Physiology 6: Chronic Kidney Disease, Electrolytes, and Bone Health
VerifiedAdded on 2022/09/26
|6
|1100
|34
Report
AI Summary
This report delves into the physiological effects of chronic kidney disease (CKD), focusing on electrolyte disturbances and bone affection. The kidneys' crucial role in maintaining fluid and electrolyte balance is highlighted, with discussions on how renal failure leads to imbalances such as hyperkalemia, metabolic acidosis, and alterations in calcium, sodium, and phosphate levels. Furthermore, the report examines the impact of CKD on bone health, detailing how impaired kidney function disrupts mineral metabolism and hormone regulation, resulting in conditions like hyperparathyroid bone disease and increased fracture risk. The report cites various research articles and provides visual aids to illustrate the concepts, offering a comprehensive overview of the physiological challenges associated with CKD.

Physiology PAGE \* MERGEFORMAT 6
Physiology
Chronic Kidney Disease Assignment
Author Name
Department
Institution of Affiliation
Author Contact information
Wd count 960
Physiology
Chronic Kidney Disease Assignment
Author Name
Department
Institution of Affiliation
Author Contact information
Wd count 960
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Physiology PAGE \* MERGEFORMAT 6
Outline electrolytes disturbance in renal failure
Figure 1 Photo illustrating kidney of an individual with chronic kidney failure.6.
It has been shown that kidneys have a homeostatic role in regulating fluid and electrolyte
balance in the body. Both chronic and acute infections which may lead to failure in the kidney
performing renal functions can cause several imbalances.3 First, a patient will experience fluid
overload as his or her kidneys are unable to reabsorb as much body fluid as usual.. Renal tubules
are unable to concentrate urine causing a change in the specific gravity from the normal range of
1.010 to 1.030 resulting in fluid overload. The fluid overload contributes towards the
development of multiple electrolyte derangements such as hyperkalemia, metabolic acidosis
(bicarbonate deficiency), hypervolemia, hypocalcemia, and hyperphosphatemia. Generally,
