Case Study Analysis: Mr. Y's BPAD with Psychosis and Treatment
VerifiedAdded on 2023/01/12
|21
|5331
|50
Case Study
AI Summary
This case study focuses on Mr. Y, a 40-year-old male diagnosed with BPAD with psychosis, detailing his first episode at 18 and subsequent manic episodes. The study explores the challenges of patient engagement, highlighting the importance of building a therapeutic relationship and addressing the biopsychosocial aspects of the illness. It examines the influence of family support, particularly from his brother, and the impact of Mr. Y's symptoms on his professional life. The case delves into the engagement process, the application of cognitive therapy, and the factors that affected the therapeutic relationship. The study also includes a biopsychosocial assessment, covering Mr. Y's chief complaint, psychiatric history, and substance use history. The analysis discusses the positive and challenging aspects of the engagement, and suggests areas for improvement in future interactions. This assignment from Desklib provides a comprehensive overview of the patient's condition, treatment, and the complexities of managing BPAD with psychosis.

Running head: BPAD WITH PSYCHOSIS 1
BPAD with Psychosis
Name
Institutional Affiliation
BPAD with Psychosis
Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BPAD WITH PSYCHOSIS 2
BPAD with Psychosis
Introduction
This case involves a case of Mr. Y who was diagnosed with the BPAD with
psychosis under the treatment of community mental health service. The patient is a male
aged 40 years. He first had his first episode occurring at age 18. At 30, Mr. Y had
evidently had manic episodes because he had been known to contact clients and
colleagues at odd hours to deliberate new ideas. Mr. Y kept enthusing regarding his
designs being original and imaginative. At his place of work, colleagues and clients
would usually complain regarding his unprofessional conduct suggesting a
misunderstanding on the part of his place of work. Mr. Y’s denial if his disease
additionally aggravated his condition. He had already exited two excellent jobs due to his
condition.
Part A) Engagement and Context
Various factors influenced my engagement with the patient and family/whanau in
both specific session and over multiple interactions. While it has been irrationally thought
that engagement within the field of nursing need to be significantly started by nurse, I have
realized that facilitating effective engagement needs inputs from a nurse, patient and
families to find “common” ground.
I came to appreciate that empowering a patient is key to management of BPAD
with psychosis (Shardlow et al., 2015). I applied the metaphorical bridge concept which I
sought to build, and this allowed me and the patient to cross back and forth to each one’s
domain. This theory allowed me as a nurse to acknowledge Mr. Y’s needs, goals or
problems hence enabling my patient to get insight into his condition, and to fathom what I
BPAD with Psychosis
Introduction
This case involves a case of Mr. Y who was diagnosed with the BPAD with
psychosis under the treatment of community mental health service. The patient is a male
aged 40 years. He first had his first episode occurring at age 18. At 30, Mr. Y had
evidently had manic episodes because he had been known to contact clients and
colleagues at odd hours to deliberate new ideas. Mr. Y kept enthusing regarding his
designs being original and imaginative. At his place of work, colleagues and clients
would usually complain regarding his unprofessional conduct suggesting a
misunderstanding on the part of his place of work. Mr. Y’s denial if his disease
additionally aggravated his condition. He had already exited two excellent jobs due to his
condition.
Part A) Engagement and Context
Various factors influenced my engagement with the patient and family/whanau in
both specific session and over multiple interactions. While it has been irrationally thought
that engagement within the field of nursing need to be significantly started by nurse, I have
realized that facilitating effective engagement needs inputs from a nurse, patient and
families to find “common” ground.
I came to appreciate that empowering a patient is key to management of BPAD
with psychosis (Shardlow et al., 2015). I applied the metaphorical bridge concept which I
sought to build, and this allowed me and the patient to cross back and forth to each one’s
domain. This theory allowed me as a nurse to acknowledge Mr. Y’s needs, goals or
problems hence enabling my patient to get insight into his condition, and to fathom what I
BPAD WITH PSYCHOSIS 3
was trying to facilitate.
I came to appreciate that a bridge between myself and Mr. Y was advantageous,
however, the challenge I recognized was how to obtain the desired resources. This is
because the rapport between me and the patient remains extremely sensitive process, and
many nurses and patient take months or weeks, or sometimes never. Thus, I knew I had a
lot of pressure exerted on me to facilitate the connection, specifically when considering
that I might have to make a formal assessment of a patient within minutes of coming into
contact with one another.
To assess my client, I had ensure I build a therapeutic relationship with Mr. Y and
implement it as soon as I could. I had recognized that therapeutic relationship remains
central aspect in nursing procedure or process. I knew that without such a relationship, my
client cold feel as though no empathy, trust or sympathy accorded by to him by me. I
understood that I had to obtain the patient’s trust to establish a meaningful therapeutic
relationship by assessing him via interview. It was only after I had built this relationship
that Mr. Y trusted me enough to get open and expressive.
I built this therapeutic relationship through a mutual respect between the client and
myself. I appreciated the importance of trust as the most influential factor. Also, used
excellent communication and interpersonal skills. I focused on ensuring that Mr. Y felt
respected, confident and important to communicate all his concerns and able to trust me. I
appreciate the importance of such personal qualities as compassion, empathy, caring, trust,
respect friendly, honesty and outstanding communication skills and I used them to build
therapeutic relationship with my patient (Macnair, 2008). This allowed me to connect with
the patient emotionally and empathize with Mr. Y by appreciating what the patient was
undergoing through and putting myself in his situation (Smith, Segal, and Segal, 2009).
The theoretical framework that helped me in this case was a bio psychological
was trying to facilitate.
I came to appreciate that a bridge between myself and Mr. Y was advantageous,
however, the challenge I recognized was how to obtain the desired resources. This is
because the rapport between me and the patient remains extremely sensitive process, and
many nurses and patient take months or weeks, or sometimes never. Thus, I knew I had a
lot of pressure exerted on me to facilitate the connection, specifically when considering
that I might have to make a formal assessment of a patient within minutes of coming into
contact with one another.
To assess my client, I had ensure I build a therapeutic relationship with Mr. Y and
implement it as soon as I could. I had recognized that therapeutic relationship remains
central aspect in nursing procedure or process. I knew that without such a relationship, my
client cold feel as though no empathy, trust or sympathy accorded by to him by me. I
understood that I had to obtain the patient’s trust to establish a meaningful therapeutic
relationship by assessing him via interview. It was only after I had built this relationship
that Mr. Y trusted me enough to get open and expressive.
