Analyzing Risks in Blood Science Lab Sample Workflow & ISO 15189
VerifiedAdded on 2023/06/15
|14
|3293
|300
Essay
AI Summary
This essay provides a comprehensive analysis of risk management within blood science laboratories, focusing on the sample workflow encompassing pre-analytical, analytical, and post-analytical phases. It begins by defining risk management according to ISO 14971 and introduces the common equipment and processes within a blood science laboratory. The essay then details each phase of the sample workflow, highlighting potential risks such as labeling errors, improper reagent mixing, and incorrect interpretation of results. Furthermore, it proposes and justifies the implementation of control measures in the pre- and post-analytical phases, including meticulous labeling procedures, validation of analytical data, and proper data entry protocols. The essay also emphasizes the importance of monitoring these control measures through quality indicators aligned with ISO 15189 standards, such as specimen rejection rates, turnaround time, and client satisfaction, ultimately aiming to improve patient safety and laboratory competence. This resource is available on Desklib, a platform offering study tools and solved assignments for students.

Running head: QUALITY IN MEDICAL LABORATORIES
QUALITY IN MEDICAL LABORATORIES
Name of the Student
Name of the university
Author’s note
QUALITY IN MEDICAL LABORATORIES
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1QUALITY IN MEDICAL LABORATORIES
Risk management in a blood science laboratory
Clinical laboratories plays a crucial role in the decision making process in health care.
Unfortunately no laboratory devices or tests can be infallible and mistakes may occur at the pre-
analytical, analytical and the post analytical phase of testing. Evaluation of the triggering factors
that can cause errors and demarcation of the necessary steps for detecting errors can prevent
patient harm (Njoroge and Nichols 2014). According to the International Organization for
Standardization (ISO) 14971, risk management is the application of the management policies,
practices and procedures for the analysis, evaluation, and control and monitoring of the risks
(Hawkins 2012). The risk management methods and the standards have been traditionally
targeted to the manufacturers, but the risk management principles are now also introduced in the
clinical laboratory (Hawkins 2012). The development of the risk management can be divided in
to four steps involving the collection of the samples, proper processing of the specimens and
correct interpretation of the results.
Introduction to the blood sciences laboratory and common equipment/processes
A blood science laboratory contains several analytical lab instruments whose purpose is
to analyze the samples qualitatively and quantitatively. The wide range of instruments allows a
wide range of testing materials. Instruments such as flow cytometers, analyzers, coagulation
analyzers and slide stainers are the important equipments of a hematology laboratory (Pagana
and Pagana 2017).
Blood science laboratories are laboratories where bloods are collected from the patients
for examination in the pathology laboratories to diagnose any illness or helps in the study of
Risk management in a blood science laboratory
Clinical laboratories plays a crucial role in the decision making process in health care.
Unfortunately no laboratory devices or tests can be infallible and mistakes may occur at the pre-
analytical, analytical and the post analytical phase of testing. Evaluation of the triggering factors
that can cause errors and demarcation of the necessary steps for detecting errors can prevent
patient harm (Njoroge and Nichols 2014). According to the International Organization for
Standardization (ISO) 14971, risk management is the application of the management policies,
practices and procedures for the analysis, evaluation, and control and monitoring of the risks
(Hawkins 2012). The risk management methods and the standards have been traditionally
targeted to the manufacturers, but the risk management principles are now also introduced in the
clinical laboratory (Hawkins 2012). The development of the risk management can be divided in
to four steps involving the collection of the samples, proper processing of the specimens and
correct interpretation of the results.
Introduction to the blood sciences laboratory and common equipment/processes
A blood science laboratory contains several analytical lab instruments whose purpose is
to analyze the samples qualitatively and quantitatively. The wide range of instruments allows a
wide range of testing materials. Instruments such as flow cytometers, analyzers, coagulation
analyzers and slide stainers are the important equipments of a hematology laboratory (Pagana
and Pagana 2017).
