NUR245 Older Persons & Ageing: Comprehensive Case Study Solution
VerifiedAdded on 2023/06/11
|15
|5002
|380
Case Study
AI Summary
This document presents a solution to a case study assignment, NUR245, focusing on older persons and ageing. It includes two case studies: one about Anthony, a 79-year-old widower with multiple health issues who experiences delirium, and another about Esther, a 67-year-old ex-smoker with respiratory problems. The solutions address questions related to assessment tools like 4AT and MOCA, nursing interventions, patient safety and human rights, SMART goals, and the roles of a multidisciplinary team in managing the patients' conditions. The assignment emphasizes person-centered care and the dignity of risk.
Student Name: _________________ Student ID:__________________
EXAMINATIONS FOR DEGREES AND DIPLOMAS
April 2022
NUR245 Older Persons and Ageing
Case Study Assessment
Instructions:
Choose two case studies and answer the questions
associated with each of these case studies.
Each case study has five (5) questions with an allocation of 20 %
for each case study.
This assessment is worth a total of 40 marks
All submitted assessments must be wholly the student’s own work and in their own words’ (no
copying of text directly from textbooks, course readings or the internet)
1
EXAMINATIONS FOR DEGREES AND DIPLOMAS
April 2022
NUR245 Older Persons and Ageing
Case Study Assessment
Instructions:
Choose two case studies and answer the questions
associated with each of these case studies.
Each case study has five (5) questions with an allocation of 20 %
for each case study.
This assessment is worth a total of 40 marks
All submitted assessments must be wholly the student’s own work and in their own words’ (no
copying of text directly from textbooks, course readings or the internet)
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Student Name: _________________ Student ID:__________________
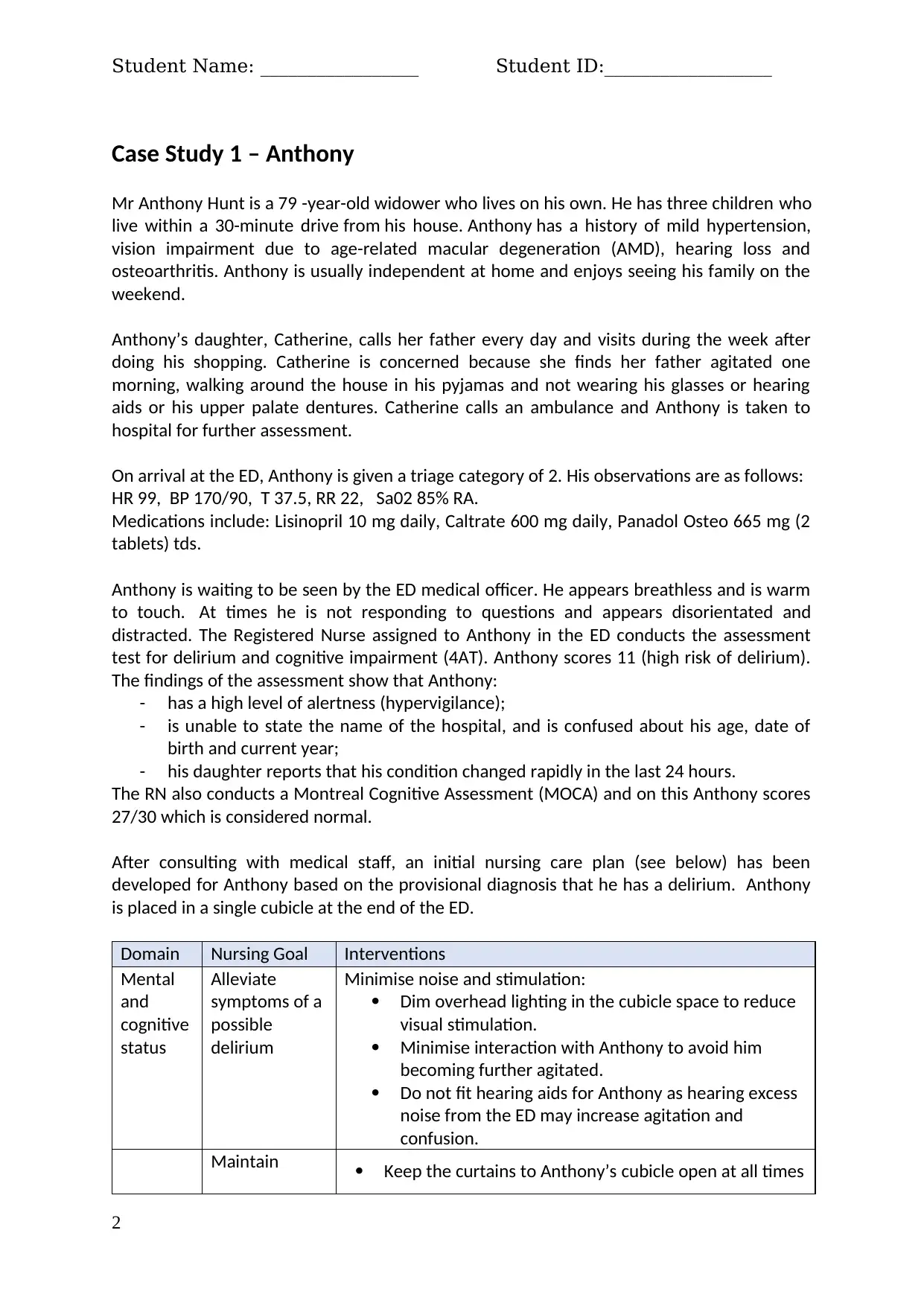
Case Study 1 – Anthony
Mr Anthony Hunt is a 79 -year-old widower who lives on his own. He has three children who
live within a 30-minute drive from his house. Anthony has a history of mild hypertension,
vision impairment due to age-related macular degeneration (AMD), hearing loss and
osteoarthritis. Anthony is usually independent at home and enjoys seeing his family on the
weekend.
Anthony’s daughter, Catherine, calls her father every day and visits during the week after
doing his shopping. Catherine is concerned because she finds her father agitated one
morning, walking around the house in his pyjamas and not wearing his glasses or hearing
aids or his upper palate dentures. Catherine calls an ambulance and Anthony is taken to
hospital for further assessment.
On arrival at the ED, Anthony is given a triage category of 2. His observations are as follows:
HR 99, BP 170/90, T 37.5, RR 22, Sa02 85% RA.
Medications include: Lisinopril 10 mg daily, Caltrate 600 mg daily, Panadol Osteo 665 mg (2
tablets) tds.
Anthony is waiting to be seen by the ED medical officer. He appears breathless and is warm
to touch. At times he is not responding to questions and appears disorientated and
distracted. The Registered Nurse assigned to Anthony in the ED conducts the assessment
test for delirium and cognitive impairment (4AT). Anthony scores 11 (high risk of delirium).
The findings of the assessment show that Anthony:
- has a high level of alertness (hypervigilance);
- is unable to state the name of the hospital, and is confused about his age, date of
birth and current year;
- his daughter reports that his condition changed rapidly in the last 24 hours.
The RN also conducts a Montreal Cognitive Assessment (MOCA) and on this Anthony scores
27/30 which is considered normal.
After consulting with medical staff, an initial nursing care plan (see below) has been
developed for Anthony based on the provisional diagnosis that he has a delirium. Anthony
is placed in a single cubicle at the end of the ED.
Domain Nursing Goal Interventions
Mental
and
cognitive
status
Alleviate
symptoms of a
possible
delirium
Minimise noise and stimulation:
Dim overhead lighting in the cubicle space to reduce
visual stimulation.
Minimise interaction with Anthony to avoid him
becoming further agitated.
Do not fit hearing aids for Anthony as hearing excess
noise from the ED may increase agitation and
confusion.
Maintain Keep the curtains to Anthony’s cubicle open at all times
2
Case Study 1 – Anthony
Mr Anthony Hunt is a 79 -year-old widower who lives on his own. He has three children who
live within a 30-minute drive from his house. Anthony has a history of mild hypertension,
vision impairment due to age-related macular degeneration (AMD), hearing loss and
osteoarthritis. Anthony is usually independent at home and enjoys seeing his family on the
weekend.
Anthony’s daughter, Catherine, calls her father every day and visits during the week after
doing his shopping. Catherine is concerned because she finds her father agitated one
morning, walking around the house in his pyjamas and not wearing his glasses or hearing
aids or his upper palate dentures. Catherine calls an ambulance and Anthony is taken to
hospital for further assessment.
On arrival at the ED, Anthony is given a triage category of 2. His observations are as follows:
HR 99, BP 170/90, T 37.5, RR 22, Sa02 85% RA.
Medications include: Lisinopril 10 mg daily, Caltrate 600 mg daily, Panadol Osteo 665 mg (2
tablets) tds.