I built this therapeutic relationship through a mutual respect between the client and
myself. I appreciated the importance of trust as the most influential factor. Also, used
excellent communication and interpersonal skills. I focused on ensuring that Mr. Y felt
respected, confident and important to communicate all his concerns and able to trust me. I
appreciate the importance of such personal qualities as compassion, empathy, caring, trust,
respect friendly, honesty and outstanding communication skills and I used them to build
therapeutic relationship with my patient (Macnair, 2008). This allowed me to connect with
the patient emotionally and empathize with Mr. Y by appreciating what the patient was
undergoing through and putting myself in his situation (Smith, Segal, and Segal, 2009).
The theoretical framework that helped me in this case was a bio psychological
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BPAD WITH PSYCHOSIS 4
framework. According to O’Carroll & Park (2007), suggested that any biological,
sociological and psychological issues of the client has to be acknowledged and integrated
into any future plan of care. I used this framework to help not to only address the
psychological issues that Mr. Y had since this would have limited my ability to deal with
main cause of this mental health problem including medical, family or financial issues
contributing to diagnosis.
Key factors that affected Engagement
The person factors that significantly affected my engagement with Mr. Y are
family, symptoms and beliefs. In term of family, Mr. Y had a supportive family that
made our engagement very easy. His brother (Smith) was supportive and showed a lot of
empathy and sympathy for his brother’s condition. He was always around to encourage
his brother to be confident and expressive of all his concerns to give me as much
information as possible during my interview. Indeed, it is Mr. Y’s brother who had really
got him to go back to medicines after he had stopped. Smith had also tried so much to
know what took place and had ensured that Mr. Y took hi medicines as required.
Smith further managed to get his sick brother to his consultant psychiatrist. Thus,
it might be perceived that it was his brother and family support together with a
discriminative behavior at his place of work that had pushed him to medication. His
brother were helpful in giving me the required information about my patient medical
history and this made me gather the required information I used to help him. Through his
brother, I managed to get someone who trusted what I was doing to the patient and this
gave me confidence. Also, because Mr. Y was a bit used to his brother he participated
well in the interview when he brother talked to him to be expressive and confident.
framework. According to O’Carroll & Park (2007), suggested that any biological,
sociological and psychological issues of the client has to be acknowledged and integrated
into any future plan of care. I used this framework to help not to only address the
psychological issues that Mr. Y had since this would have limited my ability to deal with
main cause of this mental health problem including medical, family or financial issues
contributing to diagnosis.
Key factors that affected Engagement
The person factors that significantly affected my engagement with Mr. Y are
family, symptoms and beliefs. In term of family, Mr. Y had a supportive family that
made our engagement very easy. His brother (Smith) was supportive and showed a lot of
empathy and sympathy for his brother’s condition. He was always around to encourage
his brother to be confident and expressive of all his concerns to give me as much
information as possible during my interview. Indeed, it is Mr. Y’s brother who had really
got him to go back to medicines after he had stopped. Smith had also tried so much to
know what took place and had ensured that Mr. Y took hi medicines as required.
Smith further managed to get his sick brother to his consultant psychiatrist. Thus,
it might be perceived that it was his brother and family support together with a
discriminative behavior at his place of work that had pushed him to medication. His
brother were helpful in giving me the required information about my patient medical
history and this made me gather the required information I used to help him. Through his
brother, I managed to get someone who trusted what I was doing to the patient and this
gave me confidence. Also, because Mr. Y was a bit used to his brother he participated
well in the interview when he brother talked to him to be expressive and confident.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BPAD WITH PSYCHOSIS 5
Through, Smith helped me built a rapport with his sick brother.
In regards to symptoms, Mr. Y symptoms had contributed to him quitting the
jobs despite being a talented architect. Mr. Y showed a discriminative behavior in his
place of work and he had developed a stage of bipolar disorder where he had regular
manic attack coupled with psychosis. The symptoms of Mr. Y and the resulting
consequences made me empathize with him.
For instance, he lacked support from his employers and colleagues which had
aggravated his medical condition. This made me feel empathetic towards him since
while his employers and colleagues ought to supported, he was discriminated and
rejected every time. I felt so emotionally connected to Mr. Y when he told me how he
had been forced to quit his positons in well-paying jobs because of his condition, and got
rejected in new five positions he had applied.
I used the cognitive therapy to help Mr. Y. This helped me appreciate how Mr. Y
was perceiving and structuring the world by looking at his past experiences and relation
with his colleagues, families and employers which affected his “cognition.” This
explains why Mr. Y was interpreting all his experience based on whether he is adequate
or competent which makes his thinking being dominated by schema. Mr. Y thought that
unless he does everything perfectly, he is a failure.
Thus, this symptoms made me empathize with Mr. Y because it was so emotional
seeing him react to all scenarios based on his competence even where such situations
were never linked to his competence. Despite his impressive resume, he got rejected and
hence felt disadvantaged thinking it was a result of his mental disorder. Such inequalities
made Mr. Y wanted to hide his illness and never revealing it unless it was particularly
asked about.
Through, Smith helped me built a rapport with his sick brother.
In regards to symptoms, Mr. Y symptoms had contributed to him quitting the
jobs despite being a talented architect. Mr. Y showed a discriminative behavior in his
place of work and he had developed a stage of bipolar disorder where he had regular
manic attack coupled with psychosis. The symptoms of Mr. Y and the resulting
consequences made me empathize with him.
For instance, he lacked support from his employers and colleagues which had
aggravated his medical condition. This made me feel empathetic towards him since
while his employers and colleagues ought to supported, he was discriminated and
rejected every time. I felt so emotionally connected to Mr. Y when he told me how he
had been forced to quit his positons in well-paying jobs because of his condition, and got
rejected in new five positions he had applied.
I used the cognitive therapy to help Mr. Y. This helped me appreciate how Mr. Y
was perceiving and structuring the world by looking at his past experiences and relation
with his colleagues, families and employers which affected his “cognition.” This
explains why Mr. Y was interpreting all his experience based on whether he is adequate
or competent which makes his thinking being dominated by schema. Mr. Y thought that
unless he does everything perfectly, he is a failure.
Thus, this symptoms made me empathize with Mr. Y because it was so emotional
seeing him react to all scenarios based on his competence even where such situations
were never linked to his competence. Despite his impressive resume, he got rejected and
hence felt disadvantaged thinking it was a result of his mental disorder. Such inequalities
made Mr. Y wanted to hide his illness and never revealing it unless it was particularly
asked about.
