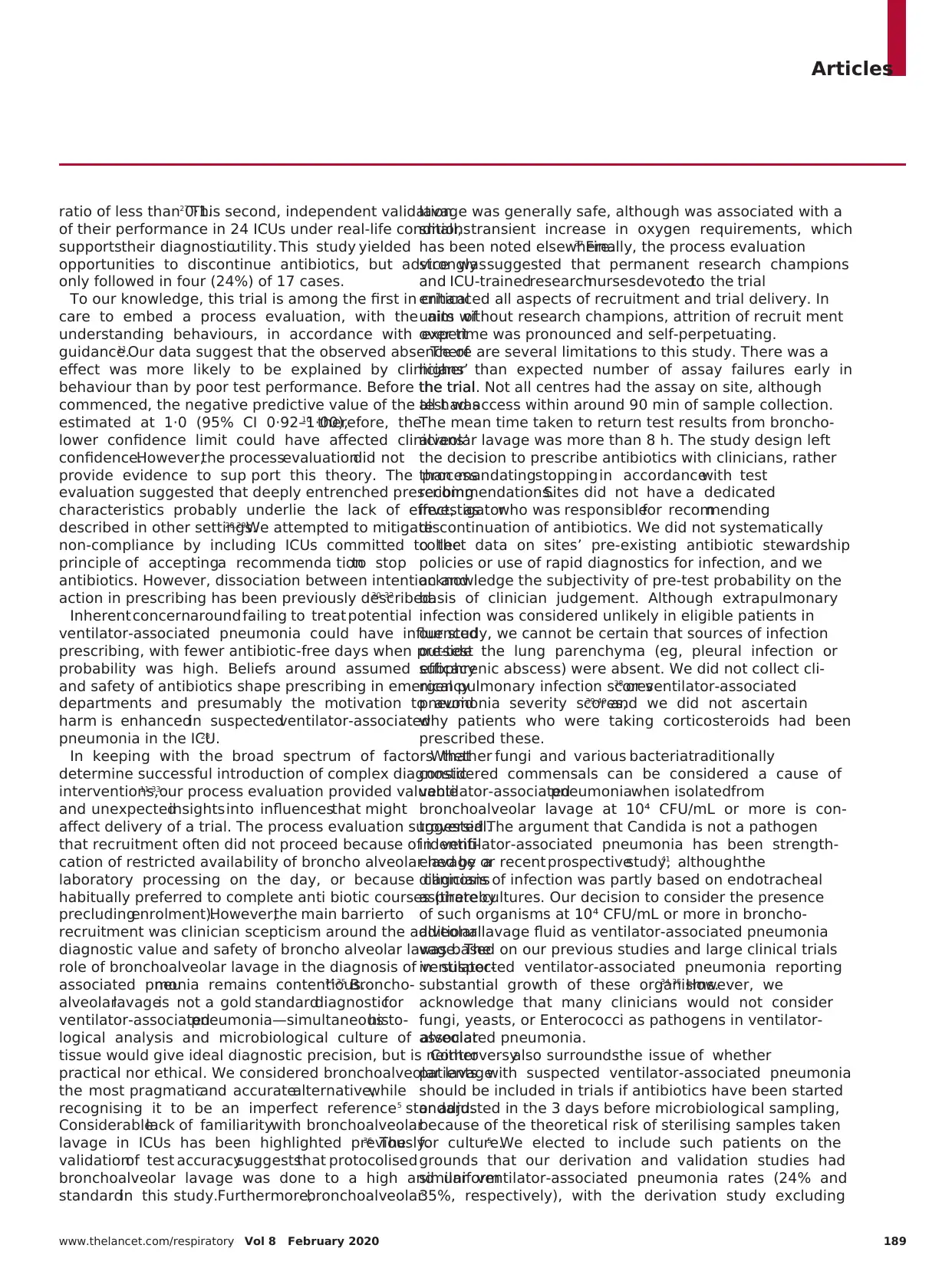
Articles
www.thelancet.com/respiratory Vol 8 February 2020 189
ratio of less than 0·1.27 This second, independent validation
of their performance in 24 ICUs under real-life conditions
supportstheir diagnosticutility. This study yielded
opportunities to discontinue antibiotics, but advice was
only followed in four (24%) of 17 cases.
To our knowledge, this trial is among the first in critical
care to embed a process evaluation, with the aim of
understanding behaviours, in accordance with expert
guidance.11 Our data suggest that the observed absence of
effect was more likely to be explained by clinicians’
behaviour than by poor test performance. Before the trial
commenced, the negative predictive value of the test was
estimated at 1·0 (95% CI 0·92–1·00),10 therefore, the
lower confidence limit could have affected clinicians’
confidence.However,the processevaluationdid not
provide evidence to sup port this theory. The process
evaluation suggested that deeply entrenched prescribing
characteristics probably underlie the lack of effect, as
described in other settings.28,29We attempted to mitigate
non-compliance by including ICUs committed to the
principle of acceptinga recommenda tionto stop
antibiotics. However, dissociation between intention and
action in prescribing has been previously described.30–32
Inherent concernaround failing to treat potential
ventilator-associated pneumonia could have influenced
prescribing, with fewer antibiotic-free days when pre-test
probability was high. Beliefs around assumed efficacy
and safety of antibiotics shape prescribing in emergency
departments and presumably the motivation to avoid
harm is enhancedin suspectedventilator-associated
pneumonia in the ICU.28
In keeping with the broad spectrum of factors that
determine successful introduction of complex diagnostic
interventions,11,33
our process evaluation provided valuable
and unexpectedinsights into influencesthat might
affect delivery of a trial. The process evaluation suggested
that recruitment often did not proceed because of identifi-
cation of restricted availability of broncho alveolar lavage or
laboratory processing on the day, or because clinicians
habitually preferred to complete anti biotic courses (thereby
precludingenrolment).However,the main barrierto
recruitment was clinician scepticism around the additional
diagnostic value and safety of broncho alveolar lavage. The
role of bronchoalveolar lavage in the diagnosis of ventilator-
associated pneumonia remains contentious.34,35 Broncho-
alveolarlavageis not a gold standarddiagnosticfor
ventilator-associatedpneumonia—simultaneoushisto-
logical analysis and microbiological culture of alveolar
tissue would give ideal diagnostic precision, but is neither
practical nor ethical. We considered bronchoalveolar lavage
the most pragmaticand accuratealternative,while
recognising it to be an imperfect reference standard.5
Considerablelack of familiaritywith bronchoalveolar
lavage in ICUs has been highlighted previously.36 The
validationof test accuracysuggeststhat protocolised
bronchoalveolar lavage was done to a high and uniform
standardin this study.Furthermore,bronchoalveolar
lavage was generally safe, although was associated with a
small, transient increase in oxygen requirements, which
has been noted elsewhere.37 Finally, the process evaluation
strongly suggested that permanent research champions
and ICU-trainedresearchnursesdevotedto the trial
enhanced all aspects of recruitment and trial delivery. In
units without research champions, attrition of recruit ment
over time was pronounced and self-perpetuating.
