Analysis of Congestive Heart Failure in Acute Care Nursing Scenario
VerifiedAdded on 2021/04/24
|11
|3166
|20
Homework Assignment
AI Summary
This assignment presents a case study of Mrs. Sharon McKenzie, a 77-year-old patient diagnosed with congestive heart failure (CHF). The document explores various risk factors contributing to CHF, including age, hypertension, history of myocardial infarction, and medication use. It details the pathophysiology of symptoms such as dyspnea, swollen ankles, dizziness, tachycardia, and lack of appetite. The assignment further discusses pharmacological interventions, focusing on ACE inhibitors and beta-blockers, and provides a comprehensive overview of nursing interventions within the first 24 hours of admission, encompassing cardiovascular and respiratory assessments and interventions. The interventions include monitoring vital signs, administering medications, and promoting respiratory function to improve patient outcomes.
S00213148
Acute Care Nursing
1
SANDHYA REGMI
Acute Care Nursing
1
SANDHYA REGMI
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
S00213148
Q.1.
There are various risk factors which are responsible for development of congestive
heart failure (CHF) including older age, high levels of cholesterol, diabetes mellitus, high
blood pressure and active smoking. In the given scenario, Mrs Sharon Mckenzie is 77 years
old which might be one the risk factor for CCF to her. According to recent literature, risk of
CHF increases with age, 2 % of the people between age 40 to 59 years and 5 % of the people
between 60 to 69 years develop CHF. In addition to this lack of physical activity, family
history, obesity and alcohol consumption are also responsible for CHF (Dhingra et al., 2014).
Since Mrs Mckenzie is elderly lady she might not be able to do sufficient physical activity,
even though she sometimes does gardening and walking with her husband this may also play
role to her recent condition. Similarly another contributing factor is hypertension, according
to given observation date in the scenario, she is hypertensive. Hypertensive females are at
four times higher risk as compared to non-hypertensive females for CHF. Female with
hypertension are more prone to congestive heart failure as compared to hypertensive female.
60 % of hypertensive female and 40 % of the hypertensive male are at risk of CHF
(Mahmood and Wang, 2013). Likewise, Lipoproteins play major role in CHF. CHF can
occur in patients with high levels of low-density lipoproteins (LDL) and low levels of high
density lipoproteins (HDL). Smoking and obesity is also prominent factor for CCF,36 %
people with smoking and 20 % people with obesity can develop CHF (Australian Institute of
Health and Welfare (2014). Dietary factors are also responsible for the development of CHF
like more consumption of saturated fats can lead to development of CHF. People with
augmented levels of β-type natriuretic peptides can develop CHF (Díaz-Toro et al., 2015).
Most of the cardiovascular abnormalities like coronary artery disease and heart attack,
faulty heart valves, cardiomyopathy, myocarditis, coronary artery disease, congenital heart
defects and heart arrhythmias are responsible for the occurrence of CHF, in case of Mrs
Mckenzie, she has history of MI which further increase risk of CCF to her. Moreover, few of
the medications consumption can lead to CHF development in people. These medications
include antidiabetic medications (rosiglitazone and pioglitazone), nonsteroidal anti-
inflammatory drugs (NSAIDs), certain anaesthetics, anti-arrhythmic medications,
antihypertensive and anticancer (Gotto Jr et al., 2012; DeSilva, 2013). In regards to Mrs
Mckenzie, she is on antihypertensive medication, which can increase risk of CCF to her.
Mortality rate is high in people with CHF. On the basis of recent statistics, approximately
half of the patients with CHF die within 5 years of diagnosis of CHF. In comparison to the
2
SANDHYA REGMI
Q.1.
There are various risk factors which are responsible for development of congestive
heart failure (CHF) including older age, high levels of cholesterol, diabetes mellitus, high
blood pressure and active smoking. In the given scenario, Mrs Sharon Mckenzie is 77 years
old which might be one the risk factor for CCF to her. According to recent literature, risk of
CHF increases with age, 2 % of the people between age 40 to 59 years and 5 % of the people
between 60 to 69 years develop CHF. In addition to this lack of physical activity, family
history, obesity and alcohol consumption are also responsible for CHF (Dhingra et al., 2014).
Since Mrs Mckenzie is elderly lady she might not be able to do sufficient physical activity,
even though she sometimes does gardening and walking with her husband this may also play
role to her recent condition. Similarly another contributing factor is hypertension, according
to given observation date in the scenario, she is hypertensive. Hypertensive females are at
four times higher risk as compared to non-hypertensive females for CHF. Female with
hypertension are more prone to congestive heart failure as compared to hypertensive female.
60 % of hypertensive female and 40 % of the hypertensive male are at risk of CHF
(Mahmood and Wang, 2013). Likewise, Lipoproteins play major role in CHF. CHF can
occur in patients with high levels of low-density lipoproteins (LDL) and low levels of high
density lipoproteins (HDL). Smoking and obesity is also prominent factor for CCF,36 %
people with smoking and 20 % people with obesity can develop CHF (Australian Institute of
Health and Welfare (2014). Dietary factors are also responsible for the development of CHF
like more consumption of saturated fats can lead to development of CHF. People with
augmented levels of β-type natriuretic peptides can develop CHF (Díaz-Toro et al., 2015).
Most of the cardiovascular abnormalities like coronary artery disease and heart attack,
faulty heart valves, cardiomyopathy, myocarditis, coronary artery disease, congenital heart
defects and heart arrhythmias are responsible for the occurrence of CHF, in case of Mrs
Mckenzie, she has history of MI which further increase risk of CCF to her. Moreover, few of
the medications consumption can lead to CHF development in people. These medications
include antidiabetic medications (rosiglitazone and pioglitazone), nonsteroidal anti-
inflammatory drugs (NSAIDs), certain anaesthetics, anti-arrhythmic medications,
antihypertensive and anticancer (Gotto Jr et al., 2012; DeSilva, 2013). In regards to Mrs
Mckenzie, she is on antihypertensive medication, which can increase risk of CCF to her.
Mortality rate is high in people with CHF. On the basis of recent statistics, approximately
half of the patients with CHF die within 5 years of diagnosis of CHF. In comparison to the
2
SANDHYA REGMI
S00213148
normal people, approximately 10 % of the people would have sudden death (Australian
Institute of Health and Welfare ,2014). Due to her recent conditions her activity of daily
living can be significantly affected, she might not be able to do her usual activities and need
someone to supervise and assist her which can impact on her psychological condition. On the
other hand, family member need to involve in her care which can be stressful for them and
the cost of treatment might pose economic burden to them. Family members and care
providers should avoid exposure of risk factors to her. Her diet and medication consumption
adherence should be monitored by care provider and dietician. Positive communication
should be maintained with the adult patients and her family members should maintain
positive communication with her to improve her moral and wellbeing. Family members
should keep positive approach to improve her condition and they should not keep on
worrying about her diseased condition. Worrying about the patient condition can divert
family member’s attention from caring him (Cooper et al., 2015; Raman, 2016).