BPAD WITH PSYCHOSIS 6
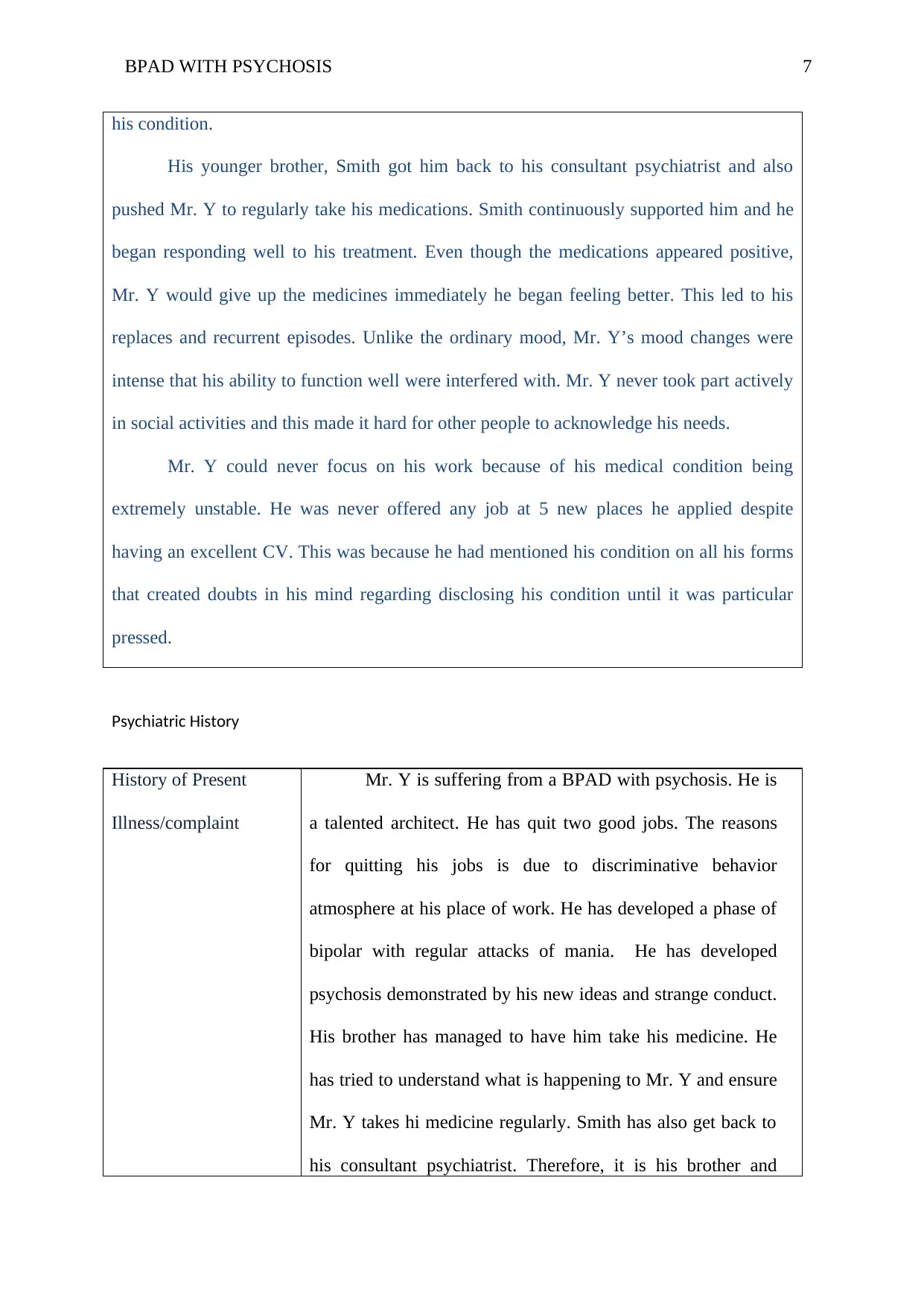
What worked well, challenging and what to be done differently
In general some my engagement with Mr. Y went on well, though it also had some
challenges. The presence of Mr. Y’s brother, Smith was of a great help to building a
therapeutic relationship between me, patient and the family. Smith was also instrumental in
revealing most of Mr. Y’s past medical history so that worked well in helping know what
kind of treatment I could recommend to Mr. Y. Another positive thing was that Mr. Y was
able be expressive and he trusted me and talked about all his concerns.
The challenge was that Mr. Y did not feel encouraged initially as he thought I
would also discriminate him like his former colleagues and employees which made him
initially to be unwilling to communicate. Also, at times, I felt so bad listening to Mr. Y
talking about his tribulations and I became emotional sometimes, but I overcame the
situation and the session went well ultimately. Next time, I would try not to get emotional
since I have realized that this would make the client lose trust in me and think that his
problem is so severe that he cannot get help.
Part B) Biopsychosocial Assessment (approx 1100)
Chief complaint and Reasons for Evaluation
Mr. Y had a BPAD with psychosis with first episode taking place at eighteen years.
At twenty-eight, Mr. Y apparently had manic episodes. This is known by Mr. Y’s behavior
of contacting colleagues and clients at odd hours to deliberate on new ideas. Mr. Y kept
enthusing regarding his designs being original and imaginative. At the his place of work,
colleagues and clients would usually complain regarding his unprofessional conduct
indicating that he lacked understanding on the part of his place of work. Mr. Y’s denial of
his illness additionally complicated his situation. He had quit two outstanding jobs due to
What worked well, challenging and what to be done differently
In general some my engagement with Mr. Y went on well, though it also had some
challenges. The presence of Mr. Y’s brother, Smith was of a great help to building a
therapeutic relationship between me, patient and the family. Smith was also instrumental in
revealing most of Mr. Y’s past medical history so that worked well in helping know what
kind of treatment I could recommend to Mr. Y. Another positive thing was that Mr. Y was
able be expressive and he trusted me and talked about all his concerns.
The challenge was that Mr. Y did not feel encouraged initially as he thought I
would also discriminate him like his former colleagues and employees which made him
initially to be unwilling to communicate. Also, at times, I felt so bad listening to Mr. Y
talking about his tribulations and I became emotional sometimes, but I overcame the
situation and the session went well ultimately. Next time, I would try not to get emotional
since I have realized that this would make the client lose trust in me and think that his
problem is so severe that he cannot get help.
Part B) Biopsychosocial Assessment (approx 1100)
Chief complaint and Reasons for Evaluation
Mr. Y had a BPAD with psychosis with first episode taking place at eighteen years.
