Leroy's Mental Health Assessment: A Detailed USQ Case Study
VerifiedAdded on 2023/06/08
|17
|5524
|168
Case Study
AI Summary
This case study provides a mental state examination of an individual named Leroy, focusing on his general appearance, behavior, speech, mood, thought process, perception, cognition, insight, and judgment. The analysis reveals symptoms related to mental health disorders, including confusion, insomnia, and lack of focus. Interventions such as dementia management, melatonin use, physical activity encouragement, and socialization are suggested to improve Leroy's condition. The case also references the Mental Health Act 2016 and discusses substitute decision-making. Desklib provides this and other solved assignments for students.
University of Southern Queensland
Date: 04/07/2022 Time: 11:10
URN:
Family Name:
Given
Name(s): Leroy
Date of Birth:
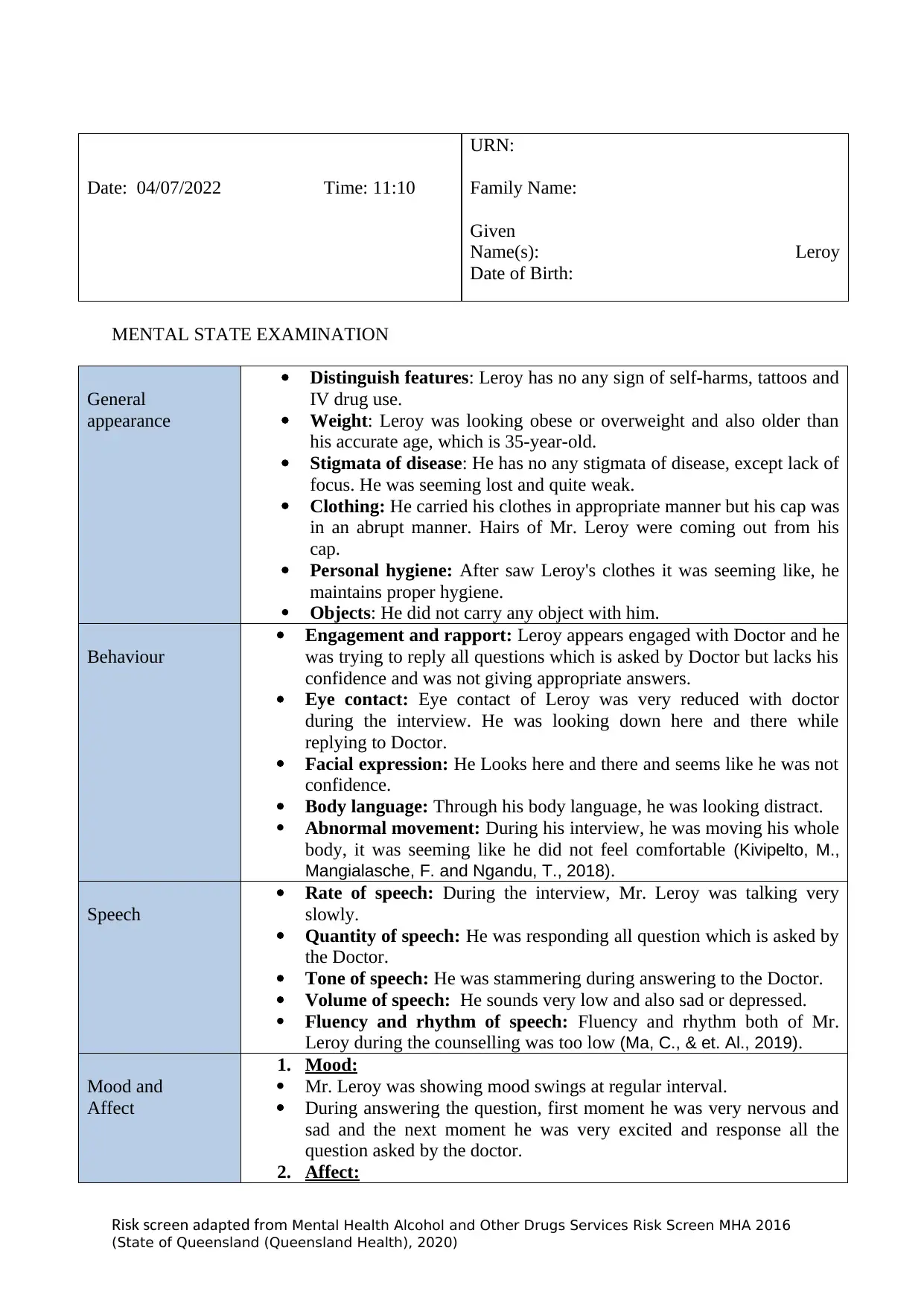
MENTAL STATE EXAMINATION
General
appearance
Distinguish features: Leroy has no any sign of self-harms, tattoos and
IV drug use.
Weight: Leroy was looking obese or overweight and also older than
his accurate age, which is 35-year-old.
Stigmata of disease: He has no any stigmata of disease, except lack of
focus. He was seeming lost and quite weak.
Clothing: He carried his clothes in appropriate manner but his cap was
in an abrupt manner. Hairs of Mr. Leroy were coming out from his
cap.
Personal hygiene: After saw Leroy's clothes it was seeming like, he
maintains proper hygiene.
Objects: He did not carry any object with him.
Behaviour
Engagement and rapport: Leroy appears engaged with Doctor and he
was trying to reply all questions which is asked by Doctor but lacks his
confidence and was not giving appropriate answers.
Eye contact: Eye contact of Leroy was very reduced with doctor
during the interview. He was looking down here and there while
replying to Doctor.
Facial expression: He Looks here and there and seems like he was not
confidence.
Body language: Through his body language, he was looking distract.
Abnormal movement: During his interview, he was moving his whole
body, it was seeming like he did not feel comfortable (Kivipelto, M.,
Mangialasche, F. and Ngandu, T., 2018).
Speech
Rate of speech: During the interview, Mr. Leroy was talking very
slowly.
Quantity of speech: He was responding all question which is asked by
the Doctor.
Tone of speech: He was stammering during answering to the Doctor.
Volume of speech: He sounds very low and also sad or depressed.
Fluency and rhythm of speech: Fluency and rhythm both of Mr.
Leroy during the counselling was too low (Ma, C., & et. Al., 2019).
Mood and
Affect
1. Mood:
Mr. Leroy was showing mood swings at regular interval.
During answering the question, first moment he was very nervous and
sad and the next moment he was very excited and response all the
question asked by the doctor.
2. Affect:
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Date: 04/07/2022 Time: 11:10
URN:
Family Name:
Given
Name(s): Leroy
Date of Birth:
MENTAL STATE EXAMINATION
General
appearance
Distinguish features: Leroy has no any sign of self-harms, tattoos and
IV drug use.
Weight: Leroy was looking obese or overweight and also older than
his accurate age, which is 35-year-old.
Stigmata of disease: He has no any stigmata of disease, except lack of
focus. He was seeming lost and quite weak.
Clothing: He carried his clothes in appropriate manner but his cap was
in an abrupt manner. Hairs of Mr. Leroy were coming out from his
cap.
Personal hygiene: After saw Leroy's clothes it was seeming like, he
maintains proper hygiene.
Objects: He did not carry any object with him.
Behaviour
Engagement and rapport: Leroy appears engaged with Doctor and he
was trying to reply all questions which is asked by Doctor but lacks his
confidence and was not giving appropriate answers.
Eye contact: Eye contact of Leroy was very reduced with doctor
during the interview. He was looking down here and there while
replying to Doctor.
Facial expression: He Looks here and there and seems like he was not
confidence.
Body language: Through his body language, he was looking distract.
Abnormal movement: During his interview, he was moving his whole
body, it was seeming like he did not feel comfortable (Kivipelto, M.,
Mangialasche, F. and Ngandu, T., 2018).
Speech
Rate of speech: During the interview, Mr. Leroy was talking very
slowly.
Quantity of speech: He was responding all question which is asked by
the Doctor.
Tone of speech: He was stammering during answering to the Doctor.
Volume of speech: He sounds very low and also sad or depressed.
Fluency and rhythm of speech: Fluency and rhythm both of Mr.
Leroy during the counselling was too low (Ma, C., & et. Al., 2019).
Mood and
Affect
1. Mood:
Mr. Leroy was showing mood swings at regular interval.
During answering the question, first moment he was very nervous and
sad and the next moment he was very excited and response all the
question asked by the doctor.