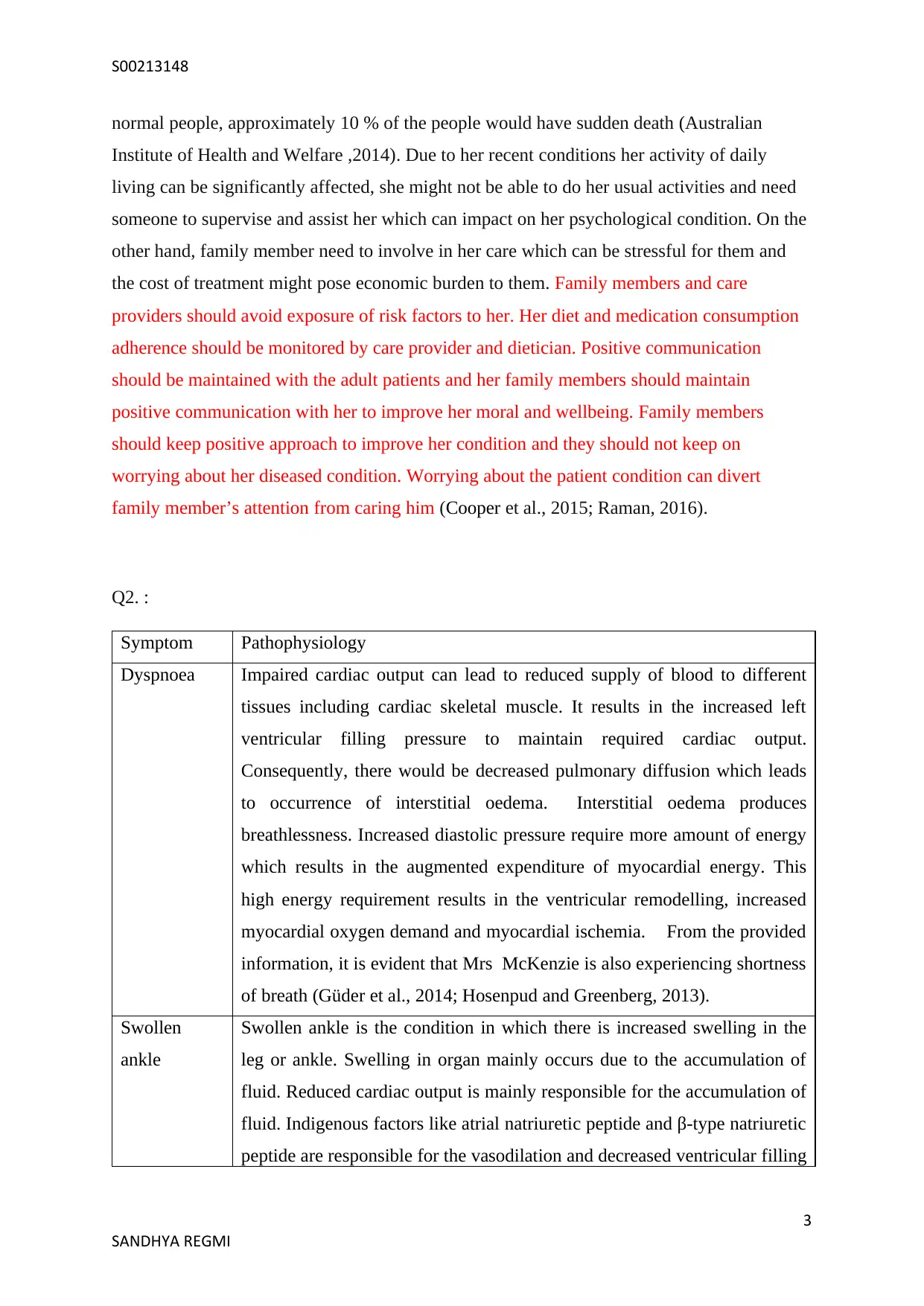
Q2. :
Symptom Pathophysiology
Dyspnoea Impaired cardiac output can lead to reduced supply of blood to different
tissues including cardiac skeletal muscle. It results in the increased left
ventricular filling pressure to maintain required cardiac output.
Consequently, there would be decreased pulmonary diffusion which leads
to occurrence of interstitial oedema. Interstitial oedema produces
breathlessness. Increased diastolic pressure require more amount of energy
which results in the augmented expenditure of myocardial energy. This
high energy requirement results in the ventricular remodelling, increased
myocardial oxygen demand and myocardial ischemia. From the provided
information, it is evident that Mrs McKenzie is also experiencing shortness
of breath (Güder et al., 2014; Hosenpud and Greenberg, 2013).
Swollen
ankle
Swollen ankle is the condition in which there is increased swelling in the
leg or ankle. Swelling in organ mainly occurs due to the accumulation of
fluid. Reduced cardiac output is mainly responsible for the accumulation of
fluid. Indigenous factors like atrial natriuretic peptide and β-type natriuretic
peptide are responsible for the vasodilation and decreased ventricular filling
3
SANDHYA REGMI
normal people, approximately 10 % of the people would have sudden death (Australian
Institute of Health and Welfare ,2014). Due to her recent conditions her activity of daily
living can be significantly affected, she might not be able to do her usual activities and need
someone to supervise and assist her which can impact on her psychological condition. On the
other hand, family member need to involve in her care which can be stressful for them and
the cost of treatment might pose economic burden to them. Family members and care
providers should avoid exposure of risk factors to her. Her diet and medication consumption
adherence should be monitored by care provider and dietician. Positive communication
should be maintained with the adult patients and her family members should maintain
positive communication with her to improve her moral and wellbeing. Family members
should keep positive approach to improve her condition and they should not keep on
worrying about her diseased condition. Worrying about the patient condition can divert
family member’s attention from caring him (Cooper et al., 2015; Raman, 2016).
Q2. :
Symptom Pathophysiology
Dyspnoea Impaired cardiac output can lead to reduced supply of blood to different
tissues including cardiac skeletal muscle. It results in the increased left
ventricular filling pressure to maintain required cardiac output.
Consequently, there would be decreased pulmonary diffusion which leads
to occurrence of interstitial oedema. Interstitial oedema produces
breathlessness. Increased diastolic pressure require more amount of energy
which results in the augmented expenditure of myocardial energy. This
high energy requirement results in the ventricular remodelling, increased
myocardial oxygen demand and myocardial ischemia. From the provided
information, it is evident that Mrs McKenzie is also experiencing shortness
of breath (Güder et al., 2014; Hosenpud and Greenberg, 2013).
Swollen
ankle
Swollen ankle is the condition in which there is increased swelling in the
leg or ankle. Swelling in organ mainly occurs due to the accumulation of
fluid. Reduced cardiac output is mainly responsible for the accumulation of
fluid. Indigenous factors like atrial natriuretic peptide and β-type natriuretic
peptide are responsible for the vasodilation and decreased ventricular filling
3
SANDHYA REGMI
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
S00213148
pressure. It results in the reduced cardiac preload and afterload. This results
in the increased back flow of blood to the heart through the veins.
Narrowing in the valve can lead to block in the blood flow, hence heart
would not be able to pump required amount of blood. Due to this
cardiovascular abnormality, Mrs McKenzie is having swollen ankle (Moe,
2013; Eisen, 2014).
Dizziness In patients with congestive heart failure, there would be reduced blood flow
to all the organs including brain. Due to this reduced blood flow to brain,
patients with CHF can experience dizziness. Abnormality in heart rate and
rhythm is mainly responsible for the reduced blood supply to brain. As a
result of this cardiovascular abnormality, Mrs McKenzie is experiencing
dizziness (Kovács et al., 2014; Hosenpud and Greenberg, 2013).
Tachycardia Patients with CHF are associated with life-threatening ventricular
arrhythmias. Ventricular dilation is responsible for ventricular arrhythmia.
Also, myocyte pathology like myocardial hypertrophy and myocardial
fibrosis are responsible for the ventricular arrhythmia (Ellis and Josephson,
2013; Eisen, 2014).
Lack of
appetite and
nausea
Less supply of blood to gastrointestinal tract in patients with CHF results in
lack of appetite and nausea. Due to less supply of blood, nerve endings in
the gastrointestinal tract can have irritation. Due to this irritation, these
nerve endings stimulate centres in brain which are responsible for nausea
and vomiting (Kemp and Conte, 2012; Hosenpud and Greenberg, 2013).
4
SANDHYA REGMI
pressure. It results in the reduced cardiac preload and afterload. This results
in the increased back flow of blood to the heart through the veins.
Narrowing in the valve can lead to block in the blood flow, hence heart
would not be able to pump required amount of blood. Due to this
cardiovascular abnormality, Mrs McKenzie is having swollen ankle (Moe,
2013; Eisen, 2014).
Dizziness In patients with congestive heart failure, there would be reduced blood flow
to all the organs including brain. Due to this reduced blood flow to brain,
patients with CHF can experience dizziness. Abnormality in heart rate and
rhythm is mainly responsible for the reduced blood supply to brain. As a
result of this cardiovascular abnormality, Mrs McKenzie is experiencing
dizziness (Kovács et al., 2014; Hosenpud and Greenberg, 2013).
Tachycardia Patients with CHF are associated with life-threatening ventricular
arrhythmias. Ventricular dilation is responsible for ventricular arrhythmia.
Also, myocyte pathology like myocardial hypertrophy and myocardial
fibrosis are responsible for the ventricular arrhythmia (Ellis and Josephson,
2013; Eisen, 2014).
Lack of
appetite and
nausea
Less supply of blood to gastrointestinal tract in patients with CHF results in
lack of appetite and nausea. Due to less supply of blood, nerve endings in
the gastrointestinal tract can have irritation. Due to this irritation, these
nerve endings stimulate centres in brain which are responsible for nausea
and vomiting (Kemp and Conte, 2012; Hosenpud and Greenberg, 2013).