potassium, magnesium and phosphate ions levels in blood will be elevated while else calcium
and sodium ions levels in blood will decrease.2
Outline electrolytes disturbance in renal failure
Figure 1 Photo illustrating kidney of an individual with chronic kidney failure.6.
It has been shown that kidneys have a homeostatic role in regulating fluid and electrolyte
balance in the body. Both chronic and acute infections which may lead to failure in the kidney
performing renal functions can cause several imbalances.3 First, a patient will experience fluid
overload as his or her kidneys are unable to reabsorb as much body fluid as usual.. Renal tubules
are unable to concentrate urine causing a change in the specific gravity from the normal range of
1.010 to 1.030 resulting in fluid overload. The fluid overload contributes towards the
development of multiple electrolyte derangements such as hyperkalemia, metabolic acidosis
(bicarbonate deficiency), hypervolemia, hypocalcemia, and hyperphosphatemia. Generally,
potassium, magnesium and phosphate ions levels in blood will be elevated while else calcium
and sodium ions levels in blood will decrease.2
Physiology PAGE \* MERGEFORMAT 6
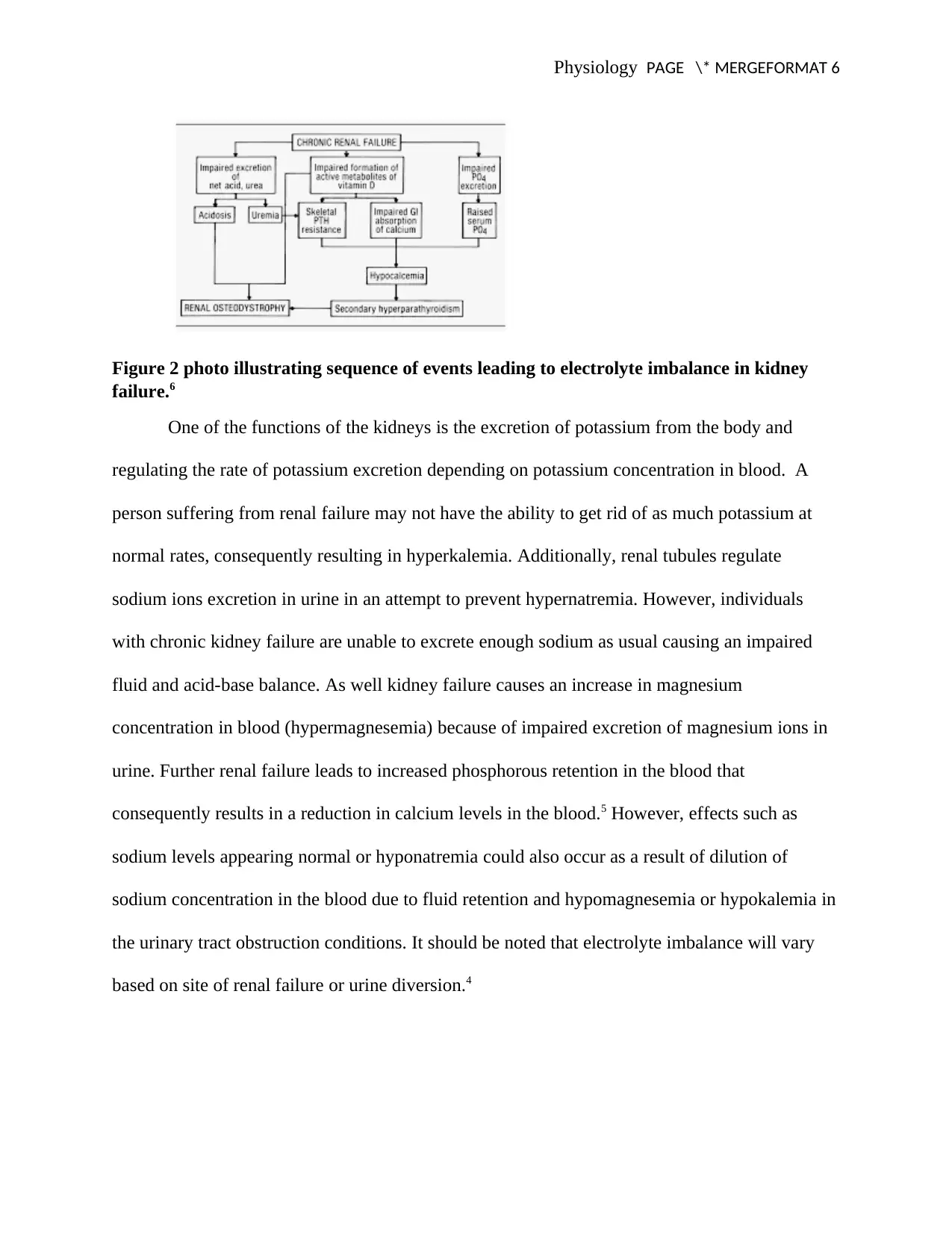
Figure 2 photo illustrating sequence of events leading to electrolyte imbalance in kidney
failure.6
One of the functions of the kidneys is the excretion of potassium from the body and
regulating the rate of potassium excretion depending on potassium concentration in blood. A
person suffering from renal failure may not have the ability to get rid of as much potassium at
normal rates, consequently resulting in hyperkalemia. Additionally, renal tubules regulate
sodium ions excretion in urine in an attempt to prevent hypernatremia. However, individuals
with chronic kidney failure are unable to excrete enough sodium as usual causing an impaired
fluid and acid-base balance. As well kidney failure causes an increase in magnesium
concentration in blood (hypermagnesemia) because of impaired excretion of magnesium ions in
urine. Further renal failure leads to increased phosphorous retention in the blood that