Anthony is waiting to be seen by the ED medical officer. He appears breathless and is warm
to touch. At times he is not responding to questions and appears disorientated and
distracted. The Registered Nurse assigned to Anthony in the ED conducts the assessment
test for delirium and cognitive impairment (4AT). Anthony scores 11 (high risk of delirium).
The findings of the assessment show that Anthony:
- has a high level of alertness (hypervigilance);
- is unable to state the name of the hospital, and is confused about his age, date of
birth and current year;
- his daughter reports that his condition changed rapidly in the last 24 hours.
The RN also conducts a Montreal Cognitive Assessment (MOCA) and on this Anthony scores
27/30 which is considered normal.
After consulting with medical staff, an initial nursing care plan (see below) has been
developed for Anthony based on the provisional diagnosis that he has a delirium. Anthony
is placed in a single cubicle at the end of the ED.
Domain Nursing Goal Interventions
Mental
and
cognitive
status
Alleviate
symptoms of a
possible
delirium
Minimise noise and stimulation:
Dim overhead lighting in the cubicle space to reduce
visual stimulation.
Minimise interaction with Anthony to avoid him
becoming further agitated.
Do not fit hearing aids for Anthony as hearing excess
noise from the ED may increase agitation and
confusion.
Maintain Keep the curtains to Anthony’s cubicle open at all times
2
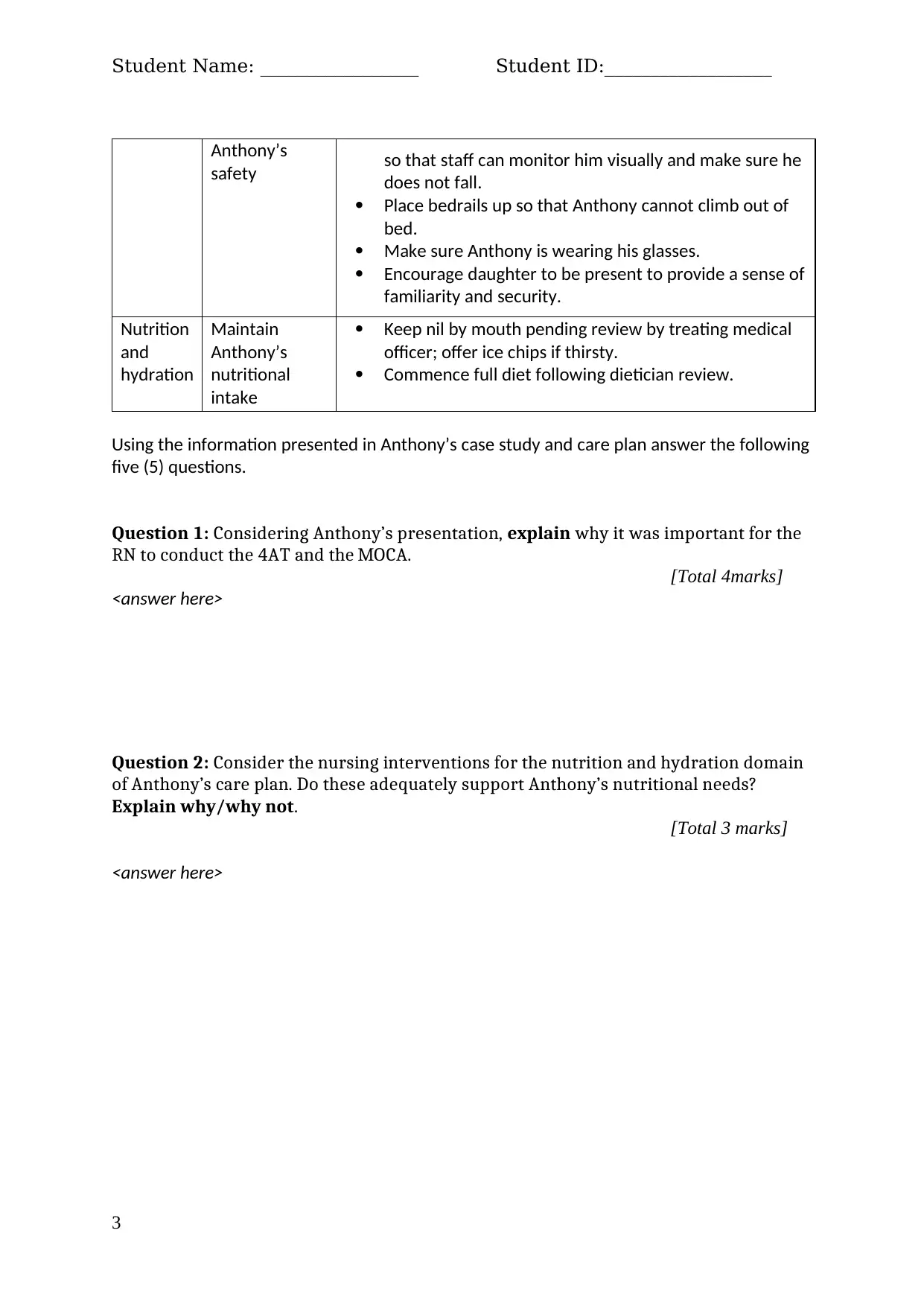
Student Name: _________________ Student ID:__________________
Anthony’s
safety so that staff can monitor him visually and make sure he
does not fall.
Place bedrails up so that Anthony cannot climb out of
bed.
Make sure Anthony is wearing his glasses.
Encourage daughter to be present to provide a sense of
familiarity and security.
Nutrition
and
hydration
Maintain
Anthony’s
nutritional
intake
Keep nil by mouth pending review by treating medical
officer; offer ice chips if thirsty.
Commence full diet following dietician review.
Using the information presented in Anthony’s case study and care plan answer the following
five (5) questions.
Question 1: Considering Anthony’s presentation, explain why it was important for the
RN to conduct the 4AT and the MOCA.
[Total 4marks]
<answer here>
Question 2: Consider the nursing interventions for the nutrition and hydration domain
of Anthony’s care plan. Do these adequately support Anthony’s nutritional needs?
Explain why/why not.
[Total 3 marks]
<answer here>
3
Anthony’s
safety so that staff can monitor him visually and make sure he
does not fall.
Place bedrails up so that Anthony cannot climb out of
bed.
Make sure Anthony is wearing his glasses.
Encourage daughter to be present to provide a sense of
familiarity and security.
Nutrition
and
hydration
Maintain
Anthony’s
nutritional
intake
Keep nil by mouth pending review by treating medical
officer; offer ice chips if thirsty.
Commence full diet following dietician review.
Using the information presented in Anthony’s case study and care plan answer the following
five (5) questions.
Question 1: Considering Anthony’s presentation, explain why it was important for the
RN to conduct the 4AT and the MOCA.
[Total 4marks]
<answer here>
Question 2: Consider the nursing interventions for the nutrition and hydration domain
of Anthony’s care plan. Do these adequately support Anthony’s nutritional needs?
Explain why/why not.
[Total 3 marks]
<answer here>
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Student Name: _________________ Student ID:__________________
Question 3: Evaluate the Interventions that are documented to maintain Anthony’s safety.
Identify one (1) intervention that does not protect Anthony’s Human rights and provide an
alternative person-centred intervention. To answer this question, fill in the below table.
[Total 4marks]
Which intervention
does not protect
Anthony’s Human
rights (1 mark)?
Which Human right is not
protected and why (1
mark)
Provide an alternative intervention
and justification (2 marks)
<insert answer here> <answer here> <answer here>
Question 4: Consider the nursing interventions for the mental and cognitive status domain
of Neville’s care plan and evaluate whether these interventions are appropriate to alleviate
symptoms of Anthony’s delirium. Explain why/why not. (2 marks each).
[Total 6 marks]
<answer here>
Question 5: What key information should the nurse be providing to Anthony’s daughter
about delirium?
[Total 3 marks]
<answer here>
4
Question 3: Evaluate the Interventions that are documented to maintain Anthony’s safety.
Identify one (1) intervention that does not protect Anthony’s Human rights and provide an
alternative person-centred intervention. To answer this question, fill in the below table.
[Total 4marks]
Which intervention
does not protect
Anthony’s Human
rights (1 mark)?
Which Human right is not
protected and why (1
mark)
Provide an alternative intervention
and justification (2 marks)
<insert answer here> <answer here> <answer here>
Question 4: Consider the nursing interventions for the mental and cognitive status domain
of Neville’s care plan and evaluate whether these interventions are appropriate to alleviate
symptoms of Anthony’s delirium. Explain why/why not. (2 marks each).
[Total 6 marks]
<answer here>
Question 5: What key information should the nurse be providing to Anthony’s daughter
about delirium?
