Meeting Needs of People with Disability: Individual Support Assessment
VerifiedAdded on 2023/04/22
|10
|2043
|387
Homework Assignment
AI Summary
This document presents a completed assessment for a Certificate III in Individual Support (Disability) course, addressing the module on meeting the needs of people with a disability. The assignment explores key concepts such as behaviors of concern, positive behavior support, and person-centered practice. It includes case studies of individuals with various disabilities like cerebral palsy, paraplegia, multiple sclerosis, and Down syndrome, analyzing their potential behaviors, triggers, and support strategies. The assessment covers patient assessment, environmental factors, and training plans. It also examines scenarios involving challenging behaviors, intervention procedures, and communication techniques, including the use of visual aids and active listening. The document further addresses restrictive and prohibited practices, care plan modifications, and referral processes for additional professional support, such as dieticians and counselors. The assignment provides a comprehensive overview of the skills and knowledge required to support individuals with disabilities, emphasizing the importance of individualized care and effective communication.

Running Head: INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Name of the student:
Student ID-
Name of the university:
Author note:
INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Name of the student:
Student ID-
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Part 1
A. Behaviours of concern:
Behaviour of concern can be defined as the action and words that describes
inappropriate behaviour of a person. It is a behaviour done by people, which creates
complication to others as well as to themselves (Gifford and Nilsson 2014).
B. Positive behaviour support
Positive behaviour support is a support strategy used to comprehend a person’s
challenging behaviour. Usually an individual’s behaviour is influenced by their surrounding
and cannot be changed easily as they are functional. Their inappropriate actions assist a
purpose for them (Hassiotis et al. 2014).
C. Ji-yoon-
Ji-yoon was born with cerebral palsy that damages the movement,
posture and coordination. To assist her in maintaining her body posture
and movement, walking aids, body braces could be suggested by Julie.
Hearing aids and eye glasses could also be recommended to maintain
her coordination.
To deal with her learning speech difficulty, speech therapy could be
conducted.
Counselling and recreational therapy could be conducted in minimising
her outbursts.
To control her recurrent seizure, exercise and specific diet could be
advised by Julie.
Part 1
A. Behaviours of concern:
Behaviour of concern can be defined as the action and words that describes
inappropriate behaviour of a person. It is a behaviour done by people, which creates
complication to others as well as to themselves (Gifford and Nilsson 2014).
B. Positive behaviour support
Positive behaviour support is a support strategy used to comprehend a person’s
challenging behaviour. Usually an individual’s behaviour is influenced by their surrounding
and cannot be changed easily as they are functional. Their inappropriate actions assist a
purpose for them (Hassiotis et al. 2014).
C. Ji-yoon-
Ji-yoon was born with cerebral palsy that damages the movement,
posture and coordination. To assist her in maintaining her body posture
and movement, walking aids, body braces could be suggested by Julie.
Hearing aids and eye glasses could also be recommended to maintain
her coordination.
To deal with her learning speech difficulty, speech therapy could be
conducted.
Counselling and recreational therapy could be conducted in minimising
her outbursts.
To control her recurrent seizure, exercise and specific diet could be
advised by Julie.
2INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
D. Peter
Peter is suffering from paraplegia due to which he lost his walking
ability. To help him with that walking aids could be suggested.
He has become prone to outburst, which could be treated by
conducting counselling sessions.
Physical therapy such as, electric muscle simulation, exercise and
manual therapy could be conducted to encourage a healthy lifestyle for
peter.
Part 2
Providing safe environment to patient suffering from disability is essential in order to
get an effective result. An efficient care plan could be assessed after listening their
mental and physical problem for patient such as Ji-yoon and Emma, who are suffering
from speech delivering and walking difficulty. They should be provided with
emotional support and physical comfort such that they can share their feelings to the
worker. Patient suffering from disabilities usually afraid of getting isolated, hence
valuing and respecting the patient as a part of the society, could minimise that fear.
These patient are usually prone to aggressive outbursts, which can be reduced by
conducting counselling and recreational therapy. Resident care system and transition
of care system should be provided by patient centred care to give them a healthy daily
life. Healthy diet could be provided to give them a hale and hearty lifestyle. They
should be provided with an environment where they can enjoy their life at fullest.
Part 3-
A.
D. Peter
Peter is suffering from paraplegia due to which he lost his walking
ability. To help him with that walking aids could be suggested.
He has become prone to outburst, which could be treated by
conducting counselling sessions.
Physical therapy such as, electric muscle simulation, exercise and
manual therapy could be conducted to encourage a healthy lifestyle for
peter.
Part 2
Providing safe environment to patient suffering from disability is essential in order to
get an effective result. An efficient care plan could be assessed after listening their
mental and physical problem for patient such as Ji-yoon and Emma, who are suffering
from speech delivering and walking difficulty. They should be provided with
emotional support and physical comfort such that they can share their feelings to the
worker. Patient suffering from disabilities usually afraid of getting isolated, hence
valuing and respecting the patient as a part of the society, could minimise that fear.
These patient are usually prone to aggressive outbursts, which can be reduced by
conducting counselling and recreational therapy. Resident care system and transition
of care system should be provided by patient centred care to give them a healthy daily
life. Healthy diet could be provided to give them a hale and hearty lifestyle. They
should be provided with an environment where they can enjoy their life at fullest.