consequently results in a reduction in calcium levels in the blood.5 However, effects such as
sodium levels appearing normal or hyponatremia could also occur as a result of dilution of
sodium concentration in the blood due to fluid retention and hypomagnesemia or hypokalemia in
the urinary tract obstruction conditions. It should be noted that electrolyte imbalance will vary
based on site of renal failure or urine diversion.4
Figure 2 photo illustrating sequence of events leading to electrolyte imbalance in kidney
failure.6
One of the functions of the kidneys is the excretion of potassium from the body and
regulating the rate of potassium excretion depending on potassium concentration in blood. A
person suffering from renal failure may not have the ability to get rid of as much potassium at
normal rates, consequently resulting in hyperkalemia. Additionally, renal tubules regulate
sodium ions excretion in urine in an attempt to prevent hypernatremia. However, individuals
with chronic kidney failure are unable to excrete enough sodium as usual causing an impaired
fluid and acid-base balance. As well kidney failure causes an increase in magnesium
concentration in blood (hypermagnesemia) because of impaired excretion of magnesium ions in
urine. Further renal failure leads to increased phosphorous retention in the blood that
consequently results in a reduction in calcium levels in the blood.5 However, effects such as
sodium levels appearing normal or hyponatremia could also occur as a result of dilution of
sodium concentration in the blood due to fluid retention and hypomagnesemia or hypokalemia in
the urinary tract obstruction conditions. It should be noted that electrolyte imbalance will vary
based on site of renal failure or urine diversion.4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Physiology PAGE \* MERGEFORMAT 6
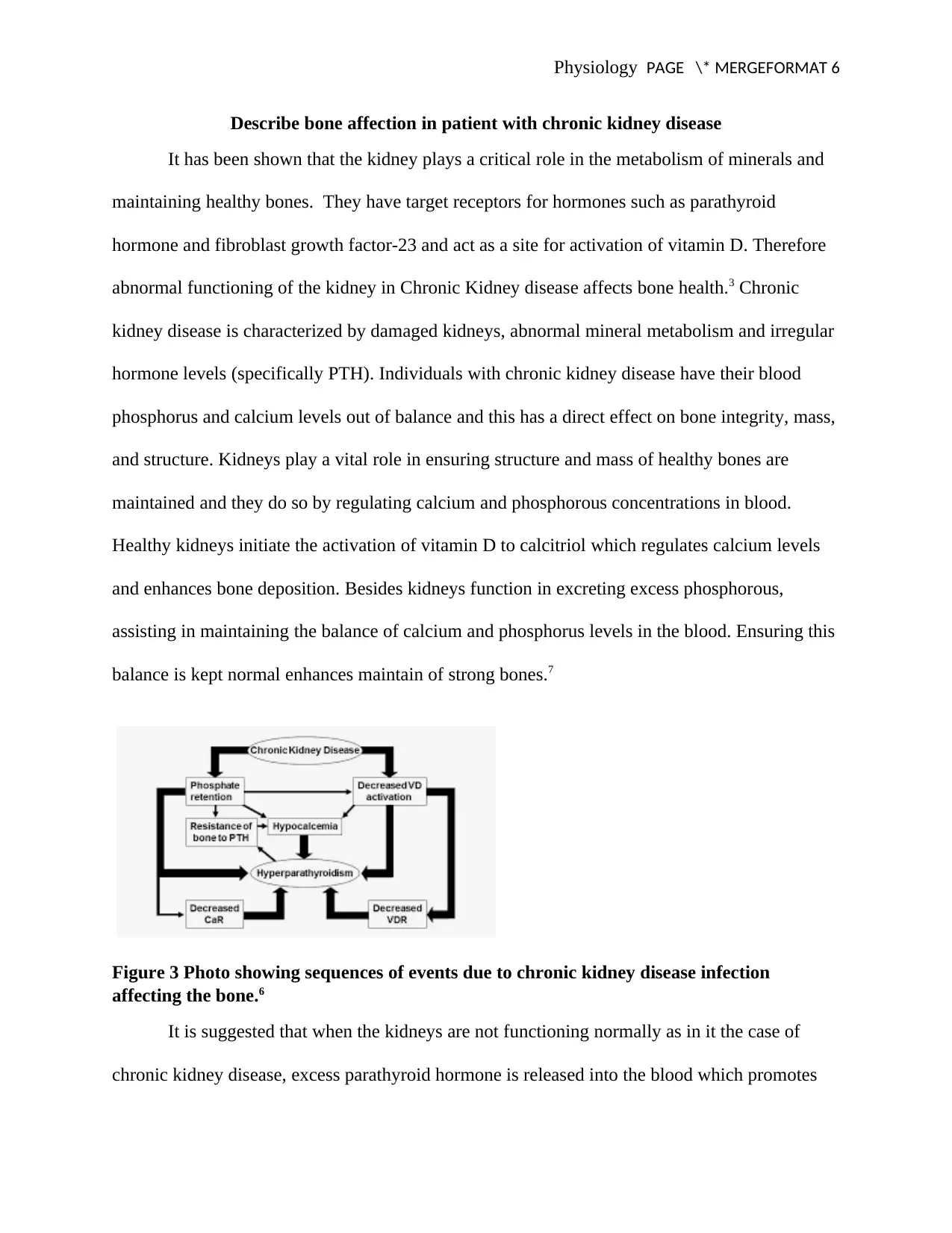
Describe bone affection in patient with chronic kidney disease
It has been shown that the kidney plays a critical role in the metabolism of minerals and
maintaining healthy bones. They have target receptors for hormones such as parathyroid
