The Impact of Dietary Calcium on Reducing Risks of Low Bone Mass
VerifiedAdded on 2021/06/17
|15
|3987
|71
Report
AI Summary
This report examines the role of calcium in reducing the risk of low bone mass. It discusses the importance of calcium for bone strength and flexibility, highlighting how bone resorption increases with age, leading to potential bone loss and related diseases. The report covers calcium's various functions, including its role in maintaining body structure, soft tissue functions, and homeostatic control mechanisms. It also addresses the bone turnover cycle, changes in bone mass across different life stages, and the impact of calcium deficiency. Epidemiological evidence and supplementation trials are reviewed, along with potential adverse effects of calcium intake. The report emphasizes the significance of dietary calcium in maintaining bone health and preventing conditions like osteopenia and osteoporosis, advocating for adequate calcium intake to support bone density and overall well-being. Desklib provides similar solved assignments for students.
Calcium as a means of reducing risk of
low bone mass
Student Name: Student ID:
Unit Name: Unit ID:
Date Due: Professor Name:
1 | P a g e
low bone mass
Student Name: Student ID:
Unit Name: Unit ID:
Date Due: Professor Name:
1 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Executive Summary
Bones form the basic building block for skeletal frameworks in humans. Calcium is the
basic mineral that builds up bones. Calcium provides bones with their strength as well
as flexibility. Calcium at an old age gets resorp more compared to production of
calcium. This often leads to loss of bone structure and various diseases of the bones to
happen. Role of calcium and its circulating mechanism has been discussed that
includes soft tissue roles and hemostatic functions. Its deficiency can adversely effect
on bones. Bone turnover cycle and changes in bone mass have been included for life
stages of puberty and childhood. Epidemiology for inclusion of supplementary trials with
generic issues has been highlighted. The scope of discussion here concerns ways
calcium can reduce low bone mass formation.
2 | P a g e
Bones form the basic building block for skeletal frameworks in humans. Calcium is the
basic mineral that builds up bones. Calcium provides bones with their strength as well
as flexibility. Calcium at an old age gets resorp more compared to production of
calcium. This often leads to loss of bone structure and various diseases of the bones to
happen. Role of calcium and its circulating mechanism has been discussed that
includes soft tissue roles and hemostatic functions. Its deficiency can adversely effect
on bones. Bone turnover cycle and changes in bone mass have been included for life
stages of puberty and childhood. Epidemiology for inclusion of supplementary trials with
generic issues has been highlighted. The scope of discussion here concerns ways
calcium can reduce low bone mass formation.
2 | P a g e
Table of Contents
Executive Summary...........................................................................................................2
1.0 Introduction..................................................................................................................4
2.0 Background of the Study: Roles of Calcium................................................................5
3.0 Nutrients affecting Pathological Process.....................................................................6
4.0 Epidemiological Evidence..........................................................................................10
5.0 Adverse Effects..........................................................................................................12
6.0 Conclusions and Recommendations.........................................................................13
7.0 Reference Lists..........................................................................................................14
Table of Figures
Figure 1: Stages of Remodelling.................................................................................................................7
Figure 2: Bone Coupling.............................................................................................................................8
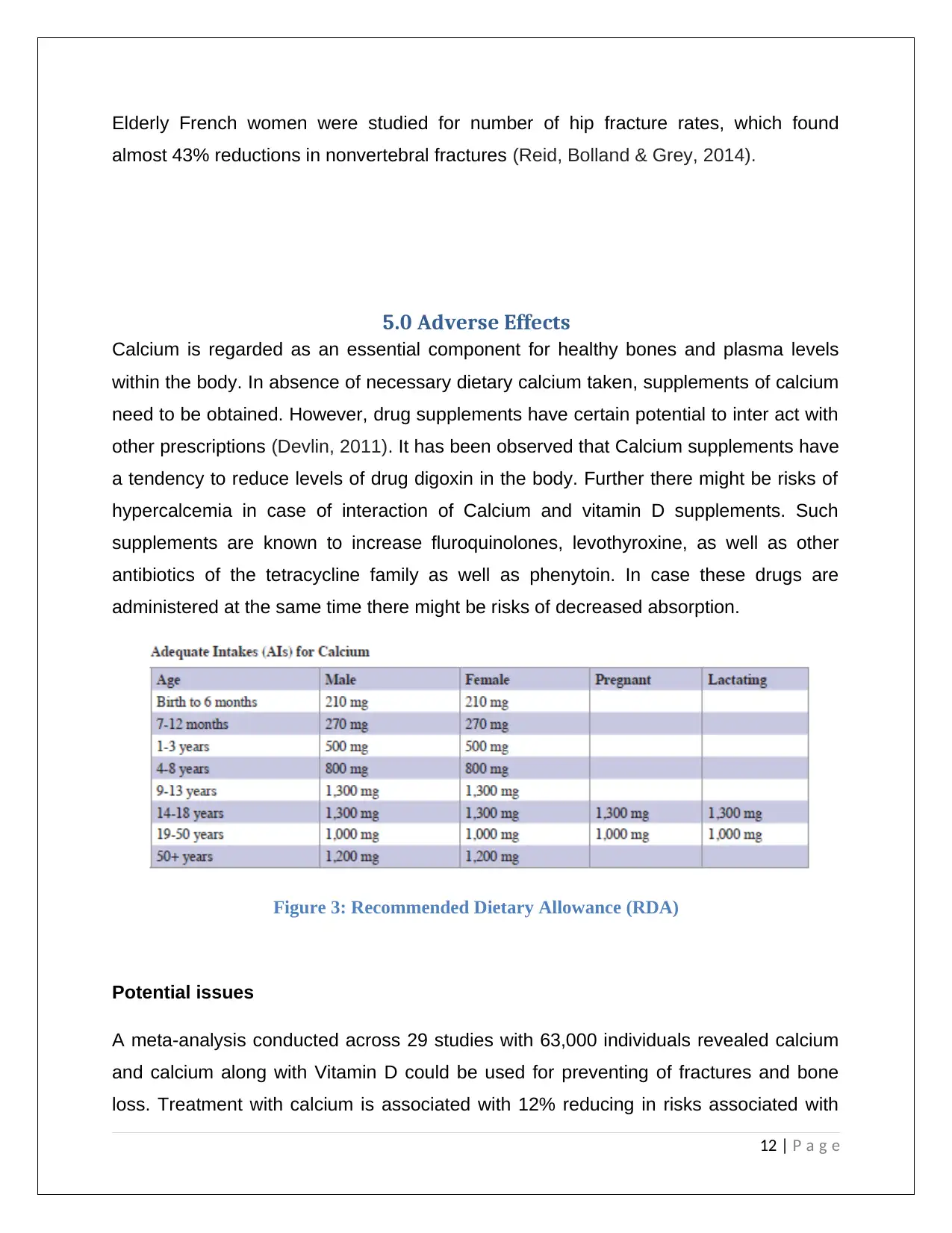
Figure 3: Recommended Dietary Allowance (RDA).................................................................................12
3 | P a g e
Executive Summary...........................................................................................................2
1.0 Introduction..................................................................................................................4
2.0 Background of the Study: Roles of Calcium................................................................5
3.0 Nutrients affecting Pathological Process.....................................................................6
4.0 Epidemiological Evidence..........................................................................................10
5.0 Adverse Effects..........................................................................................................12
6.0 Conclusions and Recommendations.........................................................................13
7.0 Reference Lists..........................................................................................................14
Table of Figures
