NUR241 Case Study: Cervical Cancer Screening and Guidelines
VerifiedAdded on 2022/09/15
|5
|863
|21
Case Study
AI Summary
This case study examines the pathophysiology of cervical cancer, focusing on the role of HPV infection and the progression from CIN stages to invasive cancer. The risk factors in Sarah's case, including high-risk HPV serotypes and a CIN III diagnosis, are identified. The assignment also outlines the latest cervical screening guidelines in Australia, emphasizing primary HPV testing, genotyping, and the recommended screening intervals for vaccinated and unvaccinated women. The rationale behind these guidelines, supported by scientific literature, is presented, highlighting the effectiveness of the screening process in reducing cervical cancer incidence. The study also mentions the introduction of the National Cancer Screening Registry and the delisting of existing cervical screening test items.

Running Head: CERVICAL CANCER: SCREENING, RISK FACTORS AND
PATHOPHYSIOLOGY
Cervical Cancer: Screening, Risk factors and Pathophysiology
Name of the Student:
Name of the University:
Author Note:
PATHOPHYSIOLOGY
Cervical Cancer: Screening, Risk factors and Pathophysiology
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Cervical Cancer: Screening, Risk factors and Pathophysiology
Answer 1:
Pathophysiology of cervical cancer
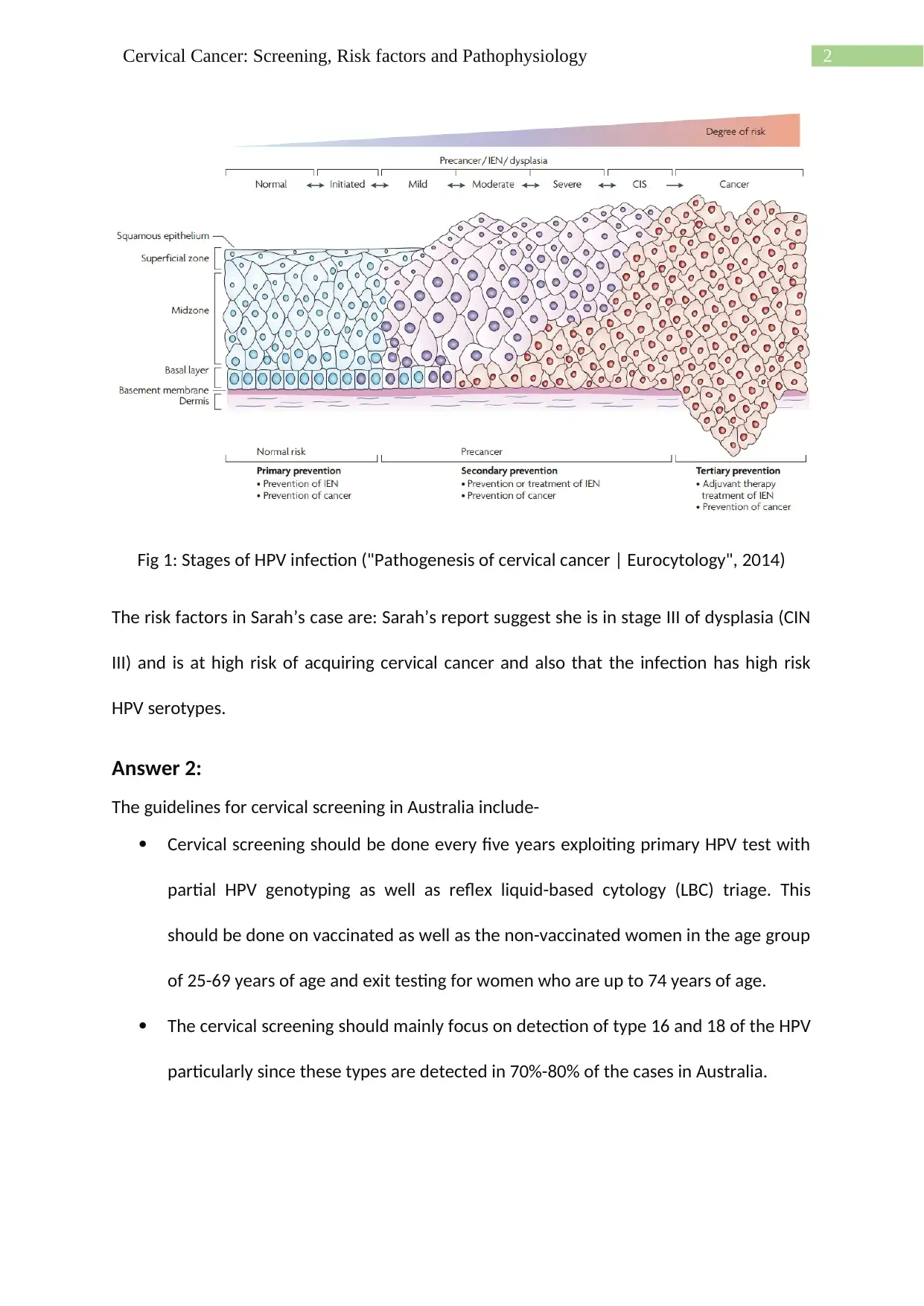
The onset for the development of cervical cancer is characterised by infection with HPV with
two major risk factors of chronic infection with high-risk HPV and ineffective clearance of
HPV. The normal HPV virus is cleared on their own in a span of few months or years. But the
high-risk HPV modify their genome sequence which affects the physiology of the body. The
process of transformation of the HPV infection to cancer is complex and it is the infection of
the basal cells present between the squamous epithelium of the ectocervix and the
columnar epithelium of the endocervix (Kurman, 2013). The replication of the viruses occurs
in the epithelial cells during the phenomenon of differentiation cycle. The stage of non-
invasive disease is termed as cervical intraepithelial neoplasia (CIN). The low-grade
neoplasia (CIN1) exploits one third of the thickness of the epithelium, CIN2 invades two
third of the thickness and the most severe form is CIN3 which refers to invasiveness in more
than two third of the epithelium (Wright et al., 2013).
Answer 1:
Pathophysiology of cervical cancer
The onset for the development of cervical cancer is characterised by infection with HPV with