Blood science laboratories are laboratories where bloods are collected from the patients
for examination in the pathology laboratories to diagnose any illness or helps in the study of
2QUALITY IN MEDICAL LABORATORIES
blood and the blood forming tissues for monitoring the disorders related to blood and bone
marrow.
The laboratory testing is classified in to three phases- the pre-analytical phase, the analytical
phases and post analytical phases.
Pre-analytical phase
Pre-analytical step is one of the main sources of mistakes that occur during the laboratory
diagnostics. It covers the steps that include preparing patient for the test, collection of sample,
transportation of sample, preparation of sample, and sample storage (Plebani et al. 2014). This is
the first step in laboratory testing. All the blood samples are generally brought in small
vacutainer tubes that are normally brought in small plastic sheets. The vacutainer tubes have to
be stored at 4-25 degree. Any tubes beyond the expiration date should not be used. All the
specimens ate provided with a specific laboratory number (Carraro et al. 2013).
Analytical phase
The second phase in the analytical phase which is considered as the actually laboratory
testing.
All the gel barriers and the additives are used by the gentle inversion 5-10 times instantly
after the draw, which assists in the process of clotting. It also helps in the homogenous
amalgamation of the additives. The serum separator tubes should clot for about 30 minutes prior
to the centrifugation in a vertical position (Sciacovelli et al. 2014).
The blood samples are at first centrifuged and the serum is generally separated. Then the
serum is divided in separate tubes. The specimens are then entered in one or more of the
blood and the blood forming tissues for monitoring the disorders related to blood and bone
marrow.
The laboratory testing is classified in to three phases- the pre-analytical phase, the analytical
phases and post analytical phases.
Pre-analytical phase
Pre-analytical step is one of the main sources of mistakes that occur during the laboratory
diagnostics. It covers the steps that include preparing patient for the test, collection of sample,
transportation of sample, preparation of sample, and sample storage (Plebani et al. 2014). This is
the first step in laboratory testing. All the blood samples are generally brought in small
vacutainer tubes that are normally brought in small plastic sheets. The vacutainer tubes have to
be stored at 4-25 degree. Any tubes beyond the expiration date should not be used. All the
specimens ate provided with a specific laboratory number (Carraro et al. 2013).
Analytical phase
The second phase in the analytical phase which is considered as the actually laboratory
testing.
All the gel barriers and the additives are used by the gentle inversion 5-10 times instantly
after the draw, which assists in the process of clotting. It also helps in the homogenous
amalgamation of the additives. The serum separator tubes should clot for about 30 minutes prior
to the centrifugation in a vertical position (Sciacovelli et al. 2014).
The blood samples are at first centrifuged and the serum is generally separated. Then the
serum is divided in separate tubes. The specimens are then entered in one or more of the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3QUALITY IN MEDICAL LABORATORIES
sophisticated analyzers. There are sometimes robotic sample handlers for optimizing the
workflow and preventing the contamination of the samples.
Post analytical phase
The post analytical steps consisted of the interpretation of the lab results, its
documentation and transport to the physician. The post analytical phase can be subdivided into a
phase that is performed in the laboratory and the other that the health care professionals receive,
interpret or react to the laboratory results.
Risks in the pre-analytical phase
In the pre analytical phase there are several steps, where the reliability of the human has
to be considered. One of the risks associated with the pre-analytical testing is the labeling of the
containers incorrectly. Labeling errors can cause bring three stages- before, during and after the
collection of the specimen (Kaushik and Green 2014). It cannot be said that the error occurs only
in the laboratory and may also involve non laboratory personnel. This risk can be detrimental to
the patient as wrong information can change the treatment regimen of a particular disease and
incorrect diagnose of diseases. The labeling errors can delay or misdirect the treatment options of
a patient Kohn et al. 2000). This damage increases the cost to the laboratory and the health care
industry, greater length of stay and reduced reputation of the organization. Errors in the
preanalytical phase are more frequent than the other two phases (Kohn et al. 2000).