At twenty-eight, Mr. Y apparently had manic episodes. This is known by Mr. Y’s behavior
of contacting colleagues and clients at odd hours to deliberate on new ideas. Mr. Y kept
enthusing regarding his designs being original and imaginative. At the his place of work,
colleagues and clients would usually complain regarding his unprofessional conduct
indicating that he lacked understanding on the part of his place of work. Mr. Y’s denial of
his illness additionally complicated his situation. He had quit two outstanding jobs due to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BPAD WITH PSYCHOSIS 7
his condition.
His younger brother, Smith got him back to his consultant psychiatrist and also
pushed Mr. Y to regularly take his medications. Smith continuously supported him and he
began responding well to his treatment. Even though the medications appeared positive,
Mr. Y would give up the medicines immediately he began feeling better. This led to his
replaces and recurrent episodes. Unlike the ordinary mood, Mr. Y’s mood changes were
intense that his ability to function well were interfered with. Mr. Y never took part actively
in social activities and this made it hard for other people to acknowledge his needs.
Mr. Y could never focus on his work because of his medical condition being
extremely unstable. He was never offered any job at 5 new places he applied despite
having an excellent CV. This was because he had mentioned his condition on all his forms
that created doubts in his mind regarding disclosing his condition until it was particular
pressed.
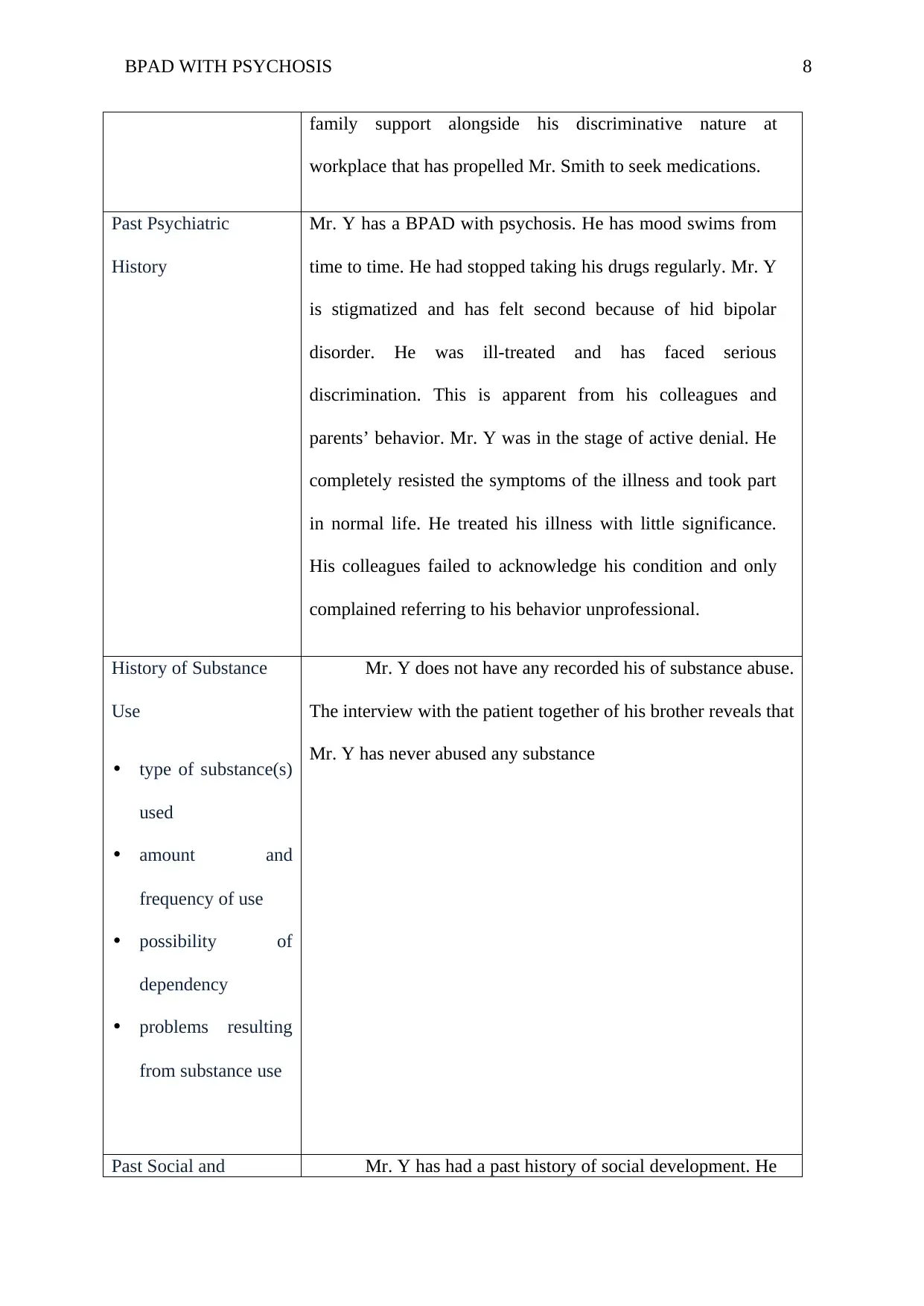
Psychiatric History
History of Present
Illness/complaint
Mr. Y is suffering from a BPAD with psychosis. He is
a talented architect. He has quit two good jobs. The reasons
for quitting his jobs is due to discriminative behavior
atmosphere at his place of work. He has developed a phase of
bipolar with regular attacks of mania. He has developed
psychosis demonstrated by his new ideas and strange conduct.
His brother has managed to have him take his medicine. He
has tried to understand what is happening to Mr. Y and ensure
Mr. Y takes hi medicine regularly. Smith has also get back to
his consultant psychiatrist. Therefore, it is his brother and
his condition.
His younger brother, Smith got him back to his consultant psychiatrist and also
pushed Mr. Y to regularly take his medications. Smith continuously supported him and he
began responding well to his treatment. Even though the medications appeared positive,
Mr. Y would give up the medicines immediately he began feeling better. This led to his
replaces and recurrent episodes. Unlike the ordinary mood, Mr. Y’s mood changes were
intense that his ability to function well were interfered with. Mr. Y never took part actively
in social activities and this made it hard for other people to acknowledge his needs.
Mr. Y could never focus on his work because of his medical condition being
extremely unstable. He was never offered any job at 5 new places he applied despite
having an excellent CV. This was because he had mentioned his condition on all his forms
that created doubts in his mind regarding disclosing his condition until it was particular
pressed.