two major risk factors of chronic infection with high-risk HPV and ineffective clearance of
HPV. The normal HPV virus is cleared on their own in a span of few months or years. But the
high-risk HPV modify their genome sequence which affects the physiology of the body. The
process of transformation of the HPV infection to cancer is complex and it is the infection of
the basal cells present between the squamous epithelium of the ectocervix and the
columnar epithelium of the endocervix (Kurman, 2013). The replication of the viruses occurs
in the epithelial cells during the phenomenon of differentiation cycle. The stage of non-
invasive disease is termed as cervical intraepithelial neoplasia (CIN). The low-grade
neoplasia (CIN1) exploits one third of the thickness of the epithelium, CIN2 invades two
third of the thickness and the most severe form is CIN3 which refers to invasiveness in more
than two third of the epithelium (Wright et al., 2013).
2Cervical Cancer: Screening, Risk factors and Pathophysiology
Fig 1: Stages of HPV infection ("Pathogenesis of cervical cancer | Eurocytology", 2014)
The risk factors in Sarah’s case are: Sarah’s report suggest she is in stage III of dysplasia (CIN
III) and is at high risk of acquiring cervical cancer and also that the infection has high risk
HPV serotypes.
Answer 2:
The guidelines for cervical screening in Australia include-
Cervical screening should be done every five years exploiting primary HPV test with
partial HPV genotyping as well as reflex liquid-based cytology (LBC) triage. This
should be done on vaccinated as well as the non-vaccinated women in the age group
of 25-69 years of age and exit testing for women who are up to 74 years of age.
The cervical screening should mainly focus on detection of type 16 and 18 of the HPV
particularly since these types are detected in 70%-80% of the cases in Australia.
Fig 1: Stages of HPV infection ("Pathogenesis of cervical cancer | Eurocytology", 2014)
The risk factors in Sarah’s case are: Sarah’s report suggest she is in stage III of dysplasia (CIN
III) and is at high risk of acquiring cervical cancer and also that the infection has high risk
HPV serotypes.
Answer 2:
The guidelines for cervical screening in Australia include-
Cervical screening should be done every five years exploiting primary HPV test with
partial HPV genotyping as well as reflex liquid-based cytology (LBC) triage. This
should be done on vaccinated as well as the non-vaccinated women in the age group
of 25-69 years of age and exit testing for women who are up to 74 years of age.
