Case Study: ECG, Cardiac Conditions, and Treatment
VerifiedAdded on 2022/09/18
|9
|3407
|24
Case Study
AI Summary
This case study presents a detailed analysis of a patient's condition presenting with chest pain at the emergency department. The assessment begins with an electrocardiogram (ECG) revealing ST elevation, indicative of potential heart distress. The case explores the diagnosis of coronary atherosclerosis and myocardial ischemia, detailing their etiologies and pathogenesis. The patient receives a combination of medications, including aspirin, glycerine trinitrate (GTN), and morphine, each with specific physiological effects aimed at reducing chest pain and preventing further cardiac complications. The case further examines the protocols followed in the emergency department for assessing chest pain, including ECG examination, patient history, and the use of diagnostic tools. The discussion emphasizes the importance of rapid and accurate assessment, adhering to established guidelines, and the challenges faced by healthcare providers in making critical decisions regarding patient management, including the decision to admit or discharge patients. The case highlights the role of various factors, such as patient history, ECG results, risk factors, and the use of validated assessment tools, in the overall management of patients presenting with chest pain in the emergency department.
QUESTION 1
The electrocardiogram – ECG is a critical test undertaken in the medical assessment
protocols. The ECG has ST elevation which depicts serious heart distress signal and this
necessitates heart treatment immediately. ECG is recommended when the patient has a
depiction of chest pain and signs of shortness of breathing as depicted by the patient in the
case study (Karimian, Guo, Tehranipoor & Forte, 2016).
ECG offers an electronic reading assessment and reflects impulses which activate the
heart muscles and the overall blood pumping ability. The electrodes fixed at various sites of
the body sends signals to be assessed. The ECG offers an avenue of pattern recognition
which is essential in diagnosing the state of the patient (Breen, Kelly & Kernohan, 2019).
During a normal heartbeat, the activity often depicts small pacemaker patch cells
indicating electrical activity. The various electrodes affixed to the body on the chests and
arms produces the electrical impulses which are crucial for assessing the pumping mechanism
of the heart. During the normal heartbeat, the electrical activity indicates small patches
referred to as the sinus node. Activation of the atria by the impulse produces small blip
referred to as the P wave. Thereafter the pumping chamber, ventricles produces up and down
in the middle referred to as the QRS complex. The T wave at the end refers to the recovery
period during the reverse impulse movement (Sullivian et al., 2018).
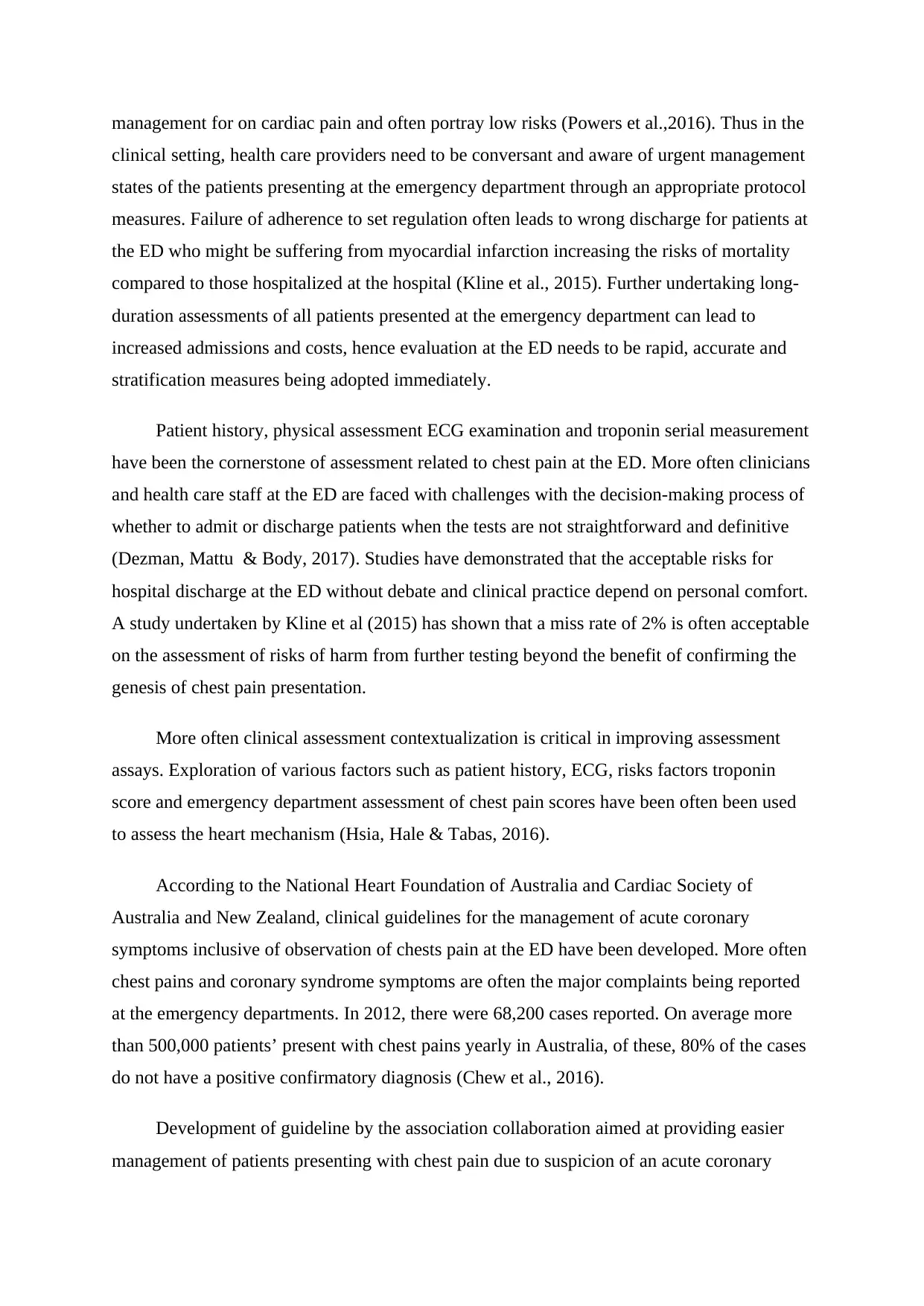
As the patient symptoms signify intense chest pains, referred to as angina, the heart
muscles work in a strenuous state getting inadequate blood and oxygen, the ST portion dips
downwards instead of showing flat level. This is indicated in Lead I, II and III, as observed in
the arrow indicated in the diagrammatic representation below.
