Case Study: Managing COPD with the Roper-Logan-Tierney Nursing Model
VerifiedAdded on 2023/04/20
|22
|8178
|310
Case Study
AI Summary
This case study presents a comprehensive analysis of a 65-year-old patient, Delroy, suffering from Chronic Obstructive Pulmonary Disease (COPD) and multiple comorbidities. It delves into the pathophysiology of COPD, breathlessness, and malnutrition, linking these to Delroy's medical history, including smoking, osteoarthritis, and cardiovascular events. The paper critically analyzes the Roper-Logan-Tierney model of nursing, emphasizing its application in assessment, diagnosis, planning, and implementation of care strategies. The role of the nurse is highlighted in conducting holistic patient assessments, developing comprehensive care plans, and managing complex multiple co-morbidities to improve patient outcomes. The assessment process includes the use of MRC Dyspnoea scale and Malnutrition Universal Screening Tool (MUST) to understand the patient's condition and nutritional status, demonstrating the integration of evidence-based knowledge into practical nursing care.

Living With Chronic Obstructive Pulmonary Disorder
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Role of nurse in providing high quality care to the patients is highly significant.
Nurses are also known for developing therapeutic relationship with patient in order to
improve health and well-being (Toney-Butler & Thayer, 2018). Nursing practice is
systematically influenced and guided by the nursing practice standards, guidelines
and codes. Nurses work closely with individual, families and communities to deliver
high quality care, improving service delivery and improving patient outcomes
(Bittencourt & Crossetti, 2013). Studies have also informed that nursing process
plays the role of a systematic guide to patient centred or client centred care in a
sequential step. Assessment, diagnosis, planning and implementation of care
strategies are the significant aspects of nursing practice. These processes require
critical thinking and problem-solving skills (Toney-Butler & Thayer, 2018). Nurses are
also required to apply the clinical judgment skills for evaluating patient’s condition,
understanding the pathophysiology of disease and implement effective care
strategies.
Therefore, this paper will focus on developing an evidence-based knowledge
regarding the role of nurse in conducting effective assessment, diagnosis and
implementation of evidence based care. This paper will discuss the case study of
Delroy, who is a 65 years old gentleman admitted to the hospital with the problem of
shortness of breath. Some of the other signs and symptoms that patient has been
experiencing are breathlessness, pain in mobility due to the presence of
osteoarthritis in the knees, malnutrition, constipation, low mood, BMI 42 and limited
mobility. Past medical history of the patient informs about the presence of chronic
obstructive pulmonary disease, osteoarthritis, acute renal failure, hypertension,
history of smoking and cardiovascular accident with residual left sided weakness.
This paper will inform about the link between the patient’s medical history and signs
and symptoms that he is experiencing with a detailed analysis of the
pathophysiology of disease, and will present a critical analysis of the Roper Logan
and Tierney (2000) framework and how the complex multiple co-morbidities can be
managed through effective nursing care.
Pathophysiology of COPD
Role of nurse in providing high quality care to the patients is highly significant.
Nurses are also known for developing therapeutic relationship with patient in order to
improve health and well-being (Toney-Butler & Thayer, 2018). Nursing practice is
systematically influenced and guided by the nursing practice standards, guidelines
and codes. Nurses work closely with individual, families and communities to deliver
high quality care, improving service delivery and improving patient outcomes
(Bittencourt & Crossetti, 2013). Studies have also informed that nursing process
plays the role of a systematic guide to patient centred or client centred care in a
sequential step. Assessment, diagnosis, planning and implementation of care
strategies are the significant aspects of nursing practice. These processes require
critical thinking and problem-solving skills (Toney-Butler & Thayer, 2018). Nurses are
also required to apply the clinical judgment skills for evaluating patient’s condition,
understanding the pathophysiology of disease and implement effective care
strategies.
Therefore, this paper will focus on developing an evidence-based knowledge
regarding the role of nurse in conducting effective assessment, diagnosis and
implementation of evidence based care. This paper will discuss the case study of
Delroy, who is a 65 years old gentleman admitted to the hospital with the problem of
shortness of breath. Some of the other signs and symptoms that patient has been
experiencing are breathlessness, pain in mobility due to the presence of
osteoarthritis in the knees, malnutrition, constipation, low mood, BMI 42 and limited
mobility. Past medical history of the patient informs about the presence of chronic
obstructive pulmonary disease, osteoarthritis, acute renal failure, hypertension,
history of smoking and cardiovascular accident with residual left sided weakness.
This paper will inform about the link between the patient’s medical history and signs
and symptoms that he is experiencing with a detailed analysis of the
pathophysiology of disease, and will present a critical analysis of the Roper Logan
and Tierney (2000) framework and how the complex multiple co-morbidities can be
managed through effective nursing care.
Pathophysiology of COPD
According to the patient’s history, the main health issue that he suffers include
Chronic Obstructive Pulmonary Disease (COPD). This is a chronic lung disease,
which is also progressive in nature and makes the process of breathing very difficult.
Berg & Wright (2016) have defined COPD as the preventable and treatable
condition, which is characterised by the limitation of the airflow. This disease is often
progressive and can also be linked to the chronic inflammatory response in the
airway that makes the breathing process very difficult. The disease can also become
severe with the associated comorbidities and exacerbations (Berg & Wright, 2016).
This condition results in limiting the airflow and results in creating breathlessness.
In the healthy lungs, when the air is inhaled it travels from the wind pipe to airway in
to the lungs through the bronchial tube. Inside the human lungs the bronchial tubes
are divided in thousands of small branches that are called as bronchioles (Kim &
Criner, 2013). At the end of these small and thin branches are present the air sacks
that are called as alveoli. These alveoli are surrounded by the bunch of the
capillaries. When the oxygen is inhaled it passes from alveoli to the blood capillaries
and enter the blood to be transferred to the body (Kim & Criner, 2013). Therefore,
the elasticity of the airway and air sacs become significant for the appropriate flow of
air. In the patients suffering with COPD the walls of the alveoli are damaged and
they lose their elasticity and the walls of the airway also thicken and get inflamed
resulting in obstructing the air flow process (Tuder & Petrache, 2012).