Figure 1: Stages of Remodelling.................................................................................................................7
Figure 2: Bone Coupling.............................................................................................................................8
Figure 3: Recommended Dietary Allowance (RDA).................................................................................12
3 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1.0 Introduction
Bones comprises of living tissues with blood supply and active metabolism, though they
might appear to be lifeless structure (Ross et al,2011). Stronger bones are essential
part of good health hence can be formed from healthy diet as well as exercises. Bones
form an integral part of our skeletal structure and support bodies. Bones stores minerals
especially calcium. Calcium stored in bones of a human body is broken down during the
process of lifetime by mean of a process known as resorption and then builds newer
bones. As age progresses old bones are broken down faster compared to making of
newer bones, leading to net loss in bones. Bone loss can often lead to low bone density
commonly known as osteopenia (Ominsky et al, 2011). Further weakening of the bones
leads to osteoporosis. Osteoporosis can lead to further complications such as bone
fractures and minimal trauma. Osteoporosis is a disease whereby bones become weak
and have increased susceptibility to fractures and are more likely to break. Calcium has
been seen as a mineral whose continuous substitution might result in reducing risks of
suffering from low bone mass. External intake of calcium is known to have several other
benefits as well that might prevent loss of bone mineral density (Bender, 2016). The
scope of the discussion concerns dietary calcium as a way for reducing low bone
mass. The nutrients pathological process that can give rise to complex health problem
is undertaken along with epidemiological evidence and adverse effects of calcium is
analysed here.
Aims of the Report:
o To evaluate links between dietary calcium intake and low bone mass
o To understand the various roles performed by calcium as soft tissue roles and
homeostatic control mechanism
o To evaluate bone turnover cycle and concept of coupling
o To understand number of supplementation trials
4 | P a g e
Bones comprises of living tissues with blood supply and active metabolism, though they
might appear to be lifeless structure (Ross et al,2011). Stronger bones are essential
part of good health hence can be formed from healthy diet as well as exercises. Bones
form an integral part of our skeletal structure and support bodies. Bones stores minerals
especially calcium. Calcium stored in bones of a human body is broken down during the
process of lifetime by mean of a process known as resorption and then builds newer
bones. As age progresses old bones are broken down faster compared to making of
newer bones, leading to net loss in bones. Bone loss can often lead to low bone density
commonly known as osteopenia (Ominsky et al, 2011). Further weakening of the bones
leads to osteoporosis. Osteoporosis can lead to further complications such as bone
fractures and minimal trauma. Osteoporosis is a disease whereby bones become weak
and have increased susceptibility to fractures and are more likely to break. Calcium has
been seen as a mineral whose continuous substitution might result in reducing risks of
suffering from low bone mass. External intake of calcium is known to have several other
benefits as well that might prevent loss of bone mineral density (Bender, 2016). The
scope of the discussion concerns dietary calcium as a way for reducing low bone
mass. The nutrients pathological process that can give rise to complex health problem
is undertaken along with epidemiological evidence and adverse effects of calcium is
analysed here.
Aims of the Report:
o To evaluate links between dietary calcium intake and low bone mass
o To understand the various roles performed by calcium as soft tissue roles and
homeostatic control mechanism
o To evaluate bone turnover cycle and concept of coupling
o To understand number of supplementation trials
4 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2.0 Background of the Study: Roles of Calcium
Bone is composed of collagen, which is a complex protein that consists of a flexible
framework. Along with collagen, bones also comprises of calcium phosphate and
calcium carbonate that provides the hardened structure of the bones along with its
strength and flexibility. Loss of Calcium or lower presence of the mineral in the bone
and blood stream might pose serious health risks as well as complications. Low density
of calcium in bones might lead to lower bone mass. More the levels of calcium present
in bone more stronger and healthier will they be. Calcium is considered the most
sample mineral in the body with 99% of calcium being in blood and teeth, rest 1% is
present in muscles, blood and soft tissues such as organs, nerves and so on. This 1%
has a major role in our health helping in muscle contractions and relaxation, blood
clotting, nerve functioning, immune defense and blood pressure. Below are some of the
roles that are catered to by calcium;
Roles of Calcium:
I. Maintaining body structure: Calcium combines with phosphorus to form bones
by making them hard and resistant to decay. Consuming enough calcium helps
maintain strong bones later in life.