hormone and fibroblast growth factor-23 and act as a site for activation of vitamin D. Therefore
abnormal functioning of the kidney in Chronic Kidney disease affects bone health.3 Chronic
kidney disease is characterized by damaged kidneys, abnormal mineral metabolism and irregular
hormone levels (specifically PTH). Individuals with chronic kidney disease have their blood
phosphorus and calcium levels out of balance and this has a direct effect on bone integrity, mass,
and structure. Kidneys play a vital role in ensuring structure and mass of healthy bones are
maintained and they do so by regulating calcium and phosphorous concentrations in blood.
Healthy kidneys initiate the activation of vitamin D to calcitriol which regulates calcium levels
and enhances bone deposition. Besides kidneys function in excreting excess phosphorous,
assisting in maintaining the balance of calcium and phosphorus levels in the blood. Ensuring this
balance is kept normal enhances maintain of strong bones.7
Figure 3 Photo showing sequences of events due to chronic kidney disease infection
affecting the bone.6
It is suggested that when the kidneys are not functioning normally as in it the case of
chronic kidney disease, excess parathyroid hormone is released into the blood which promotes
Describe bone affection in patient with chronic kidney disease
It has been shown that the kidney plays a critical role in the metabolism of minerals and
maintaining healthy bones. They have target receptors for hormones such as parathyroid
hormone and fibroblast growth factor-23 and act as a site for activation of vitamin D. Therefore
abnormal functioning of the kidney in Chronic Kidney disease affects bone health.3 Chronic
kidney disease is characterized by damaged kidneys, abnormal mineral metabolism and irregular
hormone levels (specifically PTH). Individuals with chronic kidney disease have their blood
phosphorus and calcium levels out of balance and this has a direct effect on bone integrity, mass,
and structure. Kidneys play a vital role in ensuring structure and mass of healthy bones are
maintained and they do so by regulating calcium and phosphorous concentrations in blood.