Risk in the analytical phase
Current advancements have been made for the automatic detection of the serum indices
and the hemolytic index. Visual observance of hemolysis can be abandoned due to less
sophisticated analyzers. There are sometimes robotic sample handlers for optimizing the
workflow and preventing the contamination of the samples.
Post analytical phase
The post analytical steps consisted of the interpretation of the lab results, its
documentation and transport to the physician. The post analytical phase can be subdivided into a
phase that is performed in the laboratory and the other that the health care professionals receive,
interpret or react to the laboratory results.
Risks in the pre-analytical phase
In the pre analytical phase there are several steps, where the reliability of the human has
to be considered. One of the risks associated with the pre-analytical testing is the labeling of the
containers incorrectly. Labeling errors can cause bring three stages- before, during and after the
collection of the specimen (Kaushik and Green 2014). It cannot be said that the error occurs only
in the laboratory and may also involve non laboratory personnel. This risk can be detrimental to
the patient as wrong information can change the treatment regimen of a particular disease and
incorrect diagnose of diseases. The labeling errors can delay or misdirect the treatment options of
a patient Kohn et al. 2000). This damage increases the cost to the laboratory and the health care
industry, greater length of stay and reduced reputation of the organization. Errors in the
preanalytical phase are more frequent than the other two phases (Kohn et al. 2000).
Risk in the analytical phase
Current advancements have been made for the automatic detection of the serum indices
and the hemolytic index. Visual observance of hemolysis can be abandoned due to less
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4QUALITY IN MEDICAL LABORATORIES
sensitivity and reproducibility. Errors in the analytical phase can also be caused due to improper
mixing of the reagents, interfering of the reagents, clotted specimen. Errors in the analytical
phase can be caused incompetent personnel and in places where any competency assessment has
not been performed in the past 2 years. All these may contribute to the faulty or erroneous result
of the tests, which may affect the decision making or treatment of the patient often leading to
mortality and morbidity (McPherson and Pincus 2017).
Risks in the post analytical phase
The post analytical phase is done outside the laboratory control, a clinician gets, reads
and interprets the results. Then decisions are made on the basis of the laboratory values and the
other sources. In many cases the urgent results requested by the Emergency Department are often
not assessed. The results released from the laboratory often do not contain all the information
required by the clinicians (McPherson and Pincus 2017). Some of the reason responsible for the
faults in the post analytical phase can be due to the errors in the key board entry, missed
corrections of the erroneous results. Incorrect interpretation of the laboratory results or failure to
inform the outpatients regarding their abnormal results may hamper the decision making.
Examples like patients not being informed of cholesterol as high as 8.2 mmol/L or very low
potassium levels such as 2.6mmol/L (Abdollahi et al. 2014).
Control measures in the pre-analytical phase
Pre-analytical errors in laboratory can be prevented by developing clear written
procedures, automating the different functions for both the executive and the support operations
(Lippi et al. 2013). All the electronic processes should be critiquing to avoid any bypass of the
sensitivity and reproducibility. Errors in the analytical phase can also be caused due to improper
mixing of the reagents, interfering of the reagents, clotted specimen. Errors in the analytical
phase can be caused incompetent personnel and in places where any competency assessment has
not been performed in the past 2 years. All these may contribute to the faulty or erroneous result
of the tests, which may affect the decision making or treatment of the patient often leading to
mortality and morbidity (McPherson and Pincus 2017).
Risks in the post analytical phase
The post analytical phase is done outside the laboratory control, a clinician gets, reads
and interprets the results. Then decisions are made on the basis of the laboratory values and the
other sources. In many cases the urgent results requested by the Emergency Department are often
not assessed. The results released from the laboratory often do not contain all the information
required by the clinicians (McPherson and Pincus 2017). Some of the reason responsible for the
faults in the post analytical phase can be due to the errors in the key board entry, missed
corrections of the erroneous results. Incorrect interpretation of the laboratory results or failure to
inform the outpatients regarding their abnormal results may hamper the decision making.