Therefore, COPD is considered as the progressive chronic inflammatory condition, in
which the small airways and alveoli are mainly affected. The studies have identified
that a series of physiological changes occur that impact the well-being, quality of life
and makes the survival of the patient very difficult (Tuder & Petrache, 2012). The first
problem that occurs start with the elastin proteolysis that results in reducing the
elastic recoil pressure in the lungs. The movement and the integrity of bronchioles is
mainly dependent on the elastic recoil pressure of the lungs, which is mainly
facilitated by the elastic tissue. Therefore, due to damage of the elastin in COPD
results in narrowing the airway and reduce the air flow in bronchioles and the air gets
trapped in the lungs (Hogg & Timens, 2009). The second pathophysiological problem
that occurs is associated with the fibrotic remodelling of the airway. This problem
results in permanent narrowing of the airway resulting in increased airway
Chronic Obstructive Pulmonary Disease (COPD). This is a chronic lung disease,
which is also progressive in nature and makes the process of breathing very difficult.
Berg & Wright (2016) have defined COPD as the preventable and treatable
condition, which is characterised by the limitation of the airflow. This disease is often
progressive and can also be linked to the chronic inflammatory response in the
airway that makes the breathing process very difficult. The disease can also become
severe with the associated comorbidities and exacerbations (Berg & Wright, 2016).
This condition results in limiting the airflow and results in creating breathlessness.
In the healthy lungs, when the air is inhaled it travels from the wind pipe to airway in
to the lungs through the bronchial tube. Inside the human lungs the bronchial tubes
are divided in thousands of small branches that are called as bronchioles (Kim &
Criner, 2013). At the end of these small and thin branches are present the air sacks
that are called as alveoli. These alveoli are surrounded by the bunch of the
capillaries. When the oxygen is inhaled it passes from alveoli to the blood capillaries
and enter the blood to be transferred to the body (Kim & Criner, 2013). Therefore,
the elasticity of the airway and air sacs become significant for the appropriate flow of
air. In the patients suffering with COPD the walls of the alveoli are damaged and
they lose their elasticity and the walls of the airway also thicken and get inflamed
resulting in obstructing the air flow process (Tuder & Petrache, 2012).
Therefore, COPD is considered as the progressive chronic inflammatory condition, in
which the small airways and alveoli are mainly affected. The studies have identified
that a series of physiological changes occur that impact the well-being, quality of life
and makes the survival of the patient very difficult (Tuder & Petrache, 2012). The first
problem that occurs start with the elastin proteolysis that results in reducing the
elastic recoil pressure in the lungs. The movement and the integrity of bronchioles is
mainly dependent on the elastic recoil pressure of the lungs, which is mainly
facilitated by the elastic tissue. Therefore, due to damage of the elastin in COPD
results in narrowing the airway and reduce the air flow in bronchioles and the air gets
trapped in the lungs (Hogg & Timens, 2009). The second pathophysiological problem
that occurs is associated with the fibrotic remodelling of the airway. This problem
results in permanent narrowing of the airway resulting in increased airway
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
resistance, which do not even respond effectively to the bronchodilators (Berg &
Wright, 2016).
Pathophysiology associated with Breathlessness
One of the most common symptoms that is associated with COPD is breathlessness.
The sensation of breathless ness is also called as Dyspnea (Anzueto & Miravitlles,
2017). The patient suffering from COPD experience this symptom due to many
problems, such as reduced physical activity, increased level of anxiety and
depression and airway re-modelling due to the disease manifestation. Study
conducted by Antoniu (2010) has identified that dyspnea in COPD involves a very
complex pathophysiological mechanism that significantly involves “dynamic
hyperinflation, increased ventilatory demand relative to impaired capacity,
hypoxemia, hypercapnia, and neuromechanical dissociation” (p. 217). Antoniu
(2010) further informed that during the process of breathing, already damaged and
reduced pulmonary elasticity recoil, results in increasing the expiratory lung volume,
due to which dynamic hyperinflation (DH) starts occurring. Dynamic hyperinflation
(DH) is also associated with many pathophysiological mechanisms, such as
remodelling of the airway, reconfiguration of the rib cage (which mainly occurs in
order to contain the lungs that hjave become over inflated), increased pressure on
the respiratory muscles (which occurs to manage with the problem of reduced
elasticity) (Ko et al, 2016). During the process of any kind of physical activity or
exertion, it results in increasing inflammation and increasing impairment of dynamic
hyperinflation. This whole mechanism results in placing more pressure on the
respiratory muscles to increase the inspiratory capacity (Pavord et al, 2016).
Therefore, the increased ventilatory demand, which could not be fulfilled due to this
mechanism and results in increasing the problem of shortness of breath or
breathlessness.
Pathophysiology Associated with Malnutrition
Another symptom is malnutrition that is affecting the quality of life of the patient.
Studies have identified that malnutrition occurs as the common problem among the
patients suffering with COPD and considered as the most prevalent symptom that
affects the patient’s ability to conduct activities of daily life due to weakness ( Rawal,
& Yadav, 2015). Malnutrition results in reducing the ability of physical exercise. The
Wright, 2016).
Pathophysiology associated with Breathlessness
One of the most common symptoms that is associated with COPD is breathlessness.