There are several limitations to this study. There was a
higher than expected number of assay failures early in
the trial. Not all centres had the assay on site, although
all had access within around 90 min of sample collection.
The mean time taken to return test results from broncho-
alveolar lavage was more than 8 h. The study design left
the decision to prescribe antibiotics with clinicians, rather
than mandatingstopping in accordancewith test
recommendations.Sites did not have a dedicated
investigatorwho was responsiblefor recommending
discontinuation of antibiotics. We did not systematically
collect data on sites’ pre-existing antibiotic stewardship
policies or use of rapid diagnostics for infection, and we
acknowledge the subjectivity of pre-test probability on the
basis of clinician judgement. Although extrapulmonary
infection was considered unlikely in eligible patients in
our study, we cannot be certain that sources of infection
outside the lung parenchyma (eg, pleural infection or
subphrenic abscess) were absent. We did not collect cli-
nical pulmonary infection scores38 or ventilator-associated
pneumonia severity scores,39,40 and we did not ascertain
why patients who were taking corticosteroids had been
prescribed these.
Whether fungi and various bacteriatraditionally
considered commensals can be considered a cause of
ventilator-associatedpneumoniawhen isolatedfrom
bronchoalveolar lavage at 10⁴ CFU/mL or more is con-
troversial.5 The argument that Candida is not a pathogen
in ventilator-associated pneumonia has been strength-
ened by a recent prospectivestudy,41 althoughthe
diagnosis of infection was partly based on endotracheal
aspirate cultures. Our decision to consider the presence
of such organisms at 10⁴ CFU/mL or more in broncho-
alveolar lavage fluid as ventilator-associated pneumonia
was based on our previous studies and large clinical trials
in suspected ventilator-associated pneumonia reporting
substantial growth of these organisms.34,35 However, we
acknowledge that many clinicians would not consider
fungi, yeasts, or Enterococci as pathogens in ventilator-
associated pneumonia.
Controversyalso surroundsthe issue of whether
patients with suspected ventilator-associated pneumonia
should be included in trials if antibiotics have been started
or adjusted in the 3 days before microbiological sampling,
because of the theoretical risk of sterilising samples taken
for culture.5 We elected to include such patients on the
grounds that our derivation and validation studies had
similar ventilator-associated pneumonia rates (24% and
35%, respectively), with the derivation study excluding
www.thelancet.com/respiratory Vol 8 February 2020 189
ratio of less than 0·1.27 This second, independent validation
of their performance in 24 ICUs under real-life conditions
supportstheir diagnosticutility. This study yielded
opportunities to discontinue antibiotics, but advice was
only followed in four (24%) of 17 cases.
To our knowledge, this trial is among the first in critical
care to embed a process evaluation, with the aim of
understanding behaviours, in accordance with expert
guidance.11 Our data suggest that the observed absence of
effect was more likely to be explained by clinicians’
behaviour than by poor test performance. Before the trial
commenced, the negative predictive value of the test was
estimated at 1·0 (95% CI 0·92–1·00),10 therefore, the
lower confidence limit could have affected clinicians’
confidence.However,the processevaluationdid not
provide evidence to sup port this theory. The process
evaluation suggested that deeply entrenched prescribing
characteristics probably underlie the lack of effect, as
described in other settings.28,29We attempted to mitigate
non-compliance by including ICUs committed to the
principle of acceptinga recommenda tionto stop
antibiotics. However, dissociation between intention and
action in prescribing has been previously described.30–32
Inherent concernaround failing to treat potential
ventilator-associated pneumonia could have influenced
prescribing, with fewer antibiotic-free days when pre-test
probability was high. Beliefs around assumed efficacy
and safety of antibiotics shape prescribing in emergency
departments and presumably the motivation to avoid
harm is enhancedin suspectedventilator-associated
pneumonia in the ICU.28
In keeping with the broad spectrum of factors that
determine successful introduction of complex diagnostic
interventions,11,33
our process evaluation provided valuable
and unexpectedinsights into influencesthat might
affect delivery of a trial. The process evaluation suggested
that recruitment often did not proceed because of identifi-
cation of restricted availability of broncho alveolar lavage or
laboratory processing on the day, or because clinicians
habitually preferred to complete anti biotic courses (thereby
precludingenrolment).However,the main barrierto
recruitment was clinician scepticism around the additional
diagnostic value and safety of broncho alveolar lavage. The
role of bronchoalveolar lavage in the diagnosis of ventilator-
associated pneumonia remains contentious.34,35 Broncho-
alveolarlavageis not a gold standarddiagnosticfor
ventilator-associatedpneumonia—simultaneoushisto-
logical analysis and microbiological culture of alveolar
tissue would give ideal diagnostic precision, but is neither
practical nor ethical. We considered bronchoalveolar lavage
the most pragmaticand accuratealternative,while
recognising it to be an imperfect reference standard.5
Considerablelack of familiaritywith bronchoalveolar
lavage in ICUs has been highlighted previously.36 The
validationof test accuracysuggeststhat protocolised
bronchoalveolar lavage was done to a high and uniform
standardin this study.Furthermore,bronchoalveolar
lavage was generally safe, although was associated with a
small, transient increase in oxygen requirements, which
has been noted elsewhere.37 Finally, the process evaluation
strongly suggested that permanent research champions
and ICU-trainedresearchnursesdevotedto the trial
enhanced all aspects of recruitment and trial delivery. In
units without research champions, attrition of recruit ment
over time was pronounced and self-perpetuating.
