Cervical Cancer: Treatment, Management, Screening, and Risk Factors
VerifiedAdded on 2023/03/31
|13
|2481
|291
Essay
AI Summary
This essay provides a comprehensive overview of cervical cancer, a significant health concern affecting women globally. It begins by defining cervical cancer and its prevalence, then delves into its macroscopic appearance, including Nabothian cysts and cervical ectopy, as well as its microscopic features, distinguishing between adenocarcinoma and squamous cell carcinoma. The essay explores the management of cervical cancer, discussing treatment options such as surgery, radiotherapy, chemotherapy, and the importance of accurate staging. It also covers screening methods like the Pap test and HPV testing, along with risk factors such as HPV infection, socioeconomic status, and age. The pathogenesis of cervical cancer, including its different stages and survival rates, is also examined. Finally, the essay highlights prevention strategies, particularly HPV vaccination, and emphasizes the importance of early screening and lifestyle modifications to combat the disease.

Student name
Student No.
Unit
Title: Treatment and Management of Cervical Cancer
Student No.
Unit
Title: Treatment and Management of Cervical Cancer
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
According to Makuza et al. (2015), cervical cancer is 4th leading form of cancer affection
women. It is also the 2nd most prevalent form of cancer among women aged between 15 and 44.
According to a research conducted in 2012, there were 528 000 cases of cervical cancer. Among
these cases, 266 000 died, with more than 70 percent of these deaths being reported in the
developing nations. According to Ntekim (2012) a large number of women living with cervical
cancer in the Sub-Saharan Africa are in the rural areas, with their population accounting for 22.5
percent of cancer cases.
Macroscopic appearance of cervical cancer
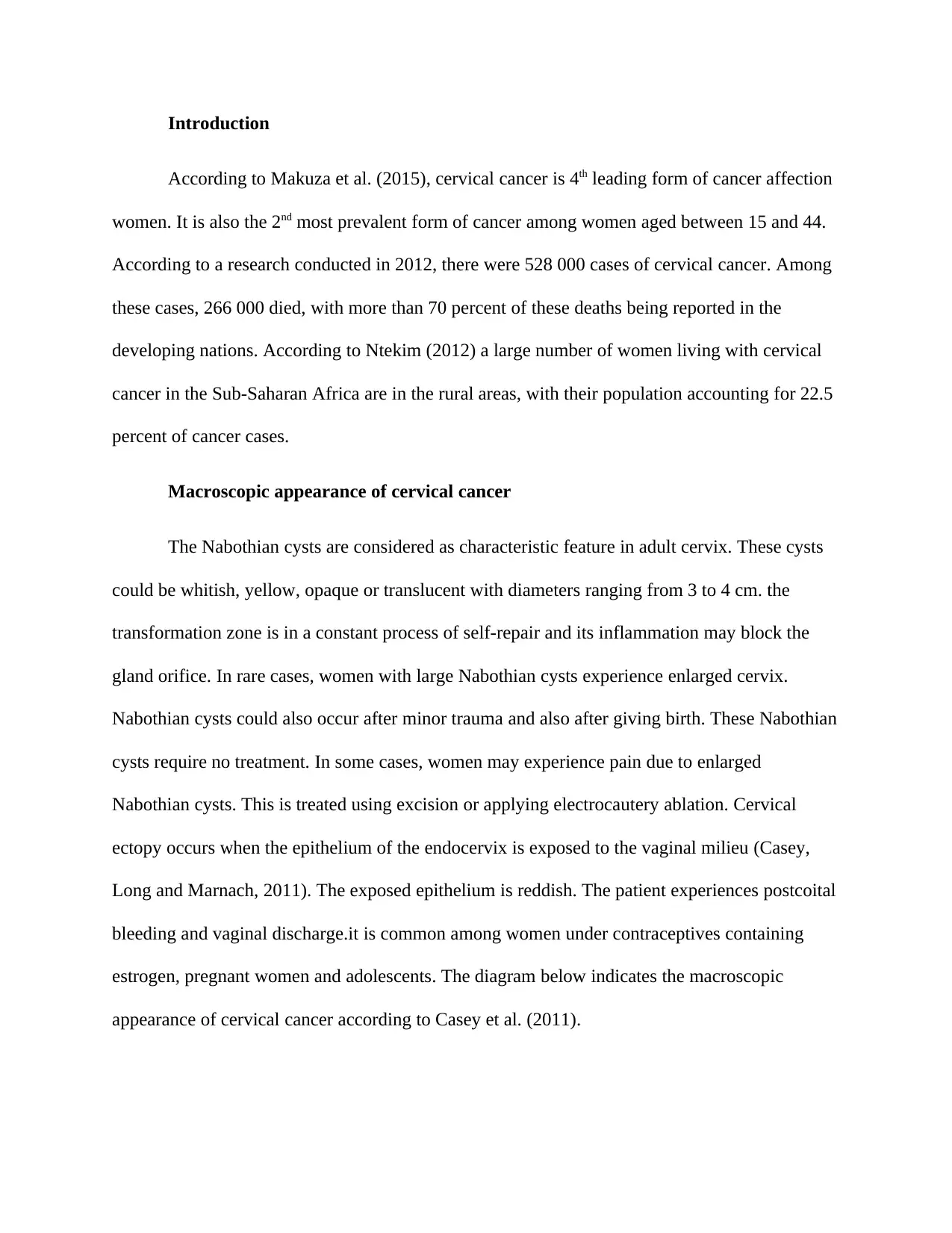
The Nabothian cysts are considered as characteristic feature in adult cervix. These cysts
could be whitish, yellow, opaque or translucent with diameters ranging from 3 to 4 cm. the
transformation zone is in a constant process of self-repair and its inflammation may block the
gland orifice. In rare cases, women with large Nabothian cysts experience enlarged cervix.
Nabothian cysts could also occur after minor trauma and also after giving birth. These Nabothian
cysts require no treatment. In some cases, women may experience pain due to enlarged
Nabothian cysts. This is treated using excision or applying electrocautery ablation. Cervical
ectopy occurs when the epithelium of the endocervix is exposed to the vaginal milieu (Casey,
Long and Marnach, 2011). The exposed epithelium is reddish. The patient experiences postcoital
bleeding and vaginal discharge.it is common among women under contraceptives containing
estrogen, pregnant women and adolescents. The diagram below indicates the macroscopic
appearance of cervical cancer according to Casey et al. (2011).
According to Makuza et al. (2015), cervical cancer is 4th leading form of cancer affection
women. It is also the 2nd most prevalent form of cancer among women aged between 15 and 44.