Part 3-
A.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
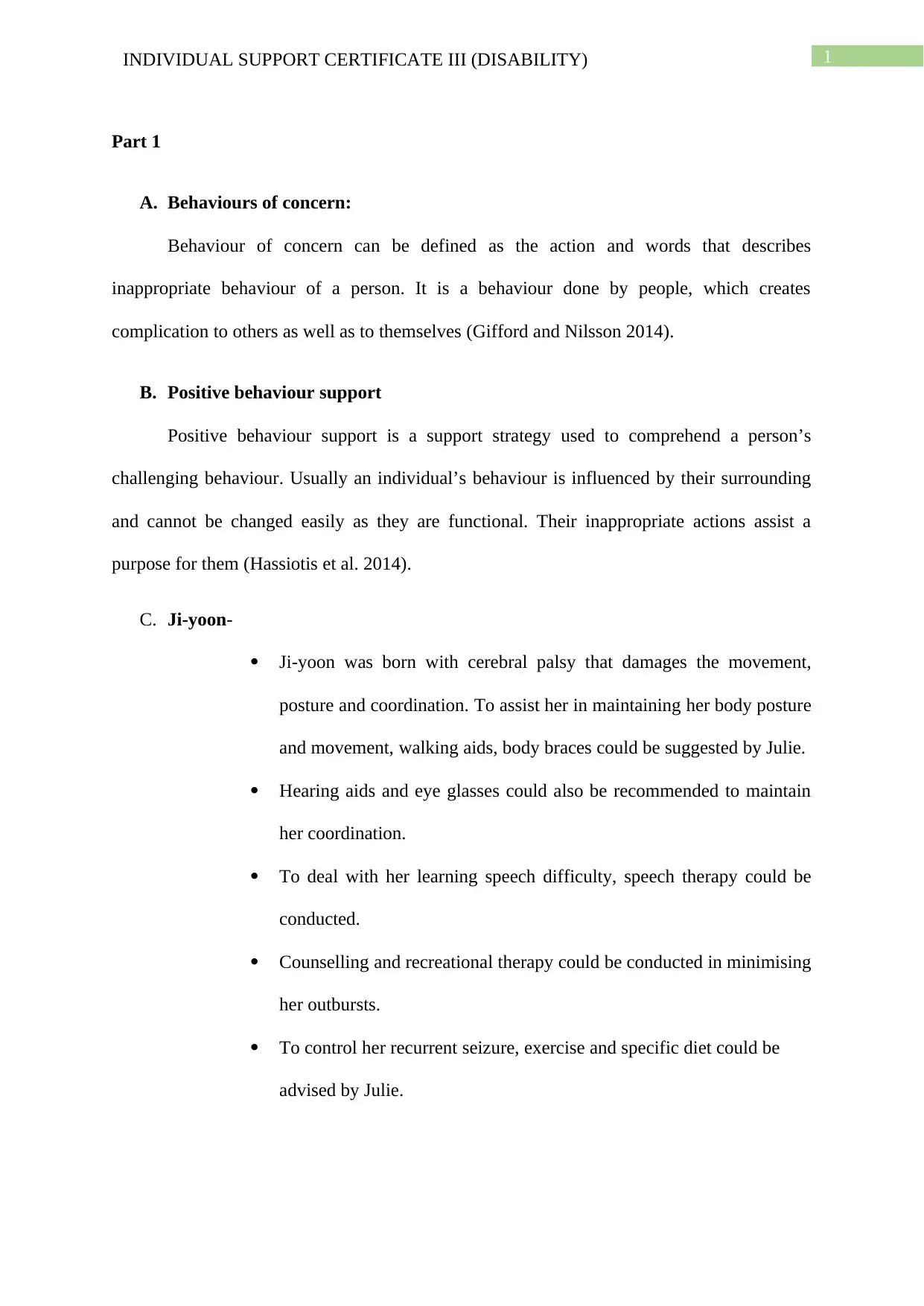
Feature of a
Behaviour Support
Plan
Brief description of this feature
Patient assessment In patient assessment, the mentality of the patient is assessed
such as, why the patient is involved in challenging behaviour.
Environment
assessment
Environment assessment is done to evaluate the
environmental factor which are responsible for such
challenging behaviour of patient. Then developing a care plan
to modify the environment to avoid such unnecessary
behaviour.
Training This plan is assessed to avoid challenging behaviour that has
been triggered by environment and emotional factor. New
skills has been demonstrated, which helps them in achieving
their needs.
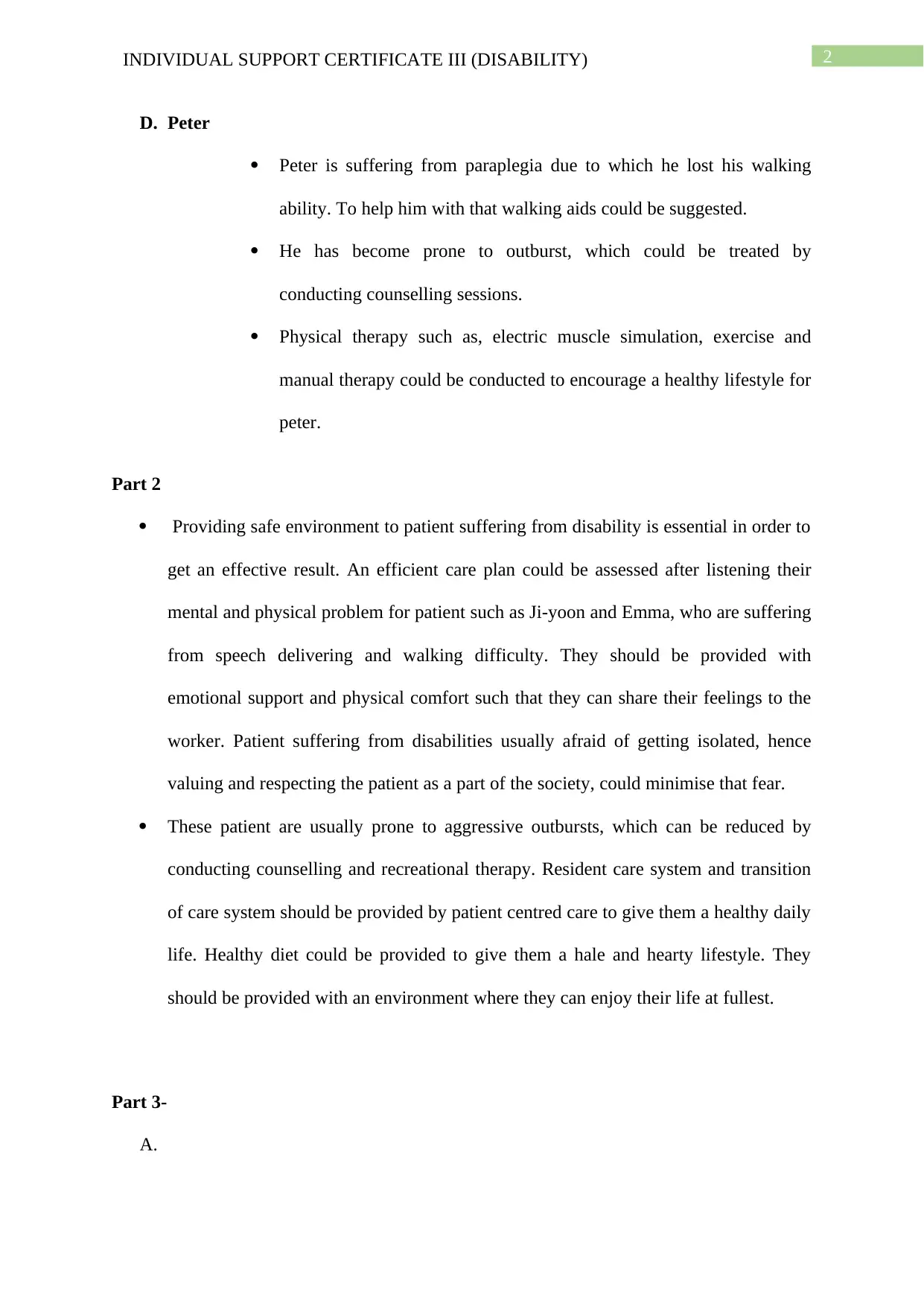
B.
Individual Disability Possible behaviour
of concern
Possible trigger
Ji-yoon, female, 7
years old
Cerebral Palsy Prone to outbursts Feels that she isn’t
being understood
Juliette, female, 33
years old
Acquired brain
injury
Prone to aggressive
outbursts.
Want to go back to
his previous lifestyle
and workplace
Feature of a
Behaviour Support
Plan
Brief description of this feature
