Effectiveness of BMI Programs in Schools: Obesity and Eating Disorders
VerifiedAdded on 2023/06/11
|15
|3587
|122
Report
AI Summary
This report examines the effectiveness of implementing Body Mass Index (BMI) programs in schools to assist parents and teachers in identifying children and adolescents at high risk of developing obesity and eating disorders. The prevalence of these conditions has significantly increased, making prevention a global public health concern. The study reviews the rising rates of obesity and eating disorders like anorexia and bulimia, highlighting the substantial healthcare expenditure and productivity losses associated with these issues. It emphasizes the importance of early intervention during adolescence, a critical period for developing lifelong habits. The report also details a school-based BMI measurement program in Virginia, evaluating its impact on managing obesity in individuals aged 10-16 years, utilizing a controlled study with intervention and control groups to assess the program's effectiveness and associated costs.

Running head: MANAGEMENT OF OBESITY AND EATING DISORDERS IN
ADOLESCENTS AND CHILDREN
1
Management of Obesity and Eating Disorders in Adolescents and Children Paper
Student’s Name
Professor’s Name
Affiliation
Date
ADOLESCENTS AND CHILDREN
1
Management of Obesity and Eating Disorders in Adolescents and Children Paper
Student’s Name
Professor’s Name
Affiliation
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 2
Question
How effective is the implementation of BMI programs in schools to aid parents and teachers in
the identification of children/adolescents who are at high risk of developing obesity and eating
disorders?
Answer
Introduction
The prevalence of obesity and several eating disorders amongst children and adolescents
has increased significantly over the past decade. The increment is mainly attributed to a culture
of unhealthy lifestyle across the world. As such, the prevention of childhood obesity has become
an international public health concern especially due to the positive correlation between eating
disorders and chronic illness. Obesity causes serious development, well-being, and general health
issues in children and adolescents. There are several international evidence based strategies that
can be implemented by families, communities, and government to aid in the mitigation of
childhood and adolescent obesity. The effectiveness of school-based BMI assessment programs
that provide statistical data to parents and teachers for development of preventive measures
should be evaluated across the world (A. J., 2008).
Part A: The perspective of the study
Increment in Obesity in Children and Adolescents
20.5% in the 2000s
82% in the 2010s
CHILDREN 2
Question
How effective is the implementation of BMI programs in schools to aid parents and teachers in
the identification of children/adolescents who are at high risk of developing obesity and eating
disorders?
Answer
Introduction
The prevalence of obesity and several eating disorders amongst children and adolescents
has increased significantly over the past decade. The increment is mainly attributed to a culture
of unhealthy lifestyle across the world. As such, the prevention of childhood obesity has become
an international public health concern especially due to the positive correlation between eating
disorders and chronic illness. Obesity causes serious development, well-being, and general health
issues in children and adolescents. There are several international evidence based strategies that
can be implemented by families, communities, and government to aid in the mitigation of
childhood and adolescent obesity. The effectiveness of school-based BMI assessment programs
that provide statistical data to parents and teachers for development of preventive measures
should be evaluated across the world (A. J., 2008).
Part A: The perspective of the study
Increment in Obesity in Children and Adolescents
20.5% in the 2000s
82% in the 2010s
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 3
Eating disorders like anorexia and bulimia are recognized as the third most common
childhood and adolescent chronic illness; where asthma and obesity at up the first and second
slots respectively. American medical reviews revealed that within the 2000s the cases of
adolescent obesity increased by 20.5%. That figure has quadrupled in the past half-decade. In
most situations, eating disorders start during a person’s late childhood and early teen years.
These conditions are most notable in girls and have been observed in children as young as 6 and
7 years of age. Research has shown that adolescents who are obese or overweight have admitted
to using laxatives and voluntary vomiting to manage their weight compare to normal teens
(Yang, et al., 2016). Eating disorders like anorexia nervosa and bulimia nervosa have also
become a common diagnosis for American teens especially in urban and rich suburban
neighborhoods. Anorexia is defined as a critical self-induced desire to maintain a given weight
range that is motivated by fear of becoming “obese” or “overweight”; even when the people is
underweight or normal weight. Anorexia is characterized by fasting, avoidance of previously
love food items, over-exercising, and a significant reduction the portions of fluid and food
consumed. While, bulimia nervosa is associated with considerable binge eating and purging that
is results in substantial abuse of laxatives and diuretic. Majority of children and adolescents with
Bulimia tend to eat a lot food in hiding and within a short period of time. Parent often notice
significant quantities of food missing and empty food containers on the kitchen counter. In
additions, these individuals are prone to taking long baths (time when purging occurs) and
frequent bathroom trips especially after meals (Yang, et al., 2016).
CHILDREN 3
Eating disorders like anorexia and bulimia are recognized as the third most common
childhood and adolescent chronic illness; where asthma and obesity at up the first and second
slots respectively. American medical reviews revealed that within the 2000s the cases of
adolescent obesity increased by 20.5%. That figure has quadrupled in the past half-decade. In
most situations, eating disorders start during a person’s late childhood and early teen years.
