Chronic Heart Failure: Pathophysiology, Diagnosis, and Management
VerifiedAdded on 2023/01/17
|12
|3495
|1
Report
AI Summary
This report provides a comprehensive overview of chronic heart failure (CHF), a condition affecting millions worldwide. It begins by defining CHF and discussing its aetiology, including coronary artery disease, heart attacks, and cardiomyopathy, along with the associated risk factors such as obesity and diabetes. The report delves into the pathophysiology of CHF, explaining the body's compensatory mechanisms and the impact on cardiac output. It details clinical manifestations, such as congested lungs, fluid retention, fatigue, and irregular heartbeats, and explores diagnostic methods like echocardiograms, ECGs, and BNP tests. The clinical course and treatment options, including pharmacological interventions like ACE inhibitors and beta-blockers, as well as surgical options like coronary artery bypass graft and heart transplant, are also discussed. The report emphasizes the importance of lifestyle changes, such as smoking cessation and weight management, in managing CHF. Overall, the report offers a thorough understanding of CHF, its causes, progression, and management strategies.
UNIT:
NAME:
DATE:
NAME:
DATE:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction.................................................................................................................................................3
Aetiology.....................................................................................................................................................3
Pathophysiology..........................................................................................................................................4
Clinical Manifestation..................................................................................................................................5
Diagnosis.....................................................................................................................................................6
Clinical Course.............................................................................................................................................7
Treatment....................................................................................................................................................8
Conclusion...................................................................................................................................................9
References.................................................................................................................................................10
Table 1: Types of Chronic Heart Failure.......................................................................................................5
Figure 1: Pathogenesis of CHF.....................................................................................................................7
Introduction.................................................................................................................................................3
Aetiology.....................................................................................................................................................3
Pathophysiology..........................................................................................................................................4
Clinical Manifestation..................................................................................................................................5
Diagnosis.....................................................................................................................................................6
Clinical Course.............................................................................................................................................7
Treatment....................................................................................................................................................8
Conclusion...................................................................................................................................................9
References.................................................................................................................................................10
Table 1: Types of Chronic Heart Failure.......................................................................................................5
Figure 1: Pathogenesis of CHF.....................................................................................................................7
Chronic Heart Failure
Introduction
Chronic heart failure is worldwide pandemic that affects more than 26 million people and
at least 300000 Australians (Taylor, Harrison, Britt, Miller, & Hobbs, 2017). Chronic heart
failure (CHF) is a lifelong limiting condition that is life threatening in the advance stage. CHF,
also known as congestive heart failure is a condition of ongoing inability of a person’s heart to
enough pump blood in all parts of the body and ensure that there is sufficient supply of oxygen
and nutrients (Atherton et al., 2018). The heart is unable to function efficiently and effectively to
enable the pumping of the blood through the body. CHF condition is different from heart attack
and cardiac arrest. Chronic heart failure involve heart muscles unable to pump blood properly
while cardiac arrest refer to heart stopping and having no pulse and heart attack refer to death of
heart muscle as a result of coronary artery blockage (Atherton et al., 2018). CHF is a serious
condition and cannot be cured but can be managed by right treatment for increased life
expectancy and improved quality of patient’s life. The following write-up discusses the chronic
heart failure aetiology, Pathophysiology and incidence of the condition in world and national
level. The write-up also discusses the CHF diagnostic tests, clinical course and prognosis,
treatment options and the public health implications.
Aetiology
Chronic Heart Failure is a condition caused by any condition in the human body that
damages the heart muscle. The first main cause of CHF is coronary artery disease. Coronary
arteries have an important role of supplying blood to the heart muscle. The blockage of coronary
arteries blocks or reduces blood supply in the heart muscle that reduce amount of oxygen and
nutrients supplied in the heart muscle. The heart muscle gets insufficient oxygen and nutrients
that are vital to enhancing the ability of the heart muscle to function properly. The second
aetiology of CHF is heart attack. Sudden blocks of coronary arteries as a result of heart attack
lead to scars in heart’s tissues. The scars in the tissues of the heart decrease how the heart
Introduction
Chronic heart failure is worldwide pandemic that affects more than 26 million people and
at least 300000 Australians (Taylor, Harrison, Britt, Miller, & Hobbs, 2017). Chronic heart
failure (CHF) is a lifelong limiting condition that is life threatening in the advance stage. CHF,
also known as congestive heart failure is a condition of ongoing inability of a person’s heart to
enough pump blood in all parts of the body and ensure that there is sufficient supply of oxygen
and nutrients (Atherton et al., 2018). The heart is unable to function efficiently and effectively to
enable the pumping of the blood through the body. CHF condition is different from heart attack
and cardiac arrest. Chronic heart failure involve heart muscles unable to pump blood properly
while cardiac arrest refer to heart stopping and having no pulse and heart attack refer to death of
heart muscle as a result of coronary artery blockage (Atherton et al., 2018). CHF is a serious
condition and cannot be cured but can be managed by right treatment for increased life
expectancy and improved quality of patient’s life. The following write-up discusses the chronic
heart failure aetiology, Pathophysiology and incidence of the condition in world and national
level. The write-up also discusses the CHF diagnostic tests, clinical course and prognosis,
treatment options and the public health implications.
Aetiology
Chronic Heart Failure is a condition caused by any condition in the human body that
damages the heart muscle. The first main cause of CHF is coronary artery disease. Coronary
arteries have an important role of supplying blood to the heart muscle. The blockage of coronary
arteries blocks or reduces blood supply in the heart muscle that reduce amount of oxygen and
nutrients supplied in the heart muscle. The heart muscle gets insufficient oxygen and nutrients
that are vital to enhancing the ability of the heart muscle to function properly. The second
aetiology of CHF is heart attack. Sudden blocks of coronary arteries as a result of heart attack
lead to scars in heart’s tissues. The scars in the tissues of the heart decrease how the heart
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
effectively pumps. The third cause of CHF is cardiomyopathy. Any damage on the heart muscle
other than blood flow or artery problems causes chronic heart failure. These other factors include
drug side effect or infections. Another cause of CHF is any condition that overworks the heart.
For instance, hypertension, valve disease, kidney disease, or diabetes conditions overwork the
heart muscles that cause CHF. The risk of CHF is increased by the following factors; obesity,
smoking, diabetes type 2, anaemia and amyloidosis.
There are around 30000 cases of CHF that are diagnosed every year in Australia with a
total of 4% of the Australian population living with the condition (Sahle, Owen, Mutowo, Krum,
& Reid, 2016). The rate of death and hospitalization as a result of CHF among Indigenous
Australian is 2-3 times more as compared to Non-Indigenous Australians. The incidence and
prevalence of CHF is more to ageing population as compared to younger people (Vongmany,
Hickman, Lewis, Newton, & Phillips, 2016).
Pathophysiology
The CHF syndromes occur as a result of abnormality in cardiac structure, rhythm,
function, or conduction. The CFC indicates the inability of a person’s heart to maintain enough
delivery of oxygen and a systematic response that attempt to compensate the inadequate oxygen
delivery. The cardiac output is impacted and the body expectation of oxygen delivery is not met.