2. Affect:
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
University of Southern Queensland
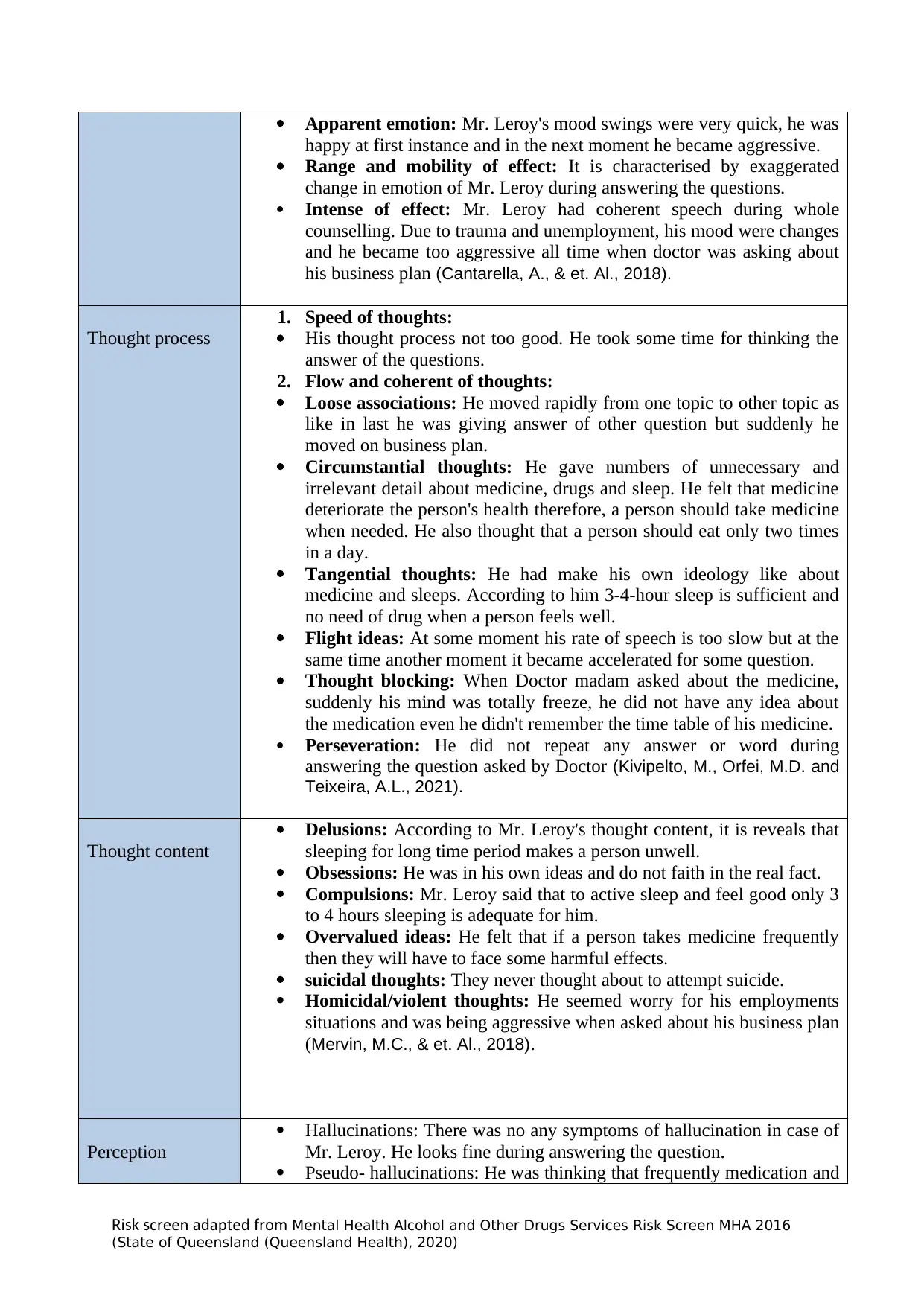
Apparent emotion: Mr. Leroy's mood swings were very quick, he was
happy at first instance and in the next moment he became aggressive.
Range and mobility of effect: It is characterised by exaggerated
change in emotion of Mr. Leroy during answering the questions.
Intense of effect: Mr. Leroy had coherent speech during whole
counselling. Due to trauma and unemployment, his mood were changes
and he became too aggressive all time when doctor was asking about
his business plan (Cantarella, A., & et. Al., 2018).
Thought process
1. Speed of thoughts:
His thought process not too good. He took some time for thinking the
answer of the questions.
2. Flow and coherent of thoughts:
Loose associations: He moved rapidly from one topic to other topic as
like in last he was giving answer of other question but suddenly he
moved on business plan.
Circumstantial thoughts: He gave numbers of unnecessary and
irrelevant detail about medicine, drugs and sleep. He felt that medicine
deteriorate the person's health therefore, a person should take medicine
when needed. He also thought that a person should eat only two times
in a day.
Tangential thoughts: He had make his own ideology like about
medicine and sleeps. According to him 3-4-hour sleep is sufficient and
no need of drug when a person feels well.
Flight ideas: At some moment his rate of speech is too slow but at the
same time another moment it became accelerated for some question.
Thought blocking: When Doctor madam asked about the medicine,
suddenly his mind was totally freeze, he did not have any idea about
the medication even he didn't remember the time table of his medicine.
Perseveration: He did not repeat any answer or word during
answering the question asked by Doctor (Kivipelto, M., Orfei, M.D. and
Teixeira, A.L., 2021).
Thought content
Delusions: According to Mr. Leroy's thought content, it is reveals that
sleeping for long time period makes a person unwell.
Obsessions: He was in his own ideas and do not faith in the real fact.
Compulsions: Mr. Leroy said that to active sleep and feel good only 3
to 4 hours sleeping is adequate for him.
Overvalued ideas: He felt that if a person takes medicine frequently
then they will have to face some harmful effects.
suicidal thoughts: They never thought about to attempt suicide.
Homicidal/violent thoughts: He seemed worry for his employments
situations and was being aggressive when asked about his business plan
(Mervin, M.C., & et. Al., 2018).
Perception
Hallucinations: There was no any symptoms of hallucination in case of
Mr. Leroy. He looks fine during answering the question.
Pseudo- hallucinations: He was thinking that frequently medication and
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Apparent emotion: Mr. Leroy's mood swings were very quick, he was
happy at first instance and in the next moment he became aggressive.
Range and mobility of effect: It is characterised by exaggerated
change in emotion of Mr. Leroy during answering the questions.
Intense of effect: Mr. Leroy had coherent speech during whole
counselling. Due to trauma and unemployment, his mood were changes
and he became too aggressive all time when doctor was asking about
his business plan (Cantarella, A., & et. Al., 2018).
Thought process
1. Speed of thoughts:
His thought process not too good. He took some time for thinking the
answer of the questions.
2. Flow and coherent of thoughts:
Loose associations: He moved rapidly from one topic to other topic as
like in last he was giving answer of other question but suddenly he
moved on business plan.
Circumstantial thoughts: He gave numbers of unnecessary and
irrelevant detail about medicine, drugs and sleep. He felt that medicine
deteriorate the person's health therefore, a person should take medicine
when needed. He also thought that a person should eat only two times
in a day.
Tangential thoughts: He had make his own ideology like about
medicine and sleeps. According to him 3-4-hour sleep is sufficient and
no need of drug when a person feels well.
Flight ideas: At some moment his rate of speech is too slow but at the
same time another moment it became accelerated for some question.
Thought blocking: When Doctor madam asked about the medicine,
suddenly his mind was totally freeze, he did not have any idea about
the medication even he didn't remember the time table of his medicine.
Perseveration: He did not repeat any answer or word during
answering the question asked by Doctor (Kivipelto, M., Orfei, M.D. and
Teixeira, A.L., 2021).
Thought content
Delusions: According to Mr. Leroy's thought content, it is reveals that
sleeping for long time period makes a person unwell.
Obsessions: He was in his own ideas and do not faith in the real fact.
Compulsions: Mr. Leroy said that to active sleep and feel good only 3
to 4 hours sleeping is adequate for him.
Overvalued ideas: He felt that if a person takes medicine frequently
then they will have to face some harmful effects.
suicidal thoughts: They never thought about to attempt suicide.
Homicidal/violent thoughts: He seemed worry for his employments
situations and was being aggressive when asked about his business plan
(Mervin, M.C., & et. Al., 2018).
Perception
Hallucinations: There was no any symptoms of hallucination in case of
Mr. Leroy. He looks fine during answering the question.
Pseudo- hallucinations: He was thinking that frequently medication and
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
University of Southern Queensland
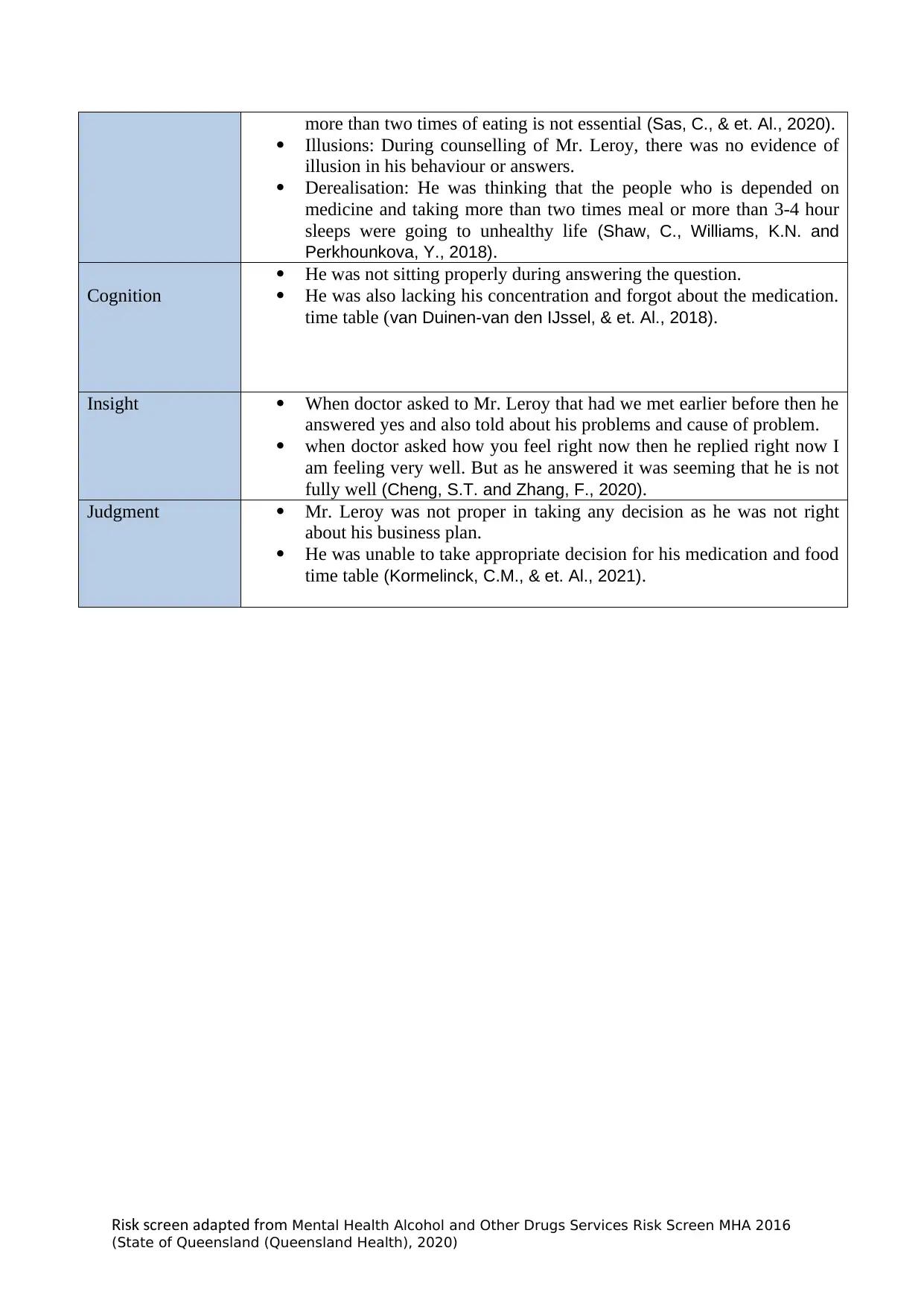
more than two times of eating is not essential (Sas, C., & et. Al., 2020).