There are several limitations to this study. There was a
higher than expected number of assay failures early in
the trial. Not all centres had the assay on site, although
all had access within around 90 min of sample collection.
The mean time taken to return test results from broncho-
alveolar lavage was more than 8 h. The study design left
the decision to prescribe antibiotics with clinicians, rather
than mandatingstopping in accordancewith test
recommendations.Sites did not have a dedicated
investigatorwho was responsiblefor recommending
discontinuation of antibiotics. We did not systematically
collect data on sites’ pre-existing antibiotic stewardship
policies or use of rapid diagnostics for infection, and we
acknowledge the subjectivity of pre-test probability on the
basis of clinician judgement. Although extrapulmonary
infection was considered unlikely in eligible patients in
our study, we cannot be certain that sources of infection
outside the lung parenchyma (eg, pleural infection or
subphrenic abscess) were absent. We did not collect cli-
nical pulmonary infection scores38 or ventilator-associated
pneumonia severity scores,39,40 and we did not ascertain
why patients who were taking corticosteroids had been
prescribed these.
Whether fungi and various bacteriatraditionally
considered commensals can be considered a cause of
ventilator-associatedpneumoniawhen isolatedfrom
bronchoalveolar lavage at 10⁴ CFU/mL or more is con-
troversial.5 The argument that Candida is not a pathogen
in ventilator-associated pneumonia has been strength-
ened by a recent prospectivestudy,41 althoughthe
diagnosis of infection was partly based on endotracheal
aspirate cultures. Our decision to consider the presence
of such organisms at 10⁴ CFU/mL or more in broncho-
alveolar lavage fluid as ventilator-associated pneumonia
was based on our previous studies and large clinical trials
in suspected ventilator-associated pneumonia reporting
substantial growth of these organisms.34,35 However, we
acknowledge that many clinicians would not consider
fungi, yeasts, or Enterococci as pathogens in ventilator-
associated pneumonia.
Controversyalso surroundsthe issue of whether
patients with suspected ventilator-associated pneumonia
should be included in trials if antibiotics have been started
or adjusted in the 3 days before microbiological sampling,
because of the theoretical risk of sterilising samples taken
for culture.5 We elected to include such patients on the
grounds that our derivation and validation studies had
similar ventilator-associated pneumonia rates (24% and
35%, respectively), with the derivation study excluding
Articles
190 www.thelancet.com/respiratory Vol 8 February 20
and the validation study including such patients. The
similar ventilator-associatedpneumoniarate in the
current study (34%) provides evidence that inclusion of
such patients did not materially alter ventilator-associated
pneumoniarates.However,althoughthere was only
one false negative result iden tified for our test, it remains
theoretically possible that bronchoalveolar lavage fluid
samples might be sterile for technical reasons, such as
inadequate sampling or delays in analysis, as has been
described for blood cultures.42,43We attempted to mitigate
this risk by implementing a protocolised bronchoalveolar
lavage, ensuring timely delivery of samples and having
quality control checks within the biomarker assay.
Finally, landmarkstudies of blood biomarkersof
infection have taken advantage of changes in diagnostic
parameters over serial timepoints.16,19,44This study was
confined to a single timepoint based on our previous data,
the desire to provide results well before bronchoalveolar
lavage fluid culture results were available to clinicians,
and becausethe mild inflammationassociatedwith
bronchoalveolarlavagewould confoundresults from
subsequent lavages. However, we cannot be certain that
we used the optimum timepoint(s) for sampling.
In conclusion, biomarker-guidedexclusion of
ventilator-associated pneumonia did not reduce antibiotic
use in centres that had committed to following test
recom mendations.Processevaluationsuggestedthat
lack of adoption of the technology and clinician behaviour
had a greater influence on trial outcomes than did test
performance. Antibiotic prescribing behaviours appear
entrenched and recalcitrant to change. Future trials of
diagnostictests for ventilator-associatedpneumonia
should incorporate detailed implementation strategies
informed by prior characterisationof factors that
influence prescribing and diagnostic decision making.
Contributors
TSW, DFM, NA (the study statistician), ACM, SS, GDP, RM, CMO’K,
DWJK, and AJS designed the study. DFM, TSW, NA, ACM, SS, GDP,
RM, CMO’K, DWJK, and AJS secured funding for the study. TPH
coordinated the study. JP was the trial manager for the study. SAB was
the trial project manager. RM provided microbiological support for the
study. LME and BB designed the process evaluation for the study. TPH,
DFM, TSW, ACM, SS, PD, AIR, GDP, LME, SEW, KK, SVB, RLP, AJR,
AA, JB-S, NMR, IDW, CB, BY, CS, SKL, JH, SB, VL, and JSo collected
the data. TVDB and GB analysed laboratory data and supervised quality
control for assays. JSc did laboratory assays. TPH, NA, AJA, GP, and AJS
analysed the data. TPH, DFM, TSW, ACM, SS, PD, GDP, LME, BB, AA,
AJA, GP, and AJS interpreted the data. TPH, DFM, TSW, NA, ACM, SS,
PD, GDP, LME, and AJS wrote the manuscript. All authors revised the
manuscript and approved the final version for publication.