Psychiatric History
History of Present
Illness/complaint
Mr. Y is suffering from a BPAD with psychosis. He is
a talented architect. He has quit two good jobs. The reasons
for quitting his jobs is due to discriminative behavior
atmosphere at his place of work. He has developed a phase of
bipolar with regular attacks of mania. He has developed
psychosis demonstrated by his new ideas and strange conduct.
His brother has managed to have him take his medicine. He
has tried to understand what is happening to Mr. Y and ensure
Mr. Y takes hi medicine regularly. Smith has also get back to
his consultant psychiatrist. Therefore, it is his brother and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BPAD WITH PSYCHOSIS 8
family support alongside his discriminative nature at
workplace that has propelled Mr. Smith to seek medications.
Past Psychiatric
History
Mr. Y has a BPAD with psychosis. He has mood swims from
time to time. He had stopped taking his drugs regularly. Mr. Y
is stigmatized and has felt second because of hid bipolar
disorder. He was ill-treated and has faced serious
discrimination. This is apparent from his colleagues and
parents’ behavior. Mr. Y was in the stage of active denial. He
completely resisted the symptoms of the illness and took part
in normal life. He treated his illness with little significance.
His colleagues failed to acknowledge his condition and only
complained referring to his behavior unprofessional.
History of Substance
Use
• type of substance(s)
used
• amount and
frequency of use
• possibility of
dependency
• problems resulting
from substance use
Mr. Y does not have any recorded his of substance abuse.
The interview with the patient together of his brother reveals that
Mr. Y has never abused any substance
Past Social and Mr. Y has had a past history of social development. He
family support alongside his discriminative nature at
workplace that has propelled Mr. Smith to seek medications.
Past Psychiatric
History
Mr. Y has a BPAD with psychosis. He has mood swims from
time to time. He had stopped taking his drugs regularly. Mr. Y
is stigmatized and has felt second because of hid bipolar
disorder. He was ill-treated and has faced serious
discrimination. This is apparent from his colleagues and
parents’ behavior. Mr. Y was in the stage of active denial. He
completely resisted the symptoms of the illness and took part
in normal life. He treated his illness with little significance.
His colleagues failed to acknowledge his condition and only
complained referring to his behavior unprofessional.
History of Substance
Use
• type of substance(s)
used
• amount and
frequency of use
• possibility of
dependency
• problems resulting
from substance use
Mr. Y does not have any recorded his of substance abuse.
The interview with the patient together of his brother reveals that
Mr. Y has never abused any substance
Past Social and Mr. Y has had a past history of social development. He
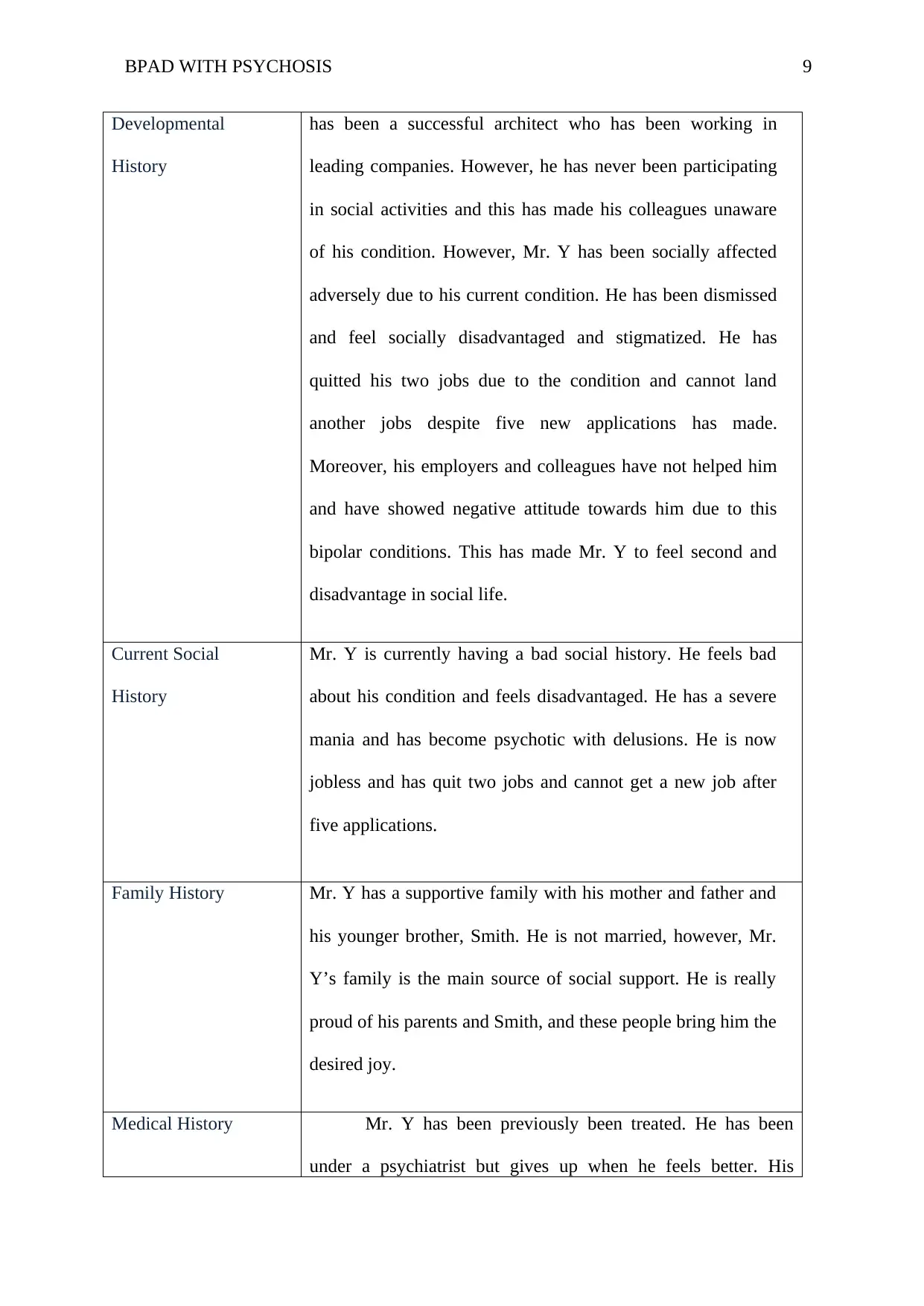
BPAD WITH PSYCHOSIS 9
Developmental
History
has been a successful architect who has been working in
leading companies. However, he has never been participating
in social activities and this has made his colleagues unaware
of his condition. However, Mr. Y has been socially affected
adversely due to his current condition. He has been dismissed
and feel socially disadvantaged and stigmatized. He has
quitted his two jobs due to the condition and cannot land
another jobs despite five new applications has made.