Illusions: During counselling of Mr. Leroy, there was no evidence of
illusion in his behaviour or answers.
Derealisation: He was thinking that the people who is depended on
medicine and taking more than two times meal or more than 3-4 hour
sleeps were going to unhealthy life (Shaw, C., Williams, K.N. and
Perkhounkova, Y., 2018).
Cognition
He was not sitting properly during answering the question.
He was also lacking his concentration and forgot about the medication.
time table (van Duinen-van den IJssel, & et. Al., 2018).
Insight When doctor asked to Mr. Leroy that had we met earlier before then he
answered yes and also told about his problems and cause of problem.
when doctor asked how you feel right now then he replied right now I
am feeling very well. But as he answered it was seeming that he is not
fully well (Cheng, S.T. and Zhang, F., 2020).
Judgment Mr. Leroy was not proper in taking any decision as he was not right
about his business plan.
He was unable to take appropriate decision for his medication and food
time table (Kormelinck, C.M., & et. Al., 2021).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
more than two times of eating is not essential (Sas, C., & et. Al., 2020).
Illusions: During counselling of Mr. Leroy, there was no evidence of
illusion in his behaviour or answers.
Derealisation: He was thinking that the people who is depended on
medicine and taking more than two times meal or more than 3-4 hour
sleeps were going to unhealthy life (Shaw, C., Williams, K.N. and
Perkhounkova, Y., 2018).
Cognition
He was not sitting properly during answering the question.
He was also lacking his concentration and forgot about the medication.
time table (van Duinen-van den IJssel, & et. Al., 2018).
Insight When doctor asked to Mr. Leroy that had we met earlier before then he
answered yes and also told about his problems and cause of problem.
when doctor asked how you feel right now then he replied right now I
am feeling very well. But as he answered it was seeming that he is not
fully well (Cheng, S.T. and Zhang, F., 2020).
Judgment Mr. Leroy was not proper in taking any decision as he was not right
about his business plan.
He was unable to take appropriate decision for his medication and food
time table (Kormelinck, C.M., & et. Al., 2021).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
University of Southern Queensland
SYMPTOM INTERVENTIONS
1.
Dementia: Confusion
As per the analysis of interview, Leroy is usually show their symptom
which is related with mental health disorder and many more. With this
symptoms, the two intervention is used to applied that help Leroy to
recover the situation and manage the excess of confusion. The
intervention is:
Offer correction and suggestion: It is usually show the context that help
to provide the correction to the activities or event that is misunderstood
by Leroy where the appropriate suggestion may quantify that help to
eradicate confusion which is persist during mental health issue.
Respond with brief explanation: It is also an aspect when the people with
the dementia or any mental patient used to face the issue of confusion
then the patient must be taking under consideration and appropriate
response with brief explanation is used to outline that help Leroy for the
retaliation of confusion which act as symptom and such response usually
show the presence of intervention for the mental health patient.
Whereas, the melatonin is help to maintain the sleep and improve
process of sleep cycle and provide reliable approach that carry the
proper reduction in sun downing in people in people with dementia. In
addition, provide the proper light. The bright light therapy in the term of
evening can lessen that sleep wake cycle disturbance in the people
which is analysed with the dementia. Adequate lighting at the night which
can minimise agitation that can be happen when the surrounding is dark
(Russell-Williams, & et. Al., 2018).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
SYMPTOM INTERVENTIONS
1.
Dementia: Confusion
As per the analysis of interview, Leroy is usually show their symptom
which is related with mental health disorder and many more. With this
symptoms, the two intervention is used to applied that help Leroy to
recover the situation and manage the excess of confusion. The
intervention is:
Offer correction and suggestion: It is usually show the context that help
to provide the correction to the activities or event that is misunderstood
by Leroy where the appropriate suggestion may quantify that help to
eradicate confusion which is persist during mental health issue.
Respond with brief explanation: It is also an aspect when the people with
the dementia or any mental patient used to face the issue of confusion
then the patient must be taking under consideration and appropriate
response with brief explanation is used to outline that help Leroy for the
retaliation of confusion which act as symptom and such response usually