4
SANDHYA REGMI
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
S00213148
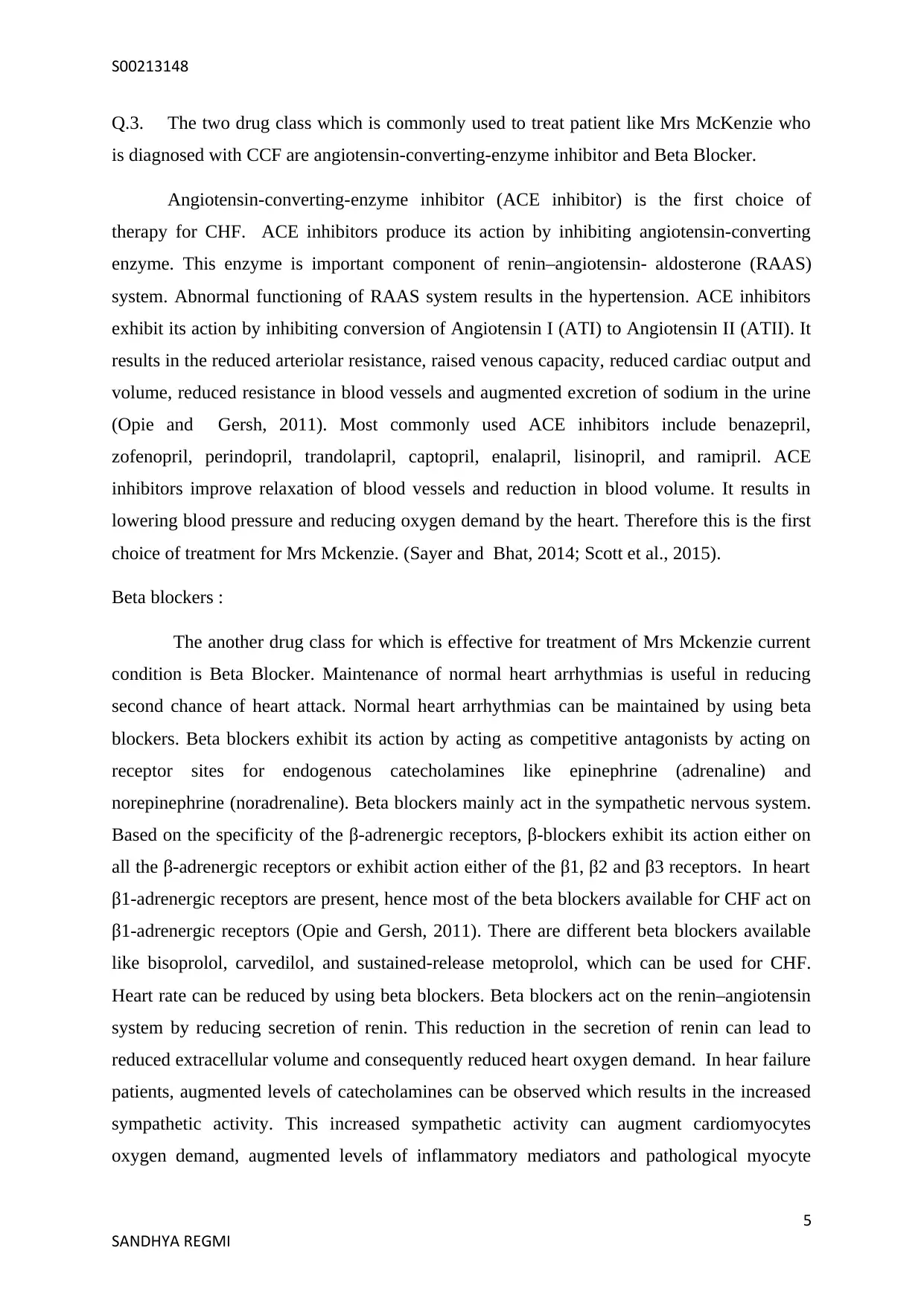
Q.3. The two drug class which is commonly used to treat patient like Mrs McKenzie who
is diagnosed with CCF are angiotensin-converting-enzyme inhibitor and Beta Blocker.
Angiotensin-converting-enzyme inhibitor (ACE inhibitor) is the first choice of
therapy for CHF. ACE inhibitors produce its action by inhibiting angiotensin-converting
enzyme. This enzyme is important component of renin–angiotensin- aldosterone (RAAS)
system. Abnormal functioning of RAAS system results in the hypertension. ACE inhibitors
exhibit its action by inhibiting conversion of Angiotensin I (ATI) to Angiotensin II (ATII). It
results in the reduced arteriolar resistance, raised venous capacity, reduced cardiac output and
volume, reduced resistance in blood vessels and augmented excretion of sodium in the urine
(Opie and Gersh, 2011). Most commonly used ACE inhibitors include benazepril,
zofenopril, perindopril, trandolapril, captopril, enalapril, lisinopril, and ramipril. ACE
inhibitors improve relaxation of blood vessels and reduction in blood volume. It results in
lowering blood pressure and reducing oxygen demand by the heart. Therefore this is the first
choice of treatment for Mrs Mckenzie. (Sayer and Bhat, 2014; Scott et al., 2015).
Beta blockers :
The another drug class for which is effective for treatment of Mrs Mckenzie current
condition is Beta Blocker. Maintenance of normal heart arrhythmias is useful in reducing
second chance of heart attack. Normal heart arrhythmias can be maintained by using beta
blockers. Beta blockers exhibit its action by acting as competitive antagonists by acting on
receptor sites for endogenous catecholamines like epinephrine (adrenaline) and
norepinephrine (noradrenaline). Beta blockers mainly act in the sympathetic nervous system.
Based on the specificity of the β-adrenergic receptors, β-blockers exhibit its action either on
all the β-adrenergic receptors or exhibit action either of the β1, β2 and β3 receptors. In heart
β1-adrenergic receptors are present, hence most of the beta blockers available for CHF act on
β1-adrenergic receptors (Opie and Gersh, 2011). There are different beta blockers available
like bisoprolol, carvedilol, and sustained-release metoprolol, which can be used for CHF.
Heart rate can be reduced by using beta blockers. Beta blockers act on the renin–angiotensin
system by reducing secretion of renin. This reduction in the secretion of renin can lead to
reduced extracellular volume and consequently reduced heart oxygen demand. In hear failure
patients, augmented levels of catecholamines can be observed which results in the increased
sympathetic activity. This increased sympathetic activity can augment cardiomyocytes
oxygen demand, augmented levels of inflammatory mediators and pathological myocyte
5
SANDHYA REGMI
Q.3. The two drug class which is commonly used to treat patient like Mrs McKenzie who
is diagnosed with CCF are angiotensin-converting-enzyme inhibitor and Beta Blocker.
Angiotensin-converting-enzyme inhibitor (ACE inhibitor) is the first choice of
therapy for CHF. ACE inhibitors produce its action by inhibiting angiotensin-converting
enzyme. This enzyme is important component of renin–angiotensin- aldosterone (RAAS)
system. Abnormal functioning of RAAS system results in the hypertension. ACE inhibitors
exhibit its action by inhibiting conversion of Angiotensin I (ATI) to Angiotensin II (ATII). It
results in the reduced arteriolar resistance, raised venous capacity, reduced cardiac output and
volume, reduced resistance in blood vessels and augmented excretion of sodium in the urine
(Opie and Gersh, 2011). Most commonly used ACE inhibitors include benazepril,
zofenopril, perindopril, trandolapril, captopril, enalapril, lisinopril, and ramipril. ACE
inhibitors improve relaxation of blood vessels and reduction in blood volume. It results in
lowering blood pressure and reducing oxygen demand by the heart. Therefore this is the first
choice of treatment for Mrs Mckenzie. (Sayer and Bhat, 2014; Scott et al., 2015).
Beta blockers :
The another drug class for which is effective for treatment of Mrs Mckenzie current
condition is Beta Blocker. Maintenance of normal heart arrhythmias is useful in reducing
second chance of heart attack. Normal heart arrhythmias can be maintained by using beta
blockers. Beta blockers exhibit its action by acting as competitive antagonists by acting on
receptor sites for endogenous catecholamines like epinephrine (adrenaline) and
norepinephrine (noradrenaline). Beta blockers mainly act in the sympathetic nervous system.
Based on the specificity of the β-adrenergic receptors, β-blockers exhibit its action either on
all the β-adrenergic receptors or exhibit action either of the β1, β2 and β3 receptors. In heart
β1-adrenergic receptors are present, hence most of the beta blockers available for CHF act on
β1-adrenergic receptors (Opie and Gersh, 2011). There are different beta blockers available
like bisoprolol, carvedilol, and sustained-release metoprolol, which can be used for CHF.
Heart rate can be reduced by using beta blockers. Beta blockers act on the renin–angiotensin
system by reducing secretion of renin. This reduction in the secretion of renin can lead to
reduced extracellular volume and consequently reduced heart oxygen demand. In hear failure
patients, augmented levels of catecholamines can be observed which results in the increased
sympathetic activity. This increased sympathetic activity can augment cardiomyocytes
oxygen demand, augmented levels of inflammatory mediators and pathological myocyte
5
SANDHYA REGMI
S00213148
remodelling. It results in the reduced efficiency of cardiac contraction and decreased ejection
fraction. All these abnormal pathological conditions can be restored by countering augmented
sympathetic activit (Buchhorn and Ross, 2014; Buchhorn and McConnell, 2014).