Patient assessment In patient assessment, the mentality of the patient is assessed
such as, why the patient is involved in challenging behaviour.
Environment
assessment
Environment assessment is done to evaluate the
environmental factor which are responsible for such
challenging behaviour of patient. Then developing a care plan
to modify the environment to avoid such unnecessary
behaviour.
Training This plan is assessed to avoid challenging behaviour that has
been triggered by environment and emotional factor. New
skills has been demonstrated, which helps them in achieving
their needs.
B.
Individual Disability Possible behaviour
of concern
Possible trigger
Ji-yoon, female, 7
years old
Cerebral Palsy Prone to outbursts Feels that she isn’t
being understood
Juliette, female, 33
years old
Acquired brain
injury
Prone to aggressive
outbursts.
Want to go back to
his previous lifestyle
and workplace
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Jose, male, 21 years
old
Multiple sclerosis Prone to verbal
aggression.
Frustrated because
she feels isolated.
Ashley, female, 13
years old
Down syndrome Impulsive behaviour Irritated because of
their speech
delivering disability
(Wiseman et al
2015).
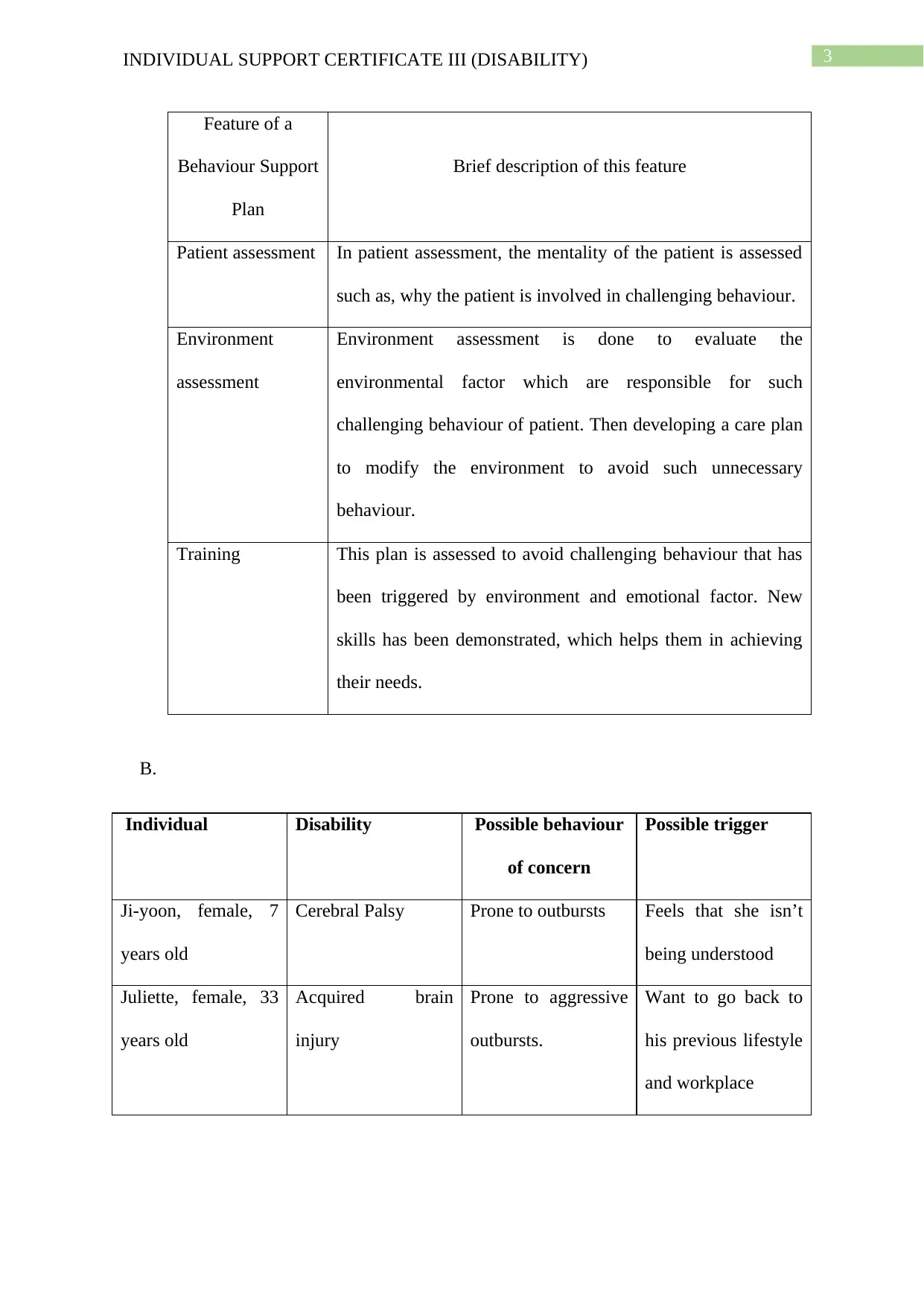
Part 4-
A.
