BMS3136: Blood Grouping, Transfusion and Biochemistry Report
VerifiedAdded on 2022/12/23
|8
|2023
|60
Report
AI Summary
This report analyzes blood grouping, focusing on ABO and Rh blood typing, compatibility, and transfusion practices. It addresses questions related to blood group identification based on provided results, including the identification of blood groups and compatible plasma transfusions. The report explains the necessity of both forward and reverse typing in routine ABO blood group typing and why reverse grouping is not required for infants under four months old. The document also discusses the concept of universal donors for red blood cells and plasma transfusions, potential errors in blood typing, the Diamed ID card, and acute haemolytic transfusion reactions. Additionally, it interprets a patient's blood group based on provided results and discusses the clinical significance of Anti-Lea antibodies. The report includes a table summarizing the findings and references relevant literature.
BLOOD GROUPING
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
QUESTIONS...................................................................................................................................3
REFERENCES................................................................................................................................8
QUESTIONS...................................................................................................................................3
REFERENCES................................................................................................................................8

QUESTIONS
1.
Persons who have group O red cells are referred as universal donors which means that red blood
cells from a type O+ donor can be transfused into patients having the blood types A+, AB+, B+
and O+. These are also known as universal donors because the red blood cells they have donated
have no Rh, A or B antigens and therefore it is very safe to give those red blood cells to people
having any blood group (Jöud, Möller and Olsson, 2018). This is not in the case of plasma
transfusions because the matching is done for avoiding the A and B antibodies in the transfused
plasma which is going to attack the red blood cells of the recipient. So, in case of plasma
transfusions, the people with type AB blood are considered as universal plasma donors. This is
because their plasma does not contain the antibodies A or B can their transfusion can be safely
done to all the blood types.
2. Blood typing is basically a test which helps in determining the blood type of the person. ABO
blood typing helps in yielding complete blood type which means all the eight groups which
include A+, B+, O+, A-, B-, O-, AB- and AB+. If only forward typing is done, then it will help
in determining the presence and absence of type of antigens in the RBC’s whether A or B while