Moreover, his employers and colleagues have not helped him
and have showed negative attitude towards him due to this
bipolar conditions. This has made Mr. Y to feel second and
disadvantage in social life.
Current Social
History
Mr. Y is currently having a bad social history. He feels bad
about his condition and feels disadvantaged. He has a severe
mania and has become psychotic with delusions. He is now
jobless and has quit two jobs and cannot get a new job after
five applications.
Family History Mr. Y has a supportive family with his mother and father and
his younger brother, Smith. He is not married, however, Mr.
Y’s family is the main source of social support. He is really
proud of his parents and Smith, and these people bring him the
desired joy.
Medical History Mr. Y has been previously been treated. He has been
under a psychiatrist but gives up when he feels better. His
Developmental
History
has been a successful architect who has been working in
leading companies. However, he has never been participating
in social activities and this has made his colleagues unaware
of his condition. However, Mr. Y has been socially affected
adversely due to his current condition. He has been dismissed
and feel socially disadvantaged and stigmatized. He has
quitted his two jobs due to the condition and cannot land
another jobs despite five new applications has made.
Moreover, his employers and colleagues have not helped him
and have showed negative attitude towards him due to this
bipolar conditions. This has made Mr. Y to feel second and
disadvantage in social life.
Current Social
History
Mr. Y is currently having a bad social history. He feels bad
about his condition and feels disadvantaged. He has a severe
mania and has become psychotic with delusions. He is now
jobless and has quit two jobs and cannot get a new job after
five applications.
Family History Mr. Y has a supportive family with his mother and father and
his younger brother, Smith. He is not married, however, Mr.
Y’s family is the main source of social support. He is really
proud of his parents and Smith, and these people bring him the
desired joy.
Medical History Mr. Y has been previously been treated. He has been
under a psychiatrist but gives up when he feels better. His
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
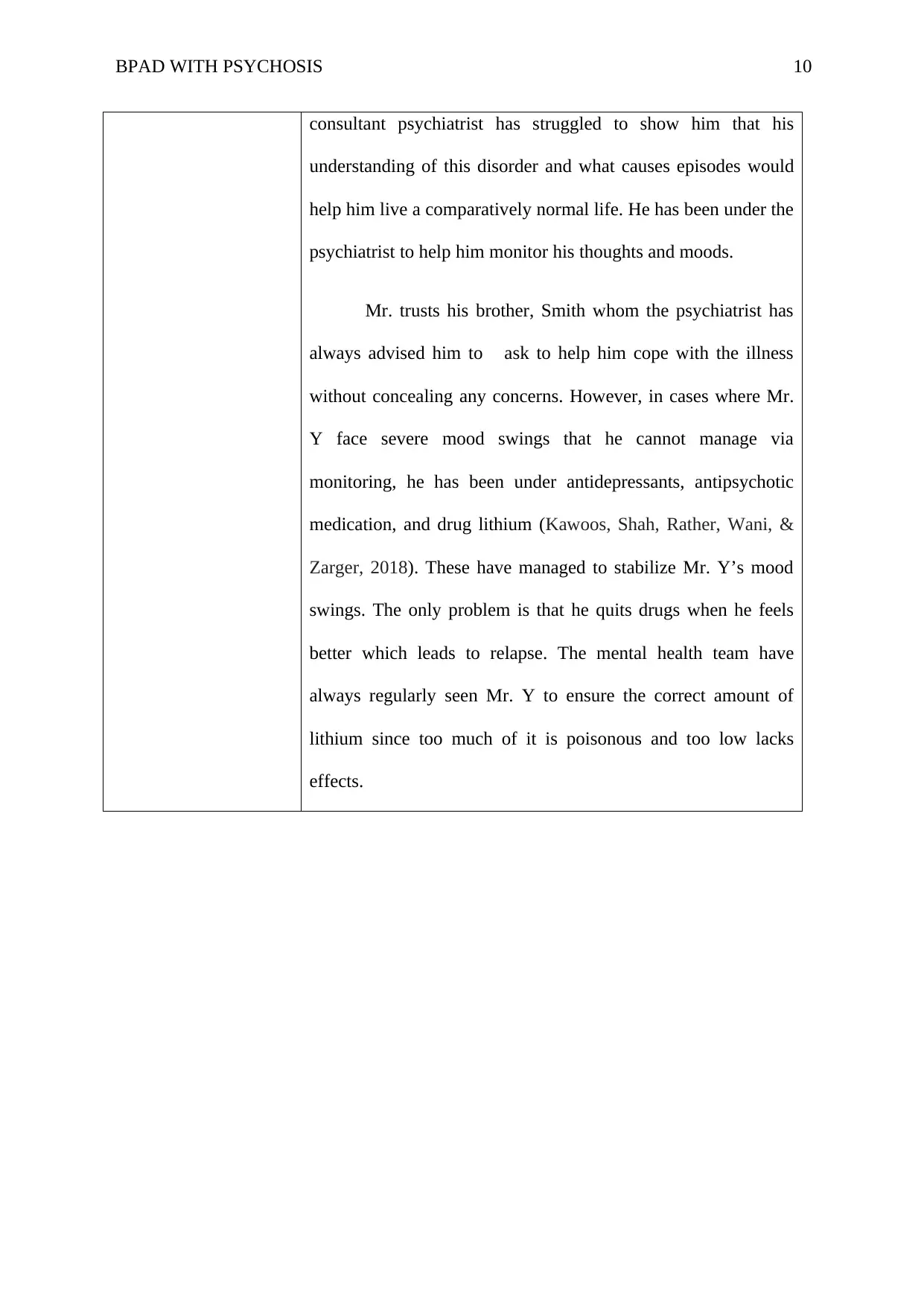
BPAD WITH PSYCHOSIS 10
consultant psychiatrist has struggled to show him that his
understanding of this disorder and what causes episodes would
help him live a comparatively normal life. He has been under the
psychiatrist to help him monitor his thoughts and moods.
Mr. trusts his brother, Smith whom the psychiatrist has
always advised him to ask to help him cope with the illness
without concealing any concerns. However, in cases where Mr.