CHF is caused by myocardial infarction, hypertension and amyloidosis that directly adversely
affect the heart muscles (Sager et al., 2016). The cardiac output is determined by the heart rate
and stroke volume. The stoke volume is determined by the volume of blood that enter the left
ventricle (preload), contractility, and blood flow from left ventricle (afterload). The heart work as
dynamic pump and depend on it inherent properties and what is pumped in and what must be
pumped against. Reduced contractility and impaired ventricular filling results to increased
systolic volume and decreased end diastolic stroke volume respectively. The reduced cardiac
output cause several changes in the heart and the whole body. One of the changes is in the
arterial blood pressure falling. This change dissimulates baroreceptors that are located in the
carotid sinus which is linked to nucleus tactus solitarii. This increases sympathetic activity that
release catecholamines in a person’s blood stream. The binding to apha-1 receptors lead to
arterial vasoconstriction that enables to restore blood pressure and has consequent effects of
increasing total peripheral resistance that increase the heart workload (Ul Haq, Wong, & Hare,
other than blood flow or artery problems causes chronic heart failure. These other factors include
drug side effect or infections. Another cause of CHF is any condition that overworks the heart.
For instance, hypertension, valve disease, kidney disease, or diabetes conditions overwork the
heart muscles that cause CHF. The risk of CHF is increased by the following factors; obesity,
smoking, diabetes type 2, anaemia and amyloidosis.
There are around 30000 cases of CHF that are diagnosed every year in Australia with a
total of 4% of the Australian population living with the condition (Sahle, Owen, Mutowo, Krum,
& Reid, 2016). The rate of death and hospitalization as a result of CHF among Indigenous
Australian is 2-3 times more as compared to Non-Indigenous Australians. The incidence and
prevalence of CHF is more to ageing population as compared to younger people (Vongmany,
Hickman, Lewis, Newton, & Phillips, 2016).
Pathophysiology
The CHF syndromes occur as a result of abnormality in cardiac structure, rhythm,
function, or conduction. The CFC indicates the inability of a person’s heart to maintain enough
delivery of oxygen and a systematic response that attempt to compensate the inadequate oxygen
delivery. The cardiac output is impacted and the body expectation of oxygen delivery is not met.
CHF is caused by myocardial infarction, hypertension and amyloidosis that directly adversely
affect the heart muscles (Sager et al., 2016). The cardiac output is determined by the heart rate
and stroke volume. The stoke volume is determined by the volume of blood that enter the left
ventricle (preload), contractility, and blood flow from left ventricle (afterload). The heart work as
dynamic pump and depend on it inherent properties and what is pumped in and what must be
pumped against. Reduced contractility and impaired ventricular filling results to increased
systolic volume and decreased end diastolic stroke volume respectively. The reduced cardiac
output cause several changes in the heart and the whole body. One of the changes is in the
arterial blood pressure falling. This change dissimulates baroreceptors that are located in the
carotid sinus which is linked to nucleus tactus solitarii. This increases sympathetic activity that
release catecholamines in a person’s blood stream. The binding to apha-1 receptors lead to
arterial vasoconstriction that enables to restore blood pressure and has consequent effects of
increasing total peripheral resistance that increase the heart workload (Ul Haq, Wong, & Hare,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2015). The binding to beta-1 receptors inside the myocardium increased heart rate making
contractions forceful while attempting to have increased cardiac output (Kotecha et al., 2017).
Secondly, increasing sympathetic stimulation cause posterior pituitary secrete antidiuretic
hormone or vasopressin that lead to fluid retention in the kidneys. This leads to increased blood
pressure and volume. The third change is that CHF limits a patient’s kidney ability to dispose
water and sodium that increase edema. The decreased blood flow stimulates the kidneys to
release rennin that catalyse production of angiotensin. Angiotensin cause more vasoconstriction
that increase secretion of aldosterone that promotes fluid and salt retention in the kidneys.
Another change as a result of CHF is reduced perfusion in the skeletal muscles that cause
atrophy of muscles fibres. This lead to weakness, decreased peak strength, and increased
fatigability that contributes to patient’s exercise intolerance.
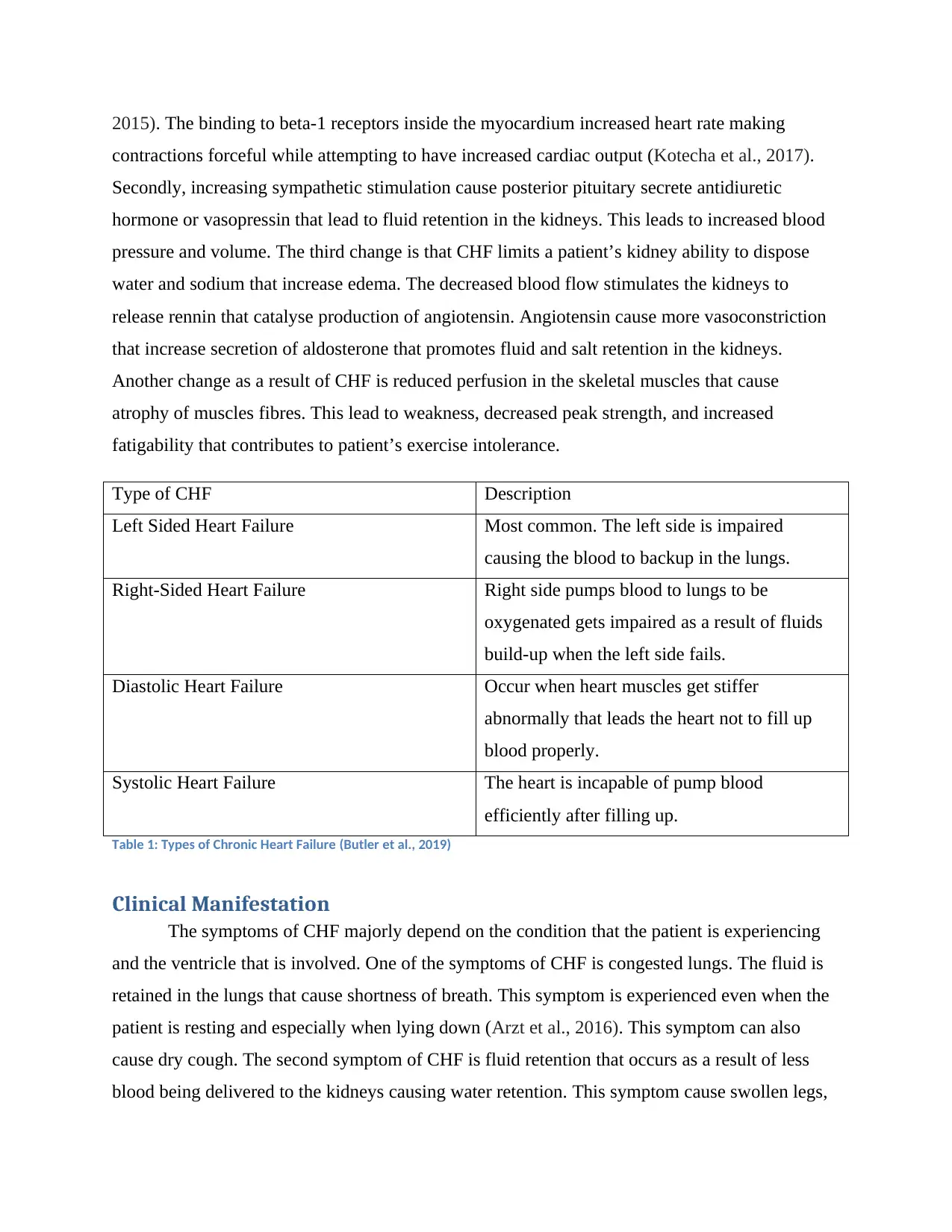
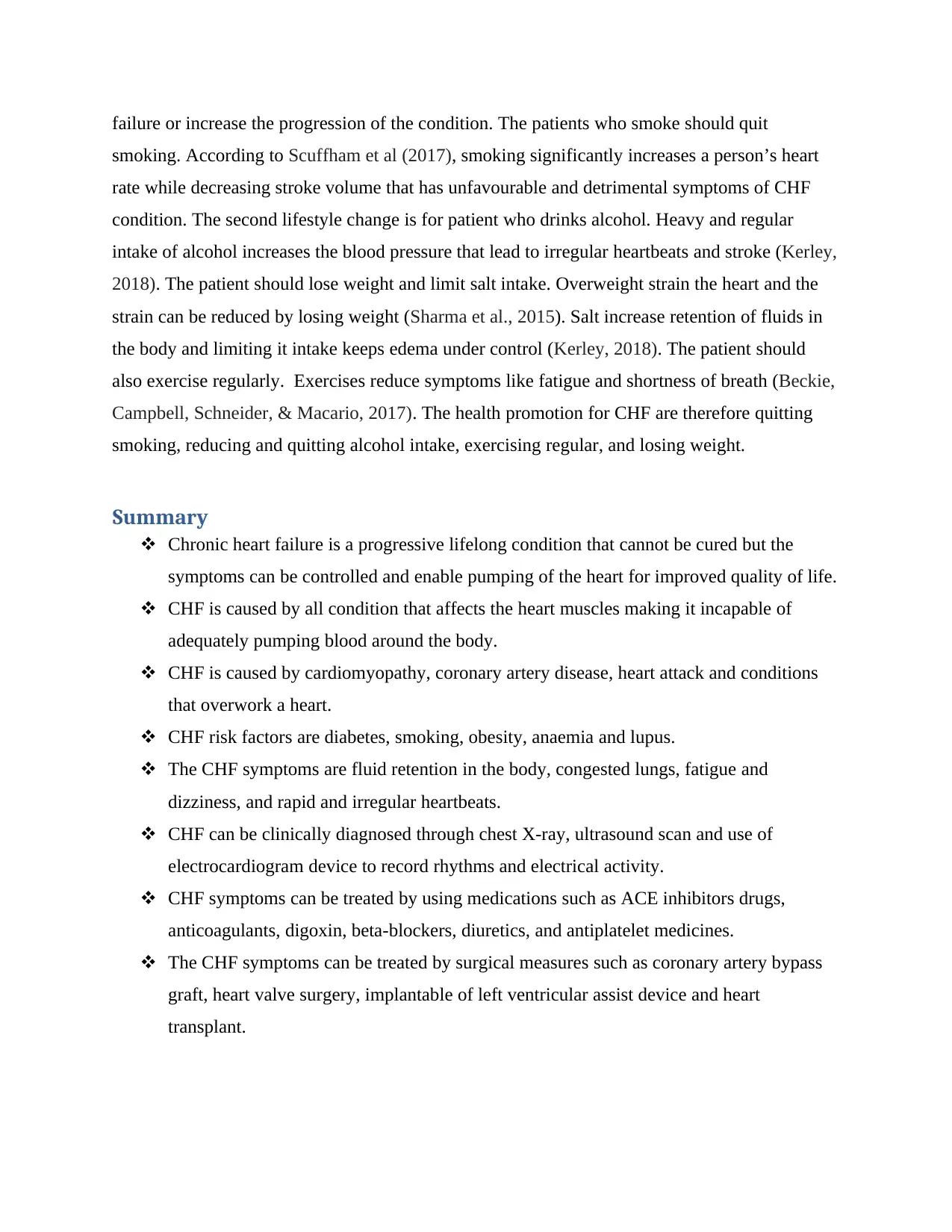
Type of CHF Description