on the other hand, the reverse grouping helps in indicating the presence and absence of the anti-
A or anti-B in the serum (Wu and et.al., 2020). ABO typing consists of both the typing forward
and reverse so that the patterns of clotting can be observed and recorded easily.
3
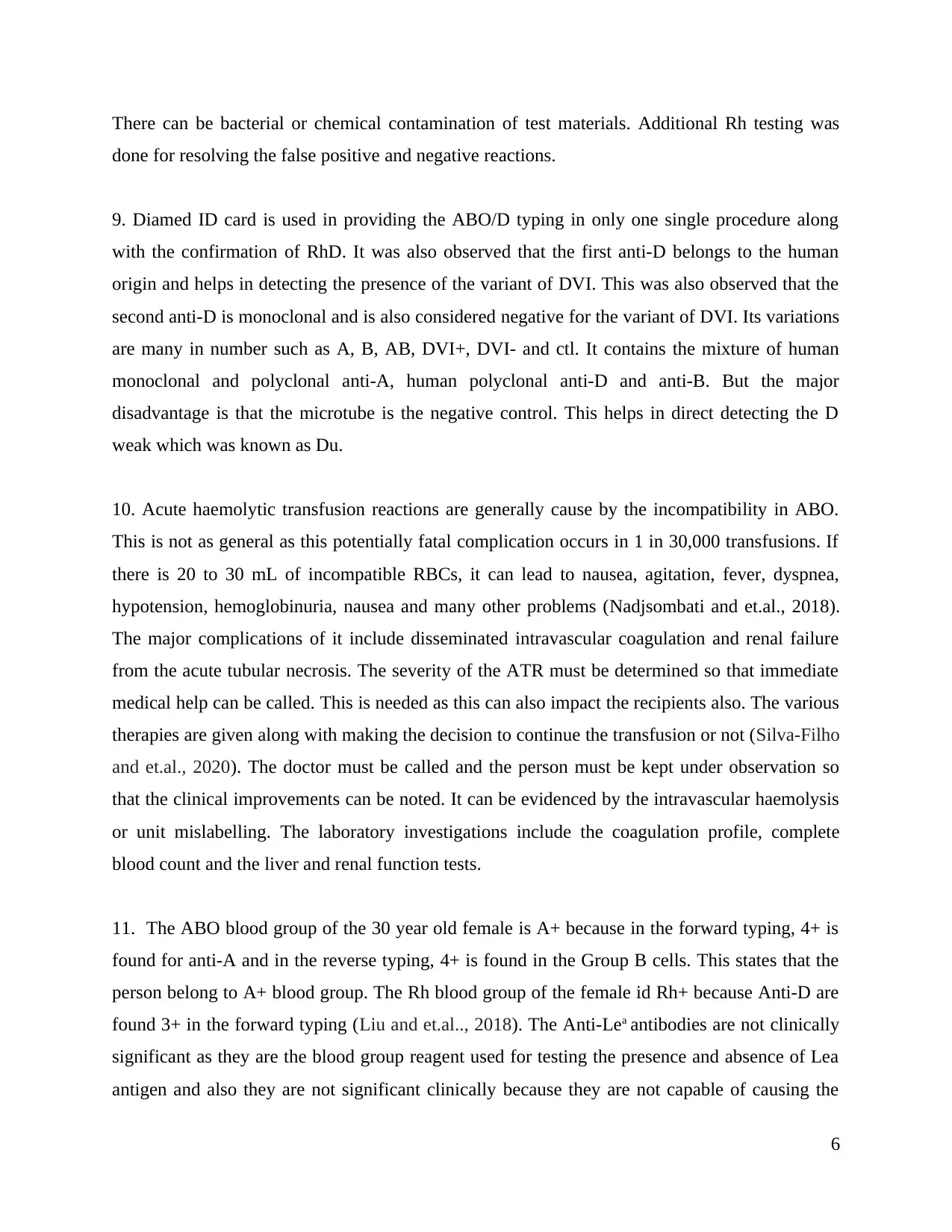
Red Blood Cell
samples
Anti-sera Blood groups Compatible blood group(s)
Anti-AAnti-BAnti-D
1 - - 3+ O+ or AB- O+, Rh-D+
2 - 4+ 3+ B+ or O+ or
A- B, O
3 4+ - 3+ A+ or O+ or
B- A, O
4 4+ 3+ - AB+ or O- AB, A, B, O
1.
Persons who have group O red cells are referred as universal donors which means that red blood
cells from a type O+ donor can be transfused into patients having the blood types A+, AB+, B+
and O+. These are also known as universal donors because the red blood cells they have donated
have no Rh, A or B antigens and therefore it is very safe to give those red blood cells to people
having any blood group (Jöud, Möller and Olsson, 2018). This is not in the case of plasma
transfusions because the matching is done for avoiding the A and B antibodies in the transfused
plasma which is going to attack the red blood cells of the recipient. So, in case of plasma
transfusions, the people with type AB blood are considered as universal plasma donors. This is
because their plasma does not contain the antibodies A or B can their transfusion can be safely
done to all the blood types.
2. Blood typing is basically a test which helps in determining the blood type of the person. ABO
blood typing helps in yielding complete blood type which means all the eight groups which
include A+, B+, O+, A-, B-, O-, AB- and AB+. If only forward typing is done, then it will help
in determining the presence and absence of type of antigens in the RBC’s whether A or B while
on the other hand, the reverse grouping helps in indicating the presence and absence of the anti-
A or anti-B in the serum (Wu and et.al., 2020). ABO typing consists of both the typing forward
and reverse so that the patterns of clotting can be observed and recorded easily.
3
Red Blood Cell
samples
Anti-sera Blood groups Compatible blood group(s)
Anti-AAnti-BAnti-D
1 - - 3+ O+ or AB- O+, Rh-D+
2 - 4+ 3+ B+ or O+ or
A- B, O
3 4+ - 3+ A+ or O+ or
B- A, O
4 4+ 3+ - AB+ or O- AB, A, B, O
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3. Reverse blood typing is confirmed by using the A, B and O cells and the serum. This is
observed that the natural antibodies start appearing in serum after the age group of 5 months
which means when the child crosses the age of 4 months, and then the natural antibodies appear
(Saxena and et.al., 2017). When the child is in the age group of 0 to 4 months, then the
antibodies which are present in the new born is just from the mother which is why when the
blood transfusion is done with the children of less than 4 months age then the cross match is
done with the serum of the mother.