Stage Should Julie have anything have done differently?
Before the incident Yes, she could have listened to her initially, while passing a café.
During the incident Yes, instead of trying her to move away from the café, she could
have taken her to that café to buy whatever she wants.
After the incident No, she had shown her different pictures to determine, what she
wants from the café and then purchased that for her.
B. Julie and Ji-yoon went out to visit a local park. In between they passed a café. Initially
Ji-yoon murmured something to Julie that she want something from that café. Julie
did not responded to her at that moment, which triggered her initial outburst of
screaming and thrashing.
C. After the incident, Julie handed her iPad to Ji-yoon to calm down her. After that with
the help of different pictures she tried to figure out what triggered Ji-yoon’s initial
outburst.
Jose, male, 21 years
old
Multiple sclerosis Prone to verbal
aggression.
Frustrated because
she feels isolated.
Ashley, female, 13
years old
Down syndrome Impulsive behaviour Irritated because of
their speech
delivering disability
(Wiseman et al
2015).
Part 4-
A.
Stage Should Julie have anything have done differently?
Before the incident Yes, she could have listened to her initially, while passing a café.
During the incident Yes, instead of trying her to move away from the café, she could
have taken her to that café to buy whatever she wants.
After the incident No, she had shown her different pictures to determine, what she
wants from the café and then purchased that for her.
B. Julie and Ji-yoon went out to visit a local park. In between they passed a café. Initially
Ji-yoon murmured something to Julie that she want something from that café. Julie