Left Sided Heart Failure Most common. The left side is impaired
causing the blood to backup in the lungs.
Right-Sided Heart Failure Right side pumps blood to lungs to be
oxygenated gets impaired as a result of fluids
build-up when the left side fails.
Diastolic Heart Failure Occur when heart muscles get stiffer
abnormally that leads the heart not to fill up
blood properly.
Systolic Heart Failure The heart is incapable of pump blood
efficiently after filling up.
Table 1: Types of Chronic Heart Failure (Butler et al., 2019)
Clinical Manifestation
The symptoms of CHF majorly depend on the condition that the patient is experiencing
and the ventricle that is involved. One of the symptoms of CHF is congested lungs. The fluid is
retained in the lungs that cause shortness of breath. This symptom is experienced even when the
patient is resting and especially when lying down (Arzt et al., 2016). This symptom can also
cause dry cough. The second symptom of CHF is fluid retention that occurs as a result of less
blood being delivered to the kidneys causing water retention. This symptom cause swollen legs,
contractions forceful while attempting to have increased cardiac output (Kotecha et al., 2017).
Secondly, increasing sympathetic stimulation cause posterior pituitary secrete antidiuretic
hormone or vasopressin that lead to fluid retention in the kidneys. This leads to increased blood
pressure and volume. The third change is that CHF limits a patient’s kidney ability to dispose
water and sodium that increase edema. The decreased blood flow stimulates the kidneys to
release rennin that catalyse production of angiotensin. Angiotensin cause more vasoconstriction
that increase secretion of aldosterone that promotes fluid and salt retention in the kidneys.
Another change as a result of CHF is reduced perfusion in the skeletal muscles that cause
atrophy of muscles fibres. This lead to weakness, decreased peak strength, and increased
fatigability that contributes to patient’s exercise intolerance.
Type of CHF Description
Left Sided Heart Failure Most common. The left side is impaired
causing the blood to backup in the lungs.
Right-Sided Heart Failure Right side pumps blood to lungs to be
oxygenated gets impaired as a result of fluids
build-up when the left side fails.
Diastolic Heart Failure Occur when heart muscles get stiffer
abnormally that leads the heart not to fill up
blood properly.
Systolic Heart Failure The heart is incapable of pump blood
efficiently after filling up.
Table 1: Types of Chronic Heart Failure (Butler et al., 2019)
Clinical Manifestation
The symptoms of CHF majorly depend on the condition that the patient is experiencing
and the ventricle that is involved. One of the symptoms of CHF is congested lungs. The fluid is
retained in the lungs that cause shortness of breath. This symptom is experienced even when the
patient is resting and especially when lying down (Arzt et al., 2016). This symptom can also
cause dry cough. The second symptom of CHF is fluid retention that occurs as a result of less
blood being delivered to the kidneys causing water retention. This symptom cause swollen legs,
ankles and abdomen. The symptoms also cause the patient to gain weight and have increased
urination. According to Butler et al (2019) study, fluid retention is symptom of right-side
ventricle of the heart being affected. The third symptom of CHF is fatigue and dizziness. This
symptom is as a result of inadequate blood reaching the body organs that make patient feel weak.
The inadequate reaching of the blood to the patient brain also causes confusion and dizziness.
Another symptom of heart failure is irregular rapid heartbeats. This symptom is as a result of the
heart trying and counteracting the inadequate blood being pumped with every contraction that
causes the heart to pump quickly.
Diagnosis
The diagnosis is based patent’s physical examination, medical history, and series of tests.
The tests identify the underlying causes of CHF. CHF can be diagnosed in several ways;
echocardiogram (ultrasound), electrocardiogram (ECG), chest X-ray, and brain natriuretic
peptide (BNP) (Atherton et al., 2018). The echocardiogram is an ultrasound can and checks the
patient’s pumping action. This diagnosis measure the percentage of blood that is being pumped
out of left ventricle with every heartbeat (ejection fraction). The electrocardiogram device tests
the electrical activity and rhythms of a person’s heart. This test also reveals damages of heart that
may be from heart attack causing heart failure. The Chest X-ray test shows if the heart has
enlarged and whether there is fluid retention in the lungs. The brain natriuretic peptide measures
NT-proBNP or BNP protein levels in the blood as they elevate when an individual has heart
failure (Kotecha et al., 2017). The BNP get released in the bloodstream when the heart of a
person is overfilled and struggles to work normally.