The sensation of breathless ness is also called as Dyspnea (Anzueto & Miravitlles,
2017). The patient suffering from COPD experience this symptom due to many
problems, such as reduced physical activity, increased level of anxiety and
depression and airway re-modelling due to the disease manifestation. Study
conducted by Antoniu (2010) has identified that dyspnea in COPD involves a very
complex pathophysiological mechanism that significantly involves “dynamic
hyperinflation, increased ventilatory demand relative to impaired capacity,
hypoxemia, hypercapnia, and neuromechanical dissociation” (p. 217). Antoniu
(2010) further informed that during the process of breathing, already damaged and
reduced pulmonary elasticity recoil, results in increasing the expiratory lung volume,
due to which dynamic hyperinflation (DH) starts occurring. Dynamic hyperinflation
(DH) is also associated with many pathophysiological mechanisms, such as
remodelling of the airway, reconfiguration of the rib cage (which mainly occurs in
order to contain the lungs that hjave become over inflated), increased pressure on
the respiratory muscles (which occurs to manage with the problem of reduced
elasticity) (Ko et al, 2016). During the process of any kind of physical activity or
exertion, it results in increasing inflammation and increasing impairment of dynamic
hyperinflation. This whole mechanism results in placing more pressure on the
respiratory muscles to increase the inspiratory capacity (Pavord et al, 2016).
Therefore, the increased ventilatory demand, which could not be fulfilled due to this
mechanism and results in increasing the problem of shortness of breath or
breathlessness.
Pathophysiology Associated with Malnutrition
Another symptom is malnutrition that is affecting the quality of life of the patient.
Studies have identified that malnutrition occurs as the common problem among the
patients suffering with COPD and considered as the most prevalent symptom that
affects the patient’s ability to conduct activities of daily life due to weakness ( Rawal,
& Yadav, 2015). Malnutrition results in reducing the ability of physical exercise. The
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
symptom of malnutrition in the COPD patients is also referred to as pulmonary
cachexia syndrome” (PCS), which is mainly character sided as the loss of the fat free
body mass and muscle wasting causing malnutrition (Rawal, & Yadav, 2015, p. 152).
The problem of weight loss is identified among 25% to 40% patients suffering with
COPD (Itoh, et al, 2013). The most significant pathophysiological condition
associated with COPD is emphysema, which results in causing breathing difficulty.
Under nutrition can also be caused due to the presence of depressive symptoms and
shortness of breath. The pathophysiology associated with the increased work of
breathing, such as the damage of alveoli, remodelling in the airway and inflammation
results in increasing pressure on the respiratory muscle and increased energy
expenditure (Mete et al, 2018). The process of systematic inflammation results in the
higher production of inflammatory cytokines such as interleukin (IL)-6, IL-8, and
tumor necrosis factor (TNF)-α, and also of chemokines (Itoh, et al, 2013). Studies
have also identified that increase in the production of TNF-α results in causing
malnutrition. Also, the increased production of IL-6 p results in affecting the patient’s
appetite. In the given case study, patient’s BMI has been found to be 42, which
indicates obesity. Therefore, in the obsess patients the level of serum IL-6 is
elevated, due to its production from the white adipose tissues. Although, the studies
have shown that clear reason of micturition or under nutrition in COPD patients has
not been identified (Itoh, et al, 2013).
The Role of Nurse
Studies have identified that role of nurses in healthcare is very prominent, as the
number of nurses is highest in the healthcare system in comparison to other
professionals and they are responsible for providing personalised care to the
patients (Bodenheimer & Bauer, 2016). Nurses are often the first person to interact
with the patient, conducting assessment, developing diagnosis and implementing
care plans (Allen, & Hughes, 2017). Therefore, the role of nurses is inevitable in
healthcare system. Nursing practice lead and influence public health on various
levels.
Roper-Logan-Tierney Model of Nursing is considered as the practice centred
theoretical model, which is “grounded in realism and accessibility” (Williams, 2015, p.
24). The main aspect of this nursing model is that it helps in the assessment,
cachexia syndrome” (PCS), which is mainly character sided as the loss of the fat free
body mass and muscle wasting causing malnutrition (Rawal, & Yadav, 2015, p. 152).
The problem of weight loss is identified among 25% to 40% patients suffering with
COPD (Itoh, et al, 2013). The most significant pathophysiological condition
associated with COPD is emphysema, which results in causing breathing difficulty.
Under nutrition can also be caused due to the presence of depressive symptoms and
shortness of breath. The pathophysiology associated with the increased work of
breathing, such as the damage of alveoli, remodelling in the airway and inflammation
results in increasing pressure on the respiratory muscle and increased energy
expenditure (Mete et al, 2018). The process of systematic inflammation results in the
higher production of inflammatory cytokines such as interleukin (IL)-6, IL-8, and
tumor necrosis factor (TNF)-α, and also of chemokines (Itoh, et al, 2013). Studies
have also identified that increase in the production of TNF-α results in causing
malnutrition. Also, the increased production of IL-6 p results in affecting the patient’s
appetite. In the given case study, patient’s BMI has been found to be 42, which
indicates obesity. Therefore, in the obsess patients the level of serum IL-6 is
elevated, due to its production from the white adipose tissues. Although, the studies
have shown that clear reason of micturition or under nutrition in COPD patients has
not been identified (Itoh, et al, 2013).
The Role of Nurse
Studies have identified that role of nurses in healthcare is very prominent, as the
number of nurses is highest in the healthcare system in comparison to other
professionals and they are responsible for providing personalised care to the
patients (Bodenheimer & Bauer, 2016). Nurses are often the first person to interact
with the patient, conducting assessment, developing diagnosis and implementing
care plans (Allen, & Hughes, 2017). Therefore, the role of nurses is inevitable in
healthcare system. Nursing practice lead and influence public health on various
levels.
Roper-Logan-Tierney Model of Nursing is considered as the practice centred
theoretical model, which is “grounded in realism and accessibility” (Williams, 2015, p.