According to a research conducted in 2012, there were 528 000 cases of cervical cancer. Among
these cases, 266 000 died, with more than 70 percent of these deaths being reported in the
developing nations. According to Ntekim (2012) a large number of women living with cervical
cancer in the Sub-Saharan Africa are in the rural areas, with their population accounting for 22.5
percent of cancer cases.
Macroscopic appearance of cervical cancer
The Nabothian cysts are considered as characteristic feature in adult cervix. These cysts
could be whitish, yellow, opaque or translucent with diameters ranging from 3 to 4 cm. the
transformation zone is in a constant process of self-repair and its inflammation may block the
gland orifice. In rare cases, women with large Nabothian cysts experience enlarged cervix.
Nabothian cysts could also occur after minor trauma and also after giving birth. These Nabothian
cysts require no treatment. In some cases, women may experience pain due to enlarged
Nabothian cysts. This is treated using excision or applying electrocautery ablation. Cervical
ectopy occurs when the epithelium of the endocervix is exposed to the vaginal milieu (Casey,
Long and Marnach, 2011). The exposed epithelium is reddish. The patient experiences postcoital
bleeding and vaginal discharge.it is common among women under contraceptives containing
estrogen, pregnant women and adolescents. The diagram below indicates the macroscopic
appearance of cervical cancer according to Casey et al. (2011).
Microscopic appearance of the lesion
According to the American Cancer Society (2018), cancer can attack any part of the body
then spread to other body parts. Cancer starts with the uncontrollable growth of body cells. They
claim that cervical cancer starts at the uterine cervix. Research on cervical cancer has shown that
most cervical cancers begin at cells around the transformation zone (the region where the
endocervix meets the exocervix). According to Lee et al. (2015), cervical cancer begins when the
cervical cell lining starts to have abnormal changes. After sometime these cells either become
cancerous or return to their normal state. The American Cancer Association (2018) say that cells
do not suddenly become cancerous but undergo pre-cancerous changes which later turn to
cancer. These changes are squamous intraepithelial lesion, dysplasia and cervical intraepithelial
neoplasia. Lee et al. (2015) claim that most women do not develop cervical cancer due to
abnormality of these cells. Cervical cancer is divided in to adenocarcinoma and squamous cell
carcinoma, with both well distinguishable as per the appearance of the cancerous cells under a
microscope. The squamous cell carcinoma attacks the thin flat lining of the cervical cells.
According to the American Cancer Society (2018), cancer can attack any part of the body
then spread to other body parts. Cancer starts with the uncontrollable growth of body cells. They
claim that cervical cancer starts at the uterine cervix. Research on cervical cancer has shown that
most cervical cancers begin at cells around the transformation zone (the region where the
endocervix meets the exocervix). According to Lee et al. (2015), cervical cancer begins when the
cervical cell lining starts to have abnormal changes. After sometime these cells either become
cancerous or return to their normal state. The American Cancer Association (2018) say that cells
do not suddenly become cancerous but undergo pre-cancerous changes which later turn to
cancer. These changes are squamous intraepithelial lesion, dysplasia and cervical intraepithelial
neoplasia. Lee et al. (2015) claim that most women do not develop cervical cancer due to
abnormality of these cells. Cervical cancer is divided in to adenocarcinoma and squamous cell
carcinoma, with both well distinguishable as per the appearance of the cancerous cells under a
microscope. The squamous cell carcinoma attacks the thin flat lining of the cervical cells.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
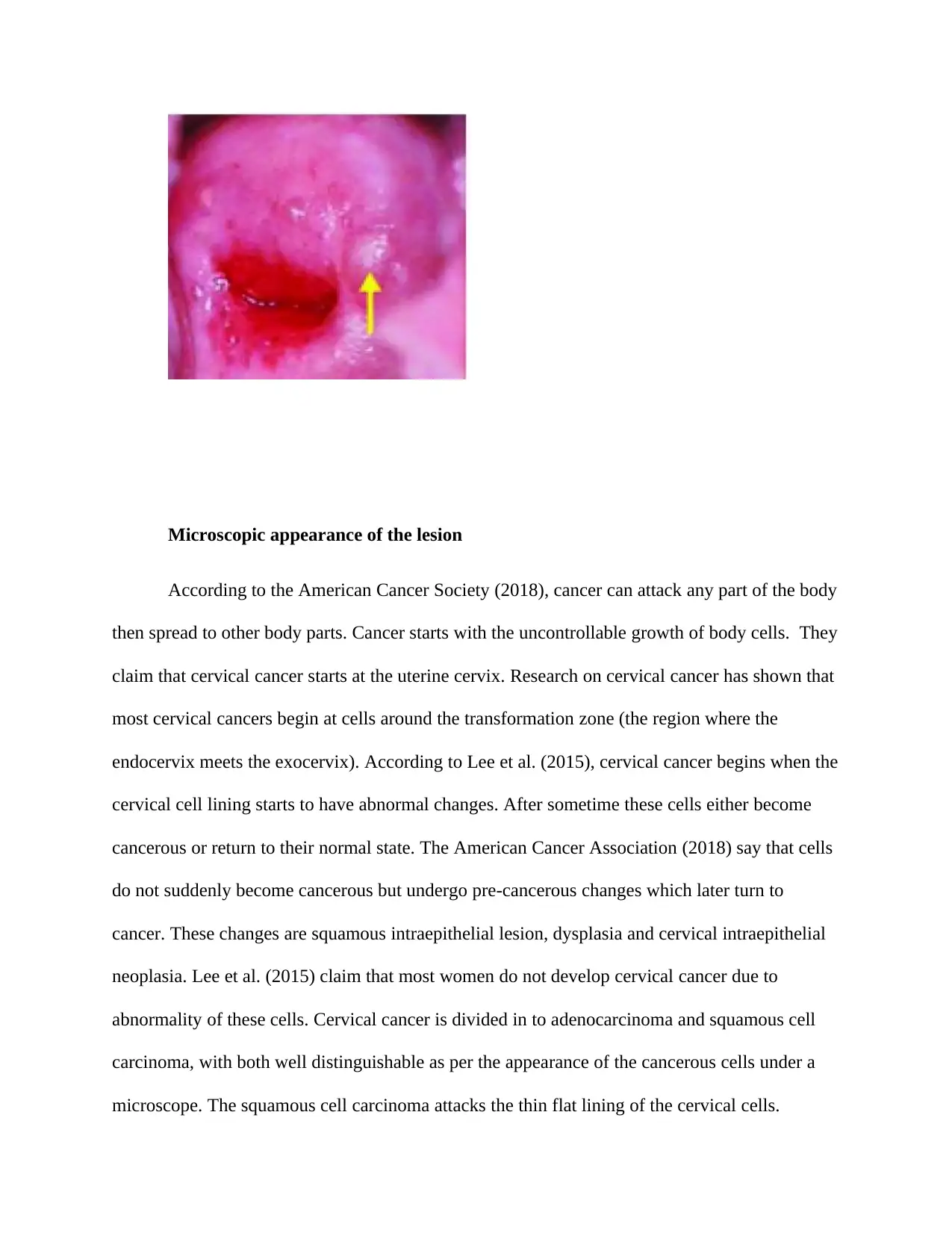
Squamous cell carcinoma is linked with more than 80 percent of all cases of this lesion.