[Total 3 marks]
<answer here>
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Student Name: _________________ Student ID:__________________
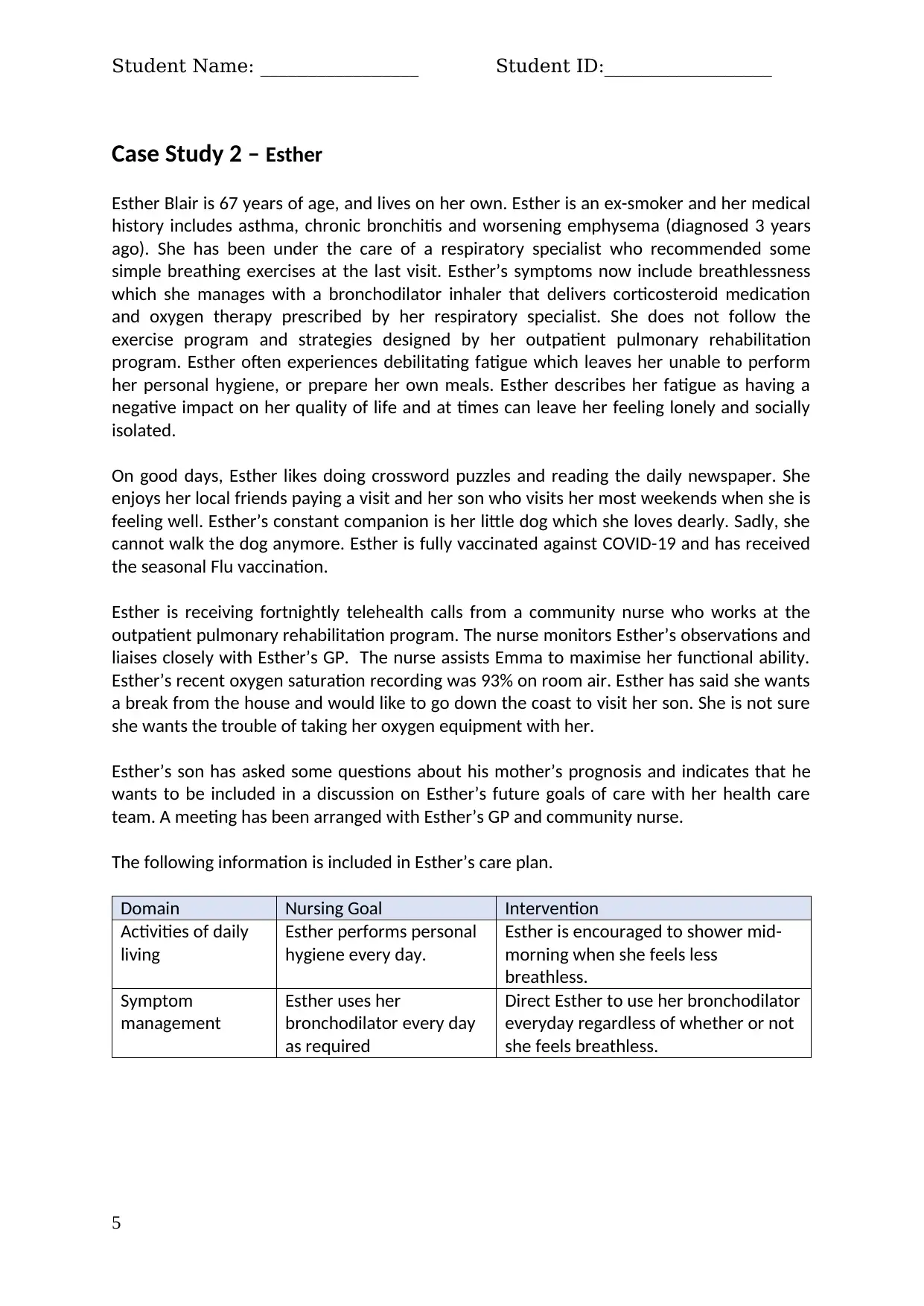
Case Study 2 – Esther
Esther Blair is 67 years of age, and lives on her own. Esther is an ex-smoker and her medical
history includes asthma, chronic bronchitis and worsening emphysema (diagnosed 3 years
ago). She has been under the care of a respiratory specialist who recommended some
simple breathing exercises at the last visit. Esther’s symptoms now include breathlessness
which she manages with a bronchodilator inhaler that delivers corticosteroid medication
and oxygen therapy prescribed by her respiratory specialist. She does not follow the
exercise program and strategies designed by her outpatient pulmonary rehabilitation
program. Esther often experiences debilitating fatigue which leaves her unable to perform
her personal hygiene, or prepare her own meals. Esther describes her fatigue as having a
negative impact on her quality of life and at times can leave her feeling lonely and socially
isolated.
On good days, Esther likes doing crossword puzzles and reading the daily newspaper. She
enjoys her local friends paying a visit and her son who visits her most weekends when she is
feeling well. Esther’s constant companion is her little dog which she loves dearly. Sadly, she
cannot walk the dog anymore. Esther is fully vaccinated against COVID-19 and has received
the seasonal Flu vaccination.
Esther is receiving fortnightly telehealth calls from a community nurse who works at the
outpatient pulmonary rehabilitation program. The nurse monitors Esther’s observations and
liaises closely with Esther’s GP. The nurse assists Emma to maximise her functional ability.
Esther’s recent oxygen saturation recording was 93% on room air. Esther has said she wants
a break from the house and would like to go down the coast to visit her son. She is not sure
she wants the trouble of taking her oxygen equipment with her.
Esther’s son has asked some questions about his mother’s prognosis and indicates that he
wants to be included in a discussion on Esther’s future goals of care with her health care
team. A meeting has been arranged with Esther’s GP and community nurse.
The following information is included in Esther’s care plan.
Domain Nursing Goal Intervention
Activities of daily
living
Esther performs personal
hygiene every day.
Esther is encouraged to shower mid-
morning when she feels less
breathless.
Symptom
management
Esther uses her
bronchodilator every day
as required
Direct Esther to use her bronchodilator
everyday regardless of whether or not
she feels breathless.
5
Case Study 2 – Esther
Esther Blair is 67 years of age, and lives on her own. Esther is an ex-smoker and her medical
history includes asthma, chronic bronchitis and worsening emphysema (diagnosed 3 years
ago). She has been under the care of a respiratory specialist who recommended some
simple breathing exercises at the last visit. Esther’s symptoms now include breathlessness
which she manages with a bronchodilator inhaler that delivers corticosteroid medication
and oxygen therapy prescribed by her respiratory specialist. She does not follow the
exercise program and strategies designed by her outpatient pulmonary rehabilitation
program. Esther often experiences debilitating fatigue which leaves her unable to perform
her personal hygiene, or prepare her own meals. Esther describes her fatigue as having a
negative impact on her quality of life and at times can leave her feeling lonely and socially
isolated.
On good days, Esther likes doing crossword puzzles and reading the daily newspaper. She
enjoys her local friends paying a visit and her son who visits her most weekends when she is
feeling well. Esther’s constant companion is her little dog which she loves dearly. Sadly, she
cannot walk the dog anymore. Esther is fully vaccinated against COVID-19 and has received
the seasonal Flu vaccination.
Esther is receiving fortnightly telehealth calls from a community nurse who works at the
outpatient pulmonary rehabilitation program. The nurse monitors Esther’s observations and
liaises closely with Esther’s GP. The nurse assists Emma to maximise her functional ability.
Esther’s recent oxygen saturation recording was 93% on room air. Esther has said she wants
a break from the house and would like to go down the coast to visit her son. She is not sure
she wants the trouble of taking her oxygen equipment with her.
Esther’s son has asked some questions about his mother’s prognosis and indicates that he
wants to be included in a discussion on Esther’s future goals of care with her health care
team. A meeting has been arranged with Esther’s GP and community nurse.
The following information is included in Esther’s care plan.
Domain Nursing Goal Intervention
Activities of daily
living
Esther performs personal
hygiene every day.
Esther is encouraged to shower mid-
morning when she feels less
breathless.
Symptom
management
Esther uses her
bronchodilator every day
as required
Direct Esther to use her bronchodilator
everyday regardless of whether or not
she feels breathless.