24). The main aspect of this nursing model is that it helps in the assessment,
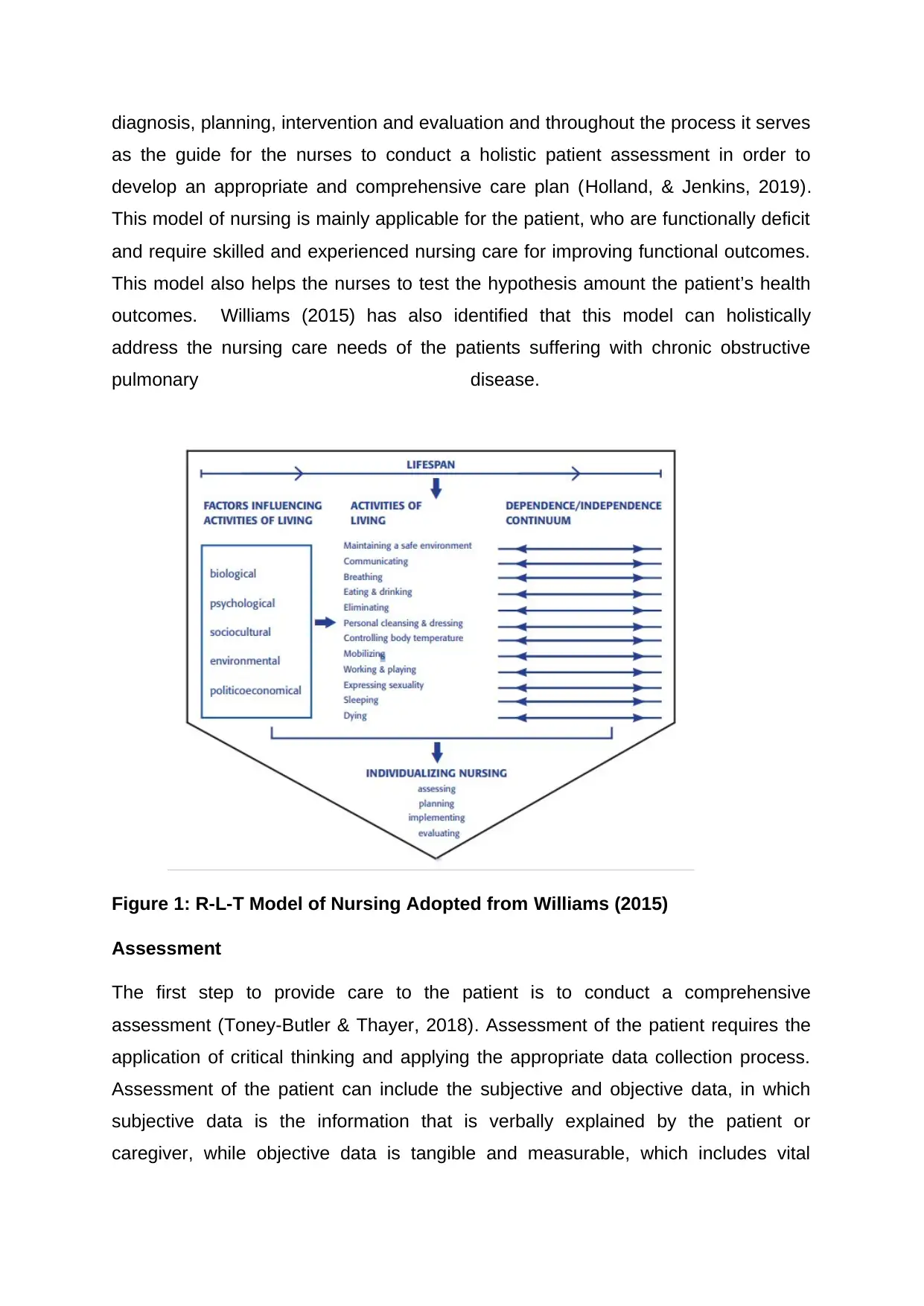
diagnosis, planning, intervention and evaluation and throughout the process it serves
as the guide for the nurses to conduct a holistic patient assessment in order to
develop an appropriate and comprehensive care plan (Holland, & Jenkins, 2019).
This model of nursing is mainly applicable for the patient, who are functionally deficit
and require skilled and experienced nursing care for improving functional outcomes.
This model also helps the nurses to test the hypothesis amount the patient’s health
outcomes. Williams (2015) has also identified that this model can holistically
address the nursing care needs of the patients suffering with chronic obstructive
pulmonary disease.
Figure 1: R-L-T Model of Nursing Adopted from Williams (2015)
Assessment
The first step to provide care to the patient is to conduct a comprehensive
assessment (Toney-Butler & Thayer, 2018). Assessment of the patient requires the
application of critical thinking and applying the appropriate data collection process.
Assessment of the patient can include the subjective and objective data, in which
subjective data is the information that is verbally explained by the patient or
caregiver, while objective data is tangible and measurable, which includes vital
as the guide for the nurses to conduct a holistic patient assessment in order to
develop an appropriate and comprehensive care plan (Holland, & Jenkins, 2019).
This model of nursing is mainly applicable for the patient, who are functionally deficit
and require skilled and experienced nursing care for improving functional outcomes.
This model also helps the nurses to test the hypothesis amount the patient’s health
outcomes. Williams (2015) has also identified that this model can holistically
address the nursing care needs of the patients suffering with chronic obstructive
pulmonary disease.
Figure 1: R-L-T Model of Nursing Adopted from Williams (2015)
Assessment
The first step to provide care to the patient is to conduct a comprehensive
assessment (Toney-Butler & Thayer, 2018). Assessment of the patient requires the
application of critical thinking and applying the appropriate data collection process.
Assessment of the patient can include the subjective and objective data, in which
subjective data is the information that is verbally explained by the patient or
caregiver, while objective data is tangible and measurable, which includes vital
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
sings, intake and output of fluid or food and physical condition of patient (Toney-
Butler & Thayer, 2018).