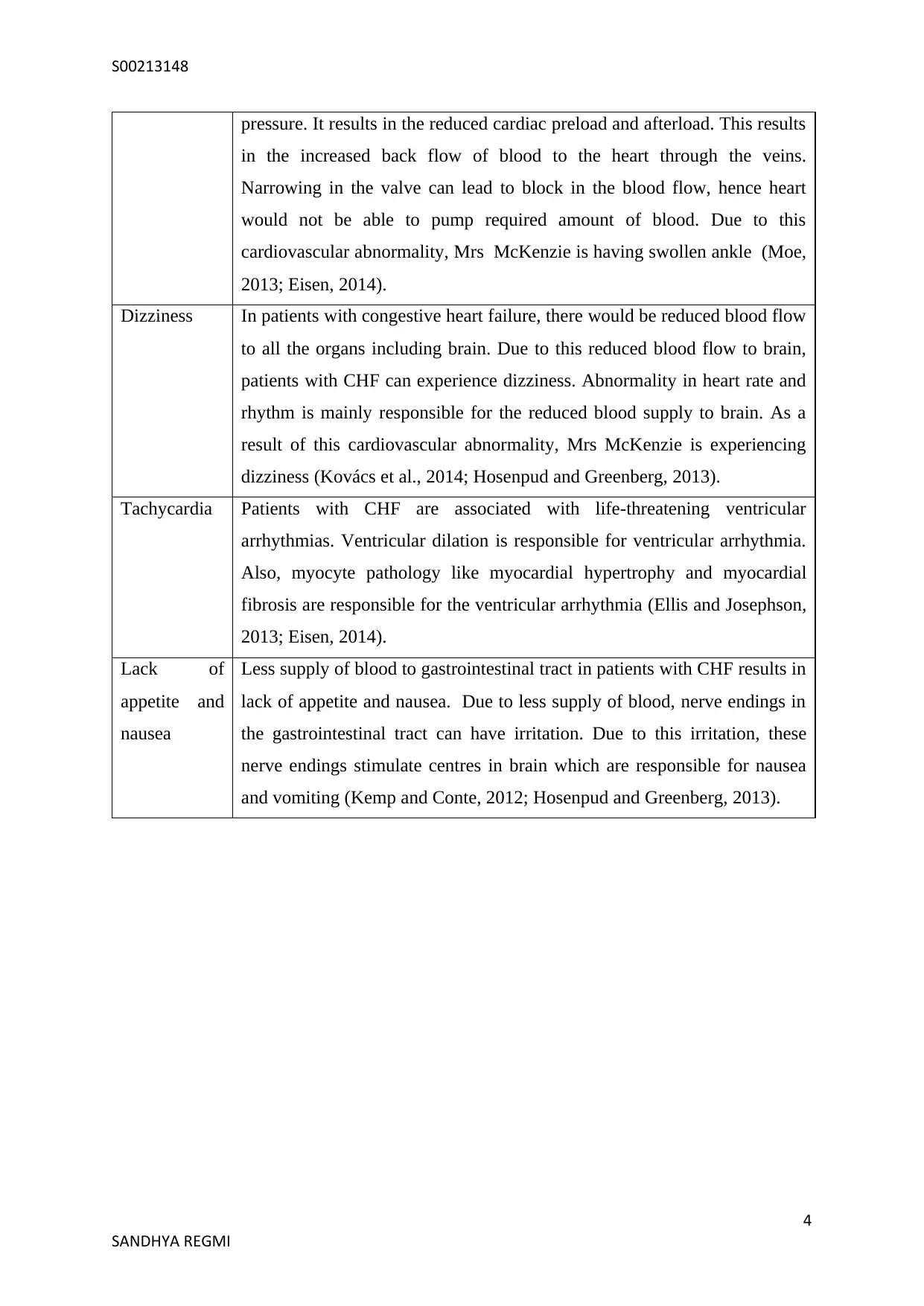
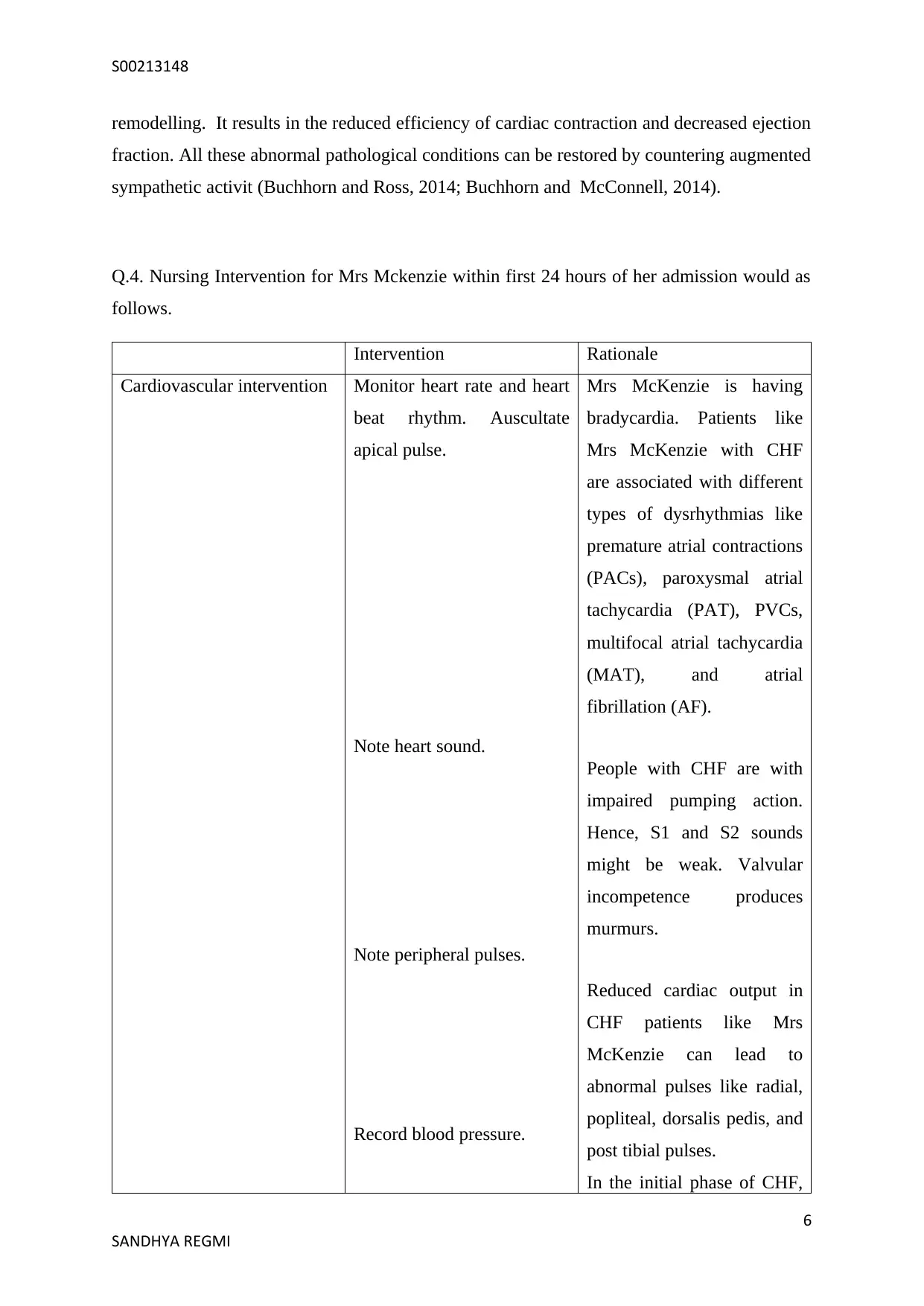
Q.4. Nursing Intervention for Mrs Mckenzie within first 24 hours of her admission would as
follows.
Intervention Rationale
Cardiovascular intervention Monitor heart rate and heart
beat rhythm. Auscultate
apical pulse.
Note heart sound.
Note peripheral pulses.
Record blood pressure.
Mrs McKenzie is having
bradycardia. Patients like
Mrs McKenzie with CHF
are associated with different
types of dysrhythmias like
premature atrial contractions
(PACs), paroxysmal atrial
tachycardia (PAT), PVCs,
multifocal atrial tachycardia
(MAT), and atrial
fibrillation (AF).
People with CHF are with
impaired pumping action.
Hence, S1 and S2 sounds
might be weak. Valvular
incompetence produces
murmurs.
Reduced cardiac output in
CHF patients like Mrs
McKenzie can lead to
abnormal pulses like radial,
popliteal, dorsalis pedis, and
post tibial pulses.