Healthy kidneys initiate the activation of vitamin D to calcitriol which regulates calcium levels
and enhances bone deposition. Besides kidneys function in excreting excess phosphorous,
assisting in maintaining the balance of calcium and phosphorus levels in the blood. Ensuring this
balance is kept normal enhances maintain of strong bones.7
Figure 3 Photo showing sequences of events due to chronic kidney disease infection
affecting the bone.6
It is suggested that when the kidneys are not functioning normally as in it the case of
chronic kidney disease, excess parathyroid hormone is released into the blood which promotes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Physiology PAGE \* MERGEFORMAT 6
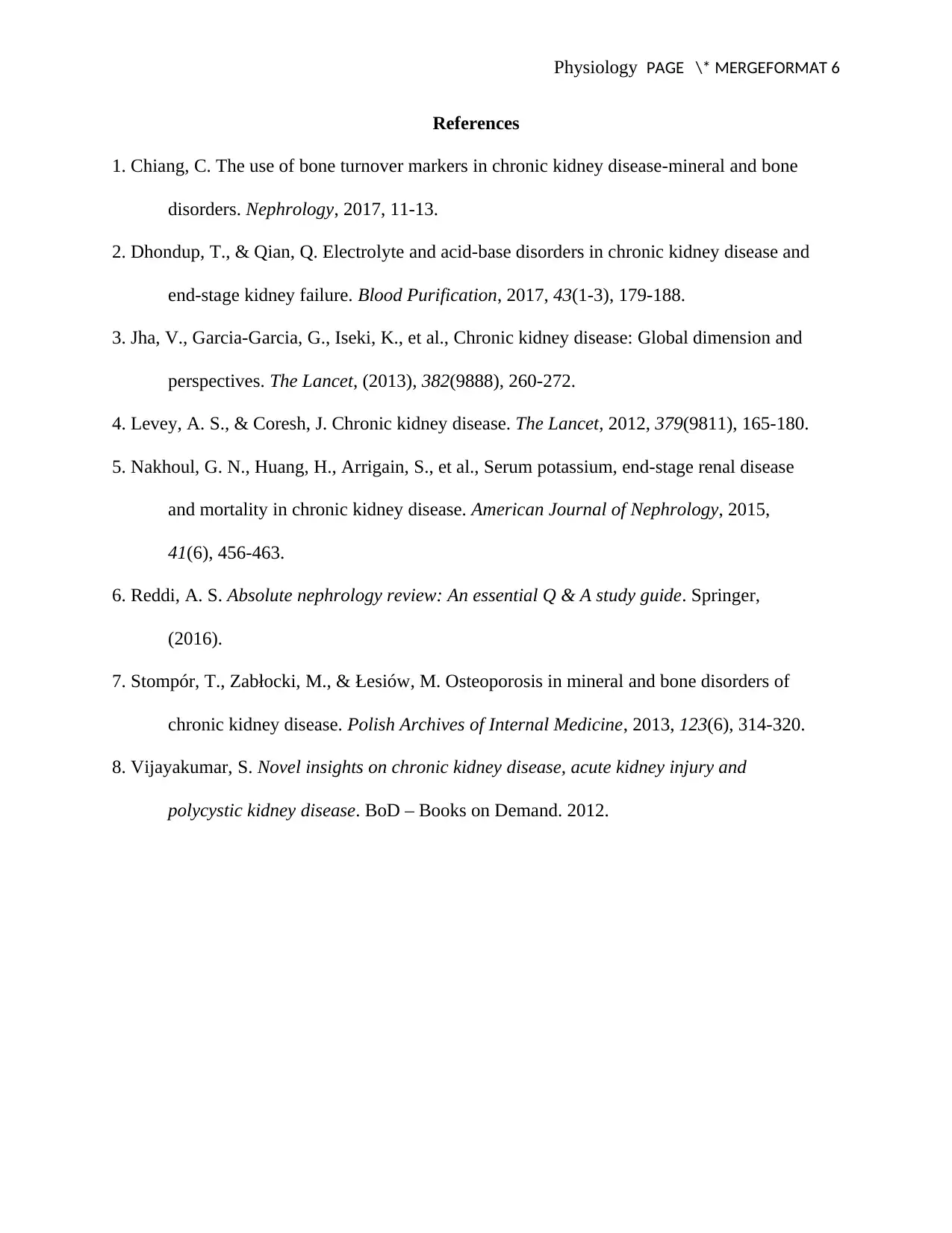
the decalcification of bones. The kidney cannot also promote the activation of vitamin D to
calcitriol. Decreased calcitriol levels in the blood will lead to an imbalance of calcium levels.
Moreover, the damaged kidney is unable to regulate levels of phosphorous in blood as required.4
Therefore, the excess phosphorus promotes calcium removal from bones hence weakening them.