Adenocarcinomas is associated with about 20 percent of all cases of this lesion. It commonly
affects the glandular cells lining the upper part of the cervix. The following images show the
appearances of both adenocarcinoma and squamous cell carcinoma under a microscope (courtesy
of Maniar and Wei, 2017)
Squamous cell carcinoma
Adenocarcinoma
According to Martin (2018), cervical cancer is triggered by a certain type of virus. The
human papillomavirus (HPV) is a group of virus (more than 40 types) is linked with cervical
cancer. Research indicates that almost 90 percent of lesion is caused by the HPV. At its fists
stages, there are hardly any signs but as it progresses the following symptoms are seen, abnormal
discharge of the vaginal, after menopause bleeding and pain or bleeding during sex. Below is an
image showing the microscopic appearance of the cervical cancer lesion according to Martin
(2018)
Adenocarcinomas is associated with about 20 percent of all cases of this lesion. It commonly
affects the glandular cells lining the upper part of the cervix. The following images show the
appearances of both adenocarcinoma and squamous cell carcinoma under a microscope (courtesy
of Maniar and Wei, 2017)
Squamous cell carcinoma
Adenocarcinoma
According to Martin (2018), cervical cancer is triggered by a certain type of virus. The
human papillomavirus (HPV) is a group of virus (more than 40 types) is linked with cervical
cancer. Research indicates that almost 90 percent of lesion is caused by the HPV. At its fists
stages, there are hardly any signs but as it progresses the following symptoms are seen, abnormal
discharge of the vaginal, after menopause bleeding and pain or bleeding during sex. Below is an
image showing the microscopic appearance of the cervical cancer lesion according to Martin
(2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Management of cervical cancer
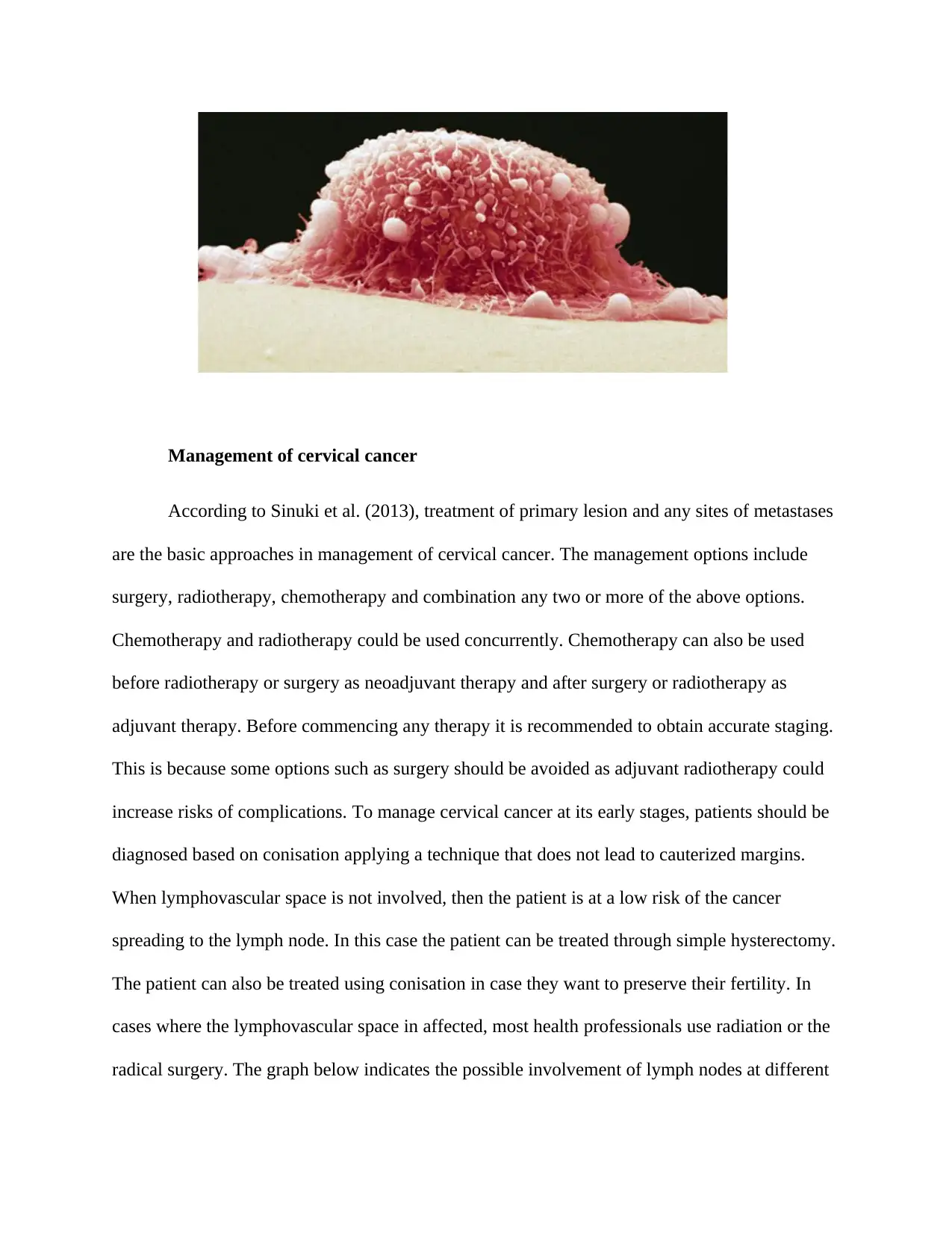
According to Sinuki et al. (2013), treatment of primary lesion and any sites of metastases
are the basic approaches in management of cervical cancer. The management options include
surgery, radiotherapy, chemotherapy and combination any two or more of the above options.