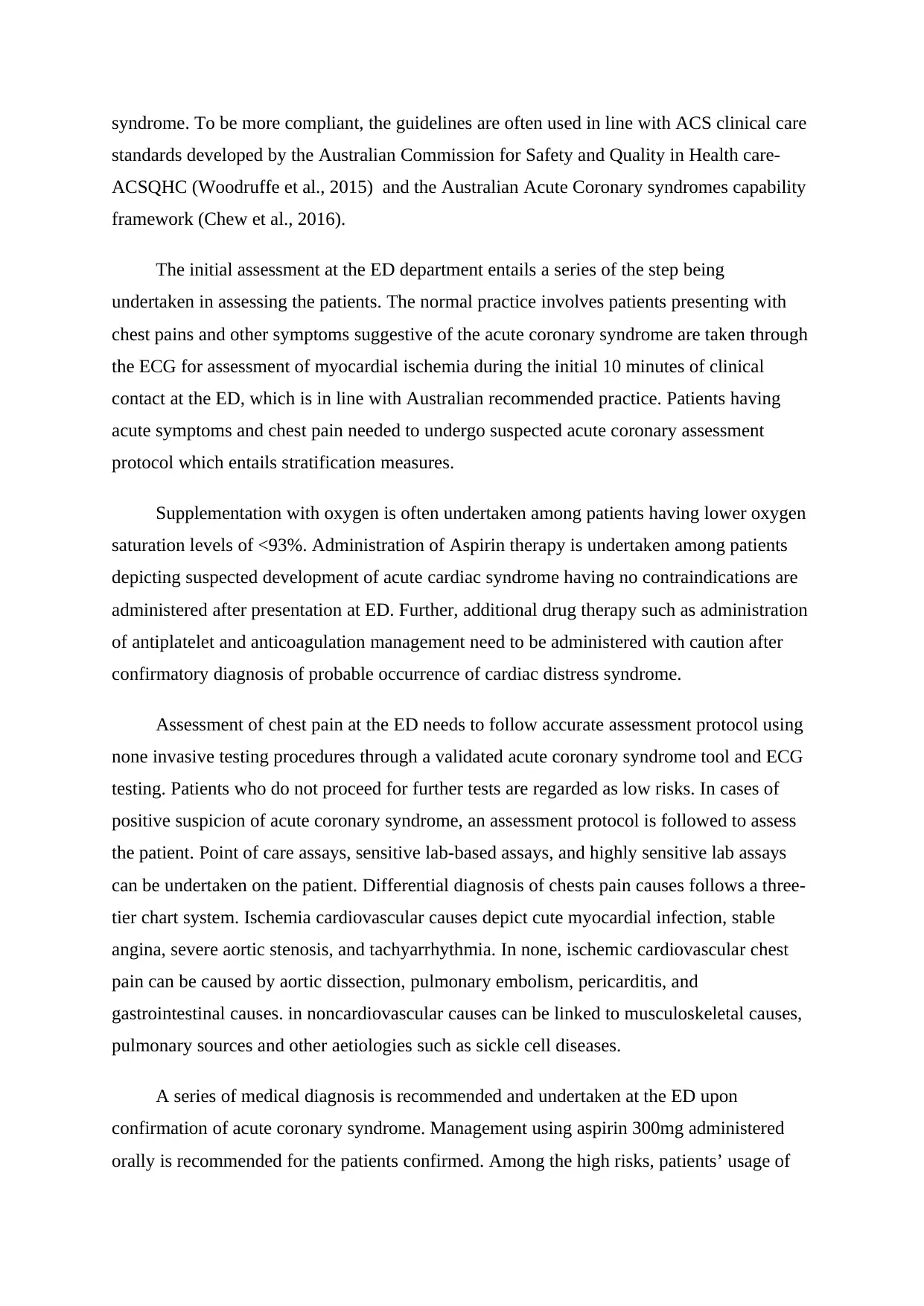
Further, from the ECG assessment of serious heart attack can be diagnosed. The ST
segments of the ECG in normal patient assessment often are flat. The occurrence of humped
and raised appearances indicates a serious heart attack (Doubell, 2017). This is depicted in
the diagram below obtained from the image of the patient.
The electrocardiogram – ECG is a critical test undertaken in the medical assessment
protocols. The ECG has ST elevation which depicts serious heart distress signal and this
necessitates heart treatment immediately. ECG is recommended when the patient has a
depiction of chest pain and signs of shortness of breathing as depicted by the patient in the
case study (Karimian, Guo, Tehranipoor & Forte, 2016).
ECG offers an electronic reading assessment and reflects impulses which activate the
heart muscles and the overall blood pumping ability. The electrodes fixed at various sites of
the body sends signals to be assessed. The ECG offers an avenue of pattern recognition
which is essential in diagnosing the state of the patient (Breen, Kelly & Kernohan, 2019).