did not responded to her at that moment, which triggered her initial outburst of
screaming and thrashing.
C. After the incident, Julie handed her iPad to Ji-yoon to calm down her. After that with
the help of different pictures she tried to figure out what triggered Ji-yoon’s initial
outburst.
5INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
D. During Ji-yoon’s initial outburst, she hit Julie on the side of her face with her arm and
also started screaming and thrashing. To ensure safety of herself as well as ji-yoon,
she should follow CareShore’s procedures.
E. Julie needs to follow CareShore’s intervention and notification procedures to avoid
such incidents in future and to confirm the safety of patients and healthcare workers
and to demonstrate the reason behind the event.
F. Ji-yoon felt that she was being neglected by Julie and hence, she started screaming
and thrashing her out of her wheel chair. After that she got irritated because she feels
that she is not being understood, which lead to her outburst.
G. The behaviour support plan of Ji-yoon should include her behaviour of getting
irritated, when she feels that she is being neglected or not being understood.
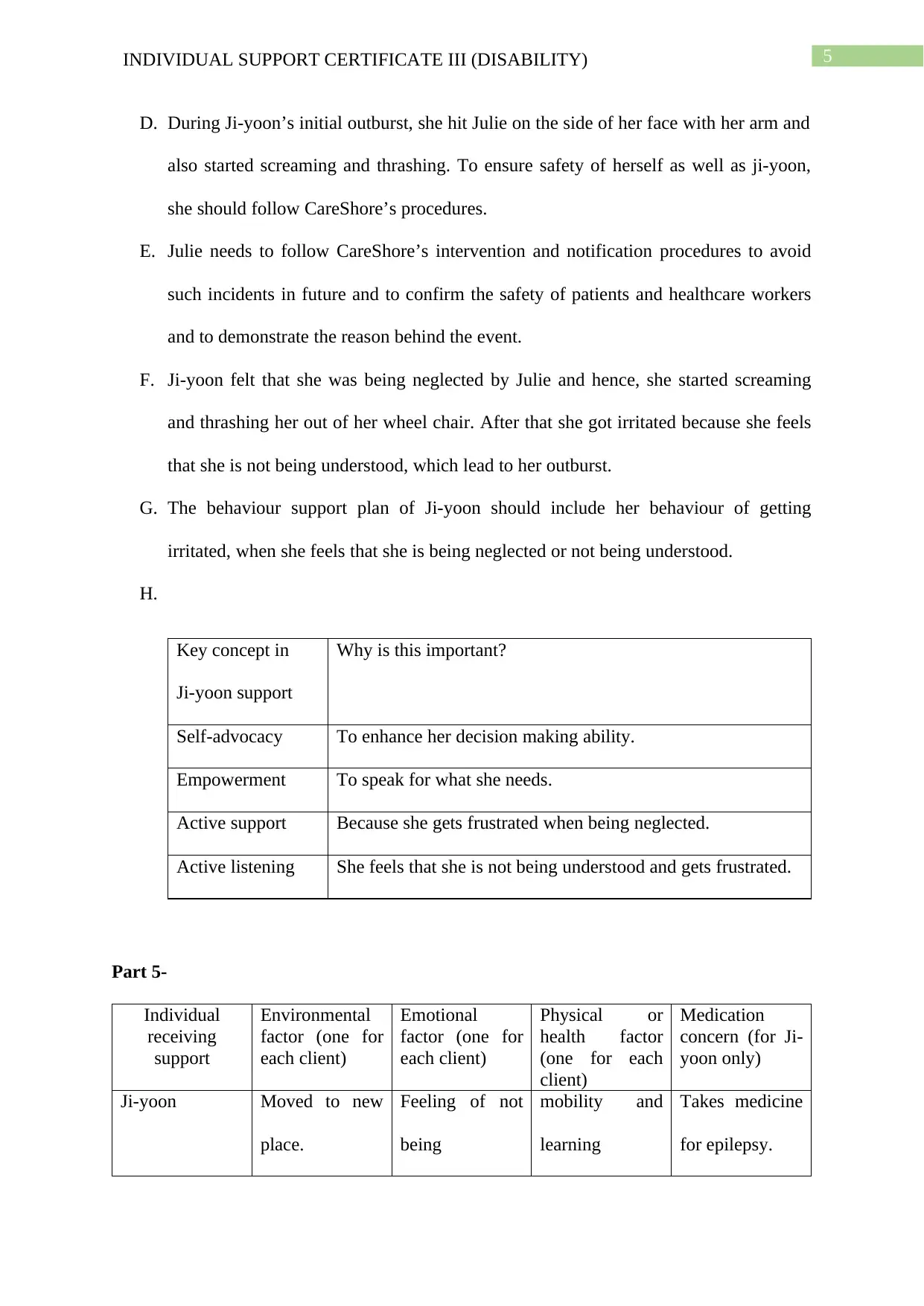
H.
Key concept in
Ji-yoon support
Why is this important?
Self-advocacy To enhance her decision making ability.
Empowerment To speak for what she needs.
Active support Because she gets frustrated when being neglected.
Active listening She feels that she is not being understood and gets frustrated.
Part 5-
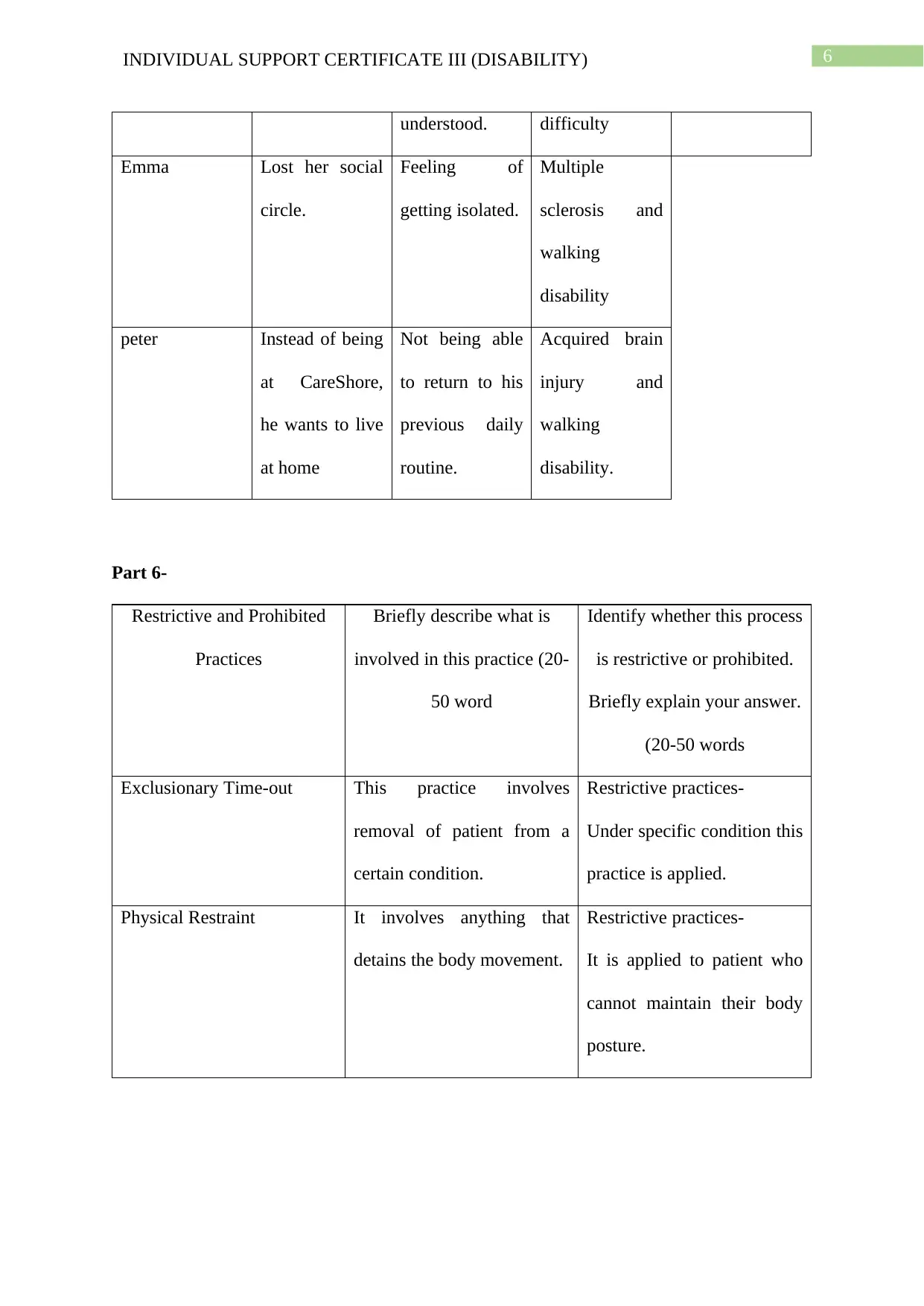
Individual
receiving
support
Environmental
factor (one for
each client)
Emotional
factor (one for
each client)
Physical or
health factor
(one for each
client)
Medication
concern (for Ji-
yoon only)
Ji-yoon Moved to new
place.