5
Student Name: _________________ Student ID:__________________
Using the information presented in Esther’s case study and care plan to answer the
following five (5) questions
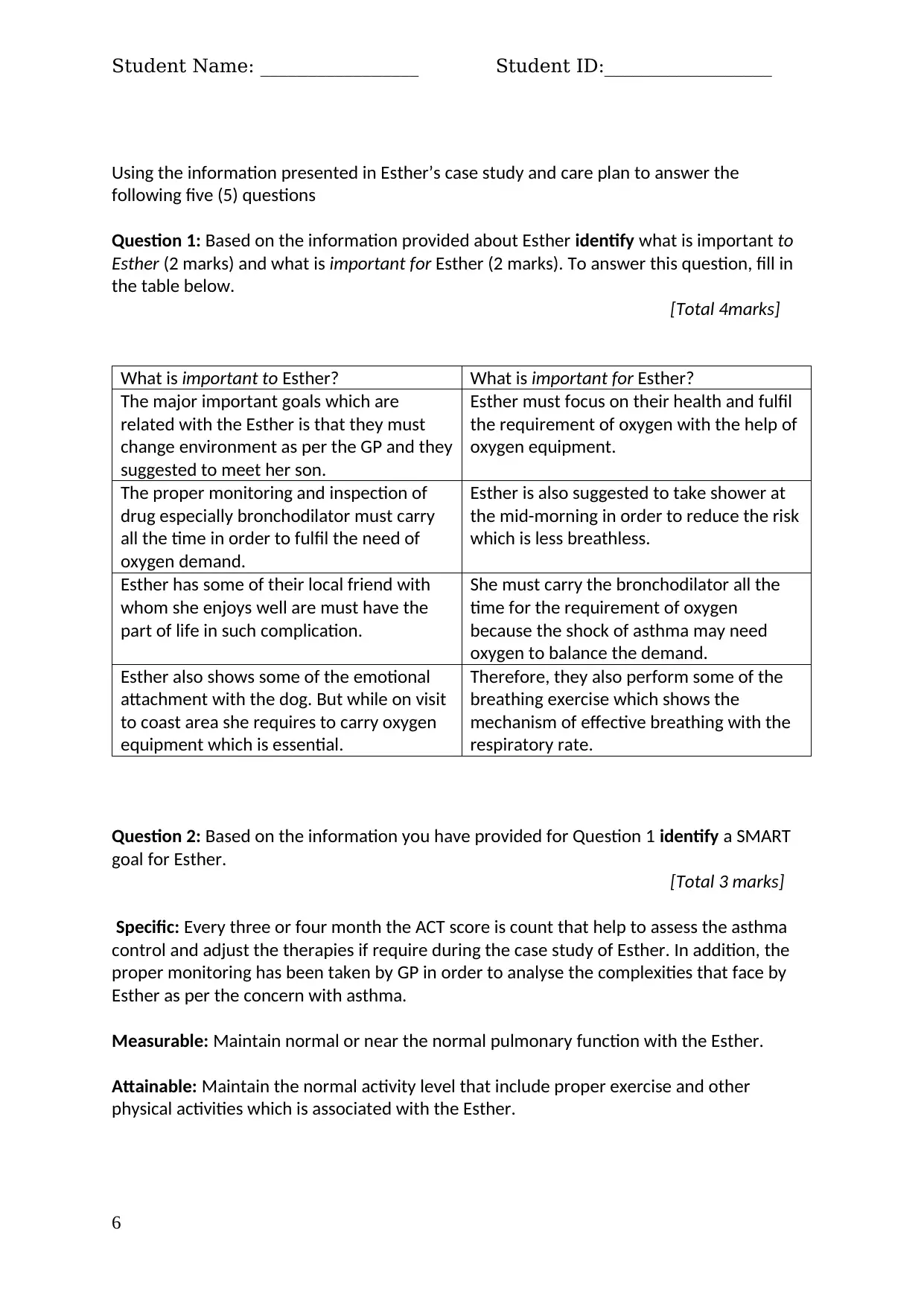
Question 1: Based on the information provided about Esther identify what is important to
Esther (2 marks) and what is important for Esther (2 marks). To answer this question, fill in
the table below.
[Total 4marks]
What is important to Esther? What is important for Esther?
The major important goals which are
related with the Esther is that they must
change environment as per the GP and they
suggested to meet her son.
Esther must focus on their health and fulfil
the requirement of oxygen with the help of
oxygen equipment.
The proper monitoring and inspection of
drug especially bronchodilator must carry
all the time in order to fulfil the need of
oxygen demand.
Esther is also suggested to take shower at
the mid-morning in order to reduce the risk
which is less breathless.
Esther has some of their local friend with
whom she enjoys well are must have the
part of life in such complication.
She must carry the bronchodilator all the
time for the requirement of oxygen
because the shock of asthma may need
oxygen to balance the demand.
Esther also shows some of the emotional
attachment with the dog. But while on visit
to coast area she requires to carry oxygen
equipment which is essential.
Therefore, they also perform some of the
breathing exercise which shows the
mechanism of effective breathing with the
respiratory rate.
Question 2: Based on the information you have provided for Question 1 identify a SMART
goal for Esther.
[Total 3 marks]
Specific: Every three or four month the ACT score is count that help to assess the asthma
control and adjust the therapies if require during the case study of Esther. In addition, the
proper monitoring has been taken by GP in order to analyse the complexities that face by
Esther as per the concern with asthma.
Measurable: Maintain normal or near the normal pulmonary function with the Esther.
Attainable: Maintain the normal activity level that include proper exercise and other
physical activities which is associated with the Esther.
6
Using the information presented in Esther’s case study and care plan to answer the
following five (5) questions
Question 1: Based on the information provided about Esther identify what is important to
Esther (2 marks) and what is important for Esther (2 marks). To answer this question, fill in
the table below.
[Total 4marks]
What is important to Esther? What is important for Esther?
The major important goals which are
related with the Esther is that they must
change environment as per the GP and they
suggested to meet her son.
Esther must focus on their health and fulfil
the requirement of oxygen with the help of
oxygen equipment.
The proper monitoring and inspection of
drug especially bronchodilator must carry
all the time in order to fulfil the need of
oxygen demand.
Esther is also suggested to take shower at
the mid-morning in order to reduce the risk
which is less breathless.
Esther has some of their local friend with
whom she enjoys well are must have the
part of life in such complication.
She must carry the bronchodilator all the
time for the requirement of oxygen
because the shock of asthma may need
oxygen to balance the demand.
Esther also shows some of the emotional
attachment with the dog. But while on visit
to coast area she requires to carry oxygen
equipment which is essential.
Therefore, they also perform some of the
breathing exercise which shows the
mechanism of effective breathing with the
respiratory rate.
Question 2: Based on the information you have provided for Question 1 identify a SMART
goal for Esther.
[Total 3 marks]
Specific: Every three or four month the ACT score is count that help to assess the asthma
control and adjust the therapies if require during the case study of Esther. In addition, the
proper monitoring has been taken by GP in order to analyse the complexities that face by
Esther as per the concern with asthma.
Measurable: Maintain normal or near the normal pulmonary function with the Esther.
Attainable: Maintain the normal activity level that include proper exercise and other
physical activities which is associated with the Esther.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
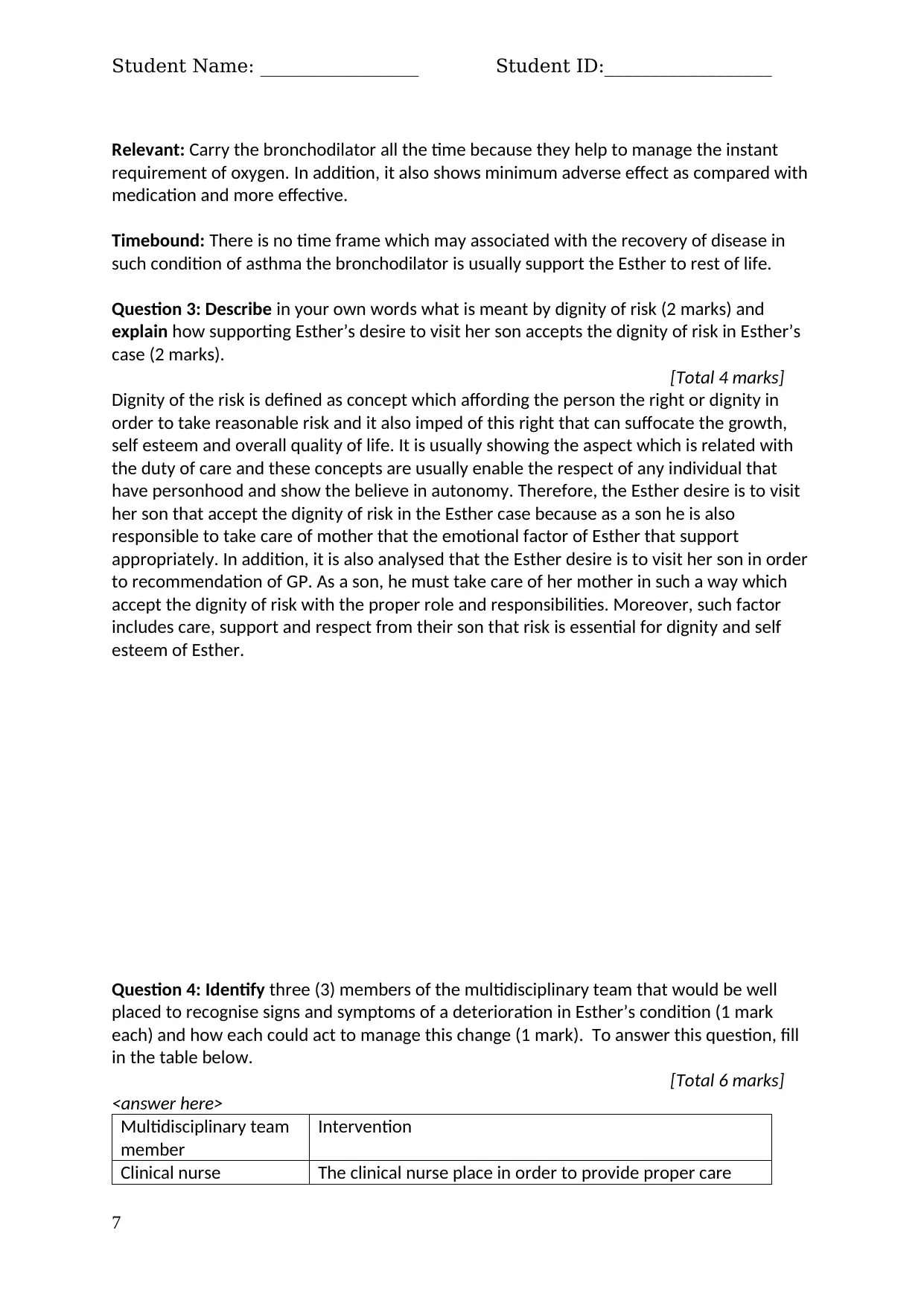
Student Name: _________________ Student ID:__________________
Relevant: Carry the bronchodilator all the time because they help to manage the instant
requirement of oxygen. In addition, it also shows minimum adverse effect as compared with
medication and more effective.