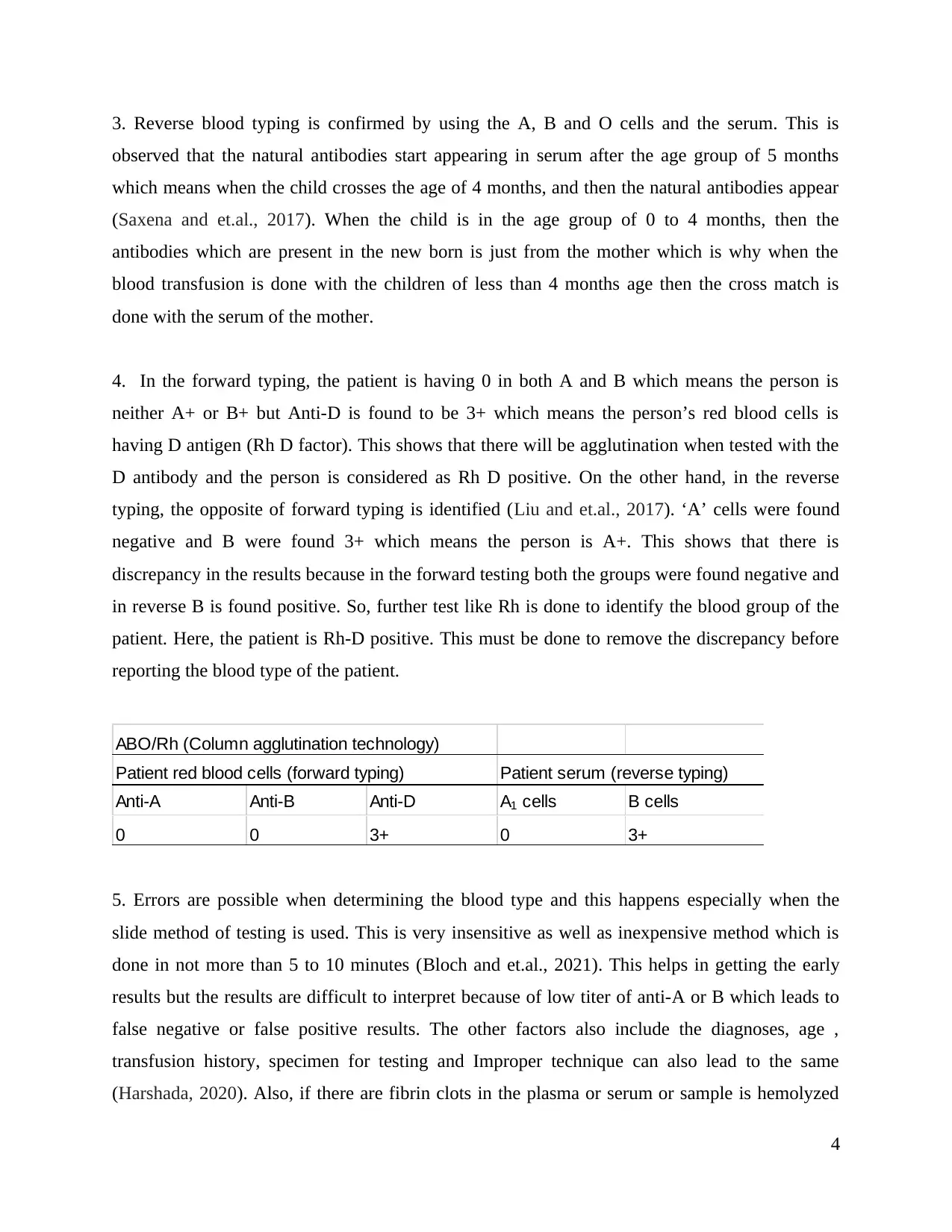
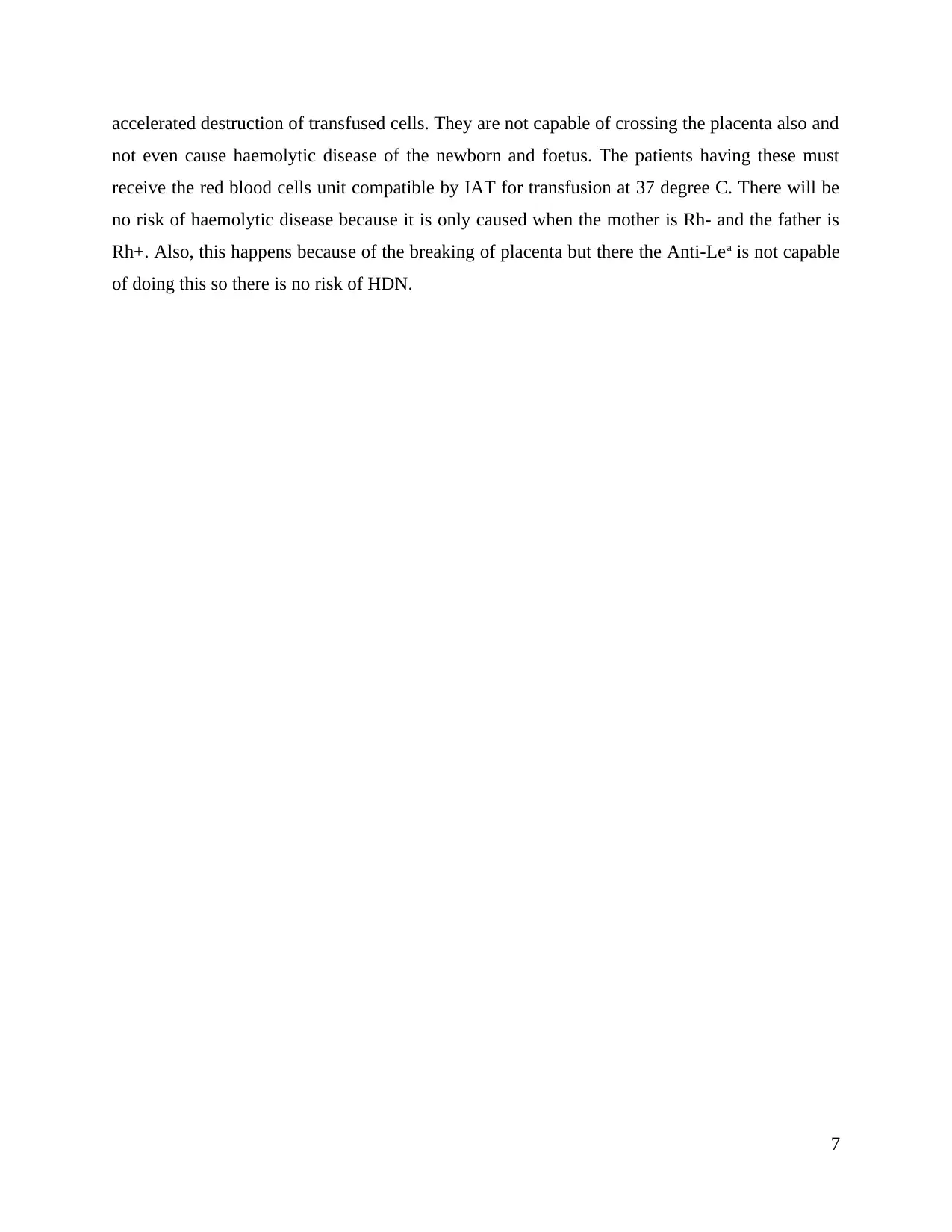
4. In the forward typing, the patient is having 0 in both A and B which means the person is
neither A+ or B+ but Anti-D is found to be 3+ which means the person’s red blood cells is
having D antigen (Rh D factor). This shows that there will be agglutination when tested with the
D antibody and the person is considered as Rh D positive. On the other hand, in the reverse
typing, the opposite of forward typing is identified (Liu and et.al., 2017). ‘A’ cells were found
negative and B were found 3+ which means the person is A+. This shows that there is
discrepancy in the results because in the forward testing both the groups were found negative and
in reverse B is found positive. So, further test like Rh is done to identify the blood group of the
patient. Here, the patient is Rh-D positive. This must be done to remove the discrepancy before
reporting the blood type of the patient.
ABO/Rh (Column agglutination technology)
Anti-A Anti-B Anti-D A1 cells B cells
0 0 3+ 0 3+
Patient red blood cells (forward typing) Patient serum (reverse typing)
5. Errors are possible when determining the blood type and this happens especially when the
slide method of testing is used. This is very insensitive as well as inexpensive method which is
done in not more than 5 to 10 minutes (Bloch and et.al., 2021). This helps in getting the early
results but the results are difficult to interpret because of low titer of anti-A or B which leads to
false negative or false positive results. The other factors also include the diagnoses, age ,
transfusion history, specimen for testing and Improper technique can also lead to the same
(Harshada, 2020). Also, if there are fibrin clots in the plasma or serum or sample is hemolyzed
4
observed that the natural antibodies start appearing in serum after the age group of 5 months
which means when the child crosses the age of 4 months, and then the natural antibodies appear
(Saxena and et.al., 2017). When the child is in the age group of 0 to 4 months, then the
antibodies which are present in the new born is just from the mother which is why when the
blood transfusion is done with the children of less than 4 months age then the cross match is
done with the serum of the mother.
4. In the forward typing, the patient is having 0 in both A and B which means the person is
neither A+ or B+ but Anti-D is found to be 3+ which means the person’s red blood cells is
having D antigen (Rh D factor). This shows that there will be agglutination when tested with the
D antibody and the person is considered as Rh D positive. On the other hand, in the reverse
typing, the opposite of forward typing is identified (Liu and et.al., 2017). ‘A’ cells were found
negative and B were found 3+ which means the person is A+. This shows that there is
discrepancy in the results because in the forward testing both the groups were found negative and
in reverse B is found positive. So, further test like Rh is done to identify the blood group of the
patient. Here, the patient is Rh-D positive. This must be done to remove the discrepancy before
reporting the blood type of the patient.