show the presence of intervention for the mental health patient.
Whereas, the melatonin is help to maintain the sleep and improve
process of sleep cycle and provide reliable approach that carry the
proper reduction in sun downing in people in people with dementia. In
addition, provide the proper light. The bright light therapy in the term of
evening can lessen that sleep wake cycle disturbance in the people
which is analysed with the dementia. Adequate lighting at the night which
can minimise agitation that can be happen when the surrounding is dark
(Russell-Williams, & et. Al., 2018).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
University of Southern Queensland
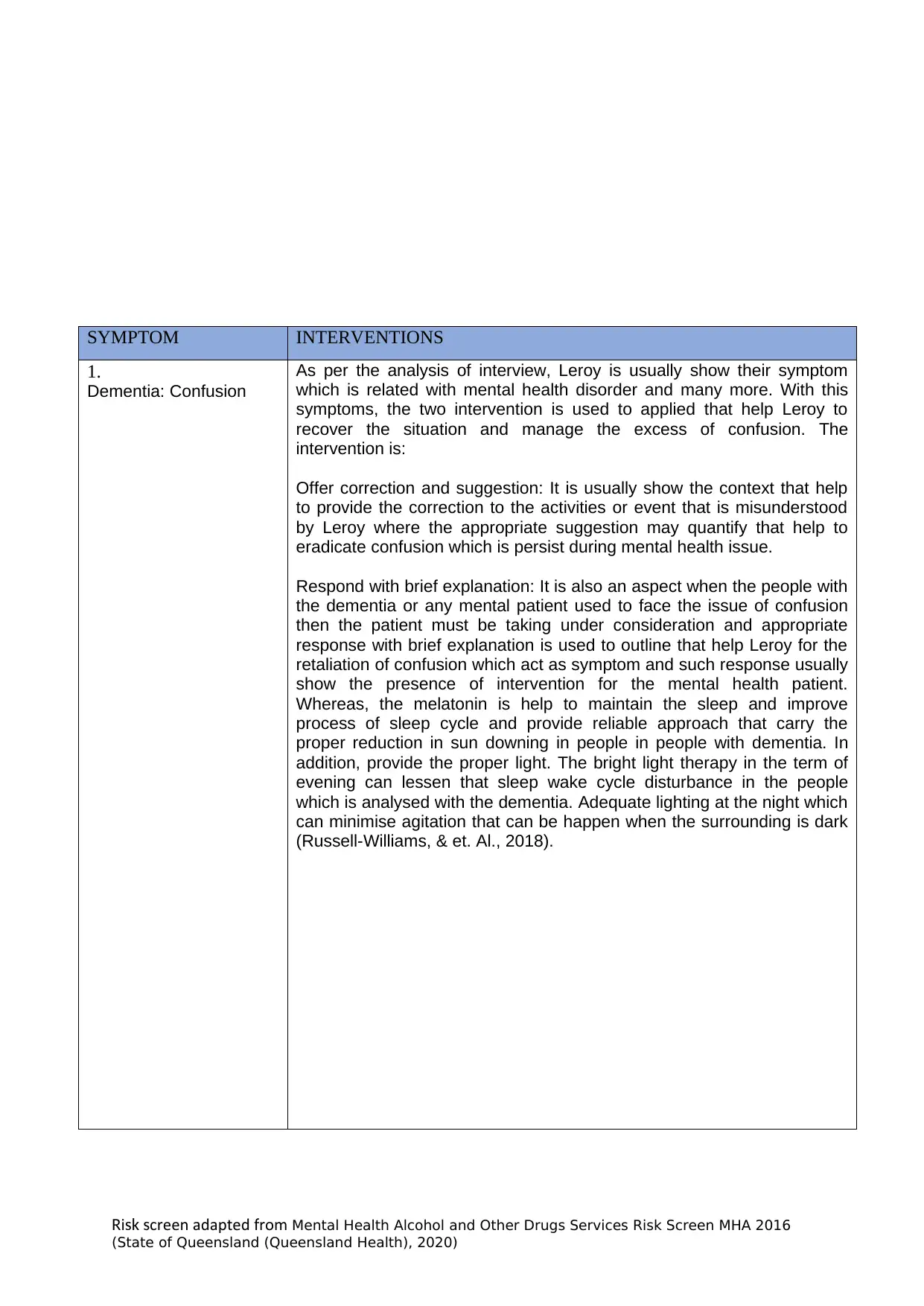
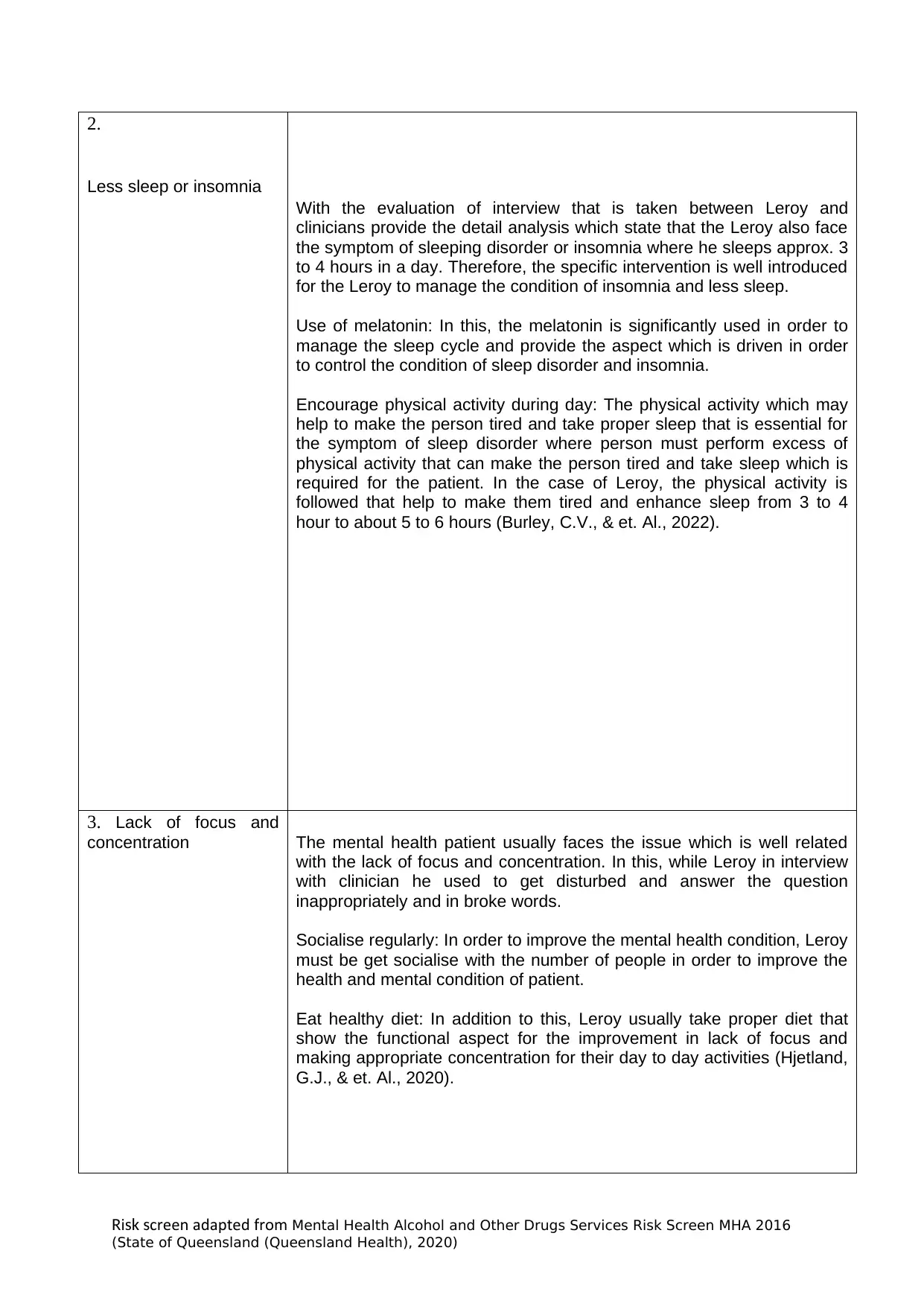
2.
Less sleep or insomnia
With the evaluation of interview that is taken between Leroy and
clinicians provide the detail analysis which state that the Leroy also face
the symptom of sleeping disorder or insomnia where he sleeps approx. 3
to 4 hours in a day. Therefore, the specific intervention is well introduced
for the Leroy to manage the condition of insomnia and less sleep.
Use of melatonin: In this, the melatonin is significantly used in order to
manage the sleep cycle and provide the aspect which is driven in order
to control the condition of sleep disorder and insomnia.
Encourage physical activity during day: The physical activity which may
help to make the person tired and take proper sleep that is essential for
the symptom of sleep disorder where person must perform excess of
physical activity that can make the person tired and take sleep which is
required for the patient. In the case of Leroy, the physical activity is
followed that help to make them tired and enhance sleep from 3 to 4
hour to about 5 to 6 hours (Burley, C.V., & et. Al., 2022).
3. Lack of focus and
concentration The mental health patient usually faces the issue which is well related
with the lack of focus and concentration. In this, while Leroy in interview
with clinician he used to get disturbed and answer the question
inappropriately and in broke words.
Socialise regularly: In order to improve the mental health condition, Leroy
must be get socialise with the number of people in order to improve the
health and mental condition of patient.
Eat healthy diet: In addition to this, Leroy usually take proper diet that
show the functional aspect for the improvement in lack of focus and
making appropriate concentration for their day to day activities (Hjetland,
G.J., & et. Al., 2020).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
2.
Less sleep or insomnia
With the evaluation of interview that is taken between Leroy and
clinicians provide the detail analysis which state that the Leroy also face
the symptom of sleeping disorder or insomnia where he sleeps approx. 3
to 4 hours in a day. Therefore, the specific intervention is well introduced
for the Leroy to manage the condition of insomnia and less sleep.
Use of melatonin: In this, the melatonin is significantly used in order to
manage the sleep cycle and provide the aspect which is driven in order
to control the condition of sleep disorder and insomnia.
Encourage physical activity during day: The physical activity which may
help to make the person tired and take proper sleep that is essential for
the symptom of sleep disorder where person must perform excess of
physical activity that can make the person tired and take sleep which is
required for the patient. In the case of Leroy, the physical activity is
followed that help to make them tired and enhance sleep from 3 to 4
hour to about 5 to 6 hours (Burley, C.V., & et. Al., 2022).
3. Lack of focus and
concentration The mental health patient usually faces the issue which is well related
with the lack of focus and concentration. In this, while Leroy in interview
with clinician he used to get disturbed and answer the question
inappropriately and in broke words.
Socialise regularly: In order to improve the mental health condition, Leroy
must be get socialise with the number of people in order to improve the
health and mental condition of patient.
Eat healthy diet: In addition to this, Leroy usually take proper diet that
show the functional aspect for the improvement in lack of focus and
making appropriate concentration for their day to day activities (Hjetland,
G.J., & et. Al., 2020).
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
University of Southern Queensland
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ...........................................................................
............................
URN: .................................................................
....................................
Family
name: .................................................................
..................
Given
name(s): ............................................................
....................
Address: ............................................................