II. Soft Tissue Roles: Calcium comprises of 70% of bone weight and 99% calcium in
the body is the bones. Calcium provides muscles to contract normally as
deficiency can lead to create cramps and spasm. It allows blood to clot in cases of
wound or cut. Presence of calcium allows nerve message to be passed across the
nervous system across other parts of the body.
Remaining part of calcium floats around in the bloodstream in which it is
responsible for varied types of functions. Calcium has other pathological functions
as well as it is responsible for nervous system impulses, contraction of the heart
muscles and in clotting of blood.
5 | P a g e
Bone is composed of collagen, which is a complex protein that consists of a flexible
framework. Along with collagen, bones also comprises of calcium phosphate and
calcium carbonate that provides the hardened structure of the bones along with its
strength and flexibility. Loss of Calcium or lower presence of the mineral in the bone
and blood stream might pose serious health risks as well as complications. Low density
of calcium in bones might lead to lower bone mass. More the levels of calcium present
in bone more stronger and healthier will they be. Calcium is considered the most
sample mineral in the body with 99% of calcium being in blood and teeth, rest 1% is
present in muscles, blood and soft tissues such as organs, nerves and so on. This 1%
has a major role in our health helping in muscle contractions and relaxation, blood
clotting, nerve functioning, immune defense and blood pressure. Below are some of the
roles that are catered to by calcium;
Roles of Calcium:
I. Maintaining body structure: Calcium combines with phosphorus to form bones
by making them hard and resistant to decay. Consuming enough calcium helps
maintain strong bones later in life.
II. Soft Tissue Roles: Calcium comprises of 70% of bone weight and 99% calcium in
the body is the bones. Calcium provides muscles to contract normally as
deficiency can lead to create cramps and spasm. It allows blood to clot in cases of
wound or cut. Presence of calcium allows nerve message to be passed across the
nervous system across other parts of the body.
Remaining part of calcium floats around in the bloodstream in which it is
responsible for varied types of functions. Calcium has other pathological functions
as well as it is responsible for nervous system impulses, contraction of the heart
muscles and in clotting of blood.
5 | P a g e

III. Homeostatic Control Mechanism: Calcium helps regulate blood pressure, as low
calcium intake has been seen to be associated high blood pressure. Role of
calcium has been found to be major in homeostatic control mechanism. Calcium
reduces risks of colon cancer and many other forms of cancers. It allows fat
binding and bile acid in large intestines. It prevents excessive growth of cells in
intestines. During childbirth, calcium plays an important role of simulating
contraction of the uterus and also supports formation of milk. Its other pathological
implications include functioning of various enzymes and hormones within the body.
Adverse effects on bone: Absence of calcium can have adverse effects on bone,
leading to weakening and causing breakage. Deficiency of calcium might lead to
severe consequences on the body.
3.0 Nutrients affecting Pathological Process
Calcium is an essential nutrient that that forms basic building blocks for bones. Calcium
not only provides strength to bones but also renders them with flexibility that allows
bones to sustain injuries (Cao, 2011). Bones can absorb various strength blows and
other injuries and prevents such harm from reaching internal organs that are much
weaker to sustain such injuries. Calcium being a critical nutrient that supports health
bone structure need to be constantly supplied to the body. Pathological significance of
calcium is significant as it is known to affects various controls and support healthy bone
structure. Loss of calcium is greater compared to its absorption procedure, after the age
of 30 calcium deficiency can easily occur. Calcium deficiency is said to be a condition
when presence of calcium is insufficient or it is not being utilized in a proper manner. An
average diet can lead to calcium deficiency (Kendler et al, 2010).
6 | P a g e
calcium intake has been seen to be associated high blood pressure. Role of
calcium has been found to be major in homeostatic control mechanism. Calcium
reduces risks of colon cancer and many other forms of cancers. It allows fat
binding and bile acid in large intestines. It prevents excessive growth of cells in
intestines. During childbirth, calcium plays an important role of simulating
contraction of the uterus and also supports formation of milk. Its other pathological
implications include functioning of various enzymes and hormones within the body.
Adverse effects on bone: Absence of calcium can have adverse effects on bone,
leading to weakening and causing breakage. Deficiency of calcium might lead to
severe consequences on the body.
3.0 Nutrients affecting Pathological Process
Calcium is an essential nutrient that that forms basic building blocks for bones. Calcium
not only provides strength to bones but also renders them with flexibility that allows
bones to sustain injuries (Cao, 2011). Bones can absorb various strength blows and
other injuries and prevents such harm from reaching internal organs that are much
weaker to sustain such injuries. Calcium being a critical nutrient that supports health
bone structure need to be constantly supplied to the body. Pathological significance of
calcium is significant as it is known to affects various controls and support healthy bone
structure. Loss of calcium is greater compared to its absorption procedure, after the age
of 30 calcium deficiency can easily occur. Calcium deficiency is said to be a condition
when presence of calcium is insufficient or it is not being utilized in a proper manner. An
average diet can lead to calcium deficiency (Kendler et al, 2010).