Examples like patients not being informed of cholesterol as high as 8.2 mmol/L or very low
potassium levels such as 2.6mmol/L (Abdollahi et al. 2014).
Control measures in the pre-analytical phase
Pre-analytical errors in laboratory can be prevented by developing clear written
procedures, automating the different functions for both the executive and the support operations
(Lippi et al. 2013). All the electronic processes should be critiquing to avoid any bypass of the
5QUALITY IN MEDICAL LABORATORIES
barcode safety functions. The labeling of the containers has to be checked and cross checked to
avoid errors (Abdollahi et al. 2014).
Prevention of the identification error: critical scrutiny of the inpatient samples via patient’s
name, bar-coded wristband and birth-date. Patient room number or location should not be used
for identification process.
Proper recording of the patient order: Either via phone or via face to face contact and then
repeating the entire order after noting it down in order to cross verify.
(Hawkins 2012)
Control measures in the post- analytical phase
Proper validation of the analytical data: It will help to safe-guard the threat of erroneous
validation of analytical data. This proper validation must be done in two step process first via
trained yet experienced laboratory technique and then via a registered doctor.
Proper addressing of the report: This should be executed by a trained, experienced and registered
doctor. Addressing of the report should contain detailed remarks along with the normal range of
the blood parameters.
Proper entry of data: This will prevent the generation of erroneous results arising from improper
data entry. The entered data must be cross-checked twice.
(Hawkins 2012)
barcode safety functions. The labeling of the containers has to be checked and cross checked to
avoid errors (Abdollahi et al. 2014).
Prevention of the identification error: critical scrutiny of the inpatient samples via patient’s
name, bar-coded wristband and birth-date. Patient room number or location should not be used
for identification process.
Proper recording of the patient order: Either via phone or via face to face contact and then
repeating the entire order after noting it down in order to cross verify.
(Hawkins 2012)
Control measures in the post- analytical phase
Proper validation of the analytical data: It will help to safe-guard the threat of erroneous
validation of analytical data. This proper validation must be done in two step process first via
trained yet experienced laboratory technique and then via a registered doctor.
Proper addressing of the report: This should be executed by a trained, experienced and registered
doctor. Addressing of the report should contain detailed remarks along with the normal range of
the blood parameters.
Proper entry of data: This will prevent the generation of erroneous results arising from improper
data entry. The entered data must be cross-checked twice.
(Hawkins 2012)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6QUALITY IN MEDICAL LABORATORIES
Monitoring of the control measures
ISO 15189 Medical laboratories are an International standard that specifies the system of
quality management particular to the medical laboratories. It was developed by the International
Organization for the standardization's Technical committee. The standards contain medical codes
of practice for enhancing the safety in the laboratory including the collection of the specimen
sample, analysis of sample and interpretation of the lab results. It contains instructions as to how
testing should be managed during medical emergency. The working group responsible for
preparing the standard also set up rules for the lab's role in educating and training the staffs
(Abdollahi et al. 2014). .
The success of the laboratory competence can be measured by some quality indicators.
These quality indicators are evaluated by the laboratory management (Head of the department).
The IOS defines the health care domains by patient safety, equity, effectiveness, patient
centeredness, efficiency and timeliness.
The seven key indicators that can assist in the evaluation off the success are the rejection
rates of the specimen, the turnaround time, the performance of proficiency testing, client
satisfaction, equipment down time, reagent rejection rate and the reagents stock out (Plebani et
al. 2013).