During a normal heartbeat, the activity often depicts small pacemaker patch cells
indicating electrical activity. The various electrodes affixed to the body on the chests and
arms produces the electrical impulses which are crucial for assessing the pumping mechanism
of the heart. During the normal heartbeat, the electrical activity indicates small patches
referred to as the sinus node. Activation of the atria by the impulse produces small blip
referred to as the P wave. Thereafter the pumping chamber, ventricles produces up and down
in the middle referred to as the QRS complex. The T wave at the end refers to the recovery
period during the reverse impulse movement (Sullivian et al., 2018).
As the patient symptoms signify intense chest pains, referred to as angina, the heart
muscles work in a strenuous state getting inadequate blood and oxygen, the ST portion dips
downwards instead of showing flat level. This is indicated in Lead I, II and III, as observed in
the arrow indicated in the diagrammatic representation below.
Further, from the ECG assessment of serious heart attack can be diagnosed. The ST
segments of the ECG in normal patient assessment often are flat. The occurrence of humped
and raised appearances indicates a serious heart attack (Doubell, 2017). This is depicted in
the diagram below obtained from the image of the patient.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
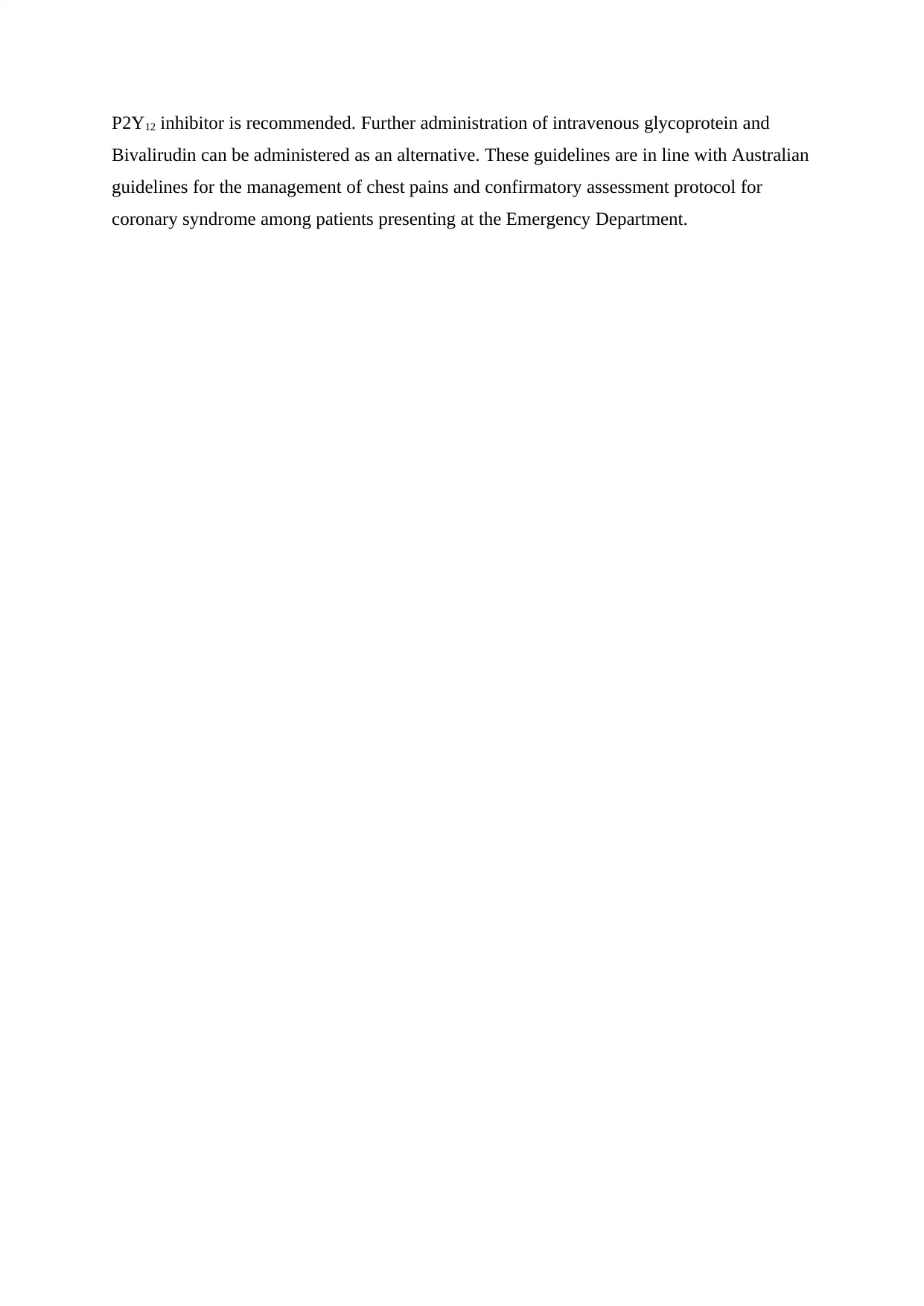
Further, signs of atrial fibrillation on the upper chambers of the heart are indicative on
the ECG. There is an occurrence of chaotic observation and irregular pumping occurring
(Magnusson, et al., 2019). The P wave does not reflect and occurrence of the jumpy baseline
is observed. the occurrence of the QRS complex is observed on lead II lower line on the ECG
diagram as observed on the image below;
Coronary atherosclerosis
Etiology
Coronary atherosclerosis is a pathological process which hampers the large and
medium arteries leading to coronary artery disease. Atherosclerosis reflects chronic
cumulative plaque formed on the vessels walls leading to necrotic cores, modified lipids and
inflamed smooth muscles. Coronary heart disease relates to the reduction of blood movement
to the muscles as a result of build-up plaque on the heart arteries. It is often the most common
form of cardiovascular diseases. Various types of this state entail stable angina, unstable
angina, myocardial infarction, and even cardiac arrest (Ambrose & Singh, 2015).