Declaration of interests
DFM reports a grant from the Wellcome Trust and UK Department of
Health (for the conduct of the study); personal fees from consultancy for
GlaxoSmithKline, Boehringer Ingelheim, and Bayer, all outside of the
current work; that his institution has received funds from grants from
the UK National Institute for Health Research (NIHR), Wellcome Trust,
Innovate UK, the UK Medical Research Council, Northern Ireland Health
and Social Care Research and Development Division Research, the
National Institutes of Health, and the Health Research Board (Ireland);
and that he is a Director of Research for the Intensive Care Society and
Programme Director of the NIHR Efficacy and Mechanism Evaluation
programme. TSW reports a grant from the Wellcome Trust and UK
Department of Health (for the conduct of the study). ACM is a member
of the advisory board for Serendex Pharmaceuticals. SS has received fee
from Ambu for key opinion leader meetings. PD reports clinical advisory
board membership with DNA Electronics and receipt of grants relating to
sepsis and severe infection from the UK NIHR, all outside of the
submitted work. CMO’K reports a grant from the Wellcome Trust and
UK Department of Health (for the conduct of the study); and that her
spouse has received personal fees from consultancy for GlaxoSmithKline
Boehringer Ingelheim, and Bayer, outside of the submitted work.
TVDB, GB, and DWJK were employees of Becton Dickinson Biosciences
during the study. AJS reports a grant from the Wellcome Trust and
UK Department of Health (for the conduct of the study); that his
institution has received funds from grants surrounding sepsis and
pneumonia from the UK Medical Research Council, and UK NIHR; and
that he is Director of the NIHR Newcastle In Vitro Diagnostics
Co-operative. All other authors declare no competing interests.
Data sharing
Data collected for this study will be made available (in the form of any o
all from the de-identified data on the study database, study protocol,
statistical analysis plan, and analytic code) to researchers who provide a
methodologically sound research proposal, to assist with achievement o
aims in the approved proposal. Data will be available from the time of
publication of the Article in print. Proposals should be directed to the
Newcastle Clinical Trials Unit.
Acknowledgments
This publication presents independent research supported by the
Health Innovation Challenge Fund (HICF-510-078; 094949/Z/10/X), a
parallel funding partnership between the UK Department of Health
and Wellcome Trust. The views expressed in this publication are those
of the authors and not necessarily those of the UK Department of
Health or Wellcome Trust. The study was also supported by the
National Institute for Health Research (NIHR) Newcastle Biomedical
Research Centre (IS-BRC-1215-20001) and the Medical Research
Council SHIELD antimicrobial resistance consortium (MR/
N02995X/1). ACM is supported by a Clinical Research Career
Development Fellowship from the Wellcome Trust
(WT 2055214/Z/16/Z). GDP is an NIHR Senior Investigator. Trial
delivery was supported by the NIHR National Clinical Research
Network in Critical Care, the Northern Ireland Clinical Research
Network, and the UK Intensive Care Foundation.
References
1 Magill SS, Edwards JR, Bamberg W, et al. Multistate
point-prevalence survey of health care-associated infections.
N Engl J Med 2014; 370: 1198–208.
2 Blot S, Koulenti D, Dimopoulos G, et al. Prevalence, risk factors,
and mortality for ventilator-associated pneumonia in middle-aged,
old, and very old critically ill patients. Crit Care Med 2014;
42: 601–09.
3 Kalil AC, Metersky ML, Klompas M, et al. Management of adults
with hospital-acquired and ventilator-associated pneumonia:
2016 Clinical Practice Guidelines by the Infectious Diseases Society
of America and the American Thoracic Society. Clin Infect Dis 2016;
63: e61–111.
4 Torres A, Niederman MS, Chastre J, et al. International
ERS/ESICM/ESCMID/ALAT guidelines for the management of
hospital-acquired pneumonia and ventilator-associated pneumonia:
guidelines for the management of hospital-acquired pneumonia
(HAP)/ventilator-associated pneumonia (VAP) of the European
Respiratory Society (ERS), European Society of Intensive Care
Medicine (ESICM), European Society of Clinical Microbiology and
Infectious Diseases (ESCMID) and Asociación Latinoamericana del
Tórax (ALAT). Eur Respir J 2017; 50: 1700582.
5 Chastre J, Fagon JY. Ventilator-associated pneumonia.
Am J Respir Crit Care Med 2002; 165: 867–903.
6 Vincent JL, Rello J, Marshall J, et al. International study of the
prevalence and outcomes of infection in intensive care units. JAMA
2009; 302: 2323–29.
7 Hanberger H, Arman D, Gill H, et al. Surveillance of microbial
resistance in European Intensive Care Units: a first report from the
Care-ICU programme for improved infection control.
Intensive Care Med 2009; 35: 91–100.
astle
ee
nctu/
190 www.thelancet.com/respiratory Vol 8 February 20
and the validation study including such patients. The
similar ventilator-associatedpneumoniarate in the
current study (34%) provides evidence that inclusion of
such patients did not materially alter ventilator-associated
pneumoniarates.However,althoughthere was only
one false negative result iden tified for our test, it remains
theoretically possible that bronchoalveolar lavage fluid
samples might be sterile for technical reasons, such as
inadequate sampling or delays in analysis, as has been
described for blood cultures.42,43We attempted to mitigate
this risk by implementing a protocolised bronchoalveolar
lavage, ensuring timely delivery of samples and having
quality control checks within the biomarker assay.