Chemotherapy and radiotherapy could be used concurrently. Chemotherapy can also be used
before radiotherapy or surgery as neoadjuvant therapy and after surgery or radiotherapy as
adjuvant therapy. Before commencing any therapy it is recommended to obtain accurate staging.
This is because some options such as surgery should be avoided as adjuvant radiotherapy could
increase risks of complications. To manage cervical cancer at its early stages, patients should be
diagnosed based on conisation applying a technique that does not lead to cauterized margins.
When lymphovascular space is not involved, then the patient is at a low risk of the cancer
spreading to the lymph node. In this case the patient can be treated through simple hysterectomy.
The patient can also be treated using conisation in case they want to preserve their fertility. In
cases where the lymphovascular space in affected, most health professionals use radiation or the
radical surgery. The graph below indicates the possible involvement of lymph nodes at different
According to Sinuki et al. (2013), treatment of primary lesion and any sites of metastases
are the basic approaches in management of cervical cancer. The management options include
surgery, radiotherapy, chemotherapy and combination any two or more of the above options.
Chemotherapy and radiotherapy could be used concurrently. Chemotherapy can also be used
before radiotherapy or surgery as neoadjuvant therapy and after surgery or radiotherapy as
adjuvant therapy. Before commencing any therapy it is recommended to obtain accurate staging.
This is because some options such as surgery should be avoided as adjuvant radiotherapy could
increase risks of complications. To manage cervical cancer at its early stages, patients should be
diagnosed based on conisation applying a technique that does not lead to cauterized margins.
When lymphovascular space is not involved, then the patient is at a low risk of the cancer
spreading to the lymph node. In this case the patient can be treated through simple hysterectomy.
The patient can also be treated using conisation in case they want to preserve their fertility. In
cases where the lymphovascular space in affected, most health professionals use radiation or the
radical surgery. The graph below indicates the possible involvement of lymph nodes at different
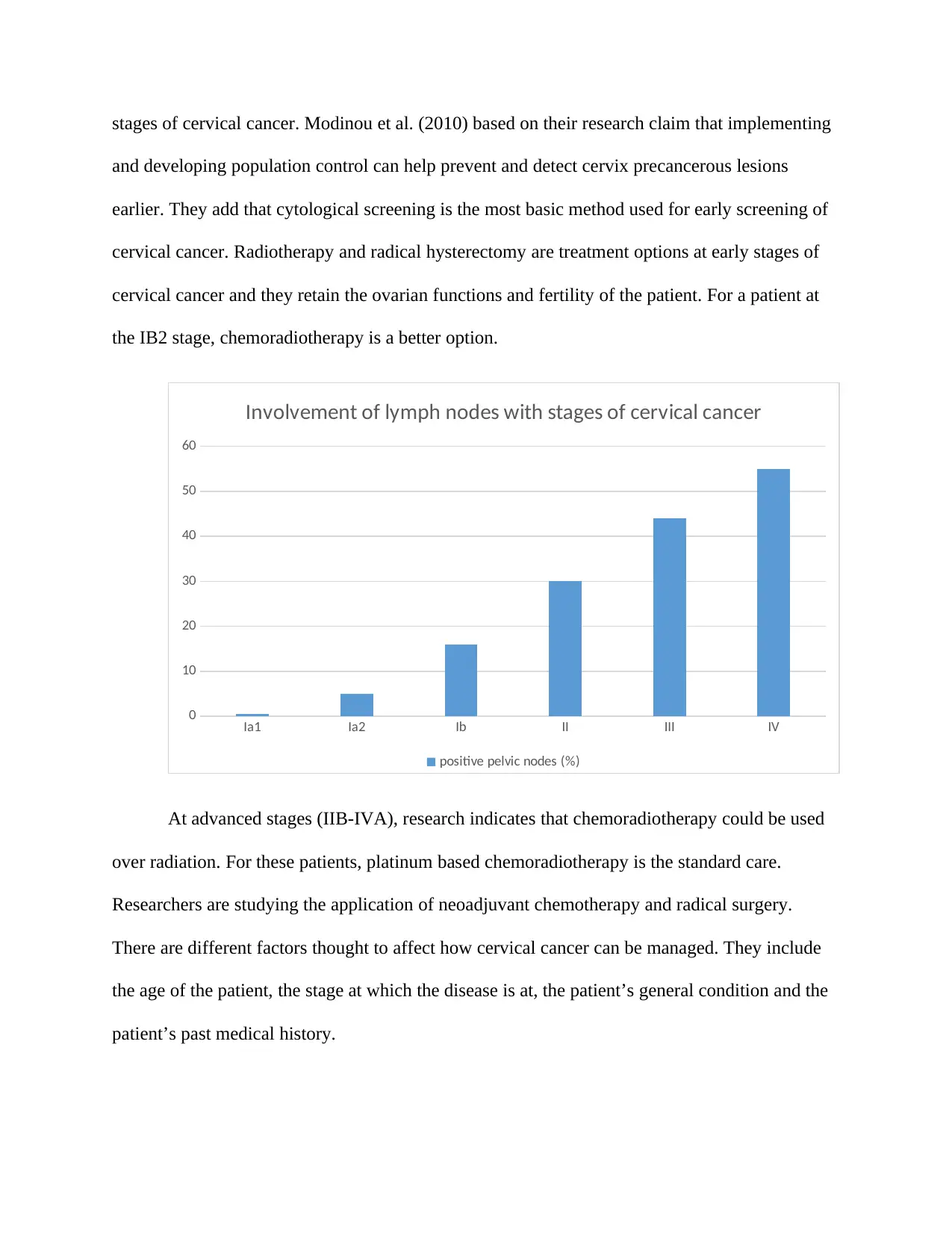
stages of cervical cancer. Modinou et al. (2010) based on their research claim that implementing
and developing population control can help prevent and detect cervix precancerous lesions
earlier. They add that cytological screening is the most basic method used for early screening of
cervical cancer. Radiotherapy and radical hysterectomy are treatment options at early stages of
cervical cancer and they retain the ovarian functions and fertility of the patient. For a patient at
the IB2 stage, chemoradiotherapy is a better option.
Ia1 Ia2 Ib II III IV
0
10
20
30
40
50
60
Involvement of lymph nodes with stages of cervical cancer
positive pelvic nodes (%)
At advanced stages (IIB-IVA), research indicates that chemoradiotherapy could be used
over radiation. For these patients, platinum based chemoradiotherapy is the standard care.