In the initial phase of CHF,
6
SANDHYA REGMI
remodelling. It results in the reduced efficiency of cardiac contraction and decreased ejection
fraction. All these abnormal pathological conditions can be restored by countering augmented
sympathetic activit (Buchhorn and Ross, 2014; Buchhorn and McConnell, 2014).
Q.4. Nursing Intervention for Mrs Mckenzie within first 24 hours of her admission would as
follows.
Intervention Rationale
Cardiovascular intervention Monitor heart rate and heart
beat rhythm. Auscultate
apical pulse.
Note heart sound.
Note peripheral pulses.
Record blood pressure.
Mrs McKenzie is having
bradycardia. Patients like
Mrs McKenzie with CHF
are associated with different
types of dysrhythmias like
premature atrial contractions
(PACs), paroxysmal atrial
tachycardia (PAT), PVCs,
multifocal atrial tachycardia
(MAT), and atrial
fibrillation (AF).
People with CHF are with
impaired pumping action.
Hence, S1 and S2 sounds
might be weak. Valvular
incompetence produces
murmurs.
Reduced cardiac output in
CHF patients like Mrs
McKenzie can lead to
abnormal pulses like radial,
popliteal, dorsalis pedis, and
post tibial pulses.
In the initial phase of CHF,
6
SANDHYA REGMI
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
S00213148
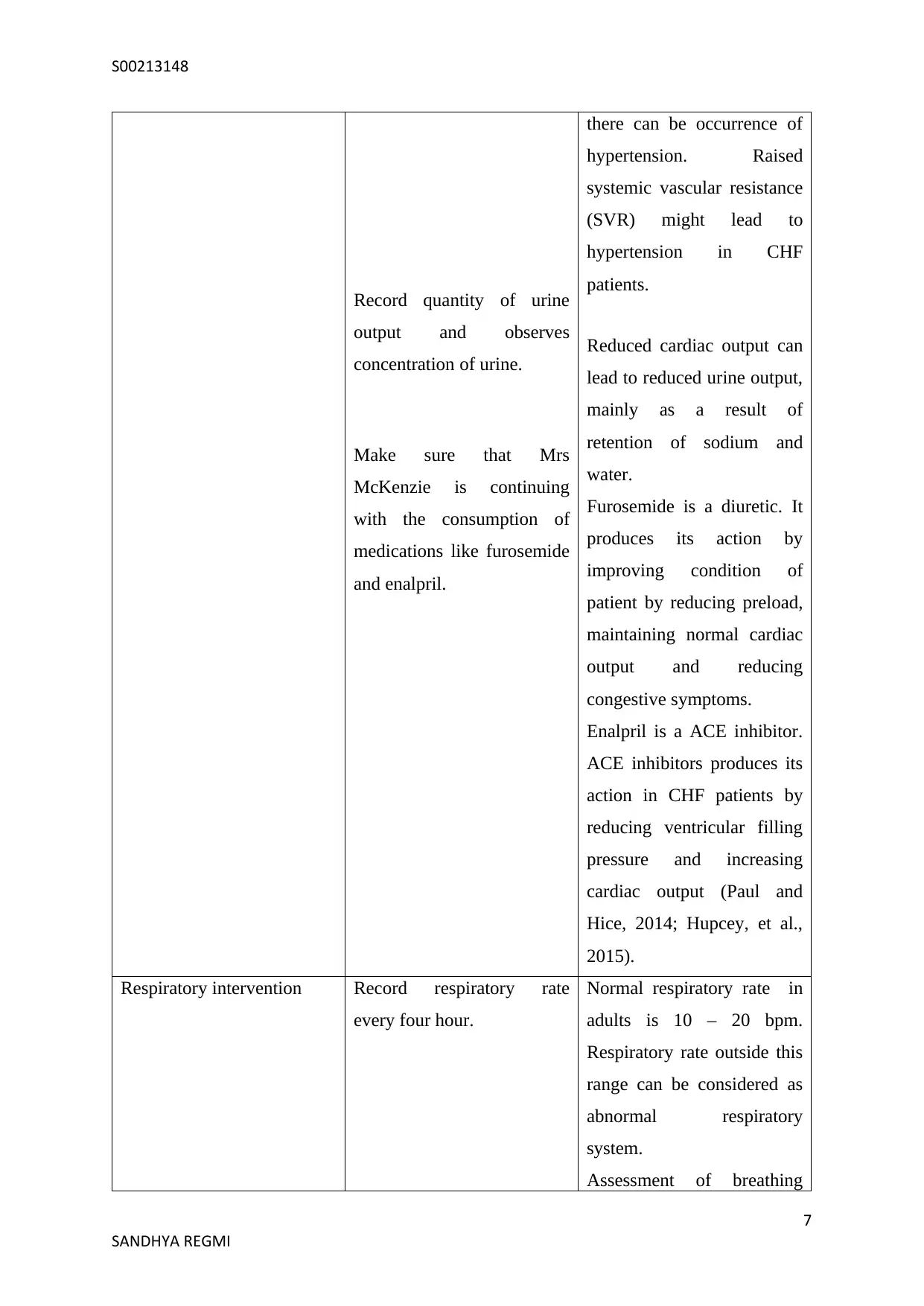
Record quantity of urine
output and observes
concentration of urine.
Make sure that Mrs
McKenzie is continuing
with the consumption of
medications like furosemide
and enalpril.
there can be occurrence of
hypertension. Raised
systemic vascular resistance
(SVR) might lead to
hypertension in CHF
patients.
Reduced cardiac output can
lead to reduced urine output,
mainly as a result of
retention of sodium and
water.
Furosemide is a diuretic. It
produces its action by
improving condition of
patient by reducing preload,
maintaining normal cardiac
output and reducing
congestive symptoms.
Enalpril is a ACE inhibitor.
ACE inhibitors produces its
action in CHF patients by
reducing ventricular filling
pressure and increasing
cardiac output (Paul and
Hice, 2014; Hupcey, et al.,
2015).
Respiratory intervention Record respiratory rate
every four hour.
Normal respiratory rate in
adults is 10 – 20 bpm.
Respiratory rate outside this
range can be considered as
abnormal respiratory
system.
Assessment of breathing
7
SANDHYA REGMI
Record quantity of urine
output and observes
concentration of urine.
Make sure that Mrs
McKenzie is continuing
with the consumption of
medications like furosemide
and enalpril.
there can be occurrence of
hypertension. Raised
systemic vascular resistance
(SVR) might lead to
hypertension in CHF
patients.
Reduced cardiac output can
lead to reduced urine output,
mainly as a result of
retention of sodium and
water.
Furosemide is a diuretic. It
produces its action by
improving condition of
patient by reducing preload,
maintaining normal cardiac
output and reducing
congestive symptoms.
Enalpril is a ACE inhibitor.
ACE inhibitors produces its
action in CHF patients by
reducing ventricular filling
pressure and increasing
cardiac output (Paul and
Hice, 2014; Hupcey, et al.,
2015).
Respiratory intervention Record respiratory rate
every four hour.
Normal respiratory rate in
adults is 10 – 20 bpm.
Respiratory rate outside this
range can be considered as
abnormal respiratory
system.