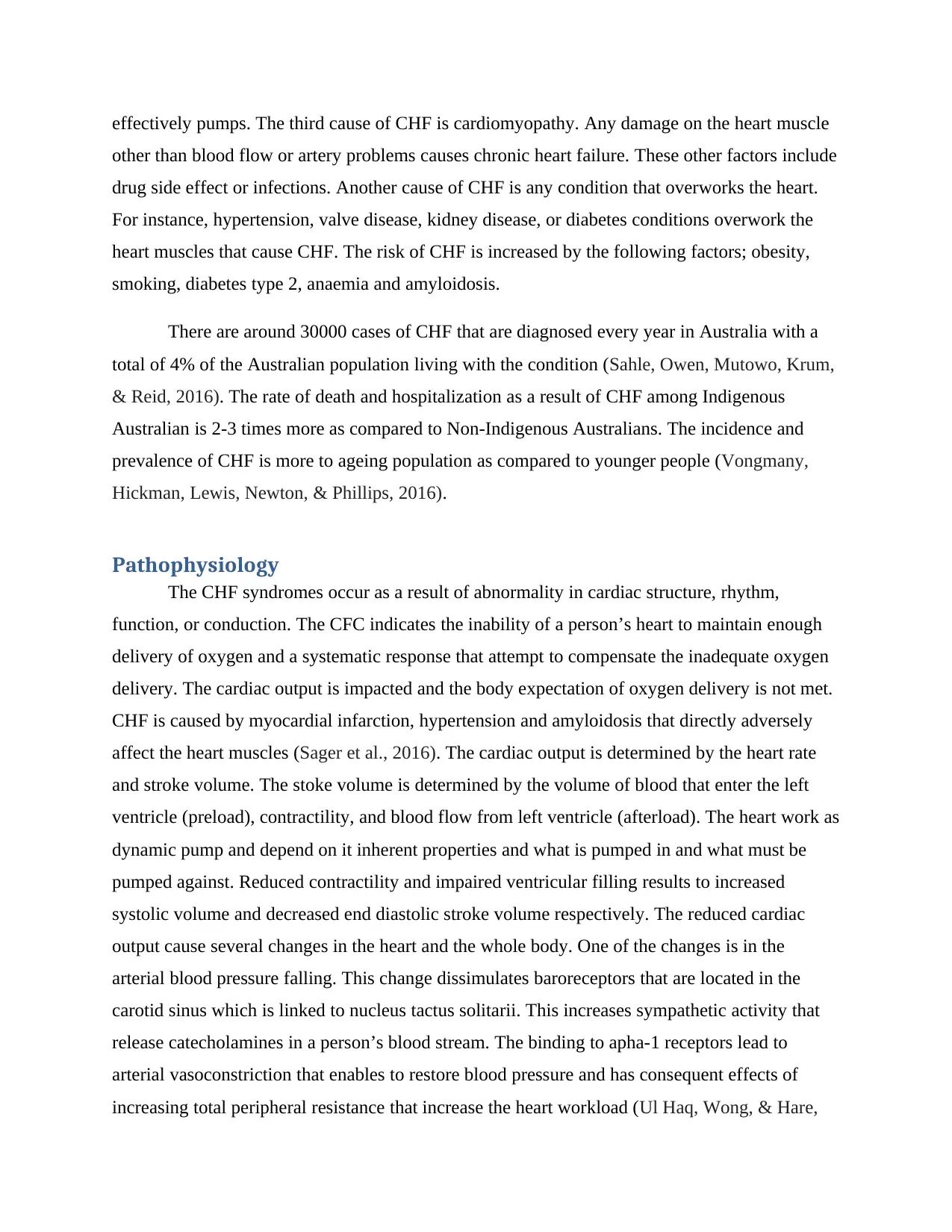
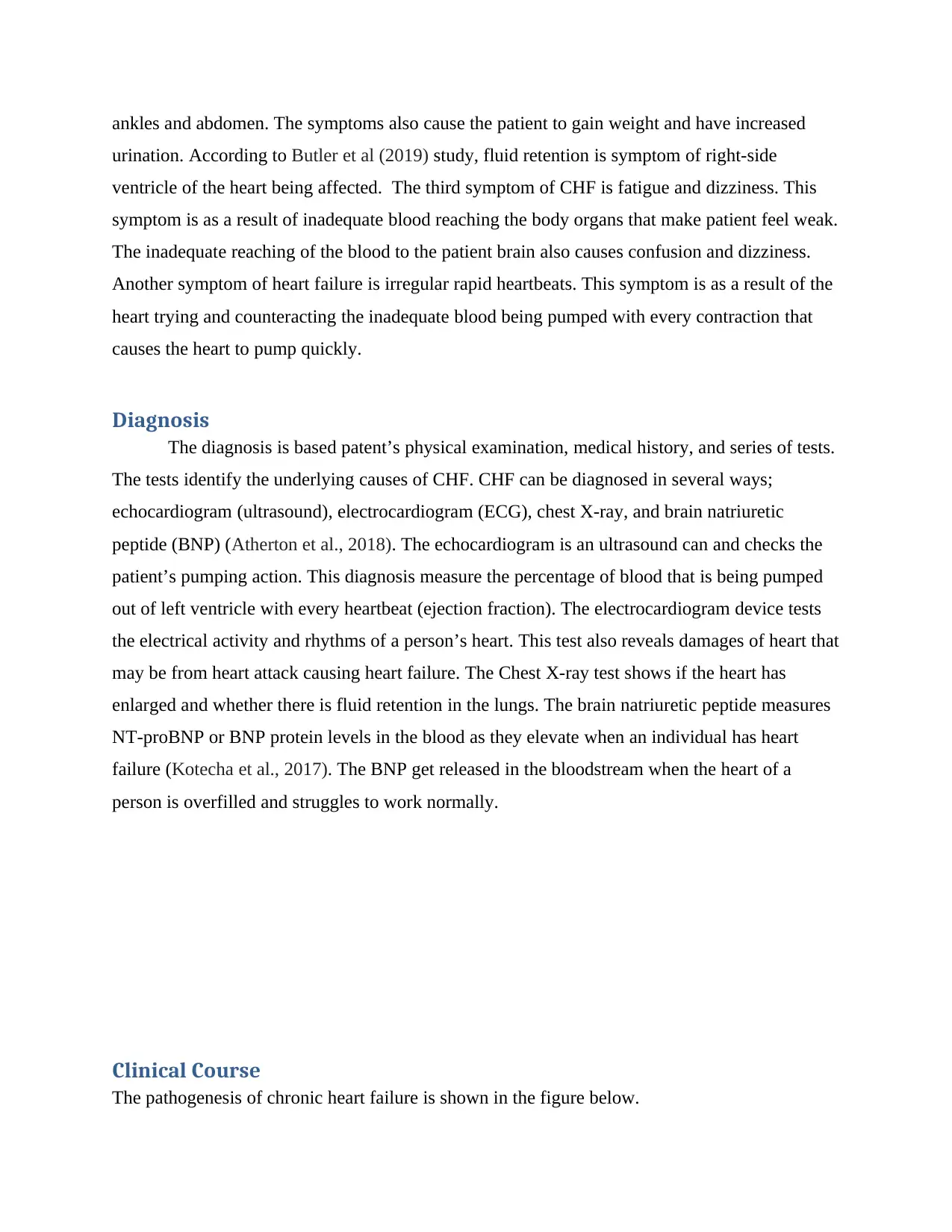
Clinical Course
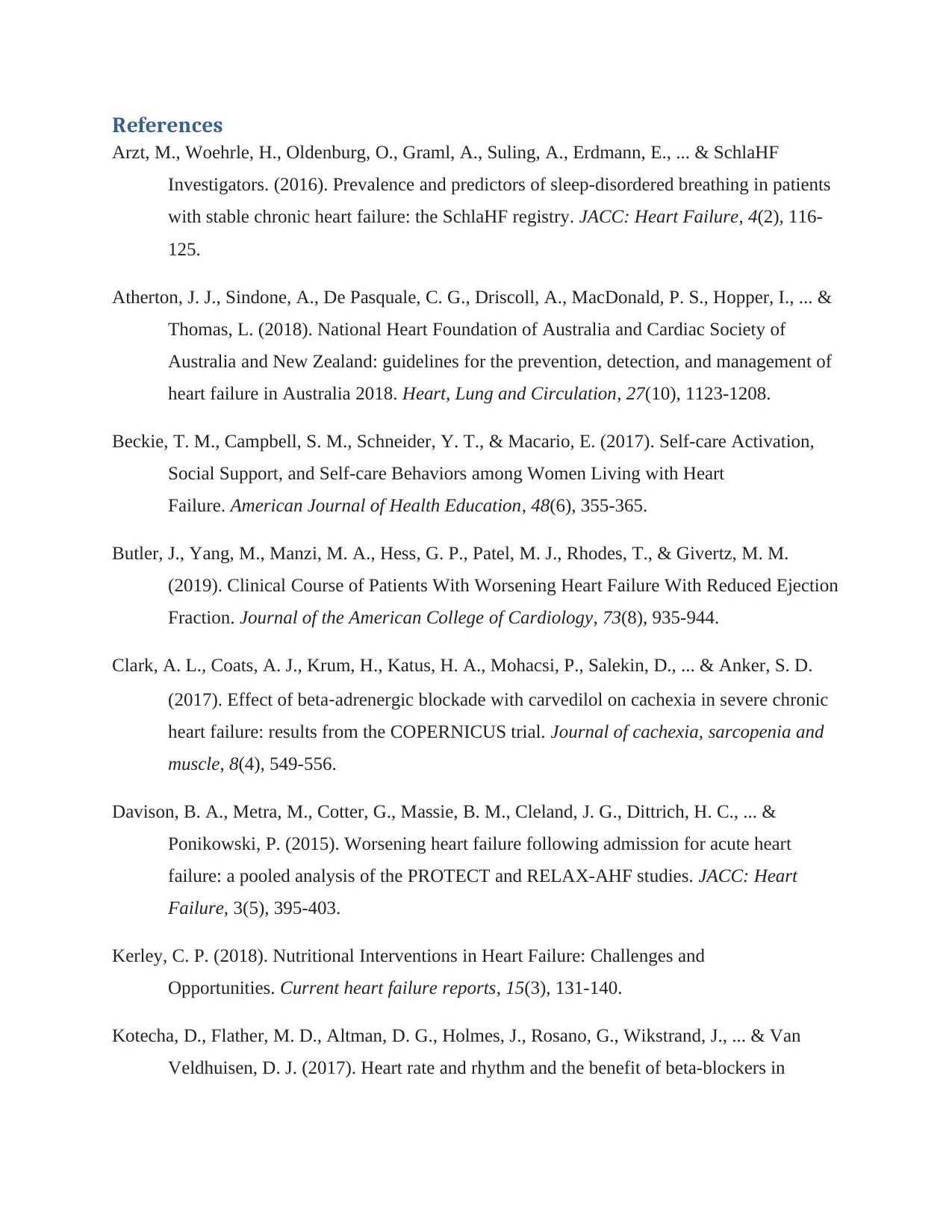
The pathogenesis of chronic heart failure is shown in the figure below.
urination. According to Butler et al (2019) study, fluid retention is symptom of right-side
ventricle of the heart being affected. The third symptom of CHF is fatigue and dizziness. This
symptom is as a result of inadequate blood reaching the body organs that make patient feel weak.
The inadequate reaching of the blood to the patient brain also causes confusion and dizziness.
Another symptom of heart failure is irregular rapid heartbeats. This symptom is as a result of the
heart trying and counteracting the inadequate blood being pumped with every contraction that
causes the heart to pump quickly.
Diagnosis
The diagnosis is based patent’s physical examination, medical history, and series of tests.
The tests identify the underlying causes of CHF. CHF can be diagnosed in several ways;
echocardiogram (ultrasound), electrocardiogram (ECG), chest X-ray, and brain natriuretic