Researchers are studying the application of neoadjuvant chemotherapy and radical surgery.
There are different factors thought to affect how cervical cancer can be managed. They include
the age of the patient, the stage at which the disease is at, the patient’s general condition and the
patient’s past medical history.
and developing population control can help prevent and detect cervix precancerous lesions
earlier. They add that cytological screening is the most basic method used for early screening of
cervical cancer. Radiotherapy and radical hysterectomy are treatment options at early stages of
cervical cancer and they retain the ovarian functions and fertility of the patient. For a patient at
the IB2 stage, chemoradiotherapy is a better option.
Ia1 Ia2 Ib II III IV
0
10
20
30
40
50
60
Involvement of lymph nodes with stages of cervical cancer
positive pelvic nodes (%)
At advanced stages (IIB-IVA), research indicates that chemoradiotherapy could be used
over radiation. For these patients, platinum based chemoradiotherapy is the standard care.
Researchers are studying the application of neoadjuvant chemotherapy and radical surgery.
There are different factors thought to affect how cervical cancer can be managed. They include
the age of the patient, the stage at which the disease is at, the patient’s general condition and the
patient’s past medical history.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Screening of cervical cancer
The Pap test is a traditional method of detecting the presence of human papillomavirus. It
is used for patients above 30 years. This test detects any high risk HPV in cervical cancer. There
are different guidelines for cervical cancer screening according to WHO (2013). These
guidelines include, a woman should start lesion screening with Pap test at the age of 21. For
patients above 30, there are 3 options for them, the next Pap test should be carried out after every
3 years, an HPV test alone should be undertaken after every 5 years and co-testing using both
HPV test and Pap test should be after every 5 years. Depending on the Pap and HPV test results,
the health practitioner may recommend additional procedures or screening. Over the years, the
application of the Pap test has recorded tremendous improvements in fighting against cervical
cancer. It is however faced with some challenges such as lack of resources, trained health
professionals and other infrastructure in developing nations. The Pap test is subjective and
requires frequent screening hence increasing the cost of its application. Just like the Pap test,
HPV test is used to detect presence of HPV. Just like the Pap test, this method applies collecting
cervical cells using a certain soft brush, then the collected cells are taken to the lab.
There are however other method that have been applied in treatment of precancerous and
cancerous cervical lesions. These include visual inspection with acetic acid, HPV DNA testing
and cryotherapy. The visual inspection using acetic acid (VIA) can be carried out in the clinic
hence eliminating the need for a laboratory. HPV DNA test is used in detecting types of HPV in
the vaginal and cervical cells (Kassa, 2018). This method is recommended for patients above 30
years. HPV DNA test is considered among the most sensitive methods in detection of abnormal
precancerous lesions. It is a sensitivity of between 67 and 96 percent.
The Pap test is a traditional method of detecting the presence of human papillomavirus. It
is used for patients above 30 years. This test detects any high risk HPV in cervical cancer. There
are different guidelines for cervical cancer screening according to WHO (2013). These
guidelines include, a woman should start lesion screening with Pap test at the age of 21. For
patients above 30, there are 3 options for them, the next Pap test should be carried out after every
3 years, an HPV test alone should be undertaken after every 5 years and co-testing using both
HPV test and Pap test should be after every 5 years. Depending on the Pap and HPV test results,
the health practitioner may recommend additional procedures or screening. Over the years, the
application of the Pap test has recorded tremendous improvements in fighting against cervical
cancer. It is however faced with some challenges such as lack of resources, trained health
professionals and other infrastructure in developing nations. The Pap test is subjective and
requires frequent screening hence increasing the cost of its application. Just like the Pap test,
HPV test is used to detect presence of HPV. Just like the Pap test, this method applies collecting
cervical cells using a certain soft brush, then the collected cells are taken to the lab.
There are however other method that have been applied in treatment of precancerous and
cancerous cervical lesions. These include visual inspection with acetic acid, HPV DNA testing
and cryotherapy. The visual inspection using acetic acid (VIA) can be carried out in the clinic
hence eliminating the need for a laboratory. HPV DNA test is used in detecting types of HPV in
the vaginal and cervical cells (Kassa, 2018). This method is recommended for patients above 30
years. HPV DNA test is considered among the most sensitive methods in detection of abnormal
precancerous lesions. It is a sensitivity of between 67 and 96 percent.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Risk factors for the lesion
According to Makuza et al. (2015) the following factors increase the risk of a woman
contracting this lesion. HPV infection is the leading in causing this type of cancer. The American
Cancer Society (2018) claim that there are more than 150 HPV types that could cause the lesion,
with HPV16 and HPV18 being the leading causes. Women with low immunity are at a high risk
of contracting the lesion. Low immunity could as a result of organ transplant, HIV or
suppression from corticosteroid medications. Socioeconomic status of an individual could be a
factor especially when one is unable to access cervical cancer screening due to their
socioeconomic status. Oral contraceptives are associated with an increasing risk of this disease
though these studies do not explain how the two are related. Age is a risk factor for this lesion
with girls below 15 years having a low risk of contractin this cancer (Teame et al. 2018). As the
age advances, the risk increases with those aged above 40 being at a higher risk and hence need
regular cervical cancer screening. Other risk factors include exposure to diethylstilbestrol,
smoking, herpes, chlamydia infection, obesity, history of this cancer in the family and use of
intrauterine device.