The proficiency testing performance (PTP) may be defined as the percentage of correct
proficiency testing. The client satisfaction survey can actually help to measure the percentage of
the client satisfaction with the various aspects of the services provided by the laboratory such as
courtesy, confidentiality, explanation of the procedures, instruction, and cleanliness, waiting
Monitoring of the control measures
ISO 15189 Medical laboratories are an International standard that specifies the system of
quality management particular to the medical laboratories. It was developed by the International
Organization for the standardization's Technical committee. The standards contain medical codes
of practice for enhancing the safety in the laboratory including the collection of the specimen
sample, analysis of sample and interpretation of the lab results. It contains instructions as to how
testing should be managed during medical emergency. The working group responsible for
preparing the standard also set up rules for the lab's role in educating and training the staffs
(Abdollahi et al. 2014). .
The success of the laboratory competence can be measured by some quality indicators.
These quality indicators are evaluated by the laboratory management (Head of the department).
The IOS defines the health care domains by patient safety, equity, effectiveness, patient
centeredness, efficiency and timeliness.
The seven key indicators that can assist in the evaluation off the success are the rejection
rates of the specimen, the turnaround time, the performance of proficiency testing, client
satisfaction, equipment down time, reagent rejection rate and the reagents stock out (Plebani et
al. 2013).
The proficiency testing performance (PTP) may be defined as the percentage of correct
proficiency testing. The client satisfaction survey can actually help to measure the percentage of
the client satisfaction with the various aspects of the services provided by the laboratory such as
courtesy, confidentiality, explanation of the procedures, instruction, and cleanliness, waiting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7QUALITY IN MEDICAL LABORATORIES
time, turnaround time, counseling and result information. The specimen rejection rate on the
other hand is the percentage of the rejected specimen (Plebani et al. 2013)..
The turnaround time indicator helps to understand the rate of the laboratory tests that are
not completed within the deadline. The equipment down time refers to the number of erroneous
results due to faulty equipments. This is responsible for the analytical error in a laboratory. The
reagent stock out also refers to the number of days in a month where a group of reagent has stock