peptide (BNP) (Atherton et al., 2018). The echocardiogram is an ultrasound can and checks the
patient’s pumping action. This diagnosis measure the percentage of blood that is being pumped
out of left ventricle with every heartbeat (ejection fraction). The electrocardiogram device tests
the electrical activity and rhythms of a person’s heart. This test also reveals damages of heart that
may be from heart attack causing heart failure. The Chest X-ray test shows if the heart has
enlarged and whether there is fluid retention in the lungs. The brain natriuretic peptide measures
NT-proBNP or BNP protein levels in the blood as they elevate when an individual has heart
failure (Kotecha et al., 2017). The BNP get released in the bloodstream when the heart of a
person is overfilled and struggles to work normally.
Clinical Course
The pathogenesis of chronic heart failure is shown in the figure below.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
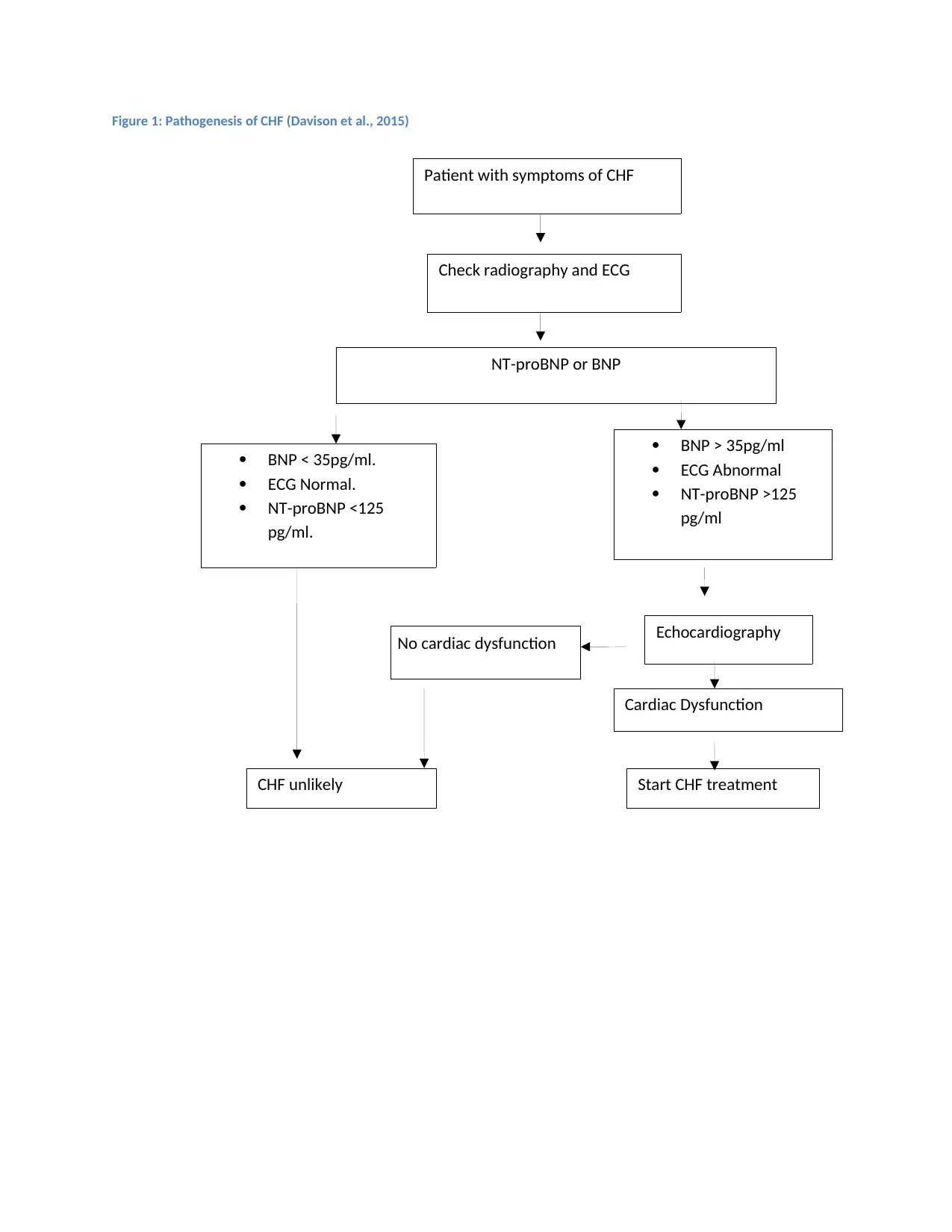
Figure 1: Pathogenesis of CHF (Davison et al., 2015)
NT-proBNP or BNP
BNP < 35pg/ml.