The development of coronary heart diseases often occurs after a longer period, which
progresses on to the development of chest pain. Diagnosis is often made from ECG
assessment.
Pathogenesis
Atherosclerosis occurrence begins with medium and large arteries which are affected
by patchy thickening of the sub- intima arterial wall encroachment. Lesion appearance is
observed by fatty streak due to lipid accumulation from cells in the artery intimal layer. Over
time the fatty streak develops into plaque leading to atherosclerosis. This leads to blockage of
blood flow. Typically the occurrence emanates from the development of atherosclerosis
the ECG. There is an occurrence of chaotic observation and irregular pumping occurring
(Magnusson, et al., 2019). The P wave does not reflect and occurrence of the jumpy baseline
is observed. the occurrence of the QRS complex is observed on lead II lower line on the ECG
diagram as observed on the image below;
Coronary atherosclerosis
Etiology
Coronary atherosclerosis is a pathological process which hampers the large and
medium arteries leading to coronary artery disease. Atherosclerosis reflects chronic
cumulative plaque formed on the vessels walls leading to necrotic cores, modified lipids and
inflamed smooth muscles. Coronary heart disease relates to the reduction of blood movement
to the muscles as a result of build-up plaque on the heart arteries. It is often the most common
form of cardiovascular diseases. Various types of this state entail stable angina, unstable
angina, myocardial infarction, and even cardiac arrest (Ambrose & Singh, 2015).
The development of coronary heart diseases often occurs after a longer period, which
progresses on to the development of chest pain. Diagnosis is often made from ECG
assessment.
Pathogenesis
Atherosclerosis occurrence begins with medium and large arteries which are affected
by patchy thickening of the sub- intima arterial wall encroachment. Lesion appearance is
observed by fatty streak due to lipid accumulation from cells in the artery intimal layer. Over
time the fatty streak develops into plaque leading to atherosclerosis. This leads to blockage of
blood flow. Typically the occurrence emanates from the development of atherosclerosis
affecting the lining of the heart muscles accumulating deposits of calcium, fatty lipids and
inflammatory cells forming a plaque which in turn blocks the blood flow to the heart (Di
Pietro, Formoso & Pandolfi, 2016).
Myocardial ischemia
Etiology
Myocardial ischemia occurs as a result of reduced blood flow to the heart due to partial
blockage of the heart arteries. The encountered regional infarcts result from lack of blood
flow on the epicedial artery blocking by the thrombus occurring due to lack of oxygenation. It
is also referred to as cardiac ischemia and reduces the ability of the heart muscles to pump
blood. Severe blockage can lead to a heart attack and is often indicative of abnormal heart
rhythms (Yahagi et al., 2016).
Pathogenesis
The occurrence of myocardial ischemia often occurs due to decreased blood flow. It
often develops over time as the arteries are blocked. States which might lead to this include,
atherosclerosis due to building plagues from cholesterol matter, blood clot due to rupture
blocking the artery and coronary spasms. Spasms occur due to a temporal tightening of the
muscles on the arterial wall thus preventing the flow of blood on the heart muscle. Various
conditions such as coronary heart disease, blood clot and coronary artery spasm can lead to
blockage of the leading to myocardial ischemia (Ibanez, Heusch, Ovize & Van de Werf,
2015).
QUESTION 2
Physiologic effects of the medications administered
The patient has been administered three drugs namely Aspirin, Glycerine Trinitrate
(GTN) and morphine to offer a combined therapeutic effect. aspirin belongs to the
acetylsalicylic acid call and is often used for the relief of pain. Often it is administered after
the occurrence of a heart attack which decreases the risks of death hence the administration at
the emergency department. On long term use, it is used to prevent the occurrence of heart
attack, ischemic strokes and blood clots especially from high risks category of people
(National Clinical Guideline Centre-UK, 2015).
inflammatory cells forming a plaque which in turn blocks the blood flow to the heart (Di
Pietro, Formoso & Pandolfi, 2016).
Myocardial ischemia
Etiology
Myocardial ischemia occurs as a result of reduced blood flow to the heart due to partial
blockage of the heart arteries. The encountered regional infarcts result from lack of blood
flow on the epicedial artery blocking by the thrombus occurring due to lack of oxygenation. It
is also referred to as cardiac ischemia and reduces the ability of the heart muscles to pump
blood. Severe blockage can lead to a heart attack and is often indicative of abnormal heart
rhythms (Yahagi et al., 2016).
Pathogenesis
The occurrence of myocardial ischemia often occurs due to decreased blood flow. It
often develops over time as the arteries are blocked. States which might lead to this include,
atherosclerosis due to building plagues from cholesterol matter, blood clot due to rupture
blocking the artery and coronary spasms. Spasms occur due to a temporal tightening of the
muscles on the arterial wall thus preventing the flow of blood on the heart muscle. Various
conditions such as coronary heart disease, blood clot and coronary artery spasm can lead to
blockage of the leading to myocardial ischemia (Ibanez, Heusch, Ovize & Van de Werf,
2015).