out. The reagent rejection rate refers to the rate at which the hematology reagents are rejected.
These key performance indicators can actually evaluate the error rates in a laboratory and
measure the improvement done.
The quality management system
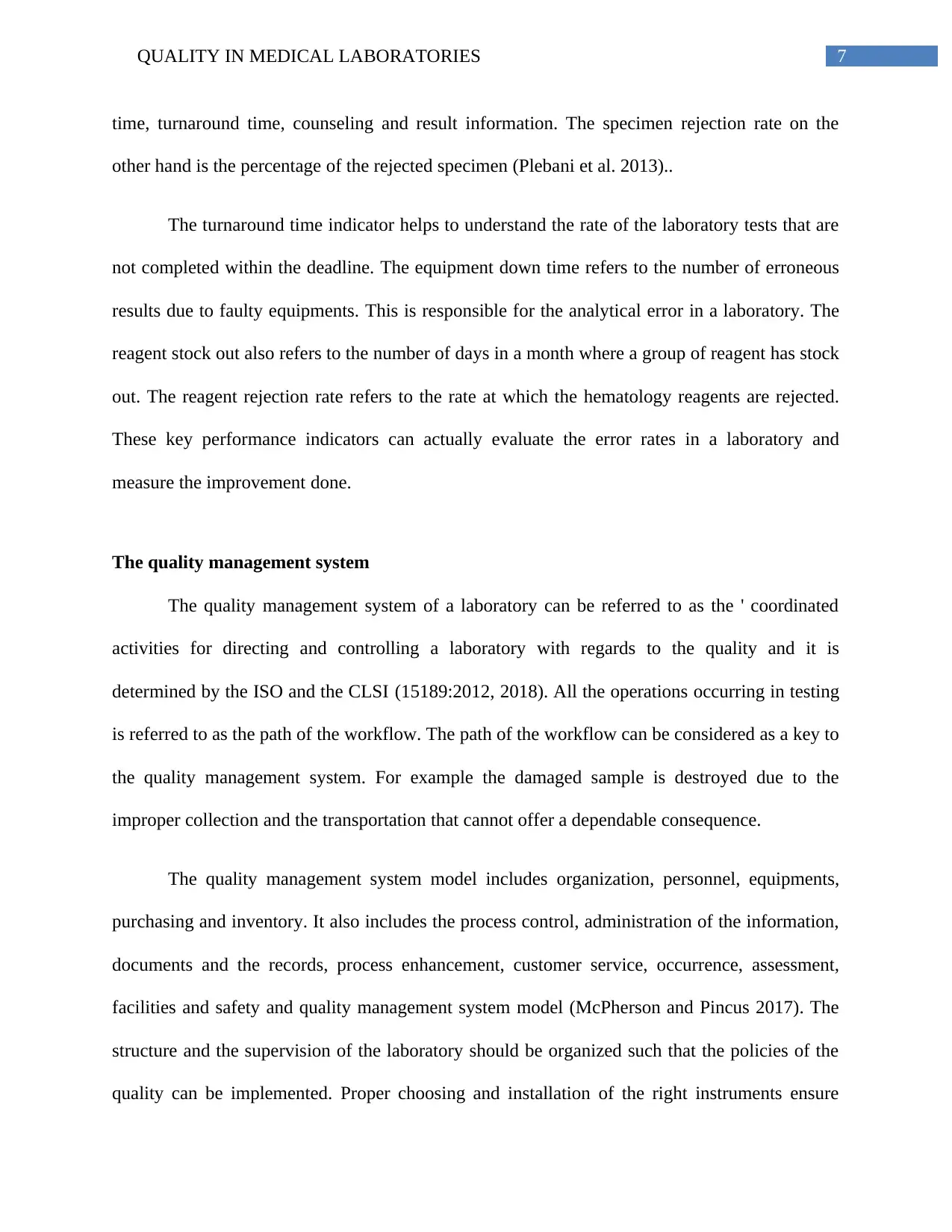
The quality management system of a laboratory can be referred to as the ' coordinated
activities for directing and controlling a laboratory with regards to the quality and it is
determined by the ISO and the CLSI (15189:2012, 2018). All the operations occurring in testing
is referred to as the path of the workflow. The path of the workflow can be considered as a key to
the quality management system. For example the damaged sample is destroyed due to the
improper collection and the transportation that cannot offer a dependable consequence.
The quality management system model includes organization, personnel, equipments,
purchasing and inventory. It also includes the process control, administration of the information,
documents and the records, process enhancement, customer service, occurrence, assessment,
facilities and safety and quality management system model (McPherson and Pincus 2017). The
structure and the supervision of the laboratory should be organized such that the policies of the
quality can be implemented. Proper choosing and installation of the right instruments ensure
time, turnaround time, counseling and result information. The specimen rejection rate on the
other hand is the percentage of the rejected specimen (Plebani et al. 2013)..
The turnaround time indicator helps to understand the rate of the laboratory tests that are
not completed within the deadline. The equipment down time refers to the number of erroneous
results due to faulty equipments. This is responsible for the analytical error in a laboratory. The
reagent stock out also refers to the number of days in a month where a group of reagent has stock
out. The reagent rejection rate refers to the rate at which the hematology reagents are rejected.
These key performance indicators can actually evaluate the error rates in a laboratory and
measure the improvement done.
The quality management system
The quality management system of a laboratory can be referred to as the ' coordinated
activities for directing and controlling a laboratory with regards to the quality and it is
determined by the ISO and the CLSI (15189:2012, 2018). All the operations occurring in testing
is referred to as the path of the workflow. The path of the workflow can be considered as a key to
the quality management system. For example the damaged sample is destroyed due to the
improper collection and the transportation that cannot offer a dependable consequence.