Assessment of breathing
7
SANDHYA REGMI
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
S00213148
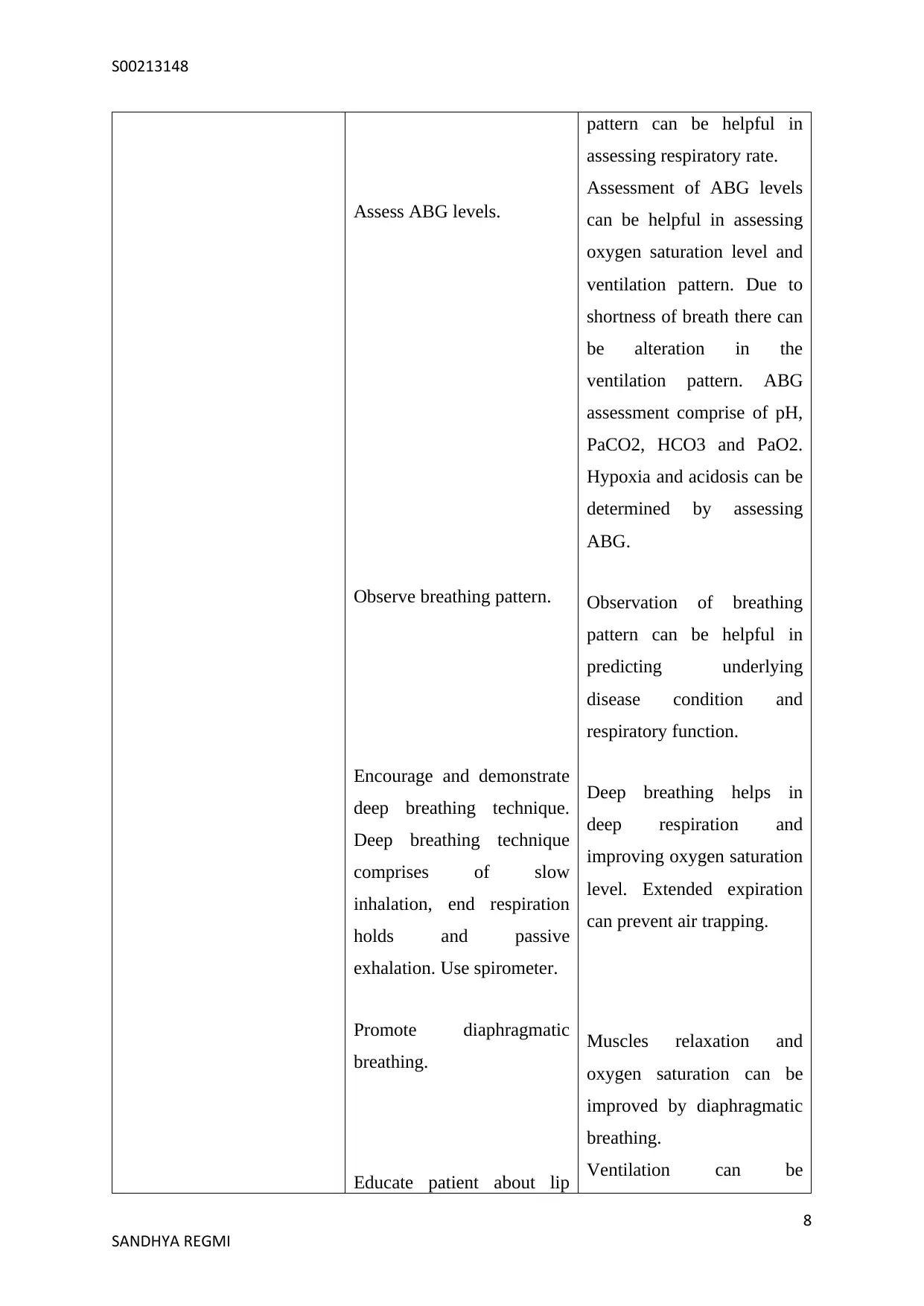
Assess ABG levels.
Observe breathing pattern.
Encourage and demonstrate
deep breathing technique.
Deep breathing technique
comprises of slow
inhalation, end respiration
holds and passive
exhalation. Use spirometer.
Promote diaphragmatic
breathing.
Educate patient about lip
pattern can be helpful in
assessing respiratory rate.
Assessment of ABG levels
can be helpful in assessing
oxygen saturation level and
ventilation pattern. Due to
shortness of breath there can
be alteration in the
ventilation pattern. ABG
assessment comprise of pH,
PaCO2, HCO3 and PaO2.
Hypoxia and acidosis can be
determined by assessing
ABG.
Observation of breathing
pattern can be helpful in
predicting underlying
disease condition and
respiratory function.
Deep breathing helps in
deep respiration and
improving oxygen saturation
level. Extended expiration
can prevent air trapping.
Muscles relaxation and
oxygen saturation can be
improved by diaphragmatic
breathing.
Ventilation can be
8
SANDHYA REGMI
Assess ABG levels.
Observe breathing pattern.
Encourage and demonstrate
deep breathing technique.
Deep breathing technique
comprises of slow
inhalation, end respiration
holds and passive
exhalation. Use spirometer.
Promote diaphragmatic
breathing.
Educate patient about lip
pattern can be helpful in
assessing respiratory rate.
Assessment of ABG levels
can be helpful in assessing
oxygen saturation level and
ventilation pattern. Due to
shortness of breath there can
be alteration in the
ventilation pattern. ABG
assessment comprise of pH,
PaCO2, HCO3 and PaO2.
Hypoxia and acidosis can be
determined by assessing
ABG.
Observation of breathing
pattern can be helpful in
predicting underlying
disease condition and
respiratory function.
Deep breathing helps in
deep respiration and
improving oxygen saturation
level. Extended expiration
can prevent air trapping.
Muscles relaxation and
oxygen saturation can be
improved by diaphragmatic
breathing.
Ventilation can be
8
SANDHYA REGMI
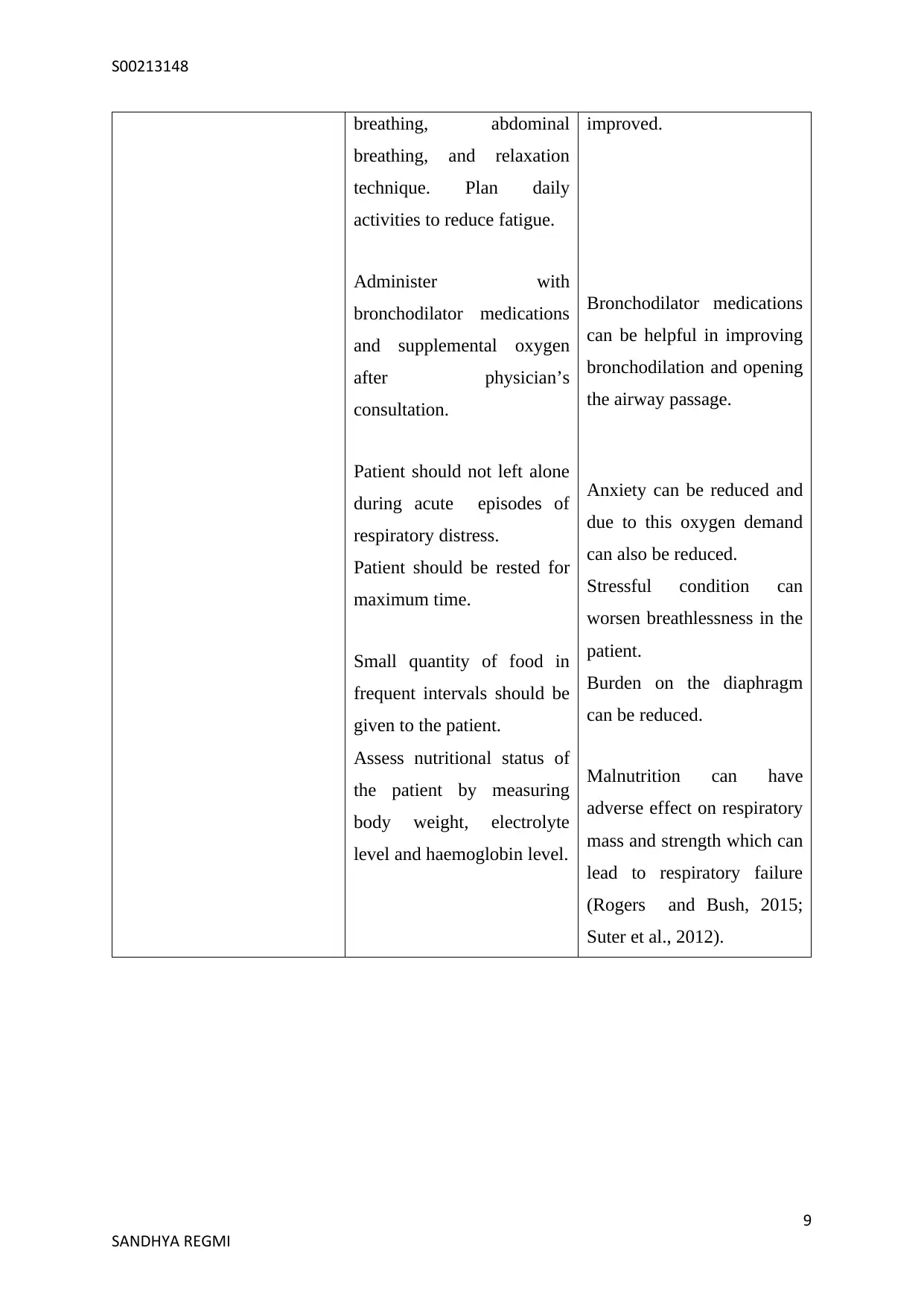
S00213148
breathing, abdominal
breathing, and relaxation
technique. Plan daily
activities to reduce fatigue.
Administer with
bronchodilator medications
and supplemental oxygen
after physician’s
consultation.
Patient should not left alone
during acute episodes of
respiratory distress.
Patient should be rested for
maximum time.
Small quantity of food in
frequent intervals should be
given to the patient.
Assess nutritional status of
the patient by measuring
body weight, electrolyte
level and haemoglobin level.
improved.