QUESTION 2
Physiologic effects of the medications administered
The patient has been administered three drugs namely Aspirin, Glycerine Trinitrate
(GTN) and morphine to offer a combined therapeutic effect. aspirin belongs to the
acetylsalicylic acid call and is often used for the relief of pain. Often it is administered after
the occurrence of a heart attack which decreases the risks of death hence the administration at
the emergency department. On long term use, it is used to prevent the occurrence of heart
attack, ischemic strokes and blood clots especially from high risks category of people
(National Clinical Guideline Centre-UK, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The role of aspirin in the occurrence of heart attack is crucial. Often previous patients
with a history of heart attack normally take aspirin daily to reduce the risks of death in heart
attack occurrence. Among patients with no history of heart attack as in the case for patient
Allan, it is offered to reduce the occurrence of nonfatal myocardial infarction however do not
reduce the overall risks of death, (Guirguis-Blake et al., 2016).
Glycerine Trinitrate-GTN is a common medication offered to patients who have had
heart failure cases and is used to manage chest pain often as a result of inadequate blood flow
to the heart. This drug is often used to manage acute myocardial infarction, angina, coronary
spasms, and severe hypertension. It is essential in the reduction of angina attacks and
reversing the state of angina developed. The drugs act quickly thus working effectively in
myocardial infarction state and is beneficial when used within the first few minutes (Bosson
et al., 2019).
Morphine belongs to the opioid analgesics class. It works by changing how the brain
works and responds to the overall pain. The morphine drug is offered as a pain medication
drug to manage both chronic and acute pain. Moreover, it is used to manage pain occurring
due to myocardial infarction. Further, the drug is beneficial in the management of shortness
of breath (Borges et al., 2016).
Combined therapeutic effects of these drugs administered to the patient are aimed at
reducing chest pain, alleviating the occurrence of myocardial infarction, angina and reduces
the risks of death due to imminent cardiac attack and heart related diseases. The history of the
patient having type II diabetes and hypertension increases the risks of heart attack and related
diseases. The therapeutical effects of these drugs aim at reducing the pain and managing the
patient state, normalizing the state thus giving room for further action. The drugs are crucial
for the patient, especially for the emergency state. The overall effect to the patient is to allow
for more internal assessment and more targeted treatment approach post-admission at the
emergency unit.
QUESTION 3
It is estimated that about 7 million patients often present at the emergency departments
yearly with costs over $5 billion (Kuhlman et al., 2019). Cardiovascular indications often
occur to about 20% of the patients showcasing chest discomfort, while approximately 5%
have acute life-threatening conditions while the remainder of the patients receive
with a history of heart attack normally take aspirin daily to reduce the risks of death in heart
attack occurrence. Among patients with no history of heart attack as in the case for patient
Allan, it is offered to reduce the occurrence of nonfatal myocardial infarction however do not
reduce the overall risks of death, (Guirguis-Blake et al., 2016).
Glycerine Trinitrate-GTN is a common medication offered to patients who have had
heart failure cases and is used to manage chest pain often as a result of inadequate blood flow
to the heart. This drug is often used to manage acute myocardial infarction, angina, coronary
spasms, and severe hypertension. It is essential in the reduction of angina attacks and
reversing the state of angina developed. The drugs act quickly thus working effectively in
myocardial infarction state and is beneficial when used within the first few minutes (Bosson
et al., 2019).
Morphine belongs to the opioid analgesics class. It works by changing how the brain
works and responds to the overall pain. The morphine drug is offered as a pain medication
drug to manage both chronic and acute pain. Moreover, it is used to manage pain occurring
due to myocardial infarction. Further, the drug is beneficial in the management of shortness
of breath (Borges et al., 2016).
Combined therapeutic effects of these drugs administered to the patient are aimed at
reducing chest pain, alleviating the occurrence of myocardial infarction, angina and reduces
the risks of death due to imminent cardiac attack and heart related diseases. The history of the
patient having type II diabetes and hypertension increases the risks of heart attack and related
diseases. The therapeutical effects of these drugs aim at reducing the pain and managing the
patient state, normalizing the state thus giving room for further action. The drugs are crucial
for the patient, especially for the emergency state. The overall effect to the patient is to allow
for more internal assessment and more targeted treatment approach post-admission at the
emergency unit.
QUESTION 3
It is estimated that about 7 million patients often present at the emergency departments
yearly with costs over $5 billion (Kuhlman et al., 2019). Cardiovascular indications often
occur to about 20% of the patients showcasing chest discomfort, while approximately 5%
have acute life-threatening conditions while the remainder of the patients receive
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
management for on cardiac pain and often portray low risks (Powers et al.,2016). Thus in the
clinical setting, health care providers need to be conversant and aware of urgent management
states of the patients presenting at the emergency department through an appropriate protocol
measures. Failure of adherence to set regulation often leads to wrong discharge for patients at
the ED who might be suffering from myocardial infarction increasing the risks of mortality
compared to those hospitalized at the hospital (Kline et al., 2015). Further undertaking long-
duration assessments of all patients presented at the emergency department can lead to
increased admissions and costs, hence evaluation at the ED needs to be rapid, accurate and
stratification measures being adopted immediately.
Patient history, physical assessment ECG examination and troponin serial measurement
have been the cornerstone of assessment related to chest pain at the ED. More often clinicians
and health care staff at the ED are faced with challenges with the decision-making process of
whether to admit or discharge patients when the tests are not straightforward and definitive
(Dezman, Mattu & Body, 2017). Studies have demonstrated that the acceptable risks for
hospital discharge at the ED without debate and clinical practice depend on personal comfort.
A study undertaken by Kline et al (2015) has shown that a miss rate of 2% is often acceptable
on the assessment of risks of harm from further testing beyond the benefit of confirming the
genesis of chest pain presentation.