ABO/Rh (Column agglutination technology)
Anti-A Anti-B Anti-D A1 cells B cells
0 0 3+ 0 3+
Patient red blood cells (forward typing) Patient serum (reverse typing)
5. Errors are possible when determining the blood type and this happens especially when the
slide method of testing is used. This is very insensitive as well as inexpensive method which is
done in not more than 5 to 10 minutes (Bloch and et.al., 2021). This helps in getting the early
results but the results are difficult to interpret because of low titer of anti-A or B which leads to
false negative or false positive results. The other factors also include the diagnoses, age ,
transfusion history, specimen for testing and Improper technique can also lead to the same
(Harshada, 2020). Also, if there are fibrin clots in the plasma or serum or sample is hemolyzed
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
then the false positive or negative results can come. The best results can be obtained by using
unhemolysed and fresh specimen.
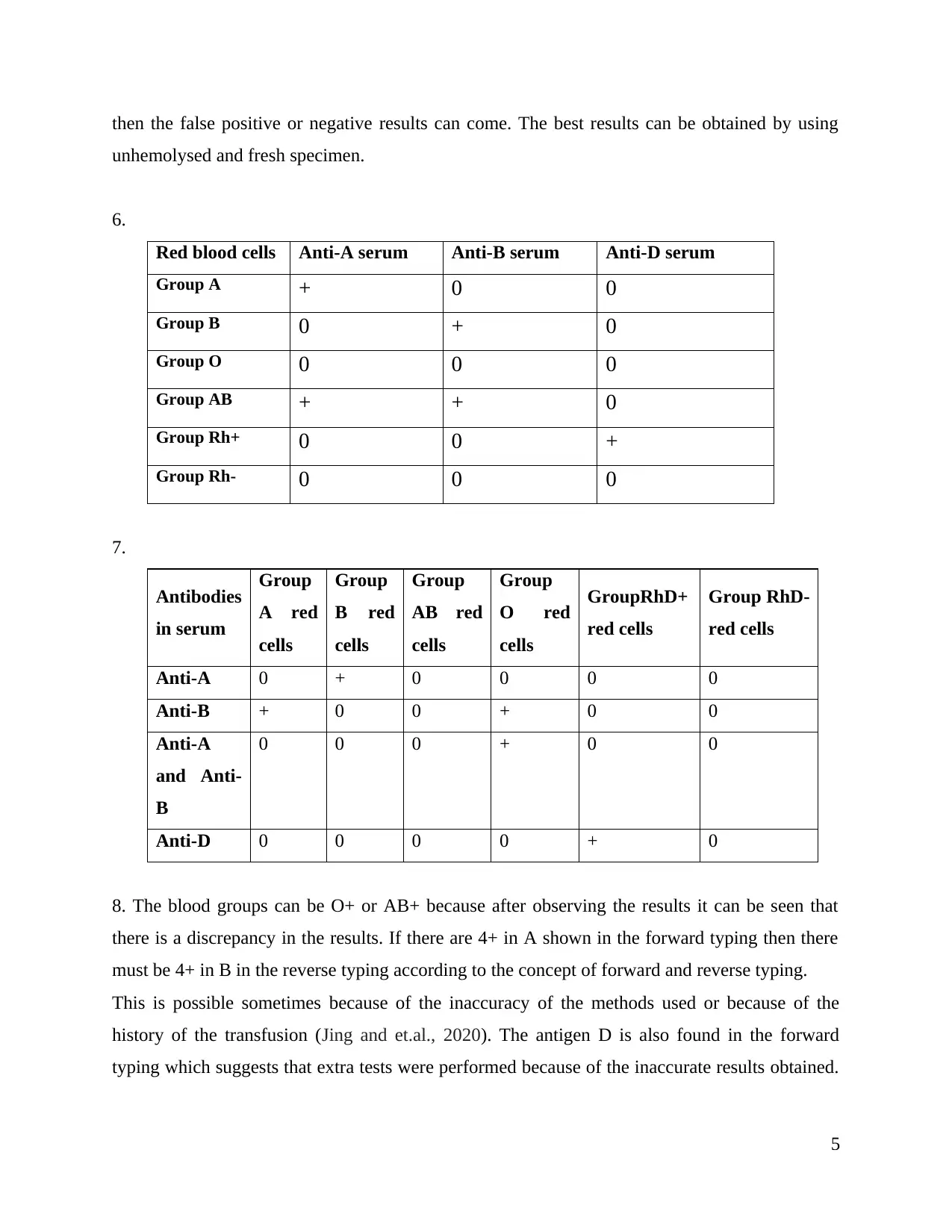
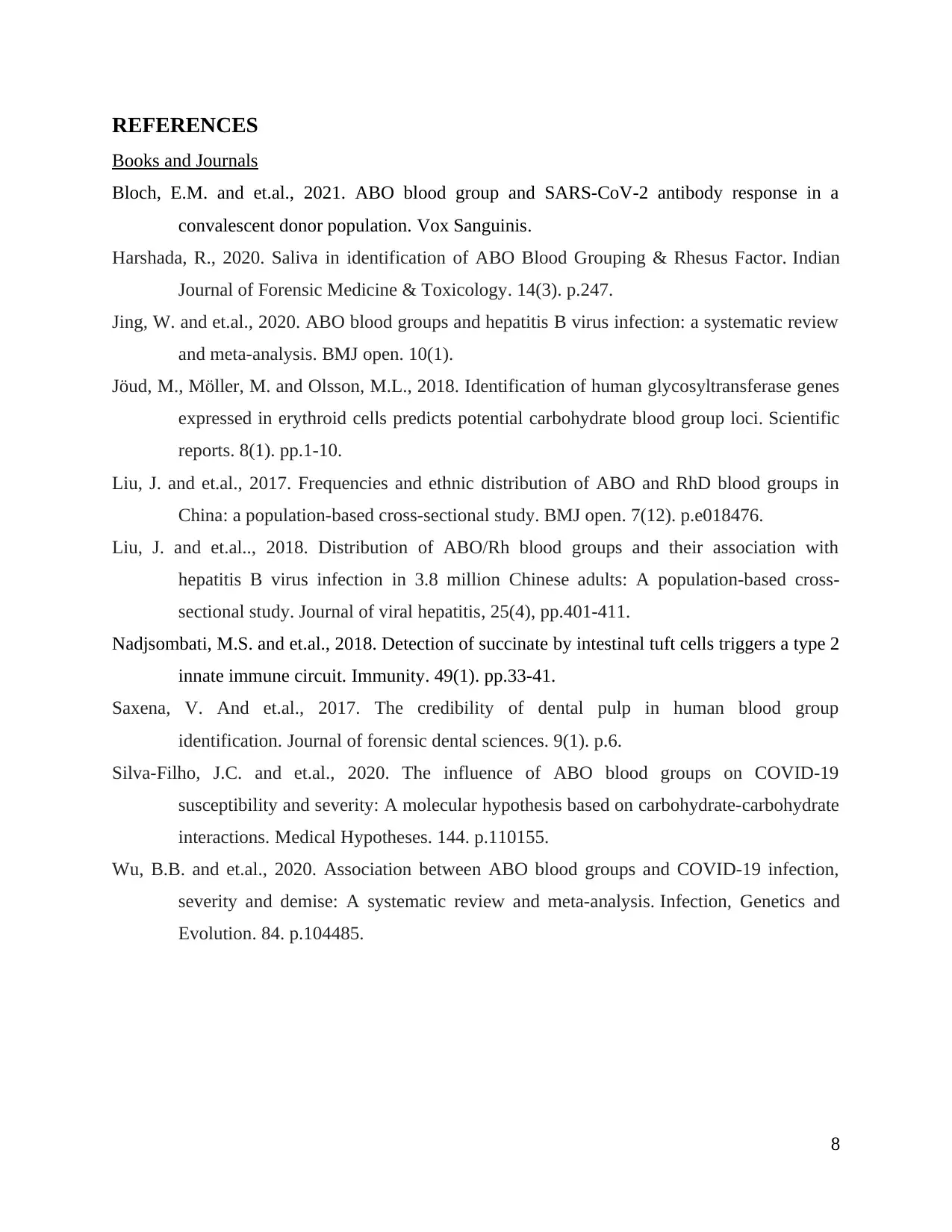
6.