..................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
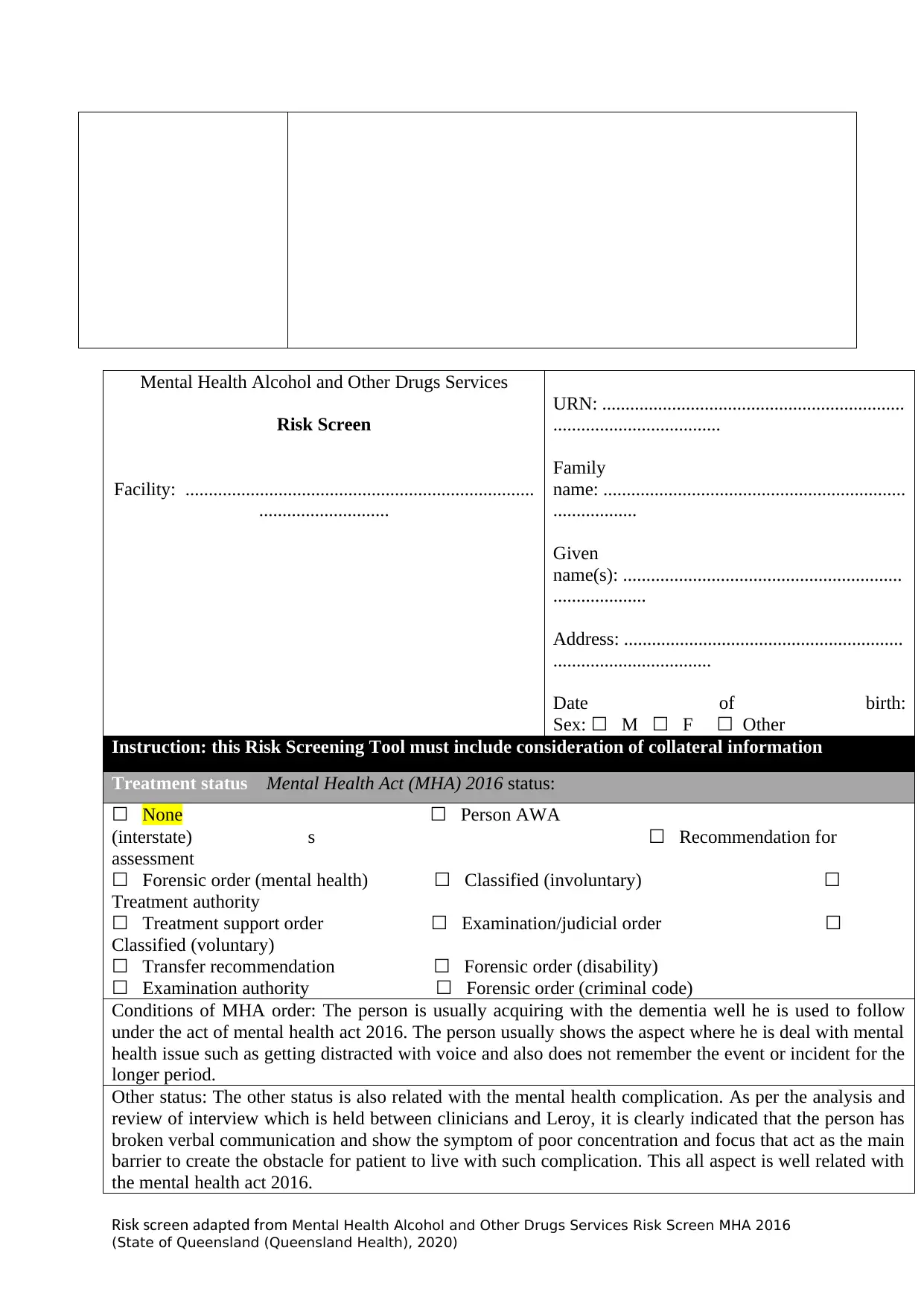
Treatment status Mental Health Act (MHA) 2016 status:
☐ None ☐ Person AWA
(interstate)s☐ Recommendation for
assessment
☐ Forensic order (mental health) ☐ Classified (involuntary) ☐
Treatment authority
☐ Treatment support order ☐ Examination/judicial order ☐
Classified (voluntary)
☐ Transfer recommendation ☐ Forensic order (disability)
☐ Examination authority ☐ Forensic order (criminal code)
Conditions of MHA order: The person is usually acquiring with the dementia well he is used to follow
under the act of mental health act 2016. The person usually shows the aspect where he is deal with mental
health issue such as getting distracted with voice and also does not remember the event or incident for the
longer period.
Other status: The other status is also related with the mental health complication. As per the analysis and
review of interview which is held between clinicians and Leroy, it is clearly indicated that the person has
broken verbal communication and show the symptom of poor concentration and focus that act as the main
barrier to create the obstacle for patient to live with such complication. This all aspect is well related with
the mental health act 2016.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ...........................................................................
............................
URN: .................................................................
....................................
Family
name: .................................................................
..................
Given
name(s): ............................................................
....................
Address: ............................................................
..................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
Treatment status Mental Health Act (MHA) 2016 status:
☐ None ☐ Person AWA
(interstate)s☐ Recommendation for
assessment
☐ Forensic order (mental health) ☐ Classified (involuntary) ☐
Treatment authority
☐ Treatment support order ☐ Examination/judicial order ☐
Classified (voluntary)
☐ Transfer recommendation ☐ Forensic order (disability)
☐ Examination authority ☐ Forensic order (criminal code)
Conditions of MHA order: The person is usually acquiring with the dementia well he is used to follow
under the act of mental health act 2016. The person usually shows the aspect where he is deal with mental
health issue such as getting distracted with voice and also does not remember the event or incident for the
longer period.
Other status: The other status is also related with the mental health complication. As per the analysis and
review of interview which is held between clinicians and Leroy, it is clearly indicated that the person has
broken verbal communication and show the symptom of poor concentration and focus that act as the main
barrier to create the obstacle for patient to live with such complication. This all aspect is well related with
the mental health act 2016.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
University of Southern Queensland
Substitute Decision-Maker Details
Substitute decision-maker: ☐ Yes ☐ No
Advance Health Directive☐ Enduring Power of Attorney☐ Guardian☐
Administrator☐
Y = yes N = no UK = unknown
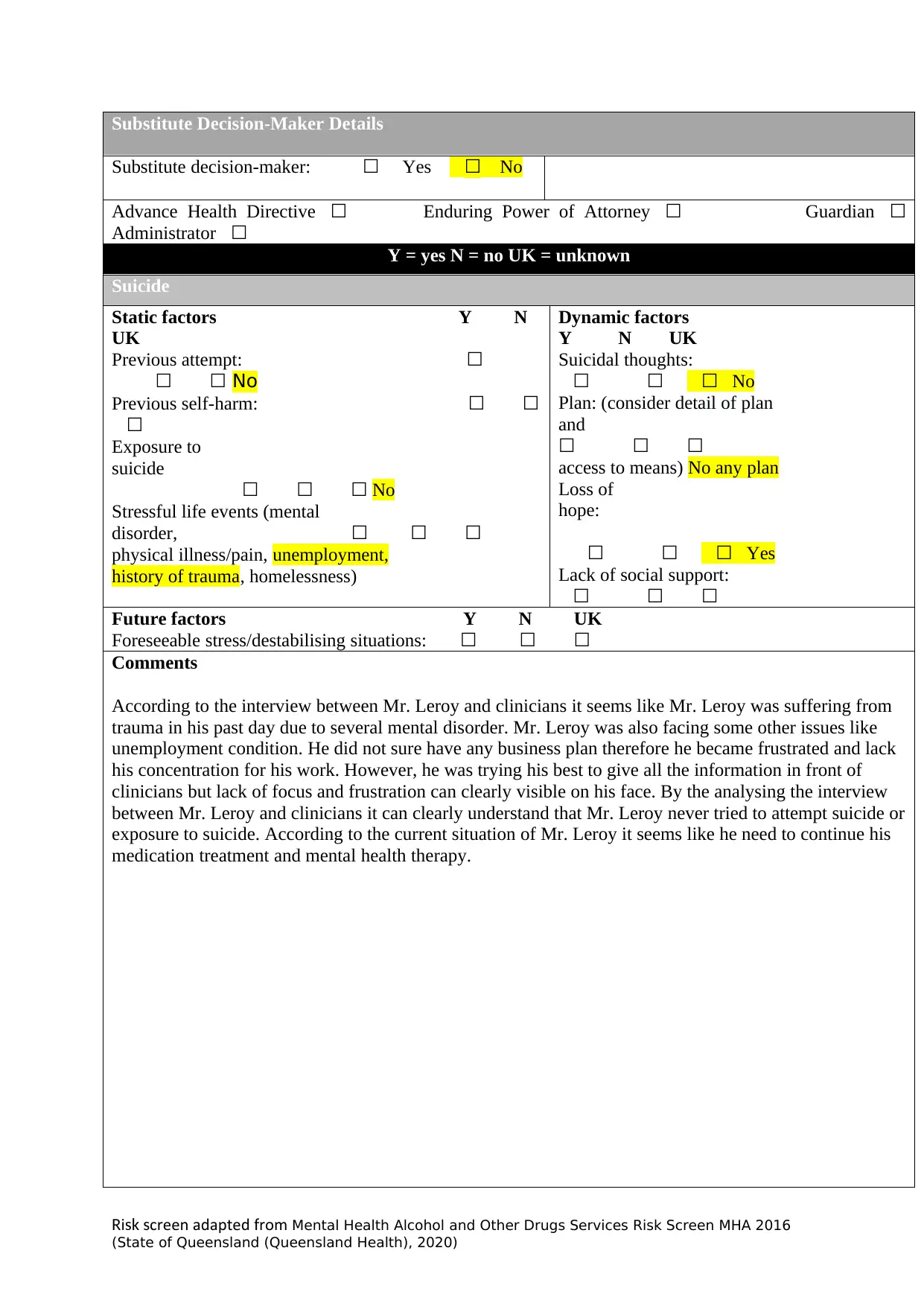
Suicide
Static factors Y N
UK
Previous attempt: ☐
☐ ☐ No
Previous self-harm: ☐ ☐
☐
Exposure to
suicide
☐ ☐ ☐ No
Stressful life events (mental
disorder,☐ ☐ ☐
physical illness/pain, unemployment,
history of trauma, homelessness)
Dynamic factors
Y N UK
Suicidal thoughts:
☐ ☐ ☐ No
Plan: (consider detail of plan
and
☐ ☐ ☐
access to means) No any plan
Loss of
hope:
☐ ☐ ☐ Yes
Lack of social support:
☐ ☐ ☐
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Comments
According to the interview between Mr. Leroy and clinicians it seems like Mr. Leroy was suffering from
trauma in his past day due to several mental disorder. Mr. Leroy was also facing some other issues like
unemployment condition. He did not sure have any business plan therefore he became frustrated and lack
his concentration for his work. However, he was trying his best to give all the information in front of
clinicians but lack of focus and frustration can clearly visible on his face. By the analysing the interview
between Mr. Leroy and clinicians it can clearly understand that Mr. Leroy never tried to attempt suicide or
exposure to suicide. According to the current situation of Mr. Leroy it seems like he need to continue his
medication treatment and mental health therapy.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Substitute Decision-Maker Details
Substitute decision-maker: ☐ Yes ☐ No
Advance Health Directive☐ Enduring Power of Attorney☐ Guardian☐
Administrator☐
Y = yes N = no UK = unknown
Suicide
Static factors Y N
UK
Previous attempt: ☐
☐ ☐ No
Previous self-harm: ☐ ☐
☐
Exposure to
suicide
☐ ☐ ☐ No
Stressful life events (mental
disorder,☐ ☐ ☐
physical illness/pain, unemployment,
history of trauma, homelessness)
Dynamic factors
Y N UK
Suicidal thoughts:
☐ ☐ ☐ No
Plan: (consider detail of plan
and
☐ ☐ ☐
access to means) No any plan
Loss of
hope:
☐ ☐ ☐ Yes
Lack of social support:
☐ ☐ ☐
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Comments
According to the interview between Mr. Leroy and clinicians it seems like Mr. Leroy was suffering from
trauma in his past day due to several mental disorder. Mr. Leroy was also facing some other issues like
unemployment condition. He did not sure have any business plan therefore he became frustrated and lack
his concentration for his work. However, he was trying his best to give all the information in front of
clinicians but lack of focus and frustration can clearly visible on his face. By the analysing the interview
between Mr. Leroy and clinicians it can clearly understand that Mr. Leroy never tried to attempt suicide or
exposure to suicide. According to the current situation of Mr. Leroy it seems like he need to continue his
medication treatment and mental health therapy.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
University of Southern Queensland
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
.........................