More often clinical assessment contextualization is critical in improving assessment
assays. Exploration of various factors such as patient history, ECG, risks factors troponin
score and emergency department assessment of chest pain scores have been often been used
to assess the heart mechanism (Hsia, Hale & Tabas, 2016).
According to the National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand, clinical guidelines for the management of acute coronary
symptoms inclusive of observation of chests pain at the ED have been developed. More often
chest pains and coronary syndrome symptoms are often the major complaints being reported
at the emergency departments. In 2012, there were 68,200 cases reported. On average more
than 500,000 patients’ present with chest pains yearly in Australia, of these, 80% of the cases
do not have a positive confirmatory diagnosis (Chew et al., 2016).
Development of guideline by the association collaboration aimed at providing easier
management of patients presenting with chest pain due to suspicion of an acute coronary
clinical setting, health care providers need to be conversant and aware of urgent management
states of the patients presenting at the emergency department through an appropriate protocol
measures. Failure of adherence to set regulation often leads to wrong discharge for patients at
the ED who might be suffering from myocardial infarction increasing the risks of mortality
compared to those hospitalized at the hospital (Kline et al., 2015). Further undertaking long-
duration assessments of all patients presented at the emergency department can lead to
increased admissions and costs, hence evaluation at the ED needs to be rapid, accurate and
stratification measures being adopted immediately.
Patient history, physical assessment ECG examination and troponin serial measurement
have been the cornerstone of assessment related to chest pain at the ED. More often clinicians
and health care staff at the ED are faced with challenges with the decision-making process of
whether to admit or discharge patients when the tests are not straightforward and definitive
(Dezman, Mattu & Body, 2017). Studies have demonstrated that the acceptable risks for
hospital discharge at the ED without debate and clinical practice depend on personal comfort.
A study undertaken by Kline et al (2015) has shown that a miss rate of 2% is often acceptable
on the assessment of risks of harm from further testing beyond the benefit of confirming the
genesis of chest pain presentation.
More often clinical assessment contextualization is critical in improving assessment
assays. Exploration of various factors such as patient history, ECG, risks factors troponin
score and emergency department assessment of chest pain scores have been often been used
to assess the heart mechanism (Hsia, Hale & Tabas, 2016).
According to the National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand, clinical guidelines for the management of acute coronary
symptoms inclusive of observation of chests pain at the ED have been developed. More often
chest pains and coronary syndrome symptoms are often the major complaints being reported
at the emergency departments. In 2012, there were 68,200 cases reported. On average more
than 500,000 patients’ present with chest pains yearly in Australia, of these, 80% of the cases
do not have a positive confirmatory diagnosis (Chew et al., 2016).
Development of guideline by the association collaboration aimed at providing easier
management of patients presenting with chest pain due to suspicion of an acute coronary
syndrome. To be more compliant, the guidelines are often used in line with ACS clinical care
standards developed by the Australian Commission for Safety and Quality in Health care-
ACSQHC (Woodruffe et al., 2015) and the Australian Acute Coronary syndromes capability
framework (Chew et al., 2016).
The initial assessment at the ED department entails a series of the step being
undertaken in assessing the patients. The normal practice involves patients presenting with
chest pains and other symptoms suggestive of the acute coronary syndrome are taken through
the ECG for assessment of myocardial ischemia during the initial 10 minutes of clinical
contact at the ED, which is in line with Australian recommended practice. Patients having
acute symptoms and chest pain needed to undergo suspected acute coronary assessment
protocol which entails stratification measures.
Supplementation with oxygen is often undertaken among patients having lower oxygen
saturation levels of <93%. Administration of Aspirin therapy is undertaken among patients
depicting suspected development of acute cardiac syndrome having no contraindications are
administered after presentation at ED. Further, additional drug therapy such as administration
of antiplatelet and anticoagulation management need to be administered with caution after
confirmatory diagnosis of probable occurrence of cardiac distress syndrome.
Assessment of chest pain at the ED needs to follow accurate assessment protocol using
none invasive testing procedures through a validated acute coronary syndrome tool and ECG
testing. Patients who do not proceed for further tests are regarded as low risks. In cases of
positive suspicion of acute coronary syndrome, an assessment protocol is followed to assess
the patient. Point of care assays, sensitive lab-based assays, and highly sensitive lab assays
can be undertaken on the patient. Differential diagnosis of chests pain causes follows a three-
tier chart system. Ischemia cardiovascular causes depict cute myocardial infection, stable
angina, severe aortic stenosis, and tachyarrhythmia. In none, ischemic cardiovascular chest
pain can be caused by aortic dissection, pulmonary embolism, pericarditis, and
gastrointestinal causes. in noncardiovascular causes can be linked to musculoskeletal causes,
pulmonary sources and other aetiologies such as sickle cell diseases.
A series of medical diagnosis is recommended and undertaken at the ED upon
confirmation of acute coronary syndrome. Management using aspirin 300mg administered
orally is recommended for the patients confirmed. Among the high risks, patients’ usage of
standards developed by the Australian Commission for Safety and Quality in Health care-
ACSQHC (Woodruffe et al., 2015) and the Australian Acute Coronary syndromes capability
framework (Chew et al., 2016).
The initial assessment at the ED department entails a series of the step being
undertaken in assessing the patients. The normal practice involves patients presenting with
chest pains and other symptoms suggestive of the acute coronary syndrome are taken through
the ECG for assessment of myocardial ischemia during the initial 10 minutes of clinical
contact at the ED, which is in line with Australian recommended practice. Patients having
acute symptoms and chest pain needed to undergo suspected acute coronary assessment
protocol which entails stratification measures.