6 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
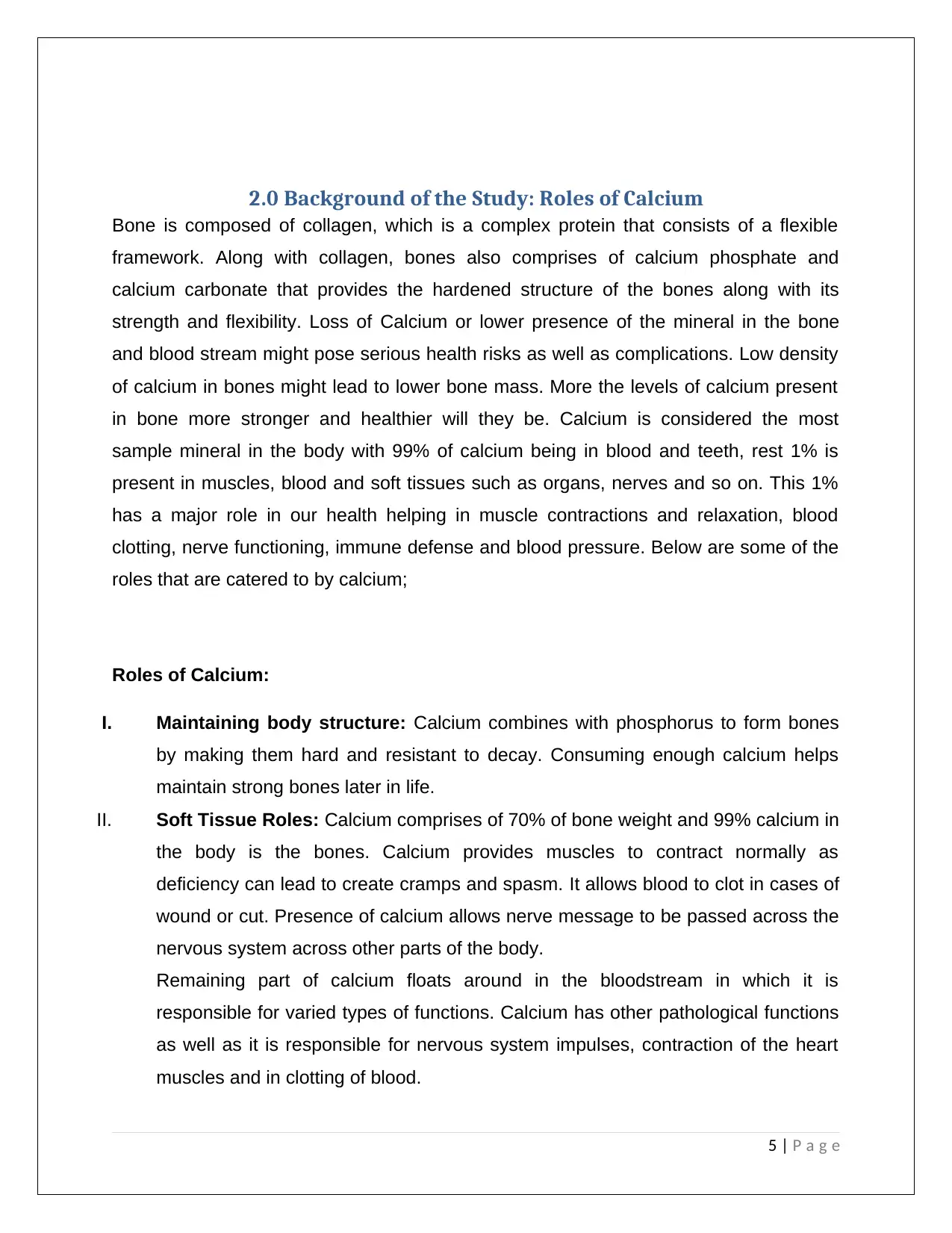
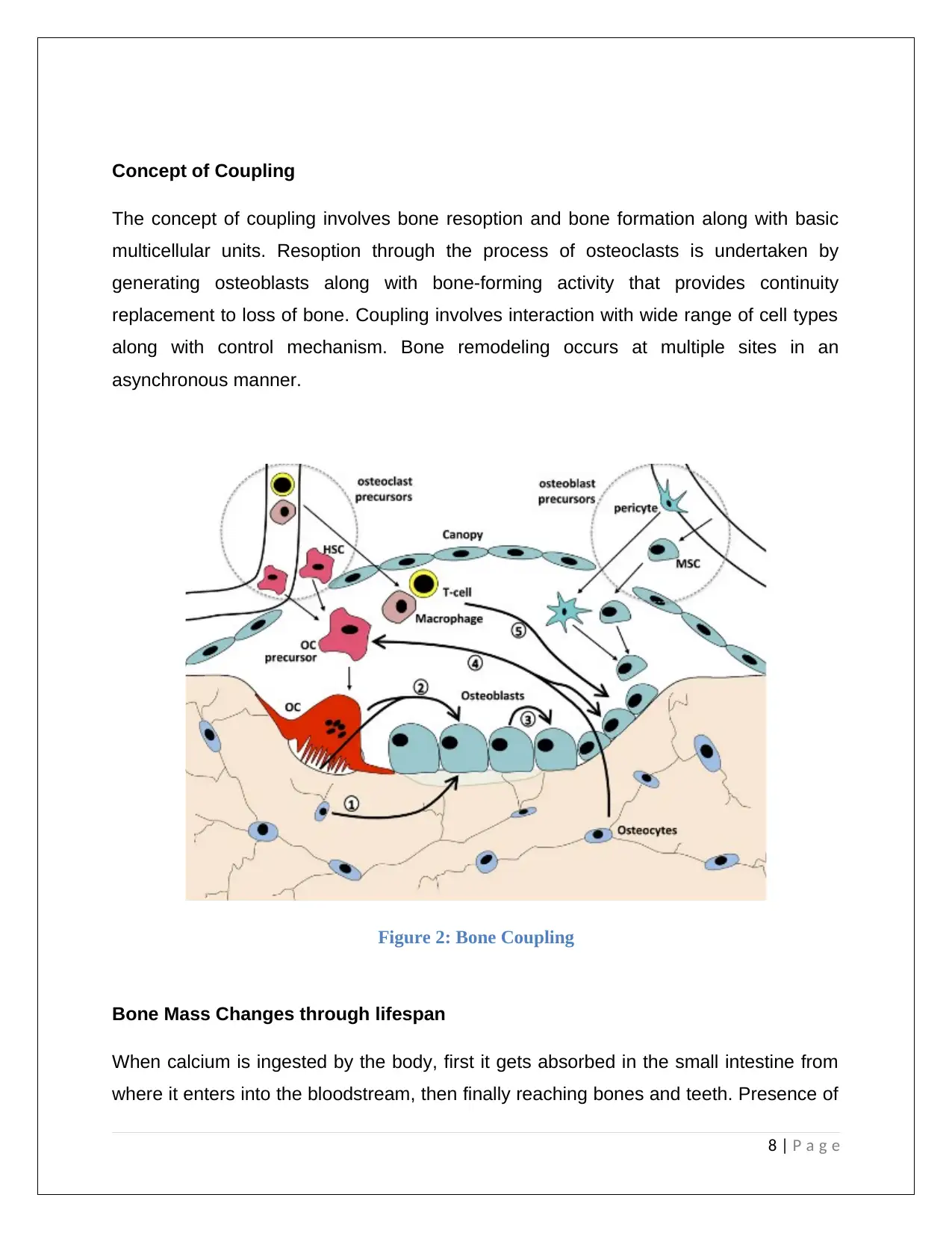
Bone Turnover Cycle
Bone turnover cycle is considered as a continuous process and occurs at an average
rate of 3.6% per year amongst healthy adults. Bone turnover cycle has double rate in
children. Bone turnover provides formation and resorption process released during the
time of remodeling. They are considered markers that have allowed understanding
physiology, clinical applications and maximizing optimizing analysis process. It
complements bone mineral density by managing osteoporosis.
Figure 1: Stages of Remodelling
Bone comprise of dynamic tissue of cells and extracellular matrix encompassing organic
(35%) and inorganic (65%) molecules. Organic matrix within bone comprises of type I
collagen (90%) along with non-collagenous proteins as osteocalcin (OC), proteoglycans
and glycoproteins. Inorganic calcium and phosphate lead to formation of hydroxyapatite
crystals which mineralize in the organic matrix. There are three types of bone cells that
are engaged I n remodeling as osteoblast, osteocytes and osteoclasts.
7 | P a g e
Bone turnover cycle is considered as a continuous process and occurs at an average
rate of 3.6% per year amongst healthy adults. Bone turnover cycle has double rate in
children. Bone turnover provides formation and resorption process released during the
time of remodeling. They are considered markers that have allowed understanding
physiology, clinical applications and maximizing optimizing analysis process. It
complements bone mineral density by managing osteoporosis.
Figure 1: Stages of Remodelling
Bone comprise of dynamic tissue of cells and extracellular matrix encompassing organic
(35%) and inorganic (65%) molecules. Organic matrix within bone comprises of type I
collagen (90%) along with non-collagenous proteins as osteocalcin (OC), proteoglycans
and glycoproteins. Inorganic calcium and phosphate lead to formation of hydroxyapatite
crystals which mineralize in the organic matrix. There are three types of bone cells that
are engaged I n remodeling as osteoblast, osteocytes and osteoclasts.
7 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
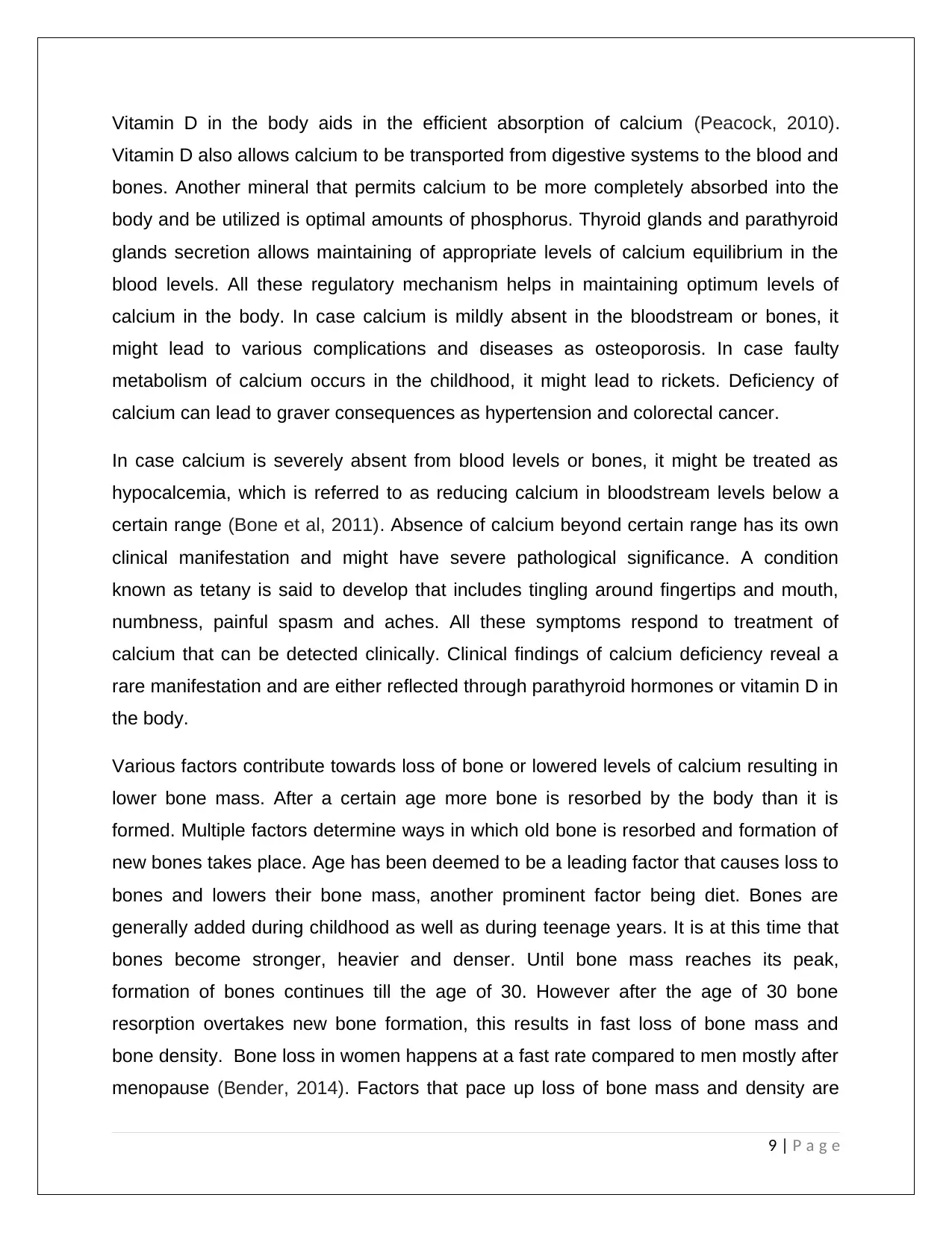
Concept of Coupling