URN: ................................................................
.....................................
Family
name: ...............................................................
....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
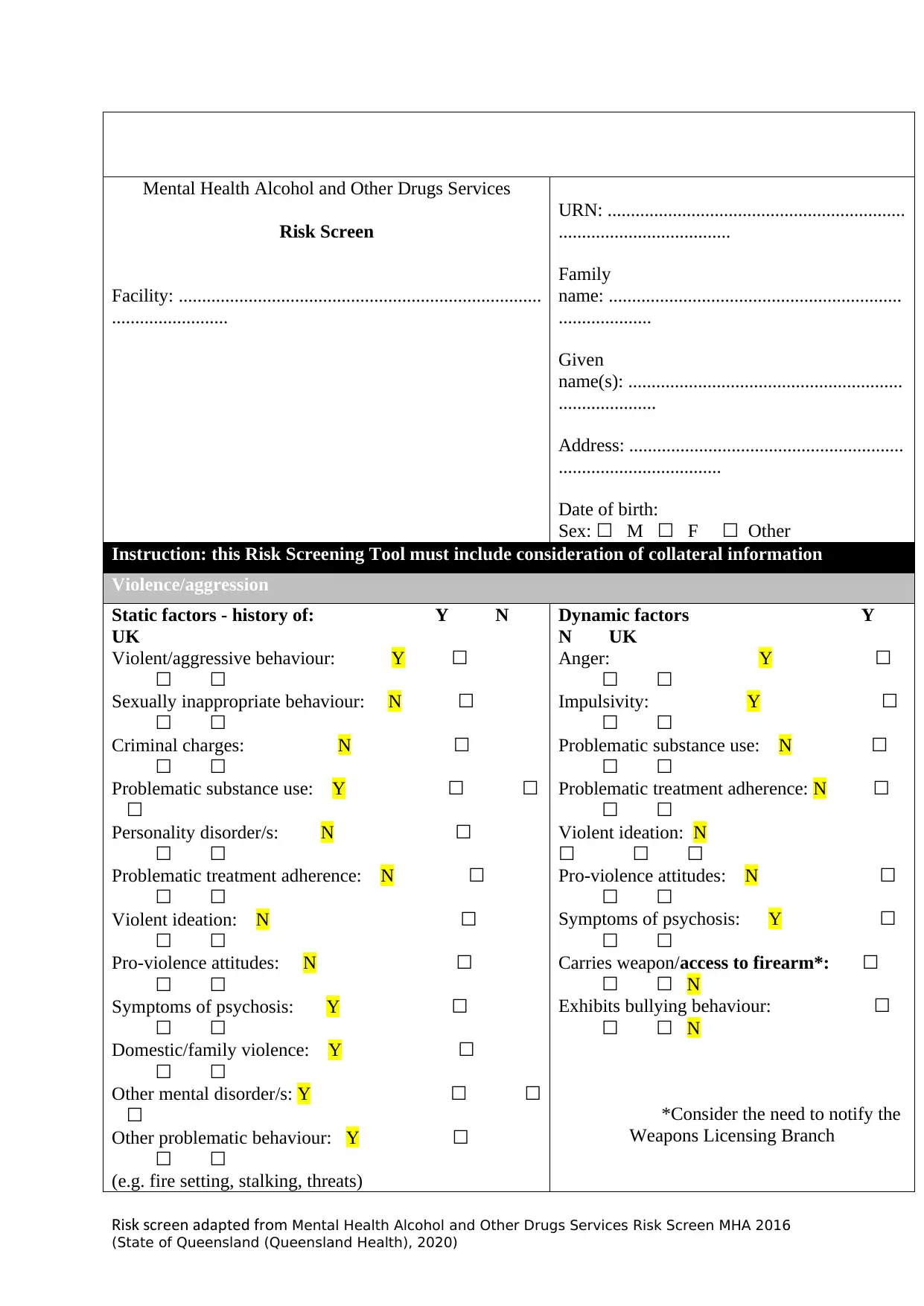
Violence/aggression
Static factors - history of: Y N
UK
Violent/aggressive behaviour: Y ☐
☐ ☐
Sexually inappropriate behaviour: N ☐
☐ ☐
Criminal charges: N ☐
☐ ☐
Problematic substance use: Y ☐ ☐
☐
Personality disorder/s: N ☐
☐ ☐
Problematic treatment adherence: N ☐
☐ ☐
Violent ideation: N ☐
☐ ☐
Pro-violence attitudes: N ☐
☐ ☐
Symptoms of psychosis: Y ☐
☐ ☐
Domestic/family violence: Y ☐
☐ ☐
Other mental disorder/s: Y ☐ ☐
☐
Other problematic behaviour: Y ☐
☐ ☐
(e.g. fire setting, stalking, threats)
Dynamic factors Y
N UK
Anger: Y ☐
☐ ☐
Impulsivity: Y ☐
☐ ☐
Problematic substance use: N ☐
☐ ☐
Problematic treatment adherence: N ☐
☐ ☐
Violent ideation: N
☐ ☐ ☐
Pro-violence attitudes: N ☐
☐ ☐
Symptoms of psychosis: Y ☐
☐ ☐
Carries weapon/access to firearm*: ☐
☐ ☐ N
Exhibits bullying behaviour: ☐
☐ ☐ N
*Consider the need to notify the
Weapons Licensing Branch
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
.........................
URN: ................................................................
.....................................
Family
name: ...............................................................
....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
Violence/aggression
Static factors - history of: Y N
UK
Violent/aggressive behaviour: Y ☐
☐ ☐
Sexually inappropriate behaviour: N ☐
☐ ☐
Criminal charges: N ☐
☐ ☐
Problematic substance use: Y ☐ ☐
☐
Personality disorder/s: N ☐
☐ ☐
Problematic treatment adherence: N ☐
☐ ☐
Violent ideation: N ☐
☐ ☐
Pro-violence attitudes: N ☐
☐ ☐
Symptoms of psychosis: Y ☐
☐ ☐
Domestic/family violence: Y ☐
☐ ☐
Other mental disorder/s: Y ☐ ☐
☐
Other problematic behaviour: Y ☐
☐ ☐
(e.g. fire setting, stalking, threats)
Dynamic factors Y
N UK
Anger: Y ☐
☐ ☐
Impulsivity: Y ☐
☐ ☐
Problematic substance use: N ☐
☐ ☐
Problematic treatment adherence: N ☐
☐ ☐
Violent ideation: N
☐ ☐ ☐
Pro-violence attitudes: N ☐
☐ ☐
Symptoms of psychosis: Y ☐
☐ ☐
Carries weapon/access to firearm*: ☐
☐ ☐ N
Exhibits bullying behaviour: ☐
☐ ☐ N
*Consider the need to notify the
Weapons Licensing Branch
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
University of Southern Queensland
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
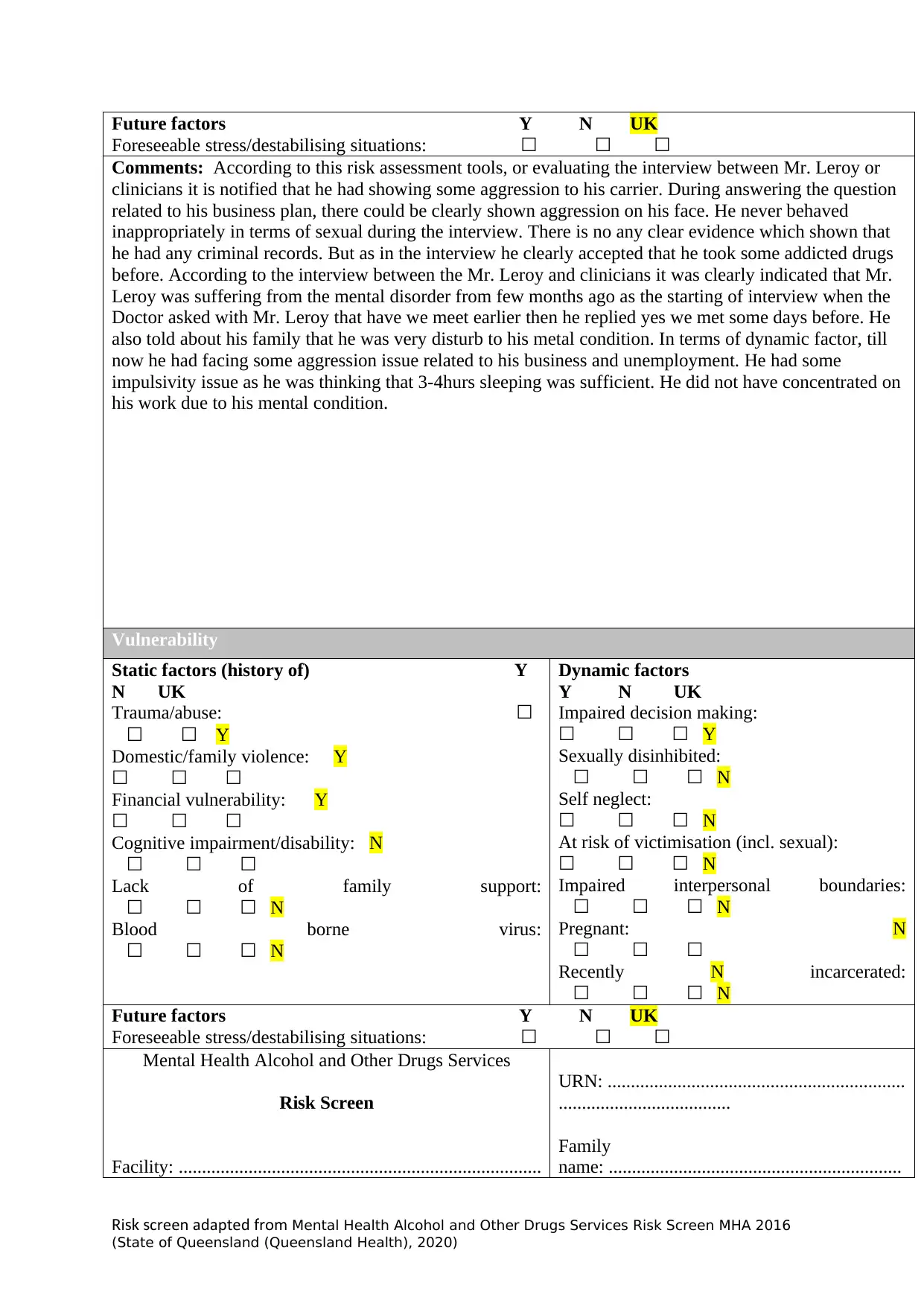
Comments: According to this risk assessment tools, or evaluating the interview between Mr. Leroy or
clinicians it is notified that he had showing some aggression to his carrier. During answering the question
related to his business plan, there could be clearly shown aggression on his face. He never behaved
inappropriately in terms of sexual during the interview. There is no any clear evidence which shown that
he had any criminal records. But as in the interview he clearly accepted that he took some addicted drugs
before. According to the interview between the Mr. Leroy and clinicians it was clearly indicated that Mr.
