ACOM103: A Comparative Essay on Buruli Ulcer and Yaws Diseases
VerifiedAdded on 2023/03/21
|3
|773
|74
Essay
AI Summary
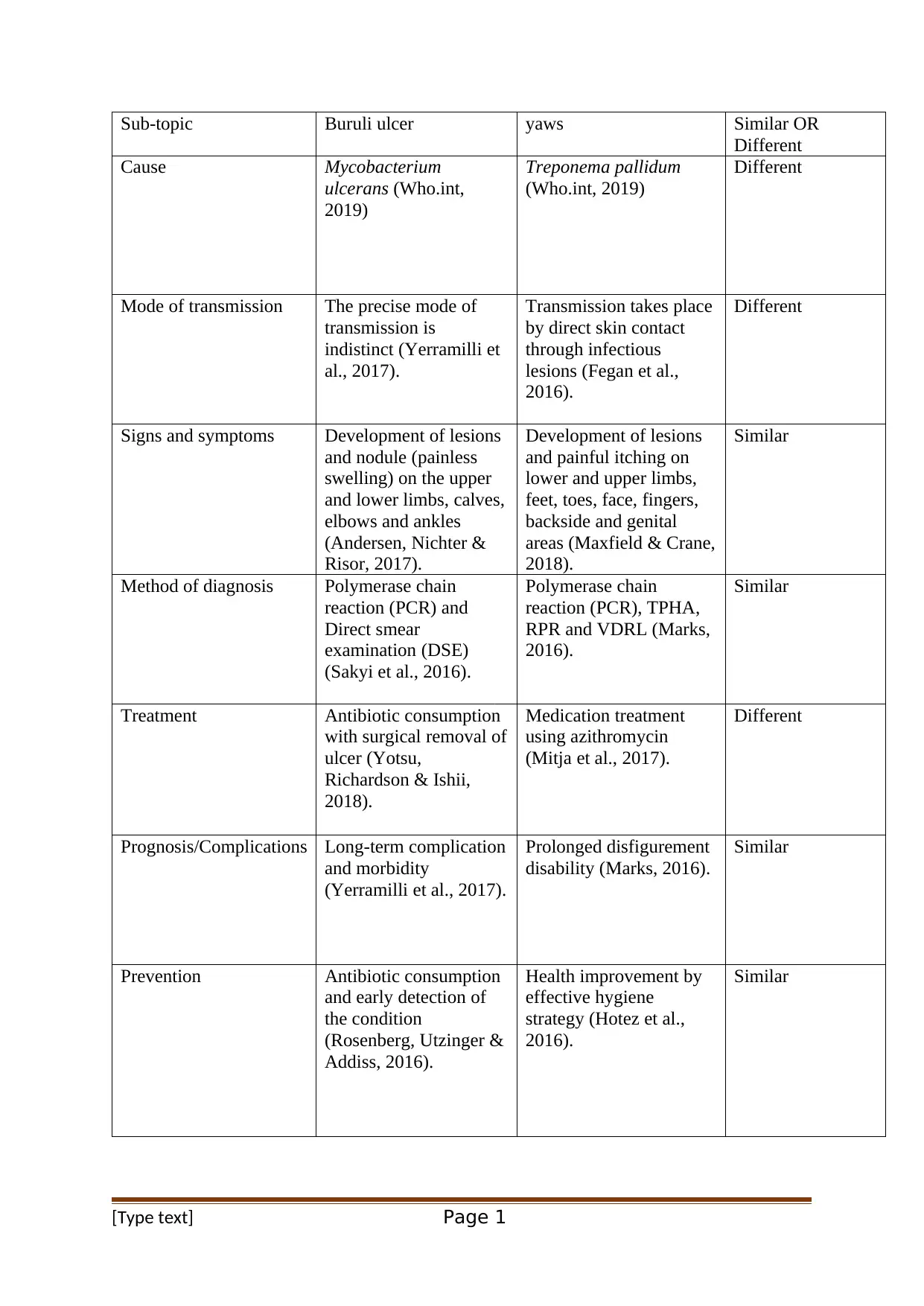
This essay provides a comparative analysis of Buruli ulcer and yaws, two distinct infectious diseases. It explores their respective causes, with Buruli ulcer caused by Mycobacterium ulcerans and yaws by Treponema pallidum. The modes of transmission differ, with Buruli ulcer's transmission being indistinct and yaws spreading through direct skin contact. The essay contrasts their signs and symptoms, diagnostic methods, and treatment approaches, noting that while both diseases involve lesion development, their specific manifestations and treatments vary. Furthermore, it addresses the prognosis and complications, highlighting long-term morbidity and disfigurement associated with each disease. Finally, the essay touches on prevention strategies, emphasizing antibiotic consumption and hygiene practices. This analysis, prepared for ACOM103: Academic English for Health Sciences 1, utilizes in-text references to support its claims and adheres to APA style guidelines. Desklib offers a wealth of similar solved assignments and past papers for students.
1 out of 3

![[object Object]](/_next/static/media/star-bottom.7253800d.svg)