Finally, landmarkstudies of blood biomarkersof
infection have taken advantage of changes in diagnostic
parameters over serial timepoints.16,19,44This study was
confined to a single timepoint based on our previous data,
the desire to provide results well before bronchoalveolar
lavage fluid culture results were available to clinicians,
and becausethe mild inflammationassociatedwith
bronchoalveolarlavagewould confoundresults from
subsequent lavages. However, we cannot be certain that
we used the optimum timepoint(s) for sampling.
In conclusion, biomarker-guidedexclusion of
ventilator-associated pneumonia did not reduce antibiotic
use in centres that had committed to following test
recom mendations.Processevaluationsuggestedthat
lack of adoption of the technology and clinician behaviour
had a greater influence on trial outcomes than did test
performance. Antibiotic prescribing behaviours appear
entrenched and recalcitrant to change. Future trials of
diagnostictests for ventilator-associatedpneumonia
should incorporate detailed implementation strategies
informed by prior characterisationof factors that
influence prescribing and diagnostic decision making.
Contributors
TSW, DFM, NA (the study statistician), ACM, SS, GDP, RM, CMO’K,
DWJK, and AJS designed the study. DFM, TSW, NA, ACM, SS, GDP,
RM, CMO’K, DWJK, and AJS secured funding for the study. TPH
coordinated the study. JP was the trial manager for the study. SAB was
the trial project manager. RM provided microbiological support for the
study. LME and BB designed the process evaluation for the study. TPH,
DFM, TSW, ACM, SS, PD, AIR, GDP, LME, SEW, KK, SVB, RLP, AJR,
AA, JB-S, NMR, IDW, CB, BY, CS, SKL, JH, SB, VL, and JSo collected
the data. TVDB and GB analysed laboratory data and supervised quality
control for assays. JSc did laboratory assays. TPH, NA, AJA, GP, and AJS
analysed the data. TPH, DFM, TSW, ACM, SS, PD, GDP, LME, BB, AA,
AJA, GP, and AJS interpreted the data. TPH, DFM, TSW, NA, ACM, SS,
PD, GDP, LME, and AJS wrote the manuscript. All authors revised the
manuscript and approved the final version for publication.
Declaration of interests
DFM reports a grant from the Wellcome Trust and UK Department of
Health (for the conduct of the study); personal fees from consultancy for
GlaxoSmithKline, Boehringer Ingelheim, and Bayer, all outside of the
current work; that his institution has received funds from grants from
the UK National Institute for Health Research (NIHR), Wellcome Trust,
Innovate UK, the UK Medical Research Council, Northern Ireland Health
and Social Care Research and Development Division Research, the
National Institutes of Health, and the Health Research Board (Ireland);
and that he is a Director of Research for the Intensive Care Society and
Programme Director of the NIHR Efficacy and Mechanism Evaluation
programme. TSW reports a grant from the Wellcome Trust and UK
Department of Health (for the conduct of the study). ACM is a member
of the advisory board for Serendex Pharmaceuticals. SS has received fee
from Ambu for key opinion leader meetings. PD reports clinical advisory
board membership with DNA Electronics and receipt of grants relating to
sepsis and severe infection from the UK NIHR, all outside of the
submitted work. CMO’K reports a grant from the Wellcome Trust and
UK Department of Health (for the conduct of the study); and that her
spouse has received personal fees from consultancy for GlaxoSmithKline
Boehringer Ingelheim, and Bayer, outside of the submitted work.
TVDB, GB, and DWJK were employees of Becton Dickinson Biosciences
during the study. AJS reports a grant from the Wellcome Trust and
UK Department of Health (for the conduct of the study); that his
institution has received funds from grants surrounding sepsis and
pneumonia from the UK Medical Research Council, and UK NIHR; and
that he is Director of the NIHR Newcastle In Vitro Diagnostics
Co-operative. All other authors declare no competing interests.
Data sharing
Data collected for this study will be made available (in the form of any o
all from the de-identified data on the study database, study protocol,
statistical analysis plan, and analytic code) to researchers who provide a
methodologically sound research proposal, to assist with achievement o
aims in the approved proposal. Data will be available from the time of
publication of the Article in print. Proposals should be directed to the
Newcastle Clinical Trials Unit.
Acknowledgments
This publication presents independent research supported by the
Health Innovation Challenge Fund (HICF-510-078; 094949/Z/10/X), a
parallel funding partnership between the UK Department of Health
and Wellcome Trust. The views expressed in this publication are those
of the authors and not necessarily those of the UK Department of
Health or Wellcome Trust. The study was also supported by the
National Institute for Health Research (NIHR) Newcastle Biomedical
Research Centre (IS-BRC-1215-20001) and the Medical Research
Council SHIELD antimicrobial resistance consortium (MR/
N02995X/1). ACM is supported by a Clinical Research Career
Development Fellowship from the Wellcome Trust
(WT 2055214/Z/16/Z). GDP is an NIHR Senior Investigator. Trial
delivery was supported by the NIHR National Clinical Research
Network in Critical Care, the Northern Ireland Clinical Research
Network, and the UK Intensive Care Foundation.
References
1 Magill SS, Edwards JR, Bamberg W, et al. Multistate
point-prevalence survey of health care-associated infections.
N Engl J Med 2014; 370: 1198–208.
2 Blot S, Koulenti D, Dimopoulos G, et al. Prevalence, risk factors,
and mortality for ventilator-associated pneumonia in middle-aged,
old, and very old critically ill patients. Crit Care Med 2014;
42: 601–09.
3 Kalil AC, Metersky ML, Klompas M, et al. Management of adults
with hospital-acquired and ventilator-associated pneumonia:
2016 Clinical Practice Guidelines by the Infectious Diseases Society
of America and the American Thoracic Society. Clin Infect Dis 2016;
63: e61–111.