Feeling of not
being
mobility and
learning
Takes medicine
for epilepsy.
D. During Ji-yoon’s initial outburst, she hit Julie on the side of her face with her arm and
also started screaming and thrashing. To ensure safety of herself as well as ji-yoon,
she should follow CareShore’s procedures.
E. Julie needs to follow CareShore’s intervention and notification procedures to avoid
such incidents in future and to confirm the safety of patients and healthcare workers
and to demonstrate the reason behind the event.
F. Ji-yoon felt that she was being neglected by Julie and hence, she started screaming
and thrashing her out of her wheel chair. After that she got irritated because she feels
that she is not being understood, which lead to her outburst.
G. The behaviour support plan of Ji-yoon should include her behaviour of getting
irritated, when she feels that she is being neglected or not being understood.
H.
Key concept in
Ji-yoon support
Why is this important?
Self-advocacy To enhance her decision making ability.
Empowerment To speak for what she needs.
Active support Because she gets frustrated when being neglected.
Active listening She feels that she is not being understood and gets frustrated.
Part 5-
Individual
receiving
support
Environmental
factor (one for
each client)
Emotional
factor (one for
each client)
Physical or
health factor
(one for each
client)
Medication
concern (for Ji-
yoon only)
Ji-yoon Moved to new
place.
Feeling of not
being
mobility and
learning
Takes medicine
for epilepsy.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
understood. difficulty
Emma Lost her social
circle.
Feeling of
getting isolated.
Multiple
sclerosis and
walking
disability
peter Instead of being
at CareShore,
he wants to live
at home
Not being able
to return to his
previous daily
routine.
Acquired brain
injury and
walking
disability.
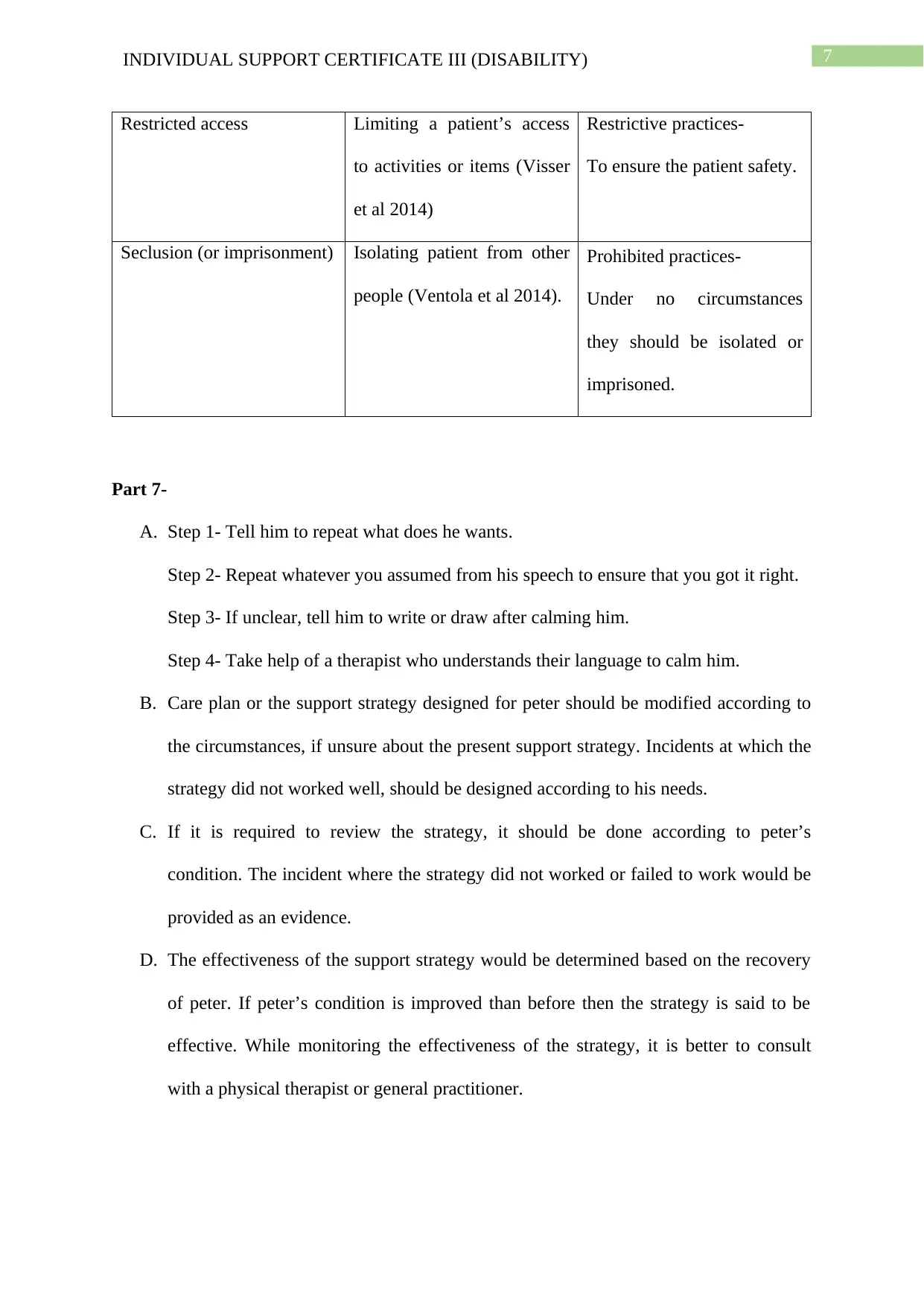
Part 6-
Restrictive and Prohibited
Practices
Briefly describe what is
involved in this practice (20-
50 word
Identify whether this process
is restrictive or prohibited.