During Acute kidney disease the parathyroid gland is overstimulated to release a parathyroid
hormone into the blood which promotes the removal of calcium from bones and increasing
calcium levels in the blood. This process works to restore the calcium and phosphorous levels
balance, but as a consequence, it deprives bones of essential calcium. As a consequence having
chronic kidney disease, this effects give rise to pathological disorders of the bone such as
hyperparathyroid bone disease that is characterized with cortical bone thinning, low bone
formation, osteoid matrix, raised abnormal trabecular bone, decreased bone strength and
increased vulnerability of the bone to develop fractures.1
Figure 4 X-ray photo showing bone appearance during extreme sclerosis due chronic
kidney disease.8
the decalcification of bones. The kidney cannot also promote the activation of vitamin D to
calcitriol. Decreased calcitriol levels in the blood will lead to an imbalance of calcium levels.
Moreover, the damaged kidney is unable to regulate levels of phosphorous in blood as required.4
Therefore, the excess phosphorus promotes calcium removal from bones hence weakening them.
During Acute kidney disease the parathyroid gland is overstimulated to release a parathyroid
hormone into the blood which promotes the removal of calcium from bones and increasing
calcium levels in the blood. This process works to restore the calcium and phosphorous levels
balance, but as a consequence, it deprives bones of essential calcium. As a consequence having
chronic kidney disease, this effects give rise to pathological disorders of the bone such as
hyperparathyroid bone disease that is characterized with cortical bone thinning, low bone
formation, osteoid matrix, raised abnormal trabecular bone, decreased bone strength and
increased vulnerability of the bone to develop fractures.1
Figure 4 X-ray photo showing bone appearance during extreme sclerosis due chronic
kidney disease.8
Physiology PAGE \* MERGEFORMAT 6
References
1. Chiang, C. The use of bone turnover markers in chronic kidney disease-mineral and bone
disorders. Nephrology, 2017, 11-13.
2. Dhondup, T., & Qian, Q. Electrolyte and acid-base disorders in chronic kidney disease and
end-stage kidney failure. Blood Purification, 2017, 43(1-3), 179-188.
3. Jha, V., Garcia-Garcia, G., Iseki, K., et al., Chronic kidney disease: Global dimension and
perspectives. The Lancet, (2013), 382(9888), 260-272.
4. Levey, A. S., & Coresh, J. Chronic kidney disease. The Lancet, 2012, 379(9811), 165-180.
5. Nakhoul, G. N., Huang, H., Arrigain, S., et al., Serum potassium, end-stage renal disease
and mortality in chronic kidney disease. American Journal of Nephrology, 2015,
41(6), 456-463.
6. Reddi, A. S. Absolute nephrology review: An essential Q & A study guide. Springer,
(2016).
7. Stompór, T., Zabłocki, M., & Łesiów, M. Osteoporosis in mineral and bone disorders of
chronic kidney disease. Polish Archives of Internal Medicine, 2013, 123(6), 314-320.
8. Vijayakumar, S. Novel insights on chronic kidney disease, acute kidney injury and
polycystic kidney disease. BoD – Books on Demand. 2012.
References
1. Chiang, C. The use of bone turnover markers in chronic kidney disease-mineral and bone
disorders. Nephrology, 2017, 11-13.
2. Dhondup, T., & Qian, Q. Electrolyte and acid-base disorders in chronic kidney disease and
end-stage kidney failure. Blood Purification, 2017, 43(1-3), 179-188.
3. Jha, V., Garcia-Garcia, G., Iseki, K., et al., Chronic kidney disease: Global dimension and
perspectives. The Lancet, (2013), 382(9888), 260-272.
4. Levey, A. S., & Coresh, J. Chronic kidney disease. The Lancet, 2012, 379(9811), 165-180.
5. Nakhoul, G. N., Huang, H., Arrigain, S., et al., Serum potassium, end-stage renal disease
and mortality in chronic kidney disease. American Journal of Nephrology, 2015,
41(6), 456-463.
6. Reddi, A. S. Absolute nephrology review: An essential Q & A study guide. Springer,
(2016).
7. Stompór, T., Zabłocki, M., & Łesiów, M. Osteoporosis in mineral and bone disorders of
chronic kidney disease. Polish Archives of Internal Medicine, 2013, 123(6), 314-320.
8. Vijayakumar, S. Novel insights on chronic kidney disease, acute kidney injury and
polycystic kidney disease. BoD – Books on Demand. 2012.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