The concept of coupling involves bone resoption and bone formation along with basic
multicellular units. Resoption through the process of osteoclasts is undertaken by
generating osteoblasts along with bone-forming activity that provides continuity
replacement to loss of bone. Coupling involves interaction with wide range of cell types
along with control mechanism. Bone remodeling occurs at multiple sites in an
asynchronous manner.
Figure 2: Bone Coupling
Bone Mass Changes through lifespan
When calcium is ingested by the body, first it gets absorbed in the small intestine from
where it enters into the bloodstream, then finally reaching bones and teeth. Presence of
8 | P a g e
The concept of coupling involves bone resoption and bone formation along with basic
multicellular units. Resoption through the process of osteoclasts is undertaken by
generating osteoblasts along with bone-forming activity that provides continuity
replacement to loss of bone. Coupling involves interaction with wide range of cell types
along with control mechanism. Bone remodeling occurs at multiple sites in an
asynchronous manner.
Figure 2: Bone Coupling
Bone Mass Changes through lifespan
When calcium is ingested by the body, first it gets absorbed in the small intestine from
where it enters into the bloodstream, then finally reaching bones and teeth. Presence of
8 | P a g e
Vitamin D in the body aids in the efficient absorption of calcium (Peacock, 2010).
Vitamin D also allows calcium to be transported from digestive systems to the blood and
bones. Another mineral that permits calcium to be more completely absorbed into the
body and be utilized is optimal amounts of phosphorus. Thyroid glands and parathyroid
glands secretion allows maintaining of appropriate levels of calcium equilibrium in the
blood levels. All these regulatory mechanism helps in maintaining optimum levels of
calcium in the body. In case calcium is mildly absent in the bloodstream or bones, it
might lead to various complications and diseases as osteoporosis. In case faulty
metabolism of calcium occurs in the childhood, it might lead to rickets. Deficiency of
calcium can lead to graver consequences as hypertension and colorectal cancer.
In case calcium is severely absent from blood levels or bones, it might be treated as