ECG Normal.
NT-proBNP <125
pg/ml.
CHF unlikely
BNP > 35pg/ml
ECG Abnormal
NT-proBNP >125
pg/ml
Start CHF treatment
Echocardiography
Cardiac Dysfunction
No cardiac dysfunction
Patient with symptoms of CHF
Check radiography and ECG
NT-proBNP or BNP
BNP < 35pg/ml.
ECG Normal.
NT-proBNP <125
pg/ml.
CHF unlikely
BNP > 35pg/ml
ECG Abnormal
NT-proBNP >125
pg/ml
Start CHF treatment
Echocardiography
Cardiac Dysfunction
No cardiac dysfunction
Patient with symptoms of CHF
Check radiography and ECG
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
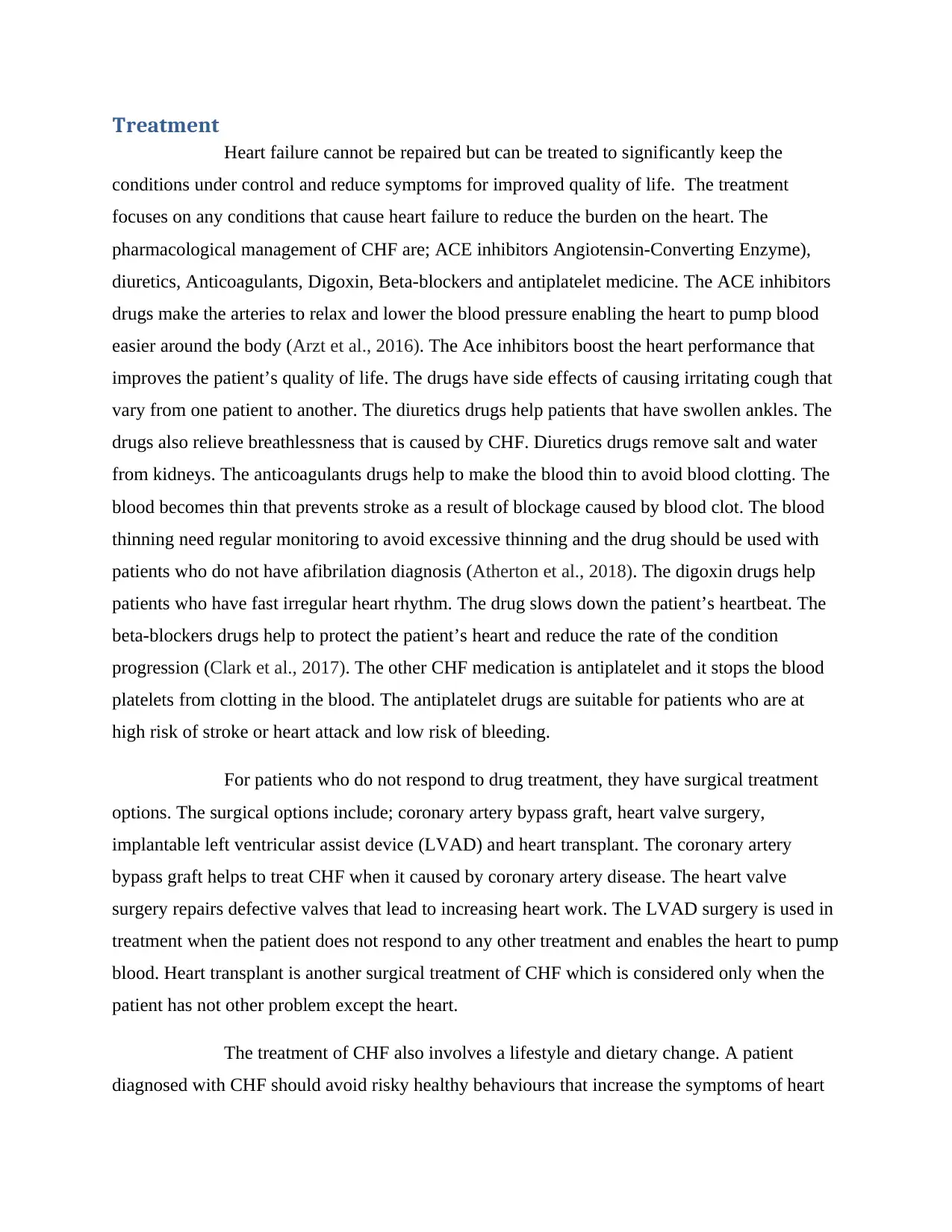
Treatment
Heart failure cannot be repaired but can be treated to significantly keep the
conditions under control and reduce symptoms for improved quality of life. The treatment
focuses on any conditions that cause heart failure to reduce the burden on the heart. The
pharmacological management of CHF are; ACE inhibitors Angiotensin-Converting Enzyme),
diuretics, Anticoagulants, Digoxin, Beta-blockers and antiplatelet medicine. The ACE inhibitors
drugs make the arteries to relax and lower the blood pressure enabling the heart to pump blood
easier around the body (Arzt et al., 2016). The Ace inhibitors boost the heart performance that
improves the patient’s quality of life. The drugs have side effects of causing irritating cough that
vary from one patient to another. The diuretics drugs help patients that have swollen ankles. The
drugs also relieve breathlessness that is caused by CHF. Diuretics drugs remove salt and water
from kidneys. The anticoagulants drugs help to make the blood thin to avoid blood clotting. The
blood becomes thin that prevents stroke as a result of blockage caused by blood clot. The blood
thinning need regular monitoring to avoid excessive thinning and the drug should be used with
patients who do not have afibrilation diagnosis (Atherton et al., 2018). The digoxin drugs help
patients who have fast irregular heart rhythm. The drug slows down the patient’s heartbeat. The
beta-blockers drugs help to protect the patient’s heart and reduce the rate of the condition
progression (Clark et al., 2017). The other CHF medication is antiplatelet and it stops the blood
platelets from clotting in the blood. The antiplatelet drugs are suitable for patients who are at
high risk of stroke or heart attack and low risk of bleeding.