These conditions are most notable in girls and have been observed in children as young as 6 and
7 years of age. Research has shown that adolescents who are obese or overweight have admitted
to using laxatives and voluntary vomiting to manage their weight compare to normal teens
(Yang, et al., 2016). Eating disorders like anorexia nervosa and bulimia nervosa have also
become a common diagnosis for American teens especially in urban and rich suburban
neighborhoods. Anorexia is defined as a critical self-induced desire to maintain a given weight
range that is motivated by fear of becoming “obese” or “overweight”; even when the people is
underweight or normal weight. Anorexia is characterized by fasting, avoidance of previously
love food items, over-exercising, and a significant reduction the portions of fluid and food
consumed. While, bulimia nervosa is associated with considerable binge eating and purging that
is results in substantial abuse of laxatives and diuretic. Majority of children and adolescents with
Bulimia tend to eat a lot food in hiding and within a short period of time. Parent often notice
significant quantities of food missing and empty food containers on the kitchen counter. In
additions, these individuals are prone to taking long baths (time when purging occurs) and
frequent bathroom trips especially after meals (Yang, et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 4
33%
67%
Expenditure on Treatment of Obesity
and Eating Disorders
Current Annual Spending
Expected Annual Spending in the next three years
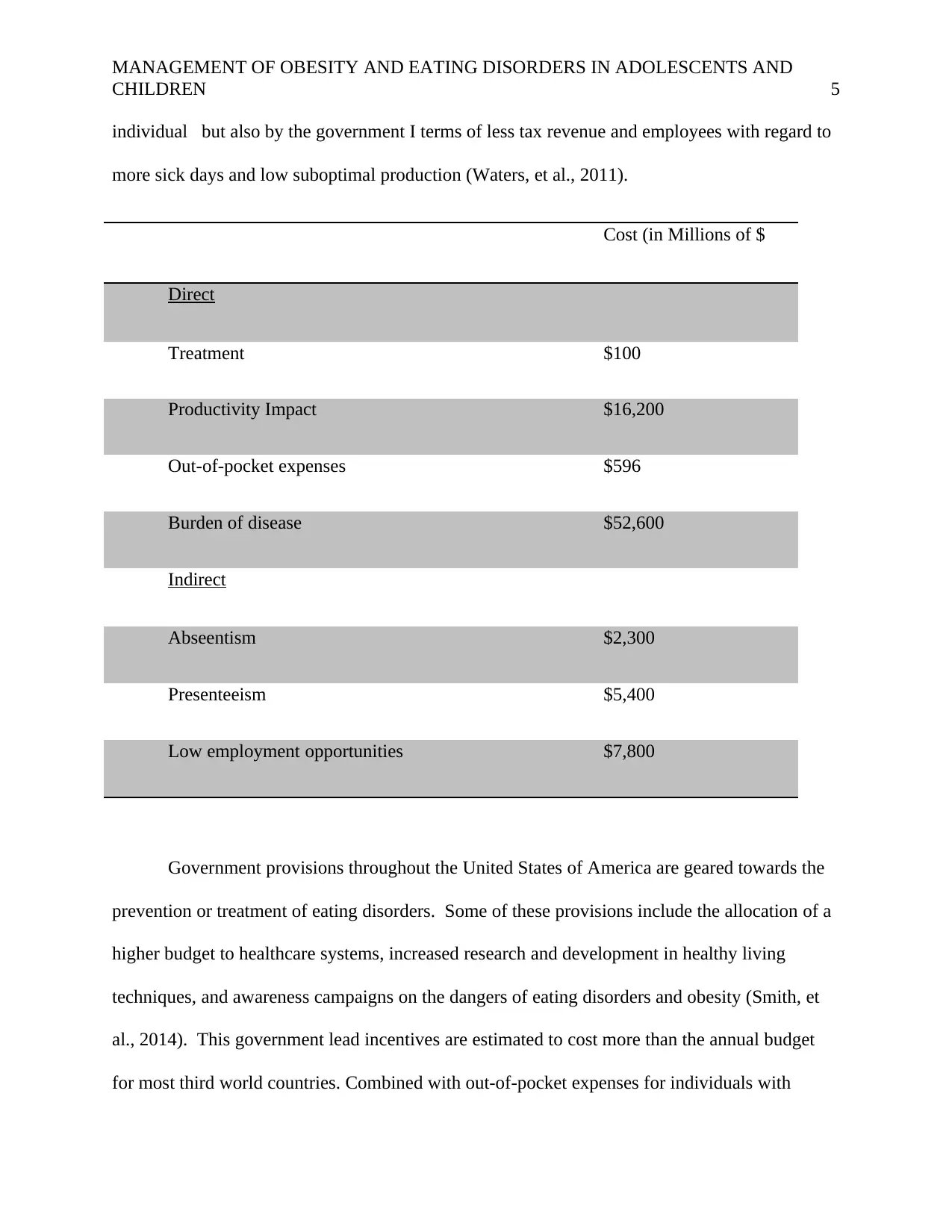
According to a report published by American Society of Clinical Oncology (ASCO) has
shown that the American health system contributes more than $100 million towards the
treatment of obesity and eating disorders annually; since 2009. Adjusting for inflation in
healthcare costs, new illness cases, and deterioration in healthy living, it is estimated that
treatment expenditure for obesity and eating disorders will be in excess of $200 million in the
next three years. The productivity impacts with regards to lost revenue and income for eating
disorders was estimated to be around $16.2 billion in 2017 (Waters, et al., 2011). According to
Access Economics, this amount was almost the same as the $17.9 billon registered for depression
and anxiety in 2010. 1.25% of this loss is attributed to unearned income from young people who
lost their lives to obesity and weight related ailments. The impacts of eating disorders normally
extend for long durations (between 10-15 years) which results in extended productivity issues
like low employment opportunities (costing $7.8 billion), higher absenteeism (costing $2.3
billion), and presenteeism (costing $5.4 billion). This productivity costs are most borne by the
CHILDREN 4
33%
67%
Expenditure on Treatment of Obesity
and Eating Disorders
Current Annual Spending
Expected Annual Spending in the next three years
According to a report published by American Society of Clinical Oncology (ASCO) has
shown that the American health system contributes more than $100 million towards the
treatment of obesity and eating disorders annually; since 2009. Adjusting for inflation in
healthcare costs, new illness cases, and deterioration in healthy living, it is estimated that
treatment expenditure for obesity and eating disorders will be in excess of $200 million in the
next three years. The productivity impacts with regards to lost revenue and income for eating
disorders was estimated to be around $16.2 billion in 2017 (Waters, et al., 2011). According to