hypocalcemia, which is referred to as reducing calcium in bloodstream levels below a
certain range (Bone et al, 2011). Absence of calcium beyond certain range has its own
clinical manifestation and might have severe pathological significance. A condition
known as tetany is said to develop that includes tingling around fingertips and mouth,
numbness, painful spasm and aches. All these symptoms respond to treatment of
calcium that can be detected clinically. Clinical findings of calcium deficiency reveal a
rare manifestation and are either reflected through parathyroid hormones or vitamin D in
the body.
Various factors contribute towards loss of bone or lowered levels of calcium resulting in
lower bone mass. After a certain age more bone is resorbed by the body than it is
formed. Multiple factors determine ways in which old bone is resorbed and formation of
new bones takes place. Age has been deemed to be a leading factor that causes loss to
bones and lowers their bone mass, another prominent factor being diet. Bones are
generally added during childhood as well as during teenage years. It is at this time that
bones become stronger, heavier and denser. Until bone mass reaches its peak,
formation of bones continues till the age of 30. However after the age of 30 bone
resorption overtakes new bone formation, this results in fast loss of bone mass and
bone density. Bone loss in women happens at a fast rate compared to men mostly after
menopause (Bender, 2014). Factors that pace up loss of bone mass and density are
9 | P a g e
Vitamin D also allows calcium to be transported from digestive systems to the blood and
bones. Another mineral that permits calcium to be more completely absorbed into the
body and be utilized is optimal amounts of phosphorus. Thyroid glands and parathyroid
glands secretion allows maintaining of appropriate levels of calcium equilibrium in the
blood levels. All these regulatory mechanism helps in maintaining optimum levels of
calcium in the body. In case calcium is mildly absent in the bloodstream or bones, it
might lead to various complications and diseases as osteoporosis. In case faulty
metabolism of calcium occurs in the childhood, it might lead to rickets. Deficiency of
calcium can lead to graver consequences as hypertension and colorectal cancer.