The quality management system model includes organization, personnel, equipments,
purchasing and inventory. It also includes the process control, administration of the information,
documents and the records, process enhancement, customer service, occurrence, assessment,
facilities and safety and quality management system model (McPherson and Pincus 2017). The
structure and the supervision of the laboratory should be organized such that the policies of the
quality can be implemented. Proper choosing and installation of the right instruments ensure
8QUALITY IN MEDICAL LABORATORIES
avoidance of analytical errors. The process control plays an important part in the laboratory
testing process (Belloum et al. 2011).
Path of workflow in a blood science laboratory
Source: (McPherson and Pincus 2017).
Accreditation and regulation
It is used by the medical laboratories for developing their system of quality supervision
system and assessment of their own competence in the medical laboratories. There are certain
basic requirements for the ISO 15189 certification which involves a well-documented analysis of
the procedures by the laboratories, a training manual provided by the laboratories, a detailed
avoidance of analytical errors. The process control plays an important part in the laboratory
testing process (Belloum et al. 2011).
Path of workflow in a blood science laboratory
Source: (McPherson and Pincus 2017).
Accreditation and regulation
It is used by the medical laboratories for developing their system of quality supervision
system and assessment of their own competence in the medical laboratories. There are certain
basic requirements for the ISO 15189 certification which involves a well-documented analysis of
the procedures by the laboratories, a training manual provided by the laboratories, a detailed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9QUALITY IN MEDICAL LABORATORIES
analysis of the medical laboratory for making sure that all the weaknesses have been identified.
ISO 15189 certification requires a detailed audit of the review of the management (15189:2012,
2018). The main aim of the certification is the quality assurance. The ISO 15189 certification
promotes the development of a sound image internationally by management systems and quality
assurance (15189:2012, 2018). It helps to provide a strong degree of consistency in compliance
with the laws of the medical laboratory from a global perspective. The certification also helps to
promote the modern laboratory technique that includes the professionalism in conducting the
medical activities in the laboratory.
Important clauses in ISO standards
The important clause that has been introduced is there had been a more logical ordering
of the sub clauses under each of the clause. The layout has been improved making it easier to
identify the specific sub clauses. Two new normative sections have been introduced. Clause
number 5.8 of the ISO 15189 has been split up in to the criteria for reporting and the result
release (15189:2012, 2018). Under the section of the management requirements the internal
audits have been split up and detailed in to Evaluation and audits, periodic review of the requests
and the requirement of the samples, assessment of the feedback of the users , staff suggestion,
internal audit , quality indicators and reviews from the external organization.
Conclusion
Patient safety focuses on the reporting, analysis and the prevention of the medical errors
that often leads to some adverse events. Besides causing lethal effect to the patient, medical
errors contribute to a huge amount of money wiped out of the international and the national
economy. Basically what should be focused on is the willingness to identify the challenges and
analysis of the medical laboratory for making sure that all the weaknesses have been identified.
ISO 15189 certification requires a detailed audit of the review of the management (15189:2012,
2018). The main aim of the certification is the quality assurance. The ISO 15189 certification
promotes the development of a sound image internationally by management systems and quality
assurance (15189:2012, 2018). It helps to provide a strong degree of consistency in compliance
with the laws of the medical laboratory from a global perspective. The certification also helps to
promote the modern laboratory technique that includes the professionalism in conducting the
medical activities in the laboratory.
Important clauses in ISO standards
The important clause that has been introduced is there had been a more logical ordering
of the sub clauses under each of the clause. The layout has been improved making it easier to
identify the specific sub clauses. Two new normative sections have been introduced. Clause
number 5.8 of the ISO 15189 has been split up in to the criteria for reporting and the result
release (15189:2012, 2018). Under the section of the management requirements the internal
audits have been split up and detailed in to Evaluation and audits, periodic review of the requests
and the requirement of the samples, assessment of the feedback of the users , staff suggestion,
internal audit , quality indicators and reviews from the external organization.