Red blood cells Anti-A serum Anti-B serum Anti-D serum
Group A + 0 0
Group B 0 + 0
Group O 0 0 0
Group AB + + 0
Group Rh+ 0 0 +
Group Rh- 0 0 0
7.
Antibodies
in serum
Group
A red
cells
Group
B red
cells
Group
AB red
cells
Group
O red
cells
GroupRhD+
red cells
Group RhD-
red cells
Anti-A 0 + 0 0 0 0
Anti-B + 0 0 + 0 0
Anti-A
and Anti-
B
0 0 0 + 0 0
Anti-D 0 0 0 0 + 0
8. The blood groups can be O+ or AB+ because after observing the results it can be seen that
there is a discrepancy in the results. If there are 4+ in A shown in the forward typing then there
must be 4+ in B in the reverse typing according to the concept of forward and reverse typing.
This is possible sometimes because of the inaccuracy of the methods used or because of the
history of the transfusion (Jing and et.al., 2020). The antigen D is also found in the forward
typing which suggests that extra tests were performed because of the inaccurate results obtained.
5
unhemolysed and fresh specimen.
6.
Red blood cells Anti-A serum Anti-B serum Anti-D serum
Group A + 0 0
Group B 0 + 0
Group O 0 0 0
Group AB + + 0
Group Rh+ 0 0 +
Group Rh- 0 0 0
7.