For patients who do not respond to drug treatment, they have surgical treatment
options. The surgical options include; coronary artery bypass graft, heart valve surgery,
implantable left ventricular assist device (LVAD) and heart transplant. The coronary artery
bypass graft helps to treat CHF when it caused by coronary artery disease. The heart valve
surgery repairs defective valves that lead to increasing heart work. The LVAD surgery is used in
treatment when the patient does not respond to any other treatment and enables the heart to pump
blood. Heart transplant is another surgical treatment of CHF which is considered only when the
patient has not other problem except the heart.
The treatment of CHF also involves a lifestyle and dietary change. A patient
diagnosed with CHF should avoid risky healthy behaviours that increase the symptoms of heart
Heart failure cannot be repaired but can be treated to significantly keep the
conditions under control and reduce symptoms for improved quality of life. The treatment
focuses on any conditions that cause heart failure to reduce the burden on the heart. The
pharmacological management of CHF are; ACE inhibitors Angiotensin-Converting Enzyme),
diuretics, Anticoagulants, Digoxin, Beta-blockers and antiplatelet medicine. The ACE inhibitors
drugs make the arteries to relax and lower the blood pressure enabling the heart to pump blood
easier around the body (Arzt et al., 2016). The Ace inhibitors boost the heart performance that
improves the patient’s quality of life. The drugs have side effects of causing irritating cough that
vary from one patient to another. The diuretics drugs help patients that have swollen ankles. The
drugs also relieve breathlessness that is caused by CHF. Diuretics drugs remove salt and water
from kidneys. The anticoagulants drugs help to make the blood thin to avoid blood clotting. The
blood becomes thin that prevents stroke as a result of blockage caused by blood clot. The blood
thinning need regular monitoring to avoid excessive thinning and the drug should be used with
patients who do not have afibrilation diagnosis (Atherton et al., 2018). The digoxin drugs help
patients who have fast irregular heart rhythm. The drug slows down the patient’s heartbeat. The
beta-blockers drugs help to protect the patient’s heart and reduce the rate of the condition
progression (Clark et al., 2017). The other CHF medication is antiplatelet and it stops the blood
platelets from clotting in the blood. The antiplatelet drugs are suitable for patients who are at
high risk of stroke or heart attack and low risk of bleeding.
For patients who do not respond to drug treatment, they have surgical treatment
options. The surgical options include; coronary artery bypass graft, heart valve surgery,
implantable left ventricular assist device (LVAD) and heart transplant. The coronary artery
bypass graft helps to treat CHF when it caused by coronary artery disease. The heart valve
surgery repairs defective valves that lead to increasing heart work. The LVAD surgery is used in
treatment when the patient does not respond to any other treatment and enables the heart to pump
blood. Heart transplant is another surgical treatment of CHF which is considered only when the
patient has not other problem except the heart.
The treatment of CHF also involves a lifestyle and dietary change. A patient
diagnosed with CHF should avoid risky healthy behaviours that increase the symptoms of heart
failure or increase the progression of the condition. The patients who smoke should quit
smoking. According to Scuffham et al (2017), smoking significantly increases a person’s heart
rate while decreasing stroke volume that has unfavourable and detrimental symptoms of CHF
condition. The second lifestyle change is for patient who drinks alcohol. Heavy and regular
intake of alcohol increases the blood pressure that lead to irregular heartbeats and stroke (Kerley,
2018). The patient should lose weight and limit salt intake. Overweight strain the heart and the
strain can be reduced by losing weight (Sharma et al., 2015). Salt increase retention of fluids in
the body and limiting it intake keeps edema under control (Kerley, 2018). The patient should
also exercise regularly. Exercises reduce symptoms like fatigue and shortness of breath (Beckie,
Campbell, Schneider, & Macario, 2017). The health promotion for CHF are therefore quitting
smoking, reducing and quitting alcohol intake, exercising regular, and losing weight.
Summary
Chronic heart failure is a progressive lifelong condition that cannot be cured but the
symptoms can be controlled and enable pumping of the heart for improved quality of life.
CHF is caused by all condition that affects the heart muscles making it incapable of
adequately pumping blood around the body.
CHF is caused by cardiomyopathy, coronary artery disease, heart attack and conditions
that overwork a heart.
CHF risk factors are diabetes, smoking, obesity, anaemia and lupus.
The CHF symptoms are fluid retention in the body, congested lungs, fatigue and
dizziness, and rapid and irregular heartbeats.
CHF can be clinically diagnosed through chest X-ray, ultrasound scan and use of
electrocardiogram device to record rhythms and electrical activity.
CHF symptoms can be treated by using medications such as ACE inhibitors drugs,
anticoagulants, digoxin, beta-blockers, diuretics, and antiplatelet medicines.
The CHF symptoms can be treated by surgical measures such as coronary artery bypass
graft, heart valve surgery, implantable of left ventricular assist device and heart
transplant.
smoking. According to Scuffham et al (2017), smoking significantly increases a person’s heart
rate while decreasing stroke volume that has unfavourable and detrimental symptoms of CHF
condition. The second lifestyle change is for patient who drinks alcohol. Heavy and regular
intake of alcohol increases the blood pressure that lead to irregular heartbeats and stroke (Kerley,
2018). The patient should lose weight and limit salt intake. Overweight strain the heart and the
strain can be reduced by losing weight (Sharma et al., 2015). Salt increase retention of fluids in
the body and limiting it intake keeps edema under control (Kerley, 2018). The patient should
also exercise regularly. Exercises reduce symptoms like fatigue and shortness of breath (Beckie,
Campbell, Schneider, & Macario, 2017). The health promotion for CHF are therefore quitting
smoking, reducing and quitting alcohol intake, exercising regular, and losing weight.
Summary
Chronic heart failure is a progressive lifelong condition that cannot be cured but the
symptoms can be controlled and enable pumping of the heart for improved quality of life.
CHF is caused by all condition that affects the heart muscles making it incapable of
adequately pumping blood around the body.
CHF is caused by cardiomyopathy, coronary artery disease, heart attack and conditions
that overwork a heart.
CHF risk factors are diabetes, smoking, obesity, anaemia and lupus.
The CHF symptoms are fluid retention in the body, congested lungs, fatigue and
dizziness, and rapid and irregular heartbeats.
CHF can be clinically diagnosed through chest X-ray, ultrasound scan and use of
electrocardiogram device to record rhythms and electrical activity.
CHF symptoms can be treated by using medications such as ACE inhibitors drugs,
anticoagulants, digoxin, beta-blockers, diuretics, and antiplatelet medicines.
The CHF symptoms can be treated by surgical measures such as coronary artery bypass
graft, heart valve surgery, implantable of left ventricular assist device and heart
transplant.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

The CHF condition can be prevented and managed by health promotion of lifestyle and
diet such as regular exercising, limiting salt intake, quitting smoking, reducing alcohol
intake and losing weight.
diet such as regular exercising, limiting salt intake, quitting smoking, reducing alcohol
intake and losing weight.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Arzt, M., Woehrle, H., Oldenburg, O., Graml, A., Suling, A., Erdmann, E., ... & SchlaHF
Investigators. (2016). Prevalence and predictors of sleep-disordered breathing in patients
with stable chronic heart failure: the SchlaHF registry. JACC: Heart Failure, 4(2), 116-
125.
Atherton, J. J., Sindone, A., De Pasquale, C. G., Driscoll, A., MacDonald, P. S., Hopper, I., ... &
Thomas, L. (2018). National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand: guidelines for the prevention, detection, and management of
heart failure in Australia 2018. Heart, Lung and Circulation, 27(10), 1123-1208.
Beckie, T. M., Campbell, S. M., Schneider, Y. T., & Macario, E. (2017). Self-care Activation,
Social Support, and Self-care Behaviors among Women Living with Heart
Failure. American Journal of Health Education, 48(6), 355-365.