Timebound: There is no time frame which may associated with the recovery of disease in
such condition of asthma the bronchodilator is usually support the Esther to rest of life.
Question 3: Describe in your own words what is meant by dignity of risk (2 marks) and
explain how supporting Esther’s desire to visit her son accepts the dignity of risk in Esther’s
case (2 marks).
[Total 4 marks]
Dignity of the risk is defined as concept which affording the person the right or dignity in
order to take reasonable risk and it also imped of this right that can suffocate the growth,
self esteem and overall quality of life. It is usually showing the aspect which is related with
the duty of care and these concepts are usually enable the respect of any individual that
have personhood and show the believe in autonomy. Therefore, the Esther desire is to visit
her son that accept the dignity of risk in the Esther case because as a son he is also
responsible to take care of mother that the emotional factor of Esther that support
appropriately. In addition, it is also analysed that the Esther desire is to visit her son in order
to recommendation of GP. As a son, he must take care of her mother in such a way which
accept the dignity of risk with the proper role and responsibilities. Moreover, such factor
includes care, support and respect from their son that risk is essential for dignity and self
esteem of Esther.
Question 4: Identify three (3) members of the multidisciplinary team that would be well
placed to recognise signs and symptoms of a deterioration in Esther’s condition (1 mark
each) and how each could act to manage this change (1 mark). To answer this question, fill
in the table below.
[Total 6 marks]
<answer here>
Multidisciplinary team
member
Intervention
Clinical nurse The clinical nurse place in order to provide proper care
7
Relevant: Carry the bronchodilator all the time because they help to manage the instant
requirement of oxygen. In addition, it also shows minimum adverse effect as compared with
medication and more effective.
Timebound: There is no time frame which may associated with the recovery of disease in
such condition of asthma the bronchodilator is usually support the Esther to rest of life.
Question 3: Describe in your own words what is meant by dignity of risk (2 marks) and
explain how supporting Esther’s desire to visit her son accepts the dignity of risk in Esther’s
case (2 marks).
[Total 4 marks]
Dignity of the risk is defined as concept which affording the person the right or dignity in
order to take reasonable risk and it also imped of this right that can suffocate the growth,
self esteem and overall quality of life. It is usually showing the aspect which is related with
the duty of care and these concepts are usually enable the respect of any individual that
have personhood and show the believe in autonomy. Therefore, the Esther desire is to visit
her son that accept the dignity of risk in the Esther case because as a son he is also
responsible to take care of mother that the emotional factor of Esther that support
appropriately. In addition, it is also analysed that the Esther desire is to visit her son in order
to recommendation of GP. As a son, he must take care of her mother in such a way which
accept the dignity of risk with the proper role and responsibilities. Moreover, such factor
includes care, support and respect from their son that risk is essential for dignity and self
esteem of Esther.
Question 4: Identify three (3) members of the multidisciplinary team that would be well
placed to recognise signs and symptoms of a deterioration in Esther’s condition (1 mark
each) and how each could act to manage this change (1 mark). To answer this question, fill
in the table below.
[Total 6 marks]
<answer here>
Multidisciplinary team
member
Intervention
Clinical nurse The clinical nurse place in order to provide proper care
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
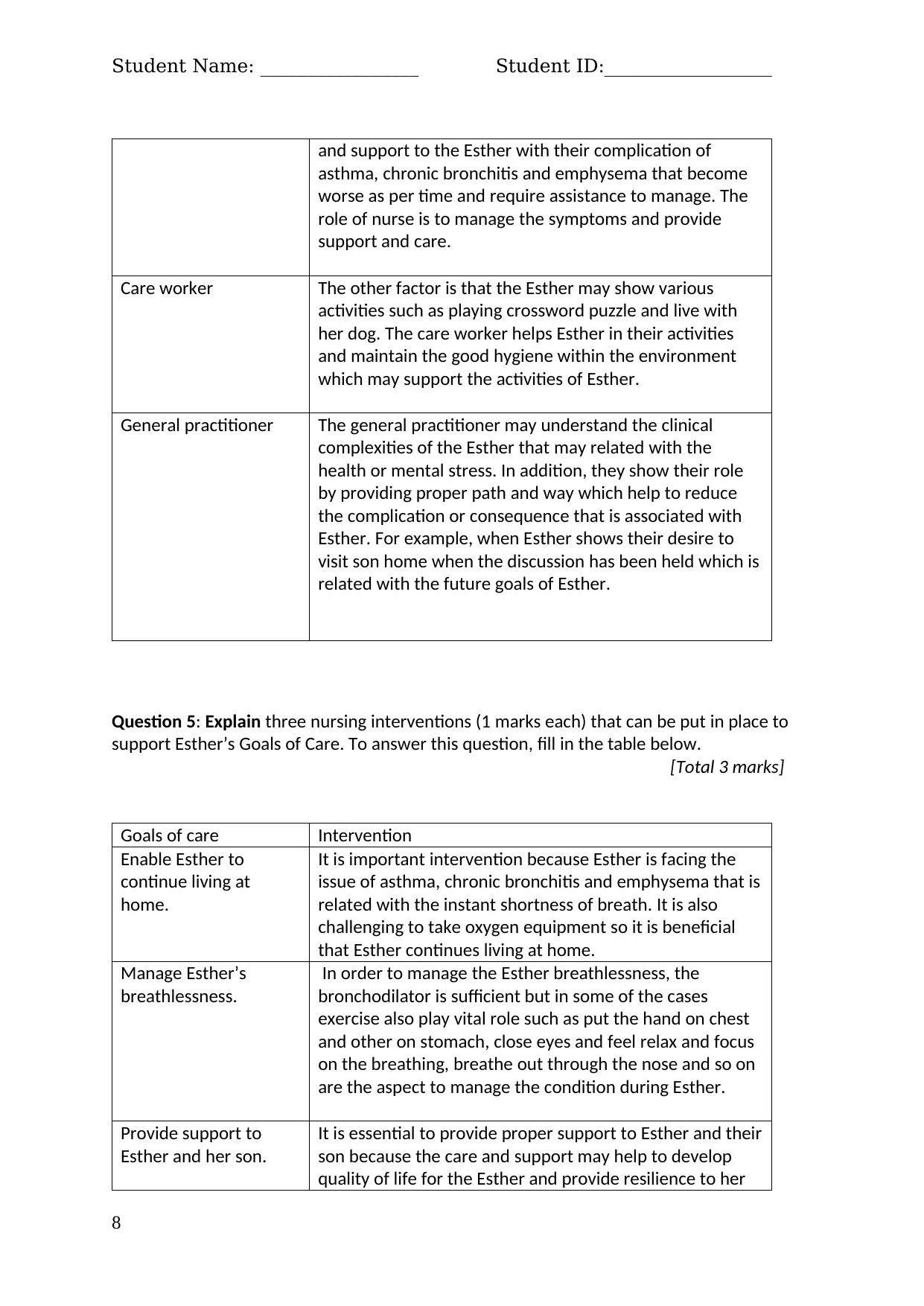
Student Name: _________________ Student ID:__________________
and support to the Esther with their complication of
asthma, chronic bronchitis and emphysema that become
worse as per time and require assistance to manage. The
role of nurse is to manage the symptoms and provide
support and care.
Care worker The other factor is that the Esther may show various
activities such as playing crossword puzzle and live with
her dog. The care worker helps Esther in their activities
and maintain the good hygiene within the environment
which may support the activities of Esther.
General practitioner The general practitioner may understand the clinical
complexities of the Esther that may related with the
health or mental stress. In addition, they show their role
by providing proper path and way which help to reduce
the complication or consequence that is associated with
Esther. For example, when Esther shows their desire to
visit son home when the discussion has been held which is
related with the future goals of Esther.