Leroy was suffering from the mental disorder from few months ago as the starting of interview when the
Doctor asked with Mr. Leroy that have we meet earlier then he replied yes we met some days before. He
also told about his family that he was very disturb to his metal condition. In terms of dynamic factor, till
now he had facing some aggression issue related to his business and unemployment. He had some
impulsivity issue as he was thinking that 3-4hurs sleeping was sufficient. He did not have concentrated on
his work due to his mental condition.
ACCORDING TO THIS RISK ASSESSMENT TOOLS
Vulnerability
Static factors (history of) Y
N UK
Trauma/abuse: ☐
☐ ☐ Y
Domestic/family violence: Y
☐ ☐ ☐
Financial vulnerability: Y
☐ ☐ ☐
Cognitive impairment/disability: N
☐ ☐ ☐
Lack of family support:
☐ ☐ ☐ N
Blood borne virus:
☐ ☐ ☐ N
Dynamic factors
Y N UK
Impaired decision making:
☐ ☐ ☐ Y
Sexually disinhibited:
☐ ☐ ☐ N
Self neglect:
☐ ☐ ☐ N
At risk of victimisation (incl. sexual):
☐ ☐ ☐ N
Impaired interpersonal boundaries:
☐ ☐ ☐ N
Pregnant: N
☐ ☐ ☐
Recently N incarcerated:
☐ ☐ ☐ N
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
URN: ................................................................
.....................................
Family
name: ...............................................................
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Comments: According to this risk assessment tools, or evaluating the interview between Mr. Leroy or
clinicians it is notified that he had showing some aggression to his carrier. During answering the question
related to his business plan, there could be clearly shown aggression on his face. He never behaved
inappropriately in terms of sexual during the interview. There is no any clear evidence which shown that
he had any criminal records. But as in the interview he clearly accepted that he took some addicted drugs
before. According to the interview between the Mr. Leroy and clinicians it was clearly indicated that Mr.
Leroy was suffering from the mental disorder from few months ago as the starting of interview when the
Doctor asked with Mr. Leroy that have we meet earlier then he replied yes we met some days before. He
also told about his family that he was very disturb to his metal condition. In terms of dynamic factor, till
now he had facing some aggression issue related to his business and unemployment. He had some
impulsivity issue as he was thinking that 3-4hurs sleeping was sufficient. He did not have concentrated on
his work due to his mental condition.
ACCORDING TO THIS RISK ASSESSMENT TOOLS
Vulnerability
Static factors (history of) Y
N UK
Trauma/abuse: ☐
☐ ☐ Y
Domestic/family violence: Y
☐ ☐ ☐
Financial vulnerability: Y
☐ ☐ ☐
Cognitive impairment/disability: N
☐ ☐ ☐
Lack of family support:
☐ ☐ ☐ N
Blood borne virus:
☐ ☐ ☐ N
Dynamic factors
Y N UK
Impaired decision making:
☐ ☐ ☐ Y
Sexually disinhibited:
☐ ☐ ☐ N
Self neglect:
☐ ☐ ☐ N
At risk of victimisation (incl. sexual):
☐ ☐ ☐ N
Impaired interpersonal boundaries:
☐ ☐ ☐ N
Pregnant: N
☐ ☐ ☐
Recently N incarcerated:
☐ ☐ ☐ N
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
URN: ................................................................
.....................................
Family
name: ...............................................................
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
University of Southern Queensland
......................... ....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
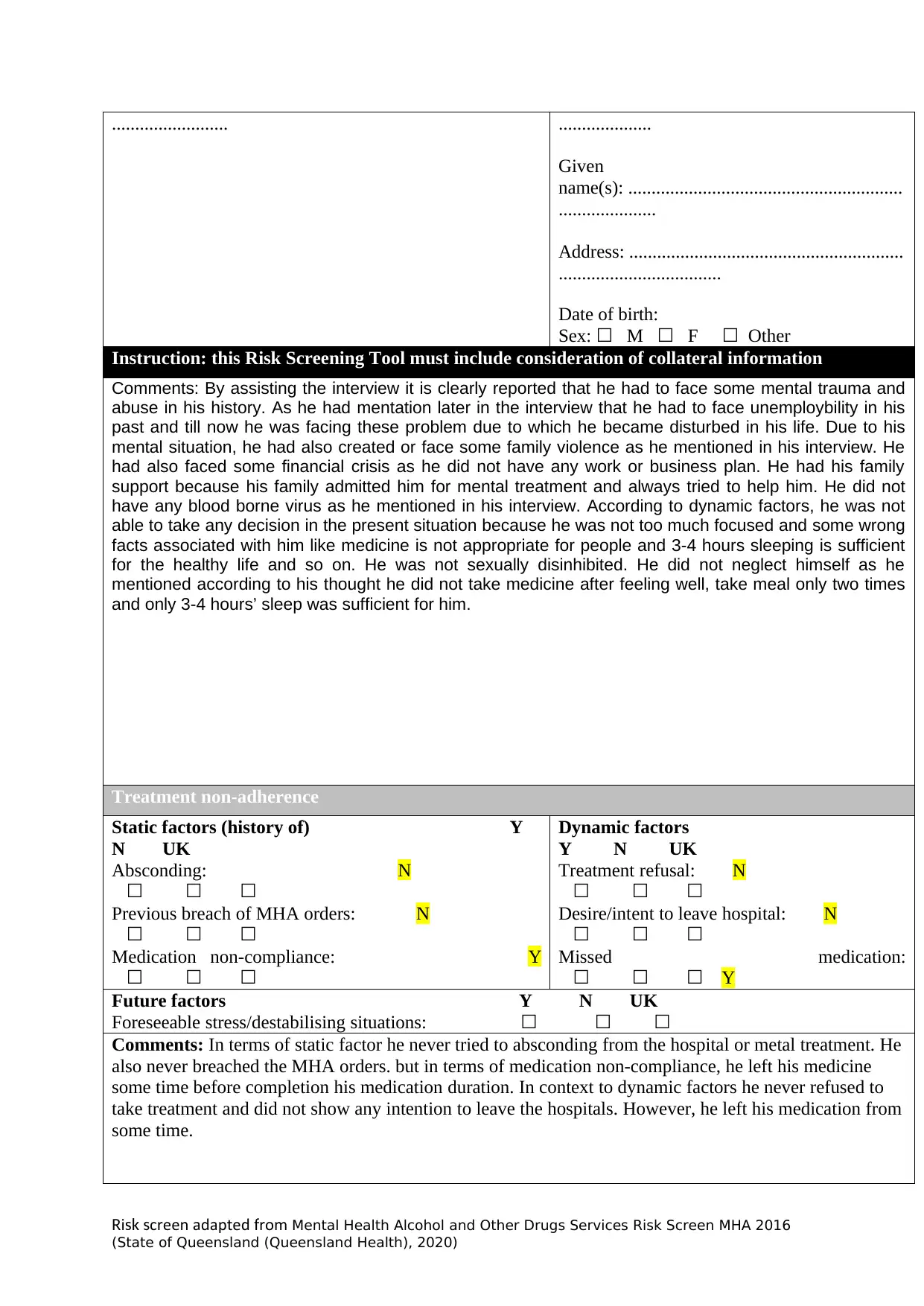
Comments: By assisting the interview it is clearly reported that he had to face some mental trauma and
abuse in his history. As he had mentation later in the interview that he had to face unemploybility in his
past and till now he was facing these problem due to which he became disturbed in his life. Due to his
mental situation, he had also created or face some family violence as he mentioned in his interview. He
had also faced some financial crisis as he did not have any work or business plan. He had his family
support because his family admitted him for mental treatment and always tried to help him. He did not
have any blood borne virus as he mentioned in his interview. According to dynamic factors, he was not
able to take any decision in the present situation because he was not too much focused and some wrong
facts associated with him like medicine is not appropriate for people and 3-4 hours sleeping is sufficient
for the healthy life and so on. He was not sexually disinhibited. He did not neglect himself as he
mentioned according to his thought he did not take medicine after feeling well, take meal only two times
and only 3-4 hours’ sleep was sufficient for him.