Access Economics, this amount was almost the same as the $17.9 billon registered for depression
and anxiety in 2010. 1.25% of this loss is attributed to unearned income from young people who
lost their lives to obesity and weight related ailments. The impacts of eating disorders normally
extend for long durations (between 10-15 years) which results in extended productivity issues
like low employment opportunities (costing $7.8 billion), higher absenteeism (costing $2.3
billion), and presenteeism (costing $5.4 billion). This productivity costs are most borne by the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 5
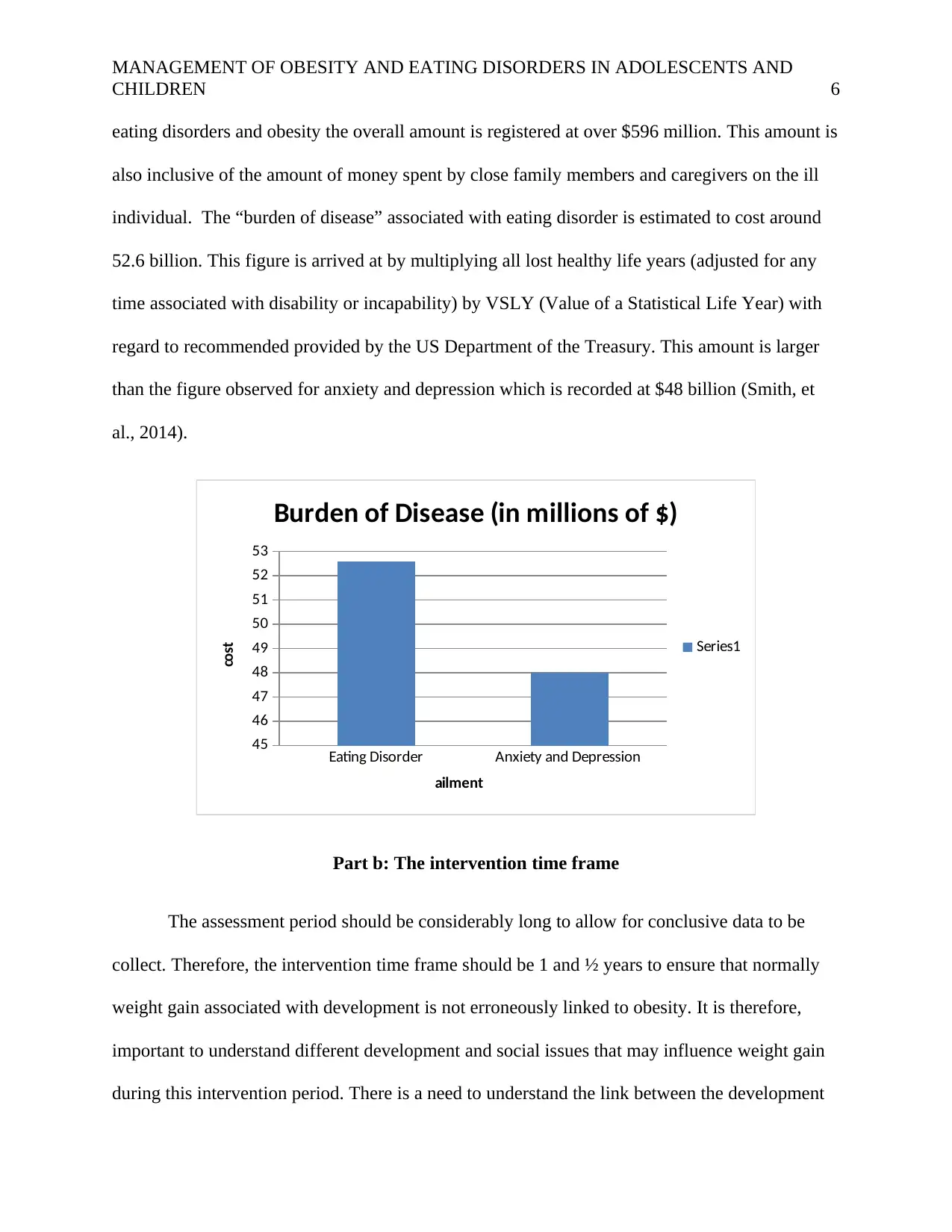
individual but also by the government I terms of less tax revenue and employees with regard to
more sick days and low suboptimal production (Waters, et al., 2011).
Cost (in Millions of $
Direct
Treatment $100
Productivity Impact $16,200
Out-of-pocket expenses $596
Burden of disease $52,600
Indirect
Abseentism $2,300
Presenteeism $5,400
Low employment opportunities $7,800
Government provisions throughout the United States of America are geared towards the
prevention or treatment of eating disorders. Some of these provisions include the allocation of a
higher budget to healthcare systems, increased research and development in healthy living
techniques, and awareness campaigns on the dangers of eating disorders and obesity (Smith, et
al., 2014). This government lead incentives are estimated to cost more than the annual budget
for most third world countries. Combined with out-of-pocket expenses for individuals with
CHILDREN 5
individual but also by the government I terms of less tax revenue and employees with regard to
more sick days and low suboptimal production (Waters, et al., 2011).
Cost (in Millions of $
Direct
Treatment $100
Productivity Impact $16,200
Out-of-pocket expenses $596
Burden of disease $52,600
Indirect
Abseentism $2,300
Presenteeism $5,400
Low employment opportunities $7,800
Government provisions throughout the United States of America are geared towards the
prevention or treatment of eating disorders. Some of these provisions include the allocation of a
higher budget to healthcare systems, increased research and development in healthy living
techniques, and awareness campaigns on the dangers of eating disorders and obesity (Smith, et
al., 2014). This government lead incentives are estimated to cost more than the annual budget
for most third world countries. Combined with out-of-pocket expenses for individuals with
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 6
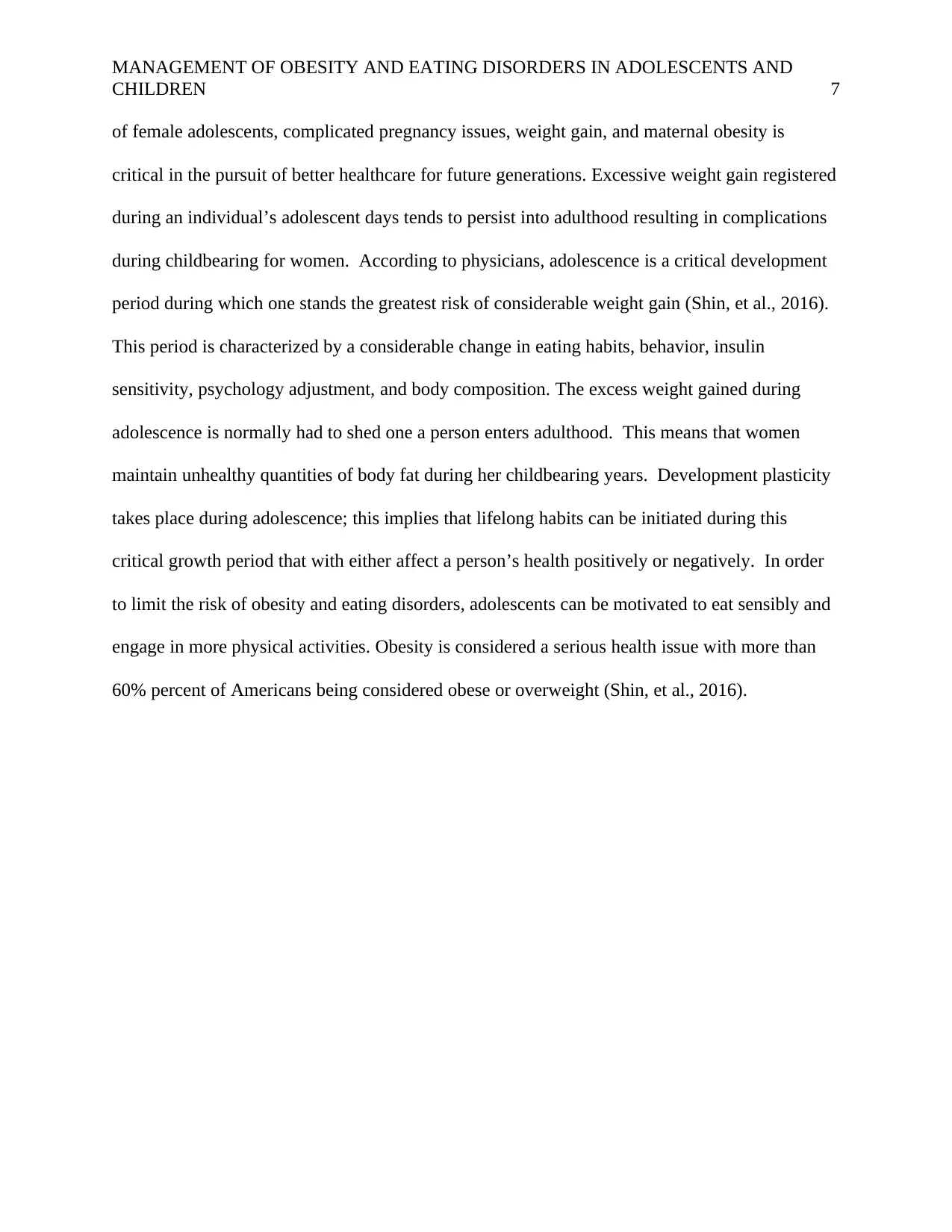
eating disorders and obesity the overall amount is registered at over $596 million. This amount is
also inclusive of the amount of money spent by close family members and caregivers on the ill
individual. The “burden of disease” associated with eating disorder is estimated to cost around
52.6 billion. This figure is arrived at by multiplying all lost healthy life years (adjusted for any
time associated with disability or incapability) by VSLY (Value of a Statistical Life Year) with
regard to recommended provided by the US Department of the Treasury. This amount is larger
than the figure observed for anxiety and depression which is recorded at $48 billion (Smith, et
al., 2014).
Eating Disorder Anxiety and Depression
45
46
47
48
49
50
51
52
53
Burden of Disease (in millions of $)
Series1
ailment
cost
Part b: The intervention time frame
The assessment period should be considerably long to allow for conclusive data to be