4 Torres A, Niederman MS, Chastre J, et al. International
ERS/ESICM/ESCMID/ALAT guidelines for the management of
hospital-acquired pneumonia and ventilator-associated pneumonia:
guidelines for the management of hospital-acquired pneumonia
(HAP)/ventilator-associated pneumonia (VAP) of the European
Respiratory Society (ERS), European Society of Intensive Care
Medicine (ESICM), European Society of Clinical Microbiology and
Infectious Diseases (ESCMID) and Asociación Latinoamericana del
Tórax (ALAT). Eur Respir J 2017; 50: 1700582.
5 Chastre J, Fagon JY. Ventilator-associated pneumonia.
Am J Respir Crit Care Med 2002; 165: 867–903.
6 Vincent JL, Rello J, Marshall J, et al. International study of the
prevalence and outcomes of infection in intensive care units. JAMA
2009; 302: 2323–29.
7 Hanberger H, Arman D, Gill H, et al. Surveillance of microbial
resistance in European Intensive Care Units: a first report from the
Care-ICU programme for improved infection control.
Intensive Care Med 2009; 35: 91–100.
astle
ee
nctu/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Articles
www.thelancet.com/respiratory Vol 8 February 2020 191
8 Kett DH, Cano E, Quartin AA, et al. Implementation of guidelines
for management of possible multidrug-resistant pneumonia in
intensive care: an observational, multicentre cohort study.
Lancet Infect Dis 2011; 11: 181–89.
9 Conway Morris A, Kefala K, Wilkinson TS, et al. Diagnostic
importance of pulmonary interleukin-1β and interleukin-8 in
ventilator-associated pneumonia. Thorax 2010; 65: 201–07.
10 Hellyer TP, Morris AC, McAuley DF, et al. Diagnostic accuracy of
pulmonary host inflammatory mediators in the exclusion of
ventilator-acquired pneumonia. Thorax 2015; 70: 41–47.
11 Moore GF, Audrey S, Barker M, et al. Process evaluation of complex
interventions: Medical Research Council guidance. BMJ 2015;
350: h1258.
12 Hellyer TP, Anderson NA, Parker J, et al. Effectiveness of
biomarker-based exclusion of ventilator-acquired pneumonia to
reduce antibiotic use (VAPrapid-2): study protocol for a randomised
controlled trial. Trials 2016; 17: 318.
13 Meduri GU, Chastre J. The standardization of bronchoscopic
techniques for ventilator-associated pneumonia. Chest 1992;
102 (suppl 1): 557–64.
14 Micek ST, Ward S, Fraser VJ, Kollef MH. A randomized controlled
trial of an antibiotic discontinuation policy for clinically suspected
ventilator-associated pneumonia. Chest 2004; 125: 1791–99.
15 Stolz D, Smyrnios N, Eggimann P, et al. Procalcitonin for reduced
antibiotic exposure in ventilator-associated pneumonia:
a randomised study. Eur Respir J 2009; 34: 1364–75.
16 Bouadma L, Luyt CE, Tubach F, et al. Use of procalcitonin to reduce
patients’ exposure to antibiotics in intensive care units (PRORATA
trial): a multicentre randomised controlled trial. Lancet 2010;
375: 463–74.
17 Jensen JU, Hein L, Lundgren B, et al. Procalcitonin-guided
interventions against infections to increase early appropriate
antibiotics and improve survival in the intensive care unit:
a randomized trial. Crit Care Med 2011; 39: 2048–58.
18 Layios N, Lambermont B, Canivet JL, et al. Procalcitonin usefulness
for the initiation of antibiotic treatment in intensive care unit
patients. Crit Care Med 2012; 40: 2304–09.
19 de Jong E, van Oers JA, Beishuizen A, et al. Efficacy and safety of
procalcitonin guidance in reducing the duration of antibiotic
treatment in critically ill patients: a randomised, controlled,
open-label trial. Lancet Infect Dis 2016; 16: 819–27.
20 Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of
procalcitonin to shorten antibiotic treatment duration in septic
patients: a randomized trial. Am J Respir Crit Care Med 2008;
177: 498–505.
21 Luyt CE, Combes A, Reynaud C, et al. Usefulness of procalcitonin
for the diagnosis of ventilator-associated pneumonia.
Intensive Care Med 2008; 34: 1434–40.
22 Jung B, Embriaco N, Roux F, et al. Microbiological data, but not
procalcitonin improve the accuracy of the clinical pulmonary
infection score. Intensive Care Med 2010; 36: 790–98.
23 Schuetz P, Wirz Y, Sager R, et al. Effect of procalcitonin-guided
antibiotic treatment on mortality in acute respiratory infections:
a patient level meta-analysis. Lancet Infect Dis 2018; 18: 95–107.
24 Huang DT, Yealy DM, Filbin MR, et al. Procalcitonin-guided use of
antibiotics for lower respiratory tract infection. N Engl J Med 2018;
379: 236–49.
25 Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of
antibiotic therapy for ventilator-associated pneumonia in adults:
a randomized trial. JAMA 2003; 290: 2588–98.
26 Swanson JM, Wood GC, Croce MA, Mueller EW, Boucher BA,
Fabian TC. Utility of preliminary bronchoalveolar lavage results in
suspected ventilator-associated pneumonia. J Trauma 2008;
65: 1271–77.
27 Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ
2004; 329: 168–69.
28 Klein EY, Martinez EM, May L, Saheed M, Reyna V,
Broniatowski DA. Categorical risk perception drives variability in
antibiotic prescribing in the emergency department: a mixed
methods observational study. J Gen Intern Med 2017; 32: 1083–89.
29 Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow
clinical practice guidelines? A framework for improvement. JAMA
1999; 282: 1458–65.