Question 5: Explain three nursing interventions (1 marks each) that can be put in place to
support Esther’s Goals of Care. To answer this question, fill in the table below.
[Total 3 marks]
Goals of care Intervention
Enable Esther to
continue living at
home.
It is important intervention because Esther is facing the
issue of asthma, chronic bronchitis and emphysema that is
related with the instant shortness of breath. It is also
challenging to take oxygen equipment so it is beneficial
that Esther continues living at home.
Manage Esther’s
breathlessness.
In order to manage the Esther breathlessness, the
bronchodilator is sufficient but in some of the cases
exercise also play vital role such as put the hand on chest
and other on stomach, close eyes and feel relax and focus
on the breathing, breathe out through the nose and so on
are the aspect to manage the condition during Esther.
Provide support to
Esther and her son.
It is essential to provide proper support to Esther and their
son because the care and support may help to develop
quality of life for the Esther and provide resilience to her
8
and support to the Esther with their complication of
asthma, chronic bronchitis and emphysema that become
worse as per time and require assistance to manage. The
role of nurse is to manage the symptoms and provide
support and care.
Care worker The other factor is that the Esther may show various
activities such as playing crossword puzzle and live with
her dog. The care worker helps Esther in their activities
and maintain the good hygiene within the environment
which may support the activities of Esther.
General practitioner The general practitioner may understand the clinical
complexities of the Esther that may related with the
health or mental stress. In addition, they show their role
by providing proper path and way which help to reduce
the complication or consequence that is associated with
Esther. For example, when Esther shows their desire to
visit son home when the discussion has been held which is
related with the future goals of Esther.
Question 5: Explain three nursing interventions (1 marks each) that can be put in place to
support Esther’s Goals of Care. To answer this question, fill in the table below.
[Total 3 marks]
Goals of care Intervention
Enable Esther to
continue living at
home.
It is important intervention because Esther is facing the
issue of asthma, chronic bronchitis and emphysema that is
related with the instant shortness of breath. It is also
challenging to take oxygen equipment so it is beneficial
that Esther continues living at home.
Manage Esther’s
breathlessness.
In order to manage the Esther breathlessness, the
bronchodilator is sufficient but in some of the cases
exercise also play vital role such as put the hand on chest
and other on stomach, close eyes and feel relax and focus
on the breathing, breathe out through the nose and so on
are the aspect to manage the condition during Esther.
Provide support to
Esther and her son.
It is essential to provide proper support to Esther and their
son because the care and support may help to develop
quality of life for the Esther and provide resilience to her
8
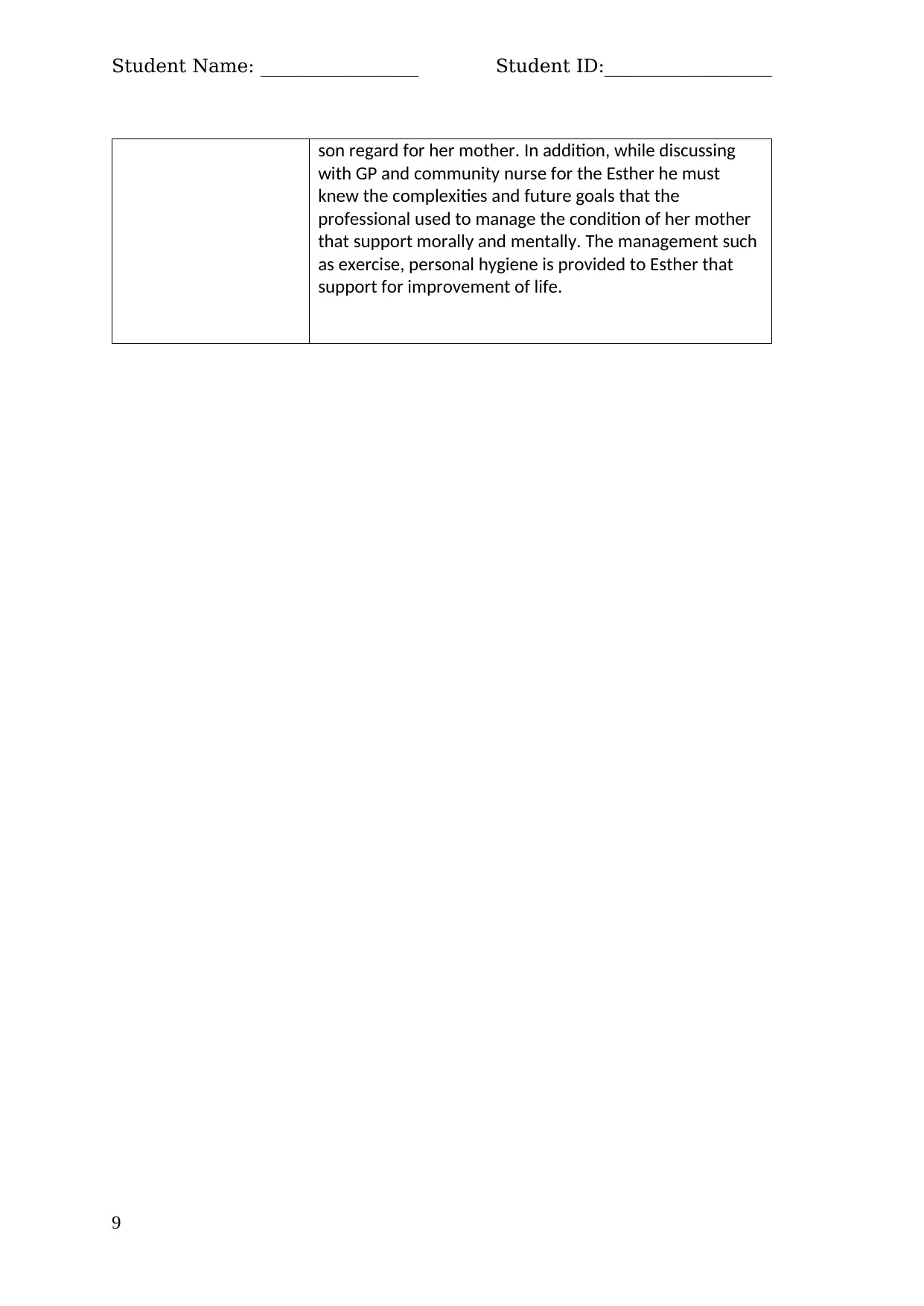
Student Name: _________________ Student ID:__________________
son regard for her mother. In addition, while discussing
with GP and community nurse for the Esther he must
knew the complexities and future goals that the
professional used to manage the condition of her mother
that support morally and mentally. The management such
as exercise, personal hygiene is provided to Esther that
support for improvement of life.