Briefly explain your answer.
(20-50 words
Exclusionary Time-out This practice involves
removal of patient from a
certain condition.
Restrictive practices-
Under specific condition this
practice is applied.
Physical Restraint It involves anything that
detains the body movement.
Restrictive practices-
It is applied to patient who
cannot maintain their body
posture.
understood. difficulty
Emma Lost her social
circle.
Feeling of
getting isolated.
Multiple
sclerosis and
walking
disability
peter Instead of being
at CareShore,
he wants to live
at home
Not being able
to return to his
previous daily
routine.
Acquired brain
injury and
walking
disability.
Part 6-
Restrictive and Prohibited
Practices
Briefly describe what is
involved in this practice (20-
50 word
Identify whether this process
is restrictive or prohibited.
Briefly explain your answer.
(20-50 words
Exclusionary Time-out This practice involves
removal of patient from a
certain condition.
Restrictive practices-
Under specific condition this
practice is applied.
Physical Restraint It involves anything that
detains the body movement.
Restrictive practices-
It is applied to patient who
cannot maintain their body
posture.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Restricted access Limiting a patient’s access
to activities or items (Visser
et al 2014)
Restrictive practices-
To ensure the patient safety.
Seclusion (or imprisonment) Isolating patient from other
people (Ventola et al 2014).
Prohibited practices-
Under no circumstances
they should be isolated or
imprisoned.
Part 7-
A. Step 1- Tell him to repeat what does he wants.
Step 2- Repeat whatever you assumed from his speech to ensure that you got it right.
Step 3- If unclear, tell him to write or draw after calming him.
Step 4- Take help of a therapist who understands their language to calm him.
B. Care plan or the support strategy designed for peter should be modified according to
the circumstances, if unsure about the present support strategy. Incidents at which the
strategy did not worked well, should be designed according to his needs.
C. If it is required to review the strategy, it should be done according to peter’s
condition. The incident where the strategy did not worked or failed to work would be
provided as an evidence.
D. The effectiveness of the support strategy would be determined based on the recovery
of peter. If peter’s condition is improved than before then the strategy is said to be
effective. While monitoring the effectiveness of the strategy, it is better to consult
with a physical therapist or general practitioner.
Restricted access Limiting a patient’s access
to activities or items (Visser
et al 2014)
Restrictive practices-
To ensure the patient safety.
Seclusion (or imprisonment) Isolating patient from other
people (Ventola et al 2014).
Prohibited practices-
Under no circumstances
they should be isolated or
imprisoned.
Part 7-
A. Step 1- Tell him to repeat what does he wants.
Step 2- Repeat whatever you assumed from his speech to ensure that you got it right.
Step 3- If unclear, tell him to write or draw after calming him.
Step 4- Take help of a therapist who understands their language to calm him.
B. Care plan or the support strategy designed for peter should be modified according to
the circumstances, if unsure about the present support strategy. Incidents at which the
strategy did not worked well, should be designed according to his needs.
C. If it is required to review the strategy, it should be done according to peter’s
condition. The incident where the strategy did not worked or failed to work would be
provided as an evidence.
D. The effectiveness of the support strategy would be determined based on the recovery
of peter. If peter’s condition is improved than before then the strategy is said to be
effective. While monitoring the effectiveness of the strategy, it is better to consult
with a physical therapist or general practitioner.
8INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
Part 8-
A. Her condition will be reported to her family and friends.
B. I will make her family and friends understand that, there is something which is
bothering her and making her depressed. She is not eating anything and appears