Y face severe mood swings that he cannot manage via
monitoring, he has been under antidepressants, antipsychotic
medication, and drug lithium (Kawoos, Shah, Rather, Wani, &
Zarger, 2018). These have managed to stabilize Mr. Y’s mood
swings. The only problem is that he quits drugs when he feels
better which leads to relapse. The mental health team have
always regularly seen Mr. Y to ensure the correct amount of
lithium since too much of it is poisonous and too low lacks
effects.
consultant psychiatrist has struggled to show him that his
understanding of this disorder and what causes episodes would
help him live a comparatively normal life. He has been under the
psychiatrist to help him monitor his thoughts and moods.
Mr. trusts his brother, Smith whom the psychiatrist has
always advised him to ask to help him cope with the illness
without concealing any concerns. However, in cases where Mr.
Y face severe mood swings that he cannot manage via
monitoring, he has been under antidepressants, antipsychotic
medication, and drug lithium (Kawoos, Shah, Rather, Wani, &
Zarger, 2018). These have managed to stabilize Mr. Y’s mood
swings. The only problem is that he quits drugs when he feels
better which leads to relapse. The mental health team have
always regularly seen Mr. Y to ensure the correct amount of
lithium since too much of it is poisonous and too low lacks
effects.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BPAD WITH PSYCHOSIS 11
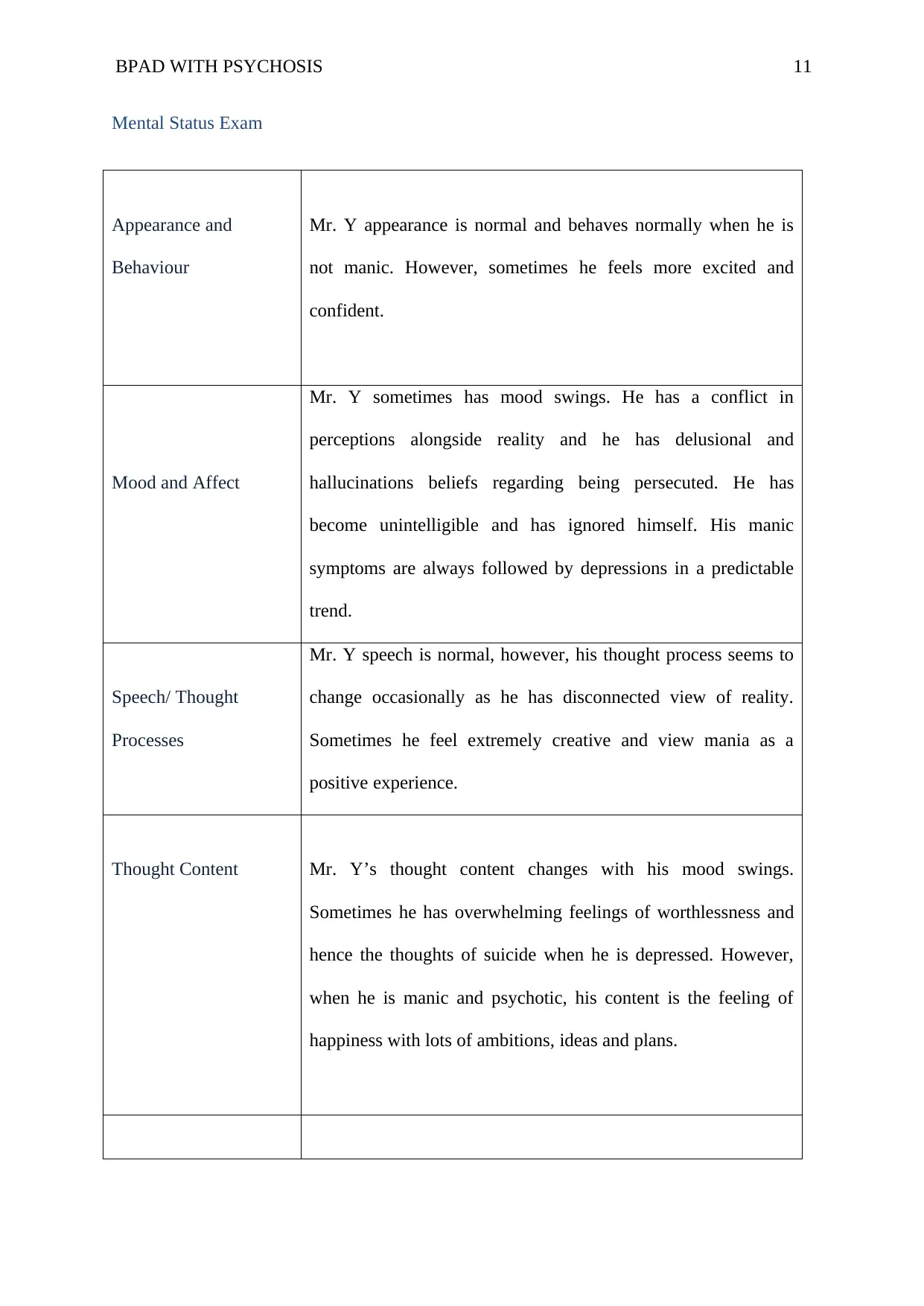
Mental Status Exam
Appearance and
Behaviour
Mr. Y appearance is normal and behaves normally when he is
not manic. However, sometimes he feels more excited and
confident.
Mood and Affect
Mr. Y sometimes has mood swings. He has a conflict in
perceptions alongside reality and he has delusional and
hallucinations beliefs regarding being persecuted. He has
become unintelligible and has ignored himself. His manic
symptoms are always followed by depressions in a predictable
trend.
Speech/ Thought
Processes
Mr. Y speech is normal, however, his thought process seems to
change occasionally as he has disconnected view of reality.
Sometimes he feel extremely creative and view mania as a
positive experience.
Thought Content Mr. Y’s thought content changes with his mood swings.
Sometimes he has overwhelming feelings of worthlessness and
hence the thoughts of suicide when he is depressed. However,
when he is manic and psychotic, his content is the feeling of
happiness with lots of ambitions, ideas and plans.
Mental Status Exam
Appearance and
Behaviour
Mr. Y appearance is normal and behaves normally when he is
not manic. However, sometimes he feels more excited and
confident.
Mood and Affect
Mr. Y sometimes has mood swings. He has a conflict in
perceptions alongside reality and he has delusional and
hallucinations beliefs regarding being persecuted. He has
become unintelligible and has ignored himself. His manic
symptoms are always followed by depressions in a predictable
trend.
Speech/ Thought
Processes
Mr. Y speech is normal, however, his thought process seems to
change occasionally as he has disconnected view of reality.
Sometimes he feel extremely creative and view mania as a
positive experience.