collect. Therefore, the intervention time frame should be 1 and ½ years to ensure that normally
weight gain associated with development is not erroneously linked to obesity. It is therefore,
important to understand different development and social issues that may influence weight gain
during this intervention period. There is a need to understand the link between the development
CHILDREN 6
eating disorders and obesity the overall amount is registered at over $596 million. This amount is
also inclusive of the amount of money spent by close family members and caregivers on the ill
individual. The “burden of disease” associated with eating disorder is estimated to cost around
52.6 billion. This figure is arrived at by multiplying all lost healthy life years (adjusted for any
time associated with disability or incapability) by VSLY (Value of a Statistical Life Year) with
regard to recommended provided by the US Department of the Treasury. This amount is larger
than the figure observed for anxiety and depression which is recorded at $48 billion (Smith, et
al., 2014).
Eating Disorder Anxiety and Depression
45
46
47
48
49
50
51
52
53
Burden of Disease (in millions of $)
Series1
ailment
cost
Part b: The intervention time frame
The assessment period should be considerably long to allow for conclusive data to be
collect. Therefore, the intervention time frame should be 1 and ½ years to ensure that normally
weight gain associated with development is not erroneously linked to obesity. It is therefore,
important to understand different development and social issues that may influence weight gain
during this intervention period. There is a need to understand the link between the development
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 7
of female adolescents, complicated pregnancy issues, weight gain, and maternal obesity is
critical in the pursuit of better healthcare for future generations. Excessive weight gain registered
during an individual’s adolescent days tends to persist into adulthood resulting in complications
during childbearing for women. According to physicians, adolescence is a critical development
period during which one stands the greatest risk of considerable weight gain (Shin, et al., 2016).
This period is characterized by a considerable change in eating habits, behavior, insulin
sensitivity, psychology adjustment, and body composition. The excess weight gained during
adolescence is normally had to shed one a person enters adulthood. This means that women
maintain unhealthy quantities of body fat during her childbearing years. Development plasticity
takes place during adolescence; this implies that lifelong habits can be initiated during this
critical growth period that with either affect a person’s health positively or negatively. In order
to limit the risk of obesity and eating disorders, adolescents can be motivated to eat sensibly and
engage in more physical activities. Obesity is considered a serious health issue with more than
60% percent of Americans being considered obese or overweight (Shin, et al., 2016).
CHILDREN 7
of female adolescents, complicated pregnancy issues, weight gain, and maternal obesity is
critical in the pursuit of better healthcare for future generations. Excessive weight gain registered
during an individual’s adolescent days tends to persist into adulthood resulting in complications
during childbearing for women. According to physicians, adolescence is a critical development
period during which one stands the greatest risk of considerable weight gain (Shin, et al., 2016).