unhappy. She is not even talking with anyone and does not want to live anymore.
C.
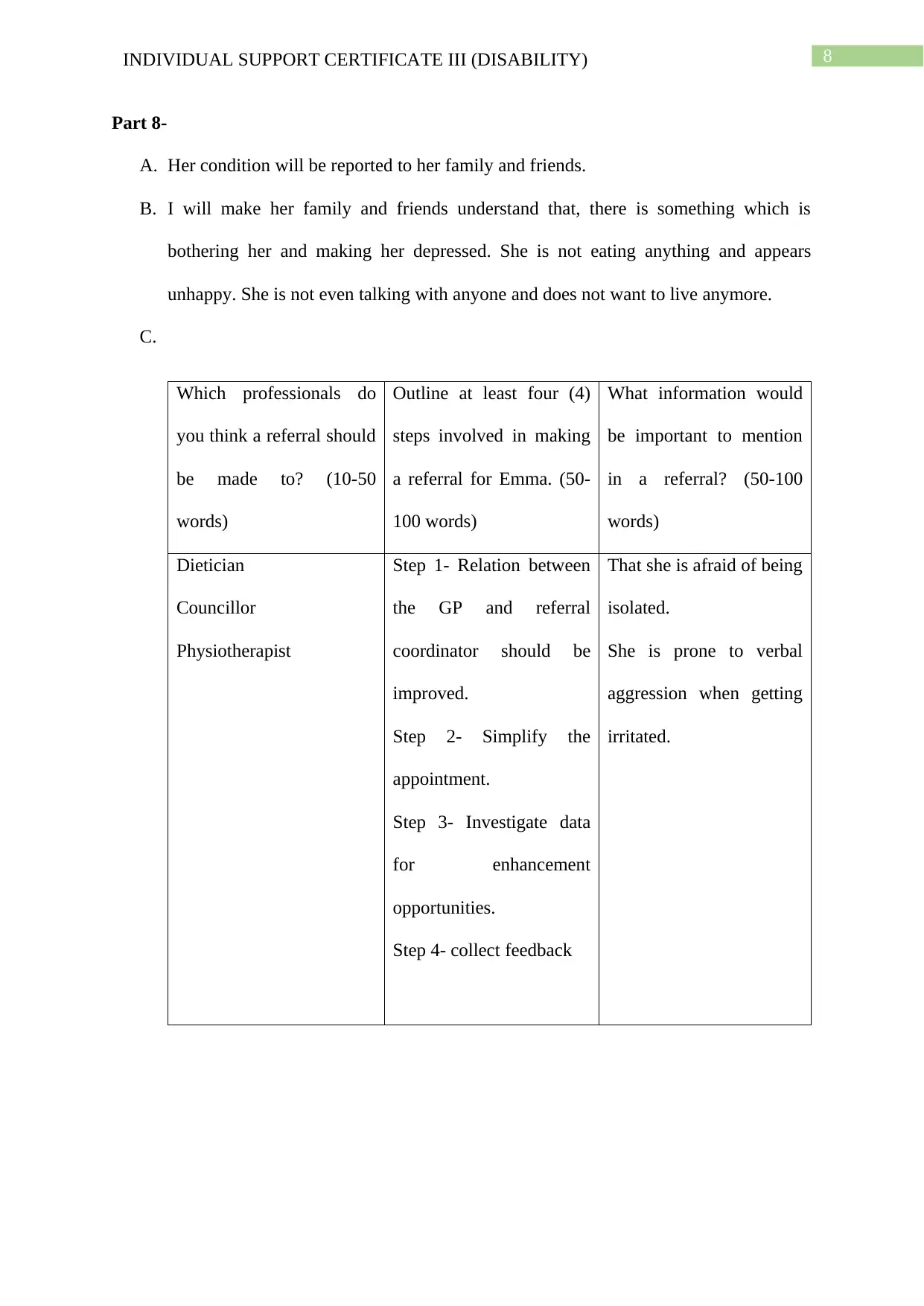
Which professionals do
you think a referral should
be made to? (10-50
words)
Outline at least four (4)
steps involved in making
a referral for Emma. (50-
100 words)
What information would
be important to mention
in a referral? (50-100
words)
Dietician
Councillor
Physiotherapist
Step 1- Relation between
the GP and referral
coordinator should be
improved.
Step 2- Simplify the
appointment.
Step 3- Investigate data
for enhancement
opportunities.
Step 4- collect feedback
That she is afraid of being
isolated.
She is prone to verbal
aggression when getting
irritated.
Part 8-
A. Her condition will be reported to her family and friends.
B. I will make her family and friends understand that, there is something which is
bothering her and making her depressed. She is not eating anything and appears
unhappy. She is not even talking with anyone and does not want to live anymore.
C.
Which professionals do
you think a referral should
be made to? (10-50
words)
Outline at least four (4)
steps involved in making
a referral for Emma. (50-
100 words)
What information would
be important to mention
in a referral? (50-100
words)
Dietician
Councillor
Physiotherapist
Step 1- Relation between
the GP and referral
coordinator should be
improved.
Step 2- Simplify the
appointment.
Step 3- Investigate data
for enhancement
opportunities.
Step 4- collect feedback
That she is afraid of being
isolated.
She is prone to verbal
aggression when getting
irritated.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9INDIVIDUAL SUPPORT CERTIFICATE III (DISABILITY)
References
Gifford, R. and Nilsson, A., 2014. Personal and social factors that influence pro‐
environmental concern and behaviour: A review. International Journal of Psychology, 49(3),
pp.141-157.
Hassiotis, A., Strydom, A., Crawford, M., Hall, I., Omar, R., Vickerstaff, V., Hunter, R.,
Crabtree, J., Cooper, V., Biswas, A. and Howie, W., 2014. Clinical and cost effectiveness of
staff training in Positive Behaviour Support (PBS) for treating challenging behaviour in
adults with intellectual disability: a cluster randomised controlled trial. BMC psychiatry,
14(1), p.219.
Ventola, C.L., 2014. Social media and health care professionals: benefits, risks, and best
practices. Pharmacy and Therapeutics, 39(7), p.491.
Visser, S.N., Danielson, M.L., Bitsko, R.H., Holbrook, J.R., Kogan, M.D., Ghandour, R.M.,
Perou, R. and Blumberg, S.J., 2014. Trends in the parent-report of health care provider-
diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011.
Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), pp.34-46.
Wiseman, F.K., Al-Janabi, T., Hardy, J., Karmiloff-Smith, A., Nizetic, D., Tybulewicz, V.L.,
Fisher, E.M. and Strydom, A., 2015. A genetic cause of Alzheimer disease: mechanistic
insights from Down syndrome. Nature Reviews Neuroscience, 16(9), p.564.
References
Gifford, R. and Nilsson, A., 2014. Personal and social factors that influence pro‐
environmental concern and behaviour: A review. International Journal of Psychology, 49(3),
pp.141-157.
Hassiotis, A., Strydom, A., Crawford, M., Hall, I., Omar, R., Vickerstaff, V., Hunter, R.,
Crabtree, J., Cooper, V., Biswas, A. and Howie, W., 2014. Clinical and cost effectiveness of
staff training in Positive Behaviour Support (PBS) for treating challenging behaviour in
adults with intellectual disability: a cluster randomised controlled trial. BMC psychiatry,
14(1), p.219.
Ventola, C.L., 2014. Social media and health care professionals: benefits, risks, and best
practices. Pharmacy and Therapeutics, 39(7), p.491.
Visser, S.N., Danielson, M.L., Bitsko, R.H., Holbrook, J.R., Kogan, M.D., Ghandour, R.M.,
Perou, R. and Blumberg, S.J., 2014. Trends in the parent-report of health care provider-
diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011.
Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), pp.34-46.
Wiseman, F.K., Al-Janabi, T., Hardy, J., Karmiloff-Smith, A., Nizetic, D., Tybulewicz, V.L.,
Fisher, E.M. and Strydom, A., 2015. A genetic cause of Alzheimer disease: mechanistic
insights from Down syndrome. Nature Reviews Neuroscience, 16(9), p.564.
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.