Delroy was presented to the hospital with the symptoms of breathlessness or
shortness of breath. A comprehensive assessment of Delroy was conducted for
understanding the reason behind his present symptoms. MRC Dyspnoea scale was
used for the assessment of Dyspnoea. This scale helped in grading patient’s
condition on the scale from 1 to 4. Firstly, the assessment included the analysis of
the patient’s past medical history. Medical history of Delroy informed that he suffers
from Chronic Obstructive Pulmonary Disease. This is a very disabling condition that
is characterised by the inflammation of the airway. Some of the studies have also
confirmed that COPD is an umbrella term to describe the various progressive
conditions, such as emphysema, chronic bronchitis and airway remodelling and
resistance (Han et al, 2010). Patient’s medical history also informed that he smokes
cigarettes and also occasionally drink alcohol. Study conducted by Barnes (2016)
has identified that smoking is a significant cause of COPD in late adulthood. Active
exposure to smoke can contribute to the problem of COPD.
Another important symptom that has been identified in the case of Delroy is that he
is undernourished. Malnutrition is also an important symptom of COPD, which is
associated to various underlying mechanism that reduces the individual’s appetite.
Malnutrition assessment of the patient was done through Malnutrition universal
screening Tool (MUST) (Chao et al, 2015). MUST is an important screening tool that
can be applied effectively with elderly patients in all healthcare settings. This is a
five-step screening tool that can significantly help in adopting the strategies that
could improve nutritional status of the patient (Chao et al, 2015). Assessment also
included the social history of the patient that informed, Delroy is unable to carry out
activities of daily life. He is significantly dependent on his wife for the activities such
as personal cleaning and dressing. Delroy also feels unable to go upstairs to his bed
for sleeping and unable to engage in sexual relationship with his wife, as the physical
activity results in worsening the symptom of breathlessness. Study conducted by
ZuWallack, & Esteban, (2014) has identified that physical activity can
exacerbate symptoms because the physical activity requires increase work of
breathing and effective gas exchange. However, in the patient suffering with COPD.
The airway is remodelled that result in causing obstruction and the increased work of
Butler & Thayer, 2018).
Delroy was presented to the hospital with the symptoms of breathlessness or
shortness of breath. A comprehensive assessment of Delroy was conducted for
understanding the reason behind his present symptoms. MRC Dyspnoea scale was
used for the assessment of Dyspnoea. This scale helped in grading patient’s
condition on the scale from 1 to 4. Firstly, the assessment included the analysis of
the patient’s past medical history. Medical history of Delroy informed that he suffers
from Chronic Obstructive Pulmonary Disease. This is a very disabling condition that
is characterised by the inflammation of the airway. Some of the studies have also
confirmed that COPD is an umbrella term to describe the various progressive
conditions, such as emphysema, chronic bronchitis and airway remodelling and
resistance (Han et al, 2010). Patient’s medical history also informed that he smokes
cigarettes and also occasionally drink alcohol. Study conducted by Barnes (2016)
has identified that smoking is a significant cause of COPD in late adulthood. Active
exposure to smoke can contribute to the problem of COPD.
Another important symptom that has been identified in the case of Delroy is that he
is undernourished. Malnutrition is also an important symptom of COPD, which is
associated to various underlying mechanism that reduces the individual’s appetite.
Malnutrition assessment of the patient was done through Malnutrition universal
screening Tool (MUST) (Chao et al, 2015). MUST is an important screening tool that
can be applied effectively with elderly patients in all healthcare settings. This is a
five-step screening tool that can significantly help in adopting the strategies that
could improve nutritional status of the patient (Chao et al, 2015). Assessment also
included the social history of the patient that informed, Delroy is unable to carry out
activities of daily life. He is significantly dependent on his wife for the activities such
as personal cleaning and dressing. Delroy also feels unable to go upstairs to his bed
for sleeping and unable to engage in sexual relationship with his wife, as the physical
activity results in worsening the symptom of breathlessness. Study conducted by
ZuWallack, & Esteban, (2014) has identified that physical activity can
exacerbate symptoms because the physical activity requires increase work of
breathing and effective gas exchange. However, in the patient suffering with COPD.
The airway is remodelled that result in causing obstruction and the increased work of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
breathing reduces the air flow in bronchioles resulting in worsening the symptom of
shortness of breath (Elsherif & Noble, 2011).
The vital sign assessment of the patient was also done, as the vital signs are
considered to be important for the baseline observation. Airway assessment of the
patient informed that he has irreversible and permanent obstruction in the airway. He
looked alert; however, he was little distressed and was experiencing breathlessness
on rest and exertion (O'Donnell et al, 2016). Respiratory rate, pulse rate,
temperature and blood pressure readings of the patient were taken in order to
understand his respiratory function and for the identification of any kind of the
predicators that could inform about the deterioration or improvement in patient’s
condition. Delroy’s respiratory rate was 29 breaths per minute and his breathing was
shallow. Delroy was using his accessory muscles for breathing. The severity of the
exacerbation was assessed through measuring the arterial blood gases and pulse
oximetry (SpO2)
Therefore, the assessment of the patient including the patient’s medical and social
history informs that symptoms are associated with the presence of COPD. History of
smoking is significantly associated with occurrence of the disease that is affecting
the life and well-being of the patient. However, the patient has improved and problem
of breathlessness is controlled. However, According to Roper-Logan-Tierney Model,
the main problems that has been identified in the case of Delroy, which can affect
him after the discharge are:
Breathing
Eating and Drinking
Maintaining a Safe Environment
Psychological Impact of Symptoms
Medical history of Delroy has informed about the presences of depression. Studies
have identified that COPD can significantly affect the individual’s quality of life. A
study conducted by Pumar et al (2014) has identified that the symptom of
breathlessness can have the significant impact of the patient’s well-being and also
on the daily activities. The severity of the symptoms has also been associated with
the increasing risk of psychological co-morbidities. Anxiety and depression have
shortness of breath (Elsherif & Noble, 2011).