Supplementation with oxygen is often undertaken among patients having lower oxygen
saturation levels of <93%. Administration of Aspirin therapy is undertaken among patients
depicting suspected development of acute cardiac syndrome having no contraindications are
administered after presentation at ED. Further, additional drug therapy such as administration
of antiplatelet and anticoagulation management need to be administered with caution after
confirmatory diagnosis of probable occurrence of cardiac distress syndrome.
Assessment of chest pain at the ED needs to follow accurate assessment protocol using
none invasive testing procedures through a validated acute coronary syndrome tool and ECG
testing. Patients who do not proceed for further tests are regarded as low risks. In cases of
positive suspicion of acute coronary syndrome, an assessment protocol is followed to assess
the patient. Point of care assays, sensitive lab-based assays, and highly sensitive lab assays
can be undertaken on the patient. Differential diagnosis of chests pain causes follows a three-
tier chart system. Ischemia cardiovascular causes depict cute myocardial infection, stable
angina, severe aortic stenosis, and tachyarrhythmia. In none, ischemic cardiovascular chest
pain can be caused by aortic dissection, pulmonary embolism, pericarditis, and
gastrointestinal causes. in noncardiovascular causes can be linked to musculoskeletal causes,
pulmonary sources and other aetiologies such as sickle cell diseases.
A series of medical diagnosis is recommended and undertaken at the ED upon
confirmation of acute coronary syndrome. Management using aspirin 300mg administered
orally is recommended for the patients confirmed. Among the high risks, patients’ usage of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
P2Y12 inhibitor is recommended. Further administration of intravenous glycoprotein and
Bivalirudin can be administered as an alternative. These guidelines are in line with Australian
guidelines for the management of chest pains and confirmatory assessment protocol for
coronary syndrome among patients presenting at the Emergency Department.
Bivalirudin can be administered as an alternative. These guidelines are in line with Australian
guidelines for the management of chest pains and confirmatory assessment protocol for
coronary syndrome among patients presenting at the Emergency Department.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

References
Ambrose, J. A., & Singh, M. (2015). Pathophysiology of coronary artery disease leading to
acute coronary syndromes. F1000prime reports, 7.
Borges, R. S., Vale, J. K., Pereira, G. A., Veiga, A. A., Junior, J. B., & da Silva, A. B. (2016).
An antioxidant mechanism of morphine and related derivatives. Medicinal Chemistry
Research, 25(5), 852-857.
Bosson, N., Isakson, B., Morgan, J. A., Kaji, A. H., Uner, A., Hurley, K., ... & Niemann, J. T.
(2019). Safety and Effectiveness of Field Nitroglycerin in Patients with Suspected ST
Elevation Myocardial Infarction. Prehospital Emergency Care, 1-9.
Breen, C. J., Kelly, G. P., & Kernohan, W. G. (2019). ECG interpretation skill acquisition: A
review of learning, teaching and assessment. Journal of electrocardiology.
Chew, D. P., Scott, I. A., Cullen, L., French, J. K., Briffa, T. G., Tideman, P. A., ... &
Aylward, P. E. (2016). National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand: Australian clinical guidelines for the management of acute
coronary syndromes 2016. Medical Journal of Australia, 205(3), 128-133.
Dezman, Z. D., Mattu, A., & Body, R. (2017). Utility of the history and physical examination
in the detection of acute coronary syndromes in emergency department patients.
Western Journal of Emergency Medicine, 18(4), 752.
Di Pietro, N., Formoso, G., & Pandolfi, A. (2016). Physiology and pathophysiology of
oxLDL uptake by vascular wall cells in atherosclerosis. Vascular pharmacology, 84, 1-
7.
Doubell, A. (2017). The ECG Atlas of Cardiac Rhythms. SAMJ South African Medical
Journal, 107(8), 652-653.
Guirguis-Blake JM, Evans CV, Senger CA, O'Connor EA, Whitlock EP (June 2016).
"Aspirin for the Primary Prevention of Cardiovascular Events: A Systematic Evidence
Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine
(Systematic Review & Meta-Analysis). 164 (12): 804–13. doi:10.7326/M15-2113.
PMID 27064410.
Hsia, R. Y., Hale, Z., & Tabas, J. A. (2016). A national study of the prevalence of life-
threatening diagnoses in patients with chest pain. JAMA internal medicine, 176(7),
1029-1032.
Ambrose, J. A., & Singh, M. (2015). Pathophysiology of coronary artery disease leading to
acute coronary syndromes. F1000prime reports, 7.
Borges, R. S., Vale, J. K., Pereira, G. A., Veiga, A. A., Junior, J. B., & da Silva, A. B. (2016).
An antioxidant mechanism of morphine and related derivatives. Medicinal Chemistry
Research, 25(5), 852-857.
Bosson, N., Isakson, B., Morgan, J. A., Kaji, A. H., Uner, A., Hurley, K., ... & Niemann, J. T.
(2019). Safety and Effectiveness of Field Nitroglycerin in Patients with Suspected ST
Elevation Myocardial Infarction. Prehospital Emergency Care, 1-9.
Breen, C. J., Kelly, G. P., & Kernohan, W. G. (2019). ECG interpretation skill acquisition: A
review of learning, teaching and assessment. Journal of electrocardiology.
Chew, D. P., Scott, I. A., Cullen, L., French, J. K., Briffa, T. G., Tideman, P. A., ... &
Aylward, P. E. (2016). National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand: Australian clinical guidelines for the management of acute
coronary syndromes 2016. Medical Journal of Australia, 205(3), 128-133.
Dezman, Z. D., Mattu, A., & Body, R. (2017). Utility of the history and physical examination
in the detection of acute coronary syndromes in emergency department patients.