This period is characterized by a considerable change in eating habits, behavior, insulin
sensitivity, psychology adjustment, and body composition. The excess weight gained during
adolescence is normally had to shed one a person enters adulthood. This means that women
maintain unhealthy quantities of body fat during her childbearing years. Development plasticity
takes place during adolescence; this implies that lifelong habits can be initiated during this
critical growth period that with either affect a person’s health positively or negatively. In order
to limit the risk of obesity and eating disorders, adolescents can be motivated to eat sensibly and
engage in more physical activities. Obesity is considered a serious health issue with more than
60% percent of Americans being considered obese or overweight (Shin, et al., 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 8
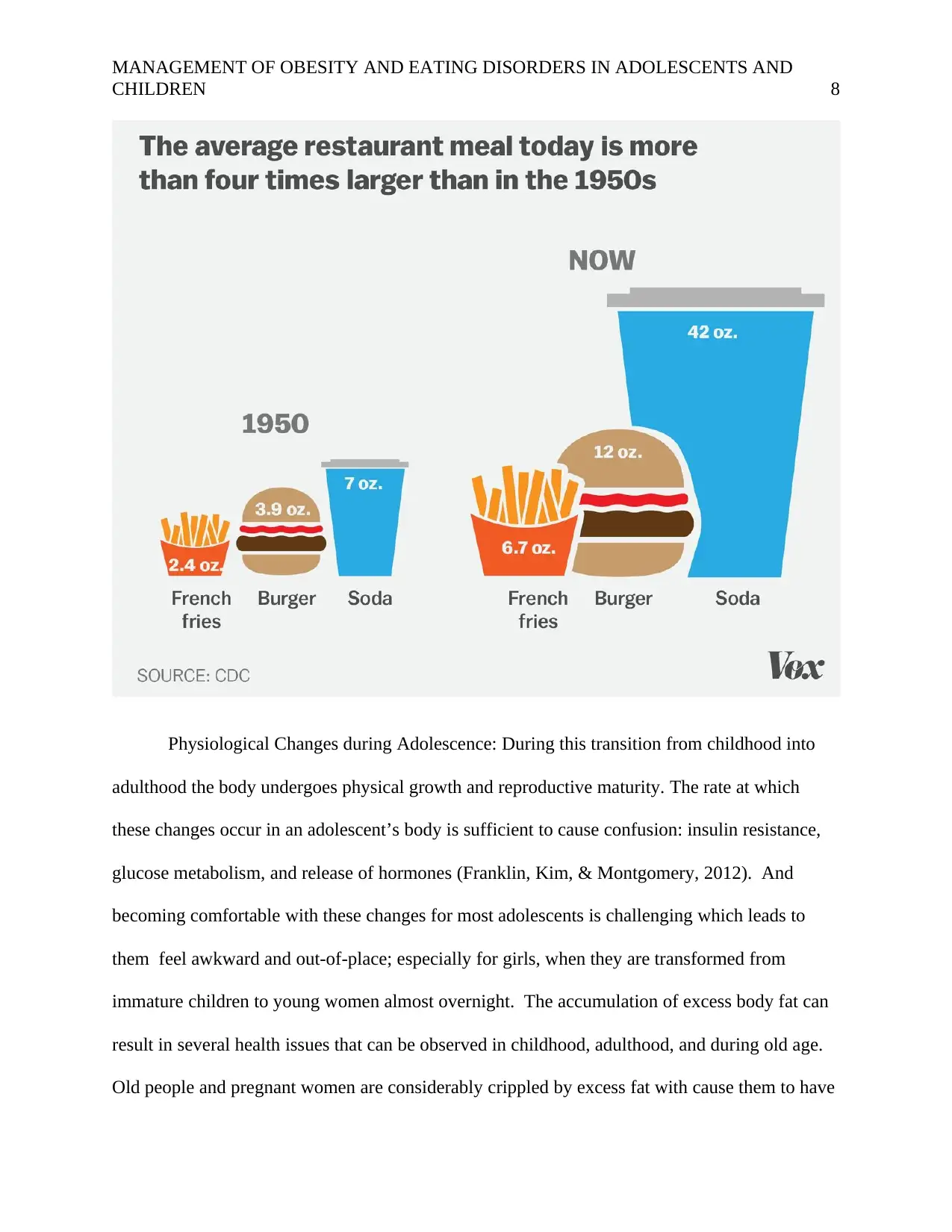
Physiological Changes during Adolescence: During this transition from childhood into
adulthood the body undergoes physical growth and reproductive maturity. The rate at which
these changes occur in an adolescent’s body is sufficient to cause confusion: insulin resistance,
glucose metabolism, and release of hormones (Franklin, Kim, & Montgomery, 2012). And
becoming comfortable with these changes for most adolescents is challenging which leads to
them feel awkward and out-of-place; especially for girls, when they are transformed from
immature children to young women almost overnight. The accumulation of excess body fat can
result in several health issues that can be observed in childhood, adulthood, and during old age.
Old people and pregnant women are considerably crippled by excess fat with cause them to have
CHILDREN 8
Physiological Changes during Adolescence: During this transition from childhood into
adulthood the body undergoes physical growth and reproductive maturity. The rate at which
these changes occur in an adolescent’s body is sufficient to cause confusion: insulin resistance,
glucose metabolism, and release of hormones (Franklin, Kim, & Montgomery, 2012). And
becoming comfortable with these changes for most adolescents is challenging which leads to
them feel awkward and out-of-place; especially for girls, when they are transformed from
immature children to young women almost overnight. The accumulation of excess body fat can
result in several health issues that can be observed in childhood, adulthood, and during old age.
Old people and pregnant women are considerably crippled by excess fat with cause them to have

MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 9
numerous health issues such as joint pains, swollen legs, and extreme shortness of breath. The
risk of contracting serious chronic illness later on in one’s life is greatly increased if that
individual happens to be obese or overweight. Moreover, eating disorders can affect the
sociability of individuals causing them to have problems relating to spouses, children, and
employers (Franklin, Kim, & Montgomery, 2012).
Such rifts in communication cause people with eating disorders to become withdrawn,
lonely, depressed, and low-income earners. Behavioral Changes during Adolescence: the
creation of captivating video gaming technology and the prevalence of smartphone usage has
greatly diminished the desire of children to engage in physical activities around the household
and outdoor games like soccer and athletics (Park, et al., 2017). Medical professionals have in
recent years termed the adolescent years as critical periods during which eating habits can either
make or break a child’s future. This transitional period is normally viewed to be just as important
as the periods when child transition from high school to higher learning institutions and from
higher learning facilities to the entrepreneurial or employment world. It is therefore necessary
that individuals take part in the development of enforceable weight control programs and
awareness incentives that will reduce the number of obese children and adolescent found across
America. It is suspect that out of the more than 60% of American who are
obese/overweight/eating disorder, 45% of this proportion is comprised of children and teenagers
(Park, et al., 2017).