Bronchodilator medications
can be helpful in improving
bronchodilation and opening
the airway passage.
Anxiety can be reduced and
due to this oxygen demand
can also be reduced.
Stressful condition can
worsen breathlessness in the
patient.
Burden on the diaphragm
can be reduced.
Malnutrition can have
adverse effect on respiratory
mass and strength which can
lead to respiratory failure
(Rogers and Bush, 2015;
Suter et al., 2012).
9
SANDHYA REGMI
breathing, abdominal
breathing, and relaxation
technique. Plan daily
activities to reduce fatigue.
Administer with
bronchodilator medications
and supplemental oxygen
after physician’s
consultation.
Patient should not left alone
during acute episodes of
respiratory distress.
Patient should be rested for
maximum time.
Small quantity of food in
frequent intervals should be
given to the patient.
Assess nutritional status of
the patient by measuring
body weight, electrolyte
level and haemoglobin level.
improved.
Bronchodilator medications
can be helpful in improving
bronchodilation and opening
the airway passage.
Anxiety can be reduced and
due to this oxygen demand
can also be reduced.
Stressful condition can
worsen breathlessness in the
patient.
Burden on the diaphragm
can be reduced.
Malnutrition can have
adverse effect on respiratory
mass and strength which can
lead to respiratory failure
(Rogers and Bush, 2015;
Suter et al., 2012).
9
SANDHYA REGMI
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
S00213148
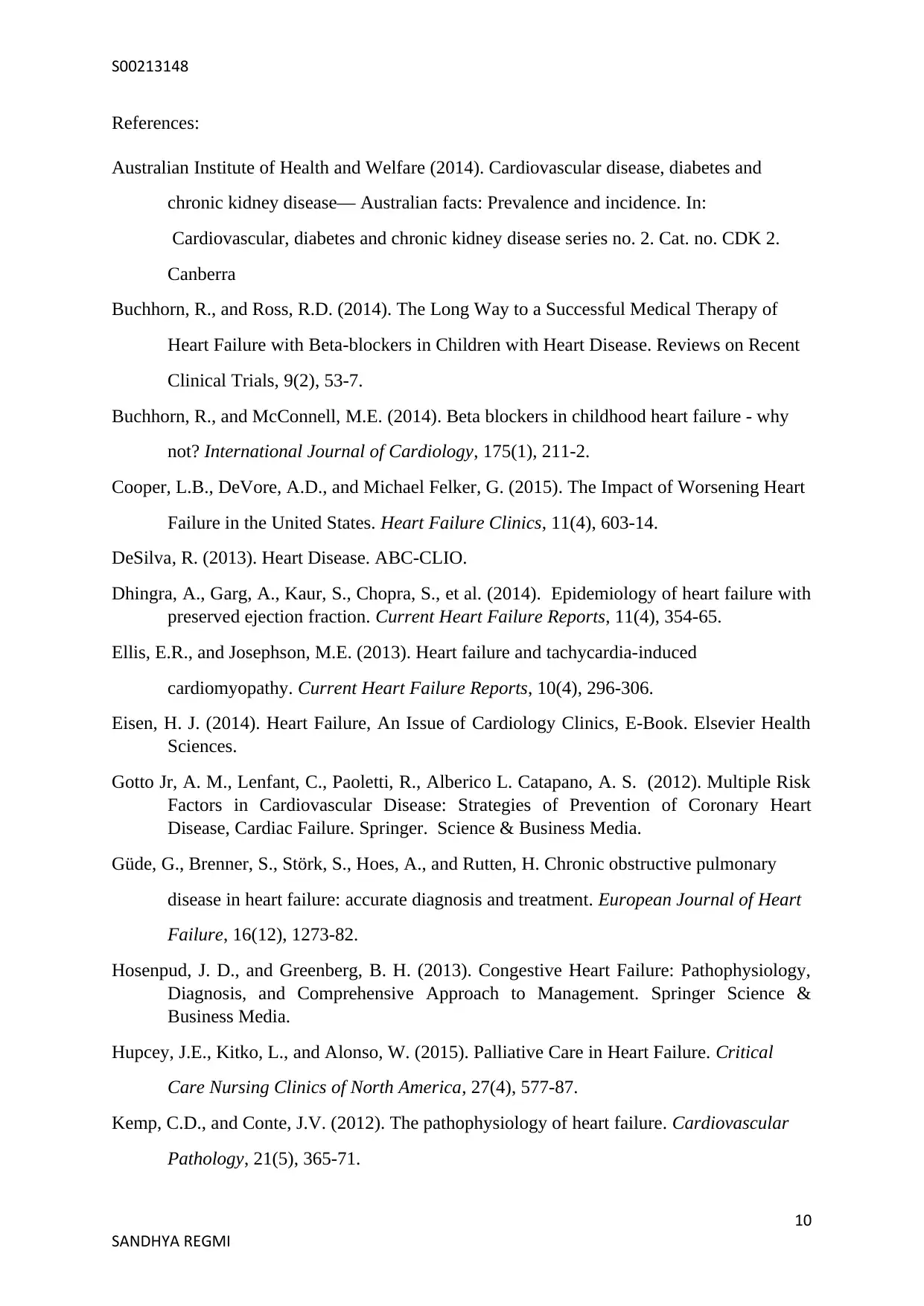
References:
Australian Institute of Health and Welfare (2014). Cardiovascular disease, diabetes and
chronic kidney disease— Australian facts: Prevalence and incidence. In:
Cardiovascular, diabetes and chronic kidney disease series no. 2. Cat. no. CDK 2.
Canberra
Buchhorn, R., and Ross, R.D. (2014). The Long Way to a Successful Medical Therapy of
Heart Failure with Beta-blockers in Children with Heart Disease. Reviews on Recent
Clinical Trials, 9(2), 53-7.
Buchhorn, R., and McConnell, M.E. (2014). Beta blockers in childhood heart failure - why
not? International Journal of Cardiology, 175(1), 211-2.
Cooper, L.B., DeVore, A.D., and Michael Felker, G. (2015). The Impact of Worsening Heart
Failure in the United States. Heart Failure Clinics, 11(4), 603-14.
DeSilva, R. (2013). Heart Disease. ABC-CLIO.
Dhingra, A., Garg, A., Kaur, S., Chopra, S., et al. (2014). Epidemiology of heart failure with
preserved ejection fraction. Current Heart Failure Reports, 11(4), 354-65.
Ellis, E.R., and Josephson, M.E. (2013). Heart failure and tachycardia-induced
cardiomyopathy. Current Heart Failure Reports, 10(4), 296-306.
Eisen, H. J. (2014). Heart Failure, An Issue of Cardiology Clinics, E-Book. Elsevier Health
Sciences.
Gotto Jr, A. M., Lenfant, C., Paoletti, R., Alberico L. Catapano, A. S. (2012). Multiple Risk
Factors in Cardiovascular Disease: Strategies of Prevention of Coronary Heart
Disease, Cardiac Failure. Springer. Science & Business Media.
Güde, G., Brenner, S., Störk, S., Hoes, A., and Rutten, H. Chronic obstructive pulmonary
disease in heart failure: accurate diagnosis and treatment. European Journal of Heart
Failure, 16(12), 1273-82.
Hosenpud, J. D., and Greenberg, B. H. (2013). Congestive Heart Failure: Pathophysiology,
Diagnosis, and Comprehensive Approach to Management. Springer Science &
Business Media.
Hupcey, J.E., Kitko, L., and Alonso, W. (2015). Palliative Care in Heart Failure. Critical
Care Nursing Clinics of North America, 27(4), 577-87.
Kemp, C.D., and Conte, J.V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-71.
10
SANDHYA REGMI
References:
Australian Institute of Health and Welfare (2014). Cardiovascular disease, diabetes and
chronic kidney disease— Australian facts: Prevalence and incidence. In:
Cardiovascular, diabetes and chronic kidney disease series no. 2. Cat. no. CDK 2.
Canberra
Buchhorn, R., and Ross, R.D. (2014). The Long Way to a Successful Medical Therapy of
Heart Failure with Beta-blockers in Children with Heart Disease. Reviews on Recent
Clinical Trials, 9(2), 53-7.
Buchhorn, R., and McConnell, M.E. (2014). Beta blockers in childhood heart failure - why
not? International Journal of Cardiology, 175(1), 211-2.
Cooper, L.B., DeVore, A.D., and Michael Felker, G. (2015). The Impact of Worsening Heart
Failure in the United States. Heart Failure Clinics, 11(4), 603-14.
DeSilva, R. (2013). Heart Disease. ABC-CLIO.
Dhingra, A., Garg, A., Kaur, S., Chopra, S., et al. (2014). Epidemiology of heart failure with
preserved ejection fraction. Current Heart Failure Reports, 11(4), 354-65.