Thought Content Mr. Y’s thought content changes with his mood swings.
Sometimes he has overwhelming feelings of worthlessness and
hence the thoughts of suicide when he is depressed. However,
when he is manic and psychotic, his content is the feeling of
happiness with lots of ambitions, ideas and plans.
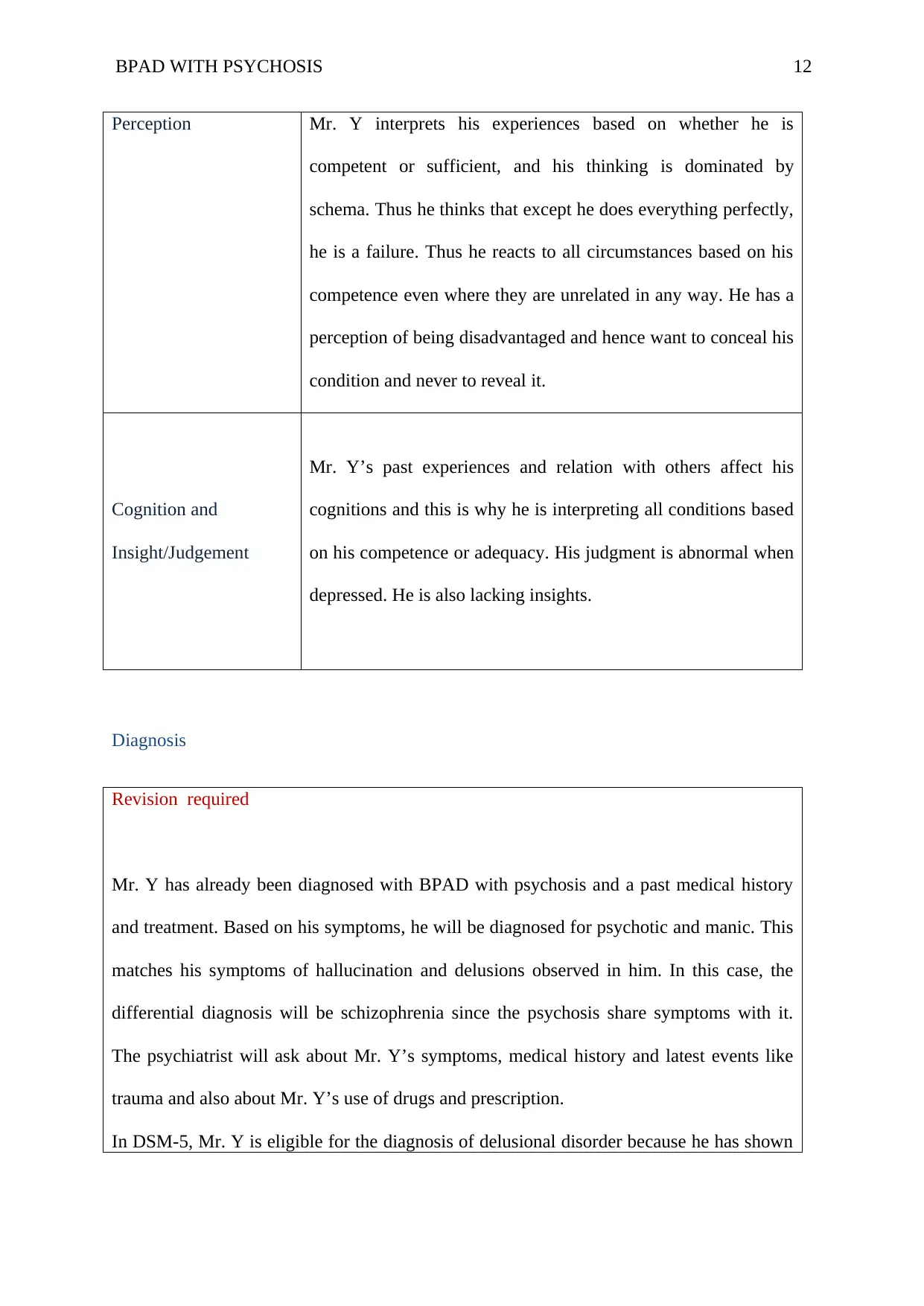
BPAD WITH PSYCHOSIS 12
Perception Mr. Y interprets his experiences based on whether he is
competent or sufficient, and his thinking is dominated by
schema. Thus he thinks that except he does everything perfectly,
he is a failure. Thus he reacts to all circumstances based on his
competence even where they are unrelated in any way. He has a
perception of being disadvantaged and hence want to conceal his
condition and never to reveal it.
Cognition and
Insight/Judgement
Mr. Y’s past experiences and relation with others affect his
cognitions and this is why he is interpreting all conditions based
on his competence or adequacy. His judgment is abnormal when
depressed. He is also lacking insights.
Diagnosis
Revision required
Mr. Y has already been diagnosed with BPAD with psychosis and a past medical history
and treatment. Based on his symptoms, he will be diagnosed for psychotic and manic. This
matches his symptoms of hallucination and delusions observed in him. In this case, the
differential diagnosis will be schizophrenia since the psychosis share symptoms with it.
The psychiatrist will ask about Mr. Y’s symptoms, medical history and latest events like
trauma and also about Mr. Y’s use of drugs and prescription.
In DSM-5, Mr. Y is eligible for the diagnosis of delusional disorder because he has shown
Perception Mr. Y interprets his experiences based on whether he is
competent or sufficient, and his thinking is dominated by
schema. Thus he thinks that except he does everything perfectly,
he is a failure. Thus he reacts to all circumstances based on his
competence even where they are unrelated in any way. He has a
perception of being disadvantaged and hence want to conceal his
condition and never to reveal it.
Cognition and
Insight/Judgement
Mr. Y’s past experiences and relation with others affect his
cognitions and this is why he is interpreting all conditions based
on his competence or adequacy. His judgment is abnormal when
depressed. He is also lacking insights.
Diagnosis
Revision required
Mr. Y has already been diagnosed with BPAD with psychosis and a past medical history
and treatment. Based on his symptoms, he will be diagnosed for psychotic and manic. This
matches his symptoms of hallucination and delusions observed in him. In this case, the
differential diagnosis will be schizophrenia since the psychosis share symptoms with it.
The psychiatrist will ask about Mr. Y’s symptoms, medical history and latest events like
trauma and also about Mr. Y’s use of drugs and prescription.
In DSM-5, Mr. Y is eligible for the diagnosis of delusional disorder because he has shown
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