Antibodies
in serum
Group
A red
cells
Group
B red
cells
Group
AB red
cells
Group
O red
cells
GroupRhD+
red cells
Group RhD-
red cells
Anti-A 0 + 0 0 0 0
Anti-B + 0 0 + 0 0
Anti-A
and Anti-
B
0 0 0 + 0 0
Anti-D 0 0 0 0 + 0
8. The blood groups can be O+ or AB+ because after observing the results it can be seen that
there is a discrepancy in the results. If there are 4+ in A shown in the forward typing then there
must be 4+ in B in the reverse typing according to the concept of forward and reverse typing.
This is possible sometimes because of the inaccuracy of the methods used or because of the
history of the transfusion (Jing and et.al., 2020). The antigen D is also found in the forward
typing which suggests that extra tests were performed because of the inaccurate results obtained.
5
There can be bacterial or chemical contamination of test materials. Additional Rh testing was
done for resolving the false positive and negative reactions.
9. Diamed ID card is used in providing the ABO/D typing in only one single procedure along
with the confirmation of RhD. It was also observed that the first anti-D belongs to the human
origin and helps in detecting the presence of the variant of DVI. This was also observed that the
second anti-D is monoclonal and is also considered negative for the variant of DVI. Its variations
are many in number such as A, B, AB, DVI+, DVI- and ctl. It contains the mixture of human
monoclonal and polyclonal anti-A, human polyclonal anti-D and anti-B. But the major
disadvantage is that the microtube is the negative control. This helps in direct detecting the D
weak which was known as Du.
10. Acute haemolytic transfusion reactions are generally cause by the incompatibility in ABO.
This is not as general as this potentially fatal complication occurs in 1 in 30,000 transfusions. If
there is 20 to 30 mL of incompatible RBCs, it can lead to nausea, agitation, fever, dyspnea,
hypotension, hemoglobinuria, nausea and many other problems (Nadjsombati and et.al., 2018).
The major complications of it include disseminated intravascular coagulation and renal failure
from the acute tubular necrosis. The severity of the ATR must be determined so that immediate
medical help can be called. This is needed as this can also impact the recipients also. The various
therapies are given along with making the decision to continue the transfusion or not (Silva-Filho
and et.al., 2020). The doctor must be called and the person must be kept under observation so
that the clinical improvements can be noted. It can be evidenced by the intravascular haemolysis
or unit mislabelling. The laboratory investigations include the coagulation profile, complete
blood count and the liver and renal function tests.
11. The ABO blood group of the 30 year old female is A+ because in the forward typing, 4+ is
found for anti-A and in the reverse typing, 4+ is found in the Group B cells. This states that the
person belong to A+ blood group. The Rh blood group of the female id Rh+ because Anti-D are
found 3+ in the forward typing (Liu and et.al.., 2018). The Anti-Lea antibodies are not clinically
significant as they are the blood group reagent used for testing the presence and absence of Lea
antigen and also they are not significant clinically because they are not capable of causing the
6
done for resolving the false positive and negative reactions.
9. Diamed ID card is used in providing the ABO/D typing in only one single procedure along
with the confirmation of RhD. It was also observed that the first anti-D belongs to the human
origin and helps in detecting the presence of the variant of DVI. This was also observed that the
second anti-D is monoclonal and is also considered negative for the variant of DVI. Its variations
are many in number such as A, B, AB, DVI+, DVI- and ctl. It contains the mixture of human
monoclonal and polyclonal anti-A, human polyclonal anti-D and anti-B. But the major
disadvantage is that the microtube is the negative control. This helps in direct detecting the D
weak which was known as Du.
10. Acute haemolytic transfusion reactions are generally cause by the incompatibility in ABO.
This is not as general as this potentially fatal complication occurs in 1 in 30,000 transfusions. If
there is 20 to 30 mL of incompatible RBCs, it can lead to nausea, agitation, fever, dyspnea,
hypotension, hemoglobinuria, nausea and many other problems (Nadjsombati and et.al., 2018).
The major complications of it include disseminated intravascular coagulation and renal failure
from the acute tubular necrosis. The severity of the ATR must be determined so that immediate
medical help can be called. This is needed as this can also impact the recipients also. The various
therapies are given along with making the decision to continue the transfusion or not (Silva-Filho
and et.al., 2020). The doctor must be called and the person must be kept under observation so
that the clinical improvements can be noted. It can be evidenced by the intravascular haemolysis
or unit mislabelling. The laboratory investigations include the coagulation profile, complete
blood count and the liver and renal function tests.