The vital sign assessment of the patient was also done, as the vital signs are
considered to be important for the baseline observation. Airway assessment of the
patient informed that he has irreversible and permanent obstruction in the airway. He
looked alert; however, he was little distressed and was experiencing breathlessness
on rest and exertion (O'Donnell et al, 2016). Respiratory rate, pulse rate,
temperature and blood pressure readings of the patient were taken in order to
understand his respiratory function and for the identification of any kind of the
predicators that could inform about the deterioration or improvement in patient’s
condition. Delroy’s respiratory rate was 29 breaths per minute and his breathing was
shallow. Delroy was using his accessory muscles for breathing. The severity of the
exacerbation was assessed through measuring the arterial blood gases and pulse
oximetry (SpO2)
Therefore, the assessment of the patient including the patient’s medical and social
history informs that symptoms are associated with the presence of COPD. History of
smoking is significantly associated with occurrence of the disease that is affecting
the life and well-being of the patient. However, the patient has improved and problem
of breathlessness is controlled. However, According to Roper-Logan-Tierney Model,
the main problems that has been identified in the case of Delroy, which can affect
him after the discharge are:
Breathing
Eating and Drinking
Maintaining a Safe Environment
Psychological Impact of Symptoms
Medical history of Delroy has informed about the presences of depression. Studies
have identified that COPD can significantly affect the individual’s quality of life. A
study conducted by Pumar et al (2014) has identified that the symptom of
breathlessness can have the significant impact of the patient’s well-being and also
on the daily activities. The severity of the symptoms has also been associated with
the increasing risk of psychological co-morbidities. Anxiety and depression have
been identified as the major psychological co-morbidities associated with the
patients suffering from COPD (Schneider et al, 2010). The problem of
breathlessness significantly affects the patient’s decision making, coping skills and
help-seeking behaviour. The problem of depression among the patients suffering
with COPD is also associated with depression, as the rate of smoking is higher
among the depressed patients.
Another reason of the high prevalence of depression among COPD patient is
‘overspill’ of the local lung inflammation and the systematic inflammation increases
discomfort resulting in depression (Yohannes, & Alexopoulos, 2014). Studies have
informed that although, depression could occur as the reason of smoking and
inflammation in the airway, but the severity of the symptom can significantly increase
prevalence of depression in COPD patients (Yohannes, & Alexopoulos, 2014).
Severity of the symptoms results in causing functional limitations to the patient and
restricting their ability to conduct activities of daily life. Secondly the increasing
severity of symptom like breathlessness can also require the higher level of
instrumental support, lack of which can result in increasing depressive symptoms
(Yohannes, & Alexopoulos, 2014). The cognitive behavioural theory has also
explained the cognitive functioning of the patient is significantly affected by their
physical functioning and the problem in appropriate physical functions can lead to
increasing cognitive and mental health problems (Mi et al, 2017).
It has also been identified that frightening experience of breathlessness can
significantly affect the patients physical and mental health condition. Therefore,
“NHS Right Care Pathway: COPD” is an important policy that encourage the use of
social support to overcome such psychological problem (NHS England, 2018). The
policy also identified that multidisciplinary support and care can help in reducing
such psychological problems among COPD patients (NHS England, 2018).
Another psychological impact of the worsening symptoms is social isolation. Social
isolation is mainly the result of stigma related to COPD. Psychological consequences
of the symptoms are such that they not only result in physical disability, but also
impact the behavioural and other social factors. Social isolation is also a significant
co-morbidity the impairs the quality of life and also reduces the adherence to the
treatment (Yohannes & Alexopoulos, 2014). Social isolation is also caused due to
patients suffering from COPD (Schneider et al, 2010). The problem of
breathlessness significantly affects the patient’s decision making, coping skills and
help-seeking behaviour. The problem of depression among the patients suffering
with COPD is also associated with depression, as the rate of smoking is higher
among the depressed patients.
Another reason of the high prevalence of depression among COPD patient is
‘overspill’ of the local lung inflammation and the systematic inflammation increases
discomfort resulting in depression (Yohannes, & Alexopoulos, 2014). Studies have
informed that although, depression could occur as the reason of smoking and
inflammation in the airway, but the severity of the symptom can significantly increase
prevalence of depression in COPD patients (Yohannes, & Alexopoulos, 2014).
Severity of the symptoms results in causing functional limitations to the patient and
restricting their ability to conduct activities of daily life. Secondly the increasing
severity of symptom like breathlessness can also require the higher level of
instrumental support, lack of which can result in increasing depressive symptoms
(Yohannes, & Alexopoulos, 2014). The cognitive behavioural theory has also
explained the cognitive functioning of the patient is significantly affected by their
physical functioning and the problem in appropriate physical functions can lead to
increasing cognitive and mental health problems (Mi et al, 2017).
It has also been identified that frightening experience of breathlessness can
significantly affect the patients physical and mental health condition. Therefore,
“NHS Right Care Pathway: COPD” is an important policy that encourage the use of
social support to overcome such psychological problem (NHS England, 2018). The
policy also identified that multidisciplinary support and care can help in reducing
such psychological problems among COPD patients (NHS England, 2018).
Another psychological impact of the worsening symptoms is social isolation. Social
isolation is mainly the result of stigma related to COPD. Psychological consequences
of the symptoms are such that they not only result in physical disability, but also
impact the behavioural and other social factors. Social isolation is also a significant
co-morbidity the impairs the quality of life and also reduces the adherence to the
treatment (Yohannes & Alexopoulos, 2014). Social isolation is also caused due to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
limited mobility, as the physical activity and mobility becomes difficult for the patient
suffering with COPD (Pinnock et al, 2011).