Pathogenesis of cervical cancer
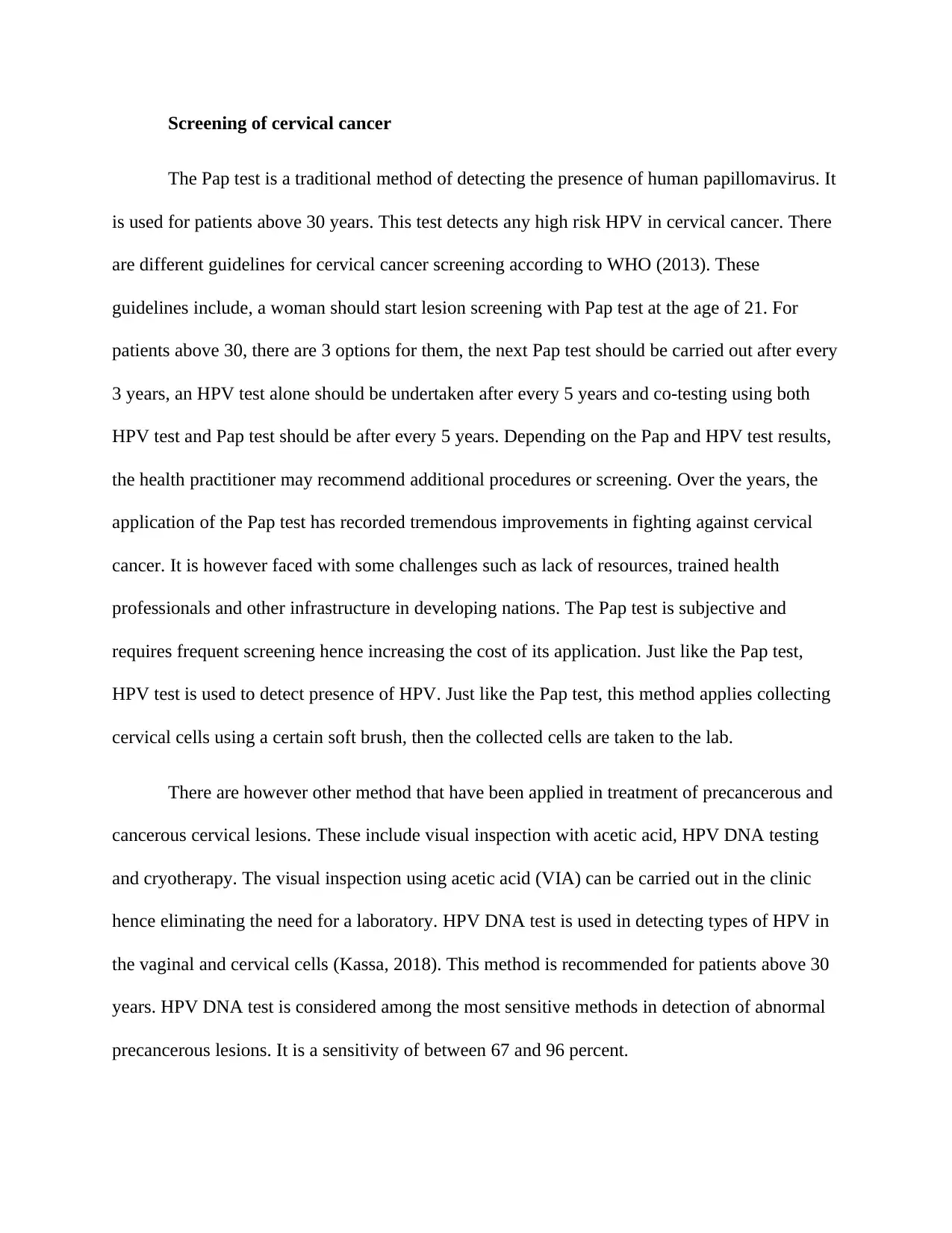
Studies on HPV carcinogenesis has shown the mechanism of HPV replication, cells
transformation and how the virus invades the patient’s immune system. There are different
developmental stages of the disease. Stage Ia1 is the first stage, whereby the tumor has spread to
a depth of not more than 3 mm and has spread to less than 7 mm horizontally (Ibeanu, 2011). in
stage Ia2 the tumour has spread to a depth greater than 3mm but less than 5 mm. the nest stages
are stages Ib1- IIa, whereby the lesions has reached the upper vagina is greater than Ia2. In stages
IIb, IIIa, IIIb and IVa, the lesions has spread to neighbouring organs. The other stage of this
According to Makuza et al. (2015) the following factors increase the risk of a woman
contracting this lesion. HPV infection is the leading in causing this type of cancer. The American
Cancer Society (2018) claim that there are more than 150 HPV types that could cause the lesion,
with HPV16 and HPV18 being the leading causes. Women with low immunity are at a high risk
of contracting the lesion. Low immunity could as a result of organ transplant, HIV or
suppression from corticosteroid medications. Socioeconomic status of an individual could be a
factor especially when one is unable to access cervical cancer screening due to their
socioeconomic status. Oral contraceptives are associated with an increasing risk of this disease
though these studies do not explain how the two are related. Age is a risk factor for this lesion
with girls below 15 years having a low risk of contractin this cancer (Teame et al. 2018). As the
age advances, the risk increases with those aged above 40 being at a higher risk and hence need
regular cervical cancer screening. Other risk factors include exposure to diethylstilbestrol,
smoking, herpes, chlamydia infection, obesity, history of this cancer in the family and use of
intrauterine device.
Pathogenesis of cervical cancer
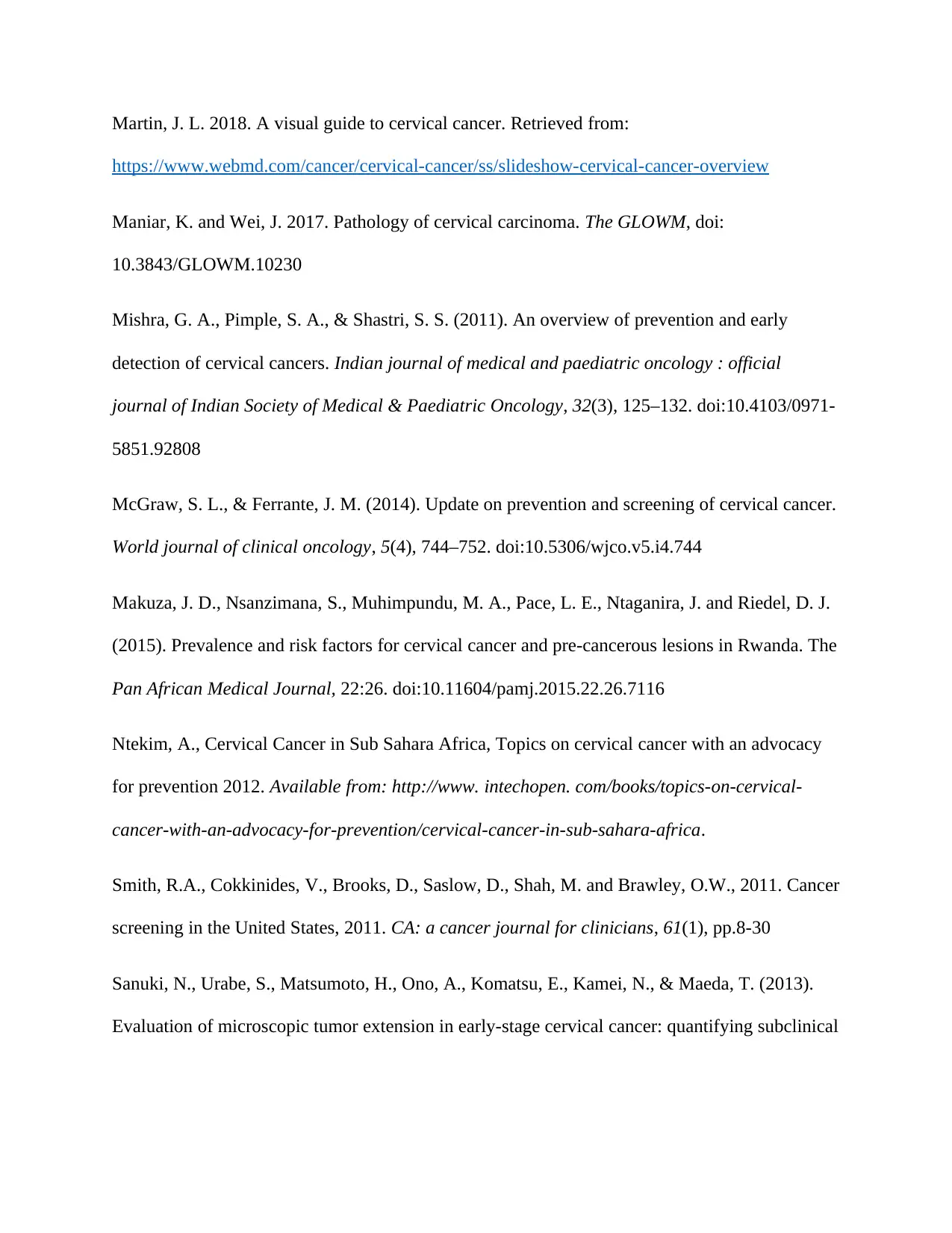
Studies on HPV carcinogenesis has shown the mechanism of HPV replication, cells
transformation and how the virus invades the patient’s immune system. There are different
developmental stages of the disease. Stage Ia1 is the first stage, whereby the tumor has spread to
a depth of not more than 3 mm and has spread to less than 7 mm horizontally (Ibeanu, 2011). in
stage Ia2 the tumour has spread to a depth greater than 3mm but less than 5 mm. the nest stages
are stages Ib1- IIa, whereby the lesions has reached the upper vagina is greater than Ia2. In stages
IIb, IIIa, IIIb and IVa, the lesions has spread to neighbouring organs. The other stage of this
disease is stage IVb. There is no standard therapy and treatment for this stage just palliative care
for the patient (Castle et al. 2017). The graph below indicates the chances of survival at every
stage of cervical cancer (courtesy of Castle et al. 2017).
Ia1 Ia2 Ib1 Ib2 IIA Iib IIIa IIIb Iva Ivb
0
20
40
60
80
100
120
Chances of surviving cervical cancer at every stage
overal survival in 5 years (%)
Prevention of the lesion
HPV vaccination is used in the lesions prevention. This vaccine is designed to prevent the
action of HPV and any cervical carcinogenesis thereof (McGraw and Ferrante, 2014). Most
important this vaccine prevents infections by HPV6, HPV11, HPV16 and HPV18. It is given in