Part c: The analysis time frame
A school-based BMI measurement solution has been developed that seeks to address the
issue of obesity and eating disorders. This idea was created due to the extensive consumption of
CHILDREN 9
numerous health issues such as joint pains, swollen legs, and extreme shortness of breath. The
risk of contracting serious chronic illness later on in one’s life is greatly increased if that
individual happens to be obese or overweight. Moreover, eating disorders can affect the
sociability of individuals causing them to have problems relating to spouses, children, and
employers (Franklin, Kim, & Montgomery, 2012).
Such rifts in communication cause people with eating disorders to become withdrawn,
lonely, depressed, and low-income earners. Behavioral Changes during Adolescence: the
creation of captivating video gaming technology and the prevalence of smartphone usage has
greatly diminished the desire of children to engage in physical activities around the household
and outdoor games like soccer and athletics (Park, et al., 2017). Medical professionals have in
recent years termed the adolescent years as critical periods during which eating habits can either
make or break a child’s future. This transitional period is normally viewed to be just as important
as the periods when child transition from high school to higher learning institutions and from
higher learning facilities to the entrepreneurial or employment world. It is therefore necessary
that individuals take part in the development of enforceable weight control programs and
awareness incentives that will reduce the number of obese children and adolescent found across
America. It is suspect that out of the more than 60% of American who are
obese/overweight/eating disorder, 45% of this proportion is comprised of children and teenagers
(Park, et al., 2017).
Part c: The analysis time frame
A school-based BMI measurement solution has been developed that seeks to address the
issue of obesity and eating disorders. This idea was created due to the extensive consumption of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 10
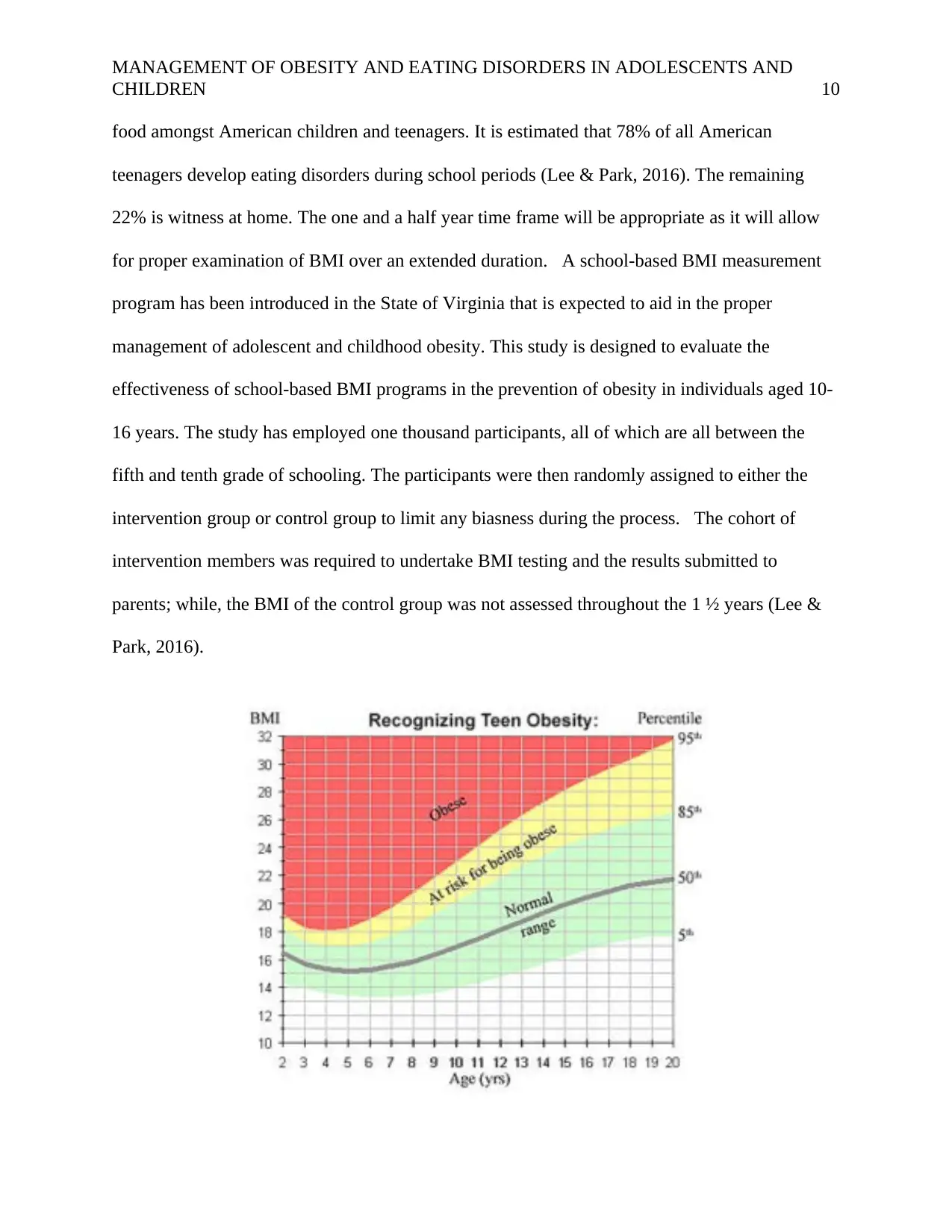
food amongst American children and teenagers. It is estimated that 78% of all American
teenagers develop eating disorders during school periods (Lee & Park, 2016). The remaining
22% is witness at home. The one and a half year time frame will be appropriate as it will allow
for proper examination of BMI over an extended duration. A school-based BMI measurement
program has been introduced in the State of Virginia that is expected to aid in the proper
management of adolescent and childhood obesity. This study is designed to evaluate the
effectiveness of school-based BMI programs in the prevention of obesity in individuals aged 10-
16 years. The study has employed one thousand participants, all of which are all between the
fifth and tenth grade of schooling. The participants were then randomly assigned to either the
intervention group or control group to limit any biasness during the process. The cohort of
intervention members was required to undertake BMI testing and the results submitted to
parents; while, the BMI of the control group was not assessed throughout the 1 ½ years (Lee &
Park, 2016).