Conclusion
Patient safety focuses on the reporting, analysis and the prevention of the medical errors
that often leads to some adverse events. Besides causing lethal effect to the patient, medical
errors contribute to a huge amount of money wiped out of the international and the national
economy. Basically what should be focused on is the willingness to identify the challenges and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10QUALITY IN MEDICAL LABORATORIES
not argue about the number of the sentinel events. Instead focus should be given on development
of a systematic workflow, identification of the critical processes, a continuous monitoring, and
prediction of the accidental events, strengthening the defenses and decreasing the vulnerability of
the errors.
not argue about the number of the sentinel events. Instead focus should be given on development
of a systematic workflow, identification of the critical processes, a continuous monitoring, and
prediction of the accidental events, strengthening the defenses and decreasing the vulnerability of
the errors.
11QUALITY IN MEDICAL LABORATORIES
References
15189:2012, I. (2018). ISO 15189:2012 - Medical laboratories -- Requirements for quality and
competence. [online] Iso.org. Available at: https://www.iso.org/standard/56115.html [Accessed
25 Feb. 2018].
Abdollahi, A., Saffar, H. and Saffar, H., 2014. Types and frequency of errors during different
phases of testing at a clinical medical laboratory of a teaching hospital in Tehran, Iran. North
American journal of medical sciences, 6(5), p.224.
Belloum, A., Inda, M.A., Vasunin, D., Korkhov, V., Zhao, Z., Rauwerda, H., Breit, T.M., Bubak,
M. and Hertzberger, L.O., 2011. Collaborative e-science experiments and scientific workflows.
IEEE Internet Computing, 15(4), pp.39-47.
Carraro, P., Zago, T. and Plebani, M., 2012. Exploring the initial steps of the testing process:
frequency and nature of pre-preanalytic errors. Clinical chemistry, 58(3), pp.638-642.
Hawkins, R., 2012. Managing the pre-and post-analytical phases of the total testing process.
Annals of laboratory medicine, 32(1), pp.5-16.
Hawkins, R., 2012. Managing the pre-and post-analytical phases of the total testing
process. Annals of laboratory medicine, 32(1), pp.5-16.
Kaushik, N. and Green, S., 2014. Pre-analytical errors: their impact and how to minimize them.
MLO Med Lab Obs, 46(5), pp.22-24.
Kohn, K., Corrigan, J., and Donaldson, M. ,2000. To err is human: Building a safer health
system. Washington, D.C.: National Academy Press.
References
15189:2012, I. (2018). ISO 15189:2012 - Medical laboratories -- Requirements for quality and
competence. [online] Iso.org. Available at: https://www.iso.org/standard/56115.html [Accessed
25 Feb. 2018].
Abdollahi, A., Saffar, H. and Saffar, H., 2014. Types and frequency of errors during different
phases of testing at a clinical medical laboratory of a teaching hospital in Tehran, Iran. North
American journal of medical sciences, 6(5), p.224.
Belloum, A., Inda, M.A., Vasunin, D., Korkhov, V., Zhao, Z., Rauwerda, H., Breit, T.M., Bubak,
M. and Hertzberger, L.O., 2011. Collaborative e-science experiments and scientific workflows.
IEEE Internet Computing, 15(4), pp.39-47.
Carraro, P., Zago, T. and Plebani, M., 2012. Exploring the initial steps of the testing process:
frequency and nature of pre-preanalytic errors. Clinical chemistry, 58(3), pp.638-642.
Hawkins, R., 2012. Managing the pre-and post-analytical phases of the total testing process.
Annals of laboratory medicine, 32(1), pp.5-16.
Hawkins, R., 2012. Managing the pre-and post-analytical phases of the total testing
process. Annals of laboratory medicine, 32(1), pp.5-16.
Kaushik, N. and Green, S., 2014. Pre-analytical errors: their impact and how to minimize them.
MLO Med Lab Obs, 46(5), pp.22-24.
Kohn, K., Corrigan, J., and Donaldson, M. ,2000. To err is human: Building a safer health
system. Washington, D.C.: National Academy Press.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