Butler, J., Yang, M., Manzi, M. A., Hess, G. P., Patel, M. J., Rhodes, T., & Givertz, M. M.
(2019). Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection
Fraction. Journal of the American College of Cardiology, 73(8), 935-944.
Clark, A. L., Coats, A. J., Krum, H., Katus, H. A., Mohacsi, P., Salekin, D., ... & Anker, S. D.
(2017). Effect of beta‐adrenergic blockade with carvedilol on cachexia in severe chronic
heart failure: results from the COPERNICUS trial. Journal of cachexia, sarcopenia and
muscle, 8(4), 549-556.
Davison, B. A., Metra, M., Cotter, G., Massie, B. M., Cleland, J. G., Dittrich, H. C., ... &
Ponikowski, P. (2015). Worsening heart failure following admission for acute heart
failure: a pooled analysis of the PROTECT and RELAX-AHF studies. JACC: Heart
Failure, 3(5), 395-403.
Kerley, C. P. (2018). Nutritional Interventions in Heart Failure: Challenges and
Opportunities. Current heart failure reports, 15(3), 131-140.
Kotecha, D., Flather, M. D., Altman, D. G., Holmes, J., Rosano, G., Wikstrand, J., ... & Van
Veldhuisen, D. J. (2017). Heart rate and rhythm and the benefit of beta-blockers in
Arzt, M., Woehrle, H., Oldenburg, O., Graml, A., Suling, A., Erdmann, E., ... & SchlaHF
Investigators. (2016). Prevalence and predictors of sleep-disordered breathing in patients
with stable chronic heart failure: the SchlaHF registry. JACC: Heart Failure, 4(2), 116-
125.
Atherton, J. J., Sindone, A., De Pasquale, C. G., Driscoll, A., MacDonald, P. S., Hopper, I., ... &
Thomas, L. (2018). National Heart Foundation of Australia and Cardiac Society of
Australia and New Zealand: guidelines for the prevention, detection, and management of
heart failure in Australia 2018. Heart, Lung and Circulation, 27(10), 1123-1208.
Beckie, T. M., Campbell, S. M., Schneider, Y. T., & Macario, E. (2017). Self-care Activation,
Social Support, and Self-care Behaviors among Women Living with Heart
Failure. American Journal of Health Education, 48(6), 355-365.
Butler, J., Yang, M., Manzi, M. A., Hess, G. P., Patel, M. J., Rhodes, T., & Givertz, M. M.
(2019). Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection
Fraction. Journal of the American College of Cardiology, 73(8), 935-944.
Clark, A. L., Coats, A. J., Krum, H., Katus, H. A., Mohacsi, P., Salekin, D., ... & Anker, S. D.
(2017). Effect of beta‐adrenergic blockade with carvedilol on cachexia in severe chronic
heart failure: results from the COPERNICUS trial. Journal of cachexia, sarcopenia and
muscle, 8(4), 549-556.
Davison, B. A., Metra, M., Cotter, G., Massie, B. M., Cleland, J. G., Dittrich, H. C., ... &
Ponikowski, P. (2015). Worsening heart failure following admission for acute heart
failure: a pooled analysis of the PROTECT and RELAX-AHF studies. JACC: Heart
Failure, 3(5), 395-403.
Kerley, C. P. (2018). Nutritional Interventions in Heart Failure: Challenges and
Opportunities. Current heart failure reports, 15(3), 131-140.
Kotecha, D., Flather, M. D., Altman, D. G., Holmes, J., Rosano, G., Wikstrand, J., ... & Van
Veldhuisen, D. J. (2017). Heart rate and rhythm and the benefit of beta-blockers in
patients with heart failure. Journal of the American College of Cardiology, 69(24), 2885-
2896.
Sager, H. B., Hulsmans, M., Lavine, K. J., Moreira, M. B., Heidt, T., Courties, G., ... &
Dahlman, J. E. (2016). Proliferation and recruitment contribute to myocardial
macrophage expansion in chronic heart failure. Circulation research, 119(7), 853-864.
Sahle, B. W., Owen, A. J., Mutowo, M. P., Krum, H., & Reid, C. M. (2016). Prevalence of heart
failure in Australia: a systematic review. BMC cardiovascular disorders, 16(1), 32.
Scuffham, P. A., Ball, J., Horowitz, J. D., Wong, C., Newton, P. J., Macdonald, P., ... & Reid, C.
M. (2017). Standard vs. intensified management of heart failure to reduce healthcare
costs: results of a multicentre, randomized controlled trial. European heart
journal, 38(30), 2340-2348.
Sharma, A., Lavie, C. J., Borer, J. S., Vallakati, A., Goel, S., Lopez-Jimenez, F., ... & Lazar, J.
M. (2015). Meta-analysis of the relation of body mass index to all-cause and
cardiovascular mortality and hospitalization in patients with chronic heart failure. The
American journal of cardiology, 115(10), 1428-1434.
Taylor, C. J., Harrison, C., Britt, H., Miller, G., & Hobbs, F. R. (2017). Heart failure and
multimorbidity in Australian general practice. Journal of comorbidity, 7(1), 44-49.
Ul Haq, M. A., Wong, C., & Hare, D. L. (2015). Heart failure with preserved ejection fraction:
an insight into its prevalence, predictors, and implications of early detection. Rev
Cardiovasc Med, 16(1), 20-7.
Vongmany, J., Hickman, L. D., Lewis, J., Newton, P. J., & Phillips, J. L. (2016). Anxiety in
chronic heart failure and the risk of increased hospitalisations and mortality: A systematic
review. European Journal of Cardiovascular Nursing, 15(7), 478-485.
2896.
Sager, H. B., Hulsmans, M., Lavine, K. J., Moreira, M. B., Heidt, T., Courties, G., ... &
Dahlman, J. E. (2016). Proliferation and recruitment contribute to myocardial
macrophage expansion in chronic heart failure. Circulation research, 119(7), 853-864.
Sahle, B. W., Owen, A. J., Mutowo, M. P., Krum, H., & Reid, C. M. (2016). Prevalence of heart
failure in Australia: a systematic review. BMC cardiovascular disorders, 16(1), 32.
Scuffham, P. A., Ball, J., Horowitz, J. D., Wong, C., Newton, P. J., Macdonald, P., ... & Reid, C.
M. (2017). Standard vs. intensified management of heart failure to reduce healthcare
costs: results of a multicentre, randomized controlled trial. European heart
journal, 38(30), 2340-2348.
Sharma, A., Lavie, C. J., Borer, J. S., Vallakati, A., Goel, S., Lopez-Jimenez, F., ... & Lazar, J.
M. (2015). Meta-analysis of the relation of body mass index to all-cause and
cardiovascular mortality and hospitalization in patients with chronic heart failure. The
American journal of cardiology, 115(10), 1428-1434.
Taylor, C. J., Harrison, C., Britt, H., Miller, G., & Hobbs, F. R. (2017). Heart failure and
multimorbidity in Australian general practice. Journal of comorbidity, 7(1), 44-49.
Ul Haq, M. A., Wong, C., & Hare, D. L. (2015). Heart failure with preserved ejection fraction:
an insight into its prevalence, predictors, and implications of early detection. Rev
Cardiovasc Med, 16(1), 20-7.
Vongmany, J., Hickman, L. D., Lewis, J., Newton, P. J., & Phillips, J. L. (2016). Anxiety in
chronic heart failure and the risk of increased hospitalisations and mortality: A systematic
review. European Journal of Cardiovascular Nursing, 15(7), 478-485.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