9
son regard for her mother. In addition, while discussing
with GP and community nurse for the Esther he must
knew the complexities and future goals that the
professional used to manage the condition of her mother
that support morally and mentally. The management such
as exercise, personal hygiene is provided to Esther that
support for improvement of life.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Student Name: _________________ Student ID:__________________
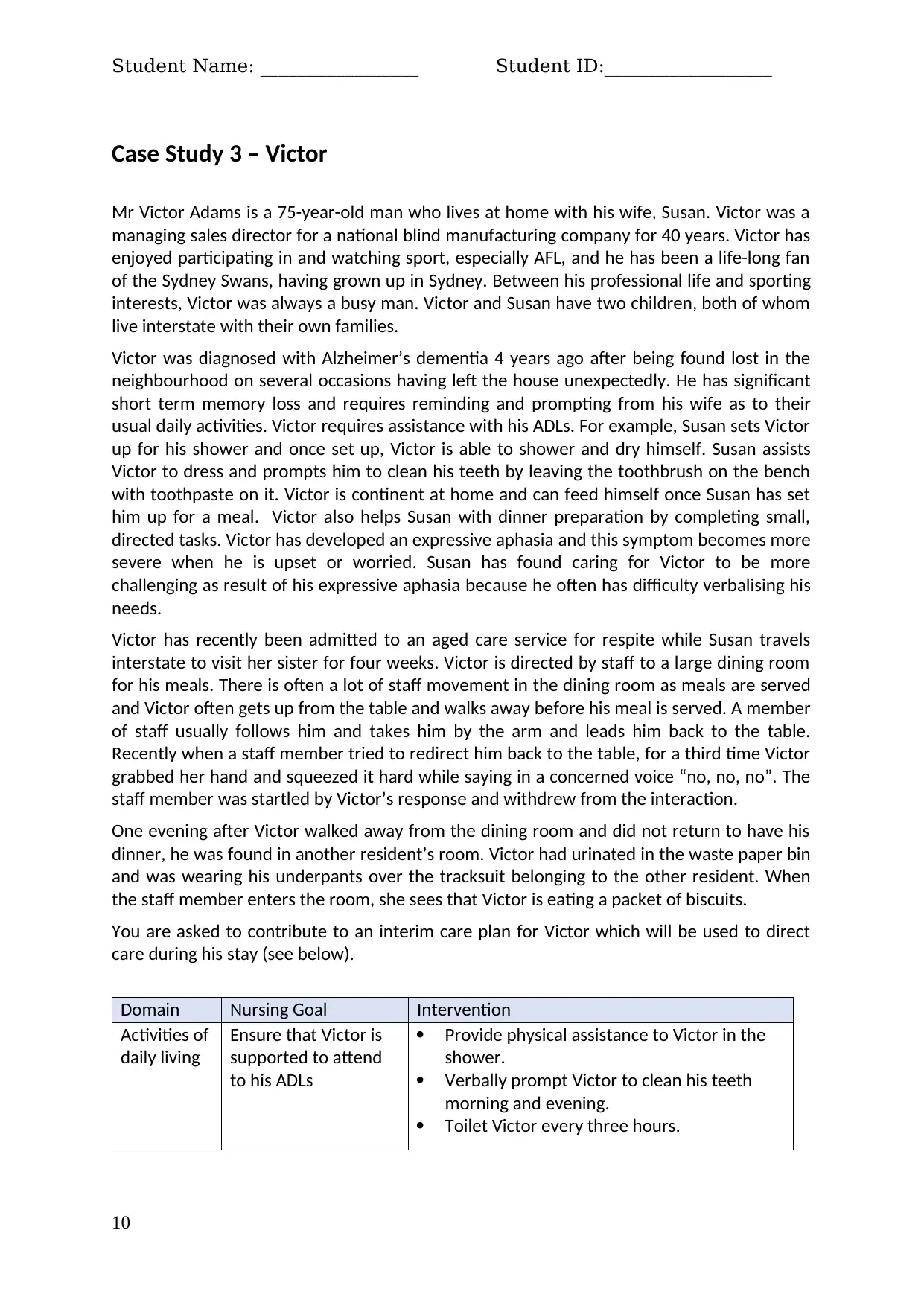
Case Study 3 – Victor
Mr Victor Adams is a 75-year-old man who lives at home with his wife, Susan. Victor was a
managing sales director for a national blind manufacturing company for 40 years. Victor has
enjoyed participating in and watching sport, especially AFL, and he has been a life-long fan
of the Sydney Swans, having grown up in Sydney. Between his professional life and sporting
interests, Victor was always a busy man. Victor and Susan have two children, both of whom
live interstate with their own families.
Victor was diagnosed with Alzheimer’s dementia 4 years ago after being found lost in the
neighbourhood on several occasions having left the house unexpectedly. He has significant
short term memory loss and requires reminding and prompting from his wife as to their
usual daily activities. Victor requires assistance with his ADLs. For example, Susan sets Victor
up for his shower and once set up, Victor is able to shower and dry himself. Susan assists
Victor to dress and prompts him to clean his teeth by leaving the toothbrush on the bench
with toothpaste on it. Victor is continent at home and can feed himself once Susan has set
him up for a meal. Victor also helps Susan with dinner preparation by completing small,
directed tasks. Victor has developed an expressive aphasia and this symptom becomes more
severe when he is upset or worried. Susan has found caring for Victor to be more
challenging as result of his expressive aphasia because he often has difficulty verbalising his
needs.
Victor has recently been admitted to an aged care service for respite while Susan travels
interstate to visit her sister for four weeks. Victor is directed by staff to a large dining room
for his meals. There is often a lot of staff movement in the dining room as meals are served
and Victor often gets up from the table and walks away before his meal is served. A member
of staff usually follows him and takes him by the arm and leads him back to the table.
Recently when a staff member tried to redirect him back to the table, for a third time Victor
grabbed her hand and squeezed it hard while saying in a concerned voice “no, no, no”. The
staff member was startled by Victor’s response and withdrew from the interaction.
One evening after Victor walked away from the dining room and did not return to have his
dinner, he was found in another resident’s room. Victor had urinated in the waste paper bin
and was wearing his underpants over the tracksuit belonging to the other resident. When
the staff member enters the room, she sees that Victor is eating a packet of biscuits.
You are asked to contribute to an interim care plan for Victor which will be used to direct
care during his stay (see below).
Domain Nursing Goal Intervention
Activities of
daily living
Ensure that Victor is
supported to attend
to his ADLs
Provide physical assistance to Victor in the
shower.
Verbally prompt Victor to clean his teeth
morning and evening.
Toilet Victor every three hours.
10
Case Study 3 – Victor
Mr Victor Adams is a 75-year-old man who lives at home with his wife, Susan. Victor was a
managing sales director for a national blind manufacturing company for 40 years. Victor has
enjoyed participating in and watching sport, especially AFL, and he has been a life-long fan
of the Sydney Swans, having grown up in Sydney. Between his professional life and sporting
interests, Victor was always a busy man. Victor and Susan have two children, both of whom
live interstate with their own families.
Victor was diagnosed with Alzheimer’s dementia 4 years ago after being found lost in the
neighbourhood on several occasions having left the house unexpectedly. He has significant
short term memory loss and requires reminding and prompting from his wife as to their
usual daily activities. Victor requires assistance with his ADLs. For example, Susan sets Victor
up for his shower and once set up, Victor is able to shower and dry himself. Susan assists
Victor to dress and prompts him to clean his teeth by leaving the toothbrush on the bench
with toothpaste on it. Victor is continent at home and can feed himself once Susan has set
him up for a meal. Victor also helps Susan with dinner preparation by completing small,
directed tasks. Victor has developed an expressive aphasia and this symptom becomes more
severe when he is upset or worried. Susan has found caring for Victor to be more
challenging as result of his expressive aphasia because he often has difficulty verbalising his
needs.
Victor has recently been admitted to an aged care service for respite while Susan travels
interstate to visit her sister for four weeks. Victor is directed by staff to a large dining room
for his meals. There is often a lot of staff movement in the dining room as meals are served
and Victor often gets up from the table and walks away before his meal is served. A member
of staff usually follows him and takes him by the arm and leads him back to the table.
Recently when a staff member tried to redirect him back to the table, for a third time Victor
grabbed her hand and squeezed it hard while saying in a concerned voice “no, no, no”. The
staff member was startled by Victor’s response and withdrew from the interaction.
One evening after Victor walked away from the dining room and did not return to have his
dinner, he was found in another resident’s room. Victor had urinated in the waste paper bin
and was wearing his underpants over the tracksuit belonging to the other resident. When
the staff member enters the room, she sees that Victor is eating a packet of biscuits.
You are asked to contribute to an interim care plan for Victor which will be used to direct
care during his stay (see below).
Domain Nursing Goal Intervention
Activities of
daily living
Ensure that Victor is
supported to attend
to his ADLs
Provide physical assistance to Victor in the
shower.
Verbally prompt Victor to clean his teeth
morning and evening.
Toilet Victor every three hours.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
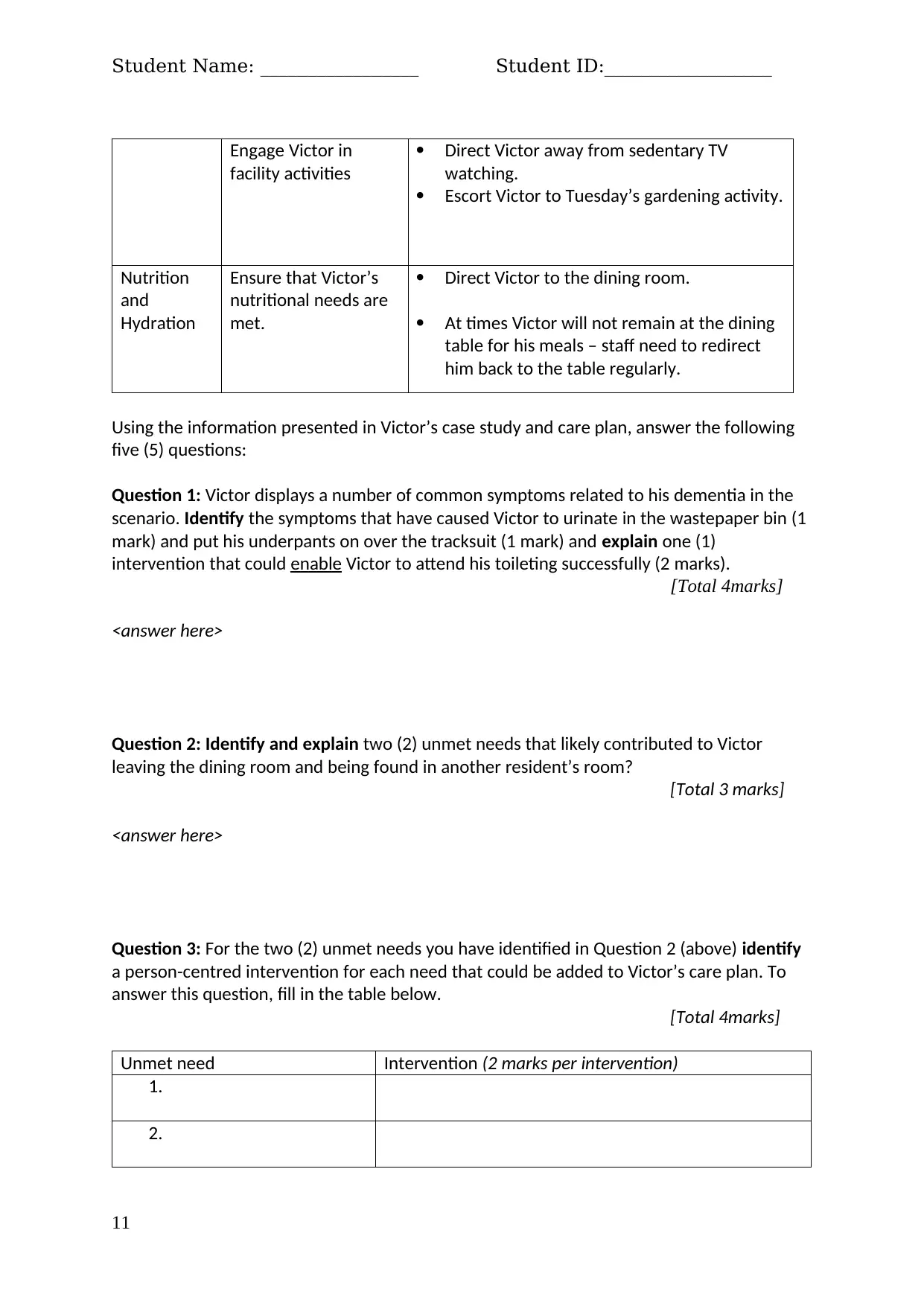
Student Name: _________________ Student ID:__________________
Engage Victor in
facility activities
Direct Victor away from sedentary TV
watching.