Study conducted by Lenferink, van der Palen, & Effing (2018) identified that social
well-being of the individual is significant for the quality of life. However, social
cognitive theory informs that lack of perceived social support and emotional coping
skills result in increasing the problem of social isolation. People suffering from COPD
often withdraw themselves from their social circles and isolate themselves due to the
stigma of suffering from chronic disorder. This withdrawal results in affecting the
psychological and emotional coping skills and lose social relationships (Lenferink,
van der Palen, & Effing, 2018). Studies have identified that social support and social
relationships are significant for reducing anxiety and distress, improving coping skills
and also for promoting self-care skills (Effing et al, 2016). Social isolation is the main
problem due to which Delroy has stopped going out and spend hours on social
media platforms and on gambling sites.
Another problem identified in the case of Delroy is that he suffers from malnutrition,
which is an important symptom of COPD and can result in many co-morbidities
(Corsonello et al, 2011). Malnutrition being an important symptom and significant
problem for the COPD patients, it is often overlooked during the management plan
(Joo et al, 2012). A significant finding was done by Mete et al (2018), which is that
COPD not only impacts the physical health of the individual, but also affects the
mental and cognitive health and this co-morbidity can result in worsening the disease
symptoms and severity.
Care Plan/ Intervention
Inhaled Therapy
The first important therapy for Delroy to manage his problem of breathlessness is
through inhaled therapy. Nice (2019) informs that patient must be recommended to
use the short-acting bronchodilators (which may include Short-acting beta2 agonists
(SABA) and short-acting muscarinic antagonists (SAMA)). This will help in
addressing the initial problem of breathless ness and activity intolerance. The
second inhaled therapy that can be recommended to Delroy is the use of
corticosteroids (ICS). However, NICE (2019) recommend that oral corticosteroids
reversibility test should not be used, as such tests are not sufficient to predict the
suffering with COPD (Pinnock et al, 2011).
Study conducted by Lenferink, van der Palen, & Effing (2018) identified that social
well-being of the individual is significant for the quality of life. However, social
cognitive theory informs that lack of perceived social support and emotional coping
skills result in increasing the problem of social isolation. People suffering from COPD
often withdraw themselves from their social circles and isolate themselves due to the
stigma of suffering from chronic disorder. This withdrawal results in affecting the
psychological and emotional coping skills and lose social relationships (Lenferink,
van der Palen, & Effing, 2018). Studies have identified that social support and social
relationships are significant for reducing anxiety and distress, improving coping skills
and also for promoting self-care skills (Effing et al, 2016). Social isolation is the main
problem due to which Delroy has stopped going out and spend hours on social
media platforms and on gambling sites.
Another problem identified in the case of Delroy is that he suffers from malnutrition,
which is an important symptom of COPD and can result in many co-morbidities
(Corsonello et al, 2011). Malnutrition being an important symptom and significant
problem for the COPD patients, it is often overlooked during the management plan
(Joo et al, 2012). A significant finding was done by Mete et al (2018), which is that
COPD not only impacts the physical health of the individual, but also affects the
mental and cognitive health and this co-morbidity can result in worsening the disease
symptoms and severity.
Care Plan/ Intervention
Inhaled Therapy
The first important therapy for Delroy to manage his problem of breathlessness is
through inhaled therapy. Nice (2019) informs that patient must be recommended to
use the short-acting bronchodilators (which may include Short-acting beta2 agonists
(SABA) and short-acting muscarinic antagonists (SAMA)). This will help in
addressing the initial problem of breathless ness and activity intolerance. The
second inhaled therapy that can be recommended to Delroy is the use of
corticosteroids (ICS). However, NICE (2019) recommend that oral corticosteroids
reversibility test should not be used, as such tests are not sufficient to predict the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
response to this inhaled therapy. Secondly the limitations and side effects of the
corticosteroids therapy must be discussed with the patient and family members as
the inhaled corticosteroids can lead to the occurrence of pneumonia (NICE, 2018).
Another inhaled therapy is the combination therapy. This kind of therapy includes the
combination of long-acting beta2 agonists (LABA), long-acting muscarinic
antagonists (LAMA), and inhaled corticosteroids (ICS). It has also been
recommended that effectiveness of this kind of therapy and the bronchodilator
therapy should not be based alone on the patient’s lung function. It must include
different measures to analyse its effectiveness, such as the changes in the ability to
carry out activities of daily life, relief in symptoms, improved physical activity
tolerance and significant improvement in symptoms (NICE, 2019). Study conducted
by Chen et al 920170 has also identified that combination therapy including long-
acting beta2 agonists (LABA), plus long-acting muscarinic antagonists (LAMA) can
also be given to the patient who do not display asthmatic symptoms (as in the case
of Delroy). This combination therapy can also be given to the patient, who continue
to display the symptoms of breathlessness, who have been provided with the
tobacco dependence treatment (Chen et al, 2017). LAMA+LABA can also be given
to the patient who have received the appropriate non-pharmacological treatment and
vaccinations, and those who are using short-acting bronchodilator.
Studies have also recommended the use of long-acting beta2 agonists (LABA) plus
inhaled corticosteroids (ICS) to the patients who have spirometrically confirmed
COPD and having the asthmatic features that suggest responsiveness towards
steroids (Pirina et al, 2018). NICE (2019) LABA+ICS is also effective for the patients
having the exacerbations and breathlessness despite of the tobacco dependence
treatment, who have received the optimised non-pharmacological treatment and
those who have used short-acting bronchodilator. The patients who have been using
the long-acting bronchodilators before the NICE guideline published in the year
2018, can be informed that they can continue with their treatment till the time their
health professional consider the change. Therefore, the choice regarding the inhaler
or the drug use in the case of Delroy should be made on the basis of the patient’s
condition, his ability to use the inhaler, impact of the drug on reducing exacerbations.
However, for managing patient’s condition it is also important to keep the number of
inhalers as minimum as possible to keep the treatment easy and self-manageable
corticosteroids therapy must be discussed with the patient and family members as
the inhaled corticosteroids can lead to the occurrence of pneumonia (NICE, 2018).