Western Journal of Emergency Medicine, 18(4), 752.
Di Pietro, N., Formoso, G., & Pandolfi, A. (2016). Physiology and pathophysiology of
oxLDL uptake by vascular wall cells in atherosclerosis. Vascular pharmacology, 84, 1-
7.
Doubell, A. (2017). The ECG Atlas of Cardiac Rhythms. SAMJ South African Medical
Journal, 107(8), 652-653.
Guirguis-Blake JM, Evans CV, Senger CA, O'Connor EA, Whitlock EP (June 2016).
"Aspirin for the Primary Prevention of Cardiovascular Events: A Systematic Evidence
Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine
(Systematic Review & Meta-Analysis). 164 (12): 804–13. doi:10.7326/M15-2113.
PMID 27064410.
Hsia, R. Y., Hale, Z., & Tabas, J. A. (2016). A national study of the prevalence of life-
threatening diagnoses in patients with chest pain. JAMA internal medicine, 176(7),
1029-1032.
Ibanez, B., Heusch, G., Ovize, M., & Van de Werf, F. (2015). Evolving therapies for
myocardial ischemia/reperfusion injury. Journal of the American College of
Cardiology, 65(14), 1454-1471.
Karimian, N., Guo, Z., Tehranipoor, M., & Forte, D. (2016). Highly reliable key generation
from electrocardiogram (ECG). IEEE Transactions on Biomedical Engineering, 64(6),
1400-1411.
Kline, J. A., Johnson, C. L., Pollack, C. V., Diercks, D. B., Hollander, J. E., Newgard, C. D.,
& Garvey, J. L. (2015). Pretest probability assessment derived from attribute matching.
BMC medical informatics and decision making, 5(1), 26.
Kuhlman, J., Moorhead, D., Kerpchar, J., Peach, D. J., Ahmad, S., & O'Brien, P. B. (2019).
Clinical Transformation Through Change Management Case Study: Chest Pain in the
Emergency Department. EClinicalMedicine, 10, 78-83.
Magnusson, P., Samuelsson, M., Pergolizzi Jr, J. V., Annabi, H., & LeQuang, J. A. (2019).
Atrial Fibrillation and the Role of Thumb ECGs. In Cardiovascular Devices.
IntechOpen.
National Clinical Guideline Centre (UK) ( 2015). "Myocardial infarction with ST-segment
elevation: the acute management of myocardial infarction with ST-segment elevation
[Internet]". NICE Clinical Guidelines (167). 17.2 Asprin. PMID 25340241
Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker,
K., ... & Jauch, E. C. (2018). 2018 guidelines for the early management of patients with
acute ischemic stroke: a guideline for healthcare professionals from the American Heart
Association/American Stroke Association. Stroke, 49(3), e46-e99.
Sullivan, A., Kaib, T. E., Nicolo, F., Szymkiewicz, S., & Whiting, J. T. (2018). U.S. Patent
Application No. 15/782,568.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G.
(2015). Australian Cardiovascular Health and Rehabilitation Association (ACRA) core
components of cardiovascular disease secondary prevention and cardiac rehabilitation
2014. Heart, Lung and Circulation, 24(5), 430-441.
Yahagi, K., Kolodgie, F. D., Otsuka, F., Finn, A. V., Davis, H. R., Joner, M., & Virmani, R.
(2016). Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis.
Nature Reviews Cardiology, 13(2), 79.
myocardial ischemia/reperfusion injury. Journal of the American College of
Cardiology, 65(14), 1454-1471.
Karimian, N., Guo, Z., Tehranipoor, M., & Forte, D. (2016). Highly reliable key generation
from electrocardiogram (ECG). IEEE Transactions on Biomedical Engineering, 64(6),
1400-1411.
Kline, J. A., Johnson, C. L., Pollack, C. V., Diercks, D. B., Hollander, J. E., Newgard, C. D.,
& Garvey, J. L. (2015). Pretest probability assessment derived from attribute matching.
BMC medical informatics and decision making, 5(1), 26.
Kuhlman, J., Moorhead, D., Kerpchar, J., Peach, D. J., Ahmad, S., & O'Brien, P. B. (2019).
Clinical Transformation Through Change Management Case Study: Chest Pain in the
Emergency Department. EClinicalMedicine, 10, 78-83.
Magnusson, P., Samuelsson, M., Pergolizzi Jr, J. V., Annabi, H., & LeQuang, J. A. (2019).
Atrial Fibrillation and the Role of Thumb ECGs. In Cardiovascular Devices.
IntechOpen.
National Clinical Guideline Centre (UK) ( 2015). "Myocardial infarction with ST-segment
elevation: the acute management of myocardial infarction with ST-segment elevation
[Internet]". NICE Clinical Guidelines (167). 17.2 Asprin. PMID 25340241
Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker,
K., ... & Jauch, E. C. (2018). 2018 guidelines for the early management of patients with
acute ischemic stroke: a guideline for healthcare professionals from the American Heart
Association/American Stroke Association. Stroke, 49(3), e46-e99.
Sullivan, A., Kaib, T. E., Nicolo, F., Szymkiewicz, S., & Whiting, J. T. (2018). U.S. Patent
Application No. 15/782,568.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G.
(2015). Australian Cardiovascular Health and Rehabilitation Association (ACRA) core
components of cardiovascular disease secondary prevention and cardiac rehabilitation
2014. Heart, Lung and Circulation, 24(5), 430-441.
Yahagi, K., Kolodgie, F. D., Otsuka, F., Finn, A. V., Davis, H. R., Joner, M., & Virmani, R.
(2016). Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis.
Nature Reviews Cardiology, 13(2), 79.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