Escort Victor to Tuesday’s gardening activity.
Nutrition
and
Hydration
Ensure that Victor’s
nutritional needs are
met.
Direct Victor to the dining room.
At times Victor will not remain at the dining
table for his meals – staff need to redirect
him back to the table regularly.
Using the information presented in Victor’s case study and care plan, answer the following
five (5) questions:
Question 1: Victor displays a number of common symptoms related to his dementia in the
scenario. Identify the symptoms that have caused Victor to urinate in the wastepaper bin (1
mark) and put his underpants on over the tracksuit (1 mark) and explain one (1)
intervention that could enable Victor to attend his toileting successfully (2 marks).
[Total 4marks]
<answer here>
Question 2: Identify and explain two (2) unmet needs that likely contributed to Victor
leaving the dining room and being found in another resident’s room?
[Total 3 marks]
<answer here>
Question 3: For the two (2) unmet needs you have identified in Question 2 (above) identify
a person-centred intervention for each need that could be added to Victor’s care plan. To
answer this question, fill in the table below.
[Total 4marks]
Unmet need Intervention (2 marks per intervention)
1.
2.
11
Engage Victor in
facility activities
Direct Victor away from sedentary TV
watching.
Escort Victor to Tuesday’s gardening activity.
Nutrition
and
Hydration
Ensure that Victor’s
nutritional needs are
met.
Direct Victor to the dining room.
At times Victor will not remain at the dining
table for his meals – staff need to redirect
him back to the table regularly.
Using the information presented in Victor’s case study and care plan, answer the following
five (5) questions:
Question 1: Victor displays a number of common symptoms related to his dementia in the
scenario. Identify the symptoms that have caused Victor to urinate in the wastepaper bin (1
mark) and put his underpants on over the tracksuit (1 mark) and explain one (1)
intervention that could enable Victor to attend his toileting successfully (2 marks).
[Total 4marks]
<answer here>
Question 2: Identify and explain two (2) unmet needs that likely contributed to Victor
leaving the dining room and being found in another resident’s room?
[Total 3 marks]
<answer here>
Question 3: For the two (2) unmet needs you have identified in Question 2 (above) identify
a person-centred intervention for each need that could be added to Victor’s care plan. To
answer this question, fill in the table below.
[Total 4marks]
Unmet need Intervention (2 marks per intervention)
1.
2.
11
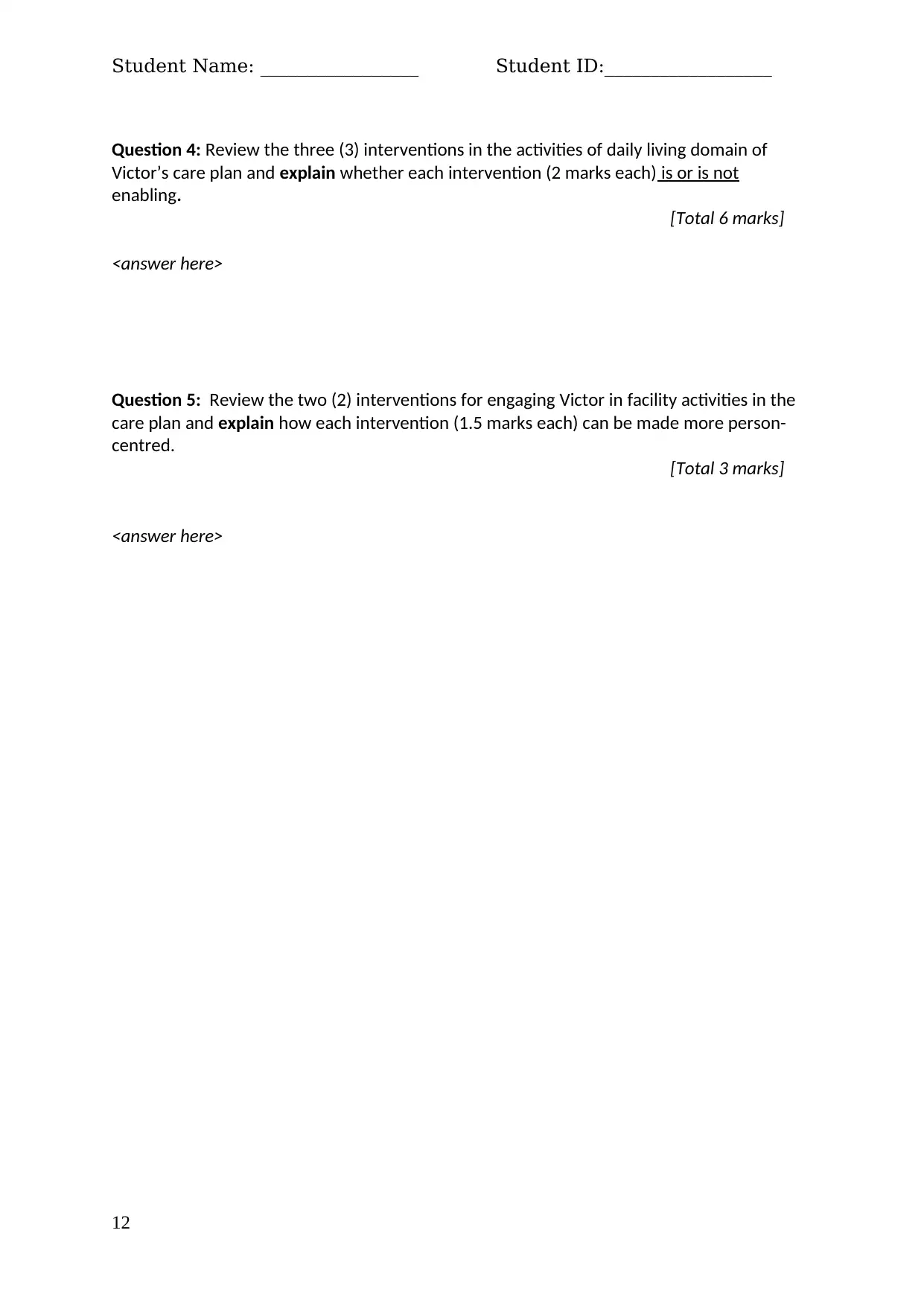
Student Name: _________________ Student ID:__________________
Question 4: Review the three (3) interventions in the activities of daily living domain of
Victor’s care plan and explain whether each intervention (2 marks each) is or is not
enabling.
[Total 6 marks]
<answer here>
Question 5: Review the two (2) interventions for engaging Victor in facility activities in the
care plan and explain how each intervention (1.5 marks each) can be made more person-
centred.
[Total 3 marks]
<answer here>
12
Question 4: Review the three (3) interventions in the activities of daily living domain of
Victor’s care plan and explain whether each intervention (2 marks each) is or is not
enabling.
[Total 6 marks]
<answer here>
Question 5: Review the two (2) interventions for engaging Victor in facility activities in the
care plan and explain how each intervention (1.5 marks each) can be made more person-
centred.
[Total 3 marks]
<answer here>
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