three vaccinations (0, 1st or 2nd month the at the 6th month) to females between the age of 9 and
26 (Choi et al. 2012). According to Mishra, Pimple and Shastri (2011), regular screening and
timely follow up are recommended. The American Cancer Society (2018) recommends that
for the patient (Castle et al. 2017). The graph below indicates the chances of survival at every
stage of cervical cancer (courtesy of Castle et al. 2017).
Ia1 Ia2 Ib1 Ib2 IIA Iib IIIa IIIb Iva Ivb
0
20
40
60
80
100
120
Chances of surviving cervical cancer at every stage
overal survival in 5 years (%)
Prevention of the lesion
HPV vaccination is used in the lesions prevention. This vaccine is designed to prevent the
action of HPV and any cervical carcinogenesis thereof (McGraw and Ferrante, 2014). Most
important this vaccine prevents infections by HPV6, HPV11, HPV16 and HPV18. It is given in
three vaccinations (0, 1st or 2nd month the at the 6th month) to females between the age of 9 and
26 (Choi et al. 2012). According to Mishra, Pimple and Shastri (2011), regular screening and
timely follow up are recommended. The American Cancer Society (2018) recommends that
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
screening of this disease should commence 3 years after initiating sexual intercourse. Women
should undergo screening annually for the first 3 years, and when the test results are normal one
can undertake the screening once in 2 or 3 years (Smith et al. 2011).
Conclusion
Cervical cancer continues to be a health pandemic in most nations, but the current
advancements in treatment and management there could be some improvement in fighting this
disease. Women are recommended to undergo early screening so that to be aware of their status.
From the discussion above it is clear that when this disease is discovered at its early staged it can
be managed. Women should also be vaccinated against this disease at the right age. They are also
encouraged to quit some lifestyle behaviors thought to lead to cervical cancer such as smoking.
should undergo screening annually for the first 3 years, and when the test results are normal one
can undertake the screening once in 2 or 3 years (Smith et al. 2011).
Conclusion
Cervical cancer continues to be a health pandemic in most nations, but the current
advancements in treatment and management there could be some improvement in fighting this
disease. Women are recommended to undergo early screening so that to be aware of their status.
From the discussion above it is clear that when this disease is discovered at its early staged it can
be managed. Women should also be vaccinated against this disease at the right age. They are also
encouraged to quit some lifestyle behaviors thought to lead to cervical cancer such as smoking.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Casey, P. M., Long, M. E., & Marnach, M. L. (2011). Abnormal cervical appearance: what to do,
when to worry?. Mayo Clinic proceedings, 86(2), 147–151. doi:10.4065/mcp.2010.0512
Choi, Y.H., Chapman, R., Gay, N. and Jit, M., 2012. Potential overestimation of HPV vaccine
impact due to unmasking of non-vaccine types: quantification using a multi-type mathematical
model. Vaccine, 30(23), pp.3383-3388.
Castle, P. E., Murokora, D., Perez, C., Alvarez, M., Quek, S. C. and Campell, C. (2017).