30 Pouwels KB, Dolk FCK, Smith DRM, Robotham JV, Smieszek T.
Actual versus ‘ideal’ antibiotic prescribing for common conditions
in English primary care. J Antimicrob Chemother 2018;
73 (suppl 2): 19–26.
31 Little P, Rumsby K, Kelly J, et al. Information leaflet and antibiotic
prescribing strategies for acute lower respiratory tract infection:
a randomized controlled trial. JAMA 2005; 293: 3029–35.
32 Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled
trial of delayed antibiotic prescribing as a strategy for managing
uncomplicated respiratory tract infection in primary care.
Br J Gen Pract 2001; 51: 200–05.
33 Ferrante di Ruffano L, Hyde CJ, McCaffery KJ, Bossuyt PM,
Deeks JJ. Assessing the value of diagnostic tests: a framework for
designing and evaluating trials. BMJ 2012; 344: e686.
34 Fagon JY, Chastre J, Wolff M, et al. Invasive and noninvasive
strategies for management of suspected ventilator-associated
pneumonia. A randomized trial. Ann Intern Med 2000; 132: 621–30.
35 Canadian Critical Care Trials Group. A randomized trial of
diagnostic techniques for ventilator-associated pneumonia.
N Engl J Med 2006; 355: 2619–30.
36 Browne E, Hellyer TP, Baudouin SV, et al. A national survey of the
diagnosis and management of suspected ventilator-associated
pneumonia. BMJ Open Respir Res 2014; 1: e000066.
37 Schnabel RM, van der Velden K, Osinski A, Rohde G,
Roekaerts PMHJ, Bergmans DCJJ. Clinical course and
complications following diagnostic bronchoalveolar lavage in
critically ill mechanically ventilated patients. BMC Pulm Med 2015;
15: 107.
38 Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM.
Diagnosis of ventilator-associated pneumonia by bacteriologic
analysis of bronchoscopic and nonbronchoscopic “blind”
bronchoalveolar lavage fluid. Am Rev Respir Dis 1991; 143: 1121–29.
39 Lisboa T, Diaz E, Sa-Borges M, et al. The ventilator-associated
pneumonia PIRO score: a tool for predicting ICU mortality and
health-care resources use in ventilator-associated pneumonia.
Chest 2008; 134: 1208–16.
40 Mirsaeidi M, Peyrani P, Ramirez JA. Predicting mortality in
patients with ventilator-associated pneumonia: the APACHE II
score versus the new IBMP-10 score. Clin Infect Dis 2009; 49: 72–77.
41 Timsit JF, Schwebel C, Styfalova L, et al. Impact of bronchial
colonization with Candida spp on the risk of bacterial
ventilator-associated pneumonia in the ICU: the FUNGIBACT
prospective cohort study. Intensive Care Med 2019: 45: 834–43.
42 Fischer GW, Longfield R, Hemming VG, Valdes-Dapena A,
Smith LP. Pneumococcal sepsis with false-negative blood cultures.
Am J Clin Pathol 1982; 78: 348–50.
43 Connell TG, Rele M, Cowley D, Buttery JP, Curtis N. How reliable
is a negative blood culture result? Volume of blood submitted for
culture in routine practice in a children’s hospital. Pediatrics 2007;
119: 891–96.
44 Schuetz P, Christ-Crain M, Thomann R, et al. Effect of
procalcitonin-based guidelines vs standard guidelines on antibiotic
use in lower respiratory tract infections: the ProHOSP randomized
controlled trial. JAMA 2009; 302: 1059–66.
www.thelancet.com/respiratory Vol 8 February 2020 191
8 Kett DH, Cano E, Quartin AA, et al. Implementation of guidelines
for management of possible multidrug-resistant pneumonia in
intensive care: an observational, multicentre cohort study.
Lancet Infect Dis 2011; 11: 181–89.
9 Conway Morris A, Kefala K, Wilkinson TS, et al. Diagnostic
importance of pulmonary interleukin-1β and interleukin-8 in
ventilator-associated pneumonia. Thorax 2010; 65: 201–07.
10 Hellyer TP, Morris AC, McAuley DF, et al. Diagnostic accuracy of
pulmonary host inflammatory mediators in the exclusion of
ventilator-acquired pneumonia. Thorax 2015; 70: 41–47.
11 Moore GF, Audrey S, Barker M, et al. Process evaluation of complex
interventions: Medical Research Council guidance. BMJ 2015;
350: h1258.
12 Hellyer TP, Anderson NA, Parker J, et al. Effectiveness of
biomarker-based exclusion of ventilator-acquired pneumonia to
reduce antibiotic use (VAPrapid-2): study protocol for a randomised
controlled trial. Trials 2016; 17: 318.
13 Meduri GU, Chastre J. The standardization of bronchoscopic
techniques for ventilator-associated pneumonia. Chest 1992;
102 (suppl 1): 557–64.
14 Micek ST, Ward S, Fraser VJ, Kollef MH. A randomized controlled
trial of an antibiotic discontinuation policy for clinically suspected
ventilator-associated pneumonia. Chest 2004; 125: 1791–99.
15 Stolz D, Smyrnios N, Eggimann P, et al. Procalcitonin for reduced
antibiotic exposure in ventilator-associated pneumonia:
a randomised study. Eur Respir J 2009; 34: 1364–75.
16 Bouadma L, Luyt CE, Tubach F, et al. Use of procalcitonin to reduce
patients’ exposure to antibiotics in intensive care units (PRORATA
trial): a multicentre randomised controlled trial. Lancet 2010;
375: 463–74.
17 Jensen JU, Hein L, Lundgren B, et al. Procalcitonin-guided
interventions against infections to increase early appropriate
antibiotics and improve survival in the intensive care unit:
a randomized trial. Crit Care Med 2011; 39: 2048–58.