Treatment non-adherence
Static factors (history of) Y
N UK
Absconding: N
☐ ☐ ☐
Previous breach of MHA orders: N
☐ ☐ ☐
Medication non-compliance: Y
☐ ☐ ☐
Dynamic factors
Y N UK
Treatment refusal: N
☐ ☐ ☐
Desire/intent to leave hospital: N
☐ ☐ ☐
Missed medication:
☐ ☐ ☐ Y
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Comments: In terms of static factor he never tried to absconding from the hospital or metal treatment. He
also never breached the MHA orders. but in terms of medication non-compliance, he left his medicine
some time before completion his medication duration. In context to dynamic factors he never refused to
take treatment and did not show any intention to leave the hospitals. However, he left his medication from
some time.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
......................... ....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
Comments: By assisting the interview it is clearly reported that he had to face some mental trauma and
abuse in his history. As he had mentation later in the interview that he had to face unemploybility in his
past and till now he was facing these problem due to which he became disturbed in his life. Due to his
mental situation, he had also created or face some family violence as he mentioned in his interview. He
had also faced some financial crisis as he did not have any work or business plan. He had his family
support because his family admitted him for mental treatment and always tried to help him. He did not
have any blood borne virus as he mentioned in his interview. According to dynamic factors, he was not
able to take any decision in the present situation because he was not too much focused and some wrong
facts associated with him like medicine is not appropriate for people and 3-4 hours sleeping is sufficient
for the healthy life and so on. He was not sexually disinhibited. He did not neglect himself as he
mentioned according to his thought he did not take medicine after feeling well, take meal only two times
and only 3-4 hours’ sleep was sufficient for him.
Treatment non-adherence
Static factors (history of) Y
N UK
Absconding: N
☐ ☐ ☐
Previous breach of MHA orders: N
☐ ☐ ☐
Medication non-compliance: Y
☐ ☐ ☐
Dynamic factors
Y N UK
Treatment refusal: N
☐ ☐ ☐
Desire/intent to leave hospital: N
☐ ☐ ☐
Missed medication:
☐ ☐ ☐ Y
Future factors Y N UK
Foreseeable stress/destabilising situations: ☐ ☐ ☐
Comments: In terms of static factor he never tried to absconding from the hospital or metal treatment. He
also never breached the MHA orders. but in terms of medication non-compliance, he left his medicine
some time before completion his medication duration. In context to dynamic factors he never refused to
take treatment and did not show any intention to leave the hospitals. However, he left his medication from
some time.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
University of Southern Queensland
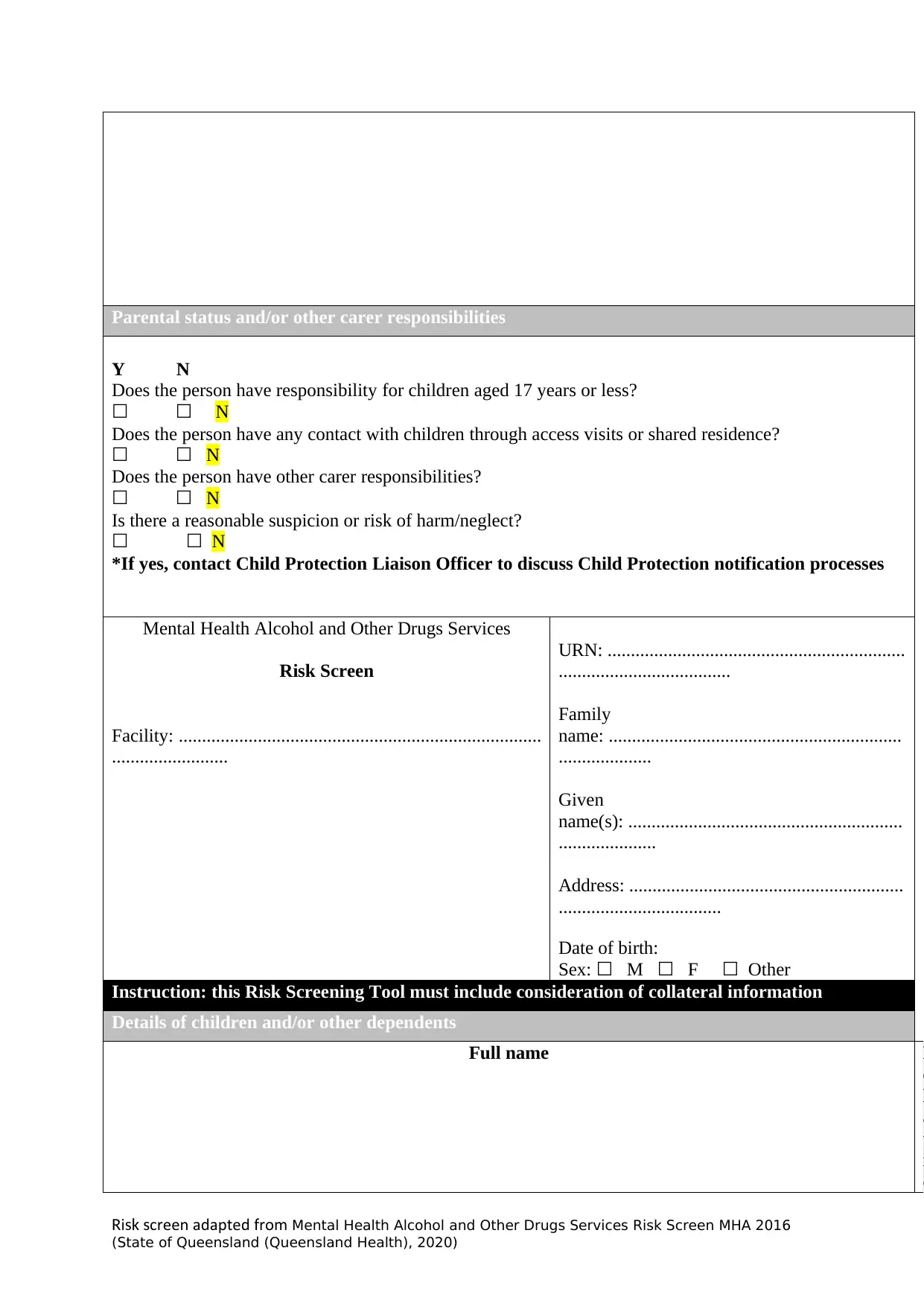
Parental status and/or other carer responsibilities
Y N
Does the person have responsibility for children aged 17 years or less?
☐ ☐ N
Does the person have any contact with children through access visits or shared residence?
☐ ☐ N
Does the person have other carer responsibilities?
☐ ☐ N
Is there a reasonable suspicion or risk of harm/neglect?
☐ ☐ N
*If yes, contact Child Protection Liaison Officer to discuss Child Protection notification processes d
support persons
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
.........................
URN: ................................................................
.....................................
Family
name: ...............................................................
....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
Details of children and/or other dependents
Full name R
e
l
a
t
i
o
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
Parental status and/or other carer responsibilities
Y N
Does the person have responsibility for children aged 17 years or less?
☐ ☐ N
Does the person have any contact with children through access visits or shared residence?
☐ ☐ N
Does the person have other carer responsibilities?
☐ ☐ N
Is there a reasonable suspicion or risk of harm/neglect?
☐ ☐ N
*If yes, contact Child Protection Liaison Officer to discuss Child Protection notification processes d
support persons
Mental Health Alcohol and Other Drugs Services
Risk Screen
Facility: ..............................................................................
.........................
URN: ................................................................
.....................................
Family
name: ...............................................................
....................
Given
name(s): ...........................................................
.....................
Address: ...........................................................
...................................
Date of birth:
Sex: ☐ M ☐ F ☐ Other
Instruction: this Risk Screening Tool must include consideration of collateral information
Details of children and/or other dependents
Full name R
e
l
a
t
i
o
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
University of Southern Queensland
n
s
h
i
p
Protective factors
By analysing the case of Mr. Leroy it is concluded that he should take their medicine till the competition
of medication course. he should also try to take some concentration making exercise and try to take
treatment in appropriate manner until he does not becomes fully well.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
n
s
h
i
p
Protective factors
By analysing the case of Mr. Leroy it is concluded that he should take their medicine till the competition
of medication course. he should also try to take some concentration making exercise and try to take
treatment in appropriate manner until he does not becomes fully well.
i creen adapted romR sk s f Mental Health Alcohol and Other Drugs Services Risk Screen MHA 2016
(State of Queensland (Queensland Health), 2020)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