Treatment of cervical intraepithelial lesions. Int. J. Gynecol Obstet, 138(Suppl. 1); 20-25. Doi:
10.1002/ijgo.12191
Ibeanu, O. A. (2011) Molecular pathogenesis of cervical cancer. Cancer Biology & Therapy,
11:3, 295-306, DOI: 10.4161/cbt.11.3.14686
Kassa, R. T. 2018. Risk factors associated with precancerous cervical lesion among women
screened at Marie Stops Ethiopia, Adama town, Ethiopia 2017: a case control study. The BMC,
11:145. Doi: 10.1186/s13104-018-3244-6
Lee, J., Youm, J., Kim, J., cho, J. Y., Kim, M. A., Suh, D. and Song, Y. 2015. Identifying a low-
risk group for parametrial involvement in microscopic Stage IB1 cervical cancer using criteria
from ongoing studies and a new MRI criterion. The BMC, 15:167. Doi: 10.1186/s12885-015-
1184-2
Modinou, O., Liaropoulos, L., Kaitelidou, D., Kioulafas, K., & Theodoraki, E. M. (2011).
Management of Precancerous Lesions of the Uterine Cervix according to Demographic Data.
ISRN obstetrics and gynecology, 2011, 301680. doi:10.5402/2011/301680
Casey, P. M., Long, M. E., & Marnach, M. L. (2011). Abnormal cervical appearance: what to do,
when to worry?. Mayo Clinic proceedings, 86(2), 147–151. doi:10.4065/mcp.2010.0512
Choi, Y.H., Chapman, R., Gay, N. and Jit, M., 2012. Potential overestimation of HPV vaccine
impact due to unmasking of non-vaccine types: quantification using a multi-type mathematical
model. Vaccine, 30(23), pp.3383-3388.
Castle, P. E., Murokora, D., Perez, C., Alvarez, M., Quek, S. C. and Campell, C. (2017).
Treatment of cervical intraepithelial lesions. Int. J. Gynecol Obstet, 138(Suppl. 1); 20-25. Doi:
10.1002/ijgo.12191
Ibeanu, O. A. (2011) Molecular pathogenesis of cervical cancer. Cancer Biology & Therapy,
11:3, 295-306, DOI: 10.4161/cbt.11.3.14686
Kassa, R. T. 2018. Risk factors associated with precancerous cervical lesion among women
screened at Marie Stops Ethiopia, Adama town, Ethiopia 2017: a case control study. The BMC,
11:145. Doi: 10.1186/s13104-018-3244-6
Lee, J., Youm, J., Kim, J., cho, J. Y., Kim, M. A., Suh, D. and Song, Y. 2015. Identifying a low-
risk group for parametrial involvement in microscopic Stage IB1 cervical cancer using criteria
from ongoing studies and a new MRI criterion. The BMC, 15:167. Doi: 10.1186/s12885-015-
1184-2
Modinou, O., Liaropoulos, L., Kaitelidou, D., Kioulafas, K., & Theodoraki, E. M. (2011).
Management of Precancerous Lesions of the Uterine Cervix according to Demographic Data.
ISRN obstetrics and gynecology, 2011, 301680. doi:10.5402/2011/301680
Martin, J. L. 2018. A visual guide to cervical cancer. Retrieved from:
https://www.webmd.com/cancer/cervical-cancer/ss/slideshow-cervical-cancer-overview
Maniar, K. and Wei, J. 2017. Pathology of cervical carcinoma. The GLOWM, doi:
10.3843/GLOWM.10230
Mishra, G. A., Pimple, S. A., & Shastri, S. S. (2011). An overview of prevention and early
detection of cervical cancers. Indian journal of medical and paediatric oncology : official
journal of Indian Society of Medical & Paediatric Oncology, 32(3), 125–132. doi:10.4103/0971-
5851.92808
McGraw, S. L., & Ferrante, J. M. (2014). Update on prevention and screening of cervical cancer.
World journal of clinical oncology, 5(4), 744–752. doi:10.5306/wjco.v5.i4.744
Makuza, J. D., Nsanzimana, S., Muhimpundu, M. A., Pace, L. E., Ntaganira, J. and Riedel, D. J.
(2015). Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. The
Pan African Medical Journal, 22:26. doi:10.11604/pamj.2015.22.26.7116
Ntekim, A., Cervical Cancer in Sub Sahara Africa, Topics on cervical cancer with an advocacy
for prevention 2012. Available from: http://www. intechopen. com/books/topics-on-cervical-
cancer-with-an-advocacy-for-prevention/cervical-cancer-in-sub-sahara-africa.
Smith, R.A., Cokkinides, V., Brooks, D., Saslow, D., Shah, M. and Brawley, O.W., 2011. Cancer
screening in the United States, 2011. CA: a cancer journal for clinicians, 61(1), pp.8-30
Sanuki, N., Urabe, S., Matsumoto, H., Ono, A., Komatsu, E., Kamei, N., & Maeda, T. (2013).
Evaluation of microscopic tumor extension in early-stage cervical cancer: quantifying subclinical
https://www.webmd.com/cancer/cervical-cancer/ss/slideshow-cervical-cancer-overview
Maniar, K. and Wei, J. 2017. Pathology of cervical carcinoma. The GLOWM, doi:
10.3843/GLOWM.10230
Mishra, G. A., Pimple, S. A., & Shastri, S. S. (2011). An overview of prevention and early
detection of cervical cancers. Indian journal of medical and paediatric oncology : official
journal of Indian Society of Medical & Paediatric Oncology, 32(3), 125–132. doi:10.4103/0971-
5851.92808
McGraw, S. L., & Ferrante, J. M. (2014). Update on prevention and screening of cervical cancer.
World journal of clinical oncology, 5(4), 744–752. doi:10.5306/wjco.v5.i4.744
Makuza, J. D., Nsanzimana, S., Muhimpundu, M. A., Pace, L. E., Ntaganira, J. and Riedel, D. J.
(2015). Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. The
Pan African Medical Journal, 22:26. doi:10.11604/pamj.2015.22.26.7116
Ntekim, A., Cervical Cancer in Sub Sahara Africa, Topics on cervical cancer with an advocacy
for prevention 2012. Available from: http://www. intechopen. com/books/topics-on-cervical-
cancer-with-an-advocacy-for-prevention/cervical-cancer-in-sub-sahara-africa.
Smith, R.A., Cokkinides, V., Brooks, D., Saslow, D., Shah, M. and Brawley, O.W., 2011. Cancer
screening in the United States, 2011. CA: a cancer journal for clinicians, 61(1), pp.8-30
Sanuki, N., Urabe, S., Matsumoto, H., Ono, A., Komatsu, E., Kamei, N., & Maeda, T. (2013).
Evaluation of microscopic tumor extension in early-stage cervical cancer: quantifying subclinical
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