The cervical screening should mainly focus on detection of type 16 and 18 of the HPV
particularly since these types are detected in 70%-80% of the cases in Australia.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Cervical Cancer: Screening, Risk factors and Pathophysiology
In case of an individual who has been under screened of never screened self-
collection of the HPV sample is being promoted by the health care providers as well
as nurses who are into the mainstream of cervical screening.
The required invitation as well as reminders should be conveyed to the women in
the age group of 25-69 years and exit communications to be send to the women who
belong to the age of 70-74 years.
The introduction of National Cancer Screening Registry in 2017 would capture the
colposcopy data effective from 1st December 2017 for the purpose of benchmarking
and quality assurance.
Delisting the present cervical screening test MBS items (Lew et al., 2017).
This proposed guideline has strong evidence of resulting in a 30% reduction of the
occurrence of cervical cancer over time. The literature studies suggest that the screening
process every five years will be more effective since the time frame from the HPV infection
to cervical cancer is 10 to 15 years (Hall et al., 2018).
In case of an individual who has been under screened of never screened self-
collection of the HPV sample is being promoted by the health care providers as well
as nurses who are into the mainstream of cervical screening.
The required invitation as well as reminders should be conveyed to the women in
the age group of 25-69 years and exit communications to be send to the women who
belong to the age of 70-74 years.
The introduction of National Cancer Screening Registry in 2017 would capture the
colposcopy data effective from 1st December 2017 for the purpose of benchmarking
and quality assurance.
Delisting the present cervical screening test MBS items (Lew et al., 2017).
This proposed guideline has strong evidence of resulting in a 30% reduction of the
occurrence of cervical cancer over time. The literature studies suggest that the screening
process every five years will be more effective since the time frame from the HPV infection
to cervical cancer is 10 to 15 years (Hall et al., 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Cervical Cancer: Screening, Risk factors and Pathophysiology
References
Hall, M. T., Simms, K. T., Lew, J. B., Smith, M. A., Saville, M., & Canfell, K. (2018) . Projected
future impact of HPV vaccination and primary HPV screening on cervical cancer rates
from 2017–2035: example from Australia. PLoS One, 13(2), e0185332.
Kurman, R. J. (Ed.). (2013). Blaustein's pathology of the female genital tract. Springer
Science & Business Media.
Lew, J. B., Simms, K. T., Smith, M. A., Hall, M., Kang, Y. J., Xu, X. M., ... & Hammond, I. (2017) .
Primary HPV testing versus cytology-based cervical screening in women in Australia
vaccinated for HPV and unvaccinated: effectiveness and economic assessment for the
National Cervical Screening Program. The Lancet Public Health, 2(2), e96-e107.
Pathogenesis of cervical cancer | Eurocytology. (2014). Retrieved 25 August 2019, from
https://www.eurocytology.eu/en/course/969
Wright, A. A., Howitt, B. E., Myers, A. P., Dahlberg, S. E., Palescandolo, E., Van Hummelen, P.,
... & Quick, C. M. (2013). Oncogenic mutations in cervical cancer: genomic differences
between adenocarcinomas and squamous cell carcinomas of the cervix. Cancer, 119(21),
3776-3783.
References
Hall, M. T., Simms, K. T., Lew, J. B., Smith, M. A., Saville, M., & Canfell, K. (2018) . Projected
future impact of HPV vaccination and primary HPV screening on cervical cancer rates
from 2017–2035: example from Australia. PLoS One, 13(2), e0185332.
Kurman, R. J. (Ed.). (2013). Blaustein's pathology of the female genital tract. Springer
Science & Business Media.
Lew, J. B., Simms, K. T., Smith, M. A., Hall, M., Kang, Y. J., Xu, X. M., ... & Hammond, I. (2017) .
Primary HPV testing versus cytology-based cervical screening in women in Australia
vaccinated for HPV and unvaccinated: effectiveness and economic assessment for the
National Cervical Screening Program. The Lancet Public Health, 2(2), e96-e107.
Pathogenesis of cervical cancer | Eurocytology. (2014). Retrieved 25 August 2019, from
https://www.eurocytology.eu/en/course/969
Wright, A. A., Howitt, B. E., Myers, A. P., Dahlberg, S. E., Palescandolo, E., Van Hummelen, P.,
... & Quick, C. M. (2013). Oncogenic mutations in cervical cancer: genomic differences
between adenocarcinomas and squamous cell carcinomas of the cervix. Cancer, 119(21),
3776-3783.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