CHILDREN 10
food amongst American children and teenagers. It is estimated that 78% of all American
teenagers develop eating disorders during school periods (Lee & Park, 2016). The remaining
22% is witness at home. The one and a half year time frame will be appropriate as it will allow
for proper examination of BMI over an extended duration. A school-based BMI measurement
program has been introduced in the State of Virginia that is expected to aid in the proper
management of adolescent and childhood obesity. This study is designed to evaluate the
effectiveness of school-based BMI programs in the prevention of obesity in individuals aged 10-
16 years. The study has employed one thousand participants, all of which are all between the
fifth and tenth grade of schooling. The participants were then randomly assigned to either the
intervention group or control group to limit any biasness during the process. The cohort of
intervention members was required to undertake BMI testing and the results submitted to
parents; while, the BMI of the control group was not assessed throughout the 1 ½ years (Lee &
Park, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 11
Part d: Data on all types of costs to be collected
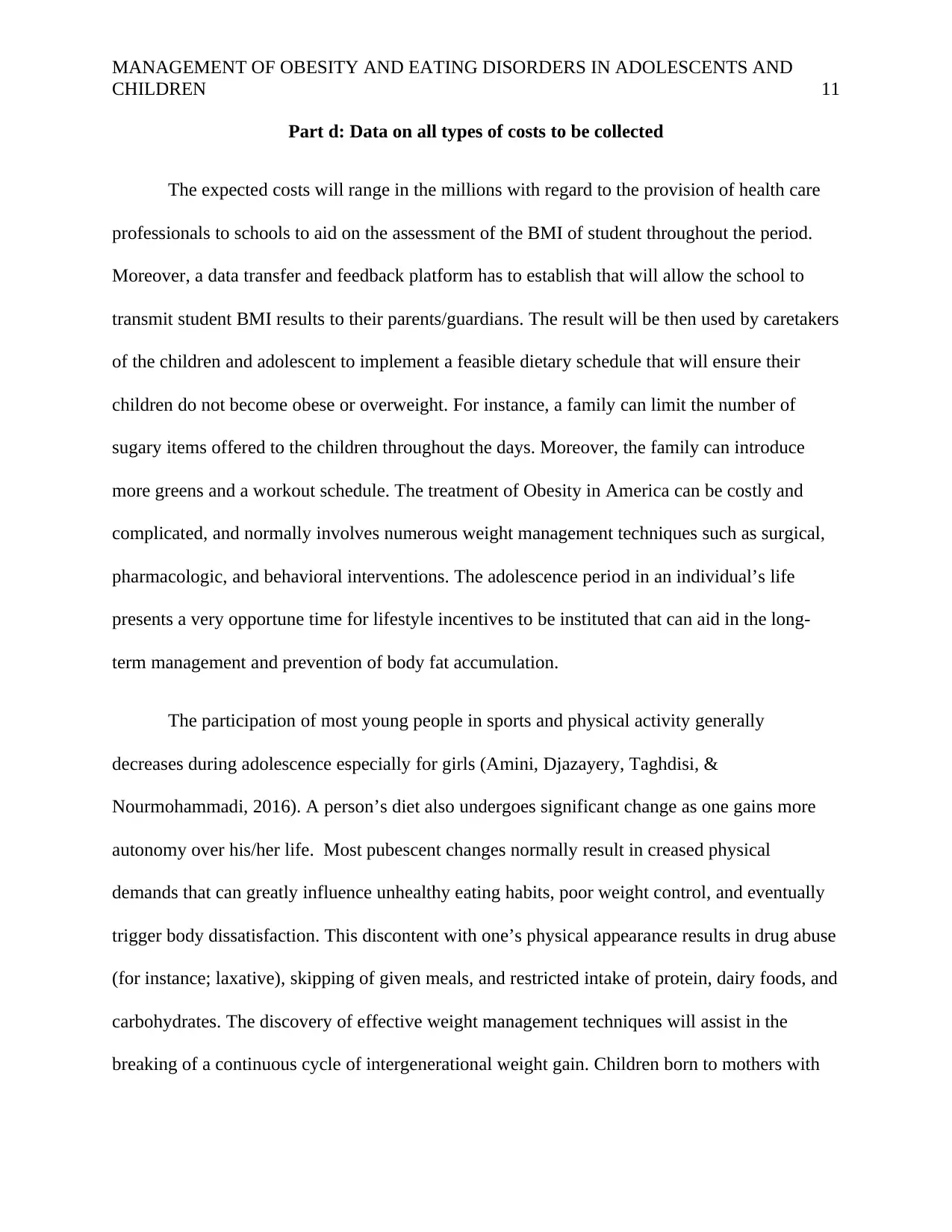
The expected costs will range in the millions with regard to the provision of health care
professionals to schools to aid on the assessment of the BMI of student throughout the period.
Moreover, a data transfer and feedback platform has to establish that will allow the school to
transmit student BMI results to their parents/guardians. The result will be then used by caretakers
of the children and adolescent to implement a feasible dietary schedule that will ensure their
children do not become obese or overweight. For instance, a family can limit the number of
sugary items offered to the children throughout the days. Moreover, the family can introduce
more greens and a workout schedule. The treatment of Obesity in America can be costly and
complicated, and normally involves numerous weight management techniques such as surgical,
pharmacologic, and behavioral interventions. The adolescence period in an individual’s life
presents a very opportune time for lifestyle incentives to be instituted that can aid in the long-
term management and prevention of body fat accumulation.
The participation of most young people in sports and physical activity generally
decreases during adolescence especially for girls (Amini, Djazayery, Taghdisi, &
Nourmohammadi, 2016). A person’s diet also undergoes significant change as one gains more
autonomy over his/her life. Most pubescent changes normally result in creased physical
demands that can greatly influence unhealthy eating habits, poor weight control, and eventually
trigger body dissatisfaction. This discontent with one’s physical appearance results in drug abuse
(for instance; laxative), skipping of given meals, and restricted intake of protein, dairy foods, and
carbohydrates. The discovery of effective weight management techniques will assist in the
breaking of a continuous cycle of intergenerational weight gain. Children born to mothers with
CHILDREN 11
Part d: Data on all types of costs to be collected
The expected costs will range in the millions with regard to the provision of health care
professionals to schools to aid on the assessment of the BMI of student throughout the period.
Moreover, a data transfer and feedback platform has to establish that will allow the school to
transmit student BMI results to their parents/guardians. The result will be then used by caretakers
of the children and adolescent to implement a feasible dietary schedule that will ensure their
children do not become obese or overweight. For instance, a family can limit the number of
sugary items offered to the children throughout the days. Moreover, the family can introduce
more greens and a workout schedule. The treatment of Obesity in America can be costly and
complicated, and normally involves numerous weight management techniques such as surgical,
pharmacologic, and behavioral interventions. The adolescence period in an individual’s life
presents a very opportune time for lifestyle incentives to be instituted that can aid in the long-
term management and prevention of body fat accumulation.