Another inhaled therapy is the combination therapy. This kind of therapy includes the
combination of long-acting beta2 agonists (LABA), long-acting muscarinic
antagonists (LAMA), and inhaled corticosteroids (ICS). It has also been
recommended that effectiveness of this kind of therapy and the bronchodilator
therapy should not be based alone on the patient’s lung function. It must include
different measures to analyse its effectiveness, such as the changes in the ability to
carry out activities of daily life, relief in symptoms, improved physical activity
tolerance and significant improvement in symptoms (NICE, 2019). Study conducted
by Chen et al 920170 has also identified that combination therapy including long-
acting beta2 agonists (LABA), plus long-acting muscarinic antagonists (LAMA) can
also be given to the patient who do not display asthmatic symptoms (as in the case
of Delroy). This combination therapy can also be given to the patient, who continue
to display the symptoms of breathlessness, who have been provided with the
tobacco dependence treatment (Chen et al, 2017). LAMA+LABA can also be given
to the patient who have received the appropriate non-pharmacological treatment and
vaccinations, and those who are using short-acting bronchodilator.
Studies have also recommended the use of long-acting beta2 agonists (LABA) plus
inhaled corticosteroids (ICS) to the patients who have spirometrically confirmed
COPD and having the asthmatic features that suggest responsiveness towards
steroids (Pirina et al, 2018). NICE (2019) LABA+ICS is also effective for the patients
having the exacerbations and breathlessness despite of the tobacco dependence
treatment, who have received the optimised non-pharmacological treatment and
those who have used short-acting bronchodilator. The patients who have been using
the long-acting bronchodilators before the NICE guideline published in the year
2018, can be informed that they can continue with their treatment till the time their
health professional consider the change. Therefore, the choice regarding the inhaler
or the drug use in the case of Delroy should be made on the basis of the patient’s
condition, his ability to use the inhaler, impact of the drug on reducing exacerbations.
However, for managing patient’s condition it is also important to keep the number of
inhalers as minimum as possible to keep the treatment easy and self-manageable
and for reducing the cost (NICE, 2018). Before recommending inhaler to Delroy, it is
also important that he is provided with appropriate information and training to use the
inhaler for managing his condition and symptoms at home.
Educational Intervention
One of the most important intervention for improving the health and well-being of
Delroy is patient empowerment through education. Most of the people suffering with
COPD have little or no awareness about the severity and progression of the disease
(Liang, Abramson & George, 2017). Therefore, educational intervention is very
important for improving their health literacy, enhancing their understanding about the
underlying condition and encouraging self-care skills (Liang, Abramson & George,
2017). Educational intervention is also important for effective disease management.
Liang, Abramson & George (2017) also identified that COPD is a preventable and
treatable condition and one of the major reasons behind the occurrence of this
disease is cigarette smoking. The treatment guidelines for treating the patients of
COPD has significantly included education of patient as an important intervention.
Educational intervention focuses providing the evidence-based knowledge and skills
to the patients that can help them to cope with the adverse consequences of
symptoms (King et al, 2018). Continuous acquisition of the new knowledge skills and
attitude of the health professionals also helps in delivering the high-quality care and
sharing their knowledge through education intervention (Newham et al, 2017).
A study conducted by Han (2017), COPD patients face significantly difficulty in
coping with the worsening symptoms and carrying out the activities of daily life.
Patients also face various emotional challenges that make the coping process more
difficult. Patients also suffer from the uncertainty about the prognosis of the disease
and the treatment regimens that resulting increasing the symptoms of depression,
anxiety, social isolation and social stigmas. Such problems could be real or
perceived but they negatively affect the patient outcomes (Han, 2017). These are
also some significant problems that also affect the well-being of the family members
and caregivers. Therefore, the health professionals through education interventions
including the communication strategies focus on helping the patients and their
families in understanding the disease, its associated symptoms, risk factors, early
detection of deterioration and empowering patients to manage their condition (van
also important that he is provided with appropriate information and training to use the
inhaler for managing his condition and symptoms at home.
Educational Intervention
One of the most important intervention for improving the health and well-being of
Delroy is patient empowerment through education. Most of the people suffering with
COPD have little or no awareness about the severity and progression of the disease
(Liang, Abramson & George, 2017). Therefore, educational intervention is very
important for improving their health literacy, enhancing their understanding about the
underlying condition and encouraging self-care skills (Liang, Abramson & George,
2017). Educational intervention is also important for effective disease management.
Liang, Abramson & George (2017) also identified that COPD is a preventable and
treatable condition and one of the major reasons behind the occurrence of this
disease is cigarette smoking. The treatment guidelines for treating the patients of
COPD has significantly included education of patient as an important intervention.
Educational intervention focuses providing the evidence-based knowledge and skills
to the patients that can help them to cope with the adverse consequences of
symptoms (King et al, 2018). Continuous acquisition of the new knowledge skills and
attitude of the health professionals also helps in delivering the high-quality care and
sharing their knowledge through education intervention (Newham et al, 2017).
A study conducted by Han (2017), COPD patients face significantly difficulty in
coping with the worsening symptoms and carrying out the activities of daily life.
Patients also face various emotional challenges that make the coping process more
difficult. Patients also suffer from the uncertainty about the prognosis of the disease
and the treatment regimens that resulting increasing the symptoms of depression,
anxiety, social isolation and social stigmas. Such problems could be real or
perceived but they negatively affect the patient outcomes (Han, 2017). These are
also some significant problems that also affect the well-being of the family members
and caregivers. Therefore, the health professionals through education interventions
including the communication strategies focus on helping the patients and their
families in understanding the disease, its associated symptoms, risk factors, early
detection of deterioration and empowering patients to manage their condition (van
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