18 Layios N, Lambermont B, Canivet JL, et al. Procalcitonin usefulness
for the initiation of antibiotic treatment in intensive care unit
patients. Crit Care Med 2012; 40: 2304–09.
19 de Jong E, van Oers JA, Beishuizen A, et al. Efficacy and safety of
procalcitonin guidance in reducing the duration of antibiotic
treatment in critically ill patients: a randomised, controlled,
open-label trial. Lancet Infect Dis 2016; 16: 819–27.
20 Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of
procalcitonin to shorten antibiotic treatment duration in septic
patients: a randomized trial. Am J Respir Crit Care Med 2008;
177: 498–505.
21 Luyt CE, Combes A, Reynaud C, et al. Usefulness of procalcitonin
for the diagnosis of ventilator-associated pneumonia.
Intensive Care Med 2008; 34: 1434–40.
22 Jung B, Embriaco N, Roux F, et al. Microbiological data, but not
procalcitonin improve the accuracy of the clinical pulmonary
infection score. Intensive Care Med 2010; 36: 790–98.
23 Schuetz P, Wirz Y, Sager R, et al. Effect of procalcitonin-guided
antibiotic treatment on mortality in acute respiratory infections:
a patient level meta-analysis. Lancet Infect Dis 2018; 18: 95–107.
24 Huang DT, Yealy DM, Filbin MR, et al. Procalcitonin-guided use of
antibiotics for lower respiratory tract infection. N Engl J Med 2018;
379: 236–49.
25 Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of
antibiotic therapy for ventilator-associated pneumonia in adults:
a randomized trial. JAMA 2003; 290: 2588–98.
26 Swanson JM, Wood GC, Croce MA, Mueller EW, Boucher BA,
Fabian TC. Utility of preliminary bronchoalveolar lavage results in
suspected ventilator-associated pneumonia. J Trauma 2008;
65: 1271–77.
27 Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ
2004; 329: 168–69.
28 Klein EY, Martinez EM, May L, Saheed M, Reyna V,
Broniatowski DA. Categorical risk perception drives variability in
antibiotic prescribing in the emergency department: a mixed
methods observational study. J Gen Intern Med 2017; 32: 1083–89.
29 Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow
clinical practice guidelines? A framework for improvement. JAMA
1999; 282: 1458–65.
30 Pouwels KB, Dolk FCK, Smith DRM, Robotham JV, Smieszek T.
Actual versus ‘ideal’ antibiotic prescribing for common conditions
in English primary care. J Antimicrob Chemother 2018;
73 (suppl 2): 19–26.
31 Little P, Rumsby K, Kelly J, et al. Information leaflet and antibiotic
prescribing strategies for acute lower respiratory tract infection:
a randomized controlled trial. JAMA 2005; 293: 3029–35.
32 Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled
trial of delayed antibiotic prescribing as a strategy for managing
uncomplicated respiratory tract infection in primary care.
Br J Gen Pract 2001; 51: 200–05.
33 Ferrante di Ruffano L, Hyde CJ, McCaffery KJ, Bossuyt PM,
Deeks JJ. Assessing the value of diagnostic tests: a framework for
designing and evaluating trials. BMJ 2012; 344: e686.
34 Fagon JY, Chastre J, Wolff M, et al. Invasive and noninvasive
strategies for management of suspected ventilator-associated
pneumonia. A randomized trial. Ann Intern Med 2000; 132: 621–30.
35 Canadian Critical Care Trials Group. A randomized trial of
diagnostic techniques for ventilator-associated pneumonia.
N Engl J Med 2006; 355: 2619–30.
36 Browne E, Hellyer TP, Baudouin SV, et al. A national survey of the
diagnosis and management of suspected ventilator-associated
pneumonia. BMJ Open Respir Res 2014; 1: e000066.
37 Schnabel RM, van der Velden K, Osinski A, Rohde G,
Roekaerts PMHJ, Bergmans DCJJ. Clinical course and
complications following diagnostic bronchoalveolar lavage in
critically ill mechanically ventilated patients. BMC Pulm Med 2015;
15: 107.
38 Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM.
Diagnosis of ventilator-associated pneumonia by bacteriologic
analysis of bronchoscopic and nonbronchoscopic “blind”
bronchoalveolar lavage fluid. Am Rev Respir Dis 1991; 143: 1121–29.
39 Lisboa T, Diaz E, Sa-Borges M, et al. The ventilator-associated
pneumonia PIRO score: a tool for predicting ICU mortality and
health-care resources use in ventilator-associated pneumonia.
Chest 2008; 134: 1208–16.
40 Mirsaeidi M, Peyrani P, Ramirez JA. Predicting mortality in
patients with ventilator-associated pneumonia: the APACHE II
score versus the new IBMP-10 score. Clin Infect Dis 2009; 49: 72–77.
41 Timsit JF, Schwebel C, Styfalova L, et al. Impact of bronchial
colonization with Candida spp on the risk of bacterial
ventilator-associated pneumonia in the ICU: the FUNGIBACT
prospective cohort study. Intensive Care Med 2019: 45: 834–43.
42 Fischer GW, Longfield R, Hemming VG, Valdes-Dapena A,
Smith LP. Pneumococcal sepsis with false-negative blood cultures.
Am J Clin Pathol 1982; 78: 348–50.
43 Connell TG, Rele M, Cowley D, Buttery JP, Curtis N. How reliable
is a negative blood culture result? Volume of blood submitted for
culture in routine practice in a children’s hospital. Pediatrics 2007;
119: 891–96.
44 Schuetz P, Christ-Crain M, Thomann R, et al. Effect of
procalcitonin-based guidelines vs standard guidelines on antibiotic
use in lower respiratory tract infections: the ProHOSP randomized
controlled trial. JAMA 2009; 302: 1059–66.
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.