The participation of most young people in sports and physical activity generally
decreases during adolescence especially for girls (Amini, Djazayery, Taghdisi, &
Nourmohammadi, 2016). A person’s diet also undergoes significant change as one gains more
autonomy over his/her life. Most pubescent changes normally result in creased physical
demands that can greatly influence unhealthy eating habits, poor weight control, and eventually
trigger body dissatisfaction. This discontent with one’s physical appearance results in drug abuse
(for instance; laxative), skipping of given meals, and restricted intake of protein, dairy foods, and
carbohydrates. The discovery of effective weight management techniques will assist in the
breaking of a continuous cycle of intergenerational weight gain. Children born to mothers with
MANAGEMENT OF OBESITY AND EATING DISORDERS IN ADOLESCENTS AND
CHILDREN 12
normal weight are at a lower like of becoming obese compared to those born to overweight
women (Amini, Djazayery, Taghdisi, & Nourmohammadi, 2016).
Part e: Data on relevant health outcomes within each of the following time frames
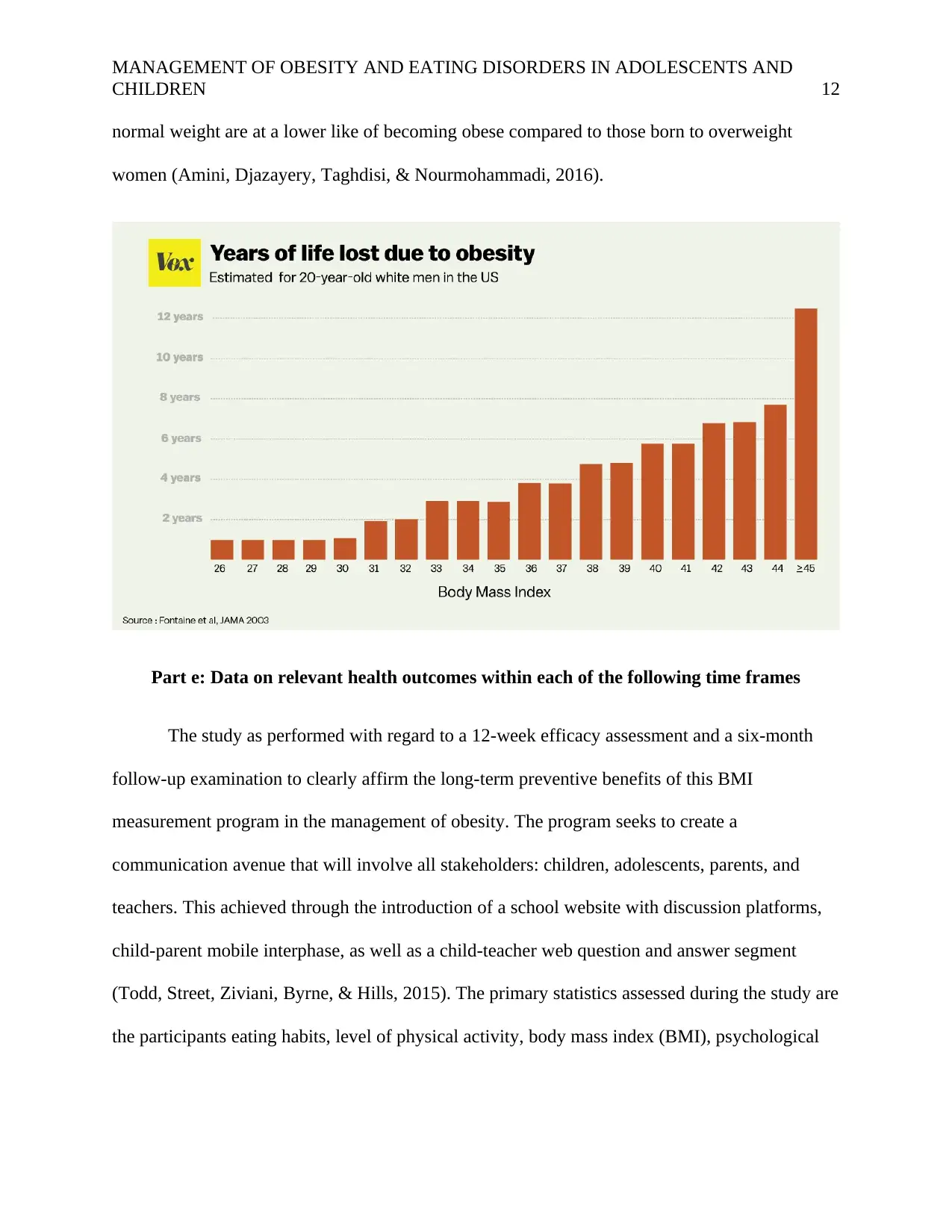
The study as performed with regard to a 12-week efficacy assessment and a six-month
follow-up examination to clearly affirm the long-term preventive benefits of this BMI
measurement program in the management of obesity. The program seeks to create a
communication avenue that will involve all stakeholders: children, adolescents, parents, and
teachers. This achieved through the introduction of a school website with discussion platforms,
child-parent mobile interphase, as well as a child-teacher web question and answer segment
(Todd, Street, Ziviani, Byrne, & Hills, 2015). The primary statistics assessed during the study are
the participants eating habits, level of physical activity, body mass index (BMI), psychological
CHILDREN 12
normal weight are at a lower like of becoming obese compared to those born to overweight
women (Amini, Djazayery, Taghdisi, & Nourmohammadi, 2016).
Part e: Data on relevant health outcomes within each of the following time frames
The study as performed with regard to a 12-week efficacy assessment and a six-month
follow-up examination to clearly affirm the long-term preventive benefits of this BMI
measurement program in the management of obesity. The program seeks to create a
communication avenue that will involve all stakeholders: children, adolescents, parents, and
teachers. This achieved through the introduction of a school website with discussion platforms,
child-parent mobile interphase, as well as a child-teacher web question and answer segment
(Todd, Street, Ziviani, Byrne, & Hills, 2015). The primary statistics assessed during the study are
the participants eating habits, level of physical activity, body mass index (BMI), psychological
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