In case calcium is severely absent from blood levels or bones, it might be treated as
hypocalcemia, which is referred to as reducing calcium in bloodstream levels below a
certain range (Bone et al, 2011). Absence of calcium beyond certain range has its own
clinical manifestation and might have severe pathological significance. A condition
known as tetany is said to develop that includes tingling around fingertips and mouth,
numbness, painful spasm and aches. All these symptoms respond to treatment of
calcium that can be detected clinically. Clinical findings of calcium deficiency reveal a
rare manifestation and are either reflected through parathyroid hormones or vitamin D in
the body.
Various factors contribute towards loss of bone or lowered levels of calcium resulting in
lower bone mass. After a certain age more bone is resorbed by the body than it is
formed. Multiple factors determine ways in which old bone is resorbed and formation of
new bones takes place. Age has been deemed to be a leading factor that causes loss to
bones and lowers their bone mass, another prominent factor being diet. Bones are
generally added during childhood as well as during teenage years. It is at this time that
bones become stronger, heavier and denser. Until bone mass reaches its peak,
formation of bones continues till the age of 30. However after the age of 30 bone
resorption overtakes new bone formation, this results in fast loss of bone mass and
bone density. Bone loss in women happens at a fast rate compared to men mostly after
menopause (Bender, 2014). Factors that pace up loss of bone mass and density are
9 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
having diet that have low quantities of calcium in them, smoking, not exercising and
taking medication as corticosteroids (Langdahl et al, 2012). Men are also at higher risks
from osteoporosis but experiences loss of bone later in their lives as well. Early
detection of bone loss is critical and important for arriving at the steps to prevent
osteoporosis from taking place. Effective prevention and treatment can only take place
in case the individual is aware regarding risks facing them of osteoporosis. Ways in
which bone solidness can be tested is by bone mineral density (BMD) that has
capability to measure solidness and mass of bones.
4.0 Epidemiological Evidence
Calcium along with Vitamin D is considered to be critical nutrients for bone health and
their maintenance. In cases of patients facing bone loss, calcium and Vitamin D care is
provided for the purpose of optimal care (Chen et al, 2012). However, research shows
that women being at greater health risks from loss of calcium and approximately 90%
women might not be getting enough calcium with 50% women receiving treatment for
bone loss might have inadequate amounts of Vitamin D. Osteoporosis is the most
eminent clinical complication arising from mal-absorption of calcium in the bloodstream.
Though osteoporosis have a number of pharmacological treatments that can enhance
bone mass by reduction in risks from fractures. The treatment has been seen to be
successful by providing sufficient amounts of Vitamin D and Calcium supplements. The
US Surgeon General has provided a pyramid approach for the purpose of treating bone
related diseases. According to the approach, preventing falling down, with maintaining
adequate quantities of vitamin D, physical activity and calcium provide the base of the
pyramid for individual facing bone diseases. At the second tier of the pyramid includes
methods aimed at treating secondary causes that leads to osteoporosis. The third tyre
includes pharmacotherapy.
10 | P a g e
taking medication as corticosteroids (Langdahl et al, 2012). Men are also at higher risks
from osteoporosis but experiences loss of bone later in their lives as well. Early
detection of bone loss is critical and important for arriving at the steps to prevent
osteoporosis from taking place. Effective prevention and treatment can only take place
in case the individual is aware regarding risks facing them of osteoporosis. Ways in
which bone solidness can be tested is by bone mineral density (BMD) that has
capability to measure solidness and mass of bones.
4.0 Epidemiological Evidence
Calcium along with Vitamin D is considered to be critical nutrients for bone health and
their maintenance. In cases of patients facing bone loss, calcium and Vitamin D care is
provided for the purpose of optimal care (Chen et al, 2012). However, research shows
that women being at greater health risks from loss of calcium and approximately 90%
women might not be getting enough calcium with 50% women receiving treatment for
bone loss might have inadequate amounts of Vitamin D. Osteoporosis is the most
eminent clinical complication arising from mal-absorption of calcium in the bloodstream.
Though osteoporosis have a number of pharmacological treatments that can enhance
bone mass by reduction in risks from fractures. The treatment has been seen to be
successful by providing sufficient amounts of Vitamin D and Calcium supplements. The
US Surgeon General has provided a pyramid approach for the purpose of treating bone
related diseases. According to the approach, preventing falling down, with maintaining
adequate quantities of vitamin D, physical activity and calcium provide the base of the
pyramid for individual facing bone diseases. At the second tier of the pyramid includes
methods aimed at treating secondary causes that leads to osteoporosis. The third tyre
includes pharmacotherapy.
10 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Review of Supplementary trial
Calcium levels being low in the blood stream or bone might impose various challenges
in the human body (Drake et al, 2012). Clinical and pathological implications might be
epidemiologically verified. Osteoporosis has become a significant public health issue
that has effects on morbidity and mortality. Till recently calcium and vitamin D had been
overlooked by health practioner and patients as an integral factor. Calcium leads to
creation of bone mass, leading to healthier bone structure and system. Calcium levels is
said to achieve its peak by the 30s. In young stage and as adults physical activity along
with adequate supplements of calcium and vitamin D intake is suggested for
maintaining proper cellular functions and body structure. Calcium as earlier established
is an essential component for bone mineral as well as extracellular fluid (ECF) or
plasma. A calcium balance dictates bone resoption and increasing levels of plasma.