Ellis, E.R., and Josephson, M.E. (2013). Heart failure and tachycardia-induced
cardiomyopathy. Current Heart Failure Reports, 10(4), 296-306.
Eisen, H. J. (2014). Heart Failure, An Issue of Cardiology Clinics, E-Book. Elsevier Health
Sciences.
Gotto Jr, A. M., Lenfant, C., Paoletti, R., Alberico L. Catapano, A. S. (2012). Multiple Risk
Factors in Cardiovascular Disease: Strategies of Prevention of Coronary Heart
Disease, Cardiac Failure. Springer. Science & Business Media.
Güde, G., Brenner, S., Störk, S., Hoes, A., and Rutten, H. Chronic obstructive pulmonary
disease in heart failure: accurate diagnosis and treatment. European Journal of Heart
Failure, 16(12), 1273-82.
Hosenpud, J. D., and Greenberg, B. H. (2013). Congestive Heart Failure: Pathophysiology,
Diagnosis, and Comprehensive Approach to Management. Springer Science &
Business Media.
Hupcey, J.E., Kitko, L., and Alonso, W. (2015). Palliative Care in Heart Failure. Critical
Care Nursing Clinics of North America, 27(4), 577-87.
Kemp, C.D., and Conte, J.V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-71.
10
SANDHYA REGMI
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
S00213148
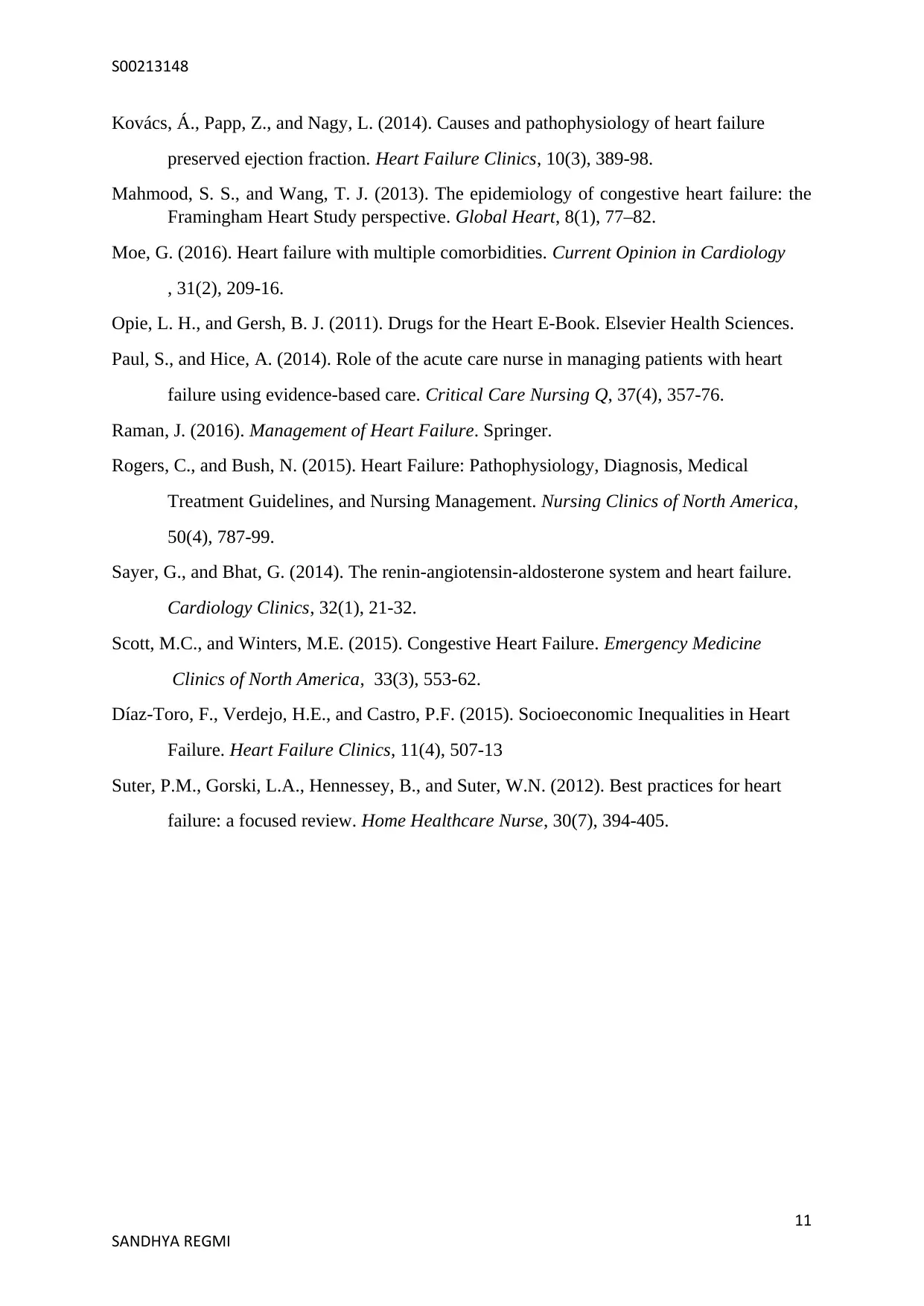
Kovács, Á., Papp, Z., and Nagy, L. (2014). Causes and pathophysiology of heart failure
preserved ejection fraction. Heart Failure Clinics, 10(3), 389-98.
Mahmood, S. S., and Wang, T. J. (2013). The epidemiology of congestive heart failure: the
Framingham Heart Study perspective. Global Heart, 8(1), 77–82.
Moe, G. (2016). Heart failure with multiple comorbidities. Current Opinion in Cardiology
, 31(2), 209-16.
Opie, L. H., and Gersh, B. J. (2011). Drugs for the Heart E-Book. Elsevier Health Sciences.
Paul, S., and Hice, A. (2014). Role of the acute care nurse in managing patients with heart
failure using evidence-based care. Critical Care Nursing Q, 37(4), 357-76.
Raman, J. (2016). Management of Heart Failure. Springer.
Rogers, C., and Bush, N. (2015). Heart Failure: Pathophysiology, Diagnosis, Medical
Treatment Guidelines, and Nursing Management. Nursing Clinics of North America,
50(4), 787-99.
Sayer, G., and Bhat, G. (2014). The renin-angiotensin-aldosterone system and heart failure.
Cardiology Clinics, 32(1), 21-32.
Scott, M.C., and Winters, M.E. (2015). Congestive Heart Failure. Emergency Medicine
Clinics of North America, 33(3), 553-62.
Díaz-Toro, F., Verdejo, H.E., and Castro, P.F. (2015). Socioeconomic Inequalities in Heart
Failure. Heart Failure Clinics, 11(4), 507-13
Suter, P.M., Gorski, L.A., Hennessey, B., and Suter, W.N. (2012). Best practices for heart
failure: a focused review. Home Healthcare Nurse, 30(7), 394-405.
11
SANDHYA REGMI
Kovács, Á., Papp, Z., and Nagy, L. (2014). Causes and pathophysiology of heart failure
preserved ejection fraction. Heart Failure Clinics, 10(3), 389-98.
Mahmood, S. S., and Wang, T. J. (2013). The epidemiology of congestive heart failure: the
Framingham Heart Study perspective. Global Heart, 8(1), 77–82.
Moe, G. (2016). Heart failure with multiple comorbidities. Current Opinion in Cardiology
, 31(2), 209-16.
Opie, L. H., and Gersh, B. J. (2011). Drugs for the Heart E-Book. Elsevier Health Sciences.
Paul, S., and Hice, A. (2014). Role of the acute care nurse in managing patients with heart
failure using evidence-based care. Critical Care Nursing Q, 37(4), 357-76.
Raman, J. (2016). Management of Heart Failure. Springer.
Rogers, C., and Bush, N. (2015). Heart Failure: Pathophysiology, Diagnosis, Medical
Treatment Guidelines, and Nursing Management. Nursing Clinics of North America,
50(4), 787-99.
Sayer, G., and Bhat, G. (2014). The renin-angiotensin-aldosterone system and heart failure.
Cardiology Clinics, 32(1), 21-32.
Scott, M.C., and Winters, M.E. (2015). Congestive Heart Failure. Emergency Medicine
Clinics of North America, 33(3), 553-62.
Díaz-Toro, F., Verdejo, H.E., and Castro, P.F. (2015). Socioeconomic Inequalities in Heart
Failure. Heart Failure Clinics, 11(4), 507-13
Suter, P.M., Gorski, L.A., Hennessey, B., and Suter, W.N. (2012). Best practices for heart
failure: a focused review. Home Healthcare Nurse, 30(7), 394-405.
11
SANDHYA REGMI
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