11. The ABO blood group of the 30 year old female is A+ because in the forward typing, 4+ is
found for anti-A and in the reverse typing, 4+ is found in the Group B cells. This states that the
person belong to A+ blood group. The Rh blood group of the female id Rh+ because Anti-D are
found 3+ in the forward typing (Liu and et.al.., 2018). The Anti-Lea antibodies are not clinically
significant as they are the blood group reagent used for testing the presence and absence of Lea
antigen and also they are not significant clinically because they are not capable of causing the
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
accelerated destruction of transfused cells. They are not capable of crossing the placenta also and
not even cause haemolytic disease of the newborn and foetus. The patients having these must
receive the red blood cells unit compatible by IAT for transfusion at 37 degree C. There will be
no risk of haemolytic disease because it is only caused when the mother is Rh- and the father is
Rh+. Also, this happens because of the breaking of placenta but there the Anti-Lea is not capable
of doing this so there is no risk of HDN.
7
not even cause haemolytic disease of the newborn and foetus. The patients having these must
receive the red blood cells unit compatible by IAT for transfusion at 37 degree C. There will be
no risk of haemolytic disease because it is only caused when the mother is Rh- and the father is
Rh+. Also, this happens because of the breaking of placenta but there the Anti-Lea is not capable
of doing this so there is no risk of HDN.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals
Bloch, E.M. and et.al., 2021. ABO blood group and SARS‐CoV‐2 antibody response in a
convalescent donor population. Vox Sanguinis.
Harshada, R., 2020. Saliva in identification of ABO Blood Grouping & Rhesus Factor. Indian
Journal of Forensic Medicine & Toxicology. 14(3). p.247.
Jing, W. and et.al., 2020. ABO blood groups and hepatitis B virus infection: a systematic review
and meta-analysis. BMJ open. 10(1).
Jöud, M., Möller, M. and Olsson, M.L., 2018. Identification of human glycosyltransferase genes
expressed in erythroid cells predicts potential carbohydrate blood group loci. Scientific
reports. 8(1). pp.1-10.
Liu, J. and et.al., 2017. Frequencies and ethnic distribution of ABO and RhD blood groups in
China: a population-based cross-sectional study. BMJ open. 7(12). p.e018476.
Liu, J. and et.al.., 2018. Distribution of ABO/Rh blood groups and their association with
hepatitis B virus infection in 3.8 million Chinese adults: A population‐based cross‐
sectional study. Journal of viral hepatitis, 25(4), pp.401-411.
Nadjsombati, M.S. and et.al., 2018. Detection of succinate by intestinal tuft cells triggers a type 2
innate immune circuit. Immunity. 49(1). pp.33-41.
Saxena, V. And et.al., 2017. The credibility of dental pulp in human blood group
identification. Journal of forensic dental sciences. 9(1). p.6.
Silva-Filho, J.C. and et.al., 2020. The influence of ABO blood groups on COVID-19
susceptibility and severity: A molecular hypothesis based on carbohydrate-carbohydrate
interactions. Medical Hypotheses. 144. p.110155.
Wu, B.B. and et.al., 2020. Association between ABO blood groups and COVID-19 infection,
severity and demise: A systematic review and meta-analysis. Infection, Genetics and
Evolution. 84. p.104485.
8
Books and Journals
Bloch, E.M. and et.al., 2021. ABO blood group and SARS‐CoV‐2 antibody response in a
convalescent donor population. Vox Sanguinis.
Harshada, R., 2020. Saliva in identification of ABO Blood Grouping & Rhesus Factor. Indian
Journal of Forensic Medicine & Toxicology. 14(3). p.247.
Jing, W. and et.al., 2020. ABO blood groups and hepatitis B virus infection: a systematic review
and meta-analysis. BMJ open. 10(1).
Jöud, M., Möller, M. and Olsson, M.L., 2018. Identification of human glycosyltransferase genes
expressed in erythroid cells predicts potential carbohydrate blood group loci. Scientific
reports. 8(1). pp.1-10.
Liu, J. and et.al., 2017. Frequencies and ethnic distribution of ABO and RhD blood groups in
China: a population-based cross-sectional study. BMJ open. 7(12). p.e018476.
Liu, J. and et.al.., 2018. Distribution of ABO/Rh blood groups and their association with
hepatitis B virus infection in 3.8 million Chinese adults: A population‐based cross‐
sectional study. Journal of viral hepatitis, 25(4), pp.401-411.
Nadjsombati, M.S. and et.al., 2018. Detection of succinate by intestinal tuft cells triggers a type 2
innate immune circuit. Immunity. 49(1). pp.33-41.
Saxena, V. And et.al., 2017. The credibility of dental pulp in human blood group
identification. Journal of forensic dental sciences. 9(1). p.6.
Silva-Filho, J.C. and et.al., 2020. The influence of ABO blood groups on COVID-19
susceptibility and severity: A molecular hypothesis based on carbohydrate-carbohydrate
interactions. Medical Hypotheses. 144. p.110155.
Wu, B.B. and et.al., 2020. Association between ABO blood groups and COVID-19 infection,
severity and demise: A systematic review and meta-analysis. Infection, Genetics and
Evolution. 84. p.104485.
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