Calcium is primarily excreted through kidneys and feces. Calcium intake is best
suggested by daily dietary intake of high calcium containing foods. Dairy sources
provide adequate calcium sources. Other sources of calcium include mineral waters
with calcium enrichment and other naturally occurring bio-calcium sources. Individuals
who do not acquire necessary amounts of calcium through their dietary intake need to
take additional amounts of calcium for meeting dietary guidelines. Research and studies
provides that an average American does not even meet the lower ends of calcium
intake suggested. Whereas women at the age of 40 intakes almost half of the calcium
that is suggested for dietary intake. Especially in postmenopausal women, calcium
intakes were found to be significantly low as compared to other women.
Readily available calcium supplements in the market can add to necessary calcium
required by an ordinary human body. The most commonly available natural calcium
supplements are calcium citrate and calcium carbonate (Rizzoli et al, 2010). These
supplements are used almost all over the world and have particularly high levels of
absorption rates when taken with food. Calcium supplements have effectively shown to
prevent osteoporosis fractures in postmenopausal women. Calcium artificial intake can
reduce risks considerably between 25% to 70% for osteoporosis. Trails of studies
shows up to 30% reduction in risks of fractures by taking in 1000 mg/day of calcium.
11 | P a g e
Calcium levels being low in the blood stream or bone might impose various challenges
in the human body (Drake et al, 2012). Clinical and pathological implications might be
epidemiologically verified. Osteoporosis has become a significant public health issue
that has effects on morbidity and mortality. Till recently calcium and vitamin D had been
overlooked by health practioner and patients as an integral factor. Calcium leads to
creation of bone mass, leading to healthier bone structure and system. Calcium levels is
said to achieve its peak by the 30s. In young stage and as adults physical activity along
with adequate supplements of calcium and vitamin D intake is suggested for
maintaining proper cellular functions and body structure. Calcium as earlier established
is an essential component for bone mineral as well as extracellular fluid (ECF) or
plasma. A calcium balance dictates bone resoption and increasing levels of plasma.
Calcium is primarily excreted through kidneys and feces. Calcium intake is best
suggested by daily dietary intake of high calcium containing foods. Dairy sources
provide adequate calcium sources. Other sources of calcium include mineral waters
with calcium enrichment and other naturally occurring bio-calcium sources. Individuals
who do not acquire necessary amounts of calcium through their dietary intake need to
take additional amounts of calcium for meeting dietary guidelines. Research and studies
provides that an average American does not even meet the lower ends of calcium
intake suggested. Whereas women at the age of 40 intakes almost half of the calcium
that is suggested for dietary intake. Especially in postmenopausal women, calcium
intakes were found to be significantly low as compared to other women.
Readily available calcium supplements in the market can add to necessary calcium
required by an ordinary human body. The most commonly available natural calcium
supplements are calcium citrate and calcium carbonate (Rizzoli et al, 2010). These
supplements are used almost all over the world and have particularly high levels of
absorption rates when taken with food. Calcium supplements have effectively shown to
prevent osteoporosis fractures in postmenopausal women. Calcium artificial intake can
reduce risks considerably between 25% to 70% for osteoporosis. Trails of studies
shows up to 30% reduction in risks of fractures by taking in 1000 mg/day of calcium.
11 | P a g e
Elderly French women were studied for number of hip fracture rates, which found
almost 43% reductions in nonvertebral fractures (Reid, Bolland & Grey, 2014).
5.0 Adverse Effects
Calcium is regarded as an essential component for healthy bones and plasma levels
within the body. In absence of necessary dietary calcium taken, supplements of calcium
need to be obtained. However, drug supplements have certain potential to inter act with
other prescriptions (Devlin, 2011). It has been observed that Calcium supplements have
a tendency to reduce levels of drug digoxin in the body. Further there might be risks of
hypercalcemia in case of interaction of Calcium and vitamin D supplements. Such
supplements are known to increase fluroquinolones, levothyroxine, as well as other
antibiotics of the tetracycline family as well as phenytoin. In case these drugs are
administered at the same time there might be risks of decreased absorption.
Figure 3: Recommended Dietary Allowance (RDA)
Potential issues
A meta-analysis conducted across 29 studies with 63,000 individuals revealed calcium
and calcium along with Vitamin D could be used for preventing of fractures and bone
loss. Treatment with calcium is associated with 12% reducing in risks associated with
12 | P a g e
almost 43% reductions in nonvertebral fractures (Reid, Bolland & Grey, 2014).
5.0 Adverse Effects
Calcium is regarded as an essential component for healthy bones and plasma levels
within the body. In absence of necessary dietary calcium taken, supplements of calcium
need to be obtained. However, drug supplements have certain potential to inter act with
other prescriptions (Devlin, 2011). It has been observed that Calcium supplements have
a tendency to reduce levels of drug digoxin in the body. Further there might be risks of
hypercalcemia in case of interaction of Calcium and vitamin D supplements. Such
supplements are known to increase fluroquinolones, levothyroxine, as well as other
antibiotics of the tetracycline family as well as phenytoin. In case these drugs are
administered at the same time there might be risks of decreased absorption.
Figure 3: Recommended Dietary Allowance (RDA)
Potential issues
A meta-analysis conducted across 29 studies with 63,000 individuals revealed calcium
and calcium along with Vitamin D could be used for preventing of fractures and bone
loss. Treatment with calcium is associated with 12% reducing in risks associated with
12